Abstract
Determining whether a particular treatment works for specific groups of people can help tailor dissemination of evidence-based alcohol treatments. It has been proposed that individuals from different racial groups might have better outcomes in treatments that are sensitive to sociocultural issues that impact alcohol use among these groups. The current study was a secondary analysis of data from the combined behavioral intervention (CBI) condition of the COMBINE study. Those randomly assigned to CBI (n = 776) had the opportunity to receive up to 9 skills training modules, which were chosen by the therapist. The goal of the current study was to determine whether receiving 1 of the CBI modules, drink refusal and social pressure skills training, predicted differential outcomes among African American clients. Results indicated that African American clients who received the drink refusal skills training module (n = 25) had significantly fewer heavy drinking days (d = 0.79) 1 year following treatment than African Americans clients who did not receive the module (n = 35). African American clients who received the module also had significantly fewer heavy drinking days (d = 0.86) than non-Hispanic White clients who received the module (n = 241). Good clinical outcomes at 1 year post treatment were observed among 80% of African Americans who received the module, compared with 54% of African Americans who did not receive the module and 52% of non-Hispanic White clients who did receive the module. Although small sample size limits interpretation, findings provide preliminary evidence supporting the inclusion of drink refusal skills training as part of alcohol interventions for African American clients.
Keywords: alcohol treatment, ethnic minority clients, drink refusal skills training
In light of evidence that many cognitive and behavioral treatments for alcohol dependence are equally effective in reducing alcohol use and alcohol-related problems (Miller & Wilbourne, 2002), it is important for researchers to evaluate whether specific treatments work equally effectively for all clients. With this goal in mind, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) sponsored a workshop to facilitate research on health disparities and alcohol treatment effectiveness among minority individuals (Lowman & Le Fauve, 2003). Based on a series of secondary analyses of existing data (Brower & Carey, 2003; Morgenstern & Bux, 2003; Taylor, 2003; Tonigan, 2003), the group concluded that alcohol treatment outcomes did not significantly differ for African American and White clients despite pretreatment health disparities (greater family history of substance abuse, more prior treatment episodes, and poorer physical health among African Americans) that would be expected to predict less positive treatment outcomes among African Americans (Lowman & Le Fauve, 2003). As noted by Brower and Carey (2003), previous studies of alcohol treatment outcome differences between African American and White clients have produced mixed results. The investigators attending the workshop concluded that more research needs to be conducted to determine whether salient sociocultural influences could explain outcomes. The investigators hypothesized that greater social support among African Americans and “unidentified beneficial mediators of treatment process and outcomes” (Lowman & Le Fauve, 2003, p. 1325) could explain positive posttreatment outcomes in the face of negative prognostic indicators at baseline.
The studies conducted for the NIAAA workshop evaluated whether specific treatments (e.g., cognitive–behavioral treatment) were equally effective; however, they recommended that future research be conducted to determine whether targeting minority-specific influences could result in better outcomes (Tonigan, 2003). For example, among African Americans, social influences, such as peer drinking and social pressure to drink, have been shown to be significantly associated with alcohol use (Griffin, Scheier, Botvin, & Diaz, 2000; Williams, Epstein, Botvin, Schinke, & Diaz, 1998), risky drinking (Beal, Ausiello, & Perrin, 2001), and alcohol treatment outcomes (Brower & Carey, 2003). Likewise, greater alcohol refusal skills in responding to social pressures to drink have been associated with a lower likelihood of drinking among minority youth (Epstein, Griffin, & Botvin, 2001; Williams et al., 1998). Finally, among individuals enrolled in substance abuse treatment, African American males have been shown to have significantly greater social exposure to alcohol (defined as the number of times someone used or offered the individual alcohol or drugs) than Caucasian males (Walton, Blow, & Booth, 2001). Together, the studies of alcohol use and social influences among African Americans suggest that targeting drink refusal skills could be an important treatment component among African American clients.
