Abstract
An important step for treatment of a particular injury etiology is the appropriate application of a treatment targeted to the population at risk. An anterior cruciate ligament (ACL) injury risk algorithm has been defined that employs field-based techniques in lieu of laboratory-based motion analysis systems to identify athletes with high ACL injury risk landing strategies. The resultant field-based assessment techniques, in combination with the developed prediction algorithm, allow for low-cost identification of athletes who may be at increased risk of sustaining ACL injury. The combined simplicity and accuracy of the field-based tool facilitate its use to identify specific factors that may increase risk of injury in female athletes. The purpose of this report is to demonstrate novel algorithmic techniques to accurately capture and analyze measures of knee valgus motion, knee flexion range of motion, body mass, tibia length and quadriceps to hamstrings ratio with video analysis software typically used by coaches, strength and conditioning specialists, and athletic trainers. The field-based measurements and software analyses were used in a prediction algorithm to identify those at potential risk of noncontact ACL injury that may directly benefit from neuromuscular training.
Keywords: anterior cruciate ligament injury, knee, drop vertical jump, landing mechanics, young athletes
Introduction
Anterior cruciate ligament (ACL) research has resulted in >5,500 scientific articles published in the past decade, which investigate injury incidence, mechanism, surgical repair techniques, and rehabilitation of this important stabilizing knee ligament (35). However, despite much scientific advancement in the treatment of ACL injury, osteoarthritis occurs at a 10 times greater rate in ACL injured individuals regardless of the treatment (conservative management versus surgical treatment) (5,29). Epidemiological research also indicates that female athletes have a fourfold to sixfold increased risk of noncontact ACL injury compared with their male counterparts playing at similar levels in the same sports (2,14). The risk of noncontact ACL injury is coupled with increased sports participation by young women over the last 30 years, ninefold increase in high school (31) and fivefold increase in collegiate sports (30). The ACL injury in young athletes can lead to the loss of entire seasons of sports participation, possible scholarship funding, significantly lowered academic performance (7), long-term disability and up to 105 times greater risk of radiographically diagnosed osteoarthritis (4). Based on the undesirable short-term effects and long-term outcomes after ACL injury, a paradigm shift from research focused on treatment and rehabilitation to injury mechanism and prevention is warranted.
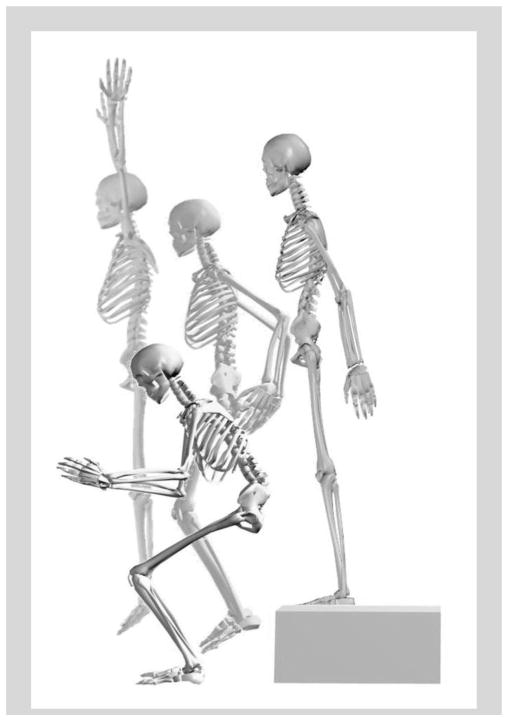
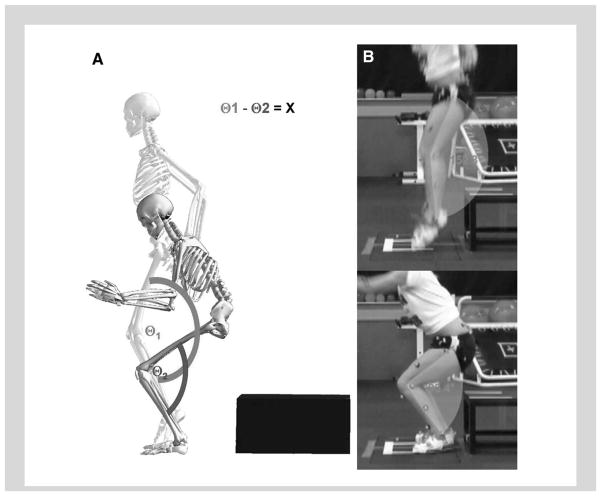
High knee abduction moments (KAM) during landing predict noncontact ACL injury risk in young female athletes with high accuracy (11). In addition, a large-scale prospective study found that military cadets who sustained ACL injury demonstrated high KAM landing mechanics (33). In validation of these findings, retrospective observation of noncontact ACL injury mechanics in female athletes report knee landing and cutting alignments associated with high KAM at the time of injury (Figure 1) (3,13,32). To achieve the objective of reducing noncontact injury risk in female athletes, identification of those who preferentially demonstrate high KAM landing mechanics appears salient.
