Abstract
Background
The anabolic response to progressive resistance exercise training (PRET) in haemodialysis patients is unclear. This pilot efficacy study aimed to determine whether high-intensity intradialytic PRET could reverse atrophy and consequently improve strength and physical function in haemodialysis patients. A second aim was to compare any anabolic response to that of healthy participants completing the same program.
Methods
In a single blind controlled study, 23 haemodialysis patients and 9 healthy individuals were randomly allocated to PRET or an attention control (SHAM) group. PRET completed high-intensity exercise leg extensions using novel equipment. SHAM completed low-intensity lower body stretching activities using ultra light resistance bands. Exercises were completed thrice weekly for 12 weeks, during dialysis in the haemodialysis patients. Outcomes included knee extensor muscle volume by magnetic resonance imaging, knee extensor strength by isometric dynamometer and lower body tests of physical function. Data were analysed by a per protocol method using between-group comparisons.
Results
PRET elicited a statistically and clinically significant anabolic response in haemodialysis patients (PRET—SHAM, mean difference [95 % CI]: 193[63 to 324] cm3) that was very similar to the response in healthy participants (PRET—SHAM, 169[−41 to 379] cm3). PRET increased strength in both haemodialysis patients and healthy participants. In contrast, PRET only enhanced lower body functional capacity in the healthy participants.
Conclusions
Intradialytic PRET elicited a normal anabolic and strength response in haemodialysis patients. The lack of a change in functional capacity was surprising and warrants further investigation.
Keywords: Weight lifting, Wasting syndrome, Chronic kidney failure, Haemodialysis
Introduction
Muscle atrophy is frequently observed with haemodialysis (HD) affecting 18–80 % of patients [1–5]. Muscle wasting in this population is a noteworthy problem as it independently predicts morbidity and mortality [6]. Strong positive correlations have been revealed between muscle quantity and strength, oxygen extraction at the muscle and functional capacity in HD patients [2, 3, 7, 8], suggesting that muscle wasting also reduces physical functioning. Thus, muscle wasting indirectly affects quality of life (QoL).
Disuse remains a consistently cited mechanism of atrophy [5] that is rarely addressed by standard routine care. Progressive resistance exercise training may be a safe, cost-effective, anabolic intervention, having already been implemented in other catabolic diseases [9, 10]. However, despite positively affecting anabolic markers such as mitochondrial biogenesis, skeletal muscle mRNA, muscle IGF-1 protein and muscle fibre cross-sectional area across all stages of chronic kidney disease [11, 12] in HD patients, the efficacy of resistance exercise on muscle quantity, as assessed using recommended nutritional endpoints [13], remains uncertain. Previously, only two intradialytic resistance exercise interventions have shown beneficial effects on muscle atrophy [14, 15] whilst the majority of studies have failed to elicit an anabolic response in this patient population [15–17].
The reason for this discouraging lack of an anabolic response to resistance exercise in HD patients is unclear [5]. Unfortunately, previous resistance exercise interventions have generally lacked attributes (such as sufficient overload and progression) necessary to elicit an anabolic effect [18, 19]. Thus, before resistance exercise can be investigated further as an adjunctive therapy for HD patients, a program meeting the guidelines deemed most effective for anabolism must be implemented. Alternatively, HD patients present with hypogonadism [20], insulin resistance [21] and a perturbed insulin-like growth factor/growth hormone axis [22], all of which are required to activate signalling pathways responsible for protein synthesis. Thus, a comparison between the anabolic response in HD patients and healthy controls would also be beneficial.
Consequently, the aim of this study was to determine whether a novel intradialytic progressive resistance exercise training technique, ensuring sufficient overload and progression for anabolism, could safely reverse atrophy and improve muscle strength and physical function in HD patients. A secondary aim was to compare any anabolic response to that of healthy participants completing the same program. It was hypothesised that progressive resistance exercise training would significantly increase muscle volume, strength and physical function in HD patients as compared to an attention control group, and that this response would be similar to that observed in healthy participants.
Methods
Study design
In this two-centre, single blind, pre-test post-test, controlled trial (clinicaltrials.gov: NCT01007838), participants were randomly allocated to receive progressive resistance exercise training (PRET) or a sham exercise attention control intervention (SHAM) using opaque envelopes in a 1:1 manner, stratified by disease, gender and centre (by DK).
Participants
Ethical approval was provided by Betsi Cadwaladr University Health Board Ethics Committee and Bangor University. Participants provided written informed consent. Haemodialysis patients were recruited from two renal units in North Wales, UK. Inclusion criteria required patients to be diagnosed with stage 5 chronic kidney disease receiving HD three times per week. Patients were excluded if they were below 18 years of age, had received HD <3 months, required support for ambulation of >50 m, presented with haemoglobin levels <11 g dL−1, presented with neuromuscular or catabolic conditions, received any anabolic treatment in the preceding 3 months, had any uncontrolled medical condition, presented with contraindications to take part in exercise or were unable to provide consent.
Sedentary healthy participants were recruited from the North Wales community using posters placed in community centres. Participants were excluded if their general practitioner deemed the participant to have a contraindication to exercise, had suffered from a catabolic condition or received an anabolic or exercise intervention in the preceding 3 months.