The recent development of an effective multicomponent treatment for alcohol dependence, combined behavioral intervention (CBI; Longabaugh, Zweben, LoCastro, & Miller, 2005), provides an opportunity to evaluate whether certain treatment components are differentially effective. CBI was developed for the COMBINE study (COMBINE Study Research Group, 2003), a multisite randomized clinical trial designed to test the effectiveness of pharmacotherapy with or without CBI in the treatment of alcohol dependence. Results indicated that CBI, with or without conjoint pharmacotherapy, resulted in significant reductions in heavy drinking up to 1 year following treatment (Anton et al., 2006; Donovan et al., 2008).
The current study was a secondary analysis of the COMBINE data to evaluate differences in drinking outcomes between African American and non-Hispanic White clients who received the CBI, while controlling for baseline characteristics and treatment group (i.e., received naltrexone, acamprosate, placebo). The primary goal of the current study was to explore whether administration of the drink refusal and social pressures skills training module resulted in differential drinking outcomes across racial groups. It was hypothesized that a skills training component that targeted responses to social influences and drink refusal would be particularly effective for African Americans, in comparison to non-Hispanic Whites.
Method
The data for this study are from the COMBINE study (Anton et al., 2006), a multisite randomized trial designed to examine the effect of combining pharmacotherapy (naltrexone or acamprosate) with behavioral intervention for alcohol dependence. Details of the rationale and procedures of the COMBINE study are described in detail elsewhere (COMBINE Study Research Group, 2003).
Participants
The sample was recruited from inpatient and outpatient referrals at the study sites and throughout the community. The final sample included 1,383 participants from 11 sites throughout the United States. The current study focused on data from the 776 individuals who were randomly assigned to the CBI condition. Thus, those in the COMBINE study who received medications without CBI were excluded. The subsample was 31% female and 69% male. Approximately 23% of the subsample self-identified as ethnic minorities. Participants identified as follows: 76.7% non-Hispanic White, 10.7% Hispanic American, 7.7% African American, 1.5% American Indian or Alaska Native, 1.0% multiracial, 0.5% Asian American or Pacific Islander, and 1.8% “other races” (as defined by the COMBINE investigators). The mean age of the subsample was 44 years, 70% had at least 12 years of education, and 43% were married.
Procedure and Assessment
On meeting inclusion and exclusion criteria, participants completed a baseline assessment and were randomly assigned to treatment. Those randomly assigned to the CBI (n = 776) had a maximum of 20 treatments sessions available to them over the 16 weeks. Participants were subsequently followed for 52 weeks posttreatment.
CBI was a multiple phase treatment. In the first phase, therapists used motivational interviewing techniques to build client’s motivation for change. The second phase consisted of conducting a functional analysis and developing a treatment plan. In the third phase, CBI was individualized to each client’s situation and needs. Treatment procedures were drawn from a menu of nine cognitive–behavioral skills training modules, and the selection of particular modules was based on the therapist’s discretion, the treatment plan, and the therapist’s assessment of the client’s personal needs and preferences. The drink refusal and social pressures module incorporated several components, including a description of the rationale that many clients resume drinking in response to social pressure, an assessment of the direct and indirect social pressures experienced by the client, an assessment of the coping responses most commonly used by the client in response to social pressure situations, and behavioral rehearsal of positive coping behaviors that can be used in social pressure situations. Thirty-nine percent (n = 302) of the sample received the drink refusal skills module (241 non-Hispanic White clients and 61 ethnic minorities [25 African Americans]).
Measures
A complete list of all assessments and schedule of assessments can be found in the previous COMBINE publication (COMBINE Study Research Group, 2003). In the current study, data from the Form 90 interview (Miller & Del Boca, 1994) was used to measure drinking outcomes, and the Drinker Inventory of Consequences (Miller, Tonigan, & Longabaugh, 1995) was used to determine whether clients experienced consequences as a result of drinking.
