Abstract
Intrathyroidal metastasis and direct extension of extrathyroidal malignancies can present with palpable thyroid nodules or may be detected as suspicious nodules in a thyroid scan. They can lead to diagnostic difficulty in fine needle aspiration cytology (FNAC) of the thyroid, especially in the absence of any previous history of such malignancies. Here we report an interesting case of intrathyroidal metastasis, which was initially suspected as a primary carcinoma of the thyroid; along with a short summary of a series of 11 cases of carcinomas of extrathyroidal origin, diagnosed in the FNACs of thyroid over the past three years in our institute. Knowledge of the potential diagnostic pitfalls in thyroid FNAC, a proper clinical evaluation, and judicious use of the ancillary techniques will help to attain a proper diagnosis.
Keywords: Cell block, fine needle aspiration cytology, intrathyroidal metastasis, immunohistochemistry
Introduction
Ultrasound imaging (USG), Computed tomography (CT), and various other imaging modalities, including nuclear scans, are increasingly being used for metastasis workup and they have greatly increased the detection of occult metastasis at various sites including thyroid. Fine needle aspiration (FNA) is a sensitive technique, which is used under the guidance of these imaging modalities or as a blind procedure to confirm these lesions. In the thyroid, both metastasis as well as direct extension of carcinomas from adjacent sites, especially the aerodigestive tract, can mimic thyroid malignancies on imaging and can lead to diagnostic difficulties in FNA, when a history regarding the presence of an extrathyroidal malignancy is unavailable. We report an interesting case of intrathyroidal metastasis, which was initially mistaken for a primary malignancy of the thyroid.
Case Report
A 62-year-old lady, a known case of hypothyroidism, presented with weakness of the left upper limb. Magnetic resonance imaging (MRI) of the brain showed an intracranial space-occupying lesion. She was put on empirical anti-tuberculosis treatment, suspecting a tuberculoma; however, her condition worsened. As a part of the workup, USG of her abdomen and neck was performed, which showed a well-defined, hypoechoic lesion, measuring 3 × 5 mm, in the right lobe of the thyroid, without calcification. We obtained a USG-guided FNA from the same. The USG of the abdomen was normal. The FNAC showed cells arranged in papillary and micro-follicular clusters. There were singly scattered plasmacytoid cells as well as binucleated cells. The cells showed minimal nuclear pleomorphism with fine chromatin. Some cells showed fine cytoplasmic granularity. Benign-looking follicular epithelial cells were seen admixed with neoplastic cells. There were no nuclear features of papillary carcinoma of the thyroid [Figure 1]. A possibility of medullary carcinoma of the thyroid was considered. However, in view of atypical morphological features like numerous papillary clusters and a vague acinar pattern, the possibility of an intrathyroidal metastatic tumor could not be excluded. A subsequent CT scan showed well-defined, randomly distributed nodules in both the lungs, suggestive of metastasis. A CT-guided biopsy and immunohistochemistry was performed of the lung nodules. The tumor cells were positive for CK7 and TTF-1; and negative for thyroglobulin and calcitonin, confirming primary adenocarcinoma of the lung.
Figure 1.
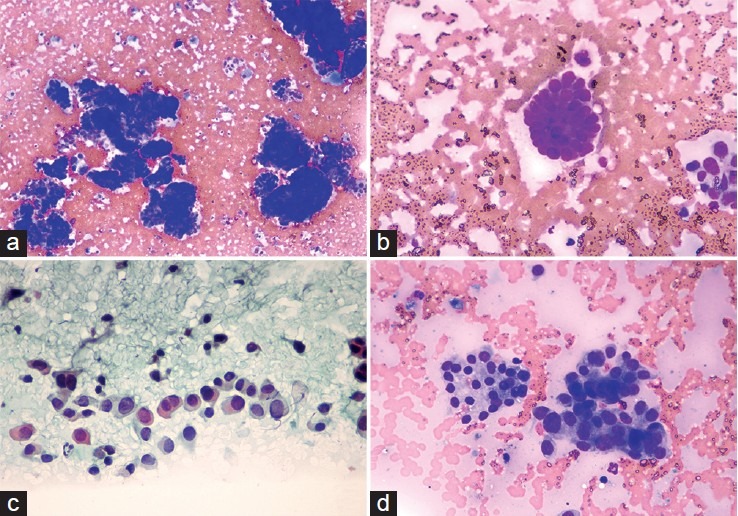
(a) Cytology smear showing neoplastic cells arranged in papillaroid clusters (MGG, ×100); (b) cells show fine granularity of the cytoplasm (MGG, ×400); (c) singly scattered plasmacytoid cells and occasional binucleated cells (Pap, ×400); (d) Neoplastic cells intimately admixed with benign follicular epithelial cells (MGG, ×400)
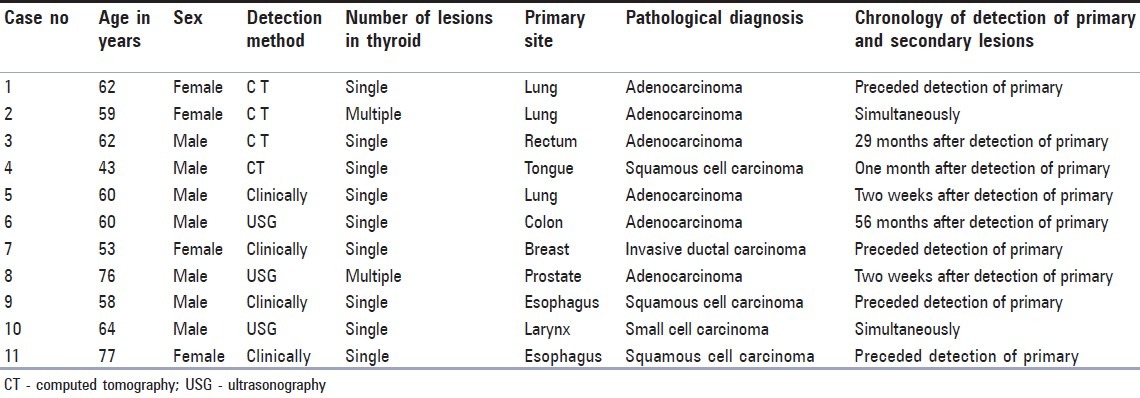