Figure 1.
Videographic depiction of an athlete displaying a kinematic pattern that is likely leading to high KAM.
Although prospective measures of high KAM during landing have identified female athletes at increased risk for sustaining ACL injury, quantification of these measures necessitates dedicated biomechanical laboratories, which require costly measurement tools, and labor-intensive data collection sessions are essential to ascertain the measurements. Therefore, we aimed to systematically develop and validate a field-based assessment to improve the potential to identify and target injury prevention training to female athletes with increased KAM (20–22,24,25). We hypothesized that clinically obtainable correlates derived from highly predictive 3-dimensional (3D) motion analysis models would demonstrate high accuracy for determination of high KAM status.
Algorithm Development
To achieve the aim to develop a field-based ACL injury prevention algorithm, we recruited female basketball and soccer players (N = 744) from a single county public school district to participate in testing of anthropometrics, maturation, laxity or flexibility, strength and landing biomechanics (22). Linear regression was used to model KAM, and logistic regression was used to examine high vs. low KAM as surrogate for ACL injury risk (22,24,25). For validation purposes, 20 female basketball, soccer, and volleyball players were tested using 3D motion analysis and field-based techniques simultaneously (21,26). Field-based measurements were validated against 3D motion analysis measures using within and between method reliability (intraclass correlations [ICC] and Bland–Altman Plots) and sensitivity and specificity comparisons (2 × 2 table of actual vs. model-predicted classifications) (21).
Laboratory-Based Algorithm
The most parsimonious linear regression model included the independent predictors (β ± 1SE) (a) peak knee abduction angle (1.78 ± 0.05; p < 0.001), (b) peak knee extensor moment (0.17 ± 0.01; p < 0.001), (c) knee flexion range of motion (ROM; 0.15 ± 0.03; p < 0.01), (d) body mass index Z-score (−1.67 ± 0.36; p < 0.001), and (e) tibia length (−0.50 ± 0.14; p < 0.001). This model accounted for 78% of the variance in KAM during landing. The logistic regression model that employed these same variables predicted high KAM status with 85% sensitivity and 93% specificity and a C-statistic of 0.96 (22).
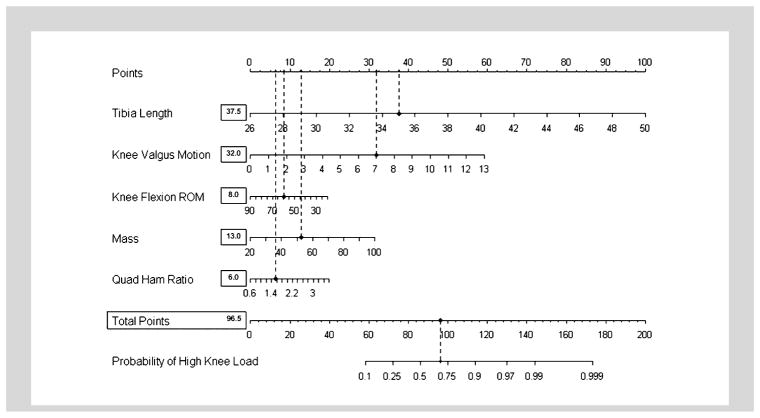
Field-Based Algorithm
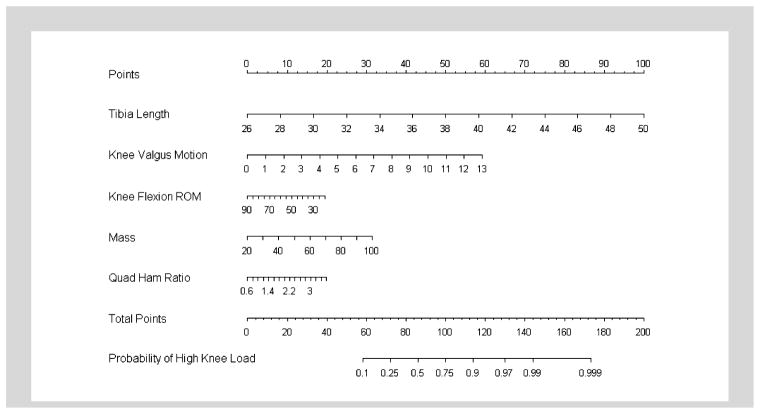
Clinical correlates to laboratory-based measures were identified and predicted high KAM status with 73% sensitivity and 70% specificity. The field-based prediction algorithm, including (odds ratio [OR], 95% confidence interval [CI]) knee valgus motion (centimeters) (OR = 1.43, 95% CI: 1.30–1.59), knee flexion ROM (degrees) (OR = 0.98, 95% CI: 0.96–1.01), body mass (kilograms) (OR = 1.04, 95% CI: 1.02–1.06), tibia length (centimeters) (OR = 1.38, 95% CI: 1.25–1.52) and quadriceps to hamstrings ratio (percent) (OR = 1.70, 95% CI: 1.06–2.70) predicted high KAM status with C-statistic 0.81 (20,24,25) (Figure 2).
