Abstract
Introduction
This retrospective cohort study compared clinical and radiographic outcomes of endodontic treatment performed in immature non-vital permanent teeth, by apexification (calcium hydroxide or apical barrier with Mineral Trioxide Aggregate (MTA)), versus revascularization.
Methods
A comprehensive chart review was performed to obtain a cohort of sequential previously completed cases with recalls. Clinical and radiographic data were collected for 31 treated teeth (19 revascularization and 12 apexification) with an average follow up time of 17 months and a recall rate of 63%. Tooth survival, success rate, and adverse events were analyzed. Changes in radiographic root length, width and area were quantified.
Results
The majority of treated teeth survived throughout the study period with 30/31 (97%) teeth surviving (18/19 (95%) revascularization, 12/12 apexification). Most cases were also clinically successful with 27/31 (87%) meeting criteria for success, (15/19 (78%) revascularization and 12/12 apexification; non-significant difference). A greater incidence of adverse events was observed in the revascularization group (8/19 (42%) versus 1/12 (11%) in apexification (Risk Ratio= 5.1, p=0.04, 95%CI (0.719, 35.48)). Although more revascularization cases than apexification cases demonstrated an increase in radiographic root area and width, the effect was not statistically significant.
Conclusion
In this study, revascularization was not superior to other apexification techniques in either clinical or radiographic outcomes. Studies with large subject cohorts, and long follow up periods are needed to evaluate outcomes of revascularization and apexification, while accounting for important co-variants relevant to clinical success.
Introduction
The treatment of infected immature permanent teeth is the one of the more challenging procedures in endodontics (1, 2). Such teeth normally have very wide canals, thin dentinal walls, and open apices, which presents difficulty to the clinician in instrumentation, working length determination, and control of irrigants and obturation materials. Importantly, immature teeth are more prone to fracture, so even cases with ideal endodontic treatment have a poor long-term prognosis (1-3).
Long-term treatment with intracanal calcium hydroxide (Ca(OH)2) was historically the treatment of choice for necrotic teeth with open apices (4). However, this treatment option requires patients to attend multiple clinic visits over an extended period of time, with treatments regularly extending over 6 months (5, 6). Also, long-term use of Ca(OH)2 may change the physical properties of dentin and ultimately reduce the root strength (5). An alternative to apexification with Ca(OH)2, is placement of an apical barrier using a material such as Mineral Trioxide Aggregate (MTA) (7, 8). Treatment with MTA apexification produces comparably favorable outcomes to long term Ca(OH)2 treatment, in regard to resolution of symptoms and periapical pathology (9-12). Despite the advantage of fewer number of visits, MTA apexification does not appear to improve root strength or produce thickening or lengthening of root canal walls (3).
More recently, a clinical protocol for revascularization was introduced, in which, after a modified disinfection technique, bleeding is stimulated from the periapical tissues and a blood clot is formed within the canal, which is hypothesized to provide a scaffold, growth factors, and possibly stem cells, which support the growth of tissues into the canal space and continued root formation (13-17). Multiple case reports and case series have demonstrated increased root width and/or length after some variation of revascularization treatment procedure (13, 14, 18-23). Animal studies (24-26) have shown that the nature of hard tissues formed in the canal of vascularized immature teeth is heterogeneous mineralized tissue resembling cementum or bone and soft tissues that appear more similar to periodontal ligament than to pulp. On the other hand, some human studies (27, 28) have shown pulpal like tissue after revascularization procedure; however, others (29-31) have shown cementum, bone and/or periodontal ligament like tissue. The reason for the variability in intracanal tissues formed is not understood at this point, but may relate to the unpredictable survival of apical pulpal tissues, apical papilla, or Hertwig's epithelial root sheath in the setting of inflammation and trauma.
Despite the seemingly clear potential benefit of continued root development, there is currently not sufficient evidence to support the claim that revascularization treatment has superior treatment outcomes relative to traditional apexification, or to measure the success rate of achieving continued root development after revascularization. The purpose of this pilot retrospective cohort study was to evaluate and compare the clinical and radiographic outcomes of apexification (Ca(OH)2 and MTA apical barrier) and revascularization treatment of immature non-vital permanent teeth, and to begin to identify patient factors that may be important to achieving successful outcomes in these cases.
Material and Methods
Subjects
The study protocol was approved by the Institutional Review Board at the New York University School of Medicine (approved 8/20/12). A query of the Dentrix database at NYU College of Dentistry was performed to identify dental charts of pediatric patients aged 6-16 who received endodontic treatment between 9/2008-9/2011. Due to inconsistencies in treatment codes used for revascularization and apexification procedures, we queried for all endodontic treatment codes including Unspecified Endo Procedure (D3999), codes relating to apexification (D3351, D3352, D3353), codes related to standard non-surgical endodontic procedures (D3330, D3320, D3310). Codes related to pulpal regeneration had not been instituted, and were not queried. A total of 338 potential cases were identified for screening (Figure 1).
Figure 1.