A retrospective audit using the hospital information system of all FNAs of thyroid performed in our institute over a period of three years, from March 2010 to February 2013, revealed a total of 11 cases of carcinomas, of extrathyroidal origin, diagnosed by FNAC. There were a total of 3703 thyroid FNAs in three years, out of which an extrathyroidal type of malignancy was diagnosed in 11 cases, which constituted 0.3%. The cases are summarized in Table 1. The most common malignancy was metastatic adenocarcinoma (six patients), followed by squamous cell carcinoma in three patients, and metastatic invasive ductal carcinoma and small cell carcinoma in one patient each. The most common primary site was the lung. The duration between the detection of primary and secondary tumors ranged from two weeks to 56 months. A delayed metastasis after 56 months was seen in a case of adenocarcinoma of the colon. Another case of rectal adenocarcinoma presented with intrathyroidal metastasis after 29 months. Follow-up is available only in four patients. One patient with carcinoma tongue expired within a month of diagnosis of metastasis. The other three patients were alive at the time of the last follow-up and had survived for a period of nine months (carcinoma colon), 12 months (carcinoma breast), and 28 months (carcinoma prostate) after the diagnosis of intrathyroidal metastasis.
Table 1.
Summary of 11 patients who were diagnosed to have tumors of extrathyroidal origin in FNA of thyroid
Discussion
The exact incidence of secondary tumors of the thyroid is not clear, because it is not often examined or routinely investigated by imaging, during a metastatic workup. Intrathyroidal metastasis is not uncommon, as the thyroid is a highly vascularized organ.[1] The incidence in our experience is 0.3% of all thyroid FNAs compared to an incidence of 7.5% of all neoplastic lesions of the thyroid, in a study by Michelow et al.[2] It ranges from 1.25 to 24% in various autopsy and clinical series.[3] With the increasing use of positron emission tomography (PET) imaging, more cases are likely to be detected in future. Kidney or breast is the most common primary site of malignancy in some series,[1,3,4,5,6] while lung is the most common site in other series.[2,7] Lung is the most common site of primary malignancy in our experience, probably reflecting the burden of lung cancer in India.[8,9] There is a high prevalence of goiter (up to 12.1%) in certain populations of India,[10] which may have an FNA diagnosis and if such patients present with a malignancy elsewhere, the thyroid lesion may not get investigated further and this likely misses at least some cases of secondary cancers of the thyroid. In two of our cases that presented with a thyroid lesion, the initial clinical diagnosis was primary malignancy of the thyroid; both of them were later proved to be metastasis from the lung. The possibility of a secondary malignancy of the thyroid should always be kept in mind. Intrathyroidal metastasis can occur after a prolonged latent period. One of our cases presented 56 months after the diagnosis of colonic adenocarcinoma. In one of the studies, a case of clear cell renal carcinoma presented 185 months after the primary diagnosis,[1] and such long latent periods can distract both the pathologist and the clinician from making a proper diagnosis. Various authors have suggested that in any patient with a previous history of malignant disease, any thyroid swelling must be considered as a potential metastatic deposit and warrants further investigation, especially FNAC.[1,11] Ideally ultrasonography and a guided rather than a blind FNA must investigate all thyroid lesions in such patients, as it can detect even the small foci of metastatic deposits. Another situation is a large thyroid swelling with simultaneous lesions in other sites, especially the lung. In such situations, the diagnostic difficulty will be to distinguish whether the thyroid or lung is the primary site of malignancy or whether both of them are independent primary sites. The judicious use of immunohistochemistry on cell-block preparations or on a biopsy helps to resolve the case. Thyroglobulin is probably the most useful marker in distinguishing lung carcinoma from thryoid cancers, while CK7, CK19, and TTF-1 are not useful, as they can be positive in both malignancies.[12,13] However, thyroglobulin need not be positive in 100% of the thyroid cancers, limiting its use in some situations. A study by Tung et al.[14] has shown that in FNA smears, only 59% of benign nodular goiters and 57% of papillary carcinomas were positive for thyroglobulin. Hence, negative staining does not completely exclude a thyroid origin. Metastatic squamous cell carcinoma is especially difficult to be distinguished from a rare primary squamous cell carcinoma as well as from anaplastic carcinoma of the thyroid. Literature shows that the prognosis of patients presenting with intrathyroidal metastasis is poor, especially in lung cancers.[1,7] However, one of our patients with carcinoma of the prostate survived for over 52 months and a case of invasive ductal carcinoma survived for over a year after the detection of thyroidal metastasis.