Intervention
PRET groups completed a 12-week resistance training program three times per week, during routine HD sessions for the patients and during university visits for the healthy participants. Each session involved a leg press exercise using equipment (Fitness Systems, Bolton, UK) designed to fit to the end of a dialysis chair (Stephen H Anatomical New, Gardhen Bilance, Italy). As obtaining large training loads using traditional plate loading machines was unsafe and impractical in the renal unit, leg press equipment was designed to utilise a series of resistance bands providing a maximum resistance equivalent to 200 kg. During training, participants completed three sets of eight to ten repetitions at 80 % of their predicted 1RM (determined from an assessment of their 5RM [23] to reduce the risk of injury associated with 1RM testing in this population [24]) with 2-min rest period between sets. Based on resistance exercise biology, this protocol is recommended for muscle hypertrophy [18, 19]. When 10–12 repetitions could be completed at a rating of perceived exertion below 15 (hard), 1RM was re-determined and the training load increased accordingly. Weekly training volume was calculated as kg per lift × lifts per session × sessions per week. The SHAM group carried out a series of unprogressive stretches using an ultra-light Thera-Band (Hygenic Corporation, Akron, Ohio).
Outcomes
Outcome measures were assessed pre and post the 12 week intervention by assessors blinded to group allocation.
Thigh muscle volume
The primary outcome measure was thigh muscle volume determined by magnetic resonance imaging. T1 and T2 images were obtained in the axial plane from the femoral tibial joint line to the top of the femoral head (3T Philips Achieva; Philips Healthcare, Best, The Netherlands). The image parameters were as follows: T1 acquisition matrix of 236 × 236, FOV 475 × 475 × 198, voxel size 2 × 2 mm2, TE 2.3 ms, TR 4 ms, slice thickness 5 mm, acquisition time 3 min. The muscle cross-sectional area of 12 evenly spaced axial slices [25] was determined using image processing software (version 4.x, Osirix, Pixmeo, Geneva). The truncated cone formula was applied to calculate muscle volume. The test re-test reliability of this protocol expressed as a coefficient of variation (CV) was 1.5 % with an interclass correlation (ICC3,k) of 0.997.
Muscle strength
Isometric bilateral knee extensor strength was measured using an isometric chair (Bodycare Products, Southam, UK) equipped with a load cell (615S, Tedea Huntleigh, Vishay, Basingstoke, UK), resolved and converted to force in Newtons by a data acquisition and analysis system (PowerLab 16SP; AD Instruments PTY, Colorado Springs, CO). Three maximal voluntary contractions were performed with a minute rest between each. The highest value was used for analysis. The ICC3,k of this was reported as 0.960 (26).
Physical function
Physical function tests included the 30-s sit to stand test, a measure of lower body strength (ICC3,k = 0.89); the 8-ft get up and go test, a measure of speed and agility (ICC3,k = 0.95) and the 6-min walk test, a measure of aerobic capacity (ICC3,k = 0.94) [27].
Harms
Information on harms was collected at the beginning and end of each session via interview and, in HD patients, by checking dialysis treatment records. Specifically, information on musculoskeletal injuries, cardiovascular events, acute hypotension and hypertension and access complications were recorded.
Unexpected and serious harms were collected as they occurred, during the trial period only. Decisions about whether events were attributable to the intervention were made by un-blinded clinicians.
Quality of life
Preliminary data on self-reported quality of life (QoL) were obtained using the Short Form-36 version 2 (SF-36v2) questionnaire [28].
Statistical analysis
Data were analysed using the Statistical Package for the Social Sciences (version 18; IBM, New York, USA) with statistical significance set at p ≤ 0.05. Weekly training volumes in the PRET groups were compared using a repeated measures analysis of variance. For the primary outcome of muscle volume, a minimum important clinical change over 12 weeks was set as 75 cm3, which over a year would equate to a change of 10 % of thigh muscle volume in healthy individuals. For muscle volume, knee extensor strength, physical function and QoL data, comparisons of the response between groups were of primary interest to this efficacy study. Therefore, independent t tests on change scores were used, analysing data on a per protocol basis. Effect sizes (d) were also calculated for these comparisons using Cohen’s method, and can be interpreted as small (0.3), medium (0.5) or large (0.8) [29]. Differences in the change scores between groups, along with the 95 % confidence intervals for these differences were also calculated. This three-step approach ensured that the response could be compared (i) between PRET and SHAM within the HD patients, (ii) between PRET and SHAM within the healthy participants and (iii) between HD patients and healthy participants within the PRET group. Data on harms and compliance were presented descriptively.