Figure 2.
A nomogram designed for use by clinicians which was developed from the regression analysis. It can be used to predict outcome based on tibia length, knee valgus motion, knee flexion ROM, body mass and quadriceps to hamstrings ratio.
Algorithm Validation
In the validation dataset, the within variable analysis showed excellent interrater reliability for all variables using both 3D motion and field-based methods, with ICCs that ranged from moderate to high, 0.60–0.78 (21). In addition, moderate to high agreement was observed between 3D motion analysis and field-based measures with ICCs ranging from 0.66 to 0.99. Bland-Altman plots confirmed that each variable provided no systematic shift between 3D motion analysis and field-based methods and no association between difference and average. Regression analysis validated previous models to predict high KAM using both the 3D motion analysis and field-based techniques, which demonstrated 80 and 75% prediction accuracy, respectively, for this sample of female subjects (21).
Field-Based Techniques to Identify ACL Injury Risk Factors
The current development and validation steps provide the critical next progression to merge the gap between laboratory identification of injury risk factors and clinical practices. The validated field-based assessment algorithm delineated 5 biomechanical factors that combined to identify high KAM during landing with high accuracy (Figure 2) (20,22,26). Implementation of the developed prediction tool may increase both the efficacy and efficiency of prevention strategies for noncontact ACL injury, and its widespread use may impact the geometric rise of this injury in female athletes (20). The purpose of the current report is to introduce novel and practical techniques to accurately capture and analyze measures of tibia length, knee valgus motion, knee flexion ROM, quadriceps to hamstrings ratio (QuadHam ratio), and body mass for use in the ACL injury prediction algorithm using field-based measurements and Dartfish software analysis.
Camera Set-Up
Two-dimensional (field-based) frontal and sagittal plane knee kinematic data can be captured with standard video cameras. Cameras should be leveled and placed at 60–80 cm in height, perpendicular to each other in the frontal and sagittal planes. To reduce perspective error, it is optimal to move the camera as far away from the capture area as possible, which allows for fully zoomed view to be focused on desired capture location (34). Two-dimensional frontal and sagittal plane cameras can be connected to a standard personal computer and captured using Dartfish ProSuite 4.5.2.0 (Alpharetta, GA, USA).