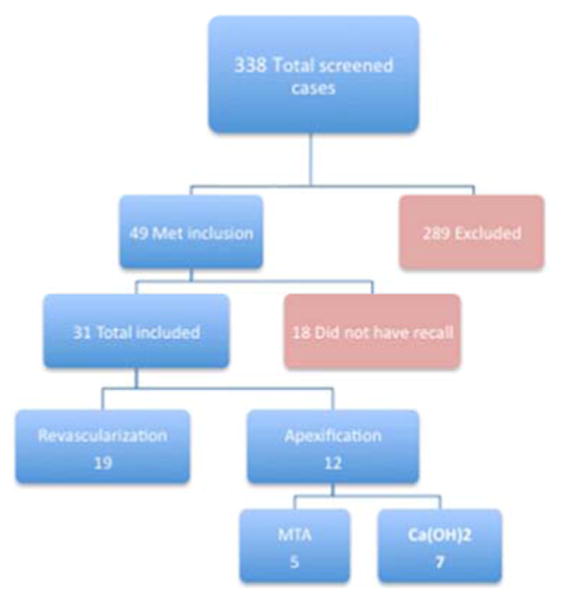
Flow chart showing number of cases screened and excluded for not meeting study criteria, or for not having documentation of a recall visit.
The clinical records identified in the data base query were reviewed for eligibility for the study using specific inclusion and exclusion criteria. To be eligible for the study the subject must have been age 6-16 at the time of treatment, have a permanent tooth in need of endodontic treatment that could be classified as calcium hydroxide apexification, MTA apexification, or revascularization, and the tooth should be immature (Stage 1-4 according to Cvek's criteria (2)). Finally, the endodontic treatment must have been completed and the final restoration placed, and at least a 3 month recall should be documented in the patient record. Exclusion criteria included missing or grossly incomplete clinical records.
Data Extraction
Cases identified that met the inclusion/exclusion criteria were assigned a research subject number, and data was extracted from their clinical record. Data collection was accomplished using a standardized electronic form designed to collect information related to subject demographic features, contributory etiology (including history and type of trauma), pre-operative signs and symptoms, number of clinical visits, details on clinical treatment, follow up visits and treatments, and any other treatment rendered on the treated tooth. The final data set was exported to Excel and saved on a secure server for analysis. All radiographs related to study cases were collected and stored in a digital format on a secure server.
Clinical Outcomes
The primary outcomes of clinical treatment evaluated were survival, clinical success, and adverse events. Survival was defined as the tooth remaining present in the arch throughout the study period. Clinical success was defined as a tooth that survived and also did not require another endodontic intervention during the recall period. Although healing of periapical radiolucencies was assessed, we did not include radiographic outcomes as part of definition of clinical success because of the inherent difficulty in assessing periapical pathology radiographically in immature teeth.
Adverse events were defined as any event involving the treated tooth, during treatment or during the follow up period that would negatively impact the patient or guardian or require additional clinic visits. We specifically looked for documentation of intra-operative or post-operative pain, flare ups, staining and/or internal bleaching, reinfection, and fracture. We characterized adverse events as:
Mild: No need for additional endodontic treatment.
Moderate: Further endodontic treatment indicated after event (e.g. pain, swelling, or sinus tract was present).
Severe: Tooth was or needed to be extracted.
Radiographic Outcomes and Analysis
Pre-operative radiographs were evaluated by study investigators for the presence or absence of periapical radiolucency, stage of root development and signs of resorption. The assessment of periapical pathology is challenging in immature teeth. However, the cases were reviewed by independent investigators (AA and JG) and consensus was obtained on questionable cases with the help of an additional study investigator (LL). Post-operative radiographs were assessed for the presence or absence of periapical radiolucency, signs of resorption, intracanal calcification, and apical calcification. In cases when a periapical radiolucency was present pre-op, the post-op the images were assessed to determine if the radiolucency appeared larger or smaller on follow up.
For quantification of changes in radiographic root dimensions, we quantified changes in radiographic root area, root length, and root width. First, the pre-operative and postoperative images of digitized radiographs were opened in the Image J software program (NIH, USA). Pre-operative and final recall radiographs were aligned using the TurboReg plug-in to minimize any dimensional changes that occurred as a result of angulation differences at the time of image taken. In some cases the differences in angulation made quantification of radiographic changes impossible. In this instance, the case was either dropped or an alternative film (usually an earlier follow up radiograph) that was better aligned was used in the analysis.
After alignment, the area, length and width were measured. The polygon tool was used to measure the total root area using the mesial and distal CEJ as the most coronal aspect of the outline. The total canal area (TCA) was measured using the most coronal aspect of the canal area at the level of the CEJ. A modified protocol was used to measure posterior teeth, where only the distal canal was quantified. The “straight-line” tool of TurboReg was used to measure the root length. The measurements were done as a straight line from the CEJ to the midpoint of the apex of the root from both the mesial and distal, and then both measurements were averaged to obtain the total root length. Width was measured a three levels of the root that were determined relative to the previously determined length (50%, 66%, and 80%). The measurements obtained at each of the widths were averaged to determine the overall percentage change in width. Every measurement was completed in duplicate and averaged to reduce variability.
Clinical Protocol
Although the AAE has recently published clinical guidelines for revascularization (32), there is little evidence available to support specific aspects of treatment including medicaments and irrigants used. As this was a retrospective study spanning a number of years, a specific clinical protocol was not implemented prior to performing the treatments. Residents under the supervision of endodontic faculty performed all cases. Revascularization cases were done in multiple visits (2 to 5). In all case, the first appointment consisted of local anesthesia, rubber dam isolation, access cavity, working length determination, and irrigation with varying concentrations of sodium hypochlorite, chlorhexidine and/or EDTA with minimal or no instrumentation. Intra-canal medicaments (triple antibiotic (ciprofloxacin, metronidazole, minocycline), double antibiotic (ciprofloxacin, metronidazole) and/or Ca(OH)2) were used for varying durations. The last appointment before completion of revascularization consisted of local anesthesia, rubber dam isolation, irrigation to remove remaining intra-canal medication and laceration of the apical tissue in an attempt to induce bleeding into the canal, although this was not achieved in all cases. Finally, all cases used MTA placed at approximately the level of cementoenamel junction, followed by placement of a resin bonded restoration.