Results
Participants, compliance and training volume
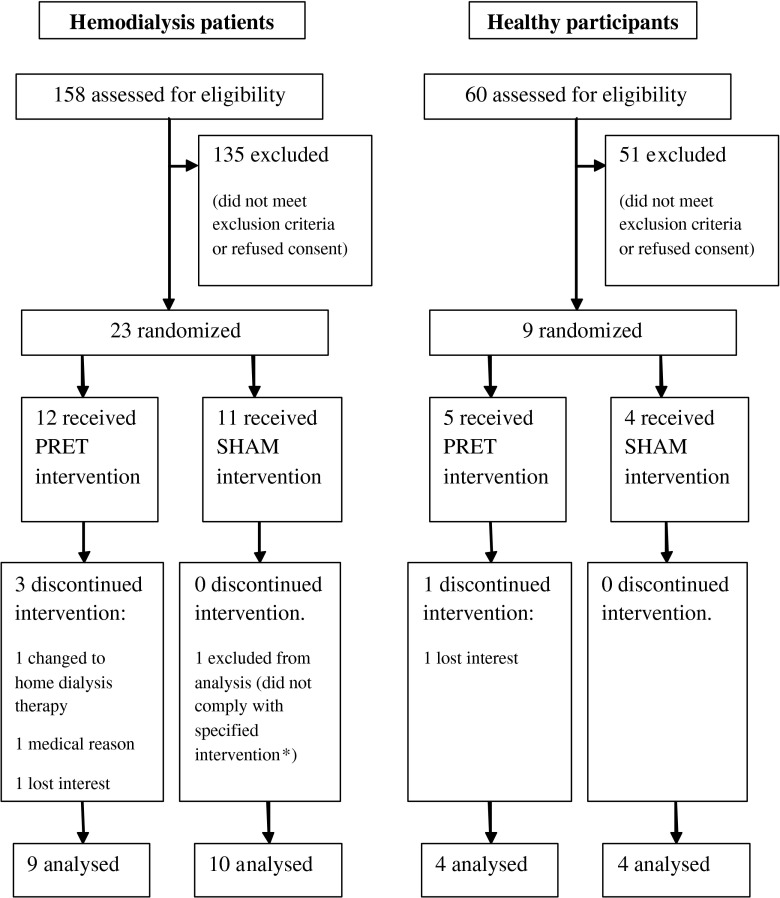
Participant flow through the study is presented in Fig. 1. Participant characteristics are presented in Table 1. There were no statistical differences between HD patients and healthy controls for age and body mass index. All HD patient baseline haematology, biochemistry and dialysis data were within renal association recommended ranges (Table 1).
Fig. 1.
Trial profile: PRET progressive resistance exercise training, SHAM attention control. * completed additional exercise
Table 1.
Baseline characteristics of all groups
| Characteristic | Haemodialysis patients | Healthy participants | p | |||
|---|---|---|---|---|---|---|
| PRET | SHAM | PRET | SHAM | HD PRET versus healthy PRET |
HD SHAM versus healthy SHAM |
|
| Age (years) | 48 ± 18 | 58 ± 15 | 50 ± 15 | 40 ± 17 | 0.8 | 0.06 |
| Body mass index (kg m2-1)§ | 25 ± 3 | 26 ± 5 | 30 ± 7 | 25 ± 5 | 0.08 | 0.5 |
| Gender (Male/Female) | 7/2 | 6/4 | 2/2 | 0/4 | ||
| Comorbid conditions | ||||||
| Hypertension Diabetes Myocardial infarction |
5 | 4 | 1 | 1 | ||
| 0 | 2 | 0 | 0 | |||
| 0 | 3 | 1 | 0 | |||
| Number on medications | ||||||
| Beta blockers Ace inhibitors Angiotensin receptor blockers Calcium channel blockers Alpha blockers Benzodiazepines Erythropoiesis stimulating agents |
5 | 2 | 1 | 0 | ||
| 3 | 4 | 0 | 0 | |||
| 0 | 0 | 0 | 0 | |||
| 2 | 5 | 0 | 0 | |||
| 1 | 2 | 0 | 0 | |||
| 0 | 4 | 0 | 1 | |||
| 6 | 7 | 0 | 0 | |||
| Aetiology of HD | ||||||
| Glomerulonephritis Infective/obstructive Hereditary Uncertain |
4 | 5 | ||||
| 1 | 1 | |||||
| 1 | 0 | |||||
| 3 | 4 | |||||
| Dialysis vintage (months) | 46 ± 54 | 66 ± 47 | ||||
| Kt/Vurea | 1.34 ± 0.13 | 1.50 ± 0.24 | ||||
| Haemoglobin (g dL−1) | 11.7 ± 1.8 | 12.1 ± 2.1 | ||||
| Albumin | 41 ± 3 | 42 ± 3 | ||||
| Serum bicarbonate (mmol L−1) | 22.4 ± 3.2 | 22.5 ± 2.7 | ||||
| Serum potassium (mmol L−1) | 4.8 ± 1.0 | 5.0 ± 0.6 | ||||
HD haemodialysis, PRET progressive resistance exercise training, SHAM attention control
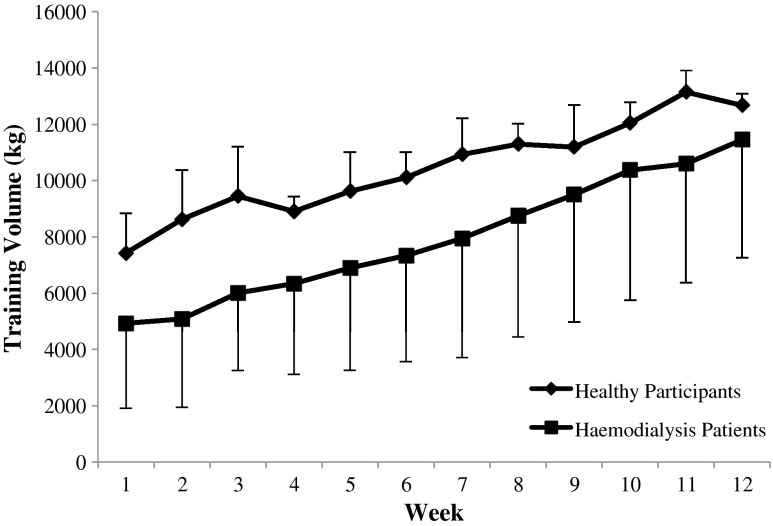
In the PRET groups, training volumes significantly increased to a similar extent in HD and healthy participants, as evidenced by a significant main effect of time (p = 0.03, Fig. 2), a non-significant group × time interaction (p = 0.3) and a non-significant main effect of group (p = 0.2). Compliance to PRET was similar in both HD patients and healthy participants with 94 ± 3 and 93 ± 3 % of training sessions completed, respectively. Reasons for missing any of the 324 offered exercise sessions in the HD PRET group were illness (14 sessions), scheduling issues (2 sessions) and dialysis equipment problems (2 sessions). Reasons for missing any of the 180 offered exercise sessions in the healthy PRET group were holidays (8 sessions) and unexplained nonattendance (4 sessions).