The primary outcome measures used in the current analyses, percentage of heavy drinking days and composite clinical outcomes 1 year following treatment, were used because they combined both frequency and intensity of drinking and presence of alcohol-related problems. Also, both measures were used as primary outcome measures in the main outcomes article (Anton et al., 2006). Percentage of heavy drinking days was defined as the percentage of days, in a 30-day period, when the individual had four or more drinks per day for women or five or more drinks per day for men. Percentage of heavy drinking days was transformed to reduce nonnormality using a square root transformation. Composite clinical outcome was categorized, based on the categorizations used in the original COMBINE study (see Anton et al., 2006) as (a) being abstinent, (b) moderately drinking without problems, (c) heavy drinking without problems or moderate drinking with problems, and (d) heavy drinking with problems (Cisler & Zweben, 1999). Moderate drinking was defined by the COMBINE investigators as a maximum number of drinks per week (11 for women, 14 for men) and having no more than 2 days of consuming three or more drinks for women and four or more drinks for men. Alcohol problems were defined by the COMBINE investigators as endorsing three or more items on the Drinker Inventory of Consequences, which assesses 45 different drinking consequences.
Data Analytic Plan
To test the hypothesis described above, we estimated regression models using MPlus Version 5.21 (Muthén & Muthén, 2007). Racial group (non-Hispanic White or African American) and receiving the drink refusal skills module (yes or no) were both dummy coded.1 We examined the direct effects of racial group and receiving the module and their interaction using moderated regression models (Aiken & West, 1991). For the percentage of heavy drinking days outcome, we used a moderated linear regression model; for the clinical outcome measure, we used a moderated multinomial logistic regression model. Considering the complex sampling design in the COMBINE study (participants recruited from 11 sites), all parameters were estimated using a weighted maximum likelihood function, and all standard errors were computed using a sandwich estimator, which adjusts the standard errors for differences across sites.2 Maximum likelihood provides the estimated variance–covariance matrix for the available data; therefore, all available data were included in the models. Maximum likelihood is a preferred method for estimation when some data are missing, assuming that data are missing at random (Schafer & Graham, 2002).
Results
Descriptive statistics for percentage of heavy drinking days and drinking consequences for the total sample and by subgroups are included in Table 1. Preliminary analyses were conducted to determine baseline differences between those who did and did not receive the drink refusal skills module and between racial groups (African American or non-Hispanic White) on demographic measures (gender, income, age, years of education), family history of alcohol dependence, number of comorbid conditions, severity of alcohol dependence, baseline drinking, baseline readiness to change, baseline drinking-related problems, working alliance, treatment attendance, treatment history, percentage of drinkers in the social network, and social support. Differences between module groups (those who did or did not receive the module) were identified for gross yearly income and client-rated therapeutic alliance. Individuals who received the module had a higher income, t(763) = −2.82, p = .005, and stronger therapeutic alliance, t(614) = −2.25, p = .03. Differences between non-Hispanic Whites and African Americans were identified for several measures, including gross yearly income, years of education, percentage of drinkers in the social network, and having a supportive significant other. African Americans had a lower income, t(646) = 6.65, p < .005, fewer years of education, t(641) = 6.39, p < .005, lower percentage of drinkers in their social network, t(649) = 6.78, p < .005, and were more likely to report having a supportive significant other, t(629) = −2.58, p = .01. All measures that were significantly different between module and racial groups were included in all subsequent analyses. In addition, COMBINE study treatment conditions (naltrexone, acamprosate) were included as covariates.
Table 1.