In the Ca(OH)2 APEX treatment, standard irrigants and instrumentation were utilized, followed by the placement of Ca(OH)2 in the canal, sometimes until an apical barrier formed, although not in all cases. The cases were ultimately obturated with gutta percha and AH Plus sealer (Dentsply, York, PA) and a resin-bonded restoration was used to restore the tooth. Cases were always completed in multiple visits (3 to 5). For the MTA APEX treatment, standard irrigants and instrumentation were utilized, and Ca(OH)2 was used as an intra-canal medication between visits for varying durations. All cases were completed in multiple visits (2 to 5). MTA was placed in the apical portion of the canal, and the remaining canal system was obturated with thermoplasticized gutta percha and AH Plus sealer.
Statistical Analysis
The data was imported from Excel into Stata (Stata/SE 11.2 for Mac, StataCorp College Station, TX) for analysis. Appropriate descriptive statistics were calculated including mean, median, and standard errors. In testing for differences between groups, a T-test was used to evaluate continuous variables, while dichotomous variables was evaluated using Fisher's exact test, and ordinal variables were tested using the Mann Whitney U Test. Risk measurements were made by calculating either risk ratios or risk differences. Statistical significance was set at p≤0.05.
Results
An initial query of the NYUCD clinical database system resulted in a total of 338 charts, identifying endodontic procedures completed in children aged 6-16 over a three year period. After applying the inclusion and exclusion criteria, only 49 cases met the study criteria (Figure 1). Of the possible 49 cases to be included, 18 cases did not have documentation of a recall visit (recall rate = 63%) and were excluded. Of the 31 cases with recall, 19 were treated with revascularization treatment (REVASC), 7 with Ca(OH)2 apexification, and 5 with MTA apexification. Due to a small number of cases in the apexification groups (Ca(OH)2 and MTA), we consolidated them in one group (APEX) with 12 APEX cases.
Baseline Study Population Characteristics
The demographics and baseline clinical characteristics of the study population were evaluated to assess comparability of the two groups (REVASC VS APEX). Age, gender, significant medical history, tooth type, etiology, preoperative signs and symptoms of pain, pre-operative periapical radiolucency, and the follow up period time were comparable between groups (Table 1). The stage of root development differed significantly between the REVASC and APEX groups with more immature teeth in the revascularization group (Table 1). Trauma was by far the predominant contributory etiology in both groups with 15 cases (78%) in the REVASC group and 9 cases (75%) in APEX. Although not significantly different, a greater proportion of cases of severe trauma, including avulsion and intrusion occurred in the REVASC group. The average follow up period was 15 and 22 months in the REVASC and APEX groups respectively, with the study representing a total follow up time of 44.6 patient years.
Table 1. Patient demographics and baseline characteristics.
| Variable | Revascularization N=19 |
Apexification N=12 |
P-value |
|---|---|---|---|
| Male Sex – no. (%)* | 9 (47) | 8 (73) | |
| Age –years | 8.8 ± 1.6 | 9.8 ± 2.0 | |
| Anterior Tooth no. (%) | 19 (100) | 9 (75) | |
| S&S of Pain Present- no./total no. (%) | 11/14 (78) | 9/10 (90) | |
| Etiology- no./total no. (%) | |||
| Trauma | 15/19 (79) | 9/12 (75) | |
| Severe Trauma** | 6/11 (55) | 1/8 (13) | 0.4 |
| Caries | 1/19 (5) | 3/12 (25) | |
| Anatomic | 3/19 (16)*** | 0/19 | |
| Periapical Radiolucency Present no./total no. (%) | 8/19 (42) | 8/12 (67) | |
| Stage of Root Development | 2.8 ± 1.0 | 3.9 ± 0.3 | 0.001# |
| Follow up Period- Months | 14.5 ± 8.5 | 21.8 ± 12.0 | 0.06 |
Continuous and ordinal variables presented as mean ± standard deviation.
Missing data reflected by the changing denominators. Continuous variables evaluated using t-test, dichotomous variables evaluated using Fisher's exact test. Only p-values approaching statistical significance are shown.
Each tooth is treated as an individual case for analysis. However, some patients had multiple teeth included in the study: 1 patient had 4 teeth, 1 patient had 3 teeth, and 2 patients had 2 teeth involved.
Severe trauma category includes avulsion and intrusion. Other trauma (i.e. not severe) includes enamel-dentin fracture, dentin- pulp fracture, and luxation. The denominator changed due to missing data about the type of trauma.
Trauma to primary teeth affected the development of permanent teeth.
Statistically significant difference using Mann Whitney U Test.
