Abstract
Background
The burden of cardiovascular disease world-wide is one of great concern to patients and health care agencies alike. Traditionally centre-based cardiac rehabilitation (CR) programmes are offered to individuals after cardiac events to aid recovery and prevent further cardiac illness. Home-based cardiac rehabilitation programmes have been introduced in an attempt to widen access and participation.
Objectives
To determine the effectiveness of home-based cardiac rehabilitation programmes compared with supervised centre-based cardiac rehabilitation on mortality and morbidity, health-related quality of life and modifiable cardiac risk factors in patients with coronary heart disease.
Search methods
We updated the search of a previous review by searching the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (2007, Issue 4), MEDLINE, EMBASE and CINAHL from 2001 to January 2008. We checked reference lists and sought advice from experts. No language restrictions were applied.
Selection criteria
Randomised controlled trials (RCTs) that compared centre-based cardiac rehabilitation (e.g. hospital, gymnasium, sports centre) with home-based programmes, in adults with myocardial infarction, angina, heart failure or who had undergone revascularisation.
Data collection and analysis
Studies were selected independently by two reviewers, and data extracted by a single reviewer and checked by a second one. Authors were contacted where possible to obtain missing information.
Main results
Twelve studies (1,938 participants) met the inclusion criteria. The majority of studies recruited a lower risk patient following an acute myocardial infarction (MI) and revascularisation. There was no difference in outcomes of home- versus centre-based cardiac rehabilitation in mortality risk ratio (RR) was 1.31 (95% confidence interval (C) 0.65 to 2.66), cardiac events, exercise capacity standardised mean difference (SMD) −0.11 (95% CI −0.35 to 0.13), as well as in modifiable risk factors (systolic blood pressure; diastolic blood pressure; total cholesterol; HDL-cholesterol; LDL-cholesterol) or proportion of smokers at follow up or health-related quality of life. There was no consistent difference in the healthcare costs of the two forms of cardiac rehabilitation.
Authors’ conclusions
Home- and centre-based cardiac rehabilitation appear to be equally effective in improving the clinical and health-related quality of life outcomes in acute MI and revascularisation patients. This finding, together with an absence of evidence of difference in healthcare costs between the two approaches, would support the extension of home-based cardiac rehabilitation programmes such as the Heart Manual to give patients a choice in line with their preferences, which may have an impact on uptake of cardiac rehabilitation in the individual case.
Medical Subject Headings (MeSH): *Home Care Services, *Rehabilitation Centers, Myocardial Infarction [*rehabilitation], Myocardial Revascularization [*rehabilitation], Randomized Controlled Trials as Topic
MeSH check words: Adult, Aged, Female, Humans, Male, Middle Aged
BACKGROUND
Coronary heart disease (CHD) is a major cause of death and disability. Globally there were an estimated 7.22 million deaths from CHD in 2002 (WHO 2004). Although CHD mortality has decreased in many developed countries, with recent advances in treatment and prevention over half of these people are surviving (Allender 2008).
Cardiac rehabilitation (CR) is offered to individuals after cardiac events to aid recovery and prevent further cardiac illness. Cardiac rehabilitation has been shown to improve physical health, and decrease subsequent morbidity and mortality (Jolliffe 2001; Taylor 2004). Cardiac rehabilitation programmes typically achieve this through exercise, education, behaviour change, counselling and support and strategies that are aimed at targeting traditional risk factors for cardiovascular disease. Cardiac rehabilitation is an essential part of the contemporary care of heart disease and is considered a priority in countries with high prevalence of CHD and heart failure (Balady 2007; Graham 2007; NICE 2007; Stone 2005).
Although the beneficial effects of cardiac rehabilitation have been shown, participation remains sub-optimal. One of the main reasons people give for not accepting the invitation to attend cardiac rehabilitation are difficulties in regularly attending sessions at their local hospital and reluctance to take part in group-based classes (Beswick 2004). Home-based cardiac rehabilitation programmes have been introduced in an attempt to widen access and participation. In the UK home-based cardiac rehabilitation with a self-help manual - the Heart Manual - supported by a nurse facilitator (Lewin 1992) is a popular method of rehabilitation. Figures from the National Audit for Cardiac Rehabilitation (NACR) indicate that of the 199 sites in UK and Republic of Ireland that currently provide cardiac rehabilitation, 39 (19.6%) of these sites are currently providing the Heart Manual with some 13,000 copies to patients in UK each year (Heart Manual 2008). The Heart Manual has also been used in Italy, Canada, Australia and New Zealand (Heart Manual 2008).
The one systematic review (of randomised controlled trials) to date comparing home- and centre-based cardiac rehabilitation concluded that the outcomes of both settings were broadly similar (Jolly 2006). However, the authors commented that this conclusion was subject to uncertainty given both the poor quality of and small size of included trials. The total sample size across all trials was only 750 patients and excluded heart failure. We are aware of the recent completion of two large UK-based randomised controlled trials comparing home- and centre-based cardiac rehabilitation (Dalal 2007; Jolly 2007). This review aims to update the evidence base for home and centre-based cardiac rehabilitation using Cochrane review methodology.
OBJECTIVES
To determine the effectiveness of home-based cardiac rehabilitation programmes compared with supervised centre-based cardiac rehabilitation on mortality and morbidity, health-related quality of life and modifiable cardiac risk factors in patients with coronary heart disease.
METHODS
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (individual or cluster level) either parallel group, cross-over or quasi-randomised design were eligible for inclusion. Systematic reviews and meta-analyses were identified as a source of additional randomised controlled trials.
Types of participants
The study population includes adults with MI, angina, or who had undergone revascularisation (coronary artery bypass grafting, percutaneous transluminal coronary angioplasty or coronary artery stent), or heart failure who have taken part, or been invited to take part, in cardiac rehabilitation.
Studies of participants with heart transplants and those implanted with either cardiac resynchronisation therapy (CRT) or implantable defibrillators (ICD) were excluded.
Types of interventions
Home-based cardiac rehabilitation is defined as a structured programme with clear objectives for the participants, including monitoring, follow up visits, letters or telephone calls from staff, or at least self-monitoring diaries. The comparison group is centre-based cardiac rehabilitation based in a variety of settings (e.g. hospital physiotherapy department, University gymnasium, community sports centre).
Types of outcome measures
Mortality (cardiac and overall), morbidity (reinfarction, revascularisation, cardiac associated hospitalisation), exercise capacity, modifiable coronary risk factors (smoking behaviour, blood lipid levels, blood pressure), health-related quality of life, adverse events (withdrawal from the exercise programme), health service utilisation or costs and cost effectiveness. During the review (and before any data analysis) it was decided that the outcome of adherence to intervention should be included, as it may have an influence on the values of the other outcomes.
Search methods for identification of studies
As this review forms part of a broader review, that includes updates of three other Cochrane systematic reviews addressing cardiac rehabilitation (Jolliffe 2001; Rees 2004a; Rees 2004b) and a new review (Davies 2008) of interventions for enhancing uptake and adherence to cardiac rehabilitation, a generic search strategy was undertaken.
Electronic searches
Randomised controlled trials were identified from a previously published systematic review (Jolly 2006). This list of studies was updated by searching the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (2007, issue 4), MEDLINE (2001 to January 2008), EMBASE (2001 to January 2008), CINAHL (2001 to January 2008), and PsycINFO (2001 to January 2008), Health Technology Assessment (HTA) and the Database of Abstracts of Reviews of Effects (DARE) databases were searched via the NHS Centre for Reviews and Dissemination (CRD) website (2001 to January 2008). Conference Proceedings were searched on Web of Science: ISI Proceedings (2001 to January 2008).
A full search of CENTRAL was undertaken. All other searches were run from 2001 as this is the earliest date of searches for the previous Cochrane reviews on cardiac rehabilitation (Jolliffe 2001; Rees 2004a; Rees 2004b). This date overlaps the dates of the searches of the previous review on this topic (Jolly 2006).
Searches were limited to RCTs, systematic reviews, and meta-analysis and a filter applied to limit by humans. No language or other limitations were imposed. Consideration was given to variations in terms used and spellings of terms in different countries so that studies were not missed by the search strategy because of such variations. Search strategies were designed with reference to those of the previous systematic review (Jolly 2006) and in accordance with Cochrane methods (Higgins 2008). See Appendix 1 for details of search strategies.
Searching other resources
Reference lists of all eligible trials and systematic reviews were searched for additional studies.
Data collection and analysis
Selection of studies
The titles and abstracts of studies identified were screened and clearly irrelevant studies discarded. The full-text reports of all potentially relevant randomised and quasi-randomised trials were obtained and assessed independently for eligibility, based on the defined inclusion criteria, by two reviewers (RST and Philippa Davies). Any disagreement was resolved by discussion and in those few occasions where uncertainty remained, the opinion of two further reviewers was taken (KJ, AZ).
Data extraction and management
A revised data extraction form was used to incorporate new additions on quality assessment in the Cochrane Handbook (Higgins 2008). Relevant data regarding inclusion criteria (study design, participants, interventions, and outcomes), risk of bias (randomisation, blinding, attrition and outcome reporting) and results were extracted. In cases where insufficient data were reported (e.g. method of randomisation, statistical methods) authors were contacted for further information. Data extraction was carried out by a single reviewer (AZ) and checked by a second reviewer (RST). Excluded studies and reasons for exclusion are detailed in Characteristics of excluded studies. Where necessary authors of included studies were contacted for missing information.
Assessment of risk of bias in included studies
In accord with the recently updated Cochrane Handbook for Systematic Reviews (Higgins 2008) and RevMan update (RevMan 5), risk of bias was assessed in terms of the of quality of random sequence generation and allocation concealment, description of drop-outs and withdrawals (including analysis by intention-to-treat), blinding (participants, personnel and outcome assessment) and selective outcome reporting. In addition evidence was sought that the groups were balanced at baseline and that intention to treat analysis was undertaken. The risk of bias in eligible trials was assessed by a single reviewer (AZ) and checked by a second reviewer (RST).
Data synthesis
Data were processed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We sought outcome results at follow up and the focus of this review was the between-group difference in home- versus centre-based groups. For dichotomous variables relative risks and 95% confidence intervals (CI) were derived for each outcome. For continuous variables mean differences and 95% CI were calculated for each outcome.
Heterogeneity amongst included studies was explored qualitatively (by comparing the characteristics of included studies) and quantitatively (using the chi-squared test of heterogeneity and I2 statistic). Where appropriate, the results from included studies were combined for each outcome to give an overall estimate of treatment effect. A fixed-effect meta-analysis was used except where statistical heterogeneity was identified, in which case a random-effects model was used.
Given the variety of exercise capacity measures reported, results for this outcome were expressed as a standardised mean difference (SMD). Otherwise continuous outcomes were pooled as weighted mean difference (WMD). For the purposes of meta-analysis, in the one study that reported continuous outcomes, findings by three age subcategories results were pooled in order to produce a single omnibus score for each group.
We had intended to use stratified meta-analysis and meta-regression to further explore heterogeneity and examine potential treatment effect modifiers. Given the small number of included trials such analyses were deemed inappropriately underpowered. However, subgroup analyses undertaken within trials were noted.
Sensitivity analysis was used to examine two areas of uncertainty in this review. Firstly, for exercise capacity, in addition to pooling all trials using SMD, the majority of trials that reported outcomes as metabolic equivalents (METs) were pooled using WMD. Secondly, because of the lack of detailed reporting there was some doubt that whether the study Kassaian 2000 was a true comparison between home- and hospital-based cardiac rehabilitation or rather a comparison of hospital-based cardiac rehabilitation versus usual care. All meta-analyses were undertaken with and without the inclusion of this trial.
Marchionni 2003 reported outcomes for home- and centre-based group according to three patient age subgroups (i.e. 45-65, 66-75, >75 years). These data have been pooled to obtain a single overall outcome result for home- and centre-based groups. Gordon et al compared two home-based exercise groups: physician-supervised nurse-case-managed programme (Gordon 2002 Supervised) and community-based programme (Gordon 2002 Community) versus centre-based cardiac rehabilitation programme, while study of Miller et al reported results in subgroups by different time of intervention: home versus centre-based brief - 11 weeks (Miller 1984 Brief) and home versus centre-based expanded - 26 weeks (Miller 1984 Expanded). For each of these two studies, outcome results are reported separately for both home versus centre comparison groups.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
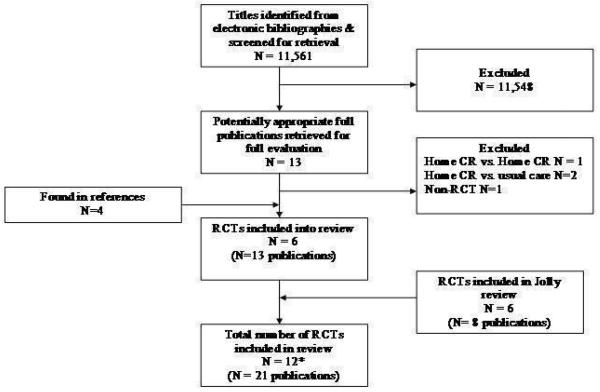
Our update cross-cardiac rehabilitation review electronic searches yielded a total 11,561 titles. After reviewing titles and abstracts 13 full papers were retrieved for possible inclusion. Reviewing reference lists of all eligible publications identified four more publications for possible inclusion. After examining the full text, four papers were excluded and six studies (reported in 13 papers) were included. The systematic review Jolly 2006 identified six trials (reported in eight papers) all of which met the inclusion criteria of this review. Therefore in total 21 papers reporting on 12 studies were included in the review. The study selection process is summarised in the QUOROM flow diagram shown in Figure 1.
Figure 1. Summary of study selection process.
* Two of the studies had three comparison arms and these have been analysed separately giving in total 14 comparisons.
Included studies
We included 12 trials (1,938 participants) comparing a home-based to a centre-based cardiac rehabilitation programme. Two of the studies had three comparison arms and these have been analysed separately giving in total 14 comparisons. Six of these studies were included in the previous systematic review, Jolly 2006 (Arthur 2002; Bell 1998; Carlson 2000; Marchionni 2003; Miller 1984 Brief, Miller 1984 Expanded; Sparks 1993). Six new trials were identified: two, whose publication dates predated the searches for Jolly 2006, but were missed from the review (Gordon 2002 Community, Gordon 2002 Supervised; Kassaian 2000), and four published since 2003 (the end search date of Jolly 2006 (Dalal 2007; Daskapan 2005; Jolly 2007; Wu 2006).
Three studies were UK-based (Bell 1998; Dalal 2007; Jolly 2007); four were based in US (Carlson 2000; Gordon et al (Gordon 2002 Community; Gordon 2002 Supervised); Miller et al (Miller 1984 Expanded; Miller 1984 Brief); Sparks 1993) and one each in Canada (Arthur 2002), Turkey (Daskapan 2005), Italy (Marchionni 2003), Iran (Kassaian 2000) and China (Wu 2006). Most studies reported outcomes up to 12-month post-randomisation. Only three studies reported longer-term follow up (Jolly 2007 24 months; Marchionni 2003 14 months; Arthur 2002 18 months). Eight studies compared comprehensive programmes (i.e. exercise plus the education and/or psychological management) while the remainder reported only an exercise intervention (Daskapan 2005; Kassaian 2000; Miller 1984 Brief; Miller 1984 Expanded; Wu 2006). The cardiac rehabilitation programmes differed considerably in duration (range: 1.5 to 6 months), frequency (1 to 5 sessions per week) and session length (20-60 minutes per session). Most programmes used individually tailored exercise prescription which makes it difficult to precisely quantify the amount of exercise undertaken. Centre-based programmes typically provided supervised cycle and treadmill exercise while virtually all home programmes were based on walking, with some level of intermittent nurse or exercise specialist telephone support. The majority of studies recruited a lower risk patient following an acute MI and revascularisation, excluding those with significant arrhythmias, ischaemia, or heart failure. Two studies included individuals with New York Heart Association (NYHA) class 2 or 3 heart failure (Daskapan 2005; Kassaian 2000).
Details of included studies are listed in Characteristics of included studies.
Excluded studies
Four papers were excluded: one was a comparison of two forms of home-based cardiac rehabilitation (Senuzun 2006), two were comparisons of home based cardiac rehabilitation versus usual care (Sinclair 2005; Tygesen 2001) and one was a non-RCT (Ades 2000). Details of excluded studies are listed in Characteristics of excluded studies.
