Abstract
Background:
The large-scale utilization of allogenic blood transfusion and its associated outcomes have been described in critically ill patients and those undergoing high-risk cardiac surgery but not in patients undergoing elective total hip arthroplasty. The objective of this study was to determine the trends in utilization and outcomes of allogenic blood transfusion in patients undergoing primary total hip arthroplasty in the United States from 2000 to 2009.
Methods:
An observational cohort of 2,087,423 patients who underwent primary total hip arthroplasty from 2000 to 2009 was identified in the Nationwide Inpatient Sample. International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes 99.03 and 99.04 were used to identify patients who received allogenic blood products during their hospital stay. Risk factors for allogenic transfusions were identified with use of multivariable logistic regression models. We used propensity score matching to estimate the adjusted association between transfusion and surgical outcomes.
Results:
The rate of allogenic blood transfusion increased from 11.8% in 2000 to 19.0% in 2009. Patient-related risk factors for receiving an allogenic blood transfusion include an older age, female sex, black race, and Medicaid insurance. Hospital-related risk factors include rural location, smaller size, and non-academic status. After adjusting for confounders, allogenic blood transfusion was associated with a longer hospital stay (0.58 ± 0.02 day; p < 0.001), increased costs ($1731 ± $49 [in 2009 U.S. dollars]; p < 0.001), increased rate of discharge to an inpatient facility (odds ratio, 1.28; 95% confidence interval, 1.26 to 1.31), and worse surgical and medical outcomes. In-hospital mortality was not affected by allogenic blood transfusion (odds ratio, 0.97; 95% confidence interval, 0.77 to 1.21).
Conclusions:
The increase in allogenic blood transfusion among total hip arthroplasty patients is concerning considering the associated increase in surgical complications and adverse events. The risk factors for transfusion and its impact on costs and inpatient outcomes can potentially be used to enhance patient care through optimizing preoperative discussions and effective utilization of blood-conservation methods.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Total hip arthroplasty is associated with substantial perioperative blood loss averaging 1000 to 2000 mL1-3 and a drop of 4.0 ± 1.5 g/dL (mean and standard deviation) in the hemoglobin level4,5. With this blood loss, allogenic blood transfusion is common in total hip arthroplasty. It was estimated that from 1996 to 1997, 16% of patients undergoing total hip arthroplasty received an allogenic blood transfusion compared with 11% of those undergoing total knee arthroplasty in the United States1. While major progress has been made in improving blood safety during the past twenty years6, serious complications of blood transfusion have not been eliminated. Concerns regarding nosocomial infections7-9 and transfusion-associated lung injury and circulatory overload10,11 have directed the efforts toward evaluating the indications for transfusion and exploring alternative methods of blood conservation. However, it is unclear whether changes in blood-management practices have led to a change in allogenic blood-transfusion rates in the U.S. during the past decade.
Several observational studies have demonstrated an association between blood transfusion and increased postoperative morbidity and mortality in patients undergoing cardiac surgery12-15, patients undergoing non-cardiac surgery16,17, and critically ill patients7,18. In orthopaedic surgery, several studies have shown an increased risk of postoperative infections, a longer hospital stay, and increased mortality1,8,19-21. However, the majority of the evidence stems from studies involving hip-fracture patients, a population known to have a heavier comorbidity burden22,23 and a higher risk of death24 in comparison with patients undergoing elective hip arthroplasty. There are limited nationally representative data on the utilization of allogenic blood transfusion among patients managed with total hip arthroplasty. Nationwide data are important for evaluating the impact of allogenic blood transfusion on the health-related outcomes of total hip arthroplasty and its financial burden.
In this study, data from the Nationwide Inpatient Sample were analyzed to examine the trends and risk factors for allogenic blood transfusion in patients undergoing primary total hip arthroplasty in the U.S. from 2000 to 2009. The data were also used to determine whether allogenic blood transfusion is associated with a longer hospital stay, higher costs, discharge to an inpatient facility, a higher rate of complications, and an increased in-hospital mortality rate for patients managed with a primary total hip arthroplasty.
Materials and Methods
Data Source
This study was a cross-sectional secondary data analysis carried out with use of the Nationwide Inpatient Sample data from 2000 to 2009. The Nationwide Inpatient Sample constitutes patient-level hospital-discharge data provided by states that participate in the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality25. The Nationwide Inpatient Sample uses a stratified random sampling design to capture 20% of inpatient discharges from non-federal U.S. hospitals, and it includes weights to provide national estimates. Data elements include patient demographic variables; insurance status; International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes; hospital characteristics; in-hospital mortality rates; and total charges. This study was deemed exempt by the hospital’s institutional review board.
