Abstract
The goal of this study was to examine the impact of supplementing Trauma-focused Cognitive Behavioral Therapy (TF-CBT; Cohen, Mannarino, & Deblinger, 2006) with evidence-based engagement strategies on foster parent and foster youth engagement in treatment, given challenges engaging foster parents in treatment. A randomized controlled trial of TF-CBT standard delivery compared to TF-CBT plus evidence-based engagement strategies was conducted with 47 children and adolescents in foster care and one of their foster parents. Attendence, engagement, and clinical outcomes were assessed 1 month into treatment, end of treatment, and 3 months post-treatment. Youth and foster parents who received TF-CBT plus evidence-based engagement strategies were more likely to be retained in treatment through four sessions and were less likely to drop out of treatment prematurely. The engagement strategies did not appear to have an effect on the number of cancelled or no-show sessions or on treatment satisfaction. Clinical outcomes did not differ by study condition, but exploratory analyses suggest that youth had significant improvements with treatment. Strategies that specifically target engagement may hold promise for increasing access to evidence-based practices and for increasing likelihood of treatment completion.
Keywords: child trauma, child welfare, foster care, engagement, Trauma-focused Cognitive Behavioral Therapy, TF-CBT
Youth in foster care have disproportionately high rates of trauma exposure and mental health problems. Over half of children entering foster care have been exposed to abuse and neglect (Leslie, Hurlburt, Landsverk, Barth, & Slymen, 2004; Pecora et al., 2003), with 85% having witnessed violence (Stein et al., 2001). Nearly 50% demonstrate clinically significant treatment needs (Garland, Landsverk, Hough, & Ellis-McLeod, 1996; Leslie et al., 2004), which is 2–3 times higher than the general population (New Freedom Commission on Mental Health, 2003). Untreated mental health problems, and particularly behavioral difficulties, have been linked to higher rates of placement disruption and lower rates of reunification and adoption for children in foster care (Hurlburt, Chamberlain, DeGarmo, Zhang, & Price, 2010; James, 2004; James, Landsverk, & Slymen, 2004). Studies involving foster care alumni suggest that high rates of mental health problems can continue into adulthood (Courtney, Dworsky, Lee, & Raap, 2010; Pecora et al., 2003). In the foster care subsample of a nationally representative child welfare study (Kolko et al., 2010), rates of Posttraumatic Stress Disorder (PTSD) were 24.9% (ages 8–10) and 15.7 % (ages 11–14).These rates are substantially higher than those in the general population (i.e., 4.7% lifetime prevalance; McLaughlin et al., 2013) and are equivalent to those of war veterans (Kulka, Fairbank, & Schlenger, 1990).
Entering foster care can be a “gateway” to receiving mental health services, as placement is associated with higher rates of service receipt (Farmer et al., 2001; Leslie et al., 2005). Nonetheless, the percentage of unmet mental health need for this population remains high, with only between 50% (Burns et al., 2004) and 64% (Leslie et al., 2005) of those with need receiving services. For those who do receive services, it is unclear whether or not they receive evidence-based treatments (EBTs) targeting their particular mental health (Landsverk, Burns, Stambaugh, & Reutz, 2006). To date, a number of EBTs for a range of child and adolescent mental health problems have been developed and, in some cases, efficacy or effectiveness has been established specifically within child welfare (for reviews, see Chaffin & Friedrich, 2004). There is substantial variation, however, in the degree to which EBTs are available in public mental health settings (Bruns & Hoagwood, 2008)—the service sector in which most children, including those in foster care, receive services.
In general, EBTs that offer a good fit for mental health needs of children in foster care include interventions addressing behavioral difficulties (e.g., Parent-Child Interaction Therapy, Triple P, Incredible Years)—given their prevalence (Garland et al., 2000)—and trauma exposure and resulting sequelae. Trauma-focused Cognitive Behavioral Therapy (TF-CBT; Cohen et al., 2006), a well-established EBT, provides a good fit for children in foster care as it is designed to address behavioral problems and trauma-related symptoms. TF-CBT includes individual sessions with children and non-offending caregivers and conjoint child-caregiver sessions delivered over approximately 12–24 sessions focused on psychoeducation, skill building (e.g., relaxation), exposure, and cognitive work (for adaptations/guidelines on including offending caregivers in TF-CBT, see Dorsey & Deblinger, 2012; Runyon & Deblinger, 2013).
To date, the empirical base for TF-CBT includes over 14 randomized controlled trials (RCTs). Efficacy data exists for preschool, school-aged, and adolescent male and female children (for reviews, seeDorsey, Briggs, & Woods, 2011; Silverman et al., 2008). Studies have included a substantial percentage of African American children, with no significant differences by ethnicity (e.g., Cohen, Deblinger, Mannarino, & Steer, 2004). Although initial studies focused on sexually abused children (e.g., Cohen et al., 2004; Cohen & Mannarino, 1996; Deblinger, Lippmann, & Steer, 1996), recent RCTs, quasi-experimental trials, and open trials (e.g., CATS Consortium, 2007; Cohen, Mannarino, & Iyengar, 2011; Jaycox et al., 2010) include children exposed to other diverse traumatic event types (e.g., traumatic death, domestic violence, natural disasters).
For TF-CBT to be most effective, research suggests caregivers need to be involved in treatment (Deblinger, Mannarino, Cohen, Runyon, & Steer, 2011). Deblinger, Mannarino, Cohen, and Steer (2006) found that while posttraumatic stress (PTS) symptoms improved even without parental involvement, behavior problems did not. Caregivers help promote optimal treatment outcomes by reinforcing both skills (e.g., affect modulation) and psychoeducation about traumatic events, and by implementing behavior management in the home environment. However, engaging caregivers—and potentially foster parent caregivers—in treatment can be challenging. To our knowledge, empirical studies examining rates of foster parent engagement in treatment are not available. A recent open trial examining TF-CBT with children in foster care (Weiner, Schneider, & Lyons, 2009) found that treatment completion was linked to foster parent involvement. Those who received 11 or more sessions—defined as an active dose of treatment—had significant reductions in PTS symptoms (Weiner et al., 2009). However, the children who completed treatment or were still in treatment at the end of the study had high rates (76–79%) of foster parent involvement (Northwestern University, 2008). In comparison, for the nearly one third of children who dropped out of treatment, only 10% had a foster parent involved.
Engagement challenges are not unique to the foster parent population. Rates of engagement in community mental health treatment can be low for all families. Less than half of families attend the first scheduled visit (Harrison, McKay, & Bannon, 2004) and less than 10% remain in treatment after 3 months, with more than two-thirds dropping out within seven sessions (McKay, Harrison, Gonzales, Kim, & Quintana, 2002; Miller, Southam-Gerow, & Allin, 2008). Engaging foster parents is likely as important as engaging biological or adoptive families. In foster care, learning and implementing behavior management is critical, given the high rates of behavior problems and the negative association between behavior problems and placement stability, reunification, and adoption (James et al., 2004). In general, foster parents are inadequately trained and prepared for the behavioral problems of children in foster care (Dorsey et al., 2008). Interventions that build behavior management skills have stabilized placements and increased “positive exits” from foster care (e.g., reunification, adoption; Price, Chamberlain, Landsverk, & Reid, 2009), with better outcomes for children in their care when foster parents attend treatment and are active participants (DeGarmo, Chamberlain, Leve, & Price, 2009).
In response to these challenges, engagement interventions have been developed. Three relatively recent reviews (Becker et al., 2013; Ingoldsby, 2010; Lindsey et al., 2013) describe common elements of engagement interventions from over 40 RCTs. Studies have tested the combination of EBTs and specialized engagement strategies for a range of populations, including Latino families, child-welfare involved parents, and parents of children with behavioral disorders (e.g., Chaffin, Funderburk, Bard, Valle, & Gurwitch, 2011; Nock & Kazdin, 2005; Szapocznik, Dantisteban, Rio, Perez-Vidal, & Santisteban, 1989). These studies have demonstrated higher rates of engagement with the inclusion of a specific engagement-focused intervention, and in turn, better clinical outcomes, given that participants receive a higher dose of treatment and/or are more likely to complete treatment. EBTs are associated with positive outcomes for a range of child mental health problems, but only when children and families attend treatment and receive a sufficient dose of the EBT. In addition to achieving better clinical outcomes by leading to receipt of a higher dose of treatment, some studies that included engagement interventions have demonstrated further clinical benefit, potentially because they led to increased motivation for participants to actively participate in treatment (Chaffin et al., 2011).