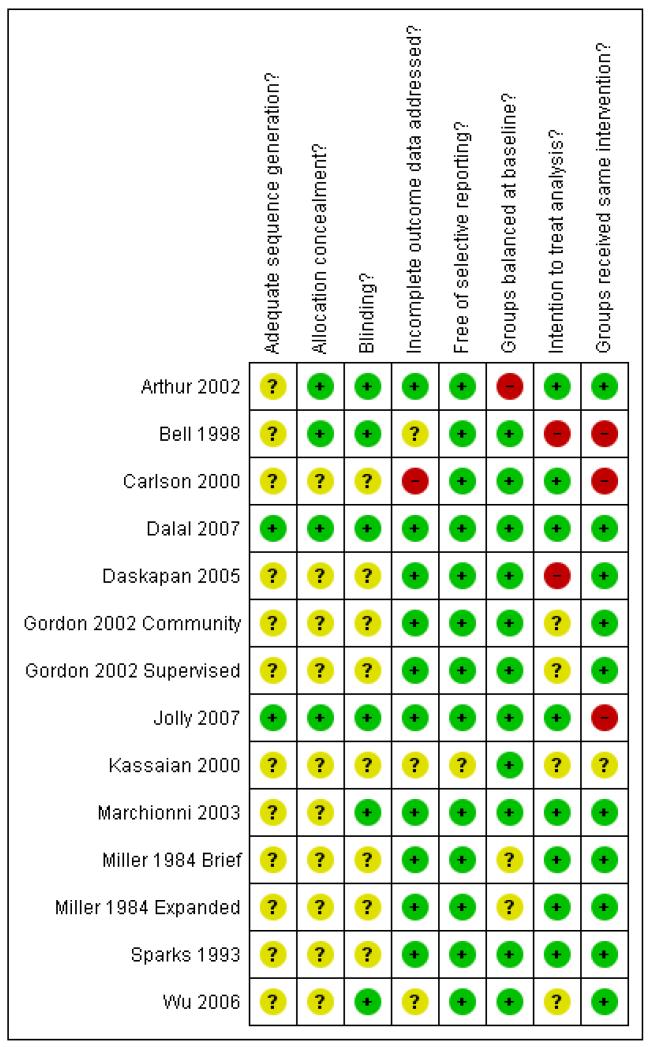
Risk of bias in included studies
A number of studies failed to give sufficient detail to assess their potential risk of bias (Figure 2). Details of generation and concealment of random allocation sequence were particularly reported. In one case there was objective evidence of imbalance in baseline characteristics (Arthur 2002). Blinding of patients and carers in studies on CR is impossible; in such situations, blinding outcome assessment to knowledge of allocation may be of great importance. However only six of the studies stated that they took measures to blind outcome assessment, this may have weakened their conclusions.
Figure 2. Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Where reported, losses to follow up varied considerably across studies and was often asymmetric across home- and centre-based cardiac rehabilitation groups. Although often not stated, all studies appeared to undertake an intention to treat analysis in that groups were analysed according to initial random allocation. The impact of losses to follow up or drop out was only examined in a few trials. As discussed above, the rehabilitation intervention was usually tailored to the individual patient and therefore it is difficult to quantify the precise level of intervention. However, based on the general description of the intervention reported by authors, there appeared to be substantive differences in the nature of the rehabilitation input between home- and centre-based arm. For example, the studies Bell 1998, Dalal 2007 and Jolly 2007 included hospital cardiac rehabilitation programmes which were fixed in terms frequency and content over the period of the study. In contrast the home-based intervention in these studies consisted of the Heart Manual where the patients could self-regulate the frequency and nature of rehabilitation sessions they undertook.
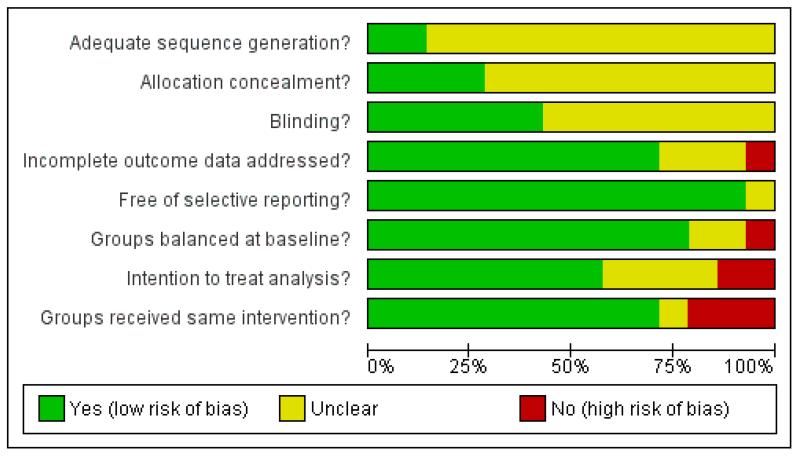
Methodological quality graph (Figure 3) presents review authors’ judgements about each methodological quality item presented as percentages across all included studies. Given the small number of included trials we were unable to assess publication bias using Funnel plot approach (Higgins 2008).
Figure 3. Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Effects of interventions
Exercise capacity
All 12 included studies reported exercise capacity in the short-term (3 to 12 months follow up), while three (Arthur 2002; Jolly 2007; Marchionni 2003) presented longer-term data (12 to 24 months follow up). All reported exercise capacity at follow up, except one (Gordon 2002 Supervised; Gordon 2002 Community) which instead reported change in exercise capacity at follow up compared to baseline.
Nine studies reported exercise capacity as maximal oxygen uptake (VO2max) either as metabolic equivalents (METs) or millilitres per kilogram of body mass per minute (ml/kg/min) or millilitres (ml) (Sparks 1993). Jolly (Jolly 2007) reported incremental shuttle walking distance (in metres, m), Marchionni 2003 reported total cycle work capacity (in kilograms of body mass multiplied by meters (kg*m)) and Gordon (Gordon 2002 Community; Gordon 2002 Supervised) reported change data only as METs.
In the pooled analysis across all studies reporting short-term data (1,938 patients) there was no evidence of a statistically significant difference in short-term exercise capacity between home-based and centre-based cardiac rehabilitation (random effects SMD = −0.11, 95% CI −0.35 to 0.13, Analysis 1.1). There was evidence of substantial heterogeneity (I2 = 79%; Chi2 = 60.91; P < 0.00001). The same findings were seen when pooling was limited to the eight trials reporting VO2max (random effects WMD = −0.30, 95% CI −1.22 to 0.63; I2 = 88%; Chi2 = 68.6; P < 0.0001). Excluding Kassaian 2000 from the later analysis reduced the degree of heterogeneity but produced the same finding of no evidence of significant difference between group (random effects WMD = 0.16, 95% CI −0.44 to 0.77, P = 0.59; I2 = 69%; Chi2 = 22.2; P = 0.002).
In a pooled analysis of three studies (Arthur 2002; Jolly 2007; Marchionni 2003) reporting longer-term data (12 to 24 months; 1,074 patients) there was some evidence, albeit not statistically significant, of superior exercise capacity in the home- compared to the centre-based group (fixed effect SMD 0.11, 95% CI −0.01 to 0.23; I2 = 0%; Chi2 = 0.97; P = 0.62; Analysis 1.2).
In all studies except two (Dalal 2007; Jolly 2007) exercise capacity was assessed at baseline. In the remaining studies there was consistent evidence of increase in exercise capacity at follow up compared to baseline for both home- and centre-based groups.
Modifiable risk factors
Blood pressure
Seven of the included trials reported both systolic blood pressure (SBP) and diastolic blood pressure (DBP) (Carlson 2000; Dalal 2007; Daskapan 2005; Gordon 2002 Community; Gordon 2002 Supervised; Jolly 2007; Kassaian 2000), or SBP alone (Bell 1998). All studies reported outcome at follow-up, with the exception of one (Gordon 2002 Supervised; Gordon 2002 Community) that instead reported change from baseline. For Dalal (Dalal 2007) non-published follow-up values were obtained on request from the authors. Blood pressure (BP) has been reported as millimetres of Hg (mmHg).
At 3 to 12 months follow up, although no between-group difference was found in pooled systolic blood pressure (random effects WMD = −0.58 mmHg, 95% CI −3.29 to 4.44; I2 = 70%; Chi2=23.01; P = 0.002; Analysis 2.1; 1,053 patients), there was a slightly higher pooled diastolic BP at follow up for home-based compared to centre-based cardiac rehabilitation (fixed effect WMD = 1.85 mmHg; 95%CI 0.74 to 2.96; I2 = 25%; Chi2= 7.97; P = 0.24; 927 patients; Analysis 2.2). However, this difference is not clinically relevant. On excluding Kassaian 2000 this difference in DBP was no longer statistically significant (fixed effect WMD 1.00 mmHg; 95%CI −0.32 to 2.31; I2 = 0%; Chi2= 2.28; P = 0.81) while the finding of no difference in SBP remained (fixed effect WMD = −1.06 mmHg, 95%CI −3.40 to 1.31; I2 = 32%; Chi2= 8.76; P = 0.19). At 24-months follow up, Jolly 2007 reported no significant difference in SBP (mean 0.85 mmHg; 95%CI −2.48 to 4.18), or DBP (mean 0.76 mmHg,95% CI −1.12 to 2.64) between home- and centre-based CR groups. There was no consistent trend across studies in change in blood pressure at follow up compared to baseline.
Blood lipids
Seven of the included trials reported data on blood lipids (Bell 1998; Carlson 2000; Dalal 2007; Gordon 2002 Community; Gordon 2002 Supervised; Jolly 2007; Kassaian 2000), all reporting total cholesterol values, four (Carlson 2000; Gordon 2002 Community; Gordon 2002 Supervised; Jolly 2007; Kassaian 2000) reporting HDL-cholesterol, and three (Carlson 2000; Gordon 2002 Community; Gordon 2002 Supervised; Kassaian 2000) reporting LDL-cholesterol and triglycerides values. All studies but Gordon 2002 reported follow up data, while Gordon (Gordon 2002 Community; Gordon 2002 Supervised) only reported data for change. Study results were expressed as millimols per litre (mmol/l) (Bell 1998; Dalal 2007; Jolly 2007) or milligrams per decilitre (mg/dl) (Carlson 2000; Gordon 2002 Community; Gordon 2002 Supervised; Kassaian 2000); in the latter case there have been converted into mmol/l before being pooled in the metaanalysis.
In all studies with the exception of Kassaian 2000, compared to baseline there was evidence of a decrease in total cholesterol, LDL-cholesterol, and triglyceride levels, and increase of HDL-cholesterol levels at follow up in both home- and centre-based groups.
Total cholesterol
In the pooling analysis at 3 to 12 months follow up there was no evidence of a significant difference in the total cholesterol for the home and centre groups (random effects WMD = 0.13 mmol/l, 95% CI −0.05 to 0.31; I2 = 55%; Chi2= 13.33; P = 0.04; 1,019 patients; Analysis 3.1).
Jolly 2007 reported no significant difference between home- and centre-based cardiac rehabilitation groups in total cholesterol (mean = 0.11 mmol/l, 95% CI: −0.06 to 0.28) at 24-months follow up.
HDL-cholesterol
In the pooling analysis at 3-12 months follow up there was evidence of a lower HDL-cholesterol for the home than for centre (fixed effect WMD = −0.06 mmol/l, 95% CI −0.11 to −0.02; I2 = 38%; Chi2= 6.5; P = 0.16; 793 patients; Analysis 3.2). When Kassaian 2000 was excluded, there was no longer a significant difference between groups in HDL-cholesterol (fixed effect WMD = −0.02 mmol/l, 95% CI −0.08 to 0.04; I2 = 0%; Chi2= 0.5; P = 0.91).
Jolly 2007 reported no significant difference between home- and centre-based cardiac rehabilitation groups in HDL-cholesterol (mean = 0.03 mmol/l, 95%CI −0.10 to 0.04) at 24-months follow up.
LDL-cholesterol
In the pooling analysis at 3-12 months follow up there was no evidence of difference in LDL-cholesterol (fixed effect WMD = 0.15 mmol/l, 95% CI −0.01 to 0.31; I2 = 32%; Chi2= 4.4; P = 0.22; 324 patients; Analysis 3.3). When Kassaian 2000 was excluded between group results remained non significant.
Triglycerides
In the pooling analysis at 3-12 months follow up there was no evidence of difference in triglycerides (random effects WMD = 0.15 mmol/l, 95% CI −0.11 to 0.41; I2 = 60%; Chi2= 7.58; P = 0.06; 328 patients; Analysis 3.4). When Kassaian 2000 was excluded between group results remained non significant.
Smoking behaviour
Five of the 12 studies included reported patient self-reported smoking behaviour at 3-12 months follow up (Bell 1998; Dalal 2007; Gordon 2002 Community; Gordon 2002 Supervised; Jolly 2007). There was no evidence of difference in the proportion of smokers at follow up with centre- and home-based cardiac rehabilitation (fixed effect RR = 1.00, 95% CI 0.71 to 1.41; I2 = 11%; Chi2 = 4.48; P = 0.34; 922 patients; Analysis 4.1). Jolly 2007 reported no difference in smoking between home- and centre-based arms at 24-months (RR = 1.16, 95% CI 0.58 to 33.3).
There was evidence of a consistent reduction in self-reported smoking behaviour following both home- and centre-based cardiac rehabilitation. This finding was confirmed in the one study that used cotinine-validated assessment of smoking (Jolly 2007).
Health-related quality of life
Five out of the 12 included trials reported validated health-related quality of life (HRQoL) measures (Table 1). These included four generic HRQoL instruments EQ-5D (EuroQoL 1990), Nottingham Health Profile (Hunt 1980), Short-Form 36 (SF-36; McHorney 1993), Sickness Impact Profile (Bergner 1976) and one disease-specific instrument (MacNew; Höfer 2004). Given the wide variation in HRQoL outcomes used, pooling across studies was deemed inappropriate. The HRQoL results at follow up and between-group difference for each individual trials were not reported in the original publications and between-group P-values were calculated by the authors of this report using methods outlined in the Cochrane Handbook (Higgins 2008).
Table 1. Summary of HRQoL scores at follow up for home- and centre-based settings.
|
Tial
First author (year) |
Follow up | HRQoL measure |
Outcome values at follow up
Mean (SD) Home vs. Centre, between group P-value |
Between-group difference |
|---|---|---|---|---|
| Bell 1998 | 10.5 months | Nottingham Health Profile Energy Pain Emotional reactions Sleep Social isolation Physical mobility |
18.6 (28.4) vs. 17.3 (30. 7)P = 0.78*
6.6 (15.3) vs. 7.4 (15.5) P = 0.74* 6.6 (15.3) vs. 7.4 (15.5) P = 0.74* 6.6(15.3) vs. 16.9 (22. 8)P = 0.0007* 3.7(13.6) vs. 6.7 (15.0) P = 0.18* 6.9 (13.5) vs. 9.1 (15.9) P =0.33* |
Home = Centre Home = Centre Home = Centre Home < Centre Home = Centre Home = Centre |
| Arthur 2002 | 6-months 18-months |
SF-36 PCS MCS SF-36 PCS MCS |
51.2(6.4) vs. 48.6 (7.1) P = 0.003*
53.5 (6.4) vs. 52.0(8.1) P = 0.13* 48.3(11.7) vs.47.6 (11. 7) P = 0.67* 53.0 (10.9) vs. 50.2 (10. 9) P = 0.07* |
Home > Centre Home = Centre Home = Centre Home = Centre |
| Marchionni 2003 | 2-months 8-months 14-months |
Sickness Impact Profile | 2.83 (14.5) vs. 4.71 (11. 1) P = 0.09*
2.83 (14.5) vs. 3.40 (11. 1) P = 0.61* 2.00 (8.3) vs. 3.70 (11. 8) P = 0.06* |
Home = Centre Home = Centre Home = Centre |
| Dalal 2007 | 9-months | MacNew Global score EQ-5D |
5.60 (1.12) vs. 5.67 (1. 12) P = 0.71 0.74 (0.04) vs. 0.78 (0. 04) P = 0.57 |
Home = Centre Home = Centre |
| Jolly 2007 | 6-months 12-months 24-months |
EQ-5D SF-12 PCS MCS EQ-5D EQ-5D |
0.74 (0.26) vs. 0.76 (0. 23) P = 0.37 42.28 (10.9) 42.56 (10. 8) P = 0.8 49.19 (10.1) 50.33 (9.6) P = 0.3 0.74 (0.27) vs. 0.76 (0. 23) P = 0.52* 0.73 (0.29) vs. 0.75 (0. 26) P = 0.39* |
Home = Centre Home = Centre Home = Centre Home = Centre Home = Centre |
P-value calculated by authors of this report based on independent 2-group t-test.