Study Population
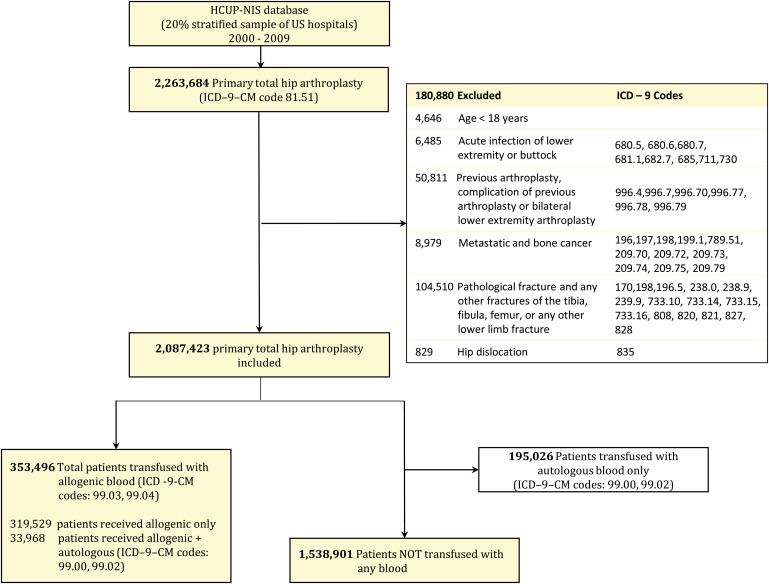
We identified cases of total hip arthroplasty by the presence of the ICD-9-CM procedure code 81.51. Discharge records carrying ICD-9-CM diagnosis codes for acute infection of the lower extremity or buttock, a diagnosis suggestive of a previous arthroplasty, a complication of previous arthroplasty, a bilateral lower-extremity arthroplasty, metastatic and/or bone cancer, lower-extremity fractures, or a hip dislocation were excluded (Fig. 1). We also excluded patients who were younger than eighteen years. The total weighted number of patients included in the study was 2,087,423. Patients who received autologous blood transfusion (ICD-9-CM codes 99.00 and 99.02) but not allogenic blood products were excluded from all analyses except to compare transfusion trends over time.
Fig. 1.
Diagram showing the number of excluded, transfused, and non-transfused cases from the total hip arthroplasty cohort (U.S., 2000 to 2009). HCUP-NIS = Healthcare Cost and Utilization Project Nationwide Impatient Sample.
Outcomes
The primary outcome of interest was annual trends in the rate of allogenic blood transfusion in total hip arthroplasty patients. The transfusion of allogenic blood products was identified with use of two ICD-9-CM procedure codes: 99.03 (other transfusion of whole blood), and 99.04 (transfusion of packed cells). The control group consisted of patients who did not receive allogenic blood products and also did not receive an autologous blood transfusion (Fig. 1). Patient-related and health-care-related risk factors for allogenic blood transfusion were identified. We also examined the association between a blood transfusion following total hip arthroplasty and other outcomes, including the length of the hospital stay, cost, discharge to an inpatient facility, surgical complications and other adverse events, and in-hospital mortality rate. Costs were calculated by multiplying the total charges by a hospital-specific cost-to-charge ratio provided by the Healthcare Cost and Utilization Project26. Discharge to an inpatient facility included disposition coding for “transfer: short-term hospital,” “skilled nursing facility,” “intermediate care facility,” and “transfer: other type of facility.” Surgical complications and adverse events were identified with use of specific ICD-9-CM diagnosis codes, as done in the study by Memtsoudis et al.27. In addition, we examined the association between blood transfusion in total hip arthroplasty and pulmonary edema and congestion (codes 514 and 518.4) as well as superficial (682.5, 682.6, and 998.59) and deep (996.66 and 996.67) surgical-site infections.
Covariates
Several correlates of transfusion, including patient demographics, patient comorbidities, and hospital characteristics, were included as covariates in the statistical models. The covariates were defined as recorded in the discharge summary. Approximately 25% of the records did not have patient race and/or ethnicity noted, since in certain states the race variable is not documented on the discharge records as an additional safeguard to protect patient confidentiality. Thus, to account for the nearly one in four discharge records with a missing value for race in our study, we created an additional race category and captured the race of these patients as “missing.” Insurance status was categorized as Medicare, Medicaid, private insurance, uninsured, or other. Hospital characteristics included geographic region, number of beds, teaching status, and urban or rural designation. Comorbidities were classified with use of the Agency for Healthcare Research and Quality Comorbidity Software, version 3.7, which uses ICD-9-CM diagnosis codes to flag the presence of thirty different comorbidities28.
Statistical Analysis
We first examined the distribution of data and calculated the baseline descriptive statistics for all variables included in the analyses. National estimates were obtained by applying weights provided in the data from the Healthcare Cost and Utilization Project, which were calculated by dividing the number of discharges in a stratum of the Nationwide Inpatient Sample data by the total number of discharges as reported in the American Hospital Association survey for that stratum. We then tested the association between each baseline variable and blood transfusion after total hip arthroplasty with use of the Pearson chi-square test for categorical variables and the Student t test for continuous variables. A logistic regression model was used to identify factors associated with the receipt of a blood transfusion. The c-statistic was used to assess model fit. Annual trends in the length of the hospital stay, costs, and in-hospital mortality for patients managed with a total hip arthroplasty with and without an allogenic blood transfusion were assessed with use of multivariable linear or logistic regressions with the calendar year as an independent variable and controlling for all other demographic, hospital, and comorbidity variables. Given the skewed continuous outcome variables, log transformation was used to achieve normal distribution.
We used propensity score matching to estimate the adjusted association between transfusion and each of our outcomes while controlling for known confounders. First, a logistic model with transfusion as the outcome and all study variables as covariates was used to estimate the predicted probability of a transfusion. This predicted probability is the propensity score. We then matched each transfusion patient to a control subject with use of a 1:1 greedy match algorithm based on the propensity score. Next, we estimated the associated effect of transfusion with use of logistic regression for binary outcomes and differences in means for continuous outcomes.