Fig. 2.
Training volume in progressive resistance exercise training groups over the 12-week intervention period. Training volume increased from week 1 to 12 similarly in both haemodialysis patients and healthy controls, as evidenced by a significant main effect of time by analysis of variance (p = 0.03), a non-significant group × time interaction (p = 0.3) and a non-significant main effect of group (p = 0.2)
Thigh muscle volume
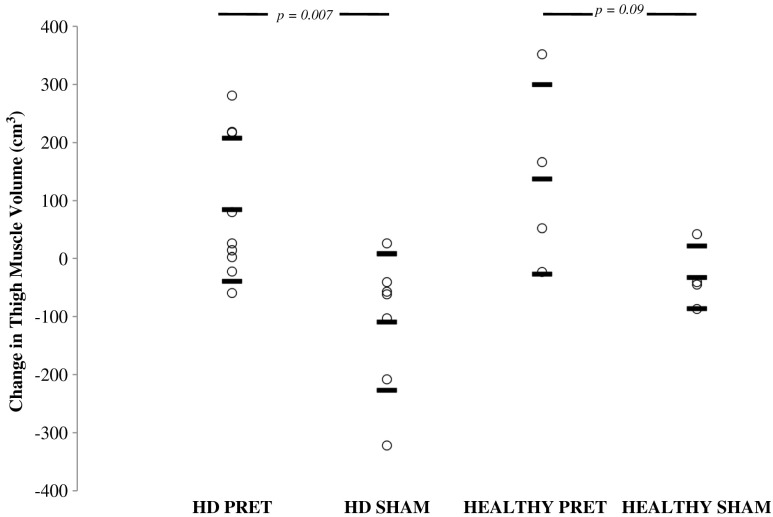
PRET elicited an anabolic response in both HD and healthy participants, as evidenced by a clinically and significantly greater change in HD PRET compared to HD SHAM (mean difference [95 % CI]: 193[63 to 324] cm3; p = 0.007; d = 0.4), a trend and strong effect size for a greater change in healthy PRET compared to healthy SHAM (mean difference [95 % CI]: 169[−41 to 379] cm3, p = 0.1; d = 0.2) and no difference in response to PRET between HD patients and healthy participants (p = 0.5; d = 0.1) (Table 2 and Fig. 3).
Table 2.
Muscle volume, strength and physical functioning absolute data before and after the 12 week intervention period
| Outcome measure | Haemodialysis patients | Healthy participants | HD PRET versus healthy PRET | HD PRET versus HD SHAM | Healthy PRET versus healthy SHAM | ||
|---|---|---|---|---|---|---|---|
| PRET | SHAM | PRET | SHAM | ||||
| Muscle volume (cm3) | |||||||
| Pre | 2,822 ± 438 | 2,490 ± 601 | 2,877 ± 710 | 2,183 ± 527 | 0.5 | 0.007 | 0.09 |
| Post | 2,906 ± 489 | 2,380 ± 643 | 3,013 ± 863 | 2,151 ± 527 | |||
| Knee extensor strength (N) | |||||||
| Pre | 179 ± 109 | 151 ± 79 | 382 ± 103 | 239 ± 80 | 0.6 | 0.012 | 0.06 |
| Post | 287 ± 86 | 201 ± 77 | 471 ± 191 | 210 ± 31 | |||
| Sit to stand (reps) | |||||||
| Pre | 11 ± 2 | 10 ± 4 | 21 ± 6 | 23 ± 6 | 0.004 | 0.2 | 0.005 |
| Post | 13 ± 3 | 11 ± 5 | 28 ± 8 | 25 ± 7 | |||
| 8-ft get up and go (s) | |||||||
| Pre | 5.8 ± 1.2 | 6.7 ± 1.8 | 4.4 ± 0.2 | 4.3 ± 0.7 | 0.5 | 0.5 | 0.09 |
| Post | 5.0 ± 0.8 | 6.2 ± 1.8 | 3.8 ± 0.4 | 4.5 ± 0.2 | |||
| 6-min walk distance (m) | |||||||
| Pre | 532 ± 95 | 460 ± 162 | 536 ± 47 | 559 ± 26 | 0.7 | 0.4 | 0.01 |
| Post | 571 ± 101 | 520 ± 160 | 600 ± 54 | 511 ± 38 | |||
PRET progressive resistance exercise training, SHAM attention control
Fig. 3.
