Abstract
Importance
Mental disorders predict future occurrences of both the same disorder (homotypic continuity) and other disorders (heterotypic continuity). Heterotypic continuity is inconsistent with a view of mental disorders as fixed entities. In contrast, hierarchical-dimensional conceptualizations of psychopathology, in which each form of psychopathology is hypothesized to have both unique and broadly shared etiologies and mechanisms, predict both homotypic and heterotypic continuity.
Objective
To test predictions derived from a hierarchical-dimensional model of psychopathology that (a) heterotypic continuity is widespread, even controlling for homotypic continuity, and (b) the relative magnitudes of heterotypic continuities recapitulate the relative magnitudes of cross-sectional correlations among diagnoses at baseline.
Design
Assess 10 prevalent diagnoses in the same persons 3 years apart.
Setting
Representative sample of adults in the United States.
Participants
The 28,958 participants in the National Epidemiologic Study of Alcohol and Related Condition aged 18–64 years who were assessed in both waves.
Main Outcome Measure
Diagnoses from reliable and valid structured interviews.
Results
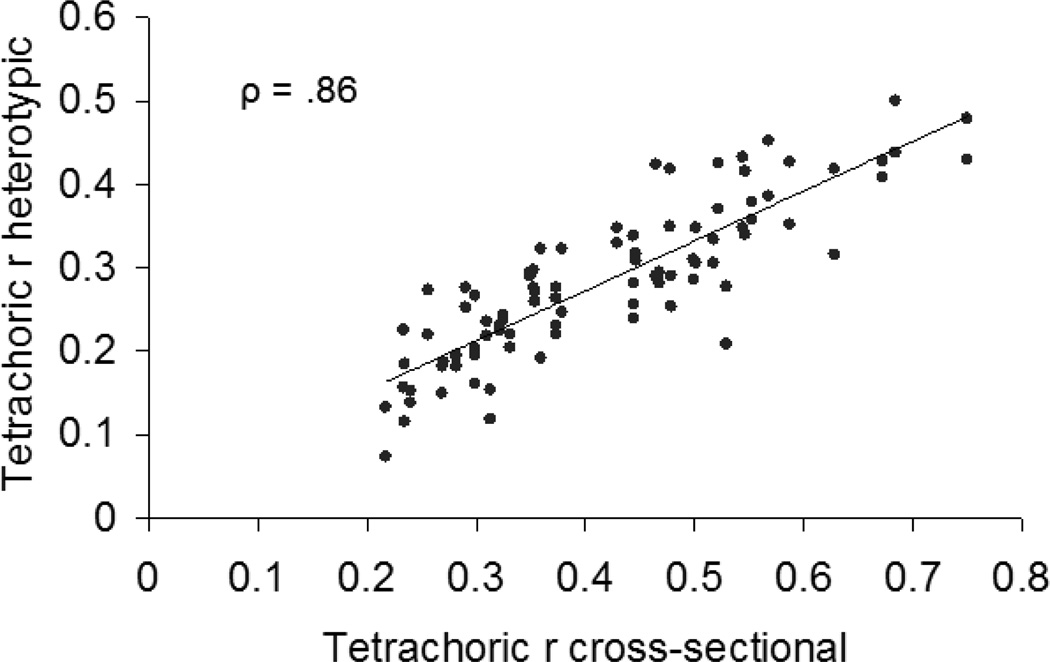
Bivariate associations of all pairs of diagnoses from wave 1 to wave 2 exceeded chance levels for all homotypic (tetrachoric ρ = 0.41 – 0.79, median = 0.54) and for nearly all heterotypic continuities (tetrachoric ρ = 0.07 – 0.50, median = 0.28), adjusted for sex and age. Significant heterotypic continuity was widespread even when all other wave 1 diagnoses (including the same diagnosis) were simultaneous predictors of each wave 2 diagnosis. The rank correlation between age and sex adjusted tetrachoric ρs for cross-sectional associations among wave 1 diagnoses and heterotypic associations from wave 1 to wave 2 diagnoses was ρ = .86.
Conclusions and Relevance
For these prevalent mental disorders, heterotypic continuity was nearly universal and not an artifact of failure to control for homotypic continuity. Furthermore, the relative magnitudes of heterotypic continuity closely mirrored the relative magnitudes of cross-sectional associations among these disorders, consistent with the hypothesis that both sets of associations reflect the same factors. Mental disorders are not fixed and independent entities. Rather, each diagnosis is robustly related to other diagnoses in a correlational structure that is manifested both concurrently and in patterns of heterotypic continuity across time.