Source of Funding
This study was made possible, in part, by the Clinical and Translational Science Collaborative of Cleveland, a grant (UL1TR000439) from the National Center for Advancing Translational Sciences component of the National Institutes of Health (NIH), and an NIH Roadmap for Medical Research. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Results
Transfusion Trends
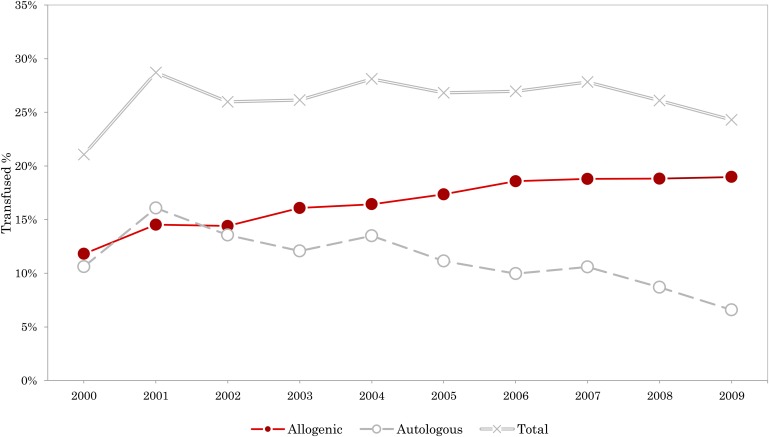
The overall allogenic blood transfusion rate in patients undergoing primary total hip arthroplasty in the U.S. from 2000 to 2009 was 17%. This represented a weighted national estimate of 353,496 from the 2,087,423 patients who underwent primary total hip arthroplasty procedures in that period. The adjusted rate of allogenic blood transfusion continued to increase, from 11.8% in 2000 to 18.6% in 2006 (odds ratio [OR], 1.47; 95% confidence interval [CI], 1.42 to 1.53), after which it plateaued (Fig. 2). The rate of autologous blood transfusion dropped during that same time period, most noticeably from 2004 (13.5%) to 2009 (6.7%). The combined allogenic and autologous blood transfusion rates after 2001 ranged from 28.1% in 2004 to 24.3% in 2009 (Fig. 2).
Fig. 2.
Graph showing the adjusted rates of allogenic, autologous, and overall blood transfusion among total hip arthroplasty patients in the U.S.
Demographics
One third of the patients receiving a blood transfusion during a hospital stay for total hip arthroplasty were individuals in the seventy to seventy-nine-year age group (Table I). The majority of the population receiving a transfusion was female (71.05%), white (64.54%), and covered by Medicare insurance (66.11%). As for hospital characteristics, most transfusions took place in urban (87.10%), non-academic (55.85%), and large (58.61%) institutions located primarily in the Southern region of the U.S. (36.55%) (Table I).
TABLE I.
Demographics and Hospital Characteristics for Primary Total Hip Arthroplasty (THA) Patients Receiving or Not Receiving an Allogenic Blood Transfusion, United States 2000-2009 (Weighted)
| All THA Patients |
Patients Receiving a Transfusion |
Patients Not Receiving a Transfusion |
|||||
| Parameter | N | % | N | % | N | % | P Value* |
| Patients | 2,087,423 | 100 | 353,496 | 16.93 | 1,538,901 | 73.72 | |
| Age (yr) | <0.0001 | ||||||
| <40 | 65,243 | 3.13 | 8774 | 2.48 | 51,387 | 3.34 | |
| 40 to 49 | 188,804 | 9.04 | 20,127 | 5.69 | 150,912 | 9.81 | |
| 50 to 59 | 418,337 | 20.04 | 50,114 | 14.18 | 324,528 | 21.09 | |
| 60 to 69 | 554,818 | 26.58 | 79,246 | 22.42 | 418,151 | 27.17 | |
| 70 to 79 | 593,565 | 28.44 | 116,974 | 33.09 | 421,503 | 27.39 | |
| 80 to 89 | 254,381 | 12.19 | 73,481 | 20.79 | 165,284 | 10.74 | |
| ≥90 | 12,275 | 0.59 | 4779 | 1.35 | 7,136 | 0.46 | |
| Sex | <0.0001 | ||||||
| Female | 1,173,544 | 56.22 | 251,150 | 71.05 | 808,920 | 52.56 | |
| Male | 909,026 | 43.55 | 102,124 | 28.89 | 725,734 | 47.16 | |
| Data missing | 4853 | 0.23 | 222 | 0.06 | 4247 | 0.28 | |
| Race | <0.0001 | ||||||
| White | 1,332,440 | 63.83 | 228,157 | 64.54 | 969,111 | 62.97 | |
| Black | 96,507 | 4.62 | 23,580 | 6.67 | 65,716 | 4.27 | |
| Hispanic | 45,414 | 2.18 | 10,059 | 2.85 | 31,573 | 2.05 | |
| Other | 45,690 | 2.19 | 9683 | 2.74 | 32,487 | 2.11 | |
| Data missing | 567,373 | 27.18 | 82,018 | 23.20 | 440,014 | 28.59 | |
| Insurance | <0.001 | ||||||
| Medicare | 1,123,456 | 53.82 | 233,699 | 66.11 | 795,114 | 51.67 | |
| Medicaid | 62,120 | 2.98 | 12,718 | 3.60 | 46,442 | 3.02 | |
| Private | 834,345 | 39.97 | 97,244 | 27.51 | 644,665 | 41.89 | |
| Uninsured | 15,288 | 0.73 | 2317 | 0.66 | 11,816 | 0.77 | |
| Other | 52,214 | 2.50 | 7517 | 2.13 | 40,863 | 2.66 | |
| Location | <0.001 | ||||||
| Rural | 233,879 | 11.20 | 45,104 | 12.76 | 171,783 | 11.16 | |
| Urban | 1,848,963 | 88.58 | 307,892 | 87.10 | 1,363,037 | 88.57 | |
| Region of U.S. | <0.0001 | ||||||
| Northeast | 433,832 | 20.78 | 81,396 | 23.03 | 295,449 | 19.20 | |
| Midwest | 559,624 | 26.81 | 69,519 | 19.67 | 460,649 | 29.93 | |
| South | 657,886 | 31.52 | 129,187 | 36.55 | 470,571 | 30.58 | |
| West | 436,081 | 20.89 | 73,394 | 20.76 | 312,233 | 20.29 | |
| Teaching status | 0.0002 | ||||||
| Nonacademic | 1,102,419 | 52.81 | 197,442 | 55.85 | 811,135 | 52.71 | |
| Academic | 980,422 | 46.97 | 155,554 | 44.00 | 723,685 | 47.03 | |
| Number of beds† | 0.0003 | ||||||
| Small | 304,836 | 14.60 | 51,274 | 14.50 | 214,864 | 13.96 | |
| Medium | 501,235 | 24.01 | 94,550 | 26.75 | 358,840 | 23.32 | |
| Large | 1,276,771 | 61.16 | 207,173 | 58.61 | 961,116 | 62.45 | |
P values represent the results of the chi-square test of independence for each category.
