Abstract
Bile acids are increasingly recognized as key regulators of systemic metabolism. While bile acids have long been known to play important and direct roles in nutrient absorption, bile acids also serve as signaling molecules. Bile acid interactions with the nuclear hormone receptor farnesoid X receptor (FXR) and the membrane receptor G-protein-coupled bile acid receptor 5 (TGR5) can regulate incretin hormone and fibroblast growth factor 19 (FGF19) secretion, cholesterol metabolism, and systemic energy expenditure. Bile acid levels and distribution are altered in type 2 diabetes and increased following bariatric procedures, in parallel with reduced body weight and improved insulin sensitivity and glycemic control. Thus, modulation of bile acid levels and signaling, using bile acid binding resins, TGR5 agonists, and FXR agonists, may serve as a potent therapeutic approach for the treatment of obesity, type 2 diabetes, and other components of the metabolic syndrome in humans.
Keywords: Bile acids, FXR, TGR5, obesity, insulin resistance
Introduction
Bile is a mixture of bile acids (BAs), cholesterol, phosphatidylcholine, and bilirubin. Of these, BAs are essential constituents and play critical roles in regulation of metabolism in both humans and animal models. Bile acids have long been recognized to aid in the absorption of fat and fat-soluble vitamins and modulate cholesterol levels. However, recent data indicate that bile acids also play an important role in glucose and lipid homeostasis by activating both the nuclear receptor LXR and the cell surface receptor G protein-coupled bile acid receptor 5 (TGR5) [1-3]. Moreover, modulation of plasma bile acid levels and the total bile acid pool can affect glycemic control, body weight, and insulin sensitivity [4-6].
In this review, we will focus on the relation between bile acids and regulation of systemic metabolism and the potential for bile acids as a therapeutic approach for obesity, insulin resistance, type 2 diabetes (T2D), and other components of the metabolic syndrome.
1. Bile acid synthesis and regulation
1.1. Bile acid synthesis
BAs are amphipathic molecules with a steroid backbone which are synthesized from cholesterol in hepatocytes. It is estimated that about half of the 800 mg of cholesterol synthesized daily is used for bile acid synthesis, totaling about 200-600 mg daily in humans [7].
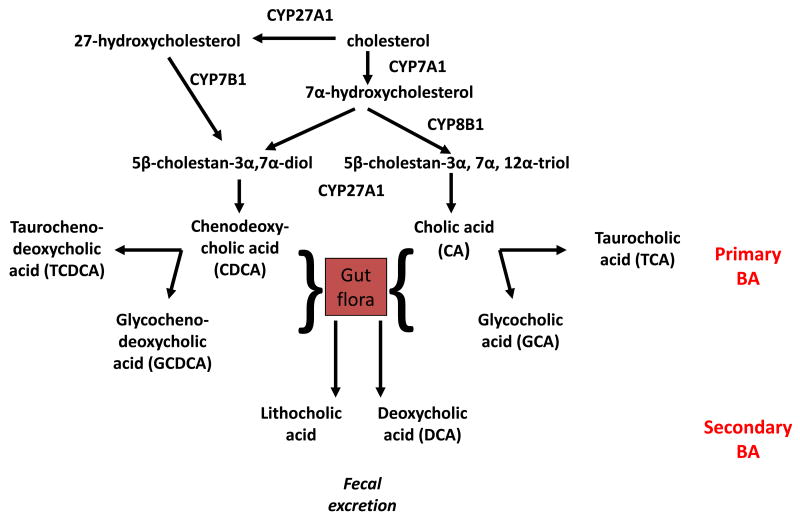
Bile acids are synthesized from cholesterol through two dominant pathways: the classic pathway and the alternative pathway (Figure 1). In the classic (or neutral) pathway, CYP7A1 catalyzes the initial and rate-limiting step converting cholesterol into 7α-hydroxycholesterol, with CYP8B1 subsequently regulating synthesis of 12α-hydroxysterols including cholic acid (CA). In the alternative (or acidic) pathway, CYP27A1 first hydroxylates the cholesterol side chain, converting cholesterol into 27-hydroxycholesterol, which is then 7α-hydroxylated by CYP7B1 prior to CYP8B1 action. In humans, the classical pathway produces the primary BA cholic acid (CA) and chenodeoxycholic acid (CDCA) in roughly equal amounts, whereas the alternative pathway produces mainly CDCA [8]. Most bile acids are conjugated with either glycine or taurine, with a 3:1 predominance of glycine over taurine [3, 5, 9].
Figure 1. Bile Acid Synthesis Pathway.
Cholesterol is converted to two primary bile acids in human liver, CA and CDCA. Key regulatory enzymes in these pathways include CYP7A1, CYP8B1, CYP27A1, and CYP7B1. CYP7A1 initiates the classic (neutral) biosynthetic pathway, while CYP27A1 initiates the alternative (acidic) pathway in liver and macrophages. CA and CDCA can be conjugated with glycine (G) and taurine (T). In the intestine, conjugated CA and CDCA are deconjugated and then dehydroxylated at the 7α-position to the secondary bile acids DCA and LCA, respectively.
Synthesized BA are stored in the gall bladder and secreted into the duodenum in response to feeding, contributing to digestion of lipids and lipid-soluble vitamins. The primary BA CA and CDCA can be dehydroxylated at the 7α position by gut microbiota to produce the secondary BAs, predominantly deoxycholic acid (DCA) and lithocholic acid (LCA) [10, 11]. Thus, bile acid levels and relative composition can be modulated by gut microbiota populations [12].
In the terminal ileum, BAs are efficiently absorbed by both active transport and passive diffusion, transported back to the liver via the portal vein, taken up at the sinusoidal membrane of hepatocytes, and secreted into bile again. Each BA molecule may complete 4-12 cycles of this enterohepatic circulation per day [1, 13]. This process is highly efficient, as only about 5% of bile acids are lost in feces [3, 14].
This process is similar in mice, although different bile acid species dominate. CDCA is efficiently converted into muricholic acid (MCA), and BAs are conjugated to taurine.
Given that different BA have different structures, hydrophobicity, and affinities for membrane and nuclear receptors, interindividual differences in BA pool composition resulting from differential regulation of the complex BA synthesis pathway may have functional consequences for systemic metabolism.
