Abstract
Objective
To assess the reported indications for elective colon resection for diverticulitis and concordance with professional guidelines.
Background
Despite modern professional guidelines recommending delay in elective colon resection beyond 2 episodes of uncomplicated diverticulitis, the incidence of elective colectomy has increased dramatically in the last 2 decades. Whether surgeons have changed their threshold for recommending a surgical intervention is unknown. In 2010, Washington State’s Surgical Care and Outcomes Assessment Program initiated a benchmarking and education initiative related to the indications for colon resection.
Methods
Prospective cohort study evaluating indications from chronic complications (fistula, stricture, bleeding) or the number of previously treated diverticulitis episodes for patients undergoing elective colectomy at 1 of 49 participating hospitals (2010–2013).
Results
Among 2724 patients (58.7 ± 13 years; 46% men), 29.4% had a chronic complication indication (15.6% fistula, 7.4% stricture, 3.0% bleeding, 5.8% other). For the 70.5% with an episode-based indication, 39.4% had 2 or fewer episodes, 56.5% had 3 to 10 episodes, and 4.1% had more than 10 episodes. Thirty-one percent of patients failed to meet indications for either a chronic complication or 3 or more episodes. Over the 4 years, the proportion of patients with an indication of 3 or more episodes increased from 36.6% to 52.7% (P < 0.001) whereas the proportion of those who failed to meet either clinical or episode-based indications decreased from 38.4% to 26.4% (P < 0.001). The annual rate of emergency resections did not increase significantly, varying from 5.6 to 5.9 per year (P = 0.81).
Conclusions
Adherence to a guideline based on 3 or more episodes for elective colectomy increased concurrently with a benchmarking and peer-to-peer messaging initiative. Improving adherence to professional guidelines related to appropriate care is critical and can be facilitated by quality improvement collaboratives.
Keywords: appropriateness, benchmarking, diverticulitis, elective colectomy, guidelines
Acute diverticulitis is one of the most common indications for hospitalization related to the gastrointestinal tract and a leading indication for both elective colon resection and emergency colostomy.1–4 For more than 50 years, surgeons have been trained to recommend elective, “prophylactic” colectomy after 2 episodes of uncomplicated diverticulitis, and even after 1 episode for those younger than 50 years, in presumed hope of reducing the risk of colostomy.5–7 Contemporary data have brought into question the preventive role of elective surgery for diverticulitis and highlighted the very low risk of emergency colectomy in patients undergoing nonoperative management. In the last 10 years, several surgical societies have produced guidelines that have recommended delaying elective resection until after more than 2 episodes.8–11 The most recent American Society of Colon and Rectal Surgeons (ASCRS) guidelines “strongly advise” against elective resection for uncomplicated diverticulitis and consider multiple episodes as an indication only for those with “complicated disease.”12 Surprisingly, despite these recommendations, the use of elective surgery seems to be increasing faster than the incidence of diverticulitis,13–15 with a recent statewide analysis showing a 3-fold increase in the incidence of elective colectomy for diverticulitis during the laparoscopic era (Flum et al, unpublished data, 2014).
Given the escalating costs of care and a focus on value-added interventions, there has been increasing interest in establishing appropriateness criteria for many surgical procedures.16–20 Assessing compliance with appropriateness of care recommendations, such as delaying elective resection for diverticulitis, has been problematic because detailed information about the indications for surgery is not commonly gathered by existing registries. In 2010, Washington State’s Surgical Care and Outcomes Assessment Program (SCOAP) began surveillance, benchmarking, and education related to the indications for colon resection related to diverticulitis. The aim of this study was to assess the clinician-reported indications for elective colectomy and describe trends in the number of prior episodes of diverticulitis, concurrent to SCOAP’s messaging and benchmarking initiative related to established guidelines.
METHODS
Study Design
Consecutive patients who underwent elective colon resection after recovery from diverticulitis between January 1, 2010, and December 31, 2013, in 49 Washington State hospitals participating in SCOAP were included in the primary cohort. This study was exempted from human subjects review by agreement of the University of Washington Human Subject Review Committee and Washington State Department of Health. The Comparative Effectiveness Research Translation Network (CERTAIN) provided research and analytic support to SCOAP.21 Patients undergoing emergent colectomy for diverticulitis were included both for descriptive statistical comparison and for measuring trends over the time course of the study alone.