The number of beds depends on the location and teaching status of the hospital. For a rural hospital, small is fewer than fifty beds, medium is fifty to ninety-nine beds, and large is more than ninety-nine beds. For a teaching hospital, small is fewer than 300 beds, medium is 300 to 500 beds, and large is more than 500 beds.
Comorbidities
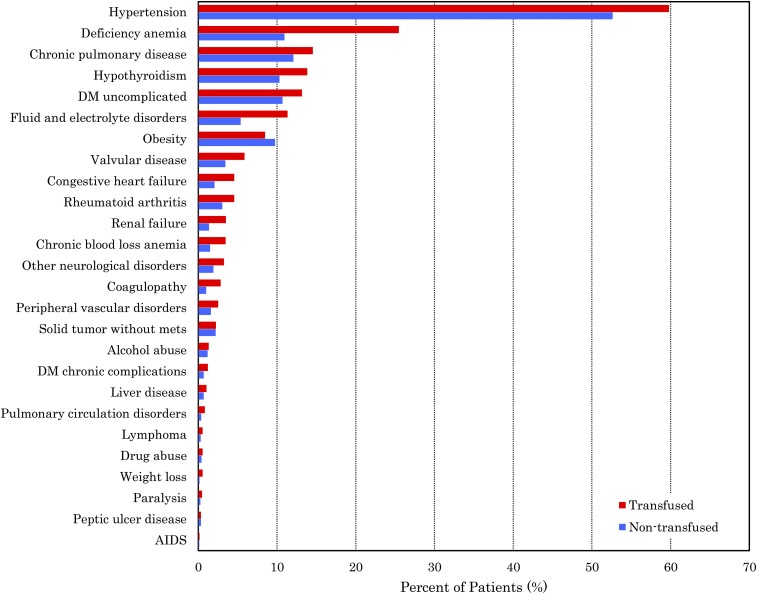
The prevalence of most comorbidities was higher in the patients who received a transfusion compared with those who did not (p < 0.001), except for obesity, which was more common among the patients who did not receive a transfusion (p < 0.001). The prevalence of acquired immune deficiency syndrome (AIDS) was not different between the two groups (p > 0.05) (Fig. 3). The rate of allogenic blood transfusion was highest among patients with unintentional weight loss (39.2%), coagulopathy (37.8%), renal failure (34.1%), deficiency anemia (32.0%), and chronic blood loss anemia (32.1%).
Fig. 3.
Graph showing the prevalence of comorbidities in patients receiving and not receiving a blood transfusion following total hip arthroplasty. DM = diabetes mellitus, and mets = metastasis.
Risk Factors for Allogenic Blood Transfusion
Multivariable logistic regression analysis revealed a number of independent risk factors for allogenic blood transfusion perioperatively in total hip arthroplasty patients (c-statistic = 0.711) (Table II). Patient-related factors that significantly increased the risk for allogenic blood transfusion were age, black race (OR, 1.63; 95% CI, 1.57 to 1.69), and Medicaid insurance (OR, 1.58; 95% CI, 1.51 to 1.66). Almost all comorbidities were associated with increased risk of transfusion following total hip arthroplasty (p < 0.001) except for peptic ulcer disease (p = 0.0584). Particularly, deficiency anemia, chronic blood loss anemia, and coagulopathy increased the risk of transfusion by more than twofold.
TABLE II.