In developmental studies of both adaptive and maladaptive behavior, two types of continuity in behavior over time are distinguished. When a behavior predicts itself at a later time in the same individual, the term homotypic continuity is used; in contrast, heterotypic continuity applies when a behavior predicts a different form of behavior in the same individual at a later time.1, 2 In the present study, we use the concepts of homotypic and heterotypic continuity to interrogate the basic nature of psychopathology during adulthood. If heterotypic continuity among diagnoses of mental disorders is common, that would further disconfirm the increasingly untenable view of mental disorders as fixed and independent entities.3 Rather, widespread heterotypic continuity would argue for a reconceptualization of psychopathology as phenomena that are subject to “changing manifestations”4 and “phenotypic plasticity.”5
Previous studies have documented both homotypic6–11 and heterotypic continuity7, 12–19 in a range of common forms of psychopathology during childhood and adolescence. There has been little study of heterotypic continuity of mental disorders during adulthood, however.7, 20 This is an important omission because it is possible that heterotypic continuity is limited to periods when developmental changes are rapid.21 Therefore, we assessed heterotypic continuity in a longitudinal study of a representative cohort of adults. Our first goal is to determine if heterotypic continuity is an artifact of homotypic continuity. In these first analyses, heterotypic continuity will be demonstrated only when disorder X at time 1 (X1) predicts disorder Y at time 2 (Y2) when disorder Y at time 1 (Y1) is controlled.11 This analysis ensures that X1 does not predict Y2 solely because X and Y are correlated at both time points.
Our second goal is to test a key prediction derived from emerging hierarchical-dimensional models of psychopathology.5, 22–27 Cross-sectional studies of correlations among mental disorders show that subgroups of disorders load on broad second-order factors of psychopathology defined by their patterns of correlations. Some studies modeled two second-order domains of psychopathology (internalizing and externalizing), whereas other studies divided the internalizing domain into correlated fears and distress subdomains.22, 24, 28, 29 Twin studies indicate that cross-sectional correlations among mental disorders reflect a hierarchical combination of both broadly shared and disorder-specific etiologic influences.25, 30, 31 This supports a hierarchical-dimensional conceptualization of psychopathology in which different forms of psychopathology are correlated to the extent to which they share etiologic influences.22, 25 A number of direct and indirect ways in which such sharing of etiologic influences could occur have been described by Krueger and Markon.22
Although hierarchical-dimensional models of psychopathology were derived from cross-sectional data,24, 25 substantial homotypic continuity of second-order factors of psychopathology (internalizing and externalizing32 or fears, distress, and externalizing33) has been documented during adulthood, including a report of homotypic continuity in the NESARC study.34 These studies provide evidence of the homotypic stability of second-order domains of psychopathology during adulthood. In the present study, we examine the heterotypic continuity among specific disorders within and between second-order domains of psychopathology.
We derive a strong prediction regarding heterotypic continuity from our hierarchical-dimensional model of psychopathology to subject this model to possible refutation.35 We predict that the relative magnitudes of cross-sectional phenotypic associations among different mental disorders at time 1 will be duplicated in the relative magnitudes of heterotypic associations from time 1 to time 2. If the relative extent to which disorder X1 predicts Y2 closely mirrors the relative magnitude of their cross-sectional (X1 and Y1) correlation at time 1, this would be consistent with the hypothesis that the same shared propensities that give rise to correlations among multiple mental disorders at time 1 also underlie the relative magnitudes of heterotypic continuities between those disorders over time. That is, if X1 and Y1 are highly correlated at time 1 partly because they share etiologic influences, the same shared etiologic influences on diagnosis X1 at time 1 would be expected to give rise to diagnosis Y2 at time 2, and vice-versa. Heterotypic prediction of Y2 from diagnosis X1 would occur because the same relatively enduring etiologic factors that increase the likelihood of X1 also increase the likelihood of Y2. Support for this prediction would be seen both in a significant rank-order correlation between cross-sectional and heterotypic correlations overall and in greater heterotypic continuity within than across second-order domains. Failure to confirm this prediction would require either substantial modification or rejection of the hierarchical-dimensional model.