Data Sources and Definitions
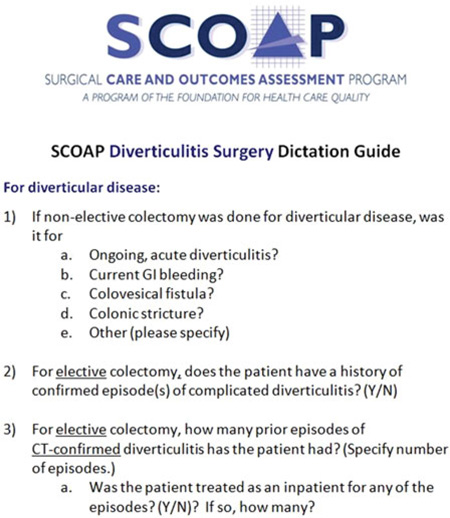
Sociodemographic and clinical characteristics were extracted from inpatient medical records by trained chart abstractors at each clinical site. Operative details, including elective or emergent nature of the operation and the indications for surgery, were abstracted from operative reports and clinical records. Standardized dictation guides were supplied to all clinicians to improve the ability of abstractors to accurately record the indications for each procedure (see the Appendix). SCOAP metrics and data dictionary are publicly available at http://www.SCOAP.org. A modified Charlson comorbidity index for each patient was calculated.22
Indications
Clinical and episode-based indications were included in the SCOAP data collection platform in 2010. These definitions were created on the basis of review of existing evidence and guidelines by an expert panel of colorectal and general surgeons across Washington State. Chronic complication indications included gastrointestinal bleeding, stricture, and fistula. In addition, starting in 2011, the category “other” was added to help capture unmeasured clinical indications. The total number of prior episodes of diverticulitis was derived from clinical records and surgeons’ dictations. Prior episodes were initially captured as a continuous variable but were converted to categories as 1, 2, 3 to 10, and more than 10 after 2010.
Performance Benchmarking and Messaging Related to Guidelines
Beginning in 2011, participating SCOAP hospitals were provided feedback to disseminate to their surgeons about the proportion of their procedures that failed to indicate the presence of a clinical indication, or were absent as a clinical indication, or had 2 or fewer prior episodes of diverticulitis. Comparative data from all sites were made available in each report, and a series of presentations and alerts about the benchmarking program and available guidelines9,23,24 related to indications for elective surgery in diverticulitis is distributed through newsletters, Web-based messages, regional and statewide meetings, and an informal peer network. This included broad dissemination of the 2006 ASCRS guidelines,9 as they were the most up-to-date available at that time.
Statistical Analysis
Patient characteristics were summarized using frequency distributions for categorical variables and mean (SD) for continuous variables. Descriptive and comparative statistics were applied using STATA, version 13 (STATA Corp, College Station, TX). Categorical variables were compared using Pearson χ2 statistic, and change over time is reported using a test of trend. A P value of less than 0.05 was considered statistically significant.
RESULTS
Between 2010 and 2013, there were 3613 colectomies performed for a diverticulitis-related indication and 75.4% were elective (n = 2724).
Characteristics
The mean age of patients having elective colectomy for diverticulitis was 58.7 ± 13 years, with 24.1% of the cohort being younger than 50 years. Those younger than 50 years were more likely to be male (62.4% vs 41.6%; P < 0.001) and have lower Charlson comorbidity indices (P < 0.001) (Table 1).
TABLE 1.
Patient Characteristics, Elective Colon Resection for Diverticulitis
| Total Cohort (N = 2724; 100%) | <50 (n = 655; 24.1%) | 50+ (n = 2069; 75.9%) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | P | |
| Mean age (median) | 58.7 (59) | 41.7 (43) | 64.1 (63) | <0.001 | |||
| Sex | <0.001 | ||||||
| M | 1266 | 46.5 | 409 | 62.4 | 857 | 41.6 | |
| F | 1458 | 53.5 | 246 | 37.6 | 1212 | 58.6 | |
| Comorbidities | <0.001 | ||||||
| 0 | 1983 | 72.8 | 528 | 80.6 | 1455 | 70.3 | |
| 1 | 587 | 21.6 | 108 | 16.5 | 479 | 23.2 | |
| 2 | 123 | 4.5 | 13 | 2 | 110 | 5.3 | |
| 3 | 31 | 1.1 | 6 | 0.9 | 25 | 1.21 | |
| Indications* | |||||||
| Chronic complication | 576 | 29.5 | 83 | 17.3 | 493 | 33.4 | <0.001 |
| No. episodes | |||||||
| 1 | 311 | 15.9 | 93 | 19.4 | 218 | 14.7 | <0.001† |
| 2 | 257 | 13.1 | 71 | 14.8 | 186 | 12.6 | |
| 3–10 | 816 | 41.7 | 222 | 46.3 | 594 | 40.2 | 0.35‡ |
| >10 | 59 | 3 | 17 | 3.5 | 42 | 2.8 | |
| Zero/unspecified | 515 | 26.3 | 77 | 16 | 438 | 29.6 | |
| Missing indication | 766 | 28.1 | 175 | 26.7 | 591 | 28.6 | 0.360 |
| Laparoscopic | 1620 | 59.5 | 423 | 64.6 | 1197 | 57.9 | 0.002 |
Indication % calculated from the population with complete information (total: N = 1958; <50: n = 480; 50+: n = 1478).