Clinical Outcomes
As it is not known whether teeth treated by a revascularization procedure have comparable clinical outcomes to teeth treated by conventional apexification procedures, we assessed frequency of survival, clinical success and adverse events. During the follow up period, most cases (30/31, 97%) survived (Table 2; (18/19 (95%) revascularization, 12/12 (100%) apexification). The one extraction was in the REVASC group, when the child re-traumatized the treated tooth, fracturing it (this case was previously published (30)). Most cases were also clinically successful during the follow up period (27/31, 87%), with 15 successful cases (79%) in the REVASC group and 12 successful cases (100%) in APEX group (Table 2). Of the 4 (21%) teeth in the REVASC group that were identified as clinical failures, 3 became re-infected and required another endodontic treatment and 1 was re-traumatized as previously described. The between group differences in survival and clinical success were non-significant (Risk difference for clinical success= 0.21, 95% CI (0.03,0.39), p= 0.09; Risk difference for non-survival = 0.05, 95% CI (-0.15, 0.04), p=0.4).
Table 2. Outcome rate.
| Variable | Revascularization N (19) |
Apexification N (12) |
|---|---|---|
| Survival no. (%) | 18 (95) | 12 (100) |
| Clinical success no. (%) | 15 (79) | 12 (100) |
| All adverse events no. (%) | 8 (42) | 1 (8) |
As not much has been reported about adverse events in teeth treated by REVASC or APEX we also determined the incidence of adverse events in this study population (Table 2). We found a greater incidence of adverse events in the REVASC group with, 8 cases (42%) documenting adverse events versus 1 case (11%) in the APEX group. In the REVASC group, 4 of the cases (50%) were classified as mild, 3 cases (38%) as moderate, and 1 case (12%) as a severe adverse events (Table 3). The one adverse event case in the APEX group was classified as a mild adverse event. When comparing the risk for an adverse event occurrence, we found a slightly higher risk for adverse event occurring after revascularization treatment then apexification treatment (Risk Ratio= 5.1, p=0.04, 95% CI (0.719, 35.48)). It should be noted that teeth in which adverse events occurred had a more immature stage of root development then teeth without an adverse event incidence (Table 3).
Table 3. Type of Adverse Events.
| Variable | Class | Root Stage# | AE Type | Time (Month) | Tx |
|---|---|---|---|---|---|
| REVASC | Mild | 2 | Staining | 15 | Internal Bleaching |
| 3 | Staining | 12 | None | ||
| 1 | Pain* | 23 | None | ||
| 2 | Retraumatized | 8 | Restorative | ||
| Mod | 2 | Reinfection | 9 | Endodontic | |
| 1 | Reinfection | 8 | Endodontic | ||
| 2 | Reinfection | 37 | Endodontic | ||
| Severe | 4 | Fracture | 25 | Extraction | |
| APEX | Mild | 4 | Retraumatized | 12 | Restorative |
Intraoperative pain
Root stage was more immature in AE teeth than non-AE (p=0.002 with Mann-Whitney U Test).
Quantitative Radiographic Outcomes
In order to determine whether there was a difference in the radiographic measures of root area, length and width between REVASC and APEX treatment cases, we quantified the radiographic changes between the pre-operative radiograph and last follow radiograph in each case. As these radiographs were not collected in a standardized manner, they were occasionally not comparable despite attempting to correct discrepancies with software (Image J). Thus, 3 cases from the APEX group and 2 cases from the REVASC group were dropped. We also dropped 2 cases from the REVASC group due extensive intracanal calcification, making measurements of root width and area impossible. Given these constraints, for radiographic outcomes, the average follow up time per group was 15.4 +/- 9.0 months (n=8) for APEX and 15.5 +/- 10.4 months (n=15) for REVASC.
In terms of radiographic changes, the width measurement demonstrated the largest difference between treatment groups (1.4 +/- 3.2% for APEX vs 10.2 +/- 4.0% for REVASC Figure 2). However, none of the measured radiographic outcomes, width, length or radiographic root area (RRA), were statistically different between groups using a t-test. Cases treated by REVASC generally showed greater absolute change and greater variability in the width and RRA measurements (again not statistically different), but not length (example case with width increase shown in Fig 3 J-L). In fact, one of the cases treated by APEX showed the largest increase in root length (Fig 3 A-C shows an example of a APEX case treated by CaOH2, that demonstrated an increased root length after treatment). In terms of clinical significance, assuming a 20% increase in length or width is clinically meaningful, 3/15 (20%) REVASC cases would have met this threshold in RRA measurement, 1/8 (12.5%) APEX case did in length measurement, and 3/15 (20%) REVASC cases would have met this threshold in width measurement. In total, the number of REVASC cases with a clinically significant change (20% or greater) in any of the radiographic outcomes measured (RRA, width, or length) was 4/15 (27%) versus 1/15 of the APEX group (two cases demonstrated changes in both RRA and width; no significant difference between groups with Fisher's exact test).
Figure 2.