1.2. Regulation of Bile Acid Synthesis
BA are potent regulators of their own synthesis, serving to limit excessive accumulation of BA in the circulation via multiple redundant pathways. Feeding bile acids to rats strongly reduces CYP7A1 enzyme activity and bile acid synthesis [8, 15]. This self-regulation of BA synthesis involves activation of the nuclear receptor FXR (farnesoid X receptor, official gene name NR1H4) [16]. FXR knockout mice have increased BA synthesis and Cyp7a1 expression, verifying the central role for FXR in mediating bile acid inhibition of Cyp7a1 [17]. FXR has both direct effects on Cyp7a1 expression as well as indirect effects, mediated by induction of small heterodimer partner (SHP) which in turn inhibits transactivation of CYP7A1 and CYP8B1 by the transcription factors Hepatocyte Nuclear Factor 4α (HNF4α) and liver-related homolog-1 (LRH-1) at the bile acid response element. FXR also increases BA conjugation and upregulates expression of several genes which promote bile acid efflux from hepatocytes into the bile. An additional feedback repression mechanism involves FXR regulation of several individual fibroblast growth factors (FGFs). For example, bile acid activation of FXR results in secretion of FGF-19 from hepatocytes and enterocytes. In turn, FGF-19 can bind to fibroblast growth factor receptor 4 (FGFR4) receptors on hepatocytes, leading to suppression of CYP7A1 expression and bile acid synthesis via a SHP-independent, but c-Jun N-terminal kinase (JNK) dependent mechanism [18]. Consistent with this mechanism, FGFR4 knockout mice have increased expression of CYP7A1, in parallel with increased fecal bile acids and bile acid pool size [19]. Other nuclear receptors, such as the pregnane X receptor (PXR)[20] and vitamin D receptor (VDR) [21], can also regulate BA synthesis by suppressing CYP7A1. Moreover, activation of the nuclear receptor RORα can modulate 12α-hydroxylase (CYP8B1) expression [22, 23].
BA differ markedly in their potency to activate FXR. The hydrophobic bile acid CDCA is the most potent BA ligand of FXR, followed by lithocholic acid (LCA), deoxycholic acid (DCA), and CA; by contrast, the hydrophilic bile acids ursodeoxycholic acid (UDCA) and muricholic acid (MCA) do not activate FXR [24].
BA are also regulated in response to other elements of systemic metabolism. Early studies showed that the bile acid pool size is increased in insulin-deficient diabetic rats, with a 3-fold increase in the cholic acid pool [25]. Conversely, insulin treatment reduces bile acid pool size, inhibits CYP7A1 and CYP8B1 activity, and alters bile acid composition [26]. CYP7A1 can also be regulated by steroid hormones, activated protein kinase C, and proinflammatory cytokines [8].
2. Bile acids and regulation of systemic metabolism
FXR and TGR5 signaling mechanisms appear to dominate for BA effects on regulation of glucose, lipid, and energy metabolism [1, 27-30]. As noted above, BA are natural ligands for FXRα, a nuclear receptor highly expressed in liver, intestine, kidney and adrenal glands [17, 27]. BAs can also activate TGR5, a membrane-bound G protein-coupled BA receptor. TGR5 is expressed in many organs and tissues, with high expression in macrophages/monocytes, placenta, gallbladder, liver and intestine [31, 32]. BA stimulation of energy expenditure in brown adipose tissue (BAT) and skeletal muscle appears to be mediated via TGR5 [2].
2.1. Bile acids and lipid metabolism
BAs exert an important regulatory role in cholesterol and triglyceride (TG) metabolism. Increased bile acid synthesis increases utilization of cholesterol as substrate. Bile acid synthesis rates are correlated with serum triglyceride levels in hyperlipidemic patients [33]. Bile acid sequestrants or other interruptions in enterohepatic circulation also increase both bile acid and VLDL triglyceride synthesis. Conversely, CDCA-mediated increases in the BA pool size leads to inhibition of BA synthesis and reduced serum triglycerides in hyperlipidemic patients [34].
These effects of BA to modulate TG metabolism are likely mediated via several distinct mechanisms, predominantly BA activation of FXR [35, 36]. FXR alters the transcription of several genes involved in fatty acid and triglyceride synthesis and lipoprotein metabolism. In mice, administration of FXR agonists [GW4064,6a-ethylchenodeoxycholic acid] reduces plasma triglyceride and cholesterol levels [37-41] via repression of the lipogenic genes sterol-regulatory-element-binding protein-1c (SREBP1c) and fatty acid synthase (FAS) in liver [36]. FXR also induces expression of peroxisome proliferator activated receptor (PPAR)α, a nuclear receptor that promotes lipid oxidation [42], and of pyruvate dehydrogenase kinase, isoenzyme 4 (PDK4), leading to inhibition of pyruvate dehydrogenase and increased fatty acid oxidation [43]. Additional FXR target genes include the apolipoproteins A-V, C-III, apoE, syndecan-1, and the VLDL receptor [1, 44]. Conversely, FXR-null mice have higher serum TG levels and increased synthesis of apolipoprotein (apo) B-containing lipoproteins [17]. Thus, bile acids play central roles in lipid metabolism and in the control of TG levels, in part via FXR and downstream transcriptional targets.
Additional effects of BA on lipid metabolism may be independent of FXR. For example, the bile acid tauroursodeoxycholic acid (TUDCA) also acts as a chaperone, modulating endoplasmic reticulum stress [45]. TUDCA reduces adipogenesis in human adipocyte stem cells [46]. Similarly, in another study, UDCA (but not TUDCA) profoundly inhibits adipogenesis, in parallel with activation of extracellular regulated protein kinases 1 and 2 (ERK 1/2) [47].
2.2. Bile acids and glucose metabolism
Bile acids are also implicated in regulation of glucose metabolism [48-50]. Increasing hepatic bile acid synthesis can inhibit gluconeogenesis and stimulate glycolysis. Effects on glycogen metabolism appear complex [51]. Some studies have shown bile acids stimulate glycogen phosphorylase (GP) and glycogen breakdown to glucose-1-P [52], while other data indicate bile acids also activate glycogen synthesis (GS) [53]. Additional effects of BA on glucose metabolism and insulin action may also be mediated via reductions in endoplasmic reticulum (ER) stress, a key mediator of insulin resistance [45].