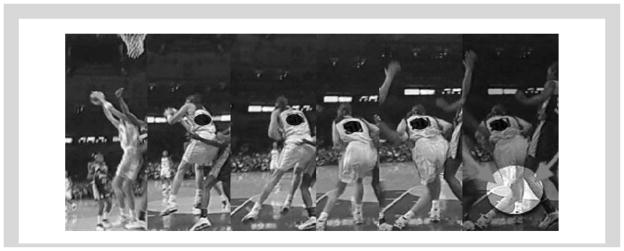
Test Instructions
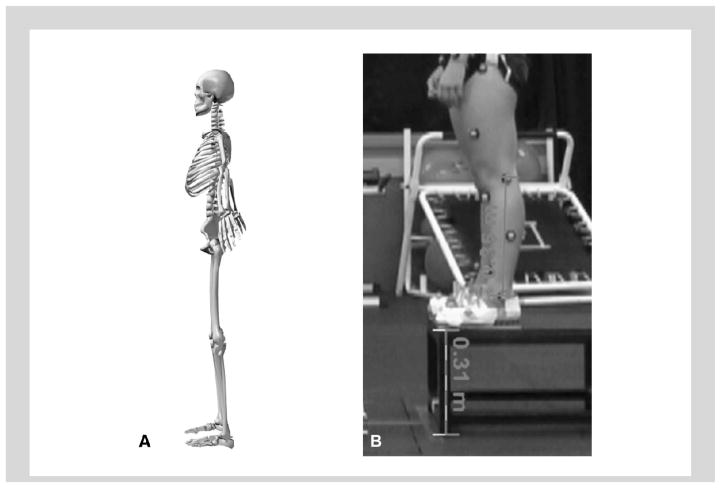
The box (31 cm high) used for the drop vertical jump (DVJ, Figure 3) should be centered on the frontal camera view and approximately 30 cm off center of sagittal plane view away from the camera in the frontal plane position. Before test performance of the DVJ, a standardized target should be placed overhead that is equal to the subject’s maximal touch height during a countermovement vertical jump. The subjects will be instructed to stand on top of a box with their feet positioned 35 cm apart. Once prepared, the subject should drop directly down off the box and immediately perform a maximum vertical jump, raising both arms toward the overhead target (Figure 3). If an overhead target is not used, the test subject is instructed to “upon landing from the box, jump as high as possible as if reaching for a basketball rebound.” (6). The subjects should be allowed one to 3 practice trials to ensure that they are able to demonstrate adequate understanding and ability to perform the instructed test maneuver.
Figure 3.
Depiction of the drop vertical jump test exercise.
Image Capture
Two-dimensional frontal and sagittal plane kinematics should be captured and measured using Dartfish ProSuite 4.5.2.0. Two digital video cameras are aligned perpendicular to each other to capture the subject movement in both the sagittal and frontal plane. The cameras are positioned at a sufficient distance so that the athlete is in view during the entire movement and far enough away to reduce perspective error. The cameras should be set up within the software to their individual specifications. For simplicity, the 4 video frames should be analyzed. (I1) frontal plane view with frame before initial contact, (I2) frontal plane view of frame with knee in maximum medial (valgus) position, (I3) sagittal plane view with frame before initial contact, and (I4) sagittal plane view of frame with knee in maximum flexion position.
Tibia length
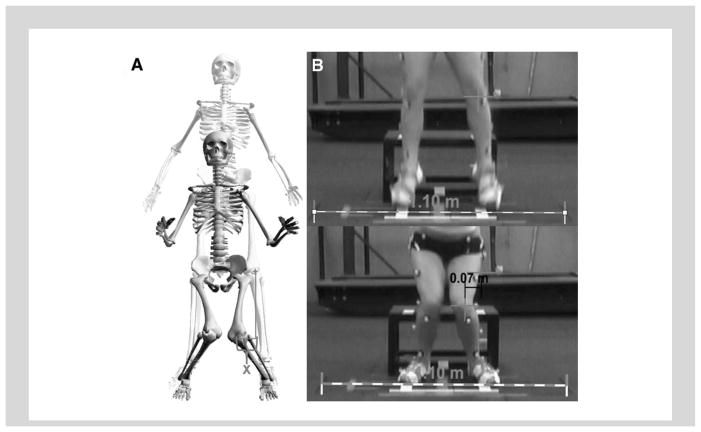
Field-based tibia length should be measured from the sagittal view camera with the subject standing with knees extended before the initiating the DVJ (Figure 4). Before measuring the distance, the video frame is calibrated to a known distance and input into the Dartfish calibration scale. The distance between the lateral knee joint line to the lateral malleous is then measured with the Dartfish measurement tool (Figure 5B).
Figure 4.