Calculated as Pearson χ2 for all episode categories between younger (<50 years) and older (50+) patients.
Calculated as Pearson χ2 for those with 3+ episodes between younger (<50 years) and older (50+) patients.
Indications
Data on the underlying indication for resection were missing in 28.1% of the patients over the entire course of the study and were similar across age groups. Of those with complete data and undergoing an elective resection, 31.3% did not report a chronic complication indication or meet a threshold of 3 or more episodes. A chronic complication was the indication for elective surgery in 29.4% of patients (15.6% fistula, 7.4% stricture, 3.0% bleeding, 5.8% other). The proportion of those with a chronic complication indication for operation was lower in younger patients (17.3% in those younger than 50 years vs 33.4% in those 50 years and older; P < 0.001). Of those having an indication based on the number of episodes, 39.4% had 2 or fewer episodes, 56.5% had 3 to 10 episodes, and 4.1% had more than 10 episodes. There was no difference between patients in the younger and older age groups in having elective surgery after fewer than 3 episodes, which occurred in 47.1% of younger and 49.7% of older patients (P = 0.35). Laparoscopic surgery was used in 59.5% of cases. Younger patients had laparoscopy in 64.6% of cases versus 57.9% in older patients (P = 0.002).
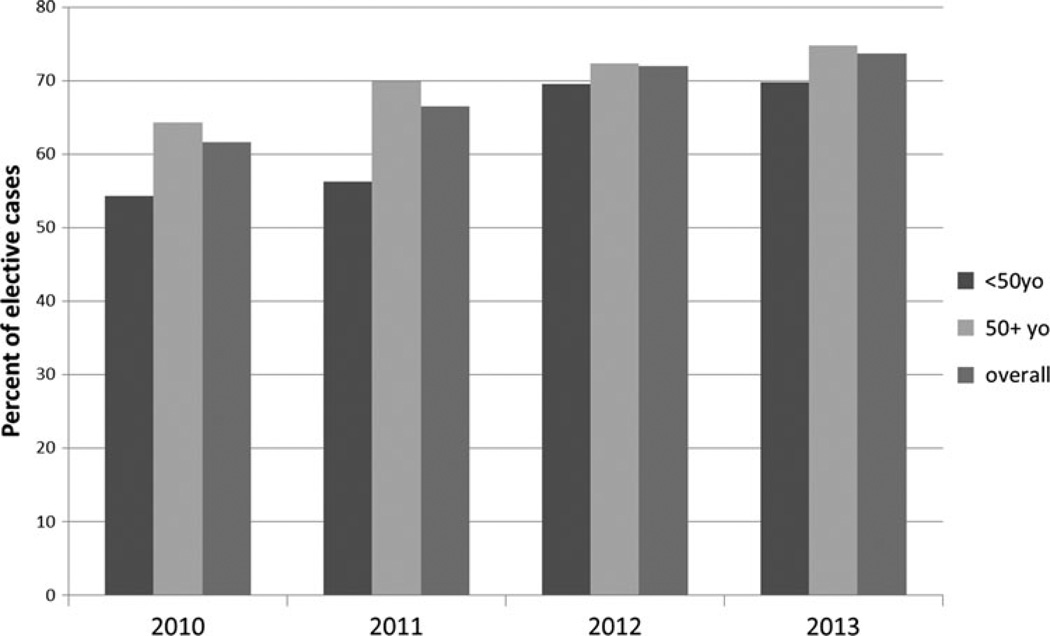
Temporal Trends
The proportion of those with chronic complication indications (gastrointestinal bleeding, fistula, stricture, and other) remained unchanged over the period of the study (P = 0.69) (Table 2). Of patients having elective colectomy based on the number of prior episodes, the proportion with 3 or more episodes of diverticulitis increased from 36.6% to 52.7% (P < 0.001) over the 3 years studied. In patients younger than 50 years, the proportion of patients with elective resections meeting indications based on chronic complication or 3+ episodes increased from 54.3% to 69.8%, (P = 0.001), whereas in those 50 years or older, this proportion increased from 64.3% to 74.8% (P = 0.003) (Fig. 1). In the whole cohort, the proportion that did not meet indications based on either complication or 3 or more episodes decreased from 38.4% to 26.4% (P < 0.001). Over the study period, the proportion of patients with missing indication data decreased from 38.1% to 21.6% (P < 0.001).
TABLE 2.