In addition to direct effects, many of the beneficial effects of BA on glucose metabolism are mediated via FXR. FXR is an important regulator of glucose metabolism, as demonstrated by reduced plasma glucose and reduced hepatic glycogen levels in FXR-null mice [49, 50, 54]. Conversely, activation of FXR is associated with increased phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase expression and glucose output from primary rat hepatocytes.
However, in vivo pharmacologic stimulation of FXR in two mouse models of obesity and T2D (db/db or KKA(y) mice) causes inhibition of gluconeogenesis, hypoglycemia, and increased insulin sensitivity [49, 50]. Thus, FXR may have a dominant effect to inhibit gluconeogenesis in diabetes, perhaps via inhibition of PEPCK by SHP-dependent inhibition of HNF4α and FoxO1 [55]. Activation of FXR can also stimulate the insulin/Akt pathway, promoting glycogen synthesis in liver [55], GLUT2 activation in pancreatic β-cells [56], and improving insulin resistance in obese ob/ob mice [57]. In this context, inhibition of gluconeogenesis, improved insulin action, and stimulation of glycogen synthesis may synergize to improve plasma glucose, insulin secretion, insulin sensitivity, and glucose tolerance. In parallel, however, GW4064 increases susceptibility to high fat diet-induced obesity and diabetes [50, 58]. These complex data highlight the importance of the specific context in which FXR is activated.
Beneficial effects of BA on glucose metabolism may also be mediated via TGR5. TGR5 is expressed in many organs and tissues, with highest expression in macrophages/monocytes, placenta, gallbladder, liver and intestine [32]. Activation of TGR5 in enterocytes can stimulate the secretion of the incretin hormone glucagon-like peptide GLP1, promoting glucose-dependent insulin secretion [59, 60]. Moreover, BA stimulation of cell-surface TGR5 on neurons may also modulate GLP-1 secretion [61]. In peripheral tissues, TGR5 activation may increase activation of the type 2 deiodinase, resulting in increased active thyroid hormone, mitochondrial oxidative capacity, and energy expenditure [2]. A recent human genetic study demonstrates that a single nucleotide polymorphism (SNP) at the TGR5 locus (rs3731859) is associated with BMI, waist circumference, intramyocellular lipids, and fasting GLP-1 levels [62]. Furthermore, TGR5-null mice have a 25% reduction in bile acid pool size, and female Tgr5 null mice show increased weight gain and fat accumulation when fed a high fat diet [63]. Further support for the regulatory role of TGR5 in glucose homeostasis comes from the finding that TGR5 agonists decrease blood glucose in animals [64].
2.3. Bile acids in humans
In healthy individuals, BA levels fluctuate with cycles of fasting and refeeding. BA robustly increase in response to an oral glucose load [65]. Such responses are increased in insulin sensitive individuals and are blunted in individuals with prediabetes [55], suggesting dysregulation of bile acid pools and/or intestinal regulation in insulin resistance.
The majority of studies have analyzed bile acid levels and species distribution in the fasting state; many of these demonstrate alterations in insulin resistance and diabetes. For example, one study demonstrated 1.6-fold increases in deoxycholic acid (DCA) in T2D [66]. Similarly, Haeusler et al demonstrated that 12α–hydroxylated species (sum of CA, DCA, and their conjugates) are significantly higher in patients with T2D [67]. Furthermore, ratios of 12-hydroxylated/non–12-hydroxylated BAs are associated with key features of IR, including higher insulin, glucose, and triglyceride (TG) levels and lower HDL cholesterol [67]. Brufau and colleagues showed that individuals with T2D had higher cholic acid (CA) synthesis rates and enlarged DCA pool size [68]. Our group recently reported that concentrations of total taurine-conjugated BA were higher in T2D and intermediate in individuals with impaired glucose tolerance [69]. Interestingly, total taurine-BA were positively associated with fasting and post-load glucose levels, fasting insulin, and HOMA-IR. However, insulin-mediated glycemic improvement in T2D patients did not change fasting serum total BA, or BA composition, suggesting dysregulation of BA levels is not directly linked to glycemic burden but possible due to other aspects of insulin resistance or the metabolic syndrome.
2.4. Bile acids are increased following bariatric surgery
Bariatric surgery is increasingly recognized as a robust method to not only reduce body weight, but also to reduce glycemia and medication requirement (so called diabetes “remission”) [70]. Bariatric surgical procedures include Roux-en-Y gastric bypass (RYGB), vertical sleeve gastrectomy (VSG), laparoscopic adjustable gastric banding (LAGB) and biliopancreatic diversion (BPD). In this context, it is interesting that several studies have demonstrated that bile acids are markedly increased following bariatric surgery [5, 6, 71, 72]. Interestingly, total bile acids in post-bypass patients are correlated with improvement in several key metabolic parameters; bile acids are inversely correlated with postprandial glucose, triglycerides, and positively correlated with adiponectin and peak GLP1 levels following a mixed meal test. These intriguing data suggest increased serum bile acid levels could contribute to improvements in insulin sensitivity, incretin secretion, and postprandial glycemia in response to bariatric surgery [6].
Despite these intriguing data, it remains uncertain whether increased BA are absolutely essential for metabolic improvements following bariatric surgery, particularly during the early postoperative period. For example, longitudinal studies in humans demonstrate that increases in BA are not detected until 1 year postoperatively [73], despite improved glucose levels and reduced hepatic glucose output within one week of surgery [74, 75]. By contrast, increases in both fasting and postprandial BA are also observed as early as 14 days following VSG in rodents [76, 77]. In addition, both RYGB and VSG can alter the distribution of bile acid species [8] [78]. By contrast, circulating BA do not change significantly after LAGB [4, 73, 79], and could contribute to reduced efficacy of this procedure for long-term resolution of T2D as compared with RYGB or VSG. Importantly, increased BA action, via FXR-mediated effects on both gut microbiome and transcriptional pathways, appears to be required to achieve the metabolic effects of surgery, at least in rodent models [77].