A) Tibia length was calculated/measured as the distance between knee joint center and ankle joint center. B) Calibration of the video is performed with the Dartfish scale tool and uses a known distance, which can be used as the video distance correction factor. In the presented example height of the box is used as the known distance. The set scale procedure is then used to input the actual distance. From this calibration step, all length measurements from this camera position are calibrated for the subjects drop vertical jump trials. The measure tool is used to measure the calibrated distance from knee center to the lateral ankle joint center.
Figure 5.
A) Knee valgus motion is the displacement measure between the two knee coordinates in the frontal plane at the frame prior to initial contact and the video frame with maximum medial knee position. B) Calibration of video is performed with the Dartfish scale tool and uses a known distance marked on the floor in the same plane as the athlete as the correction factor in the frontal plane axis. In the presented example, the line tool is used to draw a line corresponding to a known distance on the floor. The set scale procedure is then used to input this distance. From this calibration step, all length measurements from this camera position are calibrated for the subjects drop vertical jump trials. The coordinate position of knee joint center is denoted using the marker tool within Dartfish at the frame prior to initial contact. The coordinate position of knee joint center is again denoted with the marker tool at the frame with maximum medial position and is utilized as the knee valgus position. “X” denotes the calibrated displacement measure between the two digitized knee coordinates and represents the subject’s knee valgus motion during the drop vertical jump.
Knee valgus motion
For the frontal plane analysis, each trial is analyzed by selecting the data frame immediately before initial contact and the frame in which maximum medial knee position occurred for the left leg (Figure 6A). Before measurement of field-based knee valgus motion from the frontal view, the video frame should be calibrated to a known distance that is input into the Dartfish calibration scale (Figure 5B). The midpoint of the joint line is identified in both frames with the marker software tool within Dartfish. The calibrated horizontal displacement measure between the 2 digitized knee coordinates is representative of knee valgus motion during the DVJ (Figure 5B). The snapshot tool is used to save each analyzed frame for later presentation to the athlete to facilitate feedback during neuromuscular training.
Figure 6.
A) Q1 represents the initial measure of sagittal plane knee flexion angle while the subject performs the drop vertical jump. Q2 represents the sagittal plane knee flexion angle taken at maximum knee flexion during landing. The displacement of knee flexion is found by calculating the differences in knee flexion position between positions (X = Q1−Q2). B) Q1 and Q2 are captured using the Dartfish angle tool in the video frame just before initial contact (Q1) and at maximum knee flexion during landing (Q2) of the drop vertical jump.
Knee flexion ROM
The sagittal plane analysis is conducted by selection of the data frame immediately before initial contact and the frame in which maximum knee flexion angle occurred for the left leg (Figure 6A). The Dartfish angle tool is used to assess the knee flexion angle in both frames by alignment of the 3 points with the center of rotation for the knee, ankle, and hip joints. The displacement (ROM) of knee flexion is calculated as the difference in knee flexion angles at the frame before initial contact and maximum knee flexion and was representative of knee flexion ROM (Figure 6B). The snapshot tool is used to save each analyzed frame for later presentation to the athlete during neuromuscular training.
Body mass
Body mass is measured to the nearest kilogram on a calibrated physician scale.
QuadHam ratio
Isokinetic knee extension/flexion (concentric/concentric muscle action) strength is measured on a standard isokinetic testing device for each leg at 300°·s−1 (15). The QuadHam ratio is calculated as the ratio of quadriceps to hamstrings peak isokinetic torque. Some clinical settings may not have an isokinetic testing device readily available. In this case, a surrogate measure of the QuadHam ratio can be employed that was defined using linear regression analysis to predict QuadHam ratio based on the athlete’s body mass. The surrogate QuadHam ratio measure can be obtained by multiplying the female athlete’s mass by 0 .01 and addition of the resultant value to 1.10. If greater simplicity is desired, the mean value of 1.53 can be substituted into the prediction algorithm for QuadHam ratio (23).
Discussion
To use the prediction algorithm (Figure 2), a straight edge was placed vertically so that it touches the designated variable on the axis for each predictor value, and the recorded value that each of the 5 predictors was used to provide “points” on the axis at the top of the diagram. All of the recorded “points” measured using this method were then summed and this value was located on the “total points” axis. A straight edge was used to bisect the “total points line” to the “probability line,” which provided the probability that the athlete demonstrated high KAM (>21.74 N·m of knee abduction) during the DVJ based on the utilized predictive variables.