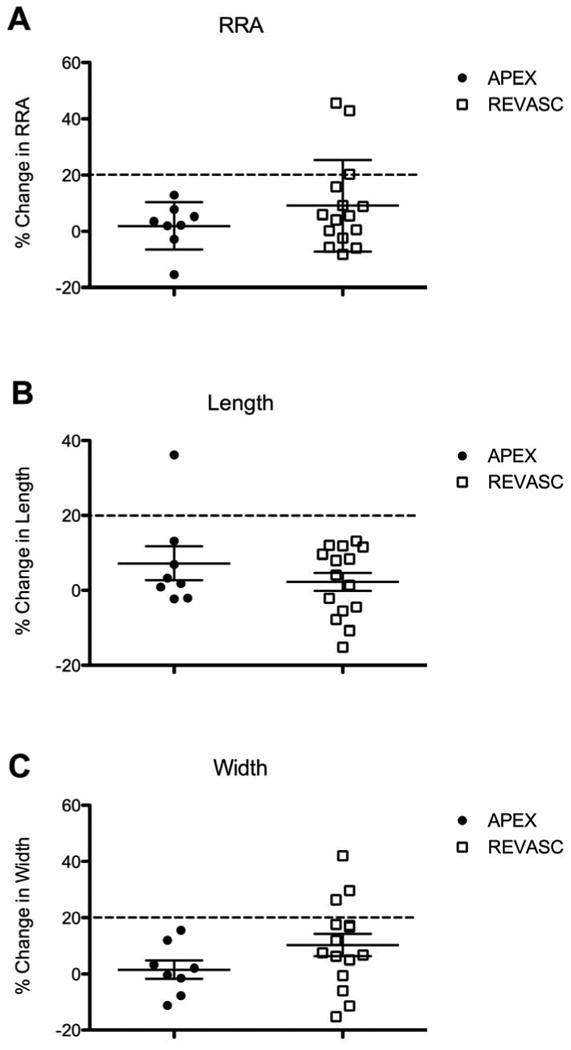
Scatter plots demonstrating the percentage change in measured radiographic root dimensions. Each dot represents an individual treated tooth with closed circles from APEX cases and open squares from REVASC cases. The middle horizontal line represents the mean and the error bars are the standard deviation. The dashed horizontal line denotes a 20% increase dimension, which represents an arbitrary cut-off point to represent a potentially clinically meaningful change. A) Graph of the percentage change in radiographic root area (RRA). Three REVASC cases had 20% or greater change in RRA. B) Graph of the percentage change in length. One APEX case had a 20% increase or greater change in length. C) Graph of the percentage change in width. Three REVASC cases had 20% or greater change in width.
Figure 3.
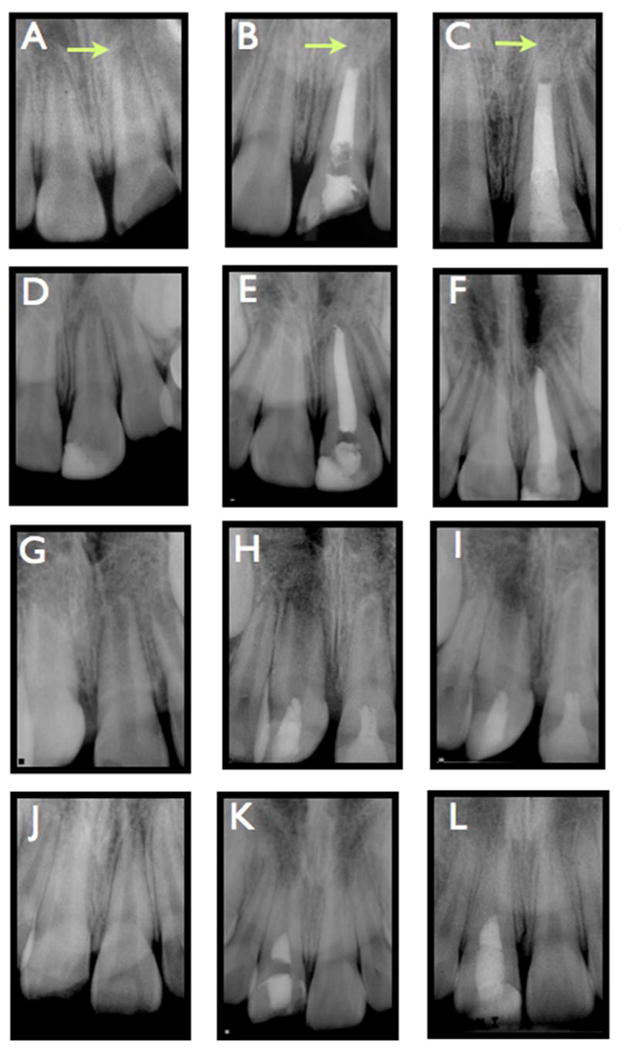
Radiographs of representative clinical cases included in this retrospective cohort study. A-C: This case involved an 8 year old male who traumatized tooth #9, causing a fracture that involved the pulp. The case was treated with calcium hydroxide APEX A: Pre-operative radiograph B: Post-operative Radiograph C: Follow up radiograph 19 months after treatment. The arrow points out the apex, to illustrate that this tooth demonstrated root lengthening after treatment as well as apical calcification. D-F: This case involved a 9 year old male with trauma to tooth #9, causing a fracture involving the pulp. The case was treated by MTA APEX. D: Pre-operative radiograph. E: Post-operative radiograph F: Follow up radiograph 10 months after treatment. G-I: This case involved a 9 year old female with intrusion trauma to teeth #8 and #9. Both teeth were treated by REVASC. G: Pre-operative radiograph. H: Post-operative radiograph. I: Follow up radiograph 12 months after treatment. Note the lack of root thickening or lengthening in tooth #8 and formation of an apical barrier in tooth #9, without obvious thickening or lengthening of the root. J-L: This case involved a 9 year old male with trauma to tooth #8. The case was treated by REVASC. J: Pre-operative radiograph. K: Post-operative radiograph. L: Follow up radiograph 23 months after treatment. Note the clear root thickening and lack of root lengthening, relative to the pre-operative image.