Intriguingly, direct modulation of small intestinal anatomy can alter bile acid levels and composition. Mid-to-distal small intestinal resection, with preservation of the terminal ileum, increases bile acid levels [80]. Similarly, interposition of the ileum into more proximal segments of gut also increases bile acid levels [81]. Nonsurgical approaches may also be effective; for example, endoluminal sleeves, which allow luminal contents to bypass the duodenal mucosa, also increase bile acids in rodents and improve glucose metabolism [82]. While there are many unanswered questions, these data suggest that modulation of segmental intestinal anatomy, and/or changes in intestinal flora which result from these modifications, may improve systemic metabolism via BA-dependent mechanisms.
3. Modulating bile acids as a potential therapeutic approach for obesity and T2D
The close links between plasma levels of bile acids and a host of key metabolic parameters raise the possibility that modulation of BA could be used as a therapeutic approach for the treatment of metabolic diseases. Dietary supplementation with cholic acid (CA) increases energy expenditure, reducing weight gain during high-fat feeding [83]. While the precise mechanism remains uncertain, BA increase expression and activity of the type 2 iodothyronine deiodinase (D2) via a TGR5-cAMP-mediated pathway, thus increasing active thyroid hormone (T3) availability and energy expenditure in tissues critical for thermogenesis, such as BAT [10]. Similarly, CDCA has been shown to increase energy expenditure by induction of UCP1 and activation of thermogenesis in BAT in mice [84]. Bile acid sequestrants, which increase the CA pool size (while reducing CDCA and DCA pools), also reduce glucose, hemoglobin A1c, and cholesterol levels in patients with type 2 diabetes [85-87]. Thus, therapeutic strategies which increase circulating BA levels or modulate relative distribution of active bile acid species could be an effective approach to improving systemic metabolism.
3.1. Bile acid-binding resins
Bile acid binding resins (BABR) (cholestyramine, colestipol, colestimide, and colesevelam) are positively charged nondigestible resins that bind to bile acids in the intestine to form an insoluble complex that is excreted in the feces. BABR have been successfully employed for the treatment of hypercholesterolemia for many years. Recently, the second-generation BABR colestimide and colesevelam were found to improve glycemic control in patients with T2D [86, 88-91]. Several possible mechanisms have been proposed for these effects. BABR not only increase plasma BA but also change the composition of the BA pool [92]. These changes in BA may promote increased energy expenditure, as observed in rodents [93]. In addition, BABRs stimulate the expression of proglucagon and release of GLP1, thus improving incretin-mediated insulin secretion and reducing plasma glucose [94]. This effect of colesevelam was achieved through regulation of FXR/FGF19 and TGR5/GLP-1 signaling pathways [89]. Colestimide also decreases postprandial plasma glucose and increases GLP-1 secretion in patients with T2D [85]. Despite these intriguing possibilities, there is not a clear relationship between BA metabolism and improvements in glycemia, and changes in FGF19 or energy expenditure are not consistently observed in human studies [68, 95]. Nevertheless, BA sequestrants regulate glucose homeostasis, potentially at least in part by modulating FXR- and TGR5-mediated pathways.
3.2. FXR agonists
Since FXR modulates many of the metabolic effects of bile acids, activation of FXR could be another approach to treat metabolic disease [96]. Treatment with the FXR ligand GW4064 significantly decreases plasma glucose, triglycerides, and cholesterol in both wild-type and diabetic db/db mice [50]. 6-ECDCA, another FXR agonist, can decrease glucose, cholesterol, free fatty acid, and triglyceride levels in Zucker fa/fa rats [54] by enhancing glucose disposal, reducing body weight, in parallel with reduced expression of PEPCK and glucose-6-phosphates (G6Pase) in ob/ob mice. Interestingly, these effects of FXR agonists are achieved despite decreased bile acid levels, largely through direct activation of hepatic FXR-SHP and intestinal FXR-FGF15/19 pathways [96]. These data again highlight the importance of FXR pathways in mediating metabolic effects of BA.
3.3. TGR5 agonists
The cell surface receptor TGR5 represents another novel pharmacological target for the treatment of the metabolic syndrome and related disorders [97, 98]. TGR5 can be activated by either synthetic ligands [10, 80], or by BA in a dose-dependent manner, with potency of activation depending on specific BA species: lithocholic acid >deoxycholic acid > chenodeoxycholic acid > cholic acid. In rodents, synthetic TGR5 agonists decrease plasma glucose and insulin levels and protect against weight gain induced by a high-fat diet [64]. The expression and activity of the type 2 deiodinase and energy expenditure can be increased with incubation of skeletal muscle with a synthetic TGR5 agonist [10].
3.4. Therapeutic modulation of BA via manipulation of the intestinal tract and its resident flora
As noted above, bariatric surgery is associated with increased plasma BA levels and alterated composition of BA species. In turn, increased BA may contribute to enhanced FXR and TGR5 activation, leading to reduced hepatic glucose production, increased GLP1 secretion, and increased systemic energy expenditure. In support of this concept, recent data implicate FXR activity as a critical mediator of the beneficial effects of bariatric surgery in rodents [85]. Given the important role of the gut microbiome in modulating bile acid pool size, composition, and enterohepatic recirculation, it is intriguing to consider whether modification of the gut microbiome could promote BA-mediated beneficial changes in metabolism. This could potentially be achieved by altered dietary fatty acid composition [99] or with probiotics which modulate gut flora [100, 101]. For example, one recent study demonstrated that probiotics could increase BA deconjugation, increase fecal BA excretion, and increase hepatic BA synthesis in an FGF-dependent mechanism [101]. These intriguing data provide hope that BA action on the gut microbiome and systemic metabolism could be harnessed to yield beneficial effects similar to those observed after bariatric surgery, but in the absence of invasive surgery. This line of investigation will be an important question for future studies.
4. Summary
Taken together, data from both humans and preclinical animal models demonstrate that BA are important signaling molecules which contribute to regulation of whole-body glucose and lipid metabolism and body weight. Such effects of BA are largely mediated by the nuclear receptor FXR and the G protein-coupled receptor TGR5. Future research employing proteomic, metabolomic, and lipidomic approaches are likely to help in identifying bile acid-related biomarkers which may be useful for predicting and assessing response to BA-related therapy for human obesity and metabolic syndrome. Moreover, novel approaches to altering biliary flow and enterohepatic recirculation, plasma BA levels, composition of BA pools, and downstream effectors of BA signaling pathways should be pursued, as they may be effective strategies for the management of obesity, insulin resistance, type 2 diabetes, and other components of the metabolic syndrome.