Means (Standard Deviations) for Primary Measures for the Total Combined Behavioral Intervention Sample and Relevant Subgroups
| Total sample | Did not receive drink refusal skills module |
Received drink refusal skills module | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Total (N = 655) | Non-Hispanic Whites (n = 595) |
African Americans (n = 60) |
Non-Hispanic Whites (n = 354) |
African Americans (n = 35) |
Non-Hispanic Whites (n = 241) |
African Americans (n = 25) |
| % heavy drinking days baseline | 65.48 (29.16) | 65.43 (28.92) | 66.16 (30.04) | 65.17 (29.77) | 65.83 (27.70) | 66.37 (30.43) | 65.87 (30.11) |
| % heavy drinking days 1 year posttreatment | 25.29 (34.09) | 26.36 (34.52) | 13.41 (24.79) | 27.98 (35.26) | 24.19 (33.48) | 20.44 (29.77) | 3.65 (9.40) |
| Drinking consequences baseline | 46.89 (20.05) | 46.46 (19.77) | 47.35 (20.49) | 47.08 (20.78) | 45.55 (18.17) | 48.94 (23.20) | 45.12 (16.15) |
| Drinking consequences one year posttreatment | 20.01 (21.90) | 19.83 (21.43) | 18.26 (24.42) | 22.31 (21.94) | 16.79 (20.44) | 20.96 (26.70) | 15.05 (21.59) |
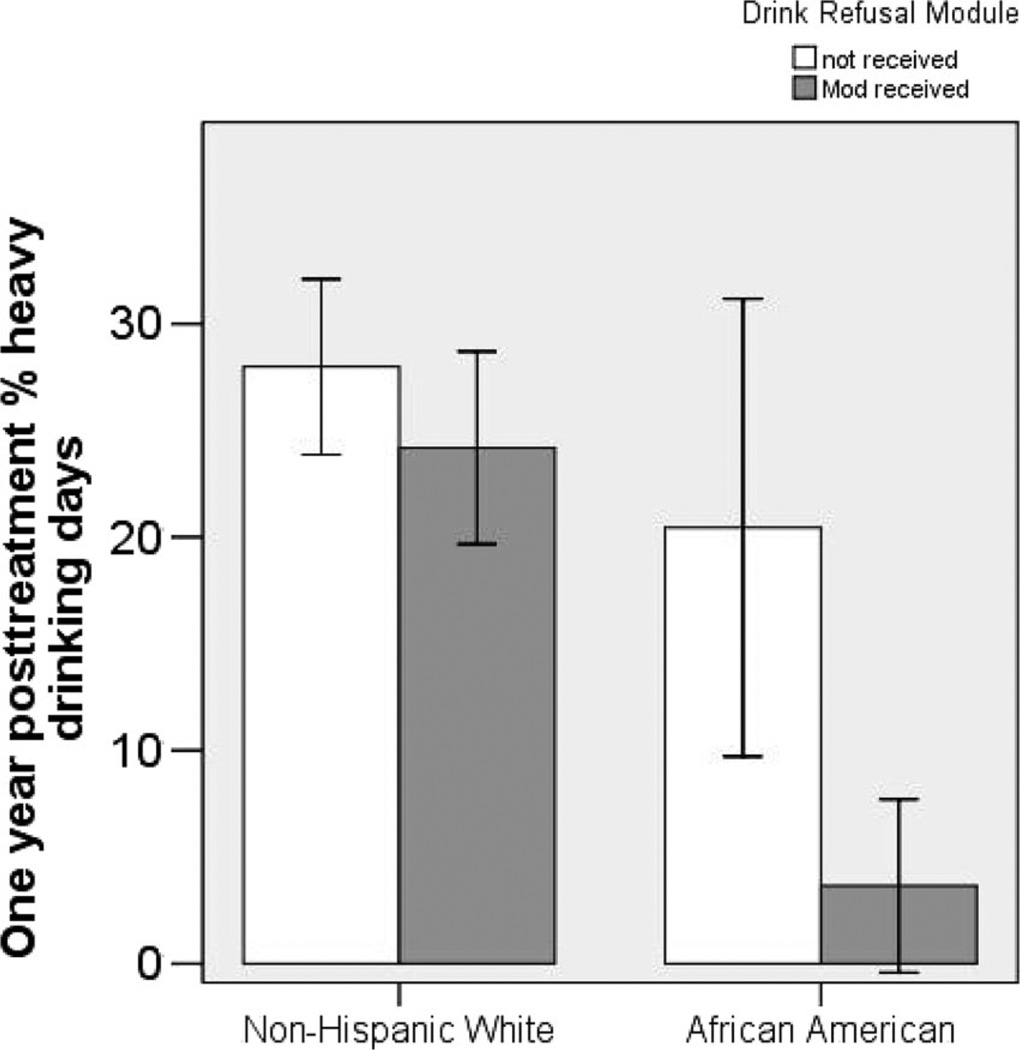
Moderated regression analyses were conducted to determine whether African Americans had better outcomes if they received the drink refusal and social pressures skills training module. Only the main effect of race (B = −0.97, SE = 0.26, = − ".08) and the interaction between race and receiving the drink refusal skills module (B = −1.63, SE = 0.75, = = −.09) were significant predictors of percentage of heavy drinking days 1 year following treatment. As seen in Figure 1, African Americans who received the module had significantly fewer heavy drinking days than African Americans who did not receive the module (d = 0.79) and fewer heavy drinking days than non-Hispanic Whites who did receive the module (d = 0.86).