Descriptive Radiographic Findings
Although measurement of radiographic resolution of periapical pathology is difficult in immature permanent teeth, we performed this analysis as well. We only identified one case in the REVASC group with persistent periapical pathology at the final recall, which was larger than at the initiation of treatment. All other cases in the study were classified as healed or healing based on resolution or smaller appearance of periapical radiolucencies. External resorption was noted on 4 cases, all in the REVASC group. In 3 of the 4 cases exhibiting resorption, the resorption appeared similar in the pre-operative radiograph to the follow up radiograph. The remaining case only showed the development of resorption on the follow up radiograph. Finally we evaluated radiographic changes after completion of treatment including apical calcification/closure, intracanal calcification, and canal obliteration. We found 6 REVASC cases and 1 APEX case showing apical calcification (see Figure 3 A-C and G-I (tooth #9)). Only REVASC cases had the potential to show intracanal calcific barrier formation and canal obliteration, and we observed 3 cases and 2 cases of each respectively.
Discussion
This retrospective cohort study found that the clinical success and survival of immature teeth receiving revascularization treatment was comparable to that of traditional apexification treatment with Ca(OH)2 or MTA. The majority of data available on clinical outcomes in the literature come from case series and case reports, the exception being one retrospective cohort study and one prospective pilot cohort study (3, 33) both of which reported 100% clinical success after treatment by revascularization. The advantages of a cohort study versus a case series study, is the implementation of measures in the study design to minimize the influence of bias in case selection. In our study, we performed a comprehensive chart review of all cases completed during a three-year period, ultimately identifying a set of cases meeting our pre-determined inclusion and exclusion criteria. Not all potentially eligible cases had a recall on file; our recall rate was 63%. It is possible that the 37% cases not included due to lack of recall, could have differing outcomes from those reported here, which is a potential source of selection bias in this study. However, 63% is a fair recall rate for a retrospective study lacking incentives for patients to return for recall visits, and we believe the results of this study are of value to understanding clinical outcomes after endodontic treatment of immature permanent teeth.
Although our observed frequency of clinical success (79%) of REVASC treatment was not different statistically from that of APEX, it was not as high as existing reports of success from prospective and retrospective cohort studies (100%). There are several possible reasons for the difference in success rate between this study and existing studies. First, our study had a very high rate of trauma as the contributory etiology with 79% of revascularization cases having a primary contributory etiology of trauma. The retrospective study by Jeeruphan et al., had only 35% of REVASC cases with trauma as the etiology, and the prospective study by Jadhav et al., did not report the etiology (3, 33). This difference in the rate of trauma could certainly contribute to differences in clinical success rate. Also, how the study defined clinical success will influence the reported success rate. We defined clinical success as a tooth that survived and also did not require another endodontic intervention during the follow up period. We decided not to include radiographic outcomes in our definition of success, although if we had, the success rate would have most likely been lower.
There are several advantages and disadvantages of a retrospective study design. Two advantages are the study is less costly than a prospective study, and it is generally more feasible to quickly observe outcomes with longer follow up periods, as the follow up has already occurred in the past. One of the major disadvantages is that there is no control over the frequency of potential confounding factors between study groups. In our study, most of the patient specific factors were evenly distributed among the treatment groups, including age, gender, tooth type, pre-operative symptoms, and pre-operative periapical pathology. However, the REVASC group had a higher incidence of treated teeth at amore immature stage of root development, than in the APEX group. More severe trauma cases were included in the REVASC group (6 versus 1), which could be clinically significant, even though the difference in frequency of severe trauma between groups was not statistically significant. Because our sample size was small, we did not have sufficient power in the study to perform multivariate analyses that could control for these factors when assessing outcomes of APEX vs REVASC treatment (currently no other studies in this area have either). Because of this limitation we cannot be sure that the trend towards higher clinical failure rate and the observed significant increase in adverse event incidence was due to the treatment modality or these uncontrolled factors. Future studies will involve expansion of the chart review over a longer period, which will increase our sample size and allow us to assess the influence of these other potentially important factors on clinical success and radiographic outcomes. Identification of predictive variables of clinical and radiographic outcomes in the treatment of immature permanent teeth is critical both for the clinical management of these patients and informed study design for future prospective cohort studies.
A surprising finding in this study was the low incidence of radiographic evidence for continued root development in the REVASC group. Statistically there was no difference between teeth treated by REVASC and APEX in terms of root length, root width and radiographic root area (Fig 2). This is in contrast to almost all existing case reports, case series, retrospective and prospective cohort studies. Although the statistical difference between groups was not significant, there were clearly individual cases where REVASC treatment led to increased root width, and total root area (although interestingly not length), but the frequency of this occurring was much lower than what would be expected from the existing literature. There are several potential explanations for this discrepancy. First, many of the published case reports and case series may represent inadvertent biases towards choosing the best cases that demonstrate striking radiographic evidence of increased root length (selection bias). Also, existing studies that did not quantify the radiographic changes in root length and width, but rather subjectively assessed changes in root dimensions, are subject to interpretation bias. This is a problematic approach to assessing radiographic changes, as retrospective studies typically utilize radiographs that were captured in a non-standardized manner from children, leading to lots of variability in angulation between pre-operative and follow up films. It was our experience that variability in angulation would make the subjective assessment of these films almost impossible, without the benefit of image correction software (this point was also made in a correspondence to the Journal of Endodontics (34)). Even with using software correction, we had to eliminate cases from the radiographic analysis because the change in angulation made comparative measurements unreliable. As mentioned previously, our population primarily consisted of cases where trauma was the primary etiology, and the incidence of successful root development with revascularization in traumatized teeth is still unknown (discussed further below). Finally, longer follow up periods could increase the incidence of clinically meaningful changes in radiographic dimensions of teeth treated by REVASC. As our study had variable follow up times, some of the cases could still have the potential for root dimension changes. However, 10/15 REVASC cases included in the radiographic analyses had greater than 12 months follow up, which should be sufficient time to observe radiographic changes, based on many case reports.