METHODS
Data on diagnoses are from the first and second wave of the National Epidemiologic Study of Alcohol and Related Conditions (NESARC). In wave 1, structured diagnostic interviews were conducted with 43,093 adults representative of the noninstitutionalized civilian population of the United States. One person per household was randomly selected, but adults aged 18–24 years were oversampled at a 2.25:1 ratio. African American and Hispanic households were oversampled, achieving 19.1% non-Hispanic African American and 19.3% Hispanic households. The sample was weighted in all analyses to adjust for probabilities of selection, nonresponse, the selection of one person per household, and oversampling. Once weighted, the data were representative of the U.S. population.36 Three years later, 34,653 of these participants were reinterviewed. Participation was 81.0% in wave 1 and 86.7% of wave 1 participants were assessed again in wave 2. The present analyses were conducted on the 28,958 individuals who were 18–65 years old in wave 1 and assessed in both waves.
Measures
The reliable 37 and valid38–40 Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version (AUDADIS-IV)37 was administered in person. The 12-month DSM-IV diagnostic categories used in these analyses are major depression, dysthymia, social phobia, specific phobia, generalized anxiety disorder, agoraphobia/panic disorder, antisocial personality disorder, tobacco dependence, alcohol dependence, and other substance dependence. The diagnosis of major depression ruled out bereavement, and all mood and anxiety disorders due to general medical conditions were excluded.
Statistical Analyses
Data were analyzed at the U. S. Census Bureau with permission of the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Because NESARC used complex probability sampling, all analyses were weighted proportionally to the inverse of sampling probability, adjusted for non-response, to accurately represent the population, and standard errors and tests accounted for the complex stratified and clustered sampling design. The two hypotheses were tested using adjusted tetrachoric correlations.41, 42 Adjusted tetrachoric correlations were estimated using linear structural equation models for binary data. In these models, a binary manifest variable is construed as a dichotomized version of a latent normal variable. For any pair of variables to be correlated, they were specified in the model as being regressed on all desired adjustors; the residual correlation among the latent continuous variables is then interpreted as an adjusted tetrachoric correlation. Models were estimated and tested in Mplus 6.1.43 All tetrachoric correlations were adjusted for age in wave 1 and sex. Bivariate correlations are first presented for cross-sectional associations in wave 1 and for homotypic continuities from wave 1 to wave 2 to aid interpretation of the analyses addressing two goals.
1. Heterotypic continuity, controlling for homotypic continuity
Goal 1 is to conduct a strict test of the existence of heterotypic continuity during adulthood. To do so wave 2 versus wave 1 tetrachoric correlations were estimated pairwise, diagnosis by diagnosis, each time controlling the other nine wave 1 diagnoses, including the same diagnosis as that being included from wave 2, in addition to sex and wave 1 age. The same diagnosis was included as an adjustor to ensure that heterotypic predictions are not simply an artifact of the uncontrolled homotypic continuity of persistent disorders. The other nine wave 1 diagnoses were included to estimate the unique heterotypic continuity of each diagnosis controlling for all other assessed diagnoses.
2. Correlation of cross-sectional and heterotypic associations
Goal 2 is to test the strong prediction that the relative magnitudes of bivariate heterotypic correlations would be substantially correlated with the relative magnitudes of bivariate cross-sectional correlations in wave 1 using Spearman’s rank correlation
RESULTS
To facilitate interpretation, the results in the three tables are grouped by the three second-order factors of fears, distress, and externalizing disorders identified in previous studies,22 including wave 1 of NESARC.24 Cross-sectional tetrachoric correlations among all pairs of the 10 diagnoses assessed in wave 1, adjusted for age and sex, are shown in Table 1 (all P < .0001). Table 2 presents the homotypic and heterotypic tetrachoric correlations between all pairs of diagnoses from wave 1 to wave 2, adjusted for sex and wave 1 age. Tetrachoric correlations for homotypic continuities in Table 2 were all significant at P < .0001, ranging from moderate (ρ = .41 for specific phobia) to strong (ρ = .79 for tobacco dependence). The magnitudes of the bivariate heterotypic continuities in Table 2 ranged considerably from ρ = .07 (wave 1 alcohol dependence to wave 2 specific phobia) to ρ = .50 (wave 1 generalized anxiety disorder to wave 2 major depression). All bivariate heterotypic correlations were significant at P < .05, except for the prediction of wave 2 other substance dependence from wave 1 specific phobia.