Temporal Trends in Indications and Approach
| 2010 | 2011 | 2012 | 2013 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | P | |
| No. episodes* | |||||||||
| 1 | 76 | 18.1 | 83 | 18 | 65 | 13.4 | 87 | 16.6 | 0.28† |
| 2 | 66 | 15.7 | 69 | 15 | 56 | 11.5 | 66 | 12.6 | |
| 3–10 | 144 | 34.2 | 177 | 38.5 | 237 | 48.8 | 258 | 49.2 | 0.001‡ |
| >10 | 10 | 2.4 | 11 | 2.4 | 20 | 4.1 | 18 | 3.4 | |
| Zero/unspecified | 125 | 29.7 | 120 | 26.1 | 108 | 22.2 | 95 | 18.1 | |
| Chronic complication* | 122 | 27.9 | 158 | 37.9 | 126 | 25.4 | 170 | 31.5 | 0.69 |
| Missing indication§ | 270 | 38.1 | 166 | 25.7 | 181 | 26.9 | 149 | 21.6 | 0.001 |
| Laparoscopic | 392 | 55.4 | 359 | 55.5 | 432 | 63.9 | 436 | 63.1 | <0.001 |
Calculated as the proportion of all those with complete indication information.
Calculated as trend for all episode categories.
Calculated as trend for 3+ episodes.
Calculated as the proportion of all elective cases performed that year.
FIGURE 1.
The proportion of patients meeting indication for 3 or more episodes or chronic clinical.
Impact on Rates of Emergency and Elective Colectomy
There were 25 hospitals where more than 10 colectomies for diverticulitis per year were performed. We limited an analysis of trends in case volume per hospital to these facilities. The yearly rate of nonelective cases did not change significantly (5.6–5.9 per year; P = 0.81), and the rate of elective colectomy remained stable (22.7–22.4 per year; P = 0.95).
DISCUSSION
In Washington State hospitals, 68.7% of all elective colon resections with complete indication information for diverticulitis were guideline concordant with either a chronic complication or 3 or more episodes of prior diverticulitis as an indication. Nearly all hospitals in the state participate in SCOAP, which began tracking detailed information about the indications for diverticulitis-related colon resection in 2010. Surgeons at SCOAP hospitals are asked to include information about the indication for elective resection into the operative note using a standard dictation template (see the Appendix). Data fields include the number of episodes of diverticulitis (not specified as in-hospital or out-of-hospital) and non–episode-based chronic complication indications (fistula, stricture, bleeding, or other that includes persistent symptoms and other clinical conditions). In the year after the initiation of indication tracking, we implemented a formal component of the program where performance benchmarking, including quarterly reports of a site’s missing data on indications, rates of indications of fewer than 3 episodes, and comparisons with average performance and best performers were delivered to every hospital. A mix of mailings, regional and statewide meetings, and peer-to-peer messaging occurred at least quarterly. Concurrent to this benchmarking, peer-to-peer messaging, and education initiative about professional guidelines, the proportion of procedures not meeting the recommendations decreased by more than a third, from 38.4% to 26.4% (P < 0.001).
Surgeons have long been trained that elective surgery should be performed after 1 to 2 episodes of diverticulitis to prevent potential complications including emergency colectomy and colostomy. More contemporary data have failed to demonstrate that this type of “preventative” surgery actually decreases the rate of emergency surgery at the population level. Most emergency colectomies for diverticulitis occur at the initial hospitalization,3,25 and the likelihood of recurrent hospitalization (5%–13%) and emergency colostomy (<5%) is quite low for those who do not have elective resection.2 Equally important is the finding that elective resection does not eliminate the risk of recurrent diverticulitis, with several studies demonstrating a 5% to 11% risk of recurrence after resection.11,26,27 Elective resection also carries the risk (1%–3%) of “rescue colostomy”11,23 for anastomotic failure. A decision analysis by our group3 that considered all these parameters demonstrated that if the recommendation for prophylactic colectomy is delayed until at least 4 episodes of hospitalization— something that occurs in less than 5% of the population2—the risk of colostomy, complications, and cost is lowest.3 The ASCRS 2006 guidelines9 incorporated these modeled data and recommended delaying surgery beyond 2 episodes. The 2014 ASCRS guidelines now recommend against elective, prophylactic surgery for uncomplicated diverticulitis.12 This is particularly relevant because despite the growing body of literature supporting delaying or avoiding elective resection, over the last decade, the incidence of elective resection has increased by more than 50%.13–15 This rise occurred at a much faster pace than emergency colon resection, another marker of incident disease.13,14 An extension of our group’s prior evaluation of trends in admissions and elective resection in Washington State28 confirms this remarkable growth in elective surgery and found a near tripling of its incidence over the past 26 years (Flum et al, unpublished data, 2014).