Figure 7 provides a completed nomogram based on the representative subject’s anthropometrics (Figure 4–tibia length = 35 cm), strength measures (QuadHam ratio = 1.55 and demonstrated landing mechanics; Figure 5–knee valgus motion = 7 cm; Figure 6–knee flexion ROM = 58.9). The ACL injury prediction algorithm indicates that the presented subject would demonstrate a 70% probability to demonstrate high KAM landing (Figure 7). Using the labor-intensive data collection procedures with expensive biomechanical laboratory equipment, we were able to confirm this subject landed with 24.2 N·m of KAM during her DVJ trial. This example demonstrates the novelty of the developed methodology that employs simplified field-based measurements and Dartfish software analysis techniques that are easily performed in the athletic training room, weight room and field to quickly and accurately screen for high KAM.
Figure 7.
Example of completed nomogram based on the representative subject’s anthropometrics (Figure 4–tibia length = 35 cm), strength measures (QuadHam ratio = 1.55 and demonstrated landing mechanics; Figure 5–knee valgus motion = 7 cm; Figure–knee flexion range of motion [ROM] = 58.9). The anterior cruciate ligament (ACL) injury prediction algorithm indicates that the subject would demonstrate a 70% probability to demonstrate high KAM.
Neuromuscular training reduces the high KAM risk factor for ACL injury, increases performance and decreases knee, and ACL injury incidence in female athletes (9,10,12,17–19,27,28). However, reevaluation of ACL injury rates in female athletes indicates that this important health issue has yet to be resolved, as increased knowledge and application of injury prevention techniques have not lead to measurable reductions in ACL injury incidence in female athletes (1). A recent investigation by Grindstaff and colleagues indicated that standard, nontargeted neuromuscular training programs may require application to 89 female athletes to prevent a single ACL injury, and current evidence indicates that limited compliance with nontargeted training may further increase the numbers needed to treat (8,36). It is possible through the use of the presented ACL injury risk algorithm that identification of female athletes who demonstrate risk factors for ACL injury, such as high KAM, could be targeted for neuromuscular training and improve the efficiency of injury prevention methods. The current methods can be used to facilitate the next critical step to bridge the gap between laboratory identification of injury risk factors (11,34) and clinical practices achieved in the field (16,23,26). Specifically, through targeted application of specific neuromuscular training techniques, interventions aimed to reduce risk factors would demonstrate improved efficiency and efficacy. Accordingly, the improved application of neuromuscular training may dramatically decrease injury risk and help young female athletes maintain the associated benefits of active lifestyle gained from sport participation.
Practical Applications
The use of the described algorithmic techniques provides a systematic methodology to accurately capture and analyze measures of body mass, tibia length, quadriceps to hamstrings ratio, knee valgus motion, and knee flexion ROM for use in the ACL injury risk prediction algorithm. The novel aspect of this methodology is that the ACL injury risk prediction algorithm uses simplified field-based measurements and Dartfish software analysis that can be easily performed in the athletic training room, weight room, or on the athletic field. The provided prediction algorithm provides a mechanism to guide targeted training techniques to specifically address and correct neuromuscular deficits that increase high KAM risk within the algorithm (16). In part II of this series, we will discuss how to use the information from the algorithm and apply training techniques that are specifically intended to reduce risk of high KAM based on the individual factors identified with the algorithmic approach.
Acknowledgments
The authors would like to acknowledge funding support from National Institutes of Health/NIAMS Grants R01-AR049735, R01-AR05563, and R01-AR056259. The authors would like to thank Boone County Kentucky, School District, especially School Superintendent Randy Poe, for participation in this study. They would also like to thank Mike Blevins, Ed Massey, Dr. Brian Blavatt, and the athletes of Boone County public school district for their participation in this study. The authors would also like to acknowledge the Cincinnati Children’s Sports Medicine Biodynamics Center Team who have contributed intellectually and physically to the presented research outcomes.