Figure 1.
Percentage of heavy drinking days 1 year following treatment for non-Hispanic Whites and African Americans who did and did not received the drink refusal skills module. Error bars indicate the 95% confidence intervals around the average percentage of heavy drinking days.
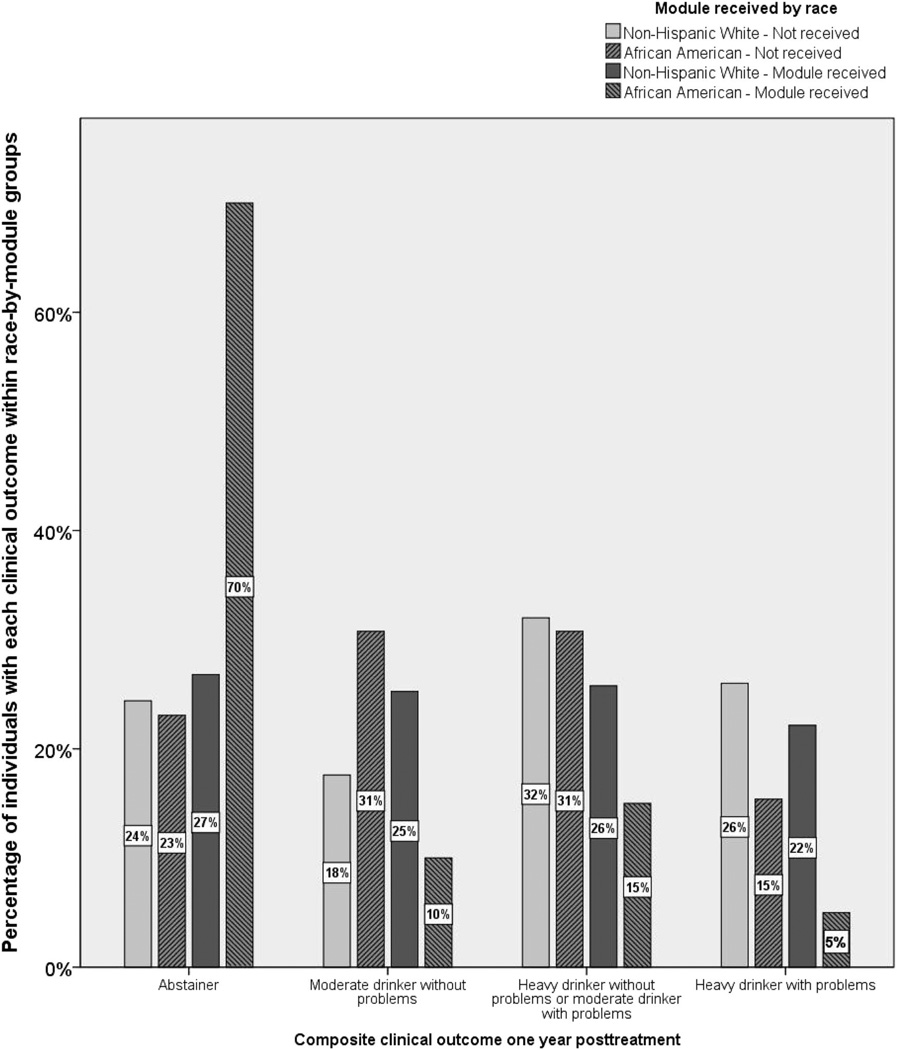
Results from the moderated multinomial logistic regression models indicated that the interaction between race and receiving the drink refusal and social pressures skills training module was a significant predictor of composite clinical outcomes (B = −0.85, SE = 0.40, = = −.15, p = .04). The main effects of receiving the module and race were not significant (module: B = −0.04, SE = 0.13, p = .77; race: B = −0.15, SE = 0.16, p = .35). Eighty percent of African Americans who received the module were either abstinent or drinking moderately without problems, compared with 52% of non-Hispanic White clients who did receive the module (see Figure 2). Only 54% of African Americans who did not receive the module were either abstinent or drinking moderately without problems.