Practice Points.
Bile acids not only regulate digestion of lipids but also act as signaling molecules to regulate systemic metabolism and insulin secretion.
Key regulators of metabolic effects of bile acids include the nuclear hormone FXR, the cell surface receptor TGR5, and intestinal bacterial flora.
Bile acid levels and composition of individual bile acids are altered in obesity and type 2 diabetes.
Modulating bile acid levels using bile acid sequestrants, FXR agonists, TGR5 ligands, or bariatric surgery represents a new approach for the treatment of obesity, type 2 diabetes, and the metabolic syndrome.
Research Agenda.
Detailed clinical studies will be required to define the efficacy of FXR or TGR5 ligands in the treatment of human type 2 diabetes.
Determining whether diversion of bile flow using nonsurgical approaches could also be used therapeutically needs to be explored.
Elucidating the factors leading to interindividual differences in bile acid composition, and their effects on metabolic risk, will be critical.
Acknowledgments
The authors gratefully acknowledge grant support from Hebei Health Department of Scientific Research Fund (to HM), P30DK036836 DRC (Joslin Diabetes Center), and the American Diabetes Association (to MEP).
Footnotes
Conflict of Interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Houten SM, Watanabe M, Auwerx J. Endocrine functions of bile acids. EMBO J. 2006;25(7):1419–25. doi: 10.1038/sj.emboj.7601049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2*.Watanabe M, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439(7075):484–9. doi: 10.1038/nature04330. [DOI] [PubMed] [Google Scholar]
- 3.Chiang JY. Bile acid metabolism and signaling. Compr Physiol. 2013;3(3):1191–212. doi: 10.1002/cphy.c120023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohli R, et al. Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab. 2013;98(4):E708–12. doi: 10.1210/jc.2012-3736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonen M, et al. Conjugated bile acids associate with altered rates of glucose and lipid oxidation after Roux-en-Y gastric bypass. Obes Surg. 2012;22(9):1473–80. doi: 10.1007/s11695-012-0673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6*.Patti ME, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring) 2009;17(9):1671–7. doi: 10.1038/oby.2009.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiang JY. Bile acids: regulation of synthesis. J Lipid Res. 2009;50(10):1955–66. doi: 10.1194/jlr.R900010-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiang JY. Regulation of bile acid synthesis. Front Biosci. 1998;3:d176–93. doi: 10.2741/a273. [DOI] [PubMed] [Google Scholar]
- 9.Deo AK, Bandiera SM. Biotransformation of lithocholic acid by rat hepatic microsomes: metabolite analysis by liquid chromatography/mass spectrometry. Drug Metab Dispos. 2008;36(2):442–51. doi: 10.1124/dmd.107.017533. [DOI] [PubMed] [Google Scholar]
- 10.Russell DW. Fifty years of advances in bile acid synthesis and metabolism. J Lipid Res. 2009;50 Suppl:S120–5. doi: 10.1194/jlr.R800026-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hofmann AF, Hagey LR. Bile acids: chemistry, pathochemistry, biology, pathobiology, and therapeutics. Cell Mol Life Sci. 2008;65(16):2461–83. doi: 10.1007/s00018-008-7568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12*.Sayin SI, et al. Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab. 2013;17(2):225–35. doi: 10.1016/j.cmet.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Moschetta A, et al. A phylogenetic survey of biliary lipids in vertebrates. J Lipid Res. 2005;46(10):2221–32. doi: 10.1194/jlr.M500178-JLR200. [DOI] [PubMed] [Google Scholar]
- 14.Hofmann AF, Borgstroem B. The Intraluminal Phase of Fat Digestion in Man: The Lipid Content of the Micellar and Oil Phases of Intestinal Content Obtained during Fat Digestion and Absorption. J Clin Invest. 1964;43:247–57. doi: 10.1172/JCI104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myant NB, Mitropoulos KA. Cholesterol 7 alpha-hydroxylase. J Lipid Res. 1977;18(2):135–53. [PubMed] [Google Scholar]
- 16.Wang H, et al. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol Cell. 1999;3(5):543–53. doi: 10.1016/s1097-2765(00)80348-2. [DOI] [PubMed] [Google Scholar]
- 17.Sinal CJ, et al. Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell. 2000;102(6):731–44. doi: 10.1016/s0092-8674(00)00062-3. [DOI] [PubMed] [Google Scholar]
- 18.Holt JA, et al. Definition of a novel growth factor-dependent signal cascade for the suppression of bile acid biosynthesis. Genes Dev. 2003;17(13):1581–91. doi: 10.1101/gad.1083503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu C, et al. Increased carbon tetrachloride-induced liver injury and fibrosis in FGFR4-deficient mice. Am J Pathol. 2002;161(6):2003–10. doi: 10.1016/S0002-9440(10)64478-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xie W, et al. An essential role for nuclear receptors SXR/PXR in detoxification of cholestatic bile acids. Proc Natl Acad Sci U S A. 2001;98(6):3375–80. doi: 10.1073/pnas.051014398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Makishima M, et al. Vitamin D receptor as an intestinal bile acid sensor. Science. 2002;296(5571):1313–6. doi: 10.1126/science.1070477. [DOI] [PubMed] [Google Scholar]
- 22*.Haeusler RA, et al. Impaired generation of 12-hydroxylated bile acids links hepatic insulin signaling with dyslipidemia. Cell Metab. 2012;15(1):65–74. doi: 10.1016/j.cmet.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pathak P, Li T, Chiang JY. Retinoic acid-related orphan receptor alpha regulates diurnal rhythm and fasting induction of sterol 12alpha-hydroxylase in bile acid synthesis. J Biol Chem. 2013;288(52):37154–65. doi: 10.1074/jbc.M113.485987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parks DJ, et al. Bile acids: natural ligands for an orphan nuclear receptor. Science. 1999;284(5418):1365–8. doi: 10.1126/science.284.5418.1365. [DOI] [PubMed] [Google Scholar]