Changes in absolute thigh muscle volume by magnetic resonance imaging over the 12-week intervention period. HD haemodialysis patients, PRET progressive resistance training, SHAM attention control. PRET elicited a similar anabolic response in haemodialysis patients and healthy participants, as evidenced by significant independent t tests between PRET and SHAM groups and moderate to large effect sizes
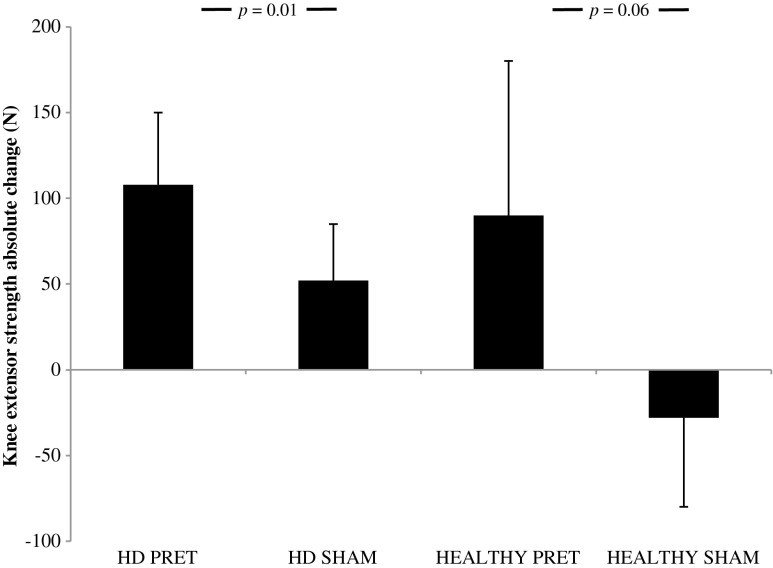
Knee extensor strength
PRET elicited a strength response in both HD and healthy participants, as evidenced by a significantly greater change in HD PRET compared to HD SHAM (mean difference [95 % CI]: 56[15 to 98] N; p = 0.01; d = 0.6), a trend and strong effect size for a greater change in healthy PRET compared to healthy SHAM (mean difference [95 % CI]: 118[−9 to 245] N; p = 0.06; d = 1.0) and no difference in response to PRET between HD patients and healthy participants (p = 0.6; d = 0.2) (Table 2).
Physical function
PRET only elicited an improvement in physical functioning in healthy participants. For sit to stand scores, a significantly greater change in healthy PRET compared to healthy SHAM was observed (mean difference [95 % CI]: 5 [3–8] units; p = 0.005; d = 0.2). In contrast, in the HD patients, the response to PRET was not different to SHAM (mean difference [95 % CI]: 1 [−1 to 4] units; p = 0.3; d = 0.3). Furthermore, the response to PRET was greater in the healthy participants than in the HD patients (p = 0.004; d = 0.8) (Table 2).
Similarly, for 6-min walk distance, a significantly greater change in healthy PRET compared to healthy SHAM (mean difference [95 % CI]: 31[36 to 188] yd; p = 0.01; d = 3.03) was observed. In contrast, in the HD patients, the response to PRET was not different to SHAM (mean difference [95 % CI]: 15[−25 to 54] yd; p = 0.4; d = −0.17). Combined with the finding that the response to PRET was similar in the healthy participants and the HD patients (p = 0.7, d = 0.32), the data reveal that PRET enhances 6-min walk distance, but in HD patients, this enhancement was no greater than SHAM exercise (Table 2).
Harms
In HD patients, expected harms reported in the PRET and SHAM groups, respectively, were musculoskeletal (cramp, 5 vs. 5; delayed onset of muscle soreness, 1 vs. 0; joint pains, 0 vs. 5) and hypotension (5 vs. 0). An unexpected reported harm was laceration of wounds on the back (PRET 1; SHAM 0). In the healthy participants, only one musculoskeletal harm was reported (delayed onset of muscle soreness) in the PRET group (Fig. 4).
Fig. 4.
Isometric knee extensor strength absolute change over the 12-week intervention period. HD haemodialysis patients, PRET progressive resistance training. PRET elicited a similar strength response in haemodialysis patients and healthy participants, as evidenced by a significant independent t tests between PRET and SHAM groups and moderate to large effect sizes
Quality of life
PRET had positive efficacy in the healthy participants on bodily pain and social functioning domains, but this was not the case in the HD patients (% change scores below; absolute data not shown). Specifically, PRET elicited a large and significant improvement in bodily pain in healthy participants (PRET, +34 ± 5 %; SHAM, −3 ± 16 %; p = 0.005; d = 2.4) but not in HD patients (PRET, 0 ± 15 %; SHAM, +2 ± 15 %; p = 0.1; d = 0.1). PRET also elicited a large significant improvement in social functioning in the healthy participants (PRET, +23 ± 20 %; SHAM, −9 ± 19 %; p = 0.05; d = 1.4) but not in HD patients (PRET, p = +7 ± 18 %; SHAM, −1.5 ± 8 %; p = 0.2; d = 0.3). PRET had no efficacy on change scores for physical function (p = 0.1), role limitation due to physical problems (p = 0.5), general health (p = 0.3), vitality (p = 0.44) and role limitation due to emotional problems (p = 0.4) in either the healthy participants or HD patients.
Discussion
The aim of this randomised controlled pilot efficacy study was to implement an intradialytic exercise program that met required resistance exercise training principles to reverse muscle atrophy in HD patients. A secondary aim was to compare the anabolic response in HD patients to healthy controls. Using novel equipment allowing adequate overload and progression, 12 weeks of high-intensity PRET elicited a clinically important and statistically significant anabolic response and strength increase in HD patients that was similar to that observed in healthy participants. However, unexpectedly, in HD patients, PRET was not efficacious at improving functional capacity.