For more than 30 years, there have been concerns that a significant proportion of health care interventions are performed in patients who do not meet the appropriate indications for the procedure, but the extent of this problem and whether it truly reflects unnecessary care have been contested.29,30 The Commonwealth Fund estimates that 1 in 3 health care dollars is spent for health care interventions that either doesn’t improve health or is unnecessary based on surveys of patients and medical records. A series of cohort studies conducted in the 1990s and repeated in the 2000s searched medical records and diagnostic images for evidence of standard indications for carotid endarterectomy, coronary artery bypass grafting, and percutaneous revascularization and also found that 1 in 3 did not meet standard criteria.31–33 In response, professional societies have increased their production of guidelines and appropriateness criteria. Insurance companies have developed a number of mechanisms to increase adherence to these appropriateness criteria including prior authorization and application of criteria as a condition of payment (eg, Milliman criteria in spine surgery).34,35 These approaches have had mixed effects in reducing rates of procedures that do not meet the designated criteria.36 There has been much less experience with performance benchmarking and peer-to-peer messaging both in addressing the question of appropriate care in surgery and in making surgeons aware of adherence to established guidelines.
Our study shows that contemporaneous to SCOAP’s performance benchmarking and education campaign related to the ASCRS guidelines, the proportion of elective surgery that did not meet episode or clinical indications decreased, with approximately 30% not meeting the recommendations overall. As the rates of surgery meeting indications increased, we did not find an increase in the rate of nonelective colectomies performed for diverticulitis.
One important challenge in promoting adherence to professional society recommendations has been the evolving definition of appropriate indications for diverticulitis surgery. For example, during the 14-year period over which the 3 most recent ASCRS Practice Parameters have been published, there have been evolving recommendations about indications for elective surgery from a soft recommendation in 2000, “after two attacks of uncomplicated diverticulitis, resection is commonly recommended,”8 to a more declarative statement in 2014 that also suggests individualization based on patient experience “the decision to recommend elective sigmoid colectomy after recovery from uncomplicated acute diverticulitis should be individualized.” Encouraging adherence to guidelines that are in evolution or include individualization is problematic. It remains to be determined whether patient experience issues were a component of the indications for resection in the 5.8% of our cohort classified as having “other” reasons for resection or in the 30% of our cohort who had an episode-based indication but were reported to have fewer than 3 episodes. None of the professional society guidelines currently define discrete measures of patient experience to assess whether a resection is appropriate for a given patient based on their experience with the condition. When determining whether an elective colectomy is a reasonable option for a given patient, surgeons occasionally encounter patients who do not meet the ASCRS recommendations but who have emotional distress or anxiety related to the possibility of an emergency, fear of travel, uncertainty about insurance and childcare coverage, intolerance of oral antibiotics, or family history. Because guidelines for appropriate indications only vaguely refer to customizing recommendations based on patient experience, measurement of compliance with indications is challenging and often not well received by surgeons who counter that they are meeting the patient’s interest and that they should not be penalized because the guidelines do not include such potentially legitimate metrics. To address this, our group is pursuing research on patient perspectives of the indications for surgery. Assessing which patient-centered metrics improve after resection may more completely capture what should be considered appropriate care. One interpretation of this study is that even when surgeons are asked to report indications, the existing metrics do not apply to a significant proportion of cases. This may call into question how useful these metrics actually are in directing initiatives aimed at more value-added care.
Concurrent to the SCOAP benchmarking initiative was the increased adoption of laparoscopy, which may affect the threshold to recommend and undergo surgery. A lowering of the threshold to recommend and undergo cholecystectomy in the late 1980s37,38 resulted in a 30% increase in the incidence of that procedure. The availability of laparoscopy led to a change in recommendations favoring surgery after a single episode of biliary colic39 and calls for prophylactic cholecystectomy in some populations.40 Indeed, with 60% of all elective colon resections in this study performed laparoscopically, it remains to be determined whether the availability of laparoscopic surgery is lowering the threshold to offer and undergo resection.
Our study has several limitations. First, the SCOAP registry is procedural rather than disease-based, and we may be missing important trends occurring in the overall population with diverticulitis. We report trends in elective and emergency surgery as being stable, but these trends should be interpreted cautiously, as the study spans only 4 years, and other studies have pointed to increasing rates of elective surgery for diverticulitis.13–15 Another limitation of this study is the substantial proportion of patients who have missing data. Although we found no differences between those with and without indication data, this may limit the generalizability of our findings. It may also mean that our findings of increasing proportions of multiple-episode indications for elective colectomy simply reflect improved documentation, which we believe to be similarly laudable. Although missing information on indications has decreased dramatically through this process, it remains to be determined why the nearly 1 in 4 patients with no documented information about indication underwent the procedure. Furthermore, the “other” category was added to capture clinical indications but was not added until 2011. The severity of each episode of diverticulitis was not characterized, but surgeons were asked to include computed tomography–confirmed episodes and hospitalized events. Finally, although SCOAP added these indication metrics with the expectation of a prospective evaluation contemporaneous to a planned intervention, the statewide intervention around indications developed organically and was likely different at each site and difficult to characterize completely. For example, dissemination of SCOAP indication metrics passed through a “surgeon champion” at individual sites and the messaging received at the level individual surgeons may have varied and is difficult to quantify.