PCS: Physical component score; MCS: Mental component score.
Home = Centre: no statistically significant difference (P > 0.05) in HRQoL between home & centre-based groups at follow up.
Home > Centre: statistically significant (P ≥ 0.05) higher HRQoL in home versus centre-based groups at follow up.
Home < Centre: statistically significant (P ≥ 0.05) lower HRQoL in home versus centre-based groups at follow up.
Overall there was no evidence of a statistically significant difference in overall HRQoL or domain score at follow up between home and centre-based groups. The two exceptions were a higher Nottingham Health Profile sleep domain score in the hospital compared to the home group in Bell 1998 and a higher SF-36 physical component score in the home compared to centre-based cardiac rehabilitation groups at 6 months in Arthur 2002.
Individual studies reported consistent improvements in HRQoL at follow up with both home and centre-based cardiac rehabilitation compared to baseline. The notable exception was the use of the EQ-5D which failed to identify significant improvements with home- or centre-based cardiac rehabilitation (Dalal 2007; Jolly 2007).
Clinical events
Mortality
Five trials reported all-cause mortality (specific cardiac death have not been separately reported in the included studies) in the period up to 1-year follow up (Bell 1998; Dalal 2007; Daskapan 2005; Jolly 2007; Miller 1984 Brief; Miller 1984 Expanded). The study of Miller (Miller 1984 Brief; Miller 1984 Expanded) reported no deaths in either the home- or centre-based CR groups over the period of the study (and so it has not been included in pooled analysis). In a pooled analysis of the remaining studies (909 patients) there was no evidence of a significant difference in mortality at 3-12 months follow up between home and centre (fixed effect RR = 1.31, 95% CI 0.65 to 2.66; I2 = 0%; Chi2= 1.0, P = 0.8; Analysis 5.1). Excluding Daskapan 2005 (because of patients with NYHA class 2/3 heart failure) the pooled result of 9-12 months studies shows no significant difference as well (RR = 1.25, 95% CI 0.61 to 2.59; I2 = 0%; Chi2= 0.74; P = 0.69). Jolly 2007 reported there to be no between-group difference in mortality at 24-months follow up (RR = 1.99, 95% CI 0.50 to 7.88).
Cardiac events
As two studies reported differing cardiac events during exercise programme: Dalal 2007 (CABG, PTCA) and Jolly 2007 (MI, revascularisations at 12 months and 24 months follow up) we were not able to pool data. No significance difference was found in cardiac events between home-based and centre-based settings in either study.
Withdrawals & adherence
Withdrawal from intervention
Although a number of studies reported drop out rates, the reasons for drop out were often unclear so it was therefore not possible to consistently estimate the number of patients withdrawing from the cardiac rehabilitation programme for each study. However, using the number of completers i.e. number of patients with outcome data at follow up, we found no difference between home based and centre based programmes (fixed effect RR 1.00, 95% CI 0.97 to 1.04; Chi2=11.44, df=10 (P=0.32), I2=13%, Analysis 6.1).
Adherence
Nine out of the 12 included studies reported adherence to the cardiac rehabilitation intervention over the duration of the study (Table 2). However, there was substantial variation in the way in which adherence was defined and measured and some studies reported more than one measure of adherence. Pooling across studies was therefore deemed inappropriate and instead findings are tabulated. Where not reported in the original publications, between-group P-values were calculated by the authors of this report using methods outlined in the Cochrane Handbook (Higgins 2008). Table 2 summarises the adherence findings for each individual trial. In four out of the remaining seven studies there was no evidence of a significant difference in adherence between home- and centre-based groups although this was not the case in Arthur 2002 and Marchionni 2003 which both showed adherence at P ≤ 0.05 in favour of home-based cardiac rehabilitation. No other study reported a significantly higher adherence in the centre-based group compared to home.
Table 2. Summary of adherence at follow up in home- and centre-based settings.
| Trial Study | Follow up | Method/definition of adherence assessment | Findings | Between-group difference |
|---|---|---|---|---|
| Miller 1984 Brief | 6-months | Ratio of exercise session completed vs. prescribed | Home: 50/70 (72%) Centre: 28/40 (71%) P-value not calculable |
Home = Centre** |
| Sparks 1993 | 3-months | Percentage of sessions attended | Home: 93% Centre: 88% P-value not calculable |
? |
| Bell 1998 | Not reported | |||
| Kassaian 2000 | Not reported | |||
| Carlson 2000 | 6-months | Attendance at all 3 nutrition/risk factor classes Total exercise over follow up - no. sessions ≥ 30 min |
Home: 27/38 (71%) Centre: 33/42 (79%) P = 0.438* Home: 111.8 (SD 29.1) Centre: 98.1 (SD 33.4) P = 0.06+ |
Home = Centre Home = Centre |
| Gordon 2002 Community | 3-months | Percentage of completed scheduled appointments (exercise sessions, office/on site visits, “telephone visits” in accordance with intervention protocol) | Home (MD supervised) : 83% Home (community-based): 86% Centre: 81% |
Home = Centre** |
| Arthur 2002 | 6-months 18-months |
Number of exercise session reported/wk Percentage of patients seeking dietician consultation Percentage of patients seeking psychologist consultation Level of physical activity - Physical Activity Scale for the Elderly (PASE) |
Home: mean 6.5 (SD 4. 6) Centre: mean 3.7 (SD 2. 6) P < 0.0001+ Home 50% (3.5±2.5 visits) Centre: 53% (3.6 SD 2. 3 visits) Home: 42% (2.6 SD 2. 4 visits) Centre: 51% (2.5 SD 2. 2 visits) Home: mean 232.6 (99. 4) Centre: mean 170.0 (89. 2) P < 0.0001 + |
Home > Centre ? Home = Centre** Home > Centre |
| Marchionni 2003 | 4-months | Number of exercise sessions completed | Home: 37.3 (SD 3.4) Centre: 34.3 (SD 4.4) P < 0.0001 + |
Home < Centre |
| Daskapan 2005 | 3-months | Percentage sessions attended | Home: 97% Centre: 81% P-value not calculable |
? |
| Dalal 2007 | 9-months | Number who participate in intervention | Home: 40/60 (67%) Centre: 32/44 (72%) P = 0.51* |
Home = Centre |
| Jolly 2007 | 3-months 6-months 12-months 24-months |
Hours of self-reported activity weighted for intensity | Home: 23.2 (SD 22.1) Centre: 18.7 (SD 19.3) P = 0.06+ Home: 16.4 (SD 17.0) Centre: 18.1 (SD 25.4) P = 0.4+ Home: 19.2 (SD 20.8) Centre: 15.9 (SD 16.7) P = 0.06+ Home: 18.9 (SD 18.4) Centre: 16.6 (SD 16.4) P = 0.16+ |
Home = Centre Home = Centre Home = Centre Home = Centre |
| Wu 2006 | Not reported |
P-value calculated by authors of this report based on chi-squared test.
P-value calculated by authors of this report based on independent t-test.
Home = Centre: no statistically significant difference (P > 0.05) in HRQoL between home & centre-based groups at follow up.
Home > Centre: statistically significant (P ≤ 0.05) higher HRQoL in home versus centre-based groups at follow up.
Home < Centre: statistically significant (P ≥ 0.05) lower HRQoL in home versus centre-based groups at follow up.
Home- & centre-based groups at follow up appear to be similar but P-value not reported or calculable.
Home- & centre-based groups at follow up appear different but P-value not reported or calculable.
Costs and healthcare utilisation
Four studies reported costs (Table 3). Given the difference in currencies and timing of studies is not possible to directly compare the costs across studies. In three (Carlson 2000; Dalal 2007; Marchionni 2003) of the four studies the healthcare costs associated with home-based cardiac rehabilitation was lower than centre. However, only in Dalal was this lower cost of home CR shown to be statistically different. Jolly 2007 found the costs of home CR to be more expensive than centre-based one although if patient costs were included the costs of the two were the same. Overall healthcare costs were not different between home and centre. Six studies reported different aspects of healthcare resource consumption that included rehospitalisations, primary care consultations and use of secondary care medication (Table 4). No significant between group differences were seen.
Table 3. Summary of costs in home- and centre-based settings.
|
Trial
First author (year) |
Currency Year of costs Follow up | Cardiac rehabilitation programme cost (per patient) | Programme costs considered | Total healthcare cost (per patient) | Additional healthcare costs considered | Comments |
|---|---|---|---|---|---|---|
| Carlson 2000 | US $ Not reported 6-months |
Home: Mean 1, 519 Centre: Mean 2, 349 |
Staff & ECG monitoring | Not reported | ||
| Marchionni 2003 | US $ 2000 14-months |
Home: Mean 1, 650 Centre: Mean 8, 841 |
Not reported | Home: 21,298 Centre: 13,246 |
Not reported | |
| Dalal 2007 | UK £ 2002-3 9-months |
Home: Mean 170 (SD 8) Centre: Mean 200 (SD 3) Difference: Mean 30 95% CI: −45 to −12 P<0.0001 |
Staff exercise equipment staff travel | Home: Mean 3, 279 (374) Centre: Mean 3, 201 (443) Difference: Mean 78 95% CI: −1,103 to 1,191 P=0.894 |
Rehospitalisations, revascularisations, secondary preventive medication, investigations, primary care consultations | |
| Jolly 2007 | UK £ 2003 24-months |
Home: Mean 198 95% CI: 189 to 209 Centre: Mean 157 95% CI: 139 to 175 P<0.05 |
Staff telephone consultations staff travel | Not reported | With inclusion of patient costs (travel and time) , the societal costs of home and centre CR were not significantly different |
Table 4. Summary of healthcare care utilisation in home- and centre-based settings.
|
Trial
First author (year) |
Dalal (2007) | Gordon (2002) | Bell (1998) | Carlson (2000) | Marchonni (2003) | Jolly (2007) | ||
|---|---|---|---|---|---|---|---|---|
| Follow up | 9-months | 3-months | 0-6 months | 6-12 months | 6-months | 14-months | 12-month | 24-month |
|
Rehospitalisations
N patient (%) Mean (SD) |
Home 9/60 (15%) Centre 6/44 (14%) P=0.845 Home 2.2 (0.9)+ Centre 1.2 (0.6) P=0.383 |
Home 21/90 (23%) Centre 19/88 (22%) P=0.78# |
13/89 (15%) 12/84 (14%) P=0.95# |
Home 0.46 (SE 0.1) Centre 0.33 (SE 0.1) P=0.49 |
(6 to 12 m) Home 0.08 (0.34) Centre 0.12 (0.41) P=0.3 |
(12 to 24 m) Home 0.20 (0.45) Centre 0.26 (0.57) P=0.3 |
||
|
Primary care consultations
Mean (SD) |
Home 6.3 (0.6) Centre 7.0 (0.9) P=0.514 |
Home 6.6 (3.6)* Centre 6.6 (4.1) P=1.00# |
5.4 (4.1) 4.6 (3.7) P=0.19# |
(9 to 12 m) Home 0.65 (1.14) Centre 0.72 (1.54) P=0.8 |
(21 to 24 m) Home 0.53 (1.14) Centre 0.66 (1.42) P=0.7 |
|||
|
Secondary prevention medication
N patients (%) β-blockers ACE inhibitors Statins Antiplatelets |
Home 31/49 (63%) Centre 24/34(71%) P=0.49 Home 30/49 (61%) Centre 24/33 (73%) P=0.28 Home 48/49 (98%)* Centre 30/35(88%)* P=0.18 Home 46/49 (94%) Centre 30/35 (86%) P=0.21 |
Home 36/97 (37%) Centre 17/45 (38%) NS Home 25/97 (26%) Centre 8/45 (18%) NS Home 73/97 (75%) Centre 33/45 (73%) NS Home 94/97 (97%)* Centre 45/45 (100%)* NS |
Home 19/38 Centre 18/42 P=0.52# Home 4/38 Centre 4/42 P=0.88# Home 5/38 Centre 8/42 P=0.47# Home 15/38 Centre 20/42 P=0.54# |
Home 169 (72.2%) Centre 171 (73.4%) P=0.8 Home 176 (75.2%)* Centre 161 (69.1%)* P=0.1 Home 216 (92.3%)** Centre 221 (94.8%)** P=0.3 Home 227 (97.0%)+ Centre 226 (97.0%)+ P=1.0 |
Home 161 (71.6%) Centre 164 (72.2%) P=0.9 Home 177 (78.7%)* Centre 156 (68.7%)* P=0.02 Home 195 (86.7%)** Centre 206 (90.7%)** P=0.2 Home 214 (95.1%)+ Centre 220 (96.9%)+ P=0.3 |
|||
| Comments | +number of nights *lipid lowering drugs |
*antiplatelets&anticoagulants | *GP consultations | *ACEi or AngIIRA **Cholesterol-lowering drugs +Aspirin or antiplatelet drugs |
P-value calculated by authors of the present report; NS: not statistically significant.
DISCUSSION
The mainstay approach to cardiac rehabilitation delivery in many countries is an inpatient and outpatient hospital-based provision, which often takes place in a supervised University, hospital or community setting. The availability of home-based programmes may provide an opportunity to widen access and participation to cardiac rehabilitation and thereby may improve uptake and adherence. Home-based cardiac rehabilitation may appear to be a less costly alternative for healthcare economies than more traditional hospital-based. UK figures suggest that 20% of cardiac rehabilitation programmes are currently home-based. This review assessed the randomised controlled trial evidence comparing outcomes of home- and centre-based cardiac rehabilitation.
Our systematic review found no evidence to support a difference in outcomes in cardiac patients receiving home-based or centre-based cardiac rehabilitation either in the short-term (3-12 months) or longer-term (up to 24-months). The study population in the trials were mainly male with a mean age of 51.6 to 69 years. Outcomes considered in this review included exercise capacity, modifiable risk factors (blood pressure, blood lipids and smoking), health-related quality of life, cardiac events (including mortality, revascularisations and rehospitalisations) and adherence. Although some results (diastolic blood pressure, HDL-cholesterol) seemed to have statistical significance, after excluding the most outlining study (Kassaian 2000) the statistically significant difference between groups has been lost. Although not the primary focus of this review, in accord with the two Cochrane reviews of exercise-based cardiac rehabilitation (Jolliffe 2001; Rees 2004a) we found there to be an improvement in the above following both home- and centre-based cardiac rehabilitation. Healthcare costs appear to depend on the healthcare economy in which cardiac rehabilitation provision is made. However, this review found no consistent evidence to support an important difference in healthcare costs of providing home- versus centre-based programmes.
Our findings are consistent with the previous non-Cochrane systematic review by Jolly (Jolly 2006). However, this updated review substantially increases the body of evidence base for home- versus centre-based cardiac rehabilitation, incorporating emerging evidence. Our review identified 12 randomised controlled trials in 1,938 cardiac patients, most of them performed during the last eight years, compared with the previous six trials in 749 patients. The Jolly review was critical of the variety of home-based cardiac rehabilitation interventions, the small and poor quality of trials. More recently, two relatively large and high quality UK NHS funded randomised controlled trials comparing home- and hospital-based cardiac rehabilitation have been published (Dalal 2007; Jolly 2007). The model of home-based provision in the largest three included trials (Bell 1998; Dalal 2007; Jolly 2007) was the Heart Manual, a home-based cardiac rehabilitation programme that consists of a self-help manual supported by a nurse facilitator (Lewin 1992).
Our review has limitations. The recruitment of the included trials was primarily limited to stable CHD patients either following an acute-MI or revascularisation. Only one trial was found comparing centre- and home-based cardiac rehabilitation in patients with heart failure. Although the majority of patients in this review were exposed to the Heart Manual model of home-based cardiac rehabilitation there was evidence of considerable statistically heterogeneity across a number of outcomes across trials. This heterogeneity may well reflect the variety of centre-based cardiac rehabilitation interventions. Trials were pooled using a random effects meta-analysis in the presence of statistical heterogeneity. The majority of studies were of relatively short duration, only one trial reporting outcomes at 24-months (Jolly 2007).