Trauma is clearly an important contributory factor to the incidence of immature permanent teeth with necrotic pulps, as an estimated 22% of children suffer trauma to the permanent dentition, with an age range peaking between 7-10 years, more frequently in males, and most commonly involving the maxillary central and lateral incisors (35-37). The risk of the dental pulp becoming necrotic increases with the severity of the trauma, with intrusion having the highest incidence at 85% (38). In animal models it was shown that damage to Hertwig's epithelial root sheath (HERS) predicted whether root development continued in transplanted immature permanent teeth (39). It is also hypothesized that stem cells of the apical papilla are important to pulpal regeneration and continued root development. The effect of trauma and long standing periapical infections subsequent to pulpal necrosis to the viability of the apical papilla and HERS, are currently not known. More studies are needed to better understand the true incidence of continued root development after revascularization procedures and the influence of patient and tooth factors such as the etiology of pulpal necrosis (e.g. trauma versus caries) age, size of apical foramen, presence, size and temporal persistence of periapical pathology etc.
The findings reported here suggest that revascularization treatment has comparable, but not superior, clinical and radiographic outcomes to traditional apexification procedures. More clinical research is needed, with large subject numbers and long follow up periods, to better understand which cases are best suited for revascularization treatment.
Acknowledgments
This work was partially supported by grants from the National Institutes of Health (K23DE019461, JLG), and the American Association of Endodontists Foundation (Grant for Resident Research Program, ASA, LMC, JL, JA, AAM).
Footnotes
The authors deny any conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dental clinics of North America. 2010 Apr;54(2):313–24. doi: 10.1016/j.cden.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992 Apr;8(2):45–55. doi: 10.1111/j.1600-9657.1992.tb00228.x. [DOI] [PubMed] [Google Scholar]
- 3.Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012 Oct;38(10):1330–6. doi: 10.1016/j.joen.2012.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Rafter M. Apexification: a review. Dent Traumatol. 2005 Feb;21(1):1–8. doi: 10.1111/j.1600-9657.2004.00284.x. [DOI] [PubMed] [Google Scholar]
- 5.Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dental traumatology : official publication of International Association for Dental Traumatology. 2002 Jun;18(3):134–7. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 6.Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: a review. British dental journal. 1997 Oct 11;183(7):241–6. doi: 10.1038/sj.bdj.4809477. [DOI] [PubMed] [Google Scholar]
- 7.Shabahang S. Treatment options: apexogenesis and apexification. Journal of endodontics. 2013 Mar;39(3 Suppl):S26–9. doi: 10.1016/j.joen.2012.11.046. [DOI] [PubMed] [Google Scholar]
- 8.Witherspoon DE, Small JC, Regan JD, Nunn M. Retrospective analysis of open apex teeth obturated with mineral trioxide aggregate. J Endod. 2008 Oct;34(10):1171–6. doi: 10.1016/j.joen.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Holden DT, Schwartz SA, Kirkpatrick TC, Schindler WG. Clinical outcomes of artificial root-end barriers with mineral trioxide aggregate in teeth with immature apices. Journal of endodontics. 2008 Jul;34(7):812–7. doi: 10.1016/j.joen.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Moore A, Howley MF, O'Connell AC. Treatment of open apex teeth using two types of white mineral trioxide aggregate after initial dressing with calcium hydroxide in children. Dental traumatology : official publication of International Association for Dental Traumatology. 2011 Jun;27(3):166–73. doi: 10.1111/j.1600-9657.2011.00984.x. [DOI] [PubMed] [Google Scholar]
- 11.El-Meligy OA, Avery DR. Comparison of mineral trioxide aggregate and calcium hydroxide as pulpotomy agents in young permanent teeth (apexogenesis) Pediatr Dent. 2006 Sep-Oct;28(5):399–404. [PubMed] [Google Scholar]
- 12.Pradhan DP, Chawla HS, Gauba K, Goyal A. Comparative evaluation of endodontic management of teeth with unformed apices with mineral trioxide aggregate and calcium hydroxide. Journal of dentistry for children. 2006 May-Aug;73(2):79–85. [PubMed] [Google Scholar]
- 13.Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004 Apr;30(4):196–200. doi: 10.1097/00004770-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatric dentistry. 2007 Jan-Feb;29(1):47–50. [PubMed] [Google Scholar]
- 15.Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod. 2007 Apr;33(4):377–90. doi: 10.1016/j.joen.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 16.Wigler R, Kaufman AY, Lin S, Steinbock N, Hazan-Molina H, Torneck CD. Revascularization: a treatment for permanent teeth with necrotic pulp and incomplete root development. J Endod. Mar;39(3):319–26. doi: 10.1016/j.joen.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Lovelace TW, Henry MA, Hargreaves KM, Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod. Feb;37(2):133–8. doi: 10.1016/j.joen.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Iwaya S, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with periradicular abscess after luxation. Dental traumatology : official publication of International Association for Dental Traumatology. 2011 Feb;27(1):55–8. doi: 10.1111/j.1600-9657.2010.00963.x. [DOI] [PubMed] [Google Scholar]