Research on engagement (McKay, Pennington, Lynn, & McCadam, 2001) highlights both perceptual (e.g., attitudes about mental health treatment) and concrete barriers (e.g., transportation challenges). In one study, perceptual barriers emerged as a primary predictive factor (McKay, Stoewe, McCadam, & Gonzales, 1998). McKay and colleagues developed an engagement intervention with a strong perceptual focus, implemented during the first telephone contact with the caregiver and during the first in-person visit (McKay & Bannon, 2004). McKay’s work builds on Szapocznik’s Brief Strategic Family Therapy engagement strategies (Szapocznik et al., 1989) in that the first telephone contact is conceptualized as the beginning of treatment and not merely as a logistics-focused encounter (e.g., scheduling).
McKay’s engagement intervention, now a manualized intervention named Training Intervention for the Engagement of Families (http://www.tiesengagement.com/) may have relevance for addressing engagement challenges with foster parents. In the first phone call, McKay’s engagement intervention involves: 1) direct discussion of perceptual barriers, including prior negative experiences with mental health treatment and lack of confidence in treatment effectiveness, and 2) identification of the caregiver’s own greatest concern about the child, which may or may not overlap with the referral reason. The clinician also elicits potential concrete barriers (e.g., transportation) and assists with problem-solving. During the first in-person visit, content from the phone call is revisited; the clinician provides and discusses a tangible resource in response to a specific caregiver-identified need (e.g., sleep problems handout) and links each intake activity to treatment.
The telephone engagement intervention alone resulted in better attendance at the first visit (McKay, Nudelman, McCadam, & Gonzales, 1996); delivery of the first visit engagement intervention improved attendance at the second appointment and treatment retention (i.e., 7.1 vs. 5.3 sessions attended). The combined intervention was most effective: families were more likely to attend the initial appointment, stay in treatment, and less likely to ‘no show’ (McKay et al., 1998). One study examined the combined engagement intervention with trauma treatments (including TF-CBT): 75% attended eight or more sessions (Hoagwood et al., 2006).
McKay’s engagement intervention holds promise, but to date it has not been tested with the foster care population. The goal of the current study was to examine the impact of supplementing TF-CBT with McKay’s evidence-based engagement strategies. Primary outcomes of interest were initial engagement (i.e., attendance at the first session), retention in treatment, and treatment completion. An additional exploratory goal was to gain a preliminary examination of the effectiveness of TF-CBT with children in foster care, given the limited research on EBTs with youth in foster care, and on TF-CBT specifically.
Method
Study Overview
Data come from a small-scale RCT of standard delivery TF-CBT compared to TF-CBT plus evidence-based engagement strategies. The study was conducted in a large metropolitan area in Washington (WA) State between 2008 and 2011. Institutional Review Board approval was obtained from the Washington State IRB.
Child and Adolescent Participants
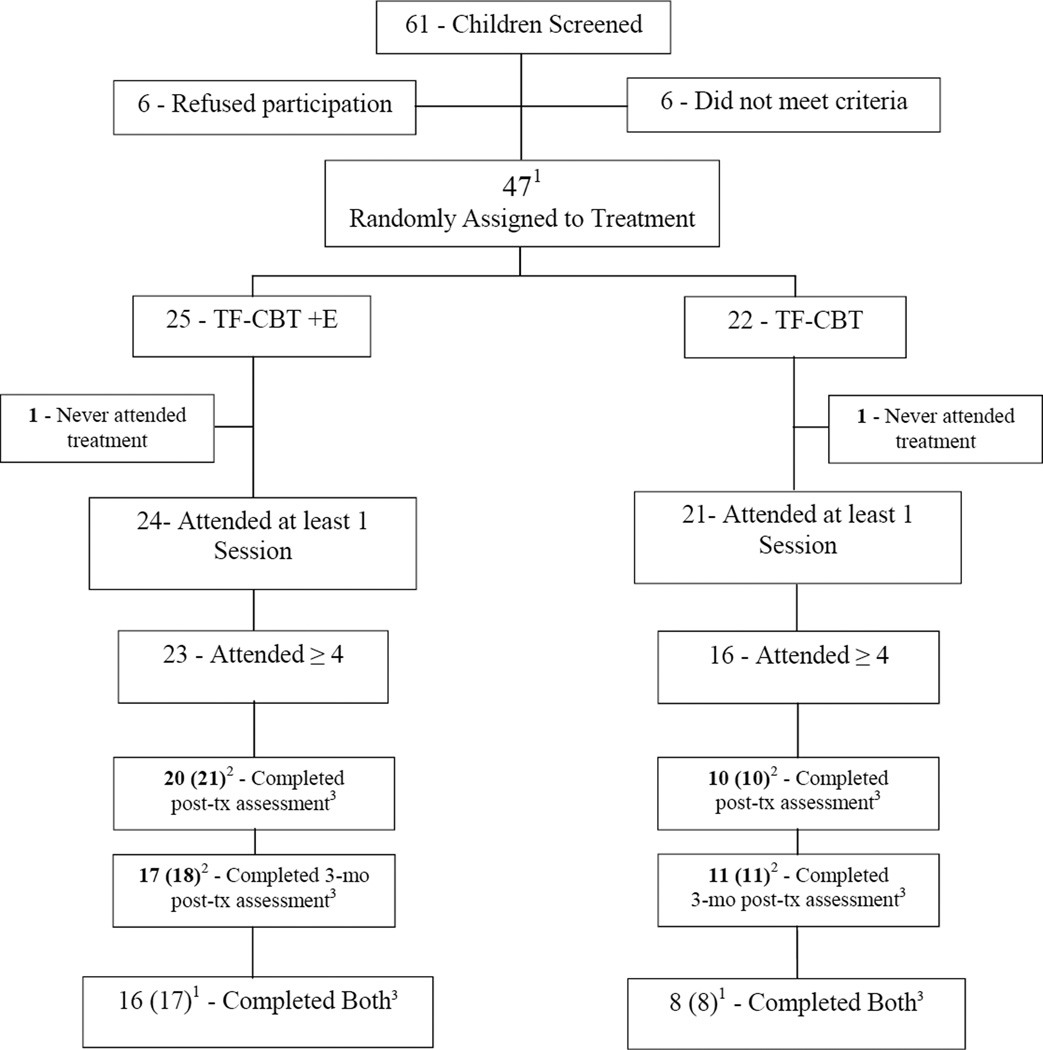
Participants were 47 children and adolescents between the ages of 6 and 15 and one of their foster parents (see Table 1). Foster parents include traditional foster parents (i.e., non-relative), kinship caregivers (i.e., relative placements), and suitable adult placements (WA-specific classification for non-licensed, non-relative placements). All participants were referred by child welfare social workers from offices in the participating region, who were asked to refer youth on their caseload with trauma histories who might benefit from TF-CBT. Prior to study initiation, research staff provided presentations to child welfare office staff on the study, trauma impact, and TF-CBT. To encourage broad, caseload-representative referrals, the study team served as a resource to provide TF-CBT treatment referral information for any youth on a social worker’s caseload, whether or not the child was eligible for the study. To be eligible for the study, children: 1) resided in their current placement for one month or more; 2) experienced one or more traumatic event(s); and 3) following procedures in prior TF-CBT studies, had one symptom from each of the Diagnostic and Statistical Manual-IV Text Revised (DSM-IV TR; American Psychiatric Association, 2000) symptom criteria for PTSD (i.e., avoidance, re-experiencing, hyperarousal), as well as one additional symptom from any area. The CONSORT diagram in Figure 1 shows participants screened, enrolled in the study, and who participated in TF-CBT.
Table 1.