- 25.Nervi FO, Severin CH, Valdivieso VD. Bile acid pool changes and regulation of cholate synthesis in experimental diabetes. Biochim Biophys Acta. 1978;529(2):212–23. doi: 10.1016/0005-2760(78)90064-4. [DOI] [PubMed] [Google Scholar]
- 26.Subbiah MT, Yunker RL. Cholesterol 7 alpha-hydroxylase of rat liver: an insulin sensitive enzyme. Biochem Biophys Res Commun. 1984;124(3):896–902. doi: 10.1016/0006-291x(84)91042-8. [DOI] [PubMed] [Google Scholar]
- 27.Lefebvre P, et al. Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev. 2009;89(1):147–91. doi: 10.1152/physrev.00010.2008. [DOI] [PubMed] [Google Scholar]
- 28.Thomas C, et al. Targeting bile-acid signalling for metabolic diseases. Nat Rev Drug Discov. 2008;7(8):678–93. doi: 10.1038/nrd2619. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen A, Bouscarel B. Bile acids and signal transduction: role in glucose homeostasis. Cell Signal. 2008;20(12):2180–97. doi: 10.1016/j.cellsig.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 30.Eloranta JJ, Kullak-Ublick GA. The role of FXR in disorders of bile acid homeostasis. Physiology (Bethesda) 2008;23:286–95. doi: 10.1152/physiol.00020.2008. [DOI] [PubMed] [Google Scholar]
- 31.Maruyama T, et al. Identification of membrane-type receptor for bile acids (M-BAR) Biochem Biophys Res Commun. 2002;298(5):714–9. doi: 10.1016/s0006-291x(02)02550-0. [DOI] [PubMed] [Google Scholar]
- 32.Vassileva G, et al. Targeted deletion of Gpbar1 protects mice from cholesterol gallstone formation. Biochem J. 2006;398(3):423–30. doi: 10.1042/BJ20060537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angelin B, et al. Bile acid kinetics in relation to endogenous tryglyceride metabolism in various types of hyperlipoproteinemia. J Lipid Res. 1978;19(8):1004–16. [PubMed] [Google Scholar]
- 34.Angelin B, et al. Effects of cholestyramine and chenodeoxycholic acid on the metabolism of endogenous triglyceride in hyperlipoproteinemia. J Lipid Res. 1978;19(8):1017–24. [PubMed] [Google Scholar]
- 35.Sirvent A, et al. The farnesoid X receptor induces very low density lipoprotein receptor gene expression. FEBS Lett. 2004;566(1-3):173–7. doi: 10.1016/j.febslet.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 36*.Watanabe M, et al. Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c. J Clin Invest. 2004;113(10):1408–18. doi: 10.1172/JCI21025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lambert G, et al. The farnesoid X-receptor is an essential regulator of cholesterol homeostasis. J Biol Chem. 2003;278(4):2563–70. doi: 10.1074/jbc.M209525200. [DOI] [PubMed] [Google Scholar]
- 38.Hanniman EA, et al. Loss of functional farnesoid X receptor increases atherosclerotic lesions in apolipoprotein E-deficient mice. J Lipid Res. 2005;46(12):2595–604. doi: 10.1194/jlr.M500390-JLR200. [DOI] [PubMed] [Google Scholar]
- 39.Mencarelli A, et al. Antiatherosclerotic effect of farnesoid X receptor. Am J Physiol Heart Circ Physiol. 2009;296(2):H272–81. doi: 10.1152/ajpheart.01075.2008. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Y, et al. FXR deficiency causes reduced atherosclerosis in Ldlr-/- mice. Arterioscler Thromb Vasc Biol. 2006;26(10):2316–21. doi: 10.1161/01.ATV.0000235697.35431.05. [DOI] [PubMed] [Google Scholar]
- 41.Hartman HB, et al. Activation of farnesoid X receptor prevents atherosclerotic lesion formation in LDLR-/- and apoE-/- mice. J Lipid Res. 2009;50(6):1090–100. doi: 10.1194/jlr.M800619-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pineda Torra I, et al. Bile acids induce the expression of the human peroxisome proliferator-activated receptor alpha gene via activation of the farnesoid X receptor. Mol Endocrinol. 2003;17(2):259–72. doi: 10.1210/me.2002-0120. [DOI] [PubMed] [Google Scholar]
- 43.Savkur RS, et al. Regulation of pyruvate dehydrogenase kinase expression by the farnesoid X receptor. Biochem Biophys Res Commun. 2005;329(1):391–6. doi: 10.1016/j.bbrc.2005.01.141. [DOI] [PubMed] [Google Scholar]
- 44.Claudel T, Staels B, Kuipers F. The Farnesoid X receptor: a molecular link between bile acid and lipid and glucose metabolism. Arterioscler Thromb Vasc Biol. 2005;25(10):2020–30. doi: 10.1161/01.ATV.0000178994.21828.a7. [DOI] [PubMed] [Google Scholar]
- 45.Ozcan U, et al. Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science. 2006;313(5790):1137–40. doi: 10.1126/science.1128294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cha BH, et al. The role of tauroursodeoxycholic acid on adipogenesis of human adipose-derived stem cells by modulation of ER stress. Biomaterials. 2014;35(9):2851–8. doi: 10.1016/j.biomaterials.2013.12.067. [DOI] [PubMed] [Google Scholar]
- 47.Malisova L, et al. Ursodeoxycholic acid but not tauroursodeoxycholic acid inhibits proliferation and differentiation of human subcutaneous adipocytes. PLoS One. 2013;8(12):e82086. doi: 10.1371/journal.pone.0082086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kobayashi M, et al. Prevention and treatment of obesity, insulin resistance, and diabetes by bile acid-binding resin. Diabetes. 2007;56(1):239–47. doi: 10.2337/db06-0353. [DOI] [PubMed] [Google Scholar]
- 49.Ma K, et al. Farnesoid X receptor is essential for normal glucose homeostasis. J Clin Invest. 2006;116(4):1102–9. doi: 10.1172/JCI25604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Y, et al. Activation of the nuclear receptor FXR improves hyperglycemia and hyperlipidemia in diabetic mice. Proc Natl Acad Sci U S A. 2006;103(4):1006–11. doi: 10.1073/pnas.0506982103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fang Y, et al. Conjugated bile acids regulate hepatocyte glycogen synthase activity in vitro and in vivo via Galphai signaling. Mol Pharmacol. 2007;71(4):1122–8. doi: 10.1124/mol.106.032060. [DOI] [PubMed] [Google Scholar]