Risk Factors for Allogenic Blood Transfusion During a Hospital Stay for Primary Total Hip Arthroplasty*
| Risk Factor | Adjusted Odds Ratio (95% CI) | P Value |
| Age group (yr) | ||
| 40 to 49 | 0.87 (0.82 to 0.93) | <0.0001 |
| 50 to 59 | 0.95 (0.90 to 1.01) | 0.102 |
| 60 to 69 | 1.06 (1.00 to 1.12) | 0.045 |
| 70 to 79 | 1.38 (1.30 to 1.46) | <0.0001 |
| 80 to 89 | 2.11 (1.99 to 2.24) | <0.0001 |
| ≥90 | 3.01 (2.72 to 3.34) | <0.0001 |
| Sex | ||
| Female | 1.92 (1.88 to 1.95) | <0.0001 |
| Race | ||
| Black | 1.63 (1.57 to 1.69) | <0.0001 |
| Hispanic | 1.37 (1.30 to 1.45) | <0.0001 |
| Other | 1.38 (1.31 to 1.46) | <0.0001 |
| Missing | 1.00 (0.97 to 1.02) | 0.4943 |
| Insurance | ||
| Medicare | 1.17 (1.14 to 1.20) | <0.0001 |
| Medicaid | 1.58 (1.51 to 1.66) | <0.0001 |
| Uninsured | 1.27 (1.14 to 1.41) | 0.0007 |
| Other | 1.19 (1.12 to 1.26) | <0.0001 |
| Comorbidities | ||
| AIDS | 1.39 (1.13 to 1.72) | 0.0007 |
| Alcohol abuse | 1.33 (1.24 to 1.44) | <0.0001 |
| Chronic blood loss anemia | 2.50 (2.38 to 2.64) | <0.0001 |
| Chronic pulmonary disease | 1.08 (1.05 to 1.10) | <0.0001 |
| Coagulopathy | 2.31 (2.18 to 2.46) | <0.0001 |
| Congestive heart failure | 1.54 (1.47 to 1.61) | <0.0001 |
| Deficiency anemia | 2.42 (2.37 to 2.47) | <0.0001 |
| Diabetes mellitus | ||
| Complicated | 1.41 (1.29 to 1.53) | <0.0001 |
| Uncomplicated | 1.16 (1.13 to 1.19) | <0.0001 |
| Drug abuse | 1.41 (1.26 to 1.59) | <0.0001 |
| Fluid and electrolyte disorders | 1.57 (1.53 to 1.62) | <0.0001 |
| Hypertension | 1.06 (1.04 to 1.08) | <0.0001 |
| Hypothyroidism | 1.04 (1.01 to 1.06) | 0.0106 |
| Liver disease | 1.41 (1.29 to 1.54) | <0.0001 |
| Lymphoma | 1.76 (1.55 to 1.99) | <0.0001 |
| Obesity | 0.90 (0.88 to 0.93) | <0.0001 |
| Other neurological disorders | 1.48 (1.41 to 1.56) | <0.0001 |
| Paralysis | 1.56 (1.37 to 1.77) | <0.0001 |
| Peptic ulcer disease | 0.89 (0.78 to 1.03) | 0.0584 |
| Peripheral vascular disorders | 1.18 (1.12 to 1.25) | <0.0001 |
| Pulmonary circulation disorders | 1.24 (1.12 to 1.37) | <0.0001 |
| Renal failure | 1.67 (1.58 to 1.76) | <0.0001 |
| Rheumatoid arthritis | 1.26 (1.20 to 1.31) | <0.0001 |
| Solid tumor without metastasis | 0.94 (0.89 to 0.99) | <0.0001 |
| Valvular disease | 1.29 (1.24 to 1.34) | <0.0001 |
| Unintentional weight loss† | 1.81 (1.58 to 2.08) | <0.0001 |
| Hospital characteristics | ||
| Urban location | 0.80 (0.78 to 0.82) | <0.0001 |
| Teaching | 0.95 (0.93 to 0.97) | <0.0001 |
| Northeastern region | 1.18 (1.15 to 1.21) | <0.0001 |
| Midwestern region | 0.66 (0.64 to 0.67) | <0.0001 |
| Southern region | 1.14 (1.11 to 1.17) | <0.0001 |
| Small number of beds | 1.13 (1.11 to 1.16) | <0.0001 |
| Medium number of beds | 1.25 (1.23 to 1.28) | <0.0001 |
The reference patient is a forty-year-old white male with private insurance and no comorbidities, admitted to a large teaching hospital in an urban area located in the Western region of the United States. C-statistic = 0.711.
Weight loss is defined to represent ICD-9-CM codes 260 through 263.9, which are for kwashiorkor, nutritional marasmus, other severe protein-calorie malnutrition, and other and unspecified protein-calorie malnutrition.
Patients admitted to urban hospitals had a 20% lower risk of getting an allogenic blood transfusion compared with those admitted to rural hospitals (OR, 0.80; 95% CI, 0.78 to 0.82) (Table II). A hospital location in the Midwestern region of the U.S. reduced the risk of allogenic blood transfusion by 34% (OR, 0.66; 95% CI, 0.64 to 0.67) compared with a hospital location in the Western region (Table II), whereas hospital locations in the Northeastern or Southern region had an increased risk of transfusion of 18% and 14%, respectively.
Length of Hospital Stay, Cost, and Discharge Disposition
The mean length of the hospital stay decreased over the study period both in patients who received a transfusion and in those who did not (see Appendix). After propensity score adjustment for patient demographics, comorbidities, and hospital characteristics, allogenic blood transfusion caused an overall increase of 0.58 ± 0.02 day in the length of the hospital stay (p < 0.001). Total costs of primary total hip arthroplasty admissions increased over the study period both in patients who received transfusion and in those who did not (see Appendix). Allogenic blood transfusion increased the total costs (in 2009 U.S. dollars) by $1731 ± $49 (p < 0.001) and total charges by $4692 ± $143 (p < 0.001) compared with total costs and charges for patients who did not receive a transfusion, after adjusting for confounders. Furthermore, discharge disposition was also affected by transfusion, with patients who received a transfusion 28% more likely to be discharged to inpatient facilities (OR, 1.28; 95% CI, 1.26 to 1.31).
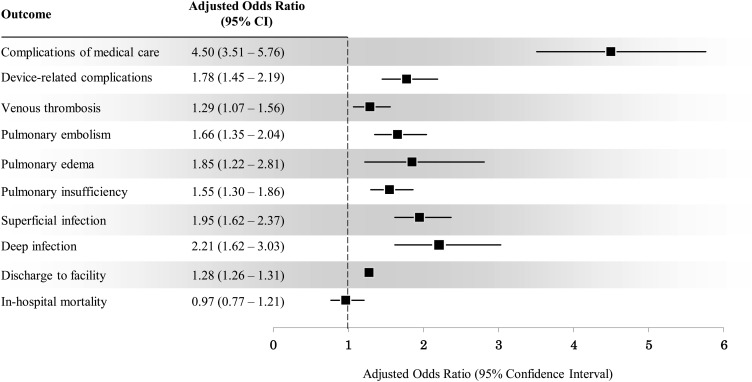
Outcomes
Allogenic blood transfusion was generally associated with worse surgical and medical outcomes after total hip arthroplasty (Fig. 4). The risk of device-related surgical complications was 78% higher in the group that received a transfusion (OR, 1.78; 95% CI, 1.45 to 2.19). More specifically, the adjusted odds of developing superficial infections (OR, 1.95; 95% CI, 1.62 to 2.37), deep infections (OR, 2.21; 95% CI, 1.62 to 3.03), pulmonary insufficiency (OR, 1.55; 95% CI, 1.30 to 1.86), pulmonary edema (OR, 1.85; 95% CI, 1.22 to 2.81), venous thrombosis (OR, 1.29; 95% CI, 1.07 to 1.56), and pulmonary embolism (OR, 1.66; 95% CI, 1.35 to 2.04) were all higher in the population receiving a blood transfusion.