CONCLUSIONS
This study describes a statewide performance surveillance and benchmarking network that used feedback and education about adherence to ASCRS-recommended indications for elective colon surgery and trends in the indications across 49 hospitals. Concurrent to this initiative, we found an increase in the proportion of cases that met expert-established guidelines for appropriate surgery, but nearly 1 in 3 still do not meet established criteria. Future work aims to better understand the reasons why patients undergo colectomy and incorporate patient-centered metrics. Including the full spectrum of relevant indications into a definition of appropriate care should advance the goal of providing more value-added surgical care.
ACKNOWLEDGMENTS
The authors thank Rebecca G. Symons for help with data analytics.
Disclosure: Supported by the Agency for Healthcare Research and Quality grant HS20025 and a training grant funded The National Institute of Diabetes and Digestive and Kidney Diseases grant 5T32DK070555-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. SCOAP is a program of the Foundation for HealthCare Quality.
APPENDIX
SCOAP Diverticulitis Operative Report Guide
DISCUSSANTS
C. Delaney (Cleveland, OH)
I would like to congratulate the authors on a timely study and a well-written article in which they evaluate not just how benchmarking can change outcomes and indications but also how an educational interventional in their participating SCOAP hospitals affected indications for diverticulitis surgery.
As you alluded to, I think this is very important because it’s a common condition, and colorectal surgery is a fairly morbid area for surgery. So trying to change what we do and improve is important. It’s done by a well-respected group, who are gaining recognition and doing very well in this comparative effectiveness area. I think that coming up with standards and indications, and then measuring their impact, really is a huge part of the future for us in doing comparative effectiveness studies.
So in this carefully performed study, the authors controlled for adverse outcomes—and this was important, I think—by also controlling for and evaluating the number of emergent colectomies performed for diverticulitis in the same time period. I think that’s an important thing to remember. They found that the increase in percentage of cases being performed for 3 or more attacks and the equal percentage across the different age groups noted in the final year of the study, I think that really shows that their intervention is likely to be working, although I agree, I think it is still shocking to see 30% to 40% of cases being performed for fewer than 3 attacks.
So I have a couple of questions.
The fact that 30% of patients had surgery without appropriate indications by your criteria may really be very much a best-case scenario. Can you describe how many hospitals aren’t members of the 55 SCOAP group and maybe even less likely to follow your guidelines? And then, within the SCOAP group of hospitals, was there a difference in fulfillment or concordance with indications for surgery?
You mentioned 1 in 3 failed the indications for surgery for elective surgery, but can you clarify how you dealt with some of the patients who in fact have an appropriate single attack as an indication because of nonresolution of symptoms or failure of adequate drainage of an abscess with computed tomography–guided drainage?
Response From V. Simianu
Your first question was about variation inside and outside the SCOAP network. Comparing our case numbers with those of the hospital discharge registry in Washington State, we know that we perform more than 80% of the volume in the state. However, it’s hard to track these indications at hospitals that don’t participate in our network with the same granularity. Within our network, the spread of indications had a normal distribution with the high-volume hospitals, sort of middle of the road. There were some extremes, 4 or 5 hospitals that were low-volume hospitals that never met indications or always met indications. But this accounted for a very small proportion of our studies.
Your second question was about which patients may have appropriate surgery but only have 1 episode, such as those with an abscess or persistent pain. In our chronic complications category, we have an “other” catch-all category. This allows us to capture other indications as long as surgeons report them. Looking at the details of this, it appears that approximately 1% of all the surgical procedures we report here happen after an abscess, and these data are included in those chronic complication numbers.
DISCUSSANTS
D. Farley (Rochester, MN)
I quibble a little bit with the high-volume centers doing 10 colectomies. Did they adhere to your guidelines better than somebody just doing 100? I’m just worried that if you are doing 10 colectomies a year with 2 or 3 surgeons, you are doing it less than once a month.
Response From V. Simianu
We did look at that. Some hospitals, like the larger academic centers in our network, do have extremely high volume. It did not appear that the distribution of indications was any different at those hospitals.
DISCUSSANTS
J. Garden (Edinburgh, Scotland)
I would pick up the points that Conor Delaney made, which actually suggest that these data are really quite shocking in a way. That in about a third of your patients, you really have no idea how their diverticulitis is being managed. You indicated that one of the ways that you are going to try to improve this is to have a surgeon leader in each of the centers. But I just wondered how else you are actually going to empower your patients, how you can try to improve their engagement with this very, very important process.