Table 1.
Bivariate cross-sectional tetrachoric correlations (standard errors), adjusted for sex and wave 1age, among wave 1 diagnoses in the NESARC sample.
| MDD1 | DYS1 | GAD1 | SPP1 | SOC1 | AGP1 | APD1 | TOB1 | ALC1 | SUB1 | |
|---|---|---|---|---|---|---|---|---|---|---|
| MDD1 | 0.75 (0.02) | 0.67 (0.02) | 0.32 (0.02) | 0.48 (0.02) | 0.55 (0.02) | 0.37 (0.02) | 0.32 (0.02) | 0.33 (0.03) | 0.48 (0.04) | |
| DYS1 | 0.68 (0.02) | 0.26 (0.03) | 0.46 (0.03) | 0.50 (0.02) | 0.36 (0.03) | 0.29 (0.02) | 0.24 (0.04) | 0.53 (0.04) | ||
| GAD1 | 0.44 (0.02) | 0.54 (0.03) | 0.59 (0.02) | 0.37 (0.03) | 0.30 (0.03) | 0.27 (0.04) | 0.50 (0.05) | |||
| SPP1 | 0.52 (0.02) | 0.44 (0.02) | 0.28 (0.03) | 0.27 (0.02) | 0.22 (0.03) | 0.31 (0.05) | ||||
| SOC1 | 0.52 (0.02) | 0.30 (0.03) | 0.23 (0.02) | 0.23 (0.04) | 0.35 (0.04) | |||||
| AGP1 | 0.35 (0.03) | 0.35 (0.02) | 0.31 (0.04) | 0.47 (0.05) | ||||||
| APD1 | 0.43 (0.02) | 0.38 (0.03) | 0.57 (0.04) | |||||||
| TOB1 | 0.45 (0.02) | 0.55 (0.03) | ||||||||
| ALC1 | 0.63 (0.05) |
All correlations P < .0001.
Note: Digit at the end of abbreviations indicates wave of assessment; MDD = major depression; DYS = dysthymia; GAD = generalized anxiety disorder; SPP = specific phobia; SOC = social phobia; AGP = agoraphobia and or panic disorder; APD = antisocial personality disorder; TOB = tobacco dependence; ALC = alcohol dependence; SUB = other substance dependence; cross-sectional associations within the same second-order class of mental disorders (distress, fears, or externalizing) in gray shading.
Table 2.
Bivariate tetrachoric correlations (standard errors) for prospective homotypic and heterotypic continuities from wave 1 diagnoses to wave 2 diagnoses in NESARC, adjusted for sex and age in wave 1.
| Wave 2 Diagnoses | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Distress | Fears | Externalizing | ||||||||
| Wave 1 Diagnoses |
MDD2 | DYS2 | GAD2 | SPP2 | SOC2 | AGP2 | APD2 | TOB2 | ALC2 | SUB2 |
| Distress | ||||||||||
| MDD1 | 0.49 (0.02) | 0.48 (0.03) | 0.41 (0.02) | 0.24 (0.02) | 0.42 (0.02) | 0.36 (0.02) | 0.28 (0.03) | 0.23 (0.02) | 0.20 (0.03) | 0.29 (0.04) |
| DYS1 | 0.43 (0.02) | 0.53 (0.03) | 0.44 (0.03) | 0.27 (0.03) | 0.42 (0.03) | 0.35 (0.03) | 0.32 (0.04) | 0.28 (0.02) | 0.15 (0.04) | 0.28 (0.05) |
| GAD1 | 0.43 (0.02) | 0.50 (0.04) | 0.47 (0.03) | 0.26 (0.03) | 0.43 (0.02) | 0.43 (0.03) | 0.26 (0.04) | 0.27 (0.03) | 0.15 (0.04) | 0.31 (0.06) |
| Fears | ||||||||||
| SPP1 | 0.24 (0.02) | 0.22 (0.04) | 0.24 (0.02) | 0.41 (0.02) | 0.33 (0.03) | 0.28 (0.03) | 0.19 (0.04) | 0.19 (0.02) | 0.13 (0.03) | 0.12 (0.08) |