Fig. 4.
Graph showing the adjusted effect of allogenic blood transfusion on the outcomes after total hip arthroplasty.
From 2001 to 2009, the unadjusted in-hospital mortality rate in total hip arthroplasty admissions each year was significantly higher in the group that received a transfusion (p < 0.001) (see Appendix). However, after adjusting for confounders, the risk of in-hospital mortality was not different between patients who received a transfusion compared with those who did not (OR, 0.97; 95% CI, 0.77 to 1.21) (Fig. 4).
Discussion
In this study, we sought to characterize national trends and predictors of allogenic blood transfusion in total hip arthroplasty in the U.S. with use of Nationwide Inpatient Sample data from 2000 to 2009. We studied the association between transfusion and the cost, length of the hospital stay, complications, and in-hospital mortality rate after total hip arthroplasty. An increase in the rate of allogenic blood transfusion was identified, and it was associated with increased costs, a longer hospital stay, and increased complications. However, this increase in the transfusion rate was not accompanied by an increased in-hospital mortality rate.
We are not aware of any recent studies examining nationwide data on transfusion trends in total hip arthroplasty. Bierbaum et al.1 had a higher overall rate of blood transfusion, of 53.7%, in primary total hip arthroplasty in a prospective study involving 235 sites in the U.S. from 1996 to 1997. Their study showed a higher autologous transfusion rate, of 37.3%, and a lower allogenic transfusion rate, of 16.4%. While the overall transfusion rate in our study was lower (26%), the allogenic blood transfusion rate continued to increase throughout the study period, reaching 19.1% in 2009. This increase may be partially due to the transition from autologous to allogenic transfusion with advances in blood bank screening and storage, as evident from the drop in autologous transfusion rates over the same time period (Fig. 2). This increase may also be due to more rigorous documentation and coding in recent years, as some older studies suggested that ICD-9 codes for transfusion underestimated the utilization of blood products29,30.
The logistic regression analysis in this study provides important insight into demographic and hospital-related factors that influence the risk of transfusion. As previously reported, older age and female sex31,32 both increase the risk of transfusion after total hip arthroplasty. The increased risk of transfusion in black patients seen in this study is probably due to the increased rates of anemia in this population33. As would be expected, patients with deficiency anemias, chronic blood loss anemia, or coagulopathies have the highest risks of transfusion because of their low hemoglobin levels and tendency to bleed. Interestingly, being admitted to urban hospitals in the Midwestern region of the U.S. is associated with a lower risk of transfusion. This difference could be a result of the variability in hospital quality and transfusion strategies, including transfusion triggers.
A previous study of Medicare Provider Analysis and Review Part A data found a 50% decline in the length of the hospital stay after primary total hip arthroplasty in the U.S. from 1991 to 200834. The decline in the length of the hospital stay was also associated with trends toward longer stays in rehabilitation units35,36 and higher readmission rates34. Although our study showed a similar overall decline in the length of the hospital stay, patients who received a transfusion consistently had longer hospitalizations and were 28% more likely to be discharged to inpatient facilities. Thus, a broader perspective that includes the length of the hospital stay and the discharge disposition should be considered when estimating the burden of transfusion.
Administrative data including cost and length of the hospital stay are important for economic evaluation and cost containment. Green et al.37 performed a cost-minimization analysis comparing the total costs of an allogenic blood-transfusion strategy for 161 primary total hip arthroplasty patients with other blood-conservation strategies. The authors concluded that the allogenic blood-transfusion strategy was the most costly, at $1769 per total hip arthroplasty patient. This is concordant with the national data presented in this study, in which allogenic blood transfusion increased total hospital costs (in 2009 U.S. dollars) among primary total hip arthroplasty patients by $1731 per admission.
A number of studies have demonstrated an association between blood transfusion and increased rates of mortality and complications following several surgical procedures8,12-15,20,38. Bierbaum et al.1 reported more frequent infections, deep vein thrombosis, and fluid overload in patients receiving allogenic blood products. Carson et al.8 studied a retrospective cohort of 9598 consecutive hip fractures and found a 35% greater risk of serious bacterial infection and a 52% greater risk of pneumonia. Our analysis confirmed an increase in surgical and medical complications. Specifically, patients receiving a transfusion had significantly higher risks of sustaining postoperative infections, pulmonary insufficiency, pulmonary edema, and venous thromboembolism. In-hospital mortality rates were consistently higher in patients who received a transfusion compared with those who did not. However, after adjusting for confounders, no effect of transfusion on mortality was demonstrated. This may be because the population receiving a transfusion had a higher prevalence of comorbidities and thus was inherently predisposed to an increased risk of death39. Several studies did not find an association between allogenic blood transfusion and short-term mortality in hip-fracture patients40-42. However, these findings cannot rule out the possible deleterious effects of allogenic blood transfusion on longer-term mortality rates.