Response From V. Simianu
It’s a great question, and it reminds me to point out that we are actually pursuing research funding in that realm. The next steps for us are to take the discussion of indication metrics into surgeons’ offices and talk to surgeons and their patients about describing and quantify these “missing” indications and try to put some data behind those.
DISCUSSANTS
P. Roberts (Burlington, MA)
We focus a lot on recurrent attacks of diverticulitis, but we see more and more patients with smoldering diverticulitis. Can you comment on those?
Response From V. Simianu
That is an important observation. We understand that the spectrum of diverticulitis as a disease is evolving. There is growing literature about coexistence of diverticulitis with bowel motility disorders and inflammatory bowel disease. So those may very well be an explanation for some of the missing indications. At this point, we are not capturing that specific metric.
Footnotes
Disclosure:
The authors declare no conflicts of interest.
Author contributions: V. V. Simianu: analysis and interpretation, data collection, writing the article, critical revision of the article; A. L. Bastawrous, A. Fichera, E. Johnson, D. O. Herzig: analysis and interpretation, data collection, critical revision of the article; R. P. Billingham, E. T. Farrokhi, S. R. Steele, R. C. Thirlby,D. R. Flum: conception/ design, analysis and interpretation, data collection, writing the article, critical revision of the article, and obtaining funding.
REFERENCES
- 1.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anaya DA, Flum DR. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg. 2005;140:681–685. doi: 10.1001/archsurg.140.7.681. [DOI] [PubMed] [Google Scholar]
- 3.Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904–912. doi: 10.1016/j.jamcollsurg.2004.07.029. [DOI] [PubMed] [Google Scholar]
- 4.Yen L, Davis KL, Hodkins P, et al. Direct costs of diverticulitis in a US managed care population. Am J Pharm. 2012;4:e118–e129. [Google Scholar]
- 5.Parks TG. Natural history of diverticular disease of the colon. A review of 521 cases. BMJ. 1969;4:639–642. doi: 10.1136/bmj.4.5684.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marquis P, Marrel A, Jambon B. Quality of life in patients with stomas: the Montreux study. Ostomy Wound Manage. 2003;49:48–55. [PubMed] [Google Scholar]
- 7.Nugent KP, Daniels P, Stewart B, et al. Quality of life in stoma patients. Dis Colon Rectum. 1999;42:1569–1574. doi: 10.1007/BF02236209. [DOI] [PubMed] [Google Scholar]
- 8.Wong WD, Wexner SD, Lowry A, et al. Practice parameters for the treatment of sigmoid diverticulitis-supporting documentation. The Standards Task Force of the American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290–297. doi: 10.1007/BF02258291. [DOI] [PubMed] [Google Scholar]
- 9.Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944. doi: 10.1007/s10350-006-0578-2. [DOI] [PubMed] [Google Scholar]
- 10.Fozard JB, Armitage NC, Schofield JB, et al. Association of Coloproctology of Great Britain and Ireland. ACPGBI position statement on elective resection for diverticulitis. Colorectal Dis. 2011;13:1–11. doi: 10.1111/j.1463-1318.2010.02531.x. [DOI] [PubMed] [Google Scholar]
- 11.Andersen JC, Bundgaard L, Elbrond H, et al. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453. [PubMed] [Google Scholar]
- 12.Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–294. doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 13.Etzioni DA, Cannom RR, Ault GT, et al. Diverticulitis in California from 1995 to 2006: increased rates of treatment for younger patients. Am Surg. 2009;75:981–985. [PubMed] [Google Scholar]
- 14.Etzioni DA, Mack TM, Beart RW, Jr, et al. Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 15.Masoomi H, Buchberg BS, Magno C, et al. Trends in diverticulitis management in the United States from 2002 to 2007. Arch Surg. 2011;146:400–406. doi: 10.1001/archsurg.2010.276. [DOI] [PubMed] [Google Scholar]
- 16.Birkmeyer JD, Shahian DM, Dimick JB, et al. Blueprint for a new American College of Surgeons: National Surgical Quality Improvement Program. J Am Coll Surg. 2008;207:777–782. doi: 10.1016/j.jamcollsurg.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 17.Raval MV, Hamilton BH, Ingraham AM, et al. The importance of assessing both inpatient and outpatient surgical quality. Ann Surg. 2011;253:611–618. doi: 10.1097/SLA.0b013e318208fd50. [DOI] [PubMed] [Google Scholar]
- 18.Brar S, Law C, McLeod R, et al. Defining surgical quality in gastric cancer: a RAND/UCLA appropriateness study. J Am Coll Surg. 2013;217:347–357. doi: 10.1016/j.jamcollsurg.2013.01.067. [DOI] [PubMed] [Google Scholar]
