Child abuse is a non-specific risk factor associated with increased risk for a range of psychiatric and substance use disorders. The paper in this issue by Dannlowski and colleagues [1] adds to a growing body of literature on the mechanisms by which adverse early experiences confer vulnerability to psychiatric illness. The paper by Nikulina and colleagues [2] delineate further genetic and other factors that account for individual differences in the outcomes of adults who were abused as children.
Dannlowski and colleagues [1] completed structural and functional magnetic resonance imaging (MRI) assessments in a large cohort of carefully screened healthy controls, with a proportion of subjects having histories of child abuse and neglect. While other studies have detected brain changes in trauma controls – individuals with a history of trauma who did not meet current criteria for Posttraumatic Stress Disorder (PTSD), the trauma controls in all prior studies included individuals with current and/or past psychiatric diagnoses other than PTSD [3]. The study by Dannlowski and colleagues is the first to examine the relationship between neuroimaging assessments and dimensional measures of child maltreatment in a healthy, never psychiatrically ill cohort. Given the association between child maltreatment and PTSD and major depression (MDD), they hypothesized a priori brain changes in areas implicated in these disorders. Consistent with this hypothesis, more severe childhood maltreatment was associated with increased amygdala activation during an emotion-processing task, and decreased volume in the hippocampus, anterior cingulate cortex (ACC), orbitofrontal cortex (OFC), medial prefrontal cortex (mPFC), and several other brain regions.
Nikulina and colleagues [2] examined the interaction between monoamine oxidase-A (MAOA) genotype and child maltreatment in predicting MDD, dysthymia, and alcohol use disorder symptoms in adults. They identified sex and race effects that moderated the impact of MAOA genotype on adult outcomes. In the original paper by Caspi and colleagues [4], MAOA genotype was found to moderate the relationship between child maltreatment and antisocial behavior in males, with the high-activity MAOA allele protecting against psychopathology. Nikulina and colleagues reported significant three-way interactions that suggested the low-activity MAOA allele was protective in women and white participants when predicting depressive symptoms, and the high activity allele was protective against depressive symptoms in non-white maltreated females. The authors proposed that 1) the effects of MAOA genotype on antisocial behavior and mood are different; and 2) the direction of the effects of MAOA genotype is different for males and females, and whites and non-whites. Alternatively, they also suggested that their results might be “chance findings.”
So, where do we go from here? Within the field there is a consensus that genes and environment interact to promote the development of depression and other stress-related psychiatric disorders, and agreement that the effects of severe stress are mediated by changes in brain structure and function. However, the nature of gene and environment interactions continues to be elusive, and the clinical significance of identified brain changes are not fully understood. What do we know, and what do we still need to learn to better understand the link between child maltreatment and psychiatric illness?
What we know, Point 1: Many of the brain regions and circuits implicated in the pathophysiology of stress-related psychiatric problems are involved in the stress response
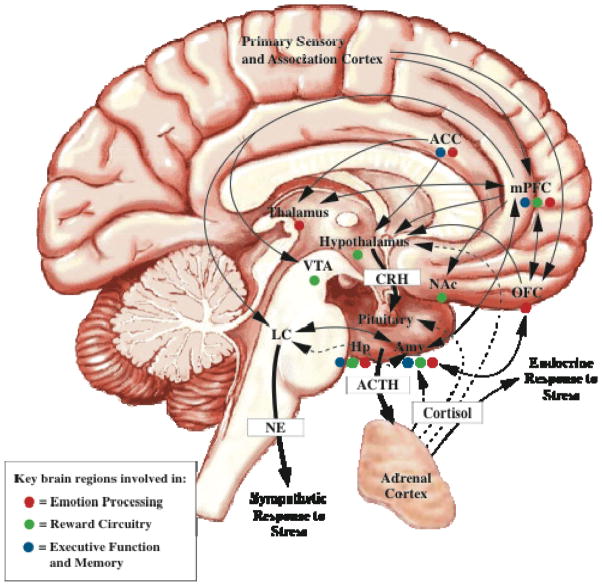
As reviewed elsewhere and depicted in the simplified schematic in Figure 1, the brain responds to stress in an orchestrated manner [5, 6]. The stress response is initiated with the release of corticotropin releasing hormone (CRH) from the hypothalamus. CRH stimulates the release of adrenocorticotropin from the pituitary, which causes release of glucocorticoids (e.g., cortisol) from the adrenals. Glucocorticoids then stimulate CRH release from the amygdala, which in turn initiates norepinephrine release from the locus coeruleus and starts the sympathetic response to stress. The ACC, OFC, and mPFC play an important role in relaying information from primary sensory and association cortices to the amygdala and other subcortical structures, and inputs from these areas and the hippocampus help to attenuate the brain’s response to stress. The stress response also innervates the mesocortical and mesolimbic systems, which includes neurons of the ventral tegmentum area (VTA) that exert a suppressive effect on the stress system, and the nucleus accumbens (NAc), which receives inputs from VTA, amygdala, and mPFC.