| SOC1 | 0.35 (0.02) | 0.29 (0.04) | 0.35 (0.03) | 0.30 (0.02) | 0.56 (0.02) | 0.37 (0.03) | 0.16 (0.04) | 0.16 (0.03) | 0.12 (0.04) | 0.27 (0.06) |
| AGP1 | 0.38 (0.02) | 0.31 (0.04) | 0.35 (0.03) | 0.34 (0.03) | 0.43 (0.03) | 0.55 (0.02) | 0.30 (0.03) | 0.30 (0.02) | 0.22 (0.04) | 0.29 (0.05) |
| Externalizing | ||||||||||
| APD1 | 0.23 (0.02) | 0.19 (0.05) | 0.22 (0.03) | 0.18 (0.03) | 0.19 (0.04) | 0.28 (0.03) | 0.42 (0.02) | 0.33 (0.02) | 0.25 (0.03) | 0.39 (0.05) |
| TOB1 | 0.22 (0.02) | 0.25 (0.03) | 0.20 (0.02) | 0.19 (0.02) | 0.22 (0.03) | 0.29 (0.02) | 0.35 (0.02) | 0.79 (0.01) | 0.32 (0.02) | 0.34 (0.04) |
| ALC1 | 0.22 (0.02) | 0.14 (0.06) | 0.18 (0.04) | 0.07 (0.03) | 0.18 (0.04) | 0.24 (0.04) | 0.32 (0.03) | 0.31 (0.02) | 0.60 0.02 | 0.32 (0.04) |
| SUB1 | 0.25 (0.04) | 0.20 (0.08) | 0.29 (0.07) | 0.15 (0.05) | 0.26 (0.06) | 0.28 (0.06) | 0.45 (0.04) | 0.42 (0.04) | 0.42 (0.05) | 0.57 (0.05) |
All correlations P < .05, except for wave 1 specific phobia 1 and wave 2 other substance dependence.
Note: Digit at the end abbreviations indicates wave of assessment; MDD = major depression; DYS = dysthymia; GAD = generalized anxiety disorder; SPP = specific phobia; SOC = social phobia; AGP = agoraphobia and or panic disorder; APD = antisocial personality disorder; TOB = tobacco dependence; ALC = alcohol dependence; SUB = other substance dependence; tetrachoric for homotypic associations are in bold ; prospective associations within the same second-order class of mental disorders (distress, fears, or externalizing) in gray shading.
Table 3 presents the homotypic and heterotypic tetrachoric correlations between all pairs of diagnoses from wave 1 to wave 2, adjusted for sex, wave 1 age, and all nine other wave 1 diagnoses. Even in these strict tests, significant heterotypic continuity was nearly universal within second-order domains. Each wave 1 diagnosis in the distress domain accounted for significant independent variance in the prediction of each other distress diagnosis in wave 2, and each wave 1 diagnosis in the fears domain independently predicted each other fears diagnosis in wave 2. Furthermore, each wave 1 diagnosis in the externalizing domain independently predicted each other externalizing diagnosis in wave 2, except for wave 1 other substance dependence and wave 2 tobacco dependence.
Table 3.
Tetrachoric correlations (standard errors) and z-statistics between each wave 1 and wave 2 diagnoses, simultaneously adjusted for sex, wave 1 age, and all other wave 1 diagnoses in NESARC.