When the temporal nature of muscle wasting is considered, the anabolic response to PRET in HD patients seems remarkably normal. In the present study, there was an approximately 7 % difference in muscle volume change between PRET and SHAM interventions, in both the HD patients and the healthy participants. These data are in contrast to the majority of previous studies [11, 16, 17, 30] and a recent meta-analysis [31] that have failed to show a significant hypertrophic response to exercise in HD populations. An explanation is that previous studies have not provided significant overload and progression; hypertrophic adaptation will only occur if a greater force is continually exerted to meet higher physiological demands [19]. It is questionable that this principle has been adhered to in previous studies that have prescribed intradialytic exercise utilising weights that can only provide a maximum lifted weight of 15 kg (compared to the 200 kg permissible with the current equipment). Note that the difference in response between studies is not due to the fact that our patients were healthier than those previously investigated: physical function was substantially decreased in the patients as compared to the healthy controls studied herein. Furthermore, despite similar muscle volumes at baseline, the HD SHAM patients lost clinically significant amounts of muscle volume over the 12-week period, signifying that these patients were in a catabolic state.
The anabolic response observed herein is supported by two previous studies [14, 15]. In fact, in those studies, the anabolic response was slightly larger (8–10 %) than observed herein, perhaps because the present study utilised only one exercise, whereas previous studies have utilised multiple lower and whole body exercises that might be expected to induce a larger systemic hypertrophic response [32].
Encouragingly, these findings suggest that if anabolic resistance is present in HD patients [5], it can be overcome by providing resistance exercise of sufficient volume. Despite perturbed sex hormone, insulin and insulin-like growth factor/growth hormone pathways [5, 20], an anabolic response to PRET is possible in HD patients. This finding is consistent with studies that have administered sex hormones [15, 26] and insulin-like growth factor/growth hormone [33], successfully increasing muscle volume.
Interestingly, the response of functional capacity to PRET differed between HD and healthy participants. Although strength increases in the HD patients following PRET appeared promising, they did not translate into improved functional capacity. This lack of an effect cannot be due to poor compliance: compliance was similarly excellent between the populations. Nor can it be due to selection bias of relatively healthy patients: the healthy controls responded to PRET despite having an even higher baseline functional capacity. Neither can it be due to insufficient intervention duration: the healthy participants herein responded to PRET within the 12-week intervention. Such a lack of effect is consistently reported in studies investigating intradialytic resistance training in HD patients [14–17]. This lack of efficacy is particularly surprising, considering that similar interventions carried out in other catabolic conditions have shown significant increases in similar measures of functional capacity [10]. It is noteworthy that for the 6-min walk test, both PRET and SHAM exercise similarly increased functional capacity; it is possible that despite familiarisation with outcome measures, patients could have been too cautious in the baseline tests, resulting in a learning effect in both groups at post-test. Variability in this learning effect may have masked potential interactions [34]. However, it is also interesting that intradialytic aerobic exercise has generally proven successful at enhancing the same functional measures in HD patients [35, 36]. Future research in this area could provide an interesting insight into the mechanisms behind enhanced functional capacity in this population.
PRET also had no effect on QoL in HD patients. Assuming this was not due to being underpowered to detect changes in QoL, a possible explanation could be that patients who volunteer to take part in exercise trials are generally healthier patients with a better QoL. In fact, the patients who took part in this study presented with QoL scores similar to age-matched Welsh normative values of healthy individuals [37]. In addition, exclusion criteria meant that patients with uncontrolled medical complications, and therefore an expected poorer QoL, were excluded from this study. It is possible that had these patients been included, they may have experienced greater QoL changes following an exercise intervention. Alternatively, the lack of change in physical function may have simply blunted any changes to quality of life.
A limitation to this study was the absence of whole body protein synthesis and diet measurements to indicate whether nutritional intake confounded body composition responses. Previous literature has shown increases in body fat percentage following PRET [15], perhaps due to an increased appetite following exercise [38]. Additionally, protein intake may moderate anabolism in response to muscle contraction [39]. Future studies should include such dietary measures and also a detailed assessment of energy balance. A further limitation lies in the small size of this pilot study, and particularly of the conveniently sampled healthy control group. Specifically, despite randomisation, the age and body composition were not exactly the same between the groups at baseline. We addressed this issue statistically by using and presenting an analysis of change scores. An alternative analysis using the baseline data as a covariate confirmed our interpretation (data not shown). Nevertheless, comparison of response between diseased and non-diseased participants should be interpreted cautiously, and results may only be generalizable to populations similar to that studied herein. However, the strength of including this comparison group is that for the first time, it allows such comparisons to be made.
In conclusion, using novel intradialytic equipment to allow adequate overload, PRET was safe and increased muscle volume and strength in HD patients. A similar anabolic response to PRET was observed in HD patients and healthy participants, precluding assumptions of anabolic resistance to exercise in this patient population. While reversing muscle wasting is theoretically beneficial for reducing morbidity and mortality, the lack of efficacy on functional capacity was surprising and warrants further investigation.
Acknowledgments
We acknowledge Loretta Davies, Nicola Carey, Hannah Lowther and Ruth Glover for invaluable help with data collection. This study was supported by unrestricted grants from the North West Wales National Health Service Trust Endowment Fund and by North Wales National Health Service Trust Research and Development-Central Area.
Authorship
The authors certify that they comply with the ethical guidelines for authorship and publishing of the Journal of Cachexia, Sarcopenia and Muscle 2010; 1:7–8 (von Haehling S, Morley JE, Coats AJ, and Anker SD).