- 52.Bouscarel B, Fromm H, Nussbaum R. Ursodeoxycholate mobilizes intracellular Ca2+ and activates phosphorylase a in isolated hepatocytes. Am J Physiol. 1993;264(2 Pt 1):G243–51. doi: 10.1152/ajpgi.1993.264.2.G243. [DOI] [PubMed] [Google Scholar]
- 53.Li T, et al. Transgenic expression of cholesterol 7alpha-hydroxylase in the liver prevents high-fat diet-induced obesity and insulin resistance in mice. Hepatology. 2010;52(2):678–90. doi: 10.1002/hep.23721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cipriani S, et al. FXR activation reverses insulin resistance and lipid abnormalities and protects against liver steatosis in Zucker (fa/fa) obese rats. J Lipid Res. 2010;51(4):771–84. doi: 10.1194/jlr.M001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamagata K, et al. Bile acids regulate gluconeogenic gene expression via small heterodimer partner-mediated repression of hepatocyte nuclear factor 4 and Foxo1. J Biol Chem. 2004;279(22):23158–65. doi: 10.1074/jbc.M314322200. [DOI] [PubMed] [Google Scholar]
- 56.Renga B, et al. The bile acid sensor FXR regulates insulin transcription and secretion. Biochim Biophys Acta. 2010;1802(3):363–72. doi: 10.1016/j.bbadis.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 57.Cariou B, et al. The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice. J Biol Chem. 2006;281(16):11039–49. doi: 10.1074/jbc.M510258200. [DOI] [PubMed] [Google Scholar]
- 58.Prawitt J, et al. Farnesoid X receptor deficiency improves glucose homeostasis in mouse models of obesity. Diabetes. 2011;60(7):1861–71. doi: 10.2337/db11-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kawamata Y, et al. A G protein-coupled receptor responsive to bile acids. J Biol Chem. 2003;278(11):9435–40. doi: 10.1074/jbc.M209706200. [DOI] [PubMed] [Google Scholar]
- 60.Katsuma S, Hirasawa A, Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun. 2005;329(1):386–90. doi: 10.1016/j.bbrc.2005.01.139. [DOI] [PubMed] [Google Scholar]
- 61.Poole DP, et al. Expression and function of the bile acid receptor GpBAR1 (TGR5) in the murine enteric nervous system. Neurogastroenterol Motil. 2010;22(7):814–25. e227–8. doi: 10.1111/j.1365-2982.2010.01487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mussig K, et al. Preliminary report: genetic variation within the GPBAR1 gene is not associated with metabolic traits in white subjects at an increased risk for type 2 diabetes mellitus. Metabolism. 2009;58(12):1809–11. doi: 10.1016/j.metabol.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 63.Maruyama T, et al. Targeted disruption of G protein-coupled bile acid receptor 1 (Gpbar1/M-Bar) in mice. J Endocrinol. 2006;191(1):197–205. doi: 10.1677/joe.1.06546. [DOI] [PubMed] [Google Scholar]
- 64.Sato H, et al. Anti-hyperglycemic activity of a TGR5 agonist isolated from Olea europaea. Biochem Biophys Res Commun. 2007;362(4):793–8. doi: 10.1016/j.bbrc.2007.06.130. [DOI] [PubMed] [Google Scholar]
- 65.Shaham O, et al. Metabolic profiling of the human response to a glucose challenge reveals distinct axes of insulin sensitivity. Mol Syst Biol. 2008;4:214. doi: 10.1038/msb.2008.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cariou B, et al. Fasting plasma chenodeoxycholic acid and cholic acid concentrations are inversely correlated with insulin sensitivity in adults. Nutr Metab (Lond) 2011;8(1):48. doi: 10.1186/1743-7075-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Haeusler RA, et al. Human insulin resistance is associated with increased plasma levels of 12alpha-hydroxylated bile acids. Diabetes. 2013;62(12):4184–91. doi: 10.2337/db13-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brufau G, et al. Improved glycemic control with colesevelam treatment in patients with type 2 diabetes is not directly associated with changes in bile acid metabolism. Hepatology. 2010;52(4):1455–64. doi: 10.1002/hep.23831. [DOI] [PubMed] [Google Scholar]
- 69*.Wewalka M, et al. Fasting serum taurine-conjugated bile acids are elevated in type 2 diabetes and do not change with intensification of insulin. J Clin Endocrinol Metab. 2014;99(4):1442–51. doi: 10.1210/jc.2013-3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schauer PR, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes -3-Year Outcomes. N Engl J Med. 2014 doi: 10.1056/NEJMoa1401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pournaras DJ, et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology. 2012;153(8):3613–9. doi: 10.1210/en.2011-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gerhard GS, et al. A role for fibroblast growth factor 19 and bile acids in diabetes remission after Roux-en-Y gastric bypass. Diabetes Care. 2013;36(7):1859–64. doi: 10.2337/dc12-2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Steinert RE, et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring) 2013;21(12):E660–8. doi: 10.1002/oby.20522. [DOI] [PubMed] [Google Scholar]
- 74*.Bojsen-Moller KN, et al. Early enhancements of hepatic and later of peripheral insulin sensitivity combined with increased postprandial insulin secretion contribute to improved glycemic control after Roux-en-Y gastric bypass. Diabetes. 2013 doi: 10.2337/db13-1307. [DOI] [PubMed] [Google Scholar]
- 75.Goldfine AB, et al. Necdin and E2F4 are modulated by rosiglitazone therapy in diabetic human adipose and muscle tissue. Diabetes. 2006;55(3):640–50. doi: 10.2337/diabetes.55.03.06.db05-1015. [DOI] [PubMed] [Google Scholar]