Study Sample: Demographics and Baseline Characteristics
| Engagement | Standard | Total | |
| Youth | n = 25 | n = 22 | N = 47 |
| Age, M (SD) | 9.52 (2.5) | 9.64 (3.2) | 9.57 (2.8) |
| Female, n (%) | 15 (60%) | 11 (50%) | 26 (55.3%) |
| Multiracial, n (%) | 18 (72%) | 7 (31.8%) | 25 (53.2%) |
| Caucasian, n (%) | 3 (12%) | 8 (36.4%) | 11 (23.4%) |
| African American, n (%) | 3 (12%) | 6 (27.3%) | 9 (19.1%) |
| Native American, n (%) | 1 (4%) | 0 (0%) | 1 (2.1%) |
| Asian, n (%) | 0 (0%) | 1 (4.5%) | 1 (2.1%) |
| Traditional foster care, n (%) | 18 (72%) | 11 (50%) | 29 (61.7%) |
| Kinship care, n (%) | 6 (24%) | 10 (45.5%) | 16 (34%) |
| Suitable adult/fictive kin, n (%) | 1 (4%) | 1 (4.5%) | 2 (4.3%) |
| Baseline Caregiver | |||
| Age, M (SD) | 45.3 (9.9) | 47.5 (12.4) | 46.3 (11.1) |
| Female, n (%) | 22 (88%) | 19 (86.4%) | 41 (85.2%) |
| Multiracial, n (%) | 5 (20%) | 1 (4.5%) | 6 (12.8%) |
| Caucasian, n (%) | 16 (64%) | 13 (59.1%) | 29 (61.7%) |
| African American, n (%) | 3 (12%) | 8 (36.4%) | 11 (23.4%) |
| Hispanic/Latino/a, n (%) | 1 (4%) | 0 (0%) | 1 (2.1%) |
| Incidence of Trauma Type | Engagement | Standard | Total |
| Foster parent endorsed… | n = 25 | n = 22 | N = 47 |
| Cumulative number of trauma exposure experienced, M (SD) | 2.6 (.9) | 3.2 (1.6) | 2.9 (1.3) |
| Accident/Natural Disaster | 0 (0%) | 4 (18.2%) | 4 (8.5) |
| Physical abuse | 13 (52%) | 14 (63.6%) | 27 (57.4%) |
| Witnessing domestic violence | 22 (88%) | 17 (77.3%) | 39 (83%) |
| Witnessing or experiencing community violence | 5 (20%) | 7 (31.8%) | 12 (25.5%) |
| Sexual abuse | 2 (8%) | 8 (36.4%) | 10 (21.3%) |
| Violent Death/Injury | 10 (40%) | 6 (27.3%) | 16 (34%) |
| Painful/scary medical treatment | 6 (24%) | 1 (4.5%) | 7 (14.9%) |
| Other | 8 (32%) | 13 (59.1%) | 21 (44.7%) |
Figure 1.
CONSORT DIAGRAM
149 child-parent dyads were randomly assigned to treatment, two standard condition youth were ineligible within a few days of randomization (one placed in group home, one ran away)
2Child (Parent)
3Two children in the standard condition and one engagement condition were still in active treatment at the end of the study.
Procedures
Washington State procedures were followed for enrolling children in foster care into the study. If legal custody was held by the state, prior to study referral social workers first notified the biological parent(s) in writing and provided 10 days for parents to notify the social worker that they did not want their child to participate in the study. If legal custody was held by biological/adoptive parent(s), the social worker asked for permission to provide the contact information of the parent(s) to the study team, and the study team contacted the parent(s) to obtain permission for child participation. For children for whom biological parents had no objections (state custody) or provided permission (parental custody), the social worker then made the first contact with the foster parent to explain the study and ask for permission to refer the child and foster parent for potential study participation. Research staff contacted the child’s foster parent by telephone to confirm basic eligibility (i.e., age, placement duration) prior to scheduling an in-person meeting to obtain informed consent and child assent, screen for clinical eligibility (trauma exposure and PTSD symptoms), and if eligible, administer study baseline questionnaires. Children could meet clinical eligibility by either child or foster parent report on the PTSD assessment measure (see Measures section). Consent forms clearly stated that the foster parent did not have to be willing to participate in treatment, only the study.
Clinicians
Clinicians (N = 16) in five of seven mental health agencies approached agreed to participate. Clinicians were randomized to TF-CBT Standard or TF-CBT plus Engagement within each participating agency (e.g., condition nested within agency). Clinicians were primarily female (87.5%), Caucasian (62.5%), and in their mid-thirties (M = 36.2; SD = 6.8), with Master’s degrees, predominantly in social work or counseling (75.1%). They had approximately five years of experience (M = 4.7; SD = 2.7) and high caseloads (M = 51.1; SD = 17). Clinicians did not receive incentives for participation; agencies received approximately $300 of resources for TF-CBT (e.g. books, games) as appreciation for participation. Prior to the RCT, clinicians in the Engagement condition participated in a small pilot of TF-CBT plus evidence-based engagement strategies to test and better tailor engagement strategies to foster parents (see MANUSCRIPT BLINDED for details).
Clinician Training
Prior to the study, all clinicians had 2 days of in-person TF-CBT training by the first author (an approved TF-CBT trainer) or another approved TF-CBT trainer as part of a State TF-CBT Initiative. Throughout the study, all clinicians received weekly group TF-CBT consultation by one of three TF-CBT experts (in agency groups, in-person and via telephone, alternate weeks). Clinicians who were randomized to the Engagement condition participated in an additional 6-hour engagement procedures training that included didactics and modeling of the telephone and first visit engagement interventions, followed by clinician role-play of both interventions with feedback from the trainer and peer trainees (see http://www.tiesengagement.com/ for more information on the training).
Fidelity Monitoring
Trauma-focused CBT
Following procedures in prior TF-CBT trials, TF-CBT fidelity was monitored via audio review. Clinicians received direct feedback, written and oral, on their implementation of TF-CBT. Feedback was provided prior to the next scheduled session, except in rare cases of delayed audio file receipt. Although not quantitatively assessed, clinicians exhibited high fidelity to the TF-CBT model based on this expert review, likely due to the support provided by weekly group consultation and regular audiotape review feedback.
Engagement Fidelity
For each case assigned to an Engagement clinician, one of the authors provided a 15–30 minute telephone booster, which included didactic review and role play, prior to both the telephone and first visit interventions. Fidelity was monitored via clinician self-report on a checklist for each intervention. As the engagement intervention was the randomized aspect of the RCT (i.e., all participants received TF-CBT; only half received the engagement intervention), a quantitative measure of fidelity was used. Clinicians reported: a) whether they completed each engagement component (four for the phone call; four for the first visit) and b) skill in delivering each component (rating from 1 “poor” to 4 “excellent”). Fidelity data were missing for 5 of 24 cases for the telephone intervention (20%) and for 8 of 23 cases for the first visit intervention (34%). For the available cases, adherence was high for both the telephone and first visit intervention (M = 3.7; M = 3.94, respectively, out of a 4-point scale). Therapists also rated reasonably high levels of skill (M = 14.27; M = 13.87), corresponding with a rating of good to excellent.
Data Collection
Data come from foster parents, children and adolescents, and clinicians. Foster parents and children ages 7 and older (children age 6 did not complete self-report measures) were assessed at baseline, 1 month into treatment (early assessment of therapuetic alliance and satisfaction), end of treatment, and 3 months post-treatment. All interviews with youth were conducted in-person. Data were collected via in-person or telephone interviews with foster parents. At the 1-month interview, if the child was 6 years old, foster parents were given a choice to complete the short 1-month interview (two measures only) by telephone or in-person. All data from clinicians were collected via secure web-based surveys.
Measures
Attendance Data
Clinicians reported participant attendance weekly: 1) if an appointment was scheduled or not and 2) whether the child and foster parent a) attended, b) cancelled, or c) no-showed for the scheduled appointment.
Posttraumatic Stress Symptoms (PTS)
Posttraumatic stress symptoms were assessed by foster parent and youth report using the UCLA Posttraumatic Stress Disorder-Reaction Index (UCLA PTSD-RI; Pynoos, Rodriguez, Steinberg, Stuber, & Frederick, 1998). The UCLA PTSD-RI assesses trauma exposure (12 possible types) and PTS. Twenty items assess PTS criteria B (Re-experiencing), C (Avoidance), and D (Increased Arousal) per the DSM-IV-TR (American Psychiatric Association, 2000). Scores 15–20 are considered to indicate mild PTS, 21–37 moderate PTS, and 38 and above clinical PTS. The measure has acceptable psychometric properties (Steinberg, Brymer, Decker, & Pynoos, 2004; Steinberg et al., 2013).