It has been hypothesised that patient preference may have an impact on uptake and adherence to home-based cardiac rehabilitation and there is evidence that white patients who work full- or part-time and who perceive time constraints are more likely to have a preference for home-based provision (Grace 2005). However, such a hypothesis is difficult to test in a traditional RCT designed study and therefore our finding of similar adherence between home and centre needs to be interpreted with caution. The included CHARMS study (Dalal 2007) employed a comprehensive cohort design in addition to the randomised element of home and centre allocation in which there was also a patient preference element (patients could choose between home and hospital-based cardiac rehabilitation). The authors reported outcomes to be very similar between the home and hospital preference arms for all the primary and secondary outcomes to that of the randomised comparison. Adherence to home-based cardiac rehabilitation was also comparable between the randomised (75%) and preference arms (73%). This finding does not support the hypothesis that patients who can choose a programme to suit their lifestyle and preferences will have a higher adherence rate and improved outcomes. As with the randomised comparison, the numbers in the preference arms were small (n=126).
AUTHORS’ CONCLUSIONS
Implications for practice
Trials of home- and hospital or centre-based cardiac rehabilitation have been often been poorly reported and therefore their risk of bias is difficult to ascertain. These trials were mainly conducted on males with a mean age of 52-69 years and may not be generalisable to the wider community of cardiac patients. However, cardiac rehabilitation in both settings appears to be equally effective in improving the clinical and health-related quality of life outcomes in acute MI, revascularisation and heart failure patients. This finding together with an absence of evidence of difference in healthcare costs between the two approaches would support the extension of home-based cardiac rehabilitation programmes such as the Heart Manual. The choice of participating in a more traditional supervised centre-based or home-based programme should reflect the preference of the individual patient, and may have an impact on uptake of cardiac rehabilitation in the individual case.
Implications for research
Data are needed to determine whether the effects of home- and centre-based cardiac rehabilitation reported in short-term trials can be confirmed in the longer term. Further comparative trials are needed to assess the relative impact of supervised centre- versus home-based cardiac rehabilitation in patients with heart failure and chronic angina pectoris. Such studies need to consider economic factors and patient-related outcomes including costs to the healthcare system and health-related quality of life.
PLAIN LANGUAGE SUMMARY.
Comparison of different modes of cardiac rehabilitation
Heart disease is one of the most common causes of premature death and ill health. Cardiac rehabilitation (CR) aims to restore people with heart disease to health through a combination of exercise with education and psychological support. Traditionally centre-based cardiac rehabilitation programmes (e.g. either based within a hospital, gymnasium or a sport centre setting) are offered to individuals after cardiac events, while home-based cardiac rehabilitation programmes have been introduced in an attempt to widen access and participation. The aim of this review has been to determine the effectiveness of home-based cardiac rehabilitation programmes compared with supervised centre-based cardiac rehabilitation.
The study population in the trials were mainly male with a mean age of 52-69 years. Study findings indicate that both home and hospital-based interventions are similar in their benefits on risk factors, health-related quality of life, death, clinical events and costs. There was some weak evidence to suggest that home-based interventions were associated with a higher level of adherence.
The limitations of the review are that the recruitment of the included trials was limited to stable coronary heart disease patients either following an acute-MI or revascularization, but no other cardiac populations, such as heart failure. There has been considerable diversity in the variety of centre-based and home-based cardiac rehabilitation interventions.
Related reviews, including four other Cochrane reviews, can be looked at for a fuller picture of a broader review and more conclusions about cardiac rehabilitation and the effectiveness of its specific contributant interventions and in CHD and heart failure populations.
ACKNOWLEDGEMENTS
We wish to express our thanks to Dr Philippa Davies who undertook selection of updated titles and abstracts from updated searches, Drs Dalal, Daskapan and Jolly for providing additional detials on his included trial and Sue Whiffen for her administrative assistance and the authors of the included studies who provided additional information for the purposes this review.
SOURCES OF SUPPORT
Internal sources
No sources of support supplied
External sources
NIHR Cochrane Heart Programme grant, UK.
Transparency of the National Health System Drug Reimbursement Decisions, Poland. co-financed by EU
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT parallel group | |
| Participants | n = 120 pts in Home-based CR group; n = 122 pts in Centre-based CR group; 100% post-CABG surgery; mean age 63.3 (SD 13); 81% male Inclusion: 35-49 days post-CABG, able to achieve 40-80% of age/sex-predicted METs on cycle ergometry, read/write English Exclusion: recurrent angina, positive graded exercise test, unable to attend rehabilitation 3×/week, physical limitations, previously participant ofout-patient cardiac rehabilitation |
|
| Interventions |
Home-based CR (intervention): Exercise: Total duration: 6-months; frequency: 5 sessions/wk; duration: 40 min/session; intensity: 60-70% VO2max; modality: walking. Also attended 1-hr exercise consultation with exercise specialist at baseline & after 3 month training & completed exercises log which reviewed every 2-months & telephone support call every 2 wks Other: dietary advice & psychological support Centre-based CR (control): Exercise: Total duration: 6-months; frequency: 3 sessions/wk; duration: 40 min/session; intensity: 60-70% VO2max; modality: cycle ergometer, treadmill, track walking & stair climbing. Supervised by exercise specialist & completed exercises log which reviewed every 1-month Other: dietary advice & psychological support |
|
| Outcomes |
Primary: Exercise capacity (METs) Secondary: HRQoL (SF-36); cardiac morbidity, mortality |
|
| Follow up | 6- & 18-months post randomisation | |
| Subgroup analyses | No subgroups described or reported | |
| Country & settings | Canada, single centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Low risk | “the data analyst, who had no role in this project, prepared the randomization schedule using a blocked format” “the resulting group assignments were than sealed in opaque envelopes that were opened in sequence after consent” |
| Blinding? All outcomes |
Low risk | “the physicians who evaluated the primary variables were blind to the patients assignment” |
| Incomplete outcome data addressed? All outcomes |
Low risk | CONSORT flow diagram shows loss to follow up 20/242 (92%) at 6-months follow up & 24/242 (90%) at 18-months follow up. No imputation of missing data undertaken |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | High risk | “There were statistically significant differences at baseline between the two groups in weight, resting heart rate, and social support. ” |
| Intention to treat analysis? | Low risk | “Analyses were performed based on an intention-to-treat approach.” |
| Groups received same intervention? | Low risk | “Similar numbers of patients in the Hosp and Home groups chose to consult with either clinic dietician or psychologist. ” |
| Methods | RCT parallel group | |
| Participants | n = 152 pts in Home-based CR group; n = 100 pts in Centre-based CR group; 100% acute MI; mean age 59 (SD 8.9); 77% male Inclusion: Acute MI (2 of: elevated serum creatinine kinase or oxaloacetic transamianase, prolonged chest pain consistent with AMI, new Q waves or evolutionary ST changes in ECG) Exclusion: physical infirmity, unable to speak or read English, dementia or psychosis, age >75 y, living >20 miles from CCU, serious persisting medical complications, any other excluding conditions (consultants opinion) (for some hospitals - participation in the previous rehab. programme) |
|
| Interventions |
Home-based CR (intervention) - Heart Manual: Exercise: Overall duration: 6-weeks; Frequency: not reported; Session duration: not reported; Intensity: not reported Other: 4 phone calls by facilitator, health education, stress management Centre-based CR (control): Exercise: Overall duration & frequency: 12 weeks of 1 session/wk or 4 weeks of 2 sessions/wk; Session duration: ≥20 min; Intensity: 3-4 on Borg RPE scale Other: Education sessions - CHD causes, medication, risk factor modification, stress management & exercise |
|
| Outcomes |
Primary: Exercise capacity (METs) Secondary: total cholesterol; systolic blood pressure; health-related quality of life (Nottingham Health Profile, NHP); smoking Mortality; readmission rate; use of primary care services |
|
| Follow up | 16 & 48 weeks post randomisation (20 & 52 weeks post MI) | |
| Subgroup analyses | No subgroups described or reported | |
| Country & settings | UK, 5 district hospitals | |
| Notes | Published as PhD thesis only | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Low risk | ”Series of sealed envelopes containing cards evenly distributed between conditions …envelopes were taken sequentially …opened envelopes were retained and returned to trial coordinator“ |
| Blinding? All outcomes |
Low risk | ”All measurements were performed ‘blind’by members of the medical staff and technicians“ |
| Incomplete outcome data addressed? All outcomes |
Unclear risk | Follow up data on all randomised patient is not reported. No CONSORT flow diagram is reported and it is difficult to determine from report those were loss to follow up or dropped out |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | There were no statistically significant differences in population demographics between two groups |
| Intention to treat analysis? | High risk | ”Statistical analysis followed the intention-to-treat principle …on the basis 7 subjects randomised to conventional treatment [centre-based CR] were classified as non-compliers“ and excluded from analysis |
| Groups received same intervention? | High risk | Although the intervention to both groups consisted of exercise, education and stress management, the nature and amount of intervention was quite different |
| Methods | RCT parallel group | |
| Participants | n = 38 pts in Home-based CR group; n = 42 pts in Centre-based CR group; diagnosis: coronary artery bypass, angioplasty, MI, angiographically confirmed CHD; case mix: MI, revascularisation & CHD; mean age 59 (SD 14); 83% male Inclusion: men & women 35-75yrs referred for first time to outpatient cardiac rehabilitation, living ≤30 miles from the rehab. facility, of low-to-moderate cardiac risk Exclusion: not reported |
|
| Interventions |
Home-based CR (intervention): Exercise: Overall duration: 25 weeks; Frequency: 2-5 sessions/wk; Duration: 30-40 mins/session; Intensity: 60-85% aerobic capacity; Modality: aerobic exercise. First 4 wks - 3 hospital based exercise session/week with ECG monitoring & then progressively reduce frequency of centre-based sessions Other: weekly educational & counselling meetings that included sessions on exercise, diet, risk factor, drugs and over coming barriers to behaviour change. Based on Bandura’s self-efficacy theory Centre-based CR (control): Exercise: Overall duration: 25 weeks; Frequency: 2-3 sessions/wk; Duration: 30-45 min/session; Intensity: 60-85% aerobic capacity; Modality: aerobic exercise Other: 3 sessions of education & counselling that included sessions on exercise, diet, risk factor & drugs |
|
| Outcomes |
Primary: Peak functional capacity (METs), LDL-cholesterol Secondary: Total cholesterol, HDL-cholesterol, triglycerides, blood pressure, cardiovascular medications, costs, adherence (exercise sessions attended) |
|
| Follow up | 6-months post randomisation | |
| Subgroup analyses | No subgroups described or reported | |
| Country & settings | USA, single hospital centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | “it was not possible to blind the clinicians to the protocol patients were assigned” Outcome blinding not reported |
| Incomplete outcome data addressed? All outcomes |
High risk | “significantly more TP [centre-based CR] participants dropped out” Because of more TP [centre-based CR] participants dropped out and failed to return for their 6-month [exercise test] evaluation, this evaluation is a representation of more compliant patients” |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | “…only significant difference between groups was a higher resting systolic blood pressure in the former [centre-based CR] …selected demographic and psychological measures including socioeconomic status and social support were comparable between the 2 groups at baseline” |
| Intention to treat analysis? | Low risk | The conduction of intention to treat analysis not stated directly, but results appear to be presented according to original random allocation |
| Groups received same intervention? | High risk | “Theprimary differences in the MP [home-based CR] compared with the TP [centre-based CR] included: …(2) an ongoing weekly education/support group, and (3) education and counselling that emphasized overcoming barriers associated with developing independent exercise and nutrition behaviours” Although both groups both received exercise training, education and counselling the amount and nature of this intervention was different between groups |
| Methods | RCT parallel group | |
| Participants | n = 60 pts in Home-based CR group; n = 44 pts in Centre-based CR group; 100% post-MI; mean age 62 (SD 15); 81% male Inclusion: Confirmed acute myocardial infarction (WHO criteria), ability to read English, registered with GP in one of two primary care trusts Exclusion: Severe heart failure, unstable angina, uncontrolled arrhythmia, history of major psychiatric illness, other significant co-morbidity precluding the ability to exercise on the treadmill, patients readmitted with acute myocardial infarction who had already received an intervention earlier in the study |
|
| Interventions |
Home-based CR (intervention) - Heart Manual: Exercise: Overall duration: 6-wks; frequency: not reported; duration: not reported; intensity: not reported; Modality: walking. Home visit in 1st week after discharge by CR nurse followed up by up to 4 telephone calls at 2, 3, 4, & 6 wks Other: Stress management & education Centre-based CR (control): Exercise: Overall duration: 8-10 wks; frequency: 1-5 sessions/wk; Duration: not reported; Modality: not reported. Superivsed and group based Other: Input from dietician, psychologist, occupational therapist & pharmacist |
|
| Outcomes |
Primary: Quality of life (MacNew questionnaire), total cholesterol Secondary: exercise capacity (METs), self-reported smoking Cardiovascular morbidity, mortality, secondary prevention medication use |
|
| Follow up | 9-months post randomisation | |
| Subgroup analyses | No subgroup analyses described or reported | |
| Country & settings | UK, single centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Low risk | “computerised random number trial allocation sequence was determined before the study” |
| Allocation concealment? | Low risk | “allocation was transferred to sequentially numbered, opaque, sealed envelopes and concealed from the research nurse, who carried out baseline assessment” |
| Blinding? All outcomes |
Low risk | “the person assessing the primary outcome questionnaires was blinded to allocation” |
| Incomplete outcome data addressed? All outcomes |
Low risk | “the last known observation carried forward to replace missing values at 9 months for the primary outcome measures. ” |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | “The randomized groups were well balanced, apart from a higher proportion of patients in employment in the home based group (51% versus 26%, p=0.013)” |
| Intention to treat analysis? | Low risk | “Data were analyzed on an intention to treat principle” |
| Groups received same intervention? | Low risk | |
| Methods | RCT parallel group | |
| Participants | n = 15 patients in Home-based CR group; n = 14 pts in Centre-based CR group; diagnosis: heart failure; case mix: CHF class II or III NYHA with ischemic or idiopathic dilated cardiomyopathy; mean age 52 (SD 8.5); 76% male Inclusion: heart failure of >3 month duration Exclusion: valvular heart disease, exercise-induced cardiac arrhythmias, symptomatic myocardial ischemia within 3 months, taking beta-blockers |
|
| Interventions |
Home-based CR (intervention): Exercise: Total duration: 12 weeks; frequency: 3 sessions/wk; duration: 45 mins/session (including warm-up, cool-down, recovery); intensity: up to 60% peak heart rate (RPE 1216); modality: walking; follow-up logs completed daily/returned biweekly. Weekly phone calls from staff monitoring adherence & progress, monthly phone calls from patients for control purposes Other: not reported Centre-based CR (control): Exercise: Total duration: 12 weeks; frequency: 3 sessions/wk; duration: 45 mins/session (including warm-up, cool-down, recovery); intensity: 60% peak heart rate; modality: walking on a treadmill. Supervised Other: not reported |
|
| Outcomes | (primary and secondary outcomes not distinguished) exercise capacity (ml/kg/min), resting BP systolic & diastolic BP, adherence, dropouts; additionally data on mortality obtained by personal contact | |
| Follow up | 12 weeks post randomisation | |
| Subgroup analyses | No subgroups described or reported | |
| Country & settings | Turkey, single centre | |
| Notes | Additional data on mortality obtained by personal contact | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | “Among patients who completed the study, no differences in demographic characteristics were seen between the 2 study groups after randomization (p>0.05). ” |
| Intention to treat analysis? | High risk | ITT not reported |
| Groups received same intervention? | Low risk | “We chose lower intensity …training prescriptions in the HETG to avoid any adverse occurrences and also in the SETG to provide comparable training intensity levels between 2 groups. ” |
| Methods | RCT parallel group | |
| Participants | n = 54 pts in physician-supervised Home-based CR group; n = 49 pts in community Home-based CR group; n = 52 pts in Centre-based CR group; diagnosis: 100% CAD (MI and/or CABG and/or PTCA and/or chronic stable angina); age: 60.4 (SD 9.4); 75% male Inclusion: diagnosed CAD (as above); low-moderate risk of cardiac events (1. no cardiac arrest within 1 year, 2. no complex ventricular dysrhythmia, 3. ejection fraction <40%. 4. no complicated MI or cardiac surgery, 5. no increasing systolic BP response to exercise testing, 6. no angina pectoris <5.0 METs); ≥4 weeks posthospitalization; age 21-75 y; no life-threatening illness and/or psychological abnormality; speak/write English; ability to complete exercise treadmill test; ability to attend 36 cardiac rehabilitation sessions Exclusion: not defined |
|
| Interventions |
Home-based CR