Figure 1. Brain Regions Involved In the Stress Response.
As discussed in the text, several brain regions and interconnected neural circuits that regulate emotion, reward, and executive function are also involved in the stress response. Given the overlap in the stress system and these other brain circuits, it is not surprising that severe stress in the form of child maltreatment is associated with increased risk for a range of psychiatric and substance use disorders which are frequently comorbid with one another.
Key: ACC=anterior cingulate cortex; ACTH=adrenocorticotropin hormone; Amy=amygdala; CRH=corticotropin releasing hormone; Hp=hippocampus; LC=locus coerelus; mPFC=medial prefrontal cortex; NAc=nucleus accumbens; OFC=orbitofrontal cortex; VTA=ventral tegmental area. (Adapted from Kaufman and Weder, 2010).
As depicted in Figure 1, many of the brain regions involved in the stress response are key structures in the emotion processing, reward, and executive function circuits --with dysregulation in these brain systems implicated in multiple stress-related psychiatric and substance use disorders [5]. For example, the amygdala, hippocampus, OFC, and mPFC, are key structures implicated in mood and anxiety disorders that are involved in the emotion processing circuit. The NAc and VTA, which receive inputs from multiple PFC areas, hippocampus, amygdala and hypothalamus, are key structures in the reward circuit and are involved in the pathophysiology of alcohol, substance use, and mood disorders. Given the overlap in the stress system and these other brain circuits, it is not surprising that severe stress in the form of child maltreatment is associated with increased risk for a range of psychiatric and substance use disorders.
What we know, Point 2: The brain is not organized according to the psychiatric Diagnostic and Statistical Manual (DSM)
There has been growing frustration with the limitations of the extant psychiatric nomenclature to delineate resilience and disease mechanisms. Consequently, the leadership of the National Institute of Mental Health (NIMH) established the Research Domain Criteria (RDoC) project, which has as its goal devising a new classification system for mental disorders that is informed by genetics, neuroscience, and psychology, and also takes into consideration the impact of trauma on the development of these conditions [7]. The three-way interactions between maltreatment history, MAOA genotype, and the demographic factors examined by Nikulina and colleagues accounted for 3%–5% of the variance in dysthymia symptoms [2]. Effect sizes have been greater in studies when genetic polymorphisms have been examined to account for individual differences in amygdala activation during emotion processing MRI tasks, accounting for approximately 10% of variance [8]. Clearly, however, something is still missing from the equation given the large proportion of unaccounted variance. With increasing appreciation of the role of epigenetics in disease processes [9], the incorporation of new molecular genetic approaches, together a RDoC perspective, will likely enhance risk and resilience research (See NIMH website for the RDoC project, http://www.nimh.nih.gov/research-funding/rdoc/index.shtml).