Satisfaction with Treatment
We administered a revised version of the Client Satisfaction Questionnaire (CSQ-8; Larsen, Attkisson, Hargreaves, & Nguyen, 1979) used in prior TF-CBT studies at 1-month and at end of treatment to foster parents and youth. The CSQ-8 is an eight-item measure that evaluates client satisfaction with clinical services. The CSQ-8 has acceptable psychometric properties, with alpha coefficients ranging from .83 to .93 (Attkisson & Zwick, 1982). Higher scores indicate higher satisfaction (range: 8–32); with scores between 8–20, 21–26, and 27–32 viewed as low, medium, and high levels of satisfaction, respectively (Larsen et al., 1979).
Treatment Alliance
Two subscales from an existing, adapted version (from MH55327, NIMH-funded; McKay, PI) of the Tolan Process Measures (Tolan, Hanish, McKay, & Dickey, 2002) assessed foster parent and youth perspectives on alliance at 1-month and end of treatment. The two subscales included Relationship with Interventionist (Parent: 10 items; Child: 8 items) and Satisfaction with Program (Parent: 13 items [one original item excluded]; Child: 8 items). For child report, items were re-worded to read “foster parents” instead of “family.” Higher scores indicate better alliance.
Depression
The total score on the 27-item Children’s Depression Inventory (CDI; Kovacs, 1992) was used to assess depressive symptoms via child report. A total score of 19 or higher is considered clinically significant. The CDI has excellent psychometric properties, with internal consistency coefficients ranging from .71 to .87 (Hodges, 1990).
Emotional and Behavioral Difficulties
The Internalizing and Externalizing Scales of the Child Behavior Checklist School-aged version (CBCL; Achenbach, 1991; Achenbach & Rescorla, 2001), completed by the foster parent, were used to assess overall emotional and behavioral difficulties. The measure has excellent psychometric properties. T-scores 60–63 are considered borderline and 64 and over are considered clinically significant.
Child Strengths
The Overall Strength Score from the 52-item Behavioral and Emotional Rating Scale (BERS) 2nd Edition (Epstein & Sharma, 1998), completed by foster parents, assessed child strengths. The BERS has strong psychometric properties and coefficient alphas above .80 for all subscales (Epstein, Harniss, & Pearson, 1999; Epstein, Ryser, & Pearson, 2002). Higher scores indicated greater strength, with scores of 115 and higher suggesting greater than normal strength, and scores 85 and lower suggesting lower than normal strength (Buckley & Epstein, 2004).
Results
Analyses
Preliminary Analyses
The study involves nested data (i.e., time within clients, clients within therapists, therapists within agencies). To examine the impact of nesting, we examined intraclass correlation coefficients (ICCs) at the therapist and agency levels, both of which were very low (.0001 – .0009) for all major outcomes by parent and child report. Additionally, comparisons of model goodness-of-fit among two- (i.e., without therapist or agency effects), three-, and four-level models were not statistically significant for any outcomes. For parsimony, data were disaggregated and therapist and agency effects were not included in models, as findings did not differ across models including, and not including, nesting.
Primary Analyses
Primary analyses examining the relation between study condition and a variety of treatment engagement variables were run using Chi-square tests for categorical data and independent-sample t-tests for continuous variables. To more rigorously examine patterns of treatment retention between conditions, competing risks Cox Regression analyses were run predicting termination via successful (i.e., treatment completion) or premature end of treatment and number of sessions until termination. This approach allows the inclusion of “censored” cases, that is, cases that did not have the event (e.g., termination) occur by the end of the study (Singer & Willett, 2003; Southern et al., 2006; Tai, Machin, White, & Gebski, 2001). All primary analyses are Intent to Treat (N = 47), with some exceptions, when appropriate to analysis question.
Exploratory Analyses
Two-level Hierarchical Linear Models (HLM) were run with time (months) nested within client to explore change in clinical outcomes, given limited (only one other study) research on TF-CBT and other EBTs specifically with youth in foster care. There was sufficient power for estimation, indicated by the fact that no model required more than 18 iterations to converge, reliability estimates were greater than .4 for all and .5 for most, and no standard errors were inflated. These analyses were conducted with a subsample (n = 37) who attended four or more sessions of TF-CBT and who were not still in treatment at the end of the study (excludes n = 3). Meta-analyses indicate that three or more CBT sessions result in some clinical improvement (Barkham, Shapiro, Hardy, & Rees, 1999), and this standard has been used in past TF-CBT efficacy trials (e.g., Deblinger et al., 2011). For this effectiveness trial, four sessions were used because in public mental health (compared to efficacy trials), the first session was predominantly an intake with TF-CBT begun in session two (allowing for a three TF-CBT session dose). Treatment duration for TF-CBT varies based on individual child need; therefore, length of time until end of treatment varied by client. To account for variation in time points, rates of change were modeled as change by month, with the intercept set at baseline and freely varying time slopes (Singer & Willett, 2003). Missing data were estimated using Full Maximum Likelihood.
Primary Analyses
Attendance
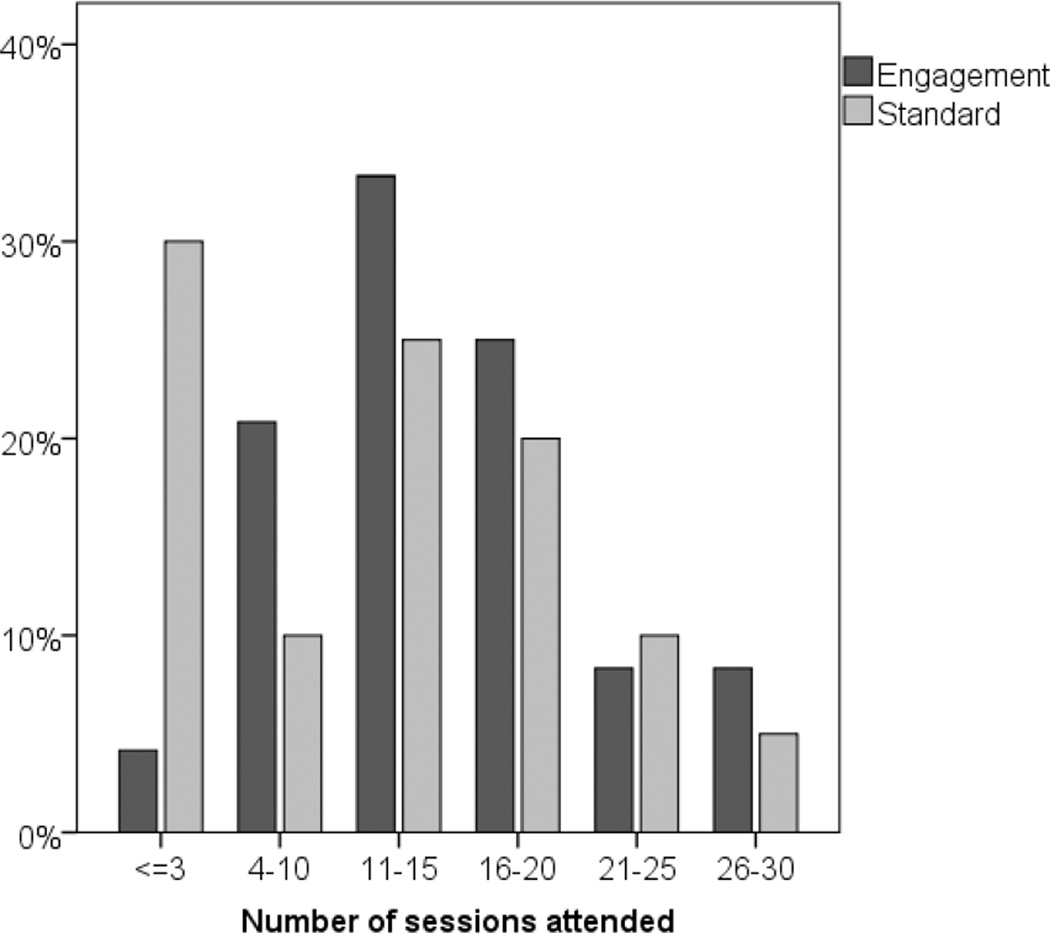
As shown in Table 2, there were no statistically significant differences between study conditions for the percentage of caregivers and youth who: a) attended the first scheduled in-person appointment (80% vs. 77.3%, for Engagement and Standard, respectively); b) attended one or more TF-CBT sessions (96% vs. 95.5%); or c) had at least one treatment cancellation or no-show appointment during the first month of treatment, although this trended in the direction of the Engagement condition (29.2% vs. 52.4%). For the subgroup (n = 42) who attended at least one session of TF-CBT (excludes n = 2) and completed treatment successfully or terminated prior to completion (excludes n = 3), there were no significant differences in total number of sessions attended over the course of treatment, although findings trended in the direction of the Engagement condition (M = 15.0 vs. 12.3, for Engagement and Standard, respectively). However, a significantly higher percentage of youth in the Engagement condition attended at least four sessions, and thus received an active dose of TF-CBT, compared to youth in the Standard condition (96.0% vs. 72.7%; see Figure 2).