Group I (Supervised Home-based CR) Exercise: Total duration: 12 weeks; frequency & intensity: individually prescribed(30-60 min of aerobic exe, 60-85% peak HR), gradually updated; appointments: 2 office visits, 4 phone calls Other: written materials, audiotapes, nutrition, weight & stress management, smoking cessation programme, individual CAD risk factors management Group II (Community Home-based CR) Exercise: Total Duration: 12 weeks; frequency & intensity: individually prescribed (30-60 min of aerobic exe, 60-85% peak HR), gradually updated; appointments: 12 on site visits or telephone calls (patient choice) Other: written materials, audiotapes, nutrition, weight & stress management, smoking cessation programme, individual CAD risk factors management Centre-based CR Exercise: Total Duration: 12 weeks; frequency: 3 sessions/wk (total of 36 sessions = appointments); intensity: individually prescribed(30-60 min of aerobic exe, 60-85% peak HR); continuous ECG telemetry during exercise Other: written materials, audiotapes, education on CAD risk factors & lifestyle modification |
|
| Outcomes | (primary & secondary risk factors not distinguished) maximal oxygen uptake, blood pressure, fasting serum lipids, self-reported smoking status, rehospitalization, adherence (completion of appointments) | |
| Follow up | 12 weeks post randomisation | |
| Subgroup analyses | Changes reported for all patients and for patients with baseline values defined as abnormal | |
| Country & settings | USA single centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | Data for 142 pts who completed exercise testing at baseline and at follow up (not all 155 pts randomised) reported only; numbers of dropouts reported and reasons described |
| Free of selective reporting? | Low risk | All outcomes mentioned in methods are reported in results |
| Groups balanced at baseline? | Low risk | “Randomization did not result in statistical significant differences among patients assigned to the3 interventions. ” |
| Intention to treat analysis? | Unclear risk | Not reported |
| Groups received same intervention? | Low risk | |
| Methods | see Gordon2002-Commun | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Follow up | ||
| Subgroup analyses | ||
| Country & settings | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | Data for 142 pts who completed exercise testing at baseline and at follow up (not all 155 pts randomised) reported only; numbers of dropouts reported and reasons described |
| Free of selective reporting? | Low risk | All outcomes mentioned in methods are reported in results |
| Groups balanced at baseline? | Low risk | “Randomization did not result in statistical significant differences among patients assigned to the3 interventions. ” |
| Intention to treat analysis? | Unclear risk | Not reported |
| Groups received same intervention? | Low risk | |
| Methods | RCT parallel group | |
| Participants | n = 263 pts in Home-based CR group; n = 262 pts in Centre-based CR group; diagnosis: MI 256 pts; PTCA 211 pts; CABG 56 pts; mean age 61 (SD 10.8); 77% male; 80.2% white Inclusion: an acute MI, coronary angioplasty (±stenting) or CABG Exclusion: inability to speak either English or Punjabi, dementia, severe hearing impairment, sight defects of sufficient severity to prevent them from reading the Heart Manual & serious persisting complications |
|
| Interventions |
Home-based CR (intervention) - Heart Manual: Exercise: Overall duration: 6 wks Heart Manual programme & 12 wks nurse support; frequency: up to daily; Duration: not reported; intensity: not reported; modality: walking Other: education on risk factors, lifestyle changes, medications & stress management (relaxation tapes) Centre-based CR (control): Exercise: Total Duration: 6-12 wks; Frequency: 1 or 2 sessions/wk; duration:25-30mins/session; intensity: 65-75% HRmax; modality: circuit training, cycle ergometer Other: education & stress management (relaxation) |
|
| Outcomes |
Primary: Serum cholesterol, total, HDL-cholesterol, blood pressure, exercise capacity (incremental shuttle walking test, ISWT), smoking cotinine-validated) Secondary: quality of life (EQ-5D), health service utilisation (hospital readmissions, primary care visits, medication) Mortality, cardiovascular events, costs |
|
| Follow up | 6, 12 & 24 months | |
| Subgroup analyses | Yes. “Interaction terms between these factors [diagnosis (MI/revascularisation), age, sex and ethnicity] and rehabilitation setting were included to investigate possible differences in treatment effect between subgroups of patients. ” | |
| Country & settings | UK, 4 hospital centres | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Low risk | “Patients who consented to randomisation were randomised on an individual basis with minimisation by (1) original diagnosis (MI/revascularisation), (2) age (<50/50-74/75+ years), (3) sex, (4) ethnicity (Caucasian/Asian/other) and (5) hospital of recruitment. ” |
| Allocation concealment? | Low risk | “Allocation was undertaken by the Birmingham Cancer Clinical Trials Unit, a group that was independent from the trial team …When a patient agreed to be randomised, …the research nurse telephoned the Clinical Trials Unit, …and was given an allocation group. ” |
| Blinding? All outcomes |
Low risk | “Assessments were blinded, with follow-up undertaken by a research nurse who had neither recruited the patient nor provided home CR support.” |
| Incomplete outcome data addressed? All outcomes |
Low risk | “A sensitivity analysis was undertaken on the 12-month data to assess the potential impact of the missing values for the ISWT, SBP, DBP, TC and the HADS scores. ” |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | “Demographic characteristics, diagnosis, past medical history and cardiac risk factors were well matched between the two arms at baseline.” |
| Intention to treat analysis? | Low risk | “All data were analysed by intention-to-treat (ITT). ” |
| Groups received same intervention? | High risk | Although both groups received exercise, education and stress management, the nature and amount of intervention between groups was different |
| Methods | RCT parallel group | |
| Participants | n = 65 pts in Centre-based CR group (active intervention); n = 60 pts in Home-based CR group (controls); diagnosis: MI 23.2%; CABG 76.8%; case mix: MI: Hosp 32.3%, Home 13.3%; CABG: Hosp 67.7%, Home 86.7%; mean age 55 (SD 9.5); 100% male Inclusion: AMI or CABG in last 1-2 month, NYHA<IV, EF≥30%, able to exercise on a treadmill & participate in exercise programme Exclusion: high-risk stress test, decompensated CHF (NYHA IV), unstable angina, uncontrolled AF, high-grade AV block (grade 2 or 3), active pericarditis or myocarditis, recent pulmonary thromboembolism, exercise-induced asthma, claudication, fixed-rate permanent pacemaker, severe medical problem |
|
| Interventions |
Centre-based CR (intervention): Exercise: Total duration: 12 weeks; frequency: 3 sessions/wk; duration: 20-30 min+10 min warm-up+10 min cool-down/session; intensity: 60-85% (not reported if relative to HRmax or V02max); modality: treadmill Other: not reported Home-based CR (control): Exercise: Total duration: 12 weeks; ; frequency: not reported; duration: not reported; intensity: “intensity based on exercise test results” Other: patients have been taught to count their pulse rate |
|
| Outcomes | (primary and secondary outcomes not distinguished) systolic BP, diastolic BP, heart rate (all resting & sub-maximal), functional capacity (METs), BMI, cholesterol: total, LDL, HDL, triglyceride | |
| Follow up | 12 weeks post randomization | |
| Subgroup analyses | Subgroup analysis: comparison of functional capacity, sub-maximal SBP, DBP & heart rate in pts with left ventricular dysfunction vs good LV function | |
| Country & settings | Iran, single centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Unclear risk | No information on loss to follow up, nor on missing data management |
| Free of selective reporting? | Unclear risk | Not all outcomes reported mentioned in methods section |
| Groups balanced at baseline? | Low risk | “Among patients who completed the study no differences in demographic characteristics were seen between the two study groups after randomisation. ” |
| Intention to treat analysis? | Unclear risk | Not reported |
| Groups received same intervention? | Unclear risk | Details of home-based intervention not reported |
| Methods | RCT parallel group | |
| Participants | n = 90 pts in Home-based CR group; n = 90 pts in Centre-based CR group; 100% MI; mean age 69 (SD 1.6); 71% male Inclusion: age >45 y, MI Exclusion: Severe cognitive impairment; physical disability; left ventricular ejection fraction <35%; contraindications to vigorous exercise; eligibility for myocardial revascularisation, living too far from CR unit |
|
| Interventions |
Home-based CR (intervention): Exercise: Overall duration; 8-wks; Frequency: 3 days/wk; Duration: 1-hour; Intensity 7085% peak HR; Modality: cycle ergometer. Physical therapist home visits every other week Other: monthly family-oriented support groups Centre-based CR (control): Exercise: Overall duration; 12-week programme; Frequency: 3 days/wk; Duration: not reported; Intensity 70-85% peak HR; Modality: cycle ergometer. Trans-telephonic ECG monitoring during exercise Other: risk factor management counselling; support group meetings |
|
| Outcomes |
Primary: Total work capacity (TWC) Secondary: Health-related quality of life (Sickness Impact Profile, SIP), mortality, morbidity (cardiovascular events), healthcare utilisation (medical visits, rehospitalisations), costs & adherence (number of completed training sessions) |
|
| Follow up | 2, 8 & 14 months post randomisation | |
| Subgroup analyses | Subgroup analysis in age groups (middle-aged 45-65 years, old 65-75 years, very old >75 years) | |
| Country & settings | Italy, single hospital centre | |
| Notes | Data presented separately for 3 age groups. Follow up data on charts only; authors contacted for numerical data at follow up & these have been supplied for TWC & SIP separately for 3 groups; data pooled across age groups by reviewers | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Low risk | “Testing personnel were blinded to patient assignment.” |
| Incomplete outcome data addressed? All outcomes |
Low risk | “we performed a sensitivity analysis comparing results obtained with and without replacement of missing data with data obtained with the expectation-maximization imputation method. Because the 2 analyses provided similar results, which were also similar with missing data substituted with data estimated in a worst-case scenario, only the data from patients who completed the study are presented |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | “baseline sociodemographic and clinical characteristics were similar across the 3 arms of the trial” Baseline characteristics by home and hospital group allocation not reported in tabular format |
| Intention to treat analysis? | Low risk | Although term ‘intention to treat analysis’ was not stated directly, on the basis of CONSORT diagram presented, the groups did appear to be analysed according to original random allocation |
| Groups received same intervention? | Low risk | |
| Methods | RCT parallel group | |
| Participants | n = 66 patients in Home-based CR group (33 in brief exercise programme subgroup & 33 inextended subgroup); n = 61 patients in Centre-based CR group (31 in brief subgroup & 30 in extended subgroup); 100% uncomplicated acute MI; mean age 52 (SD 9); 100% male Inclusion: Uncomplicated AMI (elevated serum creatinine kinase or oxaloacetic transamianase, prolonged chest pain consistent with AMI, new Q waves or evolutionary ST changes in ECG) Exclusion: Unable to undertake exercise test, congestive heart failure, unstable angina pectoris, valvular heart disease, atrial fibrillation, bundle branch block, history of bypass, stroke, orthopaedic abnormalities, peripheral vascular disease, chronic pulmonary obstructive disease, obesity |
|
| Interventions |
Home-based CR (intervention): Exercise: Overall duration: 8 wks (brief) or 23 wks (extended), Frequency: 5 sessions/wk; Duration: 30 mins/session; Intensity: 70-85% HRmax; modality: stationary cycling. Portable heart rate monitors & teletransmissions of ECG; 2 phone calls/wk by staff to verify training intensity, clinical status and medication Other: No education or psychological intervention reported Centre-based CR (control): Exercise: Overall duration: 8 wks (brief) or 23 wks (extended), Frequency: 5 sessions/wk; Duration: 60 mins/session; intensity: 70-85% HRmax; modality: walking/jogging. Group based & supervised Other: No education or psychological intervention reported |
|
| Outcomes | Exercise capacity; mortality & cardiovascular morbidity | |
| Follow up | 23 weeks post randomisation | |
| Subgroup analyses | Yes. Results reported according to the two subgroups reported i.e. brief vs extended exercise training | |
| Country & settings | USA, single hospital centre | |
| Notes | Results of two subgroups included into analysis separately | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | Drop out reported. No imputation of missing data discussed. Effect of incomplete outcome data likely to be small |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Unclear risk | Baseline characteristics not reported |
| Intention to treat analysis? | Low risk | Term ‘intention to treat analysis’ not stated directly, but results appear to be presented according to original random allocation. This is further supported by a trial flow diagram in the paper |
| Groups received same intervention? | Low risk | Both home and centre groups were very closely balanced in terms of the exercise training received |
| Methods | see Miller 1984 Brief | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Follow up | ||
| Subgroup analyses | ||
| Country & settings | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | Drop out reported. No imputation of missing data discussed. Effect of incomplete outcome data likely to be small |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Unclear risk | Baseline characteristics not reported |
| Intention to treat analysis? | Low risk | Term ‘intention to treat analysis’ not stated directly, but results appear to be presented according to original random allocation. This is further supported by a trial flow diagram in the paper |
| Groups received same intervention? | Low risk | Both home and centre groups were very closely balanced in terms of the exercise training received |
| Methods | RCT parallel groups | |
| Participants | n = 10 pts in Home-based CR group; n = 10 pts in Centre-based CR group; diagnosis: MI, CABG, PTCA; case mix: MI & revascularisation; mean age 51.6 (SD 12); 100% male Inclusion: being male cardiac patient Exclusion: not capable for exercising on a bicycle ergometer, serious arrhythmias, symptoms of frequent chest pain, shortness of breath, hypertension |
|
| Interventions |
Home-based CR (intervention): Exercise: Overall duration; 12-week programme; Frequency: 3 days/wk; Duration: 1hour; Intensity 60-75% peak HR; Modality: cycle ergometer. Trans-telephonic ECG monitoring Other: Education materials on diet, medications, risks and benefits of the exercise Centre-based CR (control): As above but no trans-telephonic ECG monitoring during exercise |
|
| Outcomes | Exercise capacity (peak VO2max); adherence (compliance with exercise); safety (drop out) | |
| Follow up | 12 weeks post randomisation | |
| Subgroup analyses | No subgroups described or reported | |
| Country & settings | USA, single hospital centre | |
| Notes | Data read from graphs | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes |
Low risk | Only 1/20 (5%) drop out reported |
| Free of selective reporting? | Low risk | All outcomes described in the methods section are reported in the results |
| Groups balanced at baseline? | Low risk | Although no statement of similarity of baseline characteristics, the characteristic of both groups in table 1 appeared similar |
| Intention to treat analysis? | Low risk | The conduction of intention to treat analysis not stated directly, but results appear to be presented according to original random allocation |
| Groups received same intervention? | Low risk | |
| Methods | RCT parallel group | |
| Participants | n = 18 pts in Home-based CR group; n = 18 pts in Centre-based CR group; 100% post CABG; mean age 61.9 (SD 7.3); 100% male Inclusion: No pervious CABG, no neurologic impairment like stroke/brain injury, no severe musculoskeletal disease, no complications during hospitalisations like infection, shock, arrhythmia, prolonged ventilation Exclusion: uncontrolled dysrhythmia or continuous ventricular tachycardia during exercise testing, no possibility of completing test at discharge or 12 wks later |
|
| Interventions |
Home-based CR (intervention): Exercise: Total duration: 12 weeks; frequency: ≥3 sessions/wk; duration: 30-60 min+10 min warm-up+10 min cool-down/session; intensity: 60-85% HRmax; modality: fast walking or jogging. Exercise documented in record book. Prescription of exercise individually given &updated every 2 wks by rehabilitation nurse Other: not reported Centre-based CR (control): Exercise: Total duration: 12 weeks; frequency: 3 sessions/wk (total 36 sessions); duration: 30-60 min+10 min warm-up+10 min cool-down/session; intensity: 60-85% HRmax; modality: cycle ergometer, treadmill. Exercise supervised by cardiopulmonary physical therapist Other: not reported |
|
| Outcomes | (primary and secondary outcomes not distinguished) exercise capacity (METs) | |
| Follow up | 12 weeks post randomisation | |
| Subgroup analyses | No subgroups described or reported | |
| Country &settings | Taiwan (China), single centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | “Subjects were randomly assigned by drawing lots ” |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes |
Low risk | “ The evaluators of the exercise stress test were also masked to the group assignments.” |
| Incomplete outcome data addressed? All outcomes |
Unclear risk | Not reported |
| Free of selective reporting? | Low risk | All outcomes described in methods section were reported in results |
| Groups balanced at baseline? | Low risk | “Randomization did not result in statistical significances among subjects assigned to the three groups. ” |
| Intention to treat analysis? | Unclear risk | Not reported, although it appears that patients were analysed according to original allocation |
| Groups received same intervention? | Low risk | |
AMI=acute myocardial infarction
CABG=coronary artery bypass graft
CAD=coronary artery disease
CCU=coronary care unit
CHD=coronary heart disease
CHF=congestive heart failure
CR=cardiac rehabilitation
ECG=electrocardiogram
HRQoL=health related quality of life
ISWT=incremental shuttle walking test
ITT=intention to treat
METs=metabolic equivalents
MI=myocardial infarction
NYHA=New York Heart Association classification
PTCA=percutaneous transluminal coronary angioplasty
RCT=randomised controlled trial
SD=standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ades 2000 | Non RCT |
| Senuzun 2006 | Trial experimental arm received home-based cardiac rehabilitation; the programme issued in control arm was not described |
| Sinclair 2005 | Trial experimental arm received home-based cardiac rehabilitation, while the control group did not receive centre based CR (only 6% [n=12] of the participants in the control group were referred to CR and only 3% [n=8] were known to have attended) |
| Tygesen 2001 | Both trial arms received home-based cardiac rehabilitation |
DATA AND ANALYSES
Comparison 1. Exercise capacity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Exercise capacity 3-12 month | 14 | 1557 | Std. Mean Difference (IV, Random, 95% CI) | −0.11 [−0.35, 0.13] |
| 2 Exercise capacity 12-24 month | 3 | 1074 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [−0.01, 0.23] |
Comparison 2. Blood Pressure [mm Hg].