There are some limitations to this study, most of which are inherent to secondary data analysis of large administrative databases. The Nationwide Inpatient Sample does not include clinical information such as type of anesthesia, amount of blood loss, perioperative hemoglobin values, and number or volume of blood units transfused. Furthermore, only inpatient data are available in the Nationwide Inpatient Sample, and thus complications, deaths, and readmissions after discharge are not captured. Therefore, conclusions should be limited to the acute inpatient setting. There is also the possibility of incomplete or inaccurate coding of blood-product administration and surgical complications. The accuracy of our estimates of blood transfusions depends on the sensitivity and specificity of the codes used, but very limited information is available on this. A study by Segal et al.29 showed 83% sensitivity and 100% specificity for the packed cell transfusion procedure code 99.04 in one tertiary-care hospital with data from 1998 to 1999. Romano and Mark30 showed a sensitivity range of 21% to 31% and 100% specificity for the same procedure code in California hospital discharge abstracts with data from 1988. These studies are not generalizable to the Nationwide Inpatient Sample data, but they indicate that the 99.04 procedure code underestimated blood use in those studies. Another limitation with regard to ICD-9-CM coding is that it can underreport comorbid conditions that are not used for administrative purposes. In an attempt to minimize confounding by indication, we used propensity score matching to account for comorbid conditions and other demographic and hospital variables that predict receiving an allogenic blood transfusion. Even though we were able to create balance between groups on known factors, we are unable to account for unmeasured confounders, which is an inherit limitation of all observational studies. Furthermore, although the cost-to-charge ratio method for estimating costs is commonly used, it is not a perfect method for determining relative hospital costs; actual costs of hospitalization may vary from the estimates produced with the use of this method43. Finally, the effect of race as a risk factor for transfusion should be interpreted with caution, as nearly 25% of these data are missing.
In conclusion, the increasing rate of allogenic blood transfusion and its burden on health-care systems is a concern in patients undergoing total hip arthroplasty. The risk factors for transfusion identified in this study, as well as the impact of transfusion on costs and inpatient outcomes, can potentially be used to enhance patient care through optimizing preoperative discussions and effective utilization of blood-conservation methods.
Appendix
Figures comparing the mean lengths of the hospital stay, mean hospitalization costs, and in-hospital mortality rates for patients receiving and not receiving a blood transfusion following total hip arthroplasty are available with the online version of this article as a data supplement at jbjs.org.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Cleveland Clinic, Cleveland, Ohio
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999January;81(1):2-10 [DOI] [PubMed] [Google Scholar]
- 2.Guerra JJ, Cuckler JM. Cost effectiveness of intraoperative autotransfusion in total hip arthroplasty surgery. Clin Orthop Relat Res. 1995June;(315):212-22 [PubMed] [Google Scholar]
- 3.Woolson ST, Watt JM. Use of autologous blood in total hip replacement. A comprehensive program. J Bone Joint Surg Am. 1991January;73(1):76-80 [PubMed] [Google Scholar]
- 4.Nuttall GA, Santrach PJ, Oliver WC Jr, Horlocker TT, Shaughnessy WJ, Cabanela ME, Bryant S. The predictors of red cell transfusions in total hip arthroplasties. Transfusion. 1996February;36(2):144-9 [DOI] [PubMed] [Google Scholar]
- 5.Keating EM, Ritter MA. Transfusion options in total joint arthroplasty. J Arthroplasty. 2002June;17(4)(Suppl 1):125-8 [DOI] [PubMed] [Google Scholar]
- 6.Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007August4;370(9585):415-26 [DOI] [PubMed] [Google Scholar]
- 7.Taylor RW, Manganaro L, O’Brien J, Trottier SJ, Parkar N, Veremakis C. Impact of allogenic packed red blood cell transfusion on nosocomial infection rates in the critically ill patient. Crit Care Med. 2002October;30(10):2249-54 [DOI] [PubMed] [Google Scholar]
- 8.Carson JL, Altman DG, Duff A, Noveck H, Weinstein MP, Sonnenberg FA, Hudson JI, Provenzano G. Risk of bacterial infection associated with allogeneic blood transfusion among patients undergoing hip fracture repair. Transfusion. 1999July;39(7):694-700 [DOI] [PubMed] [Google Scholar]
- 9.Lemos MJ, Healy WL. Blood transfusion in orthopaedic operations. J Bone Joint Surg Am. 1996August;78(8):1260-70 [DOI] [PubMed] [Google Scholar]
- 10.Popovsky MA, Audet AM, Andrzejewski C Jr. Transfusion-associated circulatory overload in orthopedic surgery patients: a multi-institutional study. Immunohematology. 1996;12(2):87-9 [PubMed] [Google Scholar]
- 11.Li G, Kojicic M, Reriani MK, Fernández Pérez ER, Thakur L, Kashyap R, Van Buskirk CM, Gajic O. Long-term survival and quality of life after transfusion-associated pulmonary edema in critically ill medical patients. Chest. 2010April;137(4):783-9 Epub 2009 Oct 16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ. Effect of blood transfusion on long-term survival after cardiac operation. Ann Thorac Surg. 2002October;74(4):1180-6 [DOI] [PubMed] [Google Scholar]
- 13.Kuduvalli M, Oo AY, Newall N, Grayson AD, Jackson M, Desmond MJ, Fabri BM, Rashid A. Effect of peri-operative red blood cell transfusion on 30-day and 1-year mortality following coronary artery bypass surgery. Eur J Cardiothorac Surg. 2005April;27(4):592-8 [DOI] [PubMed] [Google Scholar]