Table 2.
Treatment Engagement and Retention Outcomes
| Treatment condition | ||||
|---|---|---|---|---|
| Engagement (n=25) % (n) |
Standard (n=22) % (n) |
Chi-square (df) | p | |
| Showed to first scheduled intake | 80.0 (20) | 77.3 (17) | .052 (1) | .820 |
| Attended one or more sessions | 96.0 (24) | 95.5 (21) | .009 (1) | .926 |
| Attended four or more sessions | 96.0 (24) | 72.7 (16) | 5.000 (1) | .025* |
| Treatment completed or attended 111 or more sessions2 | 80 (20) | 54.5 (12) | 3.489 (1) | .062 |
| Any treatment cancellations or no-shows between intake and one month | 29.2 (7) | 52.4 (11) | 2.515 (1) | .113 |
| Treatment status, end of study | 14.373 (6) | .013* | ||
| Completed | 80.0 (20) | 40.9 (9) | ||
| Drop out | 0 (0) | 27.3 (6) | ||
| Placement disruption related | 12.0 (3) | 4.5 (1) | ||
| Declined to participate in treatment | 4.0 (1) | 4.5 (1) | ||
| Still in treatment | 4.0 (1) | 9.1 (2) | ||
| Other treatment recommended | 0 (0) | 13.6 (3) | ||
| Mean (sd) | Mean (sd) | t (df) | p | |
| Total number of sessions attended2,3 | 15.0 (6.0) | 12.3 (8.0) | −1.65 (44) | .106 |
p < .05
Figure 2.
Session Attendance by Study Condition
Treatment Satisfaction and Therapeutic Alliance
There were no significant differences between conditions at 1-month or end of treatment on satisfaction with treatment or therapeutic alliance by either child or caregiver report (analyses available on request).
Treatment Completion Status
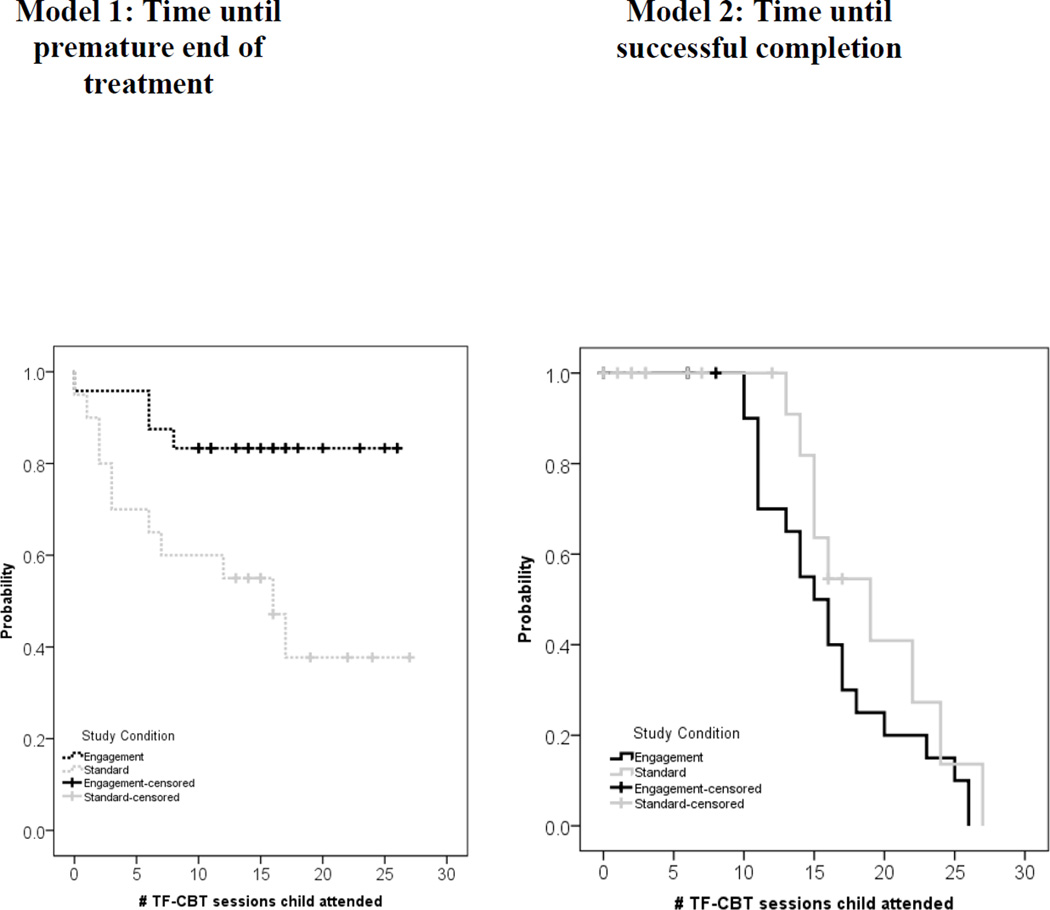
Treatment status at the end of the study was significantly different across the two conditions, excluding only the three youth still in treatment at the end of the study (n = 44). In the Engagement condition, 80% completed treatment, compared to only 40.9% in the Standard condition (see Table 2). Differences in treatment retention and completion were not accounted for by placement type (e.g., traditional vs., kinship). For the competing-risks time-to-event analysis, which included the full sample of 47, Cox regression models comparing study conditions were run with varying events of interest as dependent variables: Model 1 examined treatment ending prematurely, censoring children who successfully completed treatment. Model 2 examined successful treatment completion, censoring children who had a premature end of treatment (see Figure 3). The three children still in active treatment were included as censored cases in all models.
Figure 3.
Cox Regression Models of Premature End of Treatment and Treatment Completion
Findings from the event-specific models and a global model indicated that study condition was significantly different by model (−2 Log Likelihood global – event specific difference χ2 (1) = 7.437, p < .01; generalized Wald χ2(1) = 19.55, p < .001). Study condition was significant for premature end of treatment (Model 1; β = −1.323, p = .024), but not for successful treatment completion (Model 2; β = .518, HR = 1.679, p = .217). Youth in the Engagement condition were significantly less likely to have a premature end of treatment, and if they did end treatment prematurely, they were retained for more sessions than those in the Standard condition.
Exploratory Analyses: TF-CBT Effectiveness
We examined treatment outcomes for participants who attended at least four sessions and were not still in active treatment at the end of the study (n = 37; see Figure 1), resulting in ten participants excluded.
Missing Data
All foster parents who attended four or more sessions (n = 37) had at least one valid post-baseline interview—33 (89.2%) at end of treatment and 29 (78.4%) at the 3-month follow-up. All 29 youth 7 years and older had at least one valid post-baseline interview—24 (85.7%) at end of treatment and 23 (82.1%) at the 3-month. Missing interviews at either timepoint for parents or youth were not statistically related to study condition, baseline outcome measures (e.g., PTS severity score), or child’s sex or race/ethnicity.