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Systolic BP 3-12 month | 8 | 1053 | Mean Difference (IV, Random, 95% CI) | 0.58 [−3.29, 4.44] |
| 2 Diastolic BP 3-12 month | 7 | 927 | Mean Difference (IV, Fixed, 95% CI) | −1.85 [−2.96, −0.74] |
Comparison 3. Blood lipids [mmol/l].
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total cholesterol 3-12 month | 7 | 1019 | Mean Difference (IV, Random, 95% CI) | −0.13 [−0.31, 0.05] |
| 2 HDL cholesterol 3-12 month | 5 | 793 | Mean Difference (IV, Fixed, 95% CI) | −0.06 [−0.11, −0.02] |
| 3 LDL-cholesterol 3-12 month | 4 | 324 | Mean Difference (IV, Fixed, 95% CI) | −0.15 [−0.31, 0.01] |
| 4 Triglycerides 3-12 month | 4 | 328 | Mean Difference (IV, Random, 95% CI) | −0.15 [−0.41, 0.11] |
Comparison 4. Smoking.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Smoking 3-12 month | 5 | 922 | Risk Ratio (M-H, Random, 95% CI) | 1.00 [0.71, 1.41] |
Comparison 5. Mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 4 | 909 | Risk Ratio (M-H, Fixed, 95% CI) | 1.31 [0.65, 2.66] |
Comparison 6. Completers.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completers | 13 | 1620 | Risk Ratio (M-H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
Analysis 1.1. Comparison 1 Exercise capacity, Outcome 1 Exercise capacity 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 1 Exercise capacity
Outcome: 1 Exercise capacity 3-12 month
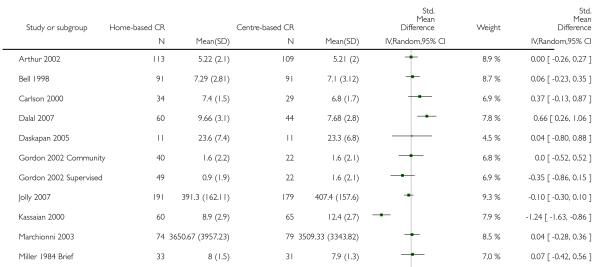
|
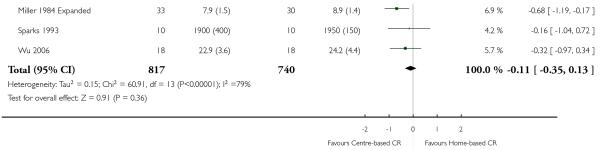
|
Analysis 1.2. Comparison 1 Exercise capacity, Outcome 2 Exercise capacity 12-24 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 1 Exercise capacity
Outcome: 2 Exercise capacity 12-24 month
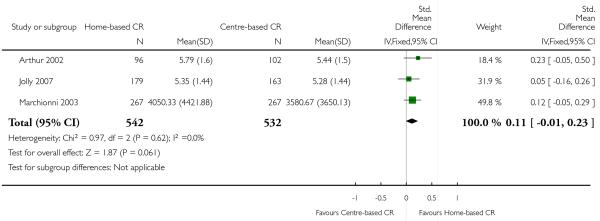
|
Analysis 2.1. Comparison 2 Blood Pressure [mm Hg], Outcome 1 Systolic BP 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 2 Blood Pressure [mm Hg]
Outcome: 1 Systolic BP 3-12 month
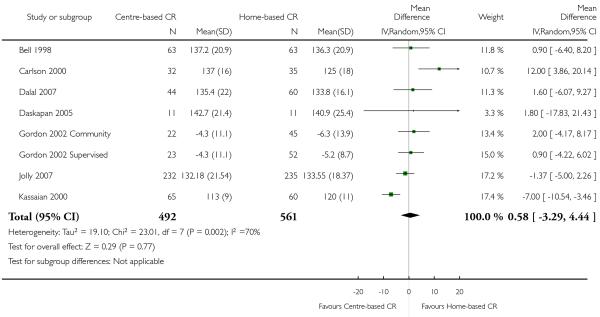
|
Analysis 2.2. Comparison 2 Blood Pressure [mm Hg], Outcome 2 Diastolic BP 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 2 Blood Pressure [mm Hg]
Outcome: 2 Diastolic BP 3-12 month
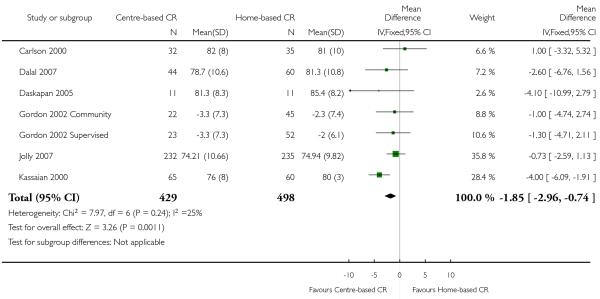
|
Analysis 3.1. Comparison 3 Blood lipids [mmol/l], Outcome 1 Total cholesterol 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 3 Blood lipids [mmol/l]
Outcome: 1 Total cholesterol 3-12 month
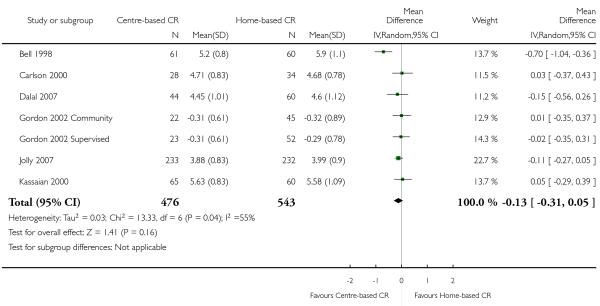
|
Analysis 3.2. Comparison 3 Blood lipids [mmol/l], Outcome 2 HDL cholesterol 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 3 Blood lipids [mmol/l]
Outcome: 2 HDL cholesterol 3-12 month
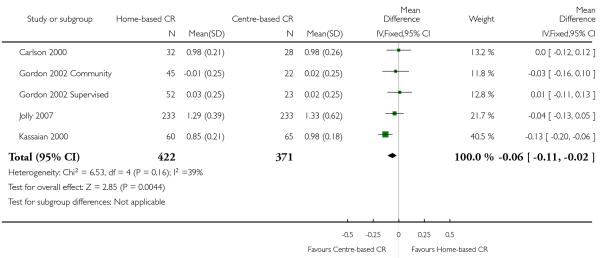
|
Analysis 3.3. Comparison 3 Blood lipids [mmol/l], Outcome 3 LDL-cholesterol 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 3 Blood lipids [mmol/l]
Outcome: 3 LDL-cholesterol 3-12 month
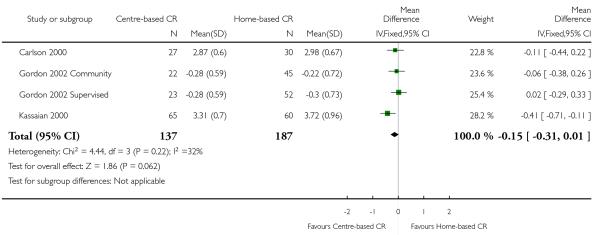
|
Analysis 3.4. Comparison 3 Blood lipids [mmol/l], Outcome 4 Triglycerides 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 3 Blood lipids [mmol/l]
Outcome: 4 Triglycerides 3-12 month
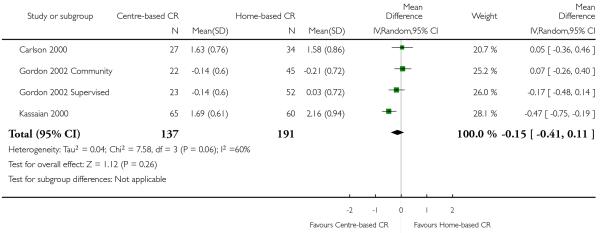
|
Analysis 4.1. Comparison 4 Smoking, Outcome 1 Smoking 3-12 month.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 4 Smoking
Outcome: 1 Smoking 3-12 month
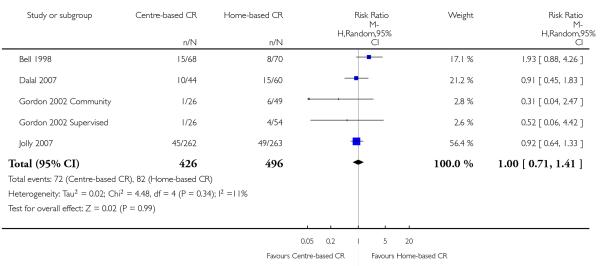
|
Analysis 5.1. Comparison 5 Mortality, Outcome 1 Mortality.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 5 Mortality
Outcome: 1 Mortality
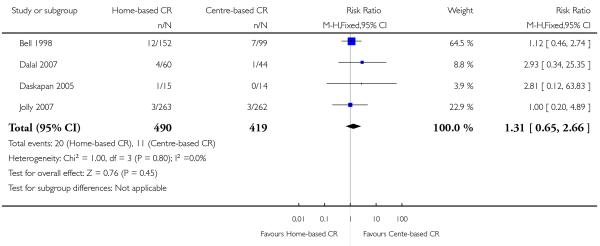
|
Analysis 6.1. Comparison 6 Completers, Outcome 1 Completers.
Review: Home-based versus centre-based cardiac rehabilitation
Comparison: 6 Completers
Outcome: 1 Completers
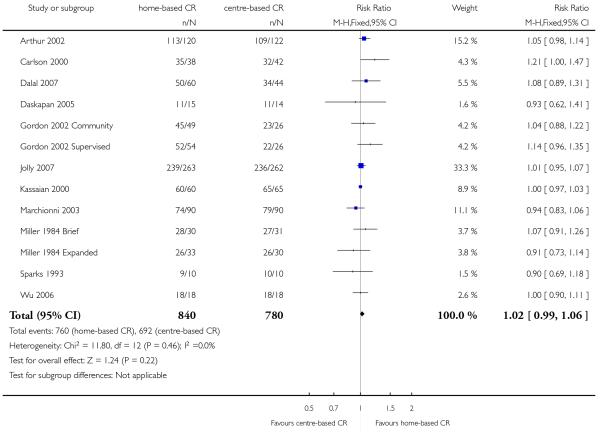
|
Appendix 1. Search strategies
CENTRAL on The Cochrane LIbrary 2007, Issue 4
#1MeSH descriptor Myocardial Ischemia explode all trees
#2(myocard* NEAR isch*mi*)
#3isch*mi* NEAR heart
#4MeSH descriptor Coronary Artery Bypass explode all trees
#5coronary
#6MeSH descriptor Coronary Disease explode all trees
#7MeSH descriptor Myocardial Revascularization explode all trees
#8MeSH descriptor Myocardial Infarction explode all trees
#9myocard* NEAR infarct*
#10heart NEAR infarct*
#11MeSH descriptor Angina Pectoris explode all trees
#12angina
#13MeSH descriptor Heart Failure, Congestive explode all trees
#14heart and (failure or attack)
#15MeSH descriptor Heart Diseases explode all trees
#16heart and disease*
#17myocard*
#18cardiac*
#19CABG
#20PTCA
#21stent* AND (heart or cardiac*)
#22MeSH descriptor Heart Bypass, Left explode all trees
#23MeSH descriptor Heart Bypass, Right explode all trees
#24(#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23)
#25MeSH descriptor Rehabilitation Centers, this term only
#26MeSH descriptor Exercise Therapy explode all trees
#27MeSH descriptor Sports, this term only
#28MeSH descriptor Exertion explode all trees
#29rehabilitat*
#30(physical* NEAR (fit* or train* or therap* or activit*))
#31MeSH descriptor Exercise explode all trees
#32(train*) near (strength* or aerobic or exercise*)
#33((exercise* or fitness) NEAR/3 (treatment or intervent* or program*))
#34MeSH descriptor Rehabilitation explode all trees
#35MeSH descriptor Patient Education explode all trees
#36(patient* NEAR/3 educat*)
#37((lifestyle or life-style) NEAR/3 (intervent* or program* or treatment*))
#38MeSH descriptor Self Care explode all trees
#39MeSH descriptor Ambulatory Care explode all trees
#40MeSH descriptor Psychotherapy explode all trees
#41psychotherap*
#42psycholog* NEAR intervent*
#43relax*
#44MeSH descriptor Mind-Body and Relaxation Techniques explode all trees
#45MeSH descriptor Counseling explode all trees
#46counsel*ing
#47MeSH descriptor Cognitive Therapy explode all trees
#48MeSH descriptor Behavior Therapy explode all trees
#49(behavio*r*) NEAR/4 (modif* or therap* or rehab* or change)
#50MeSH descriptor Stress, Psychological explode all trees
#51stress NEAR manage*
#52cognitive* NEAR therap*
#53MeSH descriptor Meditation explode all trees
#54meditat*
#55MeSH descriptor Anxiety, this term only
#56(manage*) NEAR (anxiety or depres*)
#57CBT
#58hypnotherap*
#59goal NEAR/3 setting
#60(psycho-educat*) or (psychoeducat*)
#61motivat* NEAR interv*
#62MeSH descriptor Psychopathology explode all trees
#63psychopathol*
#64MeSH descriptor Autogenic Training explode all trees
#65autogenic*
#66self near (manage* or care or motivat*)
#67distress*
#68psychosocial* or psycho-social
#69MeSH descriptor Health Education explode all trees
#70(nutrition or diet or health) NEAR education
#71heart manual
#72(#25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37)
#73(#38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71)
#74(#72 OR #73)
#75(#74 AND #24)
MEDLINE DIALOG 1950-WEEK 1 2008
SEARCH: MYOCARDIAL-ISCHEMIA#.DE.
SEARCH: MYOCARD$4 NEAR (ISCHAEMI$2 OR ISCHEMI$2)
SEARCH: (ISCHAEMI$2 OR ISCHEMI$2) NEAR HEART
SEARCH: CORONARY-ARTERY-BYPASS#.DE.
SEARCH: CORONARY.TI,AB.
SEARCH: CORONARY-DISEASE#.DE.
SEARCH: MYOCARDIAL-REVASCULARIZATION#.DE.
SEARCH: MYOCARDIAL-INFARCTION#.DE.
SEARCH: MYOCARD$5 NEAR INFARCT$5
SEARCH: HEART NEAR INFARCT$5
SEARCH: ANGINA-PECTORIS#.DE.
SEARCH: ANGINA.TI,AB.
SEARCH: HEART-FAILURE-CONGESTIVE#.DE.
SEARCH: HEART NEAR FAILURE
SEARCH: 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
SEARCH: HEART-DISEASES#.DE.
SEARCH: (HEART NEAR DISEASE$2).TI,AB.
SEARCH: MYOCARD$5.TI,AB.
SEARCH: CARDIAC$2.TI,AB.