Figure 2.
Clinical outcomes 1 year following treatment for non-Hispanic Whites and African Americans by drink refusal skills module groups.
Discussion
These secondary analyses of the COMBINE study data (Anton et al., 2006) evaluated whether drink refusal skills training, as part of a behavioral intervention for alcohol dependence, predicted different drinking and clinical outcomes among different racial groups. Results indicated that receiving the drink refusal and social pressures skills training module of the CBI was associated with significantly fewer heavy drinking days and lower likelihood of alcohol problems among African Americans, as compared to non-Hispanic White clients in the COMBINE study.
To our knowledge, this is the first study to examine racial differences in outcomes following a specific alcohol treatment component. The drink refusal and social pressures skills training module was examined because it targeted social influences (e.g., resisting social pressure to drink), which have been shown to predict alcohol use in African Americans. Consistent with the youth substance abuse prevention literature (Epstein et al., 2001), providing drink refusal skills training resulted in significantly fewer days of heavy drinking and better clinical outcomes (defined as no heavy drinking and no alcohol-related problems).
African Americans, although less likely to become alcohol dependant, have greater difficulty recovering from alcohol dependence (Brower, 2003; Scott, 2008). One of the components of the drink refusal and social pressure skills training module examined in this study involved practicing coping strategies for drink refusal. Previous studies have also found support for the effectiveness of coping behavior rehearsal in the treatment of heavy drinking in African American samples (Chiang, Hunter, & Yeh, 2004; Jones-Webb, 1998). Thus, this component of the module might explain the positive treatment outcomes seen among the African Americans.
Several limitations of the current study reduce our ability to draw strong conclusions from the current findings. Most notably, the lack of random assignment to receive the drink refusal and social pressures skills training module eliminates any possibility of testing a causal effect of the treatment module on outcomes among racial groups. Baseline measures that predicted whether or not a particular individual received the module (yearly income and client-rated therapeutic alliance) were included as covariates in all models, but other variables that were not measured in COMBINE (e.g., sociability, openness to experience) could also provide a plausible explanation for the current findings. Future research using a randomized 2 = 2 design, whereby African Americans and non-Hispanic Whites are randomly assigned to receive (or not receive) drink refusal skills training would provide a much stronger test of the interaction identified in the current analyses.
A second major limitation was the small sample size of African Americans who received (or did not receive) the drink refusal skills training module. Post hoc power analyses indicated that in the comparison of African Americans who did and did not receive the module, our sample sizes of 25 and 35 per group, respectively, resulted in power of .84 to detect a medium-to-large effect (based on a two-tailed test with α = .05). In the comparison of African Americans and non-Hispanic Whites who did receive the module, the power to detect a large effect was .98. Thus, the current study was powered to detect the observed effects. Nonetheless, replication of the current results with a larger sample size would provide greater confidence in the findings.