Effectiveness Analyses
Two-level HLMs were run for all foster parents (n = 37) and children (n = 29) with at least one follow-up (e.g., end of treatment or 3 months post-treatment), with time nested by client. There were no significant differences on any of the clinical outcomes by study condition (analyses available by request). Therefore, these exploratory analyses include the combined sample of participants (i.e., both TF-CBT Engagement and TF-CBT Standard), to provide the best preliminary estimates of TF-CBT effectiveness with children and adolescents in foster care. All outcome measures indicated statistically significant improvement over time (see Tables 3a & 3b). Per month, parents reported estimated average decreases of 1.30 in PTS severity, .87 in CBCL internalizing t-scores, .40 in CBCL externalizing scores, and 1.20 increases in BERS overall strength scores. Children reported significant decreases in PTSD severity of 1.45 and CDI total scores of .37 per month.
Table 3.
Exploratory Analyses: Clinical Outcomes for the Combined Sample
| a | |||||||
|---|---|---|---|---|---|---|---|
| Baseline1 | End of treatment |
3-month post treatment |
|||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| PTSD Severity Score2 | |||||||
| Parent-rated | 33 | 28.57 (8.85) | 30 | 18.87 (10.59) | 27 | 17.97 (12.83) | |
| Child-rated | 28 | 30.45 (11.69) | 27 | 15.59 (11.81) | 21 | 13.29 (10.98) | |
| CBCL | |||||||
| Internalizing t-score | 37 | 66.51 (7.79) | 33 | 60.73 (8.18) | 28 | 58.25 (9.86) | |
| Externalizing t-score | 37 | 63.30 (12.90) | 32 | 61.81 (9.71) | 28 | 60.61 (10.74) | |
| CDI Total | 27 | 12.01 (7.70) | 25 | 7.12 (6.76) | 24 | 7.00 (5.89) | |
| BERS (Parent) overall strength score | 35 | 84.74 (12.73) | 31 | 92.13 (16.31) | 29 | 94.66 (19.24) | |
| N | n (%) | N | n (%) | N | n (%) | ||
| b. | ||||||
|---|---|---|---|---|---|---|
| n | Intercept3 | SE | Slope4 | SE | p | |
| PTSD Severity Score | ||||||
| Parent-rated | 37 | 27.73 | 1.46 | −1.30 | <0.001 | |
| Child-rated | 29 | 28.97 | 2.22 | −1.56 | 0.28 | <0.001 |
| CBCL | ||||||
| Internalizing t-score | 37 | 66.17 | 1.20 | −0.87 | 0.21 | <0.001 |
| Externalizing t-score | 37 | 63.17 | 2.09 | −0.40 | 0.17 | 0.020 |
| CDI Total | 29 | 11.12 | 1.41 | −0.42 | 0.16 | 0.010 |
| BERS (Parent) overall strength score | 37 | 84.73 | 2.07 | 1.2 | 0.30 | <0.001 |
Includes participants with a valid score at baseline and at least one follow-up point
Scores between 15–20 are considered mild, 21–37 moderate, and 38 and above as high PTS symptoms
The intercept is an estimate of the average scale score at baseline
The slope is an estimate of the average rate of change in the scale score per month. All slopes were permitted to freely vary
Discussion
In this small study, a brief engagement intervention made a significant difference in improving treatment retention and completion for children and their foster parents involved in TF-CBT. Those who received the engagement intervention were significantly more likely to receive an active dose of TF-CBT (i.e., attend four or more sessions) and were less likely to have a premature treatment exit. Across the two conditions, however, no differences were found in attendance at the first scheduled session or in the proportion of no-show or cancelled sessions. The engagement intervention also did not appear to impact the therapeutic relationship or satisfaction with therapy, nor, in our exploratory analyses, did the engagement intervention iteslf relate to therapy outcomes. For the combined sample, collapsing across both conditions, children who received at least four sessions of TF-CBT had significant decreases in PTS and other emotional and behavioral symptoms, reflecting positive outcomes in prior TF-CBT studies. These analyses, while exploratory, underline the importance of engagement—children and youth in foster care who received TF-CBT appeared to gain some benefit, although more rigorous examinations will be required to determine if clinical improvement was related to receipt of TF-CBT.
In the continuing environment of budgetary limitations, low-cost, potentially high-impact interventions like McKay’s may be particularly attractive. The McKay engagement intervention examined in this study is relatively brief in nature, adding only minimal time to the first phone contact and to the first visit (e.g., less than 15 minutes per contact). In addition, in comparison to concrete barrier interventions, which may require restructuring of clinic procedures (e.g., offering later appointment times, providing on-site childcare) or additional funding (e.g. for transportation, childcare), perceptual interventions involve only restructuring goals and content of early interactions. Our findings reflect those of other brief engagement interventions (Nock & Kazdin, 2005), which have been found to have a positive impact despite brevity. In McKay et al.’s (1998) work, the inclusion of the engagement intervention resulted in families attending approximately two additional sessions, which mirrors our findings of a mean increase of nearly three additional sessions; although for our study, this increase was not statistically significant. In our study, the greatest impact involved keeping families in treatment through four sessions (i.e., an active dose of TF-CBT) and offering protection against premature treatment termination. Given other findings that TF-CBT is effective but engagement can be challenging in some settings (e.g., Jaycox et al., 2010), these results are promising.
Interestingly, in comparison to prior studies (e.g., McKay et al., 1996), for this foster care-focused study, the engagement intervention appeared to have little impact on initial attendance, in that almost all foster parents and youth attended the first scheduled session. Contrasting findings may be due to the specific study population. In some cases, courts mandate treatment for youth in foster care, and therefore initial engagement (first session) may be more of a requirement for foster parents, such that the engagement intervention has less of an impact at that point. Alternatively, contrasting findings may be due to the small sample size or differences in study procedures. In our study, youth referred by child welfare workers had to be screened for trauma exposure and symptoms of PTS to determine TF-CBT appropriateness, and therefore all children and foster parents had at least one prior contact with a research interviewer. Although more research is needed, potentially, this interaction was sufficiently ‘engaging’ to increase attendance at the initial session. In McKay’s studies, attendance and retention were tested at the clinic-level (for a wide range of treatment needs) and did not require an additional, upfront study contact. Regardless, for this sample engagement differences emerged subsequent to the initial session. Although our sample was small, there were few exclusionary criteria and TF-CBT was provided by community-based clinicians under usual care conditions (e.g., high caseloads). Therefore, findings likely are generalizable to the broader foster care population.
Exploratory Analyses: Treatment Effectiveness
Exploratory analyses suggest that receiving the engagement intervention did not relate to treatment effectiveness beyond being associated with higher treatment dose and treatment retention. In the literature, some studies showed improved outcomes of interest (i.e., child physical abuse recidivism) when specific engagement procedures were included (Chaffin et al., 2011), beyond that conferred by receiving a higher dose of treatment or completing treatment. Other studies, like ours, found that the engagement intervention led to higher treatment dose and retention, which, in turn, has been associated with more positive outcomes (Briones, Robbins, & Szapocznik, 2008).
This study is only one of two to date examining TF-CBT specifically with youth in foster care. Looking at children and adolescents in both conditions, findings suggest that TF-CBT may be beneficial for this population based on both child and foster parent report of significantly reduced PTS, depression, internalizing and externalizing symptoms, and increased strengths. However, as the study was uncontrolled, changes in symptoms over time may not be attributable only to the intervention and may reflect natural progression of symptoms over time. Further research should examine outcomes for the foster care population using more rigorous designs (e.g., RCT) with larger sample sizes.
Child Welfare Engagement Challenges: Not Limited Only to Foster Parents
It should be noted that obtaining referrals to TF-CBT was challenging, even though the treatment was 1) fully supported by Medicaid, 2) a good fit for the population (i.e., given high rates of trauma exposure), and 3) available in geographically disparate locations. Despite repeated, varied contacts and offers to assist in either linking potential referrals to TF-CBT (via the study or outside the study) or to another EBT, often there was little caseworker follow up. Child welfare social workers have a wide-ranging span of job duties, of which addressing child mental health needs is only one (Stiffman, Pescosolido, & Cabassa, 2004). Their critical role as brokers for mental health services is an important and often overlooked factor (Dorsey, Kerns, Trupin, Conover, & Berliner, 2012).