- 14.Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007November27;116(22):2544-52 Epub 2007 Nov 12 [DOI] [PubMed] [Google Scholar]
- 15.Surgenor SD, Kramer RS, Olmstead EM, Ross CS, Sellke FW, Likosky DS, Marrin CA, Helm RE Jr, Leavitt BJ, Morton JR, Charlesworth DC, Clough RA, Hernandez F, Frumiento C, Benak A, DioData C, O’Connor GT; Northern New England Cardiovascular Disease Study Group. The association of perioperative red blood cell transfusions and decreased long-term survival after cardiac surgery. Anesth Analg. 2009June;108(6):1741-6 [DOI] [PubMed] [Google Scholar]
- 16.Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, Salloum R, Meredith UW, Osler TM. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology. 2011February;114(2):283-92 [DOI] [PubMed] [Google Scholar]
- 17.Engoren M, Mitchell E, Perring P, Sferra J. The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma. 2008December;65(6):1411-5 [DOI] [PubMed] [Google Scholar]
- 18.Taylor RW, O’Brien J, Trottier SJ, Manganaro L, Cytron M, Lesko MF, Arnzen K, Cappadoro C, Fu M, Plisco MS, Sadaka FG, Veremakis C. Red blood cell transfusions and nosocomial infections in critically ill patients. Crit Care Med. 2006September;34(9):2302-8; quiz 2309 [DOI] [PubMed] [Google Scholar]
- 19.Murphy P, Heal JM, Blumberg N. Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion. 1991Mar-Apr;31(3):212-7 [DOI] [PubMed] [Google Scholar]
- 20.Dunne JR, Malone DL, Tracy JK, Napolitano LM. Allogenic blood transfusion in the first 24 hours after trauma is associated with increased systemic inflammatory response syndrome (SIRS) and death. Surg Infect (Larchmt). 2004Winter;5(4):395-404 [DOI] [PubMed] [Google Scholar]
- 21.Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W. Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary arthroplasty. Transfusion. 2005January;45(1):103-10 [DOI] [PubMed] [Google Scholar]
- 22.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001November;83(11):1622-9 [DOI] [PubMed] [Google Scholar]
- 23.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005December10;331(7529):1374 Epub 2005 Nov 18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robbins JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the cardiovascular health study. J Am Geriatr Soc. 2006December;54(12):1885-91 [DOI] [PubMed] [Google Scholar]
- 25.Nationwide Impatient Sample. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. 2000-2009. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 2014 Mar 17
- 26.HCUP Cost-to-Charge Ratio Files (CCR). Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. 2006-2009. http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed 2014 Mar 17
- 27.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009December;111(6):1206-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.HCUP Comorbidity Software. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. 2000-2009. http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed 2014 Mar 17
- 29.Segal JB, Ness PM, Powe NR. Validating billing data for RBC transfusions: a brief report. Transfusion. 2001April;41(4):530-3 [DOI] [PubMed] [Google Scholar]
- 30.Romano PS, Mark DH. Bias in the coding of hospital discharge data and its implications for quality assessment. Med Care. 1994January;32(1):81-90 [DOI] [PubMed] [Google Scholar]
- 31.Walsh M, Preston C, Bong M, Patel V, Di Cesare PE. Relative risk factors for requirement of blood transfusion after total hip arthroplasty. J Arthroplasty. 2007December;22(8):1162-7 Epub 2007 Apr 20 [DOI] [PubMed] [Google Scholar]
- 32.Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A. Predicting the need for blood transfusion in patients with hip fractures. Int Orthop. 2013April;37(4):693-700 Epub 2013 Feb 5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shaz BH, Zimring JC, Demmons DG, Hillyer CD. Blood donation and blood transfusion: special considerations for African Americans. Transfus Med Rev. 2008July;22(3):202-14 [DOI] [PubMed] [Google Scholar]
- 34.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012July18;94(14):e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forrest GP, Roque JM, Dawodu ST. Decreasing length of stay after total joint arthroplasty: effect on referrals to rehabilitation units. Arch Phys Med Rehabil. 1999February;80(2):192-4 [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Orthopaedic Surgeons. The burden of musculoskeletal diseases in the United States: prevalence, societal and economic cost. 1st ed.Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008 [Google Scholar]
- 37.Green WS, Toy P, Bozic KJ. Cost minimization analysis of preoperative erythropoietin vs autologous and allogeneic blood donation in total joint arthroplasty. J Arthroplasty. 2010January;25(1):93-6 Epub 2008 Dec 3 [DOI] [PubMed] [Google Scholar]
- 38.Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study. BMC Musculoskelet Disord. 2009;10:167 Epub 2009 Dec 29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carson JL, Reynolds RC, Klein HG. Bad bad blood? Crit Care Med. 2008September;36(9):2707-8 [DOI] [PubMed] [Google Scholar]
- 40.Carson JL, Duff A, Berlin JA, Lawrence VA, Poses RM, Huber EC, O’Hara DA, Noveck H, Strom BL. Perioperative blood transfusion and postoperative mortality. JAMA. 1998January21;279(3):199-205 [DOI] [PubMed] [Google Scholar]
- 41.Johnston P, Wynn-Jones H, Chakravarty D, Boyle A, Parker MJ. Is perioperative blood transfusion a risk factor for mortality or infection after hip fracture? J Orthop Trauma. 2006Nov-Dec;20(10):675-9 [DOI] [PubMed] [Google Scholar]
- 42.Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, Koval KJ, Siu AL. Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion. 2003October;43(10):1358-65 [DOI] [PubMed] [Google Scholar]
- 43.Shwartz M, Young DW, Siegrist R. The ratio of costs to charges: how good a basis for estimating costs? Inquiry. 1995-1996Winter;32(4):476-81 [PubMed] [Google Scholar]