The small sample size also limits opportunities to examine potential mechanisms by which drink refusal skills training was effective for African Americans in the COMBINE sample. Previous analyses (Witkiewitz, Donovan, & Hartzler, 2010) indicated that posttreatment changes in self-efficacy to resist social/positive drinking cues, as measured by the Alcohol Abstinence Self-Efficacy scale (DiClemente, Carbonari, Montgomery, & Hughes, 1994), mediated the association between drink refusal skills training and drinking outcomes in the COMBINE study. The mediation effect was not statistically significant when moderation by racial groups was included in the model, primarily due to a lack of power to detect a moderated mediation effect. Other potential mechanisms (e.g., openness to experience, acculturation factors, empowerment) could not be examined because objective measures of these constructs were not included in the COMBINE assessment battery.
Despite the limitations described above, the current study provides initial evidence supporting the clinical utility of incorporating drink refusal skills training into behavioral interventions for African American clients. Following recommendations of the Lowman and Le Fauve (2003) review on health disparities in substance abuse treatment outcomes, this study examined a treatment component (drink refusal skills training) that targeted a sociocultural influence on drinking outcomes (social pressure to drink). Evaluating culturally competent treatments for substance abuse, through research, is critical in eliminating disparities in health care of racial and ethnical minorities. Future research should continue to examine the effectiveness of specific treatment components in the prediction of outcomes among different groups of individuals, as well as the mechanisms by which specific treatments are effective.
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant R21AA017137 (Katie Witkiewitz, PI). We thank members of the COMBINE Study Research Group for their assistance in facilitating access to COMBINE study data.
Footnotes
The drink refusal skills module was administered more than once to 65% of those who received the module (38% received the module twice, 18% received it 3 times, and the remaining 9% received it 4 times or more). However, there were no differences between racial groups on number of times receiving the module, t(653) = 0.78, p = .44. The number of times receiving the module (i.e., the “dose”) did not have a significant effect on percentage of heavy drinking days or drinking consequences for either racial group—heavy drinking days: F(5, 542) = 1.29, p = .27; drinking consequences: F(5, 448) = 1.05, p = .39—although African Americans who received the module more than once did report a lower percentage of heavy drinking days at follow-up (module received: Monce = 4.73, SD = 13.5; Mtwice = 2.68, SD = 3.9; Mthrice = 3.04, SD = 6.8).
Given the lack of substantive reasons for differences across sites, we did not use a multilevel modeling framework.
Contributor Information
Katie Witkiewitz, Department of Psychology, Washington State University.
Nadia Aracelliz Villarroel, Alcohol and Drug Abuse Institute, University of Washington.
Bryan Hartzler, Alcohol and Drug Abuse Institute, University of Washington.
Dennis M. Donovan, Alcohol and Drug Abuse Institute, University of Washington
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM COMBINE Research Study Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE study: A randomized controlled trial. Journal of the American Medical Association. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Beal AC, Ausiello J, Perrin JM. Social influences on health-risk behaviors among minority middle school students. Journal of Adolescent Health. 2001;28:474–480. doi: 10.1016/s1054-139x(01)00194-x. [DOI] [PubMed] [Google Scholar]
- Brower KJ, Carey TL. Racially related health disparities and alcoholism treatment outcomes. Alcoholism: Clinical and Experimental Research. 2003;27:1365–1367. doi: 10.1097/01.ALC.0000080165.72243.03. [DOI] [PubMed] [Google Scholar]
- Chiang L, Hunter CD, Yeh CJ. Coping attitudes, sources, and practices among Black and Latino college students. Adolescence. 2004;39:793–815. [PubMed] [Google Scholar]