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- 1.Sakkas GK, Ball D, Mercer TH, Sargeant AJ, Tolfrey K, Naish PF. Atrophy of non-locomotor muscle in patients with end-stage renal failure. Nephrol Dial Transplant. 2003;18:2074–81. [DOI] [PubMed]
- 2.Johansen KL, Shubert T, Doyle J, Soher B, Sakkas GK, Kent-Braun JA. Muscle atrophy in patients receiving hemodialysis: effects on muscle strength, muscle quality, and physical function. Kidney Int. 2003;63:291–7. doi: 10.1046/j.1523-1755.2003.00704.x. [DOI] [PubMed] [Google Scholar]
- 3.Macdonald JH, Phanish MK, Marcora SM, Jibani M, Bloodworth LLO, Holly JMP, et al. Muscle insulin-like growth factor status, body composition, and functional capacity in hemodialysis patients. J Ren Nutr. 2004;14:248–52. doi: 10.1016/j.jrn.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Workeneh BT, Mitch WE. Review of muscle wasting associated with chronic kidney disease. Am J Clin Nutr. 2010;91:1128S–32. doi: 10.3945/ajcn.2010.28608B. [DOI] [PubMed] [Google Scholar]
- 5.Mak RH, Ikizler TA, Kovesdy CP, Raj DS, Stenvinkel P, Kalantar-Zadeh K. Wasting in chronic kidney disease (vol 2, pg 9, 2011) J Cachexia Sarcopenia Muscle. 2011;2:119. doi: 10.1007/s13539-011-0026-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang CX, Tighiouart H, Beddhu S, Cheung AK, Dwyer JT, Eknoyan G, et al. Both low muscle mass and low fat are associated with higher all-cause mortality in hemodialysis patients. Kidney Int. 2010;77:624–9. doi: 10.1038/ki.2009.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marrades RM, Roca J, Campistol JM, Diaz O, Barbera JA, Torregrosa JV, et al. Effects of erythropoietin on muscle O2 transport during exercise in patients with chronic renal failure. J Clin Invest. 1996;97:2092–100. doi: 10.1172/JCI118646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheema B, Abas H, Smith B, O’Sullivan AJ, Chan M, Patwardhan A, et al. Investigation of skeletal muscle quantity and quality in end-stage renal disease. Nephrology (Carlton) 2010;15:454–63. doi: 10.1111/j.1440-1797.2009.01261.x. [DOI] [PubMed] [Google Scholar]
- 9.Singh MAF, Ding WJ, Manfredi TJ, Solares GS, O’Neill EF, Clements KM, et al. Insulin-like growth factor I in skeletal muscle after weight-lifting exercise in frail elders. Am Physiol Endocrinol Metab. 1999;277:E135–43. doi: 10.1152/ajpendo.1999.277.1.E135. [DOI] [PubMed] [Google Scholar]
- 10.Lemmey AB, Marcora SM, Chester K, Wilson S, Casanova F, Maddison PJ. Effects of high-intensity resistance training in patients with rheumatoid arthritis: a randomized controlled trial. Arthritis Rheum. 2009;61:1726–34. doi: 10.1002/art.24891. [DOI] [PubMed] [Google Scholar]
- 11.Kopple JD, Wang H, Casaburi R, Fournier M, Lewis MI, Taylor W, et al. Exercise in maintenance hemodialysis patients induces transcriptional changes in genes favoring anabolic muscle. J Am Soc Nephrol. 2007;18:2975–86. doi: 10.1681/ASN.2006070794. [DOI] [PubMed] [Google Scholar]
- 12.Balakrishnan VS, Rao M, Menon V, Gordon PL, Pilichowska M, Castaneda F, et al. Resistance training increases muscle mitochondrial biogenesis in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:996–1002. doi: 10.2215/CJN.09141209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Senior JR, Maroni BJ. Working group session report: chronic renal and gastrointestinal disease. J Nutr. 1999;129:313S–4. doi: 10.1093/jn/129.1.313S. [DOI] [PubMed] [Google Scholar]
- 14.Chen JL, Godfrey S, Ng TT, Moorthi R, Liangos O, Ruthazer R, et al. Effect of intra-dialytic, low-intensity strength training on functional capacity in adult haemodialysis patients: a randomized pilot trial. Nephrol Dial Transplant. 2010;25:1936–43. doi: 10.1093/ndt/gfp739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansen KL, Painter PL, Sakkas GK, Gordon P, Doyle J, Shubert T. Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: a randomized, controlled trial. J Am Soc Nephrol. 2006;17:2307–14. doi: 10.1681/ASN.2006010034. [DOI] [PubMed] [Google Scholar]
- 16.Cheema B, Abas H, Smith B, O’Sullivan A, Chan M, Patwardhan A, et al. Randomized controlled trial of intradialytic resistance training to target muscle wasting in ESRD: the progressive exercise for anabolism in kidney disease (PEAK) study. Am J Kidney Dis. 2007;50:574–84. doi: 10.1053/j.ajkd.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Cheema B, Abas H, Smith B, O’Sullivan A, Chan M, Patwardhan A, et al. Progressive exercise for anabolism in kidney disease (PEAK): a randomized, controlled trial of resistance training during hemodialysis. J Am Soc Nephrol. 2007;18:1594–601. doi: 10.1681/ASN.2006121329. [DOI] [PubMed] [Google Scholar]