Engagement Challenges: Placement Disruption
A focus on engaging foster parents is important, as demonstrated by this trial, but building connections between mental health and child welfare is also critical for effectively addressing mental health needs of youth in foster care. Although not a primary focus of the study, we observed unique/substantial engagement challenges subsequent to a child or adolescent’s placement disruption. In both conditions, once placement disruption occurred, it was particularly challenging to re-engage the child in treatment, with engagement failures nearly equivalent across the study conditions. Following placement disruption, clinicians attempted to make contact with the new foster parent to continue TF-CBT but encountered challenges at a variety of points (i.e., initial contact, first visit, ongoing visits). Substantial geographic changes subsequent to placement changes (i.e., child placed outside of the county) also contributed to engagement challenges. More attention needs to be paid to mental health treatment continuity, among other pressing challenges, when placement disruption occurs.
Limitations
The study has a number of limitations within which findings should be considered. First among these is the small sample size. The study was designed to test the feasibility of combining TF-CBT with evidence-based engagement strategies and to examine any potential benefit for engagement and retention to inform a larger trial. Therefore, given the feasibility goal, participant enrollment was limited. Second, because of the specialized nature of TF-CBT, a treatment for children with trauma exposure and trauma-related sequelae, children were screened by our research team prior to their contact with their TF-CBT clinician, which may have impacted their likelihood of attending the first session. Third, since we conducted an exploratory examination of clinical outcomes without a control group, improvements may simply reflect change over time. Despite these limitations, this study is one of few examining EBTs with the foster care population, potentially the only one experimentally examining engagement with this population, and one of a limited but growing number of TF-CBT studies using community-based clinicians.
Conclusions
Short-term EBTs for children and adolescents in foster care hold promise for improving outcomes, particularly when they include strategies for involving caregivers in treatment. However, too many youth in foster care receive non-specific, long-term therapy in which caregivers are not involved. Among the benefits of the type of engagement intervention used in this trial are the limited resources required for its implementation, paired with its potential to yield greater retention in treatment, lower rates of premature dropout, and, hopefully, improved youth outcomes. Our results suggest that with a time-limited training (4–6 hours) in McKay’s engagement procedures, brief consultation on application with families, and an additional 15 minutes dedicated to using them with each family at the first two contacts, clinicians may substantially increase foster parent and youth retention, which in turn may lead to improved outcomes for this high-needs population. Given the high dropout rates and low retention rates for foster care, and all families, more studies focused on engagement are needed.
Acknowledgements
We thank the study therapists for their dedication to serving children and families in Washington State and willingness to participate in this collaboration. We also thank Elizabeth M.Z. Farmer for her mentorship and advisement on the project.
This publication was made possible by funding from from grant number R34 MH079910 (Dorsey, PI), awarded from the National Institute of Mental Health (NIMH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shannon Dorsey, Email: dorsey2@uw.edu.
Michael D. Pullmann, Email: pullmann@uw.edu.
Lucy Berliner, Email: lucyb@uw.edu.
Elizabeth Koschmann, Email: felizabe@med.umich.edu.
Mary McKay, Email: mmm25@nyu.edu.
Esther Deblinger, Email: deblines@rowan.edu.
References
- Achenbach TM. Manual for the Child Behavior Checklist: 4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV TR. Vol. 943. Washington, DC: American Psychiatric; 2000. [Google Scholar]
- Attkisson CC, Zwick R. The client satisfaction questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;6:299–314. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Barkham M, Shapiro DA, Hardy GE, Rees A. Psychotherapy in two-plus-one sessions: Outcomes of a randomized controlled trial of cognitive-behavioral and psychodynamic-interpersonal therapy for subsyndromal depression. Journal of Consulting and Clinical Psychology. 1999;67:201–211. doi: 10.1037//0022-006x.67.2.201. [DOI] [PubMed] [Google Scholar]
- Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children's mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology. 2013 doi: 10.1080/15374416.2013.814543. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Briones E, Robbins MS, Szapocznik J. Brief Strategic Family Therapy: Engagement and treatment. Alcoholism Treatment Quarterly. 2008;26:81–103. [Google Scholar]
- Bruns EJ, Hoagwood KE. State implementation of evidence-based practice for youths, part I: Responses to the state of the evidence. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:369–373. doi: 10.1097/CHI.0b013e31816485f4. [DOI] [PubMed] [Google Scholar]
- Buckley JA, Epstein MH. The Behavioral and Emotional Rating Scale–2 (BERS-2): Providing a comprehensive approach to strength-based assessment. The California School Psychologist. 2004;9:21–27. [Google Scholar]
- Burns BJ, Phillips S, Wagner HR, Barth R, Kolko D, Campbell Y, Landsverk J. Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- CATS Consortium. Implementing CBT for traumatized children and adolescents after September 11: Lessons learned from the Child and Adolescent Trauma Treatments and Services (CATS) Project. Journal of Clinical Child & Adolescent Psychology. 2007;36:581–592. doi: 10.1080/15374410701662725. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Friedrich B. Evidence-based treatments in child abuse and neglect. Children and Youth Services Review. 2004;26:1097–1113. [Google Scholar]
- Chaffin M, Funderburk B, Bard D, Valle LA, Gurwitch R. A combined motivation and Parent-Child Interaction Therapy package reduces child welfare recidivism in a randomized dismantling field trial. Journal of Consulting and Clinical Psychology. 2011;79:84–95. doi: 10.1037/a0021227. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:393–403. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: Initial findings. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York, NY: Guilford Press; 2006. [Google Scholar]
- Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2011;165:16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- Courtney ME, Dworsky AL, Lee JS, Raap M. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Ages 23 and 24. Chicago, IL: University of Chicago, Chapin Hall; 2010. [Google Scholar]
- Deblinger E, Lippmann J, Steer RA. Sexually abused children suffering posttraumatic stress symptoms: Initial treatment outcome findings. Child Maltreatment. 1996;1:310–321. [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Traumafocused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression and Anxiety. 2011;28:67–75. doi: 10.1002/da.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child Psychiatry. 2006;45:1474–1484. doi: 10.1097/01.chi.0000240839.56114.bb. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Chamberlain P, Leve LD, Price J. Foster parent intervention engagement moderating child behavior problems and placement disruption. Research on Social Work Practice. 2009;19:423–433. doi: 10.1177/1049731508329407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey S, Briggs EC, Woods BA. Cognitive-behavioral treatment for posttraumatic stress disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2011;20:255–269. doi: 10.1016/j.chc.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey S, Deblinger E. TF-CBT applications for children in foster care. In: Cohen J, Mannarino A, Deblinger E, editors. Applications of Trauma-Focused Cognitive Behavioral Therapy for children and adolescents. New York, NY: Guilford Press; 2012. pp. 49–72. [Google Scholar]
- Dorsey S, Farmer EMZ, Barth RP, Greene KM, Reid J, Landsverk J. Current status and evidence base of training for foster and treatment foster parents. Children and Youth Services Review. 2008;30:1403–1416. doi: 10.1016/j.childyouth.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey S, Kerns SEU, Trupin EW, Conover KL, Berliner L. Child welfare caseworkers as service brokers for youth in foster care: Findings from Project Focus. Child Maltreatment. 2012;17:22–31. doi: 10.1177/1077559511429593. [DOI] [PubMed] [Google Scholar]
- Epstein MH, Harniss MK, Pearson N. The Behavioral and Emotional Rating Scale: Test-retest and inter-rater reliability. Journal of Child and Family Studies. 1999;8:319–327. [Google Scholar]
- Epstein MH, Ryser G, Pearson N. Standardization of the Behavioral and Emotional Rating Scale: Factor structure, reliability and criterion validity. Journal of Behavioral Health Services and Research. 2002;29:208–216. doi: 10.1007/BF02287707. [DOI] [PubMed] [Google Scholar]
- Epstein MH, Sharma J. Behavioral and Emotional Rating Scale: A Strength-Based Approach to Assessment. Austin, TX: Pro-ED; 1998. [Google Scholar]
- Farmer E, Burns B, Chapman M, Phillips S, Angold A, Costello E. Use of mental health services by youth in contact with social services. Social Service Review. 2001;75:605–624. [Google Scholar]
- Garland AF, Hough RL, Landsverk J, McCabe KM, Yeh M, Ganger WC, Reynolds BJ. Racial and ethnic variations in mental health care utilization among children in foster care. Children's Services: Social Policy, Research, and Practice. 2000;3:133–146. [Google Scholar]
- Garland AF, Landsverk JL, Hough RL, Ellis-McLeod E. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse & Neglect. 1996;20:675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Harrison ME, McKay MM, Bannon WM., Jr Inner-city child mental health service use: The real question is why youth and families do not use services. Community Mental Health Journal. 2004;40:119–131. doi: 10.1023/b:comh.0000022732.80714.8b. [DOI] [PubMed] [Google Scholar]
- Hoagwood K, Radigan M, Rodriquez J, Levitt JM, Fernandez D, Foster J. Final Report on the Child and Adolescent Trauma Treatment and Services (CATS) Project for the Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Mental Health. 2006 Unpublished manuscript.