- Cisler RA, Zweben A. Development of a composite measure for assessing alcohol treatment outcome: Operationalization and validation. Alcoholism: Clinical and Experimental Research. 1999;23:263–271. [PubMed] [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions for alcohol dependence (the COMBINE study): A pilot feasibility study. Alcoholism: Clinical and Experimental Research. 2003;27:1123–1131. doi: 10.1097/01.ALC.0000078020.92938.0B. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Anton RF, Miller WR, Longabaugh R, Hosking JD, Youngblood M. Combined pharmacotherapies and behavioral interventions for alcohol dependence (the COMBINE Study): Examination of posttreatment drinking outcomes. Journal of Studies on Alcohol and Drugs. 2008;69:5–13. doi: 10.15288/jsad.2008.69.5. [DOI] [PubMed] [Google Scholar]
- Epstein JA, Griffin KW, Botvin GJ. Risk taking and refusal assertiveness in a longitudinal model of alcohol use among inner-city adolescents. Prevention Science. 2001;2:193–200. doi: 10.1023/a:1011562907970. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Scheier LM, Botvin GJ, Diaz T. Ethnic and gender differences in psychosocial risk, protection, and adolescent alcohol use. Prevention Science. 2000;1:199–212. doi: 10.1023/a:1026599112279. [DOI] [PubMed] [Google Scholar]
- Jones-Webb R. Drinking patterns and problems among African-Americans: Recent findings. Alcohol Health and Research World. 1998;22:260–264. [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Zweben A, LoCastro JS, Miller WR. Origins, issues and options in the development of the combined behavioral intervention. Journal of Studies on Alcohol. 2005;(Suppl 15):168–169. 179–187. doi: 10.15288/jsas.2005.s15.179. [DOI] [PubMed] [Google Scholar]
- Lowman C, Le Fauve CE. Health disparities and the relationship between race, ethnicity, and substance abuse treatment outcomes. Alcoholism: Clinical and Experimental Research. 2003;27:1324–1326. doi: 10.1097/01.ALC.0000080346.62012.DC. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal on Studies of Alcohol. 1994;(Suppl 12):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Vol. 4. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. (DHHS Publication No. 95–3911). [Google Scholar]
- Miller WR, Wilbourne PL. Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Bux DA. Examining the effects of gender and ethnicity on substance abuse treatment and mediational pathways. Alcoholism: Clinical and Experimental Research. 2003;27:1330–1332. doi: 10.1097/01.ALC.0000080344.96334.55. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPlus user’s guide. 5th ed. Los Angeles: Author; 2007. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Scott DM, Williams CD, Cain GE, Kwagyan J, Kalu N, Ehlers CL, Taylor RE. Clinical course of alcohol dependence in African Americans. Journal of Addictive Disease. 2008;27:43–50. doi: 10.1080/10550880802324754. [DOI] [PubMed] [Google Scholar]
- Taylor RE. Pharmacological and cultural considerations in alcohol treatment clinical trials: Issues in clinical research related to race and ethnicity. Alcoholism: Clinical and Experimental Research. 2003;27:1345–1348. doi: 10.1097/01.ALC.0000080341.10023.2F. [DOI] [PubMed] [Google Scholar]
- Tonigan JS. Project MATCH treatment participation and outcome by self-reported ethnicity. Alcoholism: Clinical and Experimental Research. 2003;27:1340–1344. doi: 10.1097/01.ALC.0000080673.83739.F3. [DOI] [PubMed] [Google Scholar]
- Walton MA, Blow FC, Booth BM. Diversity in relapse prevention needs: Gender and race comparisons among substance abuse treatment patients. American Journal of Drug and Alcohol Abuse. 2001;27:225–240. doi: 10.1081/ada-100103707. [DOI] [PubMed] [Google Scholar]
- Williams C, Epstein JA, Botvin GJ, Schinke SP, Diaz T. Psychosocial determinants of alcohol use among minority youth living in public housing developments. Journal of Developmental and Behavioral Pediatrics. 1998;19:145–154. doi: 10.1097/00004703-199806000-00001. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Donovan DM, Hartzler B. Drink refusal training as part of a combined behavioral intervention: Effectiveness and mechanisms of change. Manuscript in preparation; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]