- 19.Bilimoria KY, Bentrem DJ, Lillemoe KD, et al. Pancreatic Cancer Quality Indicator Development Expert Panel, American College of Surgeons. Assessment of pancreatic cancer care in the United States based on formally developed quality indicators. J Natl Cancer Inst. 2009;101:848–859. doi: 10.1093/jnci/djp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel MR, Dehmer GJ, et al. Coronary Revascularization Writing Group ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Thorac Cardiovasc Surg. 2012;143:780–803. doi: 10.1016/j.jtcvs.2012.01.061. [DOI] [PubMed] [Google Scholar]
- 21.Devine EB, Alfonso-Cristancho R, Devlin A, et al. A model for incorporating patient and stakeholder voices in a learning health care network: Washington State’s comparative effectiveness research translation network. J Clin Epidemiol. 2013;66:S122–S129. doi: 10.1016/j.jclinepi.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 23.Collins D, Winter DC. Elective resection for diverticular disease: an evidence-based review. World J Surg. 2008;32:2429–2433. doi: 10.1007/s00268-008-9705-7. [DOI] [PubMed] [Google Scholar]
- 24.Klarenbeek BR, Samuels M, van der Wal MA, et al. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670–674. doi: 10.1097/SLA.0b013e3181d3447d. [DOI] [PubMed] [Google Scholar]
- 25.Morris AM, Regenbogen SE, Hardiman KM, et al. Sigmoid diverticulitis: a systematic review. JAMA. 2014;311:287–297. doi: 10.1001/jama.2013.282025. [DOI] [PubMed] [Google Scholar]
- 26.Wolff BG, Ready RL, MacCarty RL, et al. Influence of sigmoid resection on progression of diverticular disease of the colon. Dis Colon Rectum. 1984;27:645–647. doi: 10.1007/BF02553353. [DOI] [PubMed] [Google Scholar]
- 27.Thorn M, Graf W, Stefansson T, et al. Clinical and functional results after elective colonic resection in 75 consecutive patients with diverticular disease. Am J Surg. 2002;183:7–11. doi: 10.1016/s0002-9610(01)00847-9. [DOI] [PubMed] [Google Scholar]
- 28.Salem L, Anaya DA, Flum DR. Temporal changes in the management of diverticulitis. J Surg Res. 2005;124:318–323. doi: 10.1016/j.jss.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 29.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 30.Kelley R. Where Can $ 700 Billion in Waste Be Cut Annually From the US Healthcare System. Ann Arbor, MI: Thomson Reuters; 2009. [Google Scholar]
- 31.Brook RH, Park RE, Chassin MR, et al. Predicting the appropriate use of carotid endarterectomy, upper gastrointestinal endoscopy, and coronary angiography. N Engl J Med. 1990;323:1173–1177. doi: 10.1056/NEJM199010253231705. [DOI] [PubMed] [Google Scholar]
- 32.Kahan JP, Park RE, Leape LL, et al. Variations by specialty in physician ratings of the appropriateness and necessity of indications for procedures. Med Care. 1996;34:512–523. doi: 10.1097/00005650-199606000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Winslow CM, Solomon DH, Chassin MR, et al. The appropriateness of carotid endarterectomy. N Engl J Med. 1988;318:721–727. doi: 10.1056/NEJM198803243181201. [DOI] [PubMed] [Google Scholar]
- 34.Watters WC, Bono CM, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2009;9:609–614. doi: 10.1016/j.spinee.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Resnick DK. Evidence-based guidelines for the performance of lumbar fusion. Clin Neurosurg. 2006;53:279–284. [PubMed] [Google Scholar]
- 36.Brodie BR, Stuckey T, Downey W, et al. Outcomes and complications with off-label use of drug-eluting stents: results from the STENT (Strategic Transcatheter Evaluation of New Therapies) group. JACC Cardiovasc Interv. 2008;1:405–414. doi: 10.1016/j.jcin.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Escarce JJ, Chen W, Schwartz JS. Falling cholecystectomy thresholds since the introduction of laparoscopic cholecystectomy. JAMA. 1995;273:1581–1585. [PubMed] [Google Scholar]
- 38.Cohen MM, Young W, Theriault ME, et al. Has laparoscopic cholecystectomy changed patterns of practice and patient outcome in Ontario? CMAJ. 1996;154:491–500. [PMC free article] [PubMed] [Google Scholar]
- 39.Schwesinger WH, Diehl AK. Changing indications for laparoscopic cholecystectomy. Stones without symptoms and symptoms without stones. Surg Clin North Am. 1996;76:493–504. doi: 10.1016/s0039-6109(05)70456-4. [DOI] [PubMed] [Google Scholar]
- 40.Kao LS, Flowers C, Flum DR. Prophylactic cholecystectomy in transplant patients: a decision analysis. J Gastrointest Surg. 2005;9:965–972. doi: 10.1016/j.gassur.2005.04.011. [DOI] [PubMed] [Google Scholar]