- 18.Spiering BA, Kraemer WJ, Anderson JM, Armstrong LE, Nindl BC, Volek JS, et al. Resistance exercise biology: manipulation of resistance exercise programme variables determines the responses of cellular and molecular signalling pathways. Sports Med. 2008;38:527–40. doi: 10.2165/00007256-200838070-00001. [DOI] [PubMed] [Google Scholar]
- 19.Kraemer WJ, Adams K, Cafarelli E, Dudley GA, Dooly C, Feigenbaum MS, et al. Joint position statement: progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34:364–80. doi: 10.1097/00005768-200205001-00389. [DOI] [PubMed] [Google Scholar]
- 20.Albaaj F, Sivalingham M, Haynes P, McKinnon G, Foley RN, Waldek S, et al. Prevalence of hypogonadism in male patients with renal failure. Postgrad Med J. 2006;82:693–6. doi: 10.1136/pgmj.2006.045963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mak RH. Insulin and its role in chronic kidney disease. Pediatr Nephrol. 2008;23:355–62. doi: 10.1007/s00467-007-0611-2. [DOI] [PubMed] [Google Scholar]
- 22.Mak RH, Cheung WW, Roberts CT., Jr The growth hormone-insulin-like growth factor-I axis in chronic kidney disease. Growth Horm IGF Res. 2008;18:17–25. doi: 10.1016/j.ghir.2007.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bryzycki M. Strength testing-predicting a one-rep max from a reps-to-fatigue. J Phys Edu Recreat Dance. 1993;64:88–90. doi: 10.1080/07303084.1993.10606684. [DOI] [Google Scholar]
- 24.Painter PL, Krasnoff JB. End stage metabolic disease: renal failure and liver failure. In: Durstine JL, Moore GE, Painter PL, Roberts SO, editors. ACSM’s exercise management for persons with chronic diseases and disabilities. 3. Champaign, IL: Human Kinetics; 2009. pp. 175–82. [Google Scholar]
- 25.Tracy BL, Ivey FM, Metter EJ, Fleg JL, Siegel EL, Hurley BF. A more efficient magnetic resonance imaging-based strategy for measuring quadriceps muscle volume. Med Sci Sports Exerc. 2003;35:425–33. doi: 10.1249/01.MSS.0000053722.53302.D6. [DOI] [PubMed] [Google Scholar]
- 26.Macdonald JH, Marcora SM, Jibani MM, Kumwenda MJ, Ahmed W, Lemmey AB. Nandrolone decanoate as anabolic therapy in chronic kidney disease: a randomized phase II dose-finding study. Nephron Clin Pract. 2007;106:125–35. doi: 10.1159/000103000. [DOI] [PubMed] [Google Scholar]
- 27.Rikili R, Jones C. Senior fitness test manual. Champaign, IL: Human Kinetics; 2001. [Google Scholar]
- 28.Ware JE, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s manual for the SF-36v2 health survey. QualityMetric: Lincoln, RI; 2007. [Google Scholar]
- 29.Cohen J. Statistical power analysis for the behavioural sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 30.Headley S, Germain M, Mailloux P, Mulhern J, Ashworth B, Burris J, et al. Resistance training improves strength and functional measures in patients with end-stage renal disease. Am J Kidney Dis. 2002;40:355–64. doi: 10.1053/ajkd.2002.34520. [DOI] [PubMed] [Google Scholar]
- 31.Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;10:CD003236. doi: 10.1002/14651858.CD003236.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hansen S, Kvorning T, Kjaer M, Sjogaard G. The effect of short-term strength training on human skeletal muscle: the importance of physiologically elevated hormone levels. Scand J Med Sci Sports. 2001;11:347–54. doi: 10.1034/j.1600-0838.2001.110606.x. [DOI] [PubMed] [Google Scholar]
- 33.Dong J, Ikizler TA. New insights into the role of anabolic interventions in dialysis patients with protein energy wasting. Curr Opin Nephrol Hypertens. 2009;18:469–75. doi: 10.1097/MNH.0b013e328331489d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30:1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 35.Cheema BSB, Smith BCF, Singh MAF. A rationale for intradialytic exercise training as standard clinical practice in ESRD. Am J Kid Dis. 2005;45:912–6. doi: 10.1053/j.ajkd.2005.01.030. [DOI] [PubMed] [Google Scholar]
- 36.Macdonald JH, Marcora SM, Jibani M, Phanish MK, Holly J, Lemmey AB. Intradialytic exercise as anabolic therapy in haemodialysis patients—a pilot study. Clin Physiol Funct Imaging. 2005;25:113–8. doi: 10.1111/j.1475-097X.2004.00600.x. [DOI] [PubMed] [Google Scholar]
- 37.Burholt V, Nash P. Short form 36 (SF-36) health survey questionnaire: normative data for wales. J Public Health (Oxf.) 2011;33:587–603. doi: 10.1093/pubmed/fdr006. [DOI] [PubMed] [Google Scholar]
- 38.Hopkins M, Jeukendrup A, King NA, Blundell JE. The relationship between substrate metabolism, exercise and appetite control does glycogen availability influence the motivation to eat, energy intake or food choice? Sports Med. 2011;41:507–21. doi: 10.2165/11588780-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39.Burd NA, Wall BT, van Loon LJC. The curious case of anabolic resistance: old wives’ tales or new fables? J Appl Physiol. 2012;112:1233–5. doi: 10.1152/japplphysiol.01343.2011. [DOI] [PubMed] [Google Scholar]