To summarize, secondary tumors of the thyroid are uncommon, but can create significant diagnostic dilemmas to the clinician as well as the pathologist. A newly developed thyroid lesion in any person with a known history of malignancy must be taken as a metastatic deposit, unless proven otherwise. All thyroid lesions should be preferably sampled under guidance to avoid sampling errors. A judicial use of ancillary techniques will help to distinguish the primary from the secondary tumors of thyroid.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kim TY, Kim WB, Gong G, Hong SJ, Shong YK. Metastasis to the thyroid diagnosed by fine-needle aspiration biopsy. Clin Endocrinol (Oxf) 2005;62:236–41. doi: 10.1111/j.1365-2265.2005.02206.x. [DOI] [PubMed] [Google Scholar]
- 2.Michelow PM, Leiman G. Metastases to the thyroid gland: Diagnosis by aspiration cytology. Diagn Cytopathol. 1995;13:209–13. doi: 10.1002/dc.2840130306. [DOI] [PubMed] [Google Scholar]
- 3.Nakhjavani MK, Gharib H, Goellner JR, Van Heerdan JA. Metastasis to the thyroid gland. A report of 43 cases. Cancer. 1997;79:574–8. doi: 10.1002/(sici)1097-0142(19970201)79:3<574::aid-cncr21>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 4.Ivy HK. Cancer metastatic to the thyroid: A diagnostic problem. Mayo Clin Proc. 1984;59:856–9. doi: 10.1016/s0025-6196(12)65622-5. [DOI] [PubMed] [Google Scholar]
- 5.Wychulis AR, Beahrs OH, Woolner LB. Metastasis of carcinoma to the thyroid gland. Ann Surg. 1964;160:169–77. doi: 10.1097/00000658-196408000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czech JM, Lichtor TR, Carney JA, Van Heerden JA. Neoplasms metastatic to the thyroid gland. Surg Gynecol Obstet. 1982;155:503–5. [PubMed] [Google Scholar]
- 7.Lam KY, Lo CY. Metastatic tumors of the thyroid gland: A study of 79 cases in Chinese patients. Arch Pathol Lab Med. 1998;122:37–41. [PubMed] [Google Scholar]
- 8.Behera D, Balamugesh T. Lung cancer in India. Indian J Chest Dis Allied Sci. 2004;46:269–81. [PubMed] [Google Scholar]
- 9.Noronha V, Dikshit R, Raut N. Epidemiology of lung cancer in India: Focus on the differences between non-smokers and smokers: A single-center experience. Indian J Cancer. 2012;49:74–81. doi: 10.4103/0019-509X.98925. [DOI] [PubMed] [Google Scholar]
- 10.Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H. High prevalence of undetected thyroid disorders in an iodine sufficient adult south Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- 11.McCabe DP, Farrar WB, Petkov TM, Finkelmeier W, O'Dwyer P, James A. Clinical and pathologic correlations in disease metastatic to the thyroid gland. Am J Surg. 1985;150:519–23. doi: 10.1016/0002-9610(85)90167-9. [DOI] [PubMed] [Google Scholar]
- 12.Jerome Marson V, Mazieres J, Groussard O, Garcia O, Berjaud J, Dahan M, et al. Expression of TTF-1 and cytokeratins in primary and secondary epithelial lung tumors: Correlation with histological type and grade. Histopathology. 2004;45:125–34. doi: 10.1111/j.1365-2559.2004.01893.x. [DOI] [PubMed] [Google Scholar]
- 13.Xue L, Luan Z, Liu Y, Zou S, Jiang J, Wu N, et al. Pulmonary metastasis of a papillary thyroid carcinoma and primary lung adenocarcinoma: Two coincident carcinomas at the same location. Diagn Pathol. 2013;8:26. doi: 10.1186/1746-1596-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tung CC, Chang TC, Hsieh HC. Value of immunoperoxidase staining of thyroglobulin in fine needle aspiration cytology of thyroid diseases. Acta Cytol. 1995;39:396–401. [PubMed] [Google Scholar]