- 19.Huang GT. Apexification: the beginning of its end. International endodontic journal. 2009 Oct;42(10):855–66. doi: 10.1111/j.1365-2591.2009.01577.x. [DOI] [PubMed] [Google Scholar]
- 20.Chueh LH, Huang GT. Immature teeth with periradicular periodontitis or abscess undergoing apexogenesis: a paradigm shift. Journal of endodontics. 2006 Dec;32(12):1205–13. doi: 10.1016/j.joen.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Cotti E, Mereu M, Lusso D. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: report of a case. Journal of endodontics. 2008 May;34(5):611–6. doi: 10.1016/j.joen.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 22.Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: a case series. Journal of endodontics. 2008 Jul;34(7):876–87. doi: 10.1016/j.joen.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 23.Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod. 2009 Oct;35(10):1343–9. doi: 10.1016/j.joen.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 24.da Silva LA, Nelson-Filho P, da Silva RA, Flores DS, Heilborn C, Johnson JD, et al. Revascularization and periapical repair after endodontic treatment using apical negative pressure irrigation versus conventional irrigation plus triantibiotic intracanal dressing in dogs' teeth with apical periodontitis. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2010 May;109(5):779–87. doi: 10.1016/j.tripleo.2009.12.046. [DOI] [PubMed] [Google Scholar]
- 25.Wang X, Thibodeau B, Trope M, Lin LM, Huang GT. Histologic characterization of regenerated tissues in canal space after the revitalization/revascularization procedure of immature dog teeth with apical periodontitis. Journal of endodontics. 2010 Jan;36(1):56–63. doi: 10.1016/j.joen.2009.09.039. [DOI] [PubMed] [Google Scholar]
- 26.Yamauchi N, Nagaoka H, Yamauchi S, Teixeira FB, Miguez P, Yamauchi M. Immunohistological characterization of newly formed tissues after regenerative procedure in immature dog teeth. J Endod. 2011 Dec;37(12):1636–41. doi: 10.1016/j.joen.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 27.Shimizu E, Jong G, Partridge N, Rosenberg PA, Lin LM. Histologic observation of a human immature permanent tooth with irreversible pulpitis after revascularization/regeneration procedure. Journal of endodontics. 2012 Sep;38(9):1293–7. doi: 10.1016/j.joen.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 28.Torabinejad M, Faras H. A clinical and histological report of a tooth with an open apex treated with regenerative endodontics using platelet-rich plasma. Journal of endodontics. 2012 Jun;38(6):864–8. doi: 10.1016/j.joen.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Martin G, Ricucci D, Gibbs JL, Lin LM. Histological findings of revascularized/revitalized immature permanent molar with apical periodontitis using platelet-rich plasma. Journal of endodontics. 2013 Jan;39(1):138–44. doi: 10.1016/j.joen.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 30.Shimizu E, Ricucci D, Albert J, Alobaid AS, Gibbs JL, Huang GT, et al. Clinical, radiographic, and histological observation of a human immature permanent tooth with chronic apical abscess after revitalization treatment. Journal of endodontics. 2013 Aug;39(8):1078–83. doi: 10.1016/j.joen.2013.04.032. [DOI] [PubMed] [Google Scholar]
- 31.Becerra P, Ricucci D, Loghin S, Gibbs JL, Lin LM. Histologic study of a human immature permanent premolar with chronic apical abscess after revascularization/revitalization. J Endod. 2014 Jan;40(1):133–9. doi: 10.1016/j.joen.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 32.American Association of Endodontics; 2013. Clinical considerations for regenerative procedures. http://wwwaaeorg/clinical-resources/regenerative-endodontics/considerations-for-regenerative-proceduresaspx: [Google Scholar]
- 33.Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod. 2012 Dec;38(12):1581–7. doi: 10.1016/j.joen.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 34.Messer HH. Re: Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: a pilot clinical study. J Endod. 2008 Oct;34(10):1157. doi: 10.1016/j.joen.2008.08.017. author reply. [DOI] [PubMed] [Google Scholar]
- 35.Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. International journal of oral surgery. 1972;1(5):235–9. doi: 10.1016/s0300-9785(72)80042-5. [DOI] [PubMed] [Google Scholar]
- 36.Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: a review of the literature. Australian dental journal. 2000 Mar;45(1):2–9. doi: 10.1111/j.1834-7819.2000.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 37.Clarkson BH, Longhurst P, Sheiham A. The prevalence of injured anterior teeth in English schoolchildren and adults. Journal of the International Association of Dentistry for Children. 1973 Jul;4(1):21–4. [PubMed] [Google Scholar]
- 38.Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth--the development of pulp necrosis. Endod Dent Traumatol. 1985 Dec;1(6):207–20. doi: 10.1111/j.1600-9657.1985.tb00583.x. [DOI] [PubMed] [Google Scholar]
- 39.Andreasen JO, Kristerson L, Andreasen FM. Damage of the Hertwig's epithelial root sheath: effect upon root growth after autotransplantation of teeth in monkeys. Endod Dent Traumatol. 1988 Aug;4(4):145–51. doi: 10.1111/j.1600-9657.1988.tb00313.x. [DOI] [PubMed] [Google Scholar]