SEARCH: CABG
SEARCH: PTCA
SEARCH: STENT$4 AND (HEART OR CARDIAC$4)
SEARCH: HEART-BYPASS-LEFT#.DE. OR HEART-BYPASS-RIGHT#.DE.
SEARCH: 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23
SEARCH: REHABILITATION-CENTERS.DE.
SEARCH: EXERCISE-THERAPY#.DE.
SEARCH: REHABILITATION.W..DE.
SEARCH: SPORTS#.W..DE.
SEARCH: EXERTION#.W..DE.
SEARCH: EXERCISE#.W..DE.
SEARCH: REHABILITAT$5.TI,AB.
SEARCH: PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$5 OR THERAP$5 OR ACTIVIT$5)
SEARCH: TRAIN$5 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)
SEARCH: (EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)
SEARCH: PATIENT-EDUCATION#.DE.
SEARCH: PATIENT$2 NEAR EDUCAT$4
SEARCH: (LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)
SEARCH: SELF-CARE.DE.
SEARCH: SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)
SEARCH: AMBULATORY-CARE.DE.
SEARCH: PSYCHOTHERAPY#.W..DE.
SEARCH: PSYCHOTHERAP$2.TI,AB.
SEARCH: PSYCHOLOG$5 NEAR INTERVENT$5
SEARCH: RELAX$6.TI,AB.
SEARCH: RELAXATION-TECHNIQUES#.DE. OR MIND-BODY-AND-RELAXATION-TECHNIQUES#.DE.
SEARCH: COUNSELING#.W..DE.
SEARCH: (COUNSELLING OR COUNSELING).TI,AB.
SEARCH: COGNITIVE-THERAPY#.DE.
SEARCH: BEHAVIOR-THERAPY#.DE.
SEARCH: (BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAP$2 OR CHANGE)
SEARCH: STRESS-PSYCHOLOGICAL#.DE.
SEARCH: STRESS NEAR MANAGEMENT
SEARCH: COGNITIVE NEAR THERAP$2
SEARCH: MEDITAT$4
SEARCH: MEDITATION#.W..DE.
SEARCH: ANXIETY#.W..DE.
SEARCH: MANAGE$5 NEAR (ANXIETY OR DEPRES$5)
SEARCH: CBT.TI,AB.
SEARCH: HYPNOTHERAP$5
SEARCH: GOAL NEAR SETTING
SEARCH: GOAL$2 NEAR SETTING
SEARCH: PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
SEARCH: MOTIVAT$5 NEAR (INTERVENTION OR INTERV$3)
SEARCH: PSYCHOPATHOLOGY#.W..DE.
SEARCH: PSYCHOPATHOL$4.TI,AB.
SEARCH: PSYCHOSOCIAL$4.TI,AB.
SEARCH: DISTRESS$4.TI,AB.
SEARCH: HEALTH-EDUCATION#.DE.
SEARCH: HEALTH NEAR EDUCATION
SEARCH: HEART ADJ MANUAL
SEARCH: AUTOGENIC-TRAINING#.DE.
SEARCH: AUTOGENIC$5.TI.AB.
SEARCH: 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38
SEARCH: 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71 OR 72
SEARCH: 15 OR 24
SEARCH: 73 or 74
SEARCH: 75 AND 76
SEARCH: RANDOMIZED-CONTROLLED-TRIALS#.DE.
SEARCH: PT=RANDOMIZED-CONTROLLED-TRIAL
SEARCH: PT=CONTROLLED-CLINICAL-TRIAL
SEARCH: CONTROLLED-CLINICAL-TRIALS#.DE.
SEARCH: RANDOM-ALLOCATION#.DE.
SEARCH: DOUBLE-BLIND-METHOD#.DE.
SEARCH: SINGLE-BLIND-METHOD#.DE.
SEARCH: (RANDOM$ OR PLACEBO$).TI,AB.
SEARCH: ((SINGL$3 OR DOUBL$3 OR TRIPL$3 OR TREBL$3) NEAR (BLIND$3 OR MASK$3)).TI,AB.
SEARCH: RESEARCH-DESIGN#.DE.
SEARCH: PT=CLINICAL-TRIAL#
SEARCH: CLINICAL-TRIALS#.DE.
SEARCH: (CLINIC$3 ADJ TRIAL$2).TI,AB.
SEARCH: 77 AND 90
SEARCH: (ANIMALS NOT HUMANS).SH.
SEARCH: 91 NOT 92
SEARCH: LIMIT 93 TO 2001-DATE
EMBASE DIALOG 1980-WEEK 1 2008
HEART-DISEASE#.DE.
(MYOCARD$4 NEAR (ISCHAEMI$2 OR ISCHEMI$2)).TI,AB.
((ISCHAEMI$2 OR ISCHEMI$2) NEAR HEART).TI,AB.
CORONARY-ARTERY-DISEASE#.DE.
TRANSLUMINAL-CORONARY-ANGIOPLASTY#.DE.
(CORONARY NEAR (DISEASE$2 OR BYPASS$2 OR THROMBO$5 OR ANGIOPLAST$2)).TI,AB.
HEART-INFARCTION#.DE.
(MYOCARD$4 NEAR INFARCT$5).TI,AB.
(HEART NEAR INFARC$5).TI,AB.
HEART-MUSCLE-REVASCULARIZATION#.DE.
ANGINA-PECTORIS#.DE.
ANGINA.TI,AB.
CONGESTIVE-HEART-FAILURE#.DE.
(HEART NEAR FAILURE).TI,AB.
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
(HEART NEAR DISEASE$2).TI,AB.
CARDIAC$2.TI,AB.
CABG.TI,AB.
PTCA.TI,AB.
STENT$4.TI,AB. AND HEART.TI,AB.
EXTRACORPOREAL-CIRCULATION#.DE.
16 OR 17 OR 18 OR 19 OR 20 OR 21
15 OR 22
PSYCHOTHERAPY#.W..DE.
PSYCHOTHERAP$2.TI,AB.
PSYCHOLOG$5 NEAR INTERVENT$5
RELAX$6.TI,AB.
RELAXATION-TRAINING#.DE.
COUNSELING#.W..DE.
(COUNSELLING OR COUNSELING).TI,AB.
(BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAPY$2 OR CHANGE)
STRESS-MANAGEMENT#.DE.
STRESS NEAR MANAGEMENT
MEDITATION#.W..DE.
MEDITAT$5.TI,AB.
MANAGE$5 NEAR (ANXIETY OR DEPRES$5)
CBT.TI,AB.
HYPNOTHERAP$2.TI,AB.
GOAL$2 NEAR SETTING
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
AUTOGENIC-TRAINING#.DE.
AUTOGENIC.TI,AB.
REHABILITATION#.W..DE.
REHABILITATION-CENTER#.DE.
REHABIL$.TI,AB.
SPORT#.W..DE.
KINESIOTHERAPY#.W..DE.
EXERCISE#.W..DE.
PHYSIOTHERAPY#.W..DE.
PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$5 OR THERAP$5 OR ACTIVIT$5)
TRAIN$5 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)
(EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)
AEROBIC$4 NEAR EXERCISE$4
(KINESIOTHERAPY OR PHYSIOTHERAPY).TI,AB.
PATIENT-EDUCATION#.DE.
PATIENT$2 NEAR EDUCAT$4
(LIFESTYLE OR LIFE ADJ STYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)
SELF-CARE#.DE.
SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)
AMBULATORY-CARE#.DE.
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
AUTOGENIC-TRAINING#.DE.
AUTOGENIC.TI,AB.
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49
50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71 OR 72 OR 73 OR 74 OR 75 OR 76 OR 77 OR 78 OR 79 OR 80 OR 81 OR 82
83 OR 84
(RANDOM$ OR PLACEBO$).TI,AB.
(SINGL$4 OR DOUBLE$4 OR TRIPLE$4 OR TREBLE$4).TI,AB. AND (BLIND$4 OR MASK$4).TI,AB.
(CONTROLLED ADJ CLINICAL ADJ TRIAL).TI,AB.
RANDOMIZED-CONTROLLED-TRIAL#.DE.
1 OR 2 OR 3 OR 4
23 AND 85
91 AND 92
LIMIT 92 TO 2001-2008
CINAHL DIALOG 1980-WEEK 1 2008
((MYOCARD$4 OR HEART) NEAR (ISCHAEMI$2 OR ISCHEMI$2)).TI,AB.
CORONARY.TI,AB.
((MYOCARD$4 OR HEART) NEAR INFARC$5).TI,AB.
ANGINA.TI,AB.
(HEART NEAR FAILURE).TI,AB.
(HEART NEAR DISEAS$2).TI,AB.
CARDIAC$2.TI,AB.
CABG
PTCA
STENT$4.TI,AB. AND (HEART OR CARDIAC$4).TI,AB.
MYOCARDIAL-ISCHEMIA#.DE.
MYOCARDIAL-INFARCTION#.DE.
CORONARY-ARTERY-BYPASS#.DE.
CORONARY-DISEASE#.DE.
CARDIAC-PATIENTS#.DE.
MYOCARDIAL-DISEASES#.DE.
MYOCARDIAL-REVASCULARIZATION#.DE.
HEART-DISEASES#.DE.
CARDIOVASCULAR-DISEASES#.DE.
HEART-FAILURE-CONGESTIVE#.DE.
ANGINA-PECTORIS#.DE.
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21
REHABILITATION#.W..DE.
SPORTS#.W..DE.
EXERCISE#.W..DE.
PHYSICAL-ACTIVITY#.DE.
MUSCLE-STRENGTHENING#.DE.
AEROBIC-EXERCISES#.DE.
PHYSICAL-FITNESS#.DE.
PATIENT-EDUCATION#.DE.
THERAPEUTIC-EXERCISE#.DE.
REHABILITAT$5.TI,AB.
(PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$4 OR THERAP$5 OR ACTIVIT$4)).TI,AB.
(TRAIN$4 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)).TI,AB.
((EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)).TI,AB.
(PATIENT$2 NEAR EDUCAT$4).TI,AB.
((LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)).TI,AB.
SELF-CARE#.DE.
(SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)).TI,AB.
AMBULATORY-CARE#.DE.
AEROBIC.TI,AB.
RESISTANCE ADJ TRAIN$4
MUSCLE ADJ STRENGTH$5
AEROBIC.TI,AB.
RESISTANCE ADJ TRAIN$4
MUSCLE ADJ STRENGTH$5
PSYCHOTHERAPY#.W..DE.
PSYCHOTHERAP$2.TI,AB.
(PSYCHOLOG$5 NEAR INTERVENT$5).TI,AB.
RELAX.TI,AB.
RELAXATION-TECHNIQUES#.DE.
(COUNSELLING OR COUNSELING).TI,AB.
COUNSELING#.W..DE.
((BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAP$2 OR CHANGE)).TI,AB.
STRESS-MANAGEMENT#.DE.
(STRESS NEAR MANAG$5).TI,AB.
(COGNITIVE NEAR THERAP$2).TI,AB.
MEDITATION#.W..DE.
MEDITAT$5.TI,AB.
ANXIETY#.W..DE.
(MANAGE$5 NEAR (ANXIETY OR DEPRESS$5)).TI,AB.
CBT.TI,AB.
HYPNOTHERAP$5.TI,AB.
(GOAL$2 NEAR SETTING).TI,AB.
(PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5).TI,AB.
(MOTIVAT$5 NEAR (INTERV$3 OR INTERVENT$5)).TI,AB.
PSYCHOSOCIAL$4.TI,AB.
HEALTH-EDUCATION#.DE.
(HEALTH NEAR EDUCAT$5).TI,AB.
HEART ADJ MANUAL
AUTOGENIC$3.TI,AB.
23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46
47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71
72 OR 73
22 AND 74
PT=CLINICAL-TRIAL
CLINICAL-TRIALS#.DE.
(RANDOM$5 OR PLACEBO$2).TI,AB.
(SINGL$ OR DOUBLE$ OR TRIPLE$ OR TREBLE$).TI,AB. AND (BLIND$ OR MASK$).TI,AB.
CONTROLLED ADJ CLINICAL ADJ TRIALS
76 OR 77 OR 78 OR 79 OR 80
75 AND 81
LIMIT 82 TO 2001-2008
PsycINFO DIALOG 1972 TO JAN WEEK 1
SEARCH: HEART-DISORDERS#.DE.
SEARCH: MYOCARDIAL-INFARCTIONS.DE.
SEARCH: ISCHEMIA#.W..DE.
SEARCH: HEART-SURGERY.DE.
SEARCH: ANGIOPLASTY
SEARCH: HEART ADJ BYPASS
SEARCH: CORONARY.TI,AB.
SEARCH: (ISCHEMI$3 OR ISCHAEMI$3).TI,AB.
SEARCH: (MYOCARD$5 NEAR INFARCT$5).TI,AB.
SEARCH: (HEART NEAR (INFARC$5 OR FAILURE OR ATTACK)).TI,AB.
SEARCH: ANGINA.TI,AB.
SEARCH: (HEART NEAR DISEASE$2).TI,AB.
SEARCH: MYOCARD$5.TI,AB.
SEARCH: CARDIAC$4.TI,AB.
SEARCH: CABG.TI,AB.
SEARCH: PTCA.TI,AB.
SEARCH: 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16
SEARCH: PHYSICAL-ACTIVITY#.DE.
SEARCH: SPORTS#.W..DE.
SEARCH: PHYSICAL-EDUCATION.DE.
SEARCH: HEALTH-BEHAVIOR#.DE.
SEARCH: PHYSICAL-FITNESS.DE.
SEARCH: (PHYSICAL ADJ EDUCATION).TI,AB.
SEARCH: EXERTION.TI,AB.
SEARCH: REHABILITAT$6.TI,AB.
SEARCH: (PHYSICAL NEAR (FIT$5 OR TRAIN$5 OR THERAP$5 OR ACTIVIT$4)).TI,AB.
SEARCH: (TRAIN$4 NEAR (STRENGTH$4 OR AEROBIC OR EXERCISE$2)).TI,AB.
SEARCH: ((EXERCISE$3 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$4 OR THERAP$2)).TI,AB.
SEARCH: (PATIENT WITH EDUCATION).TI,AB.
SEARCH: CLIENT-EDUCATION#.DE.
SEARCH: HEALTH-PROMOTION#.DE.
SEARCH: ((LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)).TI,AB.
SEARCH: OUTPATIENT-TREATMENT#.DE.
SEARCH: 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33
SEARCH: PSYCHOTHERAPY#.W..DE.
SEARCH: PSYCHOTHERAP$2.TI,AB.
SEARCH: TREATMENT#.W..DE.
SEARCH: (PSYCHOLOG$4 NEAR INTERVENT$5).TI,AB.
SEARCH: COUNSELING#.W..DE.
SEARCH: COPING-BEHAVIOR#.DE.
SEARCH: MEDITATION.W..DE.
SEARCH: AUTOGENIC-TRAINING.DE.
SEARCH: HEALTH-EDUCATION#.DE.
SEARCH: RELAX$6.TI,AB.
SEARCH: (COUNSELLING OR COUNSELING).TI,AB.
SEARCH: ((BEHAVIOUR OR BEHAVIOR) NEAR (MODIF$5 OR THERAP$5 OR REHABILIT$5 OR CHANGE)).TI,AB.
SEARCH: (STRESS NEAR MANAGE$5).TI,AB.
SEARCH: MEDITAT$5.TI,AB.
SEARCH: (MANAGE$5 NEAR (ANXIETY OR DEPRES$5)).TI,AB.
SEARCH: (CBT OR COGNITIV$2 NEAR THERAP$3).TI,AB.
SEARCH: HYPNOTHERAP$3.TI,AB.
SEARCH: (PSYCHO-EDUCAT$6 OR PSYCHOEDUCAT$6).TI,AB.
SEARCH: (MOTIVAT$5 NEAR INTERVENT$5).TI,AB.
SEARCH: (SELF NEAR MANAG$6).TI,AB.
SEARCH: AUTOGENIC$3.TI,AB.
SEARCH: (GOAL NEAR SETTING).TI,AB.
SEARCH: (HEALTH NEAR EDUCATION).TI,AB.
SEARCH: (HEART ADJ MANUAL).TI,AB.
SEARCH: 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58
SEARCH: 17 AND (34 OR 59)
SEARCH: (RANDOM$5 OR PLACEBO$5).TI,AB.
SEARCH: (DOUBLE$4 OR SINGLE$4 OR TRIPLE$4).TI,AB. AND (BLIND$4 OR MASK OR SHAM$4 OR DUMMY).TI,AB.