References
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: A 13-year review. Am J Sports Med. 2005;33:524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 3.Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 4.Deacon A, Bennell K, Kiss ZS, Crossley K, Brukner P. Osteoarthritis of the knee in retired, elite Australian Rules footballers. Med J Aust. 1997;166:187–190. doi: 10.5694/j.1326-5377.1997.tb140072.x. [DOI] [PubMed] [Google Scholar]
- 5.Fleming BC. Biomechanics of the anterior cruciate ligament. J Orthop Sports Phys Ther. 2003;33:A13–A15. [PubMed] [Google Scholar]
- 6.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 7.Freedman KB, Glasgow MT, Glasgow SG, Bernstein J. Anterior cruciate ligament injury and reconstruction among university students. Clin Orthop Relat Res. 1998;356:208–212. doi: 10.1097/00003086-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 8.Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: A numbers-needed-to-treat analysis. J Athl Train. 2006;41:450–456. [PMC free article] [PubMed] [Google Scholar]
- 9.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86-A:1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, Myer GD, Ford KR, Heidt RS, Jr, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 12.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 13.Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, Hewett TE, Bahr R. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. Am J Sports Med. 2007;35:359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 14.Malone TR, Hardaker WT, Garrett WE, Feagin JA, Bassett FH. Relationship of gender to anterior cruciate ligament injuries in intercollegiate basketball players. J South Orthop Assoc. 1993;2:36–39. [Google Scholar]
- 15.Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19:3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myer GD, Ford KR, Brent JL, Hewett TE. An integrated approach to change the outcome part II: Targeted neuromuscular training techniques to reduce identified ACL injury risk factors. J Strength Cond Res. 2012;26:2272–2292. doi: 10.1519/JSC.0b013e31825c2c7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on power, balance and landing force in female athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 18.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:1–7. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myer GD, Ford KR, Divine JG, Hewett TE. Specialized dynamic neuromuscular training can be utilized to induce neuromuscular spurt in female athletes. Med Sci Sports Exerc. 2004;36:343–344. [Google Scholar]
- 20.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and freeware computer analysis. Br J Sports Med. 2011;45:238–244. doi: 10.1136/bjsm.2010.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Khoury J, Hewett TE. Three-dimensional motion analysis validation of a clinic-based nomogram designed to identify high ACL injury risk in female athletes. Phys Sportsmed. 2011;39:19–28. doi: 10.3810/psm.2011.02.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2011;45:245–252. doi: 10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory based measures for use in ACL injury risk prediction algorithm. Clin Biomech (Bristol, Avon) 2010;25:693–699. doi: 10.1016/j.clinbiomech.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory measures for use in non-contact anterior cruciate ligament injury risk prediction algorithm. Clin Biomech (Bristol, Avon) 2010;25:693–699. doi: 10.1016/j.clinbiomech.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025–2033. doi: 10.1177/0363546510370933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic based prediction tool to identify high ACL injury risk female athletes. Am J Sports Med. doi: 10.1177/0363546510370933. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 28.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 29.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NCAA. NCAA Injury Surveillance System Summary. Indianapolis, IN: National Collegiate Athletic Association; 2002. [Google Scholar]
- 31.NFHS. 2002 High School Participation Survey. Indianapolis, IN: National Federation of State High School Associations; 2002. [Google Scholar]
- 32.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: A systematic video analysis. Am J Sports Med. 2004;32:1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 33.Padua DA, Marshall SW, Beutler AI, Garrett WE. Prospective cohort study of biomechanical risk factors of ACL injury: The JUMP-ACL study. American Orthopaedic Society of Sports Medicine Annual Meeting; Keystone, CO. 2009. pp. 393–395. [Google Scholar]
- 34.Paul JA, Douwes M. Two-dimensional photographic posture recording and description: A validity study. Appl Ergon. 1993;24:83–90. doi: 10.1016/0003-6870(93)90079-o. [DOI] [PubMed] [Google Scholar]
- 35.Pubmed.gov. Results from “Anterior Cruciate Ligament” MESH Search With Limits Activated. U.S. National Library of Medicine National Institutes of Health; 2010. Publication Date from 2000/01/01 to 2010/02/26. [Google Scholar]
- 36.Sugimoto D, Myer GD, Bush HM, Klugman MF, Mckeon JM, Hewett TE. Effect of compliance with neuromuscular training on ACL injury risk reduction in female athletes: A meta-analysis. J Athl Train. doi: 10.4085/1062-6050-47.6.10. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]