- 76.Myronovych A, et al. Vertical sleeve gastrectomy reduces hepatic steatosis while increasing serum bile acids in a weight-loss-independent manner. Obesity (Silver Spring) 2014;22(2):390–400. doi: 10.1002/oby.20548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77*.Ryan KK, et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014 doi: 10.1038/nature13135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahmad NN, Pfalzer A, Kaplan LM. Roux-en-Y gastric bypass normalizes the blunted postprandial bile acid excursion associated with obesity. Int J Obes (Lond) 2013;37(12):1553–9. doi: 10.1038/ijo.2013.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pournaras DJ, le Roux CW. Are bile acids the new gut hormones? Lessons from weight loss surgery models. Endocrinology. 2013;154(7):2255–6. doi: 10.1210/en.2013-1383. [DOI] [PubMed] [Google Scholar]
- 80.Duan J, et al. Mid to distal small bowel resection with the preservation of the terminal ileum improves glucose homeostasis in diabetic rats by activating the hindgut-dependent mechanism. J Gastrointest Surg. 2014;18(6):1186–93. doi: 10.1007/s11605-014-2507-3. [DOI] [PubMed] [Google Scholar]
- 81*.Cummings BP, et al. Bile-acid-mediated decrease in endoplasmic reticulum stress: a potential contributor to the metabolic benefits of ileal interposition surgery in UCD-T2DM rats. Dis Model Mech. 2013;6(2):443–56. doi: 10.1242/dmm.010421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Habegger KM, et al. GLP-1R responsiveness predicts individual gastric bypass efficacy on glucose tolerance in rats. Diabetes. 2014;63(2):505–13. doi: 10.2337/db13-0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liaset B, et al. Nutritional regulation of bile acid metabolism is associated with improved pathological characteristics of the metabolic syndrome. J Biol Chem. 2011;286(32):28382–95. doi: 10.1074/jbc.M111.234732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Teodoro JS, et al. Enhancement of brown fat thermogenesis using chenodeoxycholic acid in mice. Int J Obes (Lond) 2013 doi: 10.1038/ijo.2013.230. [DOI] [PubMed] [Google Scholar]
- 85.Staels B, Kuipers F. Bile acid sequestrants and the treatment of type 2 diabetes mellitus. Drugs. 2007;67(10):1383–92. doi: 10.2165/00003495-200767100-00001. [DOI] [PubMed] [Google Scholar]
- 86.Fonseca VA, et al. Colesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapy. Diabetes Care. 2008;31(8):1479–84. doi: 10.2337/dc08-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Watanabe M, et al. Lowering bile acid pool size with a synthetic farnesoid X receptor (FXR) agonist induces obesity and diabetes through reduced energy expenditure. J Biol Chem. 2011;286(30):26913–20. doi: 10.1074/jbc.M111.248203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Suzuki T, et al. Colestimide lowers plasma glucose levels and increases plasma glucagon-like PEPTIDE-1 (7-36) levels in patients with type 2 diabetes mellitus complicated by hypercholesterolemia. J Nippon Med Sch. 2007;74(5):338–43. doi: 10.1272/jnms.74.338. [DOI] [PubMed] [Google Scholar]
- 89.Shang Q, et al. Colesevelam improves insulin resistance in a diet-induced obesity (F-DIO) rat model by increasing the release of GLP-1. Am J Physiol Gastrointest Liver Physiol. 2010;298(3):G419–24. doi: 10.1152/ajpgi.00362.2009. [DOI] [PubMed] [Google Scholar]
- 90.Goldberg RB, et al. Efficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapy. Arch Intern Med. 2008;168(14):1531–40. doi: 10.1001/archinte.168.14.1531. [DOI] [PubMed] [Google Scholar]
- 91.Beysen C, et al. Effect of bile acid sequestrants on glucose metabolism, hepatic de novo lipogenesis, and cholesterol and bile acid kinetics in type 2 diabetes: a randomised controlled study. Diabetologia. 2012;55(2):432–42. doi: 10.1007/s00125-011-2382-3. [DOI] [PubMed] [Google Scholar]
- 92.Insull W., Jr Clinical utility of bile acid sequestrants in the treatment of dyslipidemia: a scientific review. South Med J. 2006;99(3):257–73. doi: 10.1097/01.smj.0000208120.73327.db. [DOI] [PubMed] [Google Scholar]
- 93.Watanabe M, et al. Bile acid binding resin improves metabolic control through the induction of energy expenditure. PLoS One. 2012;7(8):e38286. doi: 10.1371/journal.pone.0038286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Harach T, et al. TGR5 potentiates GLP-1 secretion in response to anionic exchange resins. Sci Rep. 2012;2:430. doi: 10.1038/srep00430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brufau G, et al. Plasma bile acids are not associated with energy metabolism in humans. Nutr Metab (Lond) 2010;7:73. doi: 10.1186/1743-7075-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Matsubara T, Li F, Gonzalez FJ. FXR signaling in the enterohepatic system. Mol Cell Endocrinol. 2013;368(1-2):17–29. doi: 10.1016/j.mce.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stepanov V, Stankov K, Mikov M. The bile acid membrane receptor TGR5: a novel pharmacological target in metabolic, inflammatory and neoplastic disorders. J Recept Signal Transduct Res. 2013;33(4):213–23. doi: 10.3109/10799893.2013.802805. [DOI] [PubMed] [Google Scholar]
- 98.Duboc H, Tache Y, Hofmann AF. The bile acid TGR5 membrane receptor: From basic research to clinical application. Dig Liver Dis. 2014;46(4):302–312. doi: 10.1016/j.dld.2013.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Costarelli V, Sanders TA. Acute effects of dietary fat composition on postprandial plasma bile acid and cholecystokinin concentrations in healthy premenopausal women. Br J Nutr. 2001;86(4):471–7. doi: 10.1079/bjn2001431. [DOI] [PubMed] [Google Scholar]
- 100.Roager HM, et al. NCFM affects vitamin E acetate metabolism and intestinal bile acid signature in monocolonized mice. Gut Microbes. 2014;5(3) doi: 10.4161/gmic.28806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101*.Degirolamo C, et al. Microbiota modification with probiotics induces hepatic bile acid synthesis via downregulation of the Fxr-Fgf15 axis in mice. Cell Rep. 2014;7(1):12–8. doi: 10.1016/j.celrep.2014.02.032. [DOI] [PubMed] [Google Scholar]