What we know, Point 3: Genetic and detrimental early environment effects are not fixed
Epigenetic mechanisms play a key role in the acute regulation of genes in response to changes in the environment [10]. Epigenetics refers to functionally relevant modifications to the genome that do not involve a change in DNA nucleotide sequence, but rather alter chromatin packing and affect the likelihood of a given gene product being transcribed. As reviewed elsewhere [10], animal models of neglect suggest early adverse rearing experiences are associated with epigenetic modification of the glucocorticoid receptor gene in the hippocampus. This results in fewer glucocorticoid receptors being made. As these receptors are key in initiating the cascade of events that put the breaks on the stress response, offspring of ‘neglectful’ dams have been found to have increased stress reactivity and exhibit anxious and depression-like behaviors. Epigenetic mechanisms have also been found to mediate brain changes in ocular dominance and visual deficits associated with early monocular deprivation experiments in cats. While these vision and brain changes were originally thought to be permanent, as reviewed elsewhere [10], emerging findings suggest they can be altered by pharmacological and environmental manipulations. Neither the effects of genes, nor early adversity, are fixed.
What we still need to learn
The two papers in this issue have helped to close the gap in our understanding of risk and resilience in individuals maltreated as children, but there is still more to learn. The paper by Dannlowski and colleagues [1] documented associations among structural and functional brain imaging parameters and dimensional measures of child maltreatment in individuals with no lifetime history of psychiatric illness. As the authors noted, these brain changes may serve as vulnerability markers for illness. Normative data on neuroimaging measures are still lacking, however, and we do not yet have brain measures that are diagnostic and predictive of impairment and distress. Nikulina and colleagues [2] identified genetic and demographic factors that accounted for individual differences in depression and alcohol misuse symptoms, although the amount of variance accounted for was relatively small. Longitudinal follow-up studies that utilize a RDoC perspective and integrate molecular genetics and imaging approaches, together with emerging technologies to examine whole genome epigenetic markers, will likely help to further elucidate the mechanisms by which early experiences of child maltreatment confer risk for psychiatric and substance use disorders later in life.
Acknowledgments
This work was supported by grant funding from the NIMH (R01MH077087), the National Center for Posttraumatic Stress Disorder-Veterans Affairs Connecticut , and the VA Depression Research Enhancement Award Program (Veterans Affairs Connecticut.).
Footnotes
Disclosure: Dr. Kaufman has served as a consultant for Bristol-Myers Squibb, Pfizer, Wyeth-Ayerst, Forest Laboratories, Johnson and Johnson Research Pharmaceutical Institute, Shire, Otsuka, and Merck Pharmaceutical.
References
- 1.Dannlowski U, et al. Limbic scars: Long-term consequences of childhood maltreatment revealed by functional and structural MRI. Biological Psychiatry. 2012 doi: 10.1016/j.biopsych.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 2.Nikulina V, Widom CS, BLM Child Abuse and Neglect, MAOA, and Mental Health Outcomes: A Prospective Examination. Biological Psychiatry. 2012 doi: 10.1016/j.biopsych.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woon FL, Sood S, Hedges DW. Hippocampal volume deficits associated with exposure to psychological trauma and posttraumatic stress disorder in adults: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(7):1181–8. doi: 10.1016/j.pnpbp.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Caspi A, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297(5582):851–4. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman J, Weder N. Neurobiology of Early Life Stress: Evolving Concepts. In: Martin Andres, MD, MPH, Scahill Lawrence, PhD, Kratochvil Christopher J., MD, editors. Pediatric Psychopharmacology. Oxford University Press; New York, NY: 2010. pp. 112–123. [Google Scholar]
- 6.Kaufman J, et al. Effects of early adverse experience on brain structure and function: clinical implications. Biol Psychiatry. 2000;48(8):778–790. doi: 10.1016/s0006-3223(00)00998-7. [DOI] [PubMed] [Google Scholar]
- 7.Sanislow CA, et al. Developing constructs for psychopathology research: research domain criteria. J Abnorm Psychol. 2010;119(4):631–9. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- 8.Munafo MR, Brown SM, Hariri AR. Serotonin transporter (5-HTTLPR) genotype and amygdala activation: a meta-analysis. Biol Psychiatry. 2008;63(9):852–7. doi: 10.1016/j.biopsych.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rakyan VK, et al. Epigenome-wide association studies for common human diseases. Nat Rev Genet. 2011;12(8):529–41. doi: 10.1038/nrg3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weder N, Kaufman J. Critical periods revisited: implications for intervention with traumatized children. J Am Acad Child Adolesc Psychiatry. 2011;50(11):1087–9. doi: 10.1016/j.jaac.2011.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]