SEARCH: RCT.TI,AB.
SEARCH: AT=TREATMENT$
SEARCH: 61 OR 62 OR 63 OR 64
SEARCH: 60 AND 66
SEARCH: LIMIT 66 TO YRS=2001-2008
ISI Proceedings, search date: 01/04/2008
# 7 807 #5 and #6
Databases=STP Timespan=2001-2008
# 6 29,517 TS=(rehab* or educat*)
Databases=STP Timespan=2001-2008
# 5 52,687 #4 OR #3 OR #2 OR #1
Databases=STP Timespan=2001-2008
# 4 27,506 TS=(angina or cardiac* or PTCA or CABG)
Databases=STP Timespan=2001-2008
# 3 11,226 TS=((heart) SAME (infarct* or isch?emia or failure or attack))
Databases=STP Timespan=2001-2008
# 2 12,618 TS=((coronary* or heart*) SAME (by?pass or disease*))
Databases=STP Timespan=2001-2008
# 1 11,809 TS=((myocard*) SAME (isch?emia or infarct* or revasculari?*))
Databases=STP Timespan=2001-2008
WHAT’S NEW
Last assessed as up-to-date: 6 July 2008.
| Date | Event | Description |
|---|---|---|
| 19 April 2010 | Amended | Minor changes to the Background section. |
HISTORY
Protocol first published: Issue 2, 2008
Review first published: Issue 1, 2010
| Date | Event | Description |
|---|---|---|
| 10 February 2010 | Amended | Forest plots of ‘Mortality’ and ‘Completers’ have been updated as home and hospital group headings were inadvertently reversed in the original review Added citation in ‘Other published versions of this review’. |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
During the review (and before any data analysis was undertaken) it was decided that: (1) because of the variability and inconsistency of reporting, only overall mortality and not report cardiac-specific mortality be reported; (2) that the outcome of adherence to intervention should be included.
In accord with the recently updated Cochrane Handbook for Systematic Reviews and RevMan update (v.5) the assessment of the risk of bias was updated by assessing the evidence that the groups were balanced at baseline and that the groups received the same intervention.
In the data synthesis process for dichotomous variables relative risks instead of odds ratios were calculated.
Given the small number of included trials stratified meta-analysis and meta-regression to further explore heterogeneity have been abandoned.
Footnotes
DECLARATIONS OF INTEREST
KJ is the first author of the previous systematic review of home-based versus centre-based cardiac rehabilitation and principal investigator of the BRUM trial of home-based versus centre-based cardiac rehabilitation. HD is principal investigator on the CHARMS trial of home-based versus centre-based cardiac rehabilitation. RST is a co-author of the previous systematic review of home-based versus centre-based cardiac rehabilitation and a co-investigator of the BRUM and CHARMS trials of home-based versus centre-based cardiac rehabilitation. TM and AZ - no known conflict of interest.
References to studies included in this review
- Arthur 2002 {published and unpublished data} .*; Arthur HM, Smith KM, Kodis J, McKelvie R. A controlled trial of hospital versus home-based exercise in cardiac patients. Medicine and Science in Sports and Exercise. 2002;34(10):1544–50. doi: 10.1097/00005768-200210000-00003. [DOI] [PubMed] [Google Scholar]
- Smith KM, Arthur HM, McKelvie RS, Kodis J. Differences in sustainability of exercise and health-related quality of life outcomes following home or hospital-based cardiac rehabilitation. European Journal of Cardiovascular Prevention and Rehabilitation. 2004;11(4):313–9. doi: 10.1097/01.hjr.0000136414.40017.10. [DOI] [PubMed] [Google Scholar]
- Bell 1998 {published and unpublished data} .Bell JM. Thesis submitted to the University of London for the degree of Doctor of Philosophy. 1998. A comparison of a multi-disciplinary home based cardiac rehabilitation programme with comprehensive conventional rehabilitation in post-myocardial infarction patients. [Google Scholar]
- Carlson 2000 {published and unpublished data} .Carlson J. A comparison of traditional and modified cardiac rehabilitation protocols on compliance to exercise, patient self-efficacy, cardiovascular outcomes, and program cost. Dissertation Abstracts International: Section B: The Sciences and Engineering. 1999;59(7-B):3388. [Google Scholar]
- *; Carlson JJ, Johnson JA, Franklin BA, VanderLaan RL. Program participation, exercise adherence, cardiovascular outcomes, and program cost of traditional versus modified cardiac rehabilitation. American Journal of Cardiology. 2000;86(1):17–23. doi: 10.1016/s0002-9149(00)00822-5. [DOI] [PubMed] [Google Scholar]
- Carlson JJ, Norman GJ, Feltz DL, Franklin BA, Johnson JA, Locke S. Self-efficacy, psychosocial factors, and exercise behavior in traditional versus modified cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2001;21(6):363–73. doi: 10.1097/00008483-200111000-00004. [DOI] [PubMed] [Google Scholar]
- Dalal 2007 {published and unpublished data} .*; Dalal HM, Evans PH, Campbell JL, Taylor RS, Watt A, Read KL, et al. Home-based versus hospital-based rehabilitation after myocardial infarction: A randomized trial with preference arms--Cornwall Heart Attack Rehabilitation Management Study (CHARMS) International Journal of Cardiology. 2007;119(2):202–11. doi: 10.1016/j.ijcard.2006.11.018. [DOI] [PubMed] [Google Scholar]
- Taylor RS, Watt A, Dalal HM, Evans PH, Campbell JL, Read KL, et al. Home-based cardiac rehabilitation versus hospital-based rehabilitation: a cost effectiveness analysis. International Journal of Cardiology. 2007;119(2):196–201. doi: 10.1016/j.ijcard.2006.07.218. [DOI] [PubMed] [Google Scholar]
- Daskapan 2005 {published and unpublished data} .*; Daskapan A, Arikan H, Caglar N, Tunali N, Ataman S. Comparison of supervised exercise training and home-based exercise training in chronic heart failure. Saudi Medical Journal. 2005;26(5):842–7. [PubMed] [Google Scholar]
- Daskapan A, Arikan H, Caglar N, Turkman N. The effects of two different exercise programs on pulmonary function tests and quality of life in chornic heart failure: a pilot study (Turkish) Fizyoterapi Rehabilitasyon. 2005;16(2):74–81. [Google Scholar]
- Gordon 2002 Community {published and unpublished data} .Gordon NF, English CD, Contractor AS, Salmon RD, Leighton RF, Franklin BA, et al. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. American Journal Cardiology. 2002;89(11):1263–8. doi: 10.1016/s0002-9149(02)02323-8. [DOI] [PubMed] [Google Scholar]
- Gordon 2002 Supervised {published and unpublished data} .Gordon NF, English CD, Contractor AS, Salmon RD, Leighton RF, Franklin BA, et al. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. American Journal of Cardiology. 2002;89(11):1263–8. doi: 10.1016/s0002-9149(02)02323-8. [DOI] [PubMed] [Google Scholar]
- Jolly 2007 {published and unpublished data} .Jolly K, Lip GY, Sandercock J, Greenfield SM, Raftery JP, Mant J, et al. Home-based versus hospital-based cardiac rehabilitation after myocardial infarction or revascularisation: design and rationale of the Birmingham Rehabilitation Uptake Maximisation Study (BRUM): a randomised controlled trial [ISRCTN72884263] BMC Cardiovascular Disorders. 2003;3:10. doi: 10.1186/1471-2261-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolly K, Lip GY, Taylor RS, Raftery JP, Mant JW, Lane D, et al. The Birmingham Rehabilitation Uptake Maximisation study (BRUM): a randomised controlled trial comparing home-based with centre-based cardiac rehabilitation. Heart. 2008 Mar 10; doi: 10.1136/hrt.2007.127209. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- *; Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technology Assessment. 2007;11(35):1–118. doi: 10.3310/hta11350. [DOI] [PubMed] [Google Scholar]
- Kassaian 2000 {published and unpublished data} .Kassaian M, Maleki M, Noohi F, Eftekharzadeh M, Arya A, Roshanali F, Momtahen M. Comparing effects of supervised vs. home-based cardiac rehabilitation. Iranian Heart Journal. 2000;1(2):95–102. [Google Scholar]
- Marchionni 2003 {published and unpublished data} .Marchionni N, Fattirolli F, Fumagalli S, Oldridge N, Del Lungo F, Morosi L, et al. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: results of a randomized, controlled trial. Circulation. 2003;107(17):2201–6. doi: 10.1161/01.CIR.0000066322.21016.4A. [DOI] [PubMed] [Google Scholar]
- Miller 1984 Brief {published and unpublished data} .DeBusk RF, Haskell WL, Miller NH, Berra K, Taylor CB, Berger WE, III, et al. Medically directed at-home rehabilitation soon after clinically uncomplicated acute myocardial infarction: a new model for patient care. American Journal of Cardiology. 1985;55(4):251–7. doi: 10.1016/0002-9149(85)90355-8. [DOI] [PubMed] [Google Scholar]
- *; Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation. 1984;70(4):645–9. doi: 10.1161/01.cir.70.4.645. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Houston-Miller N, Ahn DK, Haskell W, DeBusk RF. The effects of exercise training programs on psychosocial improvement in uncomplicated postmyocardial infarction patients. Journal of Psychosomatic Research. 1986;30(5):581–7. doi: 10.1016/0022-3999(86)90031-0. [DOI] [PubMed] [Google Scholar]
- Miller 1984 Expanded {published and unpublished data} .DeBusk RF, Haskell WL, Miller NH, Berra K, Taylor CB, Berger WE, III, et al. Medically directed at-home rehabilitation soon after clinically uncomplicated acute myocardial infarction: a new model for patient care. The American Journal of Cardiology. 1985;55(4):251–7. doi: 10.1016/0002-9149(85)90355-8. [DOI] [PubMed] [Google Scholar]
- *; Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation. 1984;70(4):645–9. doi: 10.1161/01.cir.70.4.645. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Houston-Miller N, Ahn DK, Haskell W, DeBusk RF. The effects of exercise training programs on psychosocial improvement in uncomplicated postmyocardial infarction patients. Journal of Psychosomatic Research. 1986;30(5):581–7. doi: 10.1016/0022-3999(86)90031-0. [DOI] [PubMed] [Google Scholar]
- Sparks 1993 {published and unpublished data} .Sparks KE, Shaw DK, Eddy D, Hanigosky P, Vantrese J. Alternatives for cardiac rehabilitation patients unable to return to a hospital-based program. Heart Lung. 1993;22(4):298–303. [PubMed] [Google Scholar]
- Wu 2006 {published and unpublished data} .Wu SK, Lin YW, Chen CL, Tsai SW. Cardiac rehabilitation vs. home exercise after coronary artery bypass graft surgery: a comparison of heart rate recovery. American Journal of Physical Medicine and Rehabilitation. 2006;85(9):711–7. doi: 10.1097/01.phm.0000228597.64057.66. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Ades 2000 {published and unpublished data} .Ades PA, Pashkow FJ, Fletcher G, Pina IL, Zohman LR, Nestor JR. A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. American Heart Journal. 2000;139(3):543–8. doi: 10.1016/s0002-8703(00)90100-5. [DOI] [PubMed] [Google Scholar]
- Senuzun 2006 {published and unpublished data} .Senuzun F, Fadiloglu C, Burke L, Payzin S. Effects of home-based cardiac exercise program on the exercise tolerance, serum lipid values and self-efficacy of coronary patients. European Journal of Cardiovascular Prevention and Rehabilitation. 2006;13(4):640–5. doi: 10.1097/01.hjr.0000198445.41680.ec. [DOI] [PubMed] [Google Scholar]
- Sinclair 2005 {published and unpublished data} .Sinclair A, Conroy S, Davies M, Bayer A. Post-discharge home-based support for older cardiac patients: a randomised controlled trial. Age and Ageing. 2005;34(4):338–43. doi: 10.1093/ageing/afi116. [DOI] [PubMed] [Google Scholar]
- Tygesen 2001 {published and unpublished data} .Tygesen H, Wettervik C, Wennerblom B. Intensive home-based exercise training in cardiac rehabilitation increases exercise capacity and heart rate variability. International Journal of Cardiology. 2001;79(2-3):175–82. doi: 10.1016/s0167-5273(01)00414-4. [DOI] [PubMed] [Google Scholar]
Additional references
- Allender 2008 .Allender S, Peto V, Scarborough P, Kaur A, Rayner M. Coronary heart disease statistics. British Heart Foundation; London: 2008. [Google Scholar]
- Balady 2007 .Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115(20):2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- Bergner 1976 .Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS. The sickness impact profile: validation of a health status measure. Medical Care. 1976;14:57–67. doi: 10.1097/00005650-197601000-00006. [DOI] [PubMed] [Google Scholar]
- Beswick 2004 .Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technology Assessment. 2004;8(41):1–166. doi: 10.3310/hta8410. [DOI] [PubMed] [Google Scholar]
- Davies 2008 .Davies P, Beswick A, Wise F, Harris, Moxham T, Taylor F, Taylor RS. Promoting patient uptake and adherence in cardiac rehabilitation (Protocol) Cochrane Database of Systematic Reviews. 2008;(2) doi: 10.1002/14651858.CD007131.pub2. DOI: 10.1002/14651858.CD007131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroQoL 1990 .The EuroQol Group EuroQol - a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Graham 2007 .Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) European Journal of Cardiovascular Prevention and Rehabilitation. 2007;14(Suppl 2):S1–113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- Heart Manual 2008 .Heart Manual Office . Heart Manual. Heart Manual Office; Edinburgh: 2008. http://www.theheartmanual.com. [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. [accessed 15 February 2008];Cochrane Handbook for Systematic Reviews of Interventions 4.2.6. http://www.cochrane.org/resources/handbook/hbook.htm. updated September 2006.
- Hunt 1980 .Hunt SM, McEwan T. The development of a subjective health indicator. Sociology of Health and Illness. 1980;2:231–246. doi: 10.1111/1467-9566.ep11340686. [DOI] [PubMed] [Google Scholar]
- Höfer 2004 .Höfer S, Lim L, Guyatt G, Oldridge N. The MacNew Heart Disease health-related quality of life instrument: a summary. Health Qualioty of Life Outcomes. 2004;2:3. doi: 10.1186/1477-7525-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolliffe 2001 .Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. 2001;(1) doi: 10.1002/14651858.CD001800. DOI: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- Jolly 2006 .Jolly K, Taylor RS, Lip GY. Stevens A. Home-based cardiac rehabilitation compared with centre-based rehabilitation and usual care: a systematic review and meta-analysis. International Journal of Cardiology. 2006;111(3):343–51. doi: 10.1016/j.ijcard.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Lewin 1992 .Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M. Effects of self-help post-myocardial-infarction rehabilitation on psychological adjustment and use of health services. Lancet. 1992;339(8800):1036–40. doi: 10.1016/0140-6736(92)90547-g. [DOI] [PubMed] [Google Scholar]
- McHorney 1993 .McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care. 1993;31(3):246–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- NICE 2007 .National Institute for Health and Clinical Excellence . MI: Secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction. National Institute for Health and Clinical Excellence; London, UK: [accessed 18 2 2008]. 2007. Available at http://www.nice.org.uk/CG48. [Google Scholar]
- Rees 2004a .Rees K, Taylor RS, Singh S, Coats AJS, Ebrahim S. Exercise-based rehabilitation for heart failure. Cochrane Database of Systematic Reviews. 2004;(3) doi: 10.1002/14651858.CD003331.pub2. DOI: 10.1002/14651858.CD003331.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees 2004b .Rees K, Bennett P, West R, Davey Smith G, Ebrahim S. Psychological interventions for coronary heart disease. Cochrane Database of Systematic Reviews. 2004;(2) doi: 10.1002/14651858.CD002902.pub2. DOI: 10.1002/14651858.CD002902.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone 2005 .Stone JA, Arthur HM. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention, second edition, 2004: executive summary. Canadian Journal of Cardiology. 2005;21(Suppl D):3D–19D. [PubMed] [Google Scholar]
- Taylor 2004 .Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. American Journal of Medicine. 2004;116(10):682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- WHO 2004 .World Health Organization . The Atlas of Heart Disease and Stroke. World Health Organization; Geneva: 2004. [Google Scholar]
References to other published versions of this review
- Dalal 2010 .Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ. 2010;340:b5631. doi: 10.1136/bmj.b5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Indicates the major publication for the study