- Hodges K. Depression and anxiety in children: A comparison of self-report questionnaires to clinical interview. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2(4):376–381. [Google Scholar]
- Hurlburt MS, Chamberlain P, DeGarmo D, Zhang J, Price JM. Advancing prediction of foster placement disruption using brief behavioral screening. Child Abuse & Neglect. 2010;34(12):917–926. doi: 10.1016/j.chiabu.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingoldsby EM. Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies. 2010;19:629–645. doi: 10.1007/s10826-009-9350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S. Why do foster care placements disrupt? An investigation of reasons for placement change in foster care. Social Service Review. 2004;78(4):601–627. [Google Scholar]
- James S, Landsverk J, Slymen D. Patterns of placement movement in out-of-home care. Children and Youth Services Review. 2004;26(2):185–206. [Google Scholar]
- Jaycox LH, Cohen JA, Mannarino AP, Walker DW, Langley AK, Gegenheimer KL, Schonlau M. Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress. 2010;23:223–231. doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko DJ, Hurlburt MS, Zhang J, Barth RP, Leslie LK, Burns BJ. Posttraumatic stress symptoms in children and adolescents referred for child welfare investigation: A national sample of in-home and out-of-home care. Child Maltreatment. 2010;15:48–62. doi: 10.1177/1077559509337892. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kulka R, Fairbank J, Schlenger W. Trauma and the Vietnam Generation. New York City, NY: Brunner/Mazel; 1990. [Google Scholar]
- Landsverk J, Burns BJ, Stambaugh LF, Reutz JAR. Mental Health Care for Children and Adolescents in Foster Care: Review of Research Literature. Report prepared for Casey Family Programs. Seattle, WA: 2006. [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979 doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J. Relationship between entry into child welfare and mental health service use. Psychiatric Services. 2005;56(8):981–987. doi: 10.1176/appi.ps.56.8.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, Hurlburt MS, Landsverk J, Barth R, Slymen DJ. Outpatient mental health services for children in foster care: A national perspective. Child Abuse & Neglect. 2004;28(6):697–712. doi: 10.1016/j.chiabu.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Brandt NE, Becker KD, Lee BR, Barth RP, Daleiden EL, Chorpita BF. Identifying the common elements of treatment engagement interventions in children’s mental health services. Clinical Child and Family Psychology Review. 2013 doi: 10.1007/s10567-013-0163-x. Advance online publication. doi: [DOI] [PubMed] [Google Scholar]
- McKay MM, Bannon WM. Engaging families in child mental health services. Child & Adolescent Psychiatric Clinics of North America. 2004;13(4):905–921. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- McKay MM, Harrison ME, Gonzales J, Kim L, Quintana E. Multiple-family groups for urban children with conduct difficulties and their families. Psychiatric Services. 2002;53:1467–1468. doi: 10.1176/appi.ps.53.11.1467. [DOI] [PubMed] [Google Scholar]
- McKay MM, Nudelman R, McCadam K, Gonzales J. Evaluating a social work engagement approach to involving inner-city children and their families in mental health care. Research on Social Work Practice. 1996;6:462–472. [Google Scholar]
- McKay MM, Pennington J, Lynn CJ, McCadam K. Understanding urban child mental health service use: Two studies of child, family, and environmental correlates. Journal of Behavioral Health Services and Research. 2001;28(4):475–483. doi: 10.1007/BF02287777. [DOI] [PubMed] [Google Scholar]
- McKay MM, Stoewe J, McCadam K, Gonzales J. Increasing access to child mental health services for urban children and their care givers. Health and Social Work. 1998;23:9–15. doi: 10.1093/hsw/23.1.9. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, Kessler RC. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(8):815–830. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LM, Southam-Gerow MA, Allin RB. Who stays in treatment? Child and family predictors of youth client retention in a public mental health agency. Child and Youth Care Forum. 2008;37(4):153–170. doi: 10.1007/s10566-008-9058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2003. Final Report DHHS Pub. No. SMA-03-3832. [Google Scholar]
- Nock M, Kazdin A. Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology. 2005;73(5):872–879. doi: 10.1037/0022-006X.73.5.872. [DOI] [PubMed] [Google Scholar]
- Northwestern University. 2008. Evaluation of the Implementation of Three Evidence-Based Practices to Address Trauma for Children and Youth who are Wards of the State of Illinois. Chicago: Unpublished Final Report, Mental Health Services and Policy Program. [Google Scholar]
- Pecora PJ, Williams J, Kessler RC, Downs AC, O’Brien K, Hiripi E. Assessing the Effects of Foster Care: Early Results from the Casey National Alumni Study. Seattle, WA: Casey Family Program; 2003. [Google Scholar]
- Price JM, Chamberlain P, Landsverk J, Reid J. KEEP foster-parent training intervention: Model description and effectiveness. Child & Family Social Work. 2009;14(2):233–242. [Google Scholar]
- Pynoos RS, Rodriguez N, Steinberg A, Stuber M, Frederick C. UCLA PTSD Index Trauma Screen for DSM IV. 1998 [Google Scholar]
- Runyon MK, Deblinger E. Combined Parent-Child Cognitive Behavioral Therapy: An Approach to Empower Families At-Risk for Child Physical Abuse. New York City, NY: Oxford University Press; 2013. [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran c, Burns BJ, Kolko DJ, Putnam FW, Amaya-Jackson L. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press, Inc.; 2003. [Google Scholar]
- Southern DA, Faris PD, Brant R, Galbraith PD, Norris CM, Knudtson ML, Ghali WA. Kaplan–Meier methods yielded misleading results in competing risk scenarios. Journal of Clinical Epidemiology. 2006;59(10):1110–1114. doi: 10.1016/j.jclinepi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Stein BD, Zima BT, Elliott MN, Burnam MA, Shahinfar A, Fox NA, Leavitt LA. Violence exposure among school-age children in foster care: Relationship to distress symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(5):588–594. doi: 10.1097/00004583-200105000-00019. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer M, Decker K, Pynoos RS. The UCLA PTSD Reaction Index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowsky SA, Pynoos RS. Psychometric properties of the UCLA PTSD Reaction Index: Part I. Journal of Traumatic Stress. 2013;26(1):1–9. doi: 10.1002/jts.21780. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Pescosolido B, Cabassa LJ. Building a model to understand youth service access: The gateway provider model. Mental Health Services Research. 2004;6(4):189–198. doi: 10.1023/b:mhsr.0000044745.09952.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szapocznik J, Dantisteban D, Rio A, Perez-Vidal A, Santisteban D. Family effectiveness training: An intervention to prevent drug abuse and problem behaviors in Hispanic adolescents. Hispanic Journal of Behavioral Sciences. 1989;11(1):4–27. [Google Scholar]
- Tai BC, Machin D, White I, Gebski V. Competing risks analysis of patients with osteosarcoma: A comparison of four different approaches. Statistics in Medicine. 2001;20:661–684. doi: 10.1002/sim.711. [DOI] [PubMed] [Google Scholar]
- Tolan PH, Hanish LD, McKay MM, Dickey MH. Evaluating process in child and family interventions: Aggression prevention as an example. Journal of Family Psychology. 2002;16(2):220–236. doi: 10.1037//0893-3200.16.2.220. [DOI] [PubMed] [Google Scholar]
- Weiner DA, Schneider A, Lyons JS. Evidence-based treatments for trauma among culturally diverse foster care youth: Treatment retention and outcomes. Children and Youth Services Review. 2009;31:1199–1205. [Google Scholar]