| Wave 2 Diagnoses | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Distress | Fears | Externalizing | ||||||||
| Wave 1 Diagnoses |
MDD2 | DYS2 | GAD2 | SPP2 | SOC2 | AGP2 | APD2 | TOB2 | ALC2 | SUB2 |
| Distress | ||||||||||
| MDD1 |
0.36 (0.02) z = 18.21**** |
0.30 (0.03) z = 9.56**** |
0.24 (0.02) z = 10.33**** |
0.11 (0.02) z = 5.10**** |
0.22 (0.02) z = 8.98**** |
0.15 (0.03) z = 5.23**** |
0.10 (0.03) z = 3.42*** |
0.01 (0.02) z = 0.30 |
0.07 (0.03) z = 2.17* |
0.13 (0.04) z = 3.18*** |
| DYS1 | 0.17 (0.03) z = 5.81**** |
0.31 (0.04) z = 8.03**** |
0.20 (0.04) z = 5.04**** |
0.13 (0.04) z = 3.47*** |
0.17 (0.04) z = 4.24**** |
0.07 (0.04) z = 1.75 |
0.16 (0.04) z = 3.95**** |
0.12 (0.04) z = 3.31*** |
0.01 (0.04) z = 0.27 |
−0.01 (0.06) z = −0.15 |
| GAD1 | 0.18 (0.03) z = 6.14**** |
0.27 (0.04) z = 6.14**** |
0.27 (0.03) z = 8.34**** |
0.03 (0.03) z = 0.99 |
0.14 (0.04) z = 3.71**** |
0.19 (0.04) z = 4.97**** |
0.03 (0.05) z = 0.54 |
0.08 (0.04) z = 2.21* |
−0.01 (0.04) z = −0.18 |
0.07 (0.08) z = 0.86 |
| Fears | ||||||||||
| SPP1 | 0.10 (0.02) z = 4.46**** |
0.06 (0.04) z = 1.45 |
0.10 (0.03) z = 3.50**** |
0.35 (0.02) z = 17.95**** |
0.15 (0.03) z = 4.50**** |
0.10 (0.04) z = 2.82** |
0.06 (0.04) z = 1.66 |
0.02 (0.03) z = 0.63 |
0.01 (0.04) z = 0.36 |
−0.09 (0.06) z = −1.46 |
| SOC1 | 0.16 (0.03) z = 6.03**** |
0.02 (0.05) z = 0.36 |
0.15 (0.04) z = 4.14**** |
0.13 (0.03) z = 4.95**** |
0.43 (0.03) z = 14.78**** |
0.14 (0.04) z = 3.06** |
−0.04 (0.05) z = −0.81 |
−0.05 (0.03) z = −1.43 |
−0.01 (0.04) z = −0.32 |
0.11 (0.07) z = 1.58 |
| AGP1 | 0.18 (0.03) z = 6.15**** |
0.01 (0.05) z = 0.27 |
0.15 (0.03) z = 4.44**** |
0.18 (0.03) z = 6.11**** |
0.19 (0.04) z = 5.04**** |
0.42 (0.03) z = 14.77**** |
0.11 (0.04) z = 2.72** |
0.10 (0.03) z = 3.16** |
0.06 (0.05) z = 1.38 |
0.07 (0.07) z = 1.00 |
| Externalizing | ||||||||||
| APD1 | 0.09 (0.02) z = 3.44*** |
0.00 (0.06) z = 0.04 |
0.07 (0.03) z = 2.12* |
0.08 (0.03) z = 2.69** |
0.00 (0.04) z = 0.00 |
0.12 (0.04) z = 3.23*** |
0.31 (0.03) z = 10.80**** |
0.10 (0.03) z = 3.58**** |
0.09 (0.03) z = 2.72** |
0.24 (0.05) z = 4.49**** |
| TOB1 | 0.11 (0.02) z = 5.87**** |
0.15 (0.04) z = 4.28**** |
0.09 (0.02) z = 3.67**** |
0.11 (0.02) z = 5.53**** |
0.11 (0.03) z = 3.63**** |
0.17 (0.02) z = 6.75**** |
0.22 (0.02) z = 9.76**** |
0.77 (0.01) z = 94.28**** |
0.19 (0.02) z = 7.95**** |
0.20 (0.04) z = 4.83**** |
| ALC1 | 0.10 (0.03) z = 3.81**** |
0.01 (0.06) z = 0.10 |
0.06 (0.04) z = 1.74 |
−0.04 (0.03) z = −1.38 |
0.05 (0.04) z = 1.24 |
0.09 (0.05) z = 1.90 |
0.17 (0.03) z = 5.60**** |
0.06 (0.03) z = 2.12* |
0.55 (0.02) z = 27.71**** |
0.13 (0.04) z = 3.02** |
| SUB1 | 0.02 (0.06) z = 0.33 |
−0.11 (0.13) z = −0.87 |
0.09 (0.06) z = 1.37 |
0.05 (0.07) z = −0.64 |
0.01 (0.08) z = 0.10 |
0.01 (0.08) z = 0.12 |
0.23 (0.05) z = 4.48**** |
0.09 (0.05) z = 1.92 |
0.16 (0.05) z = 3.01** |
0.44 (0.06) z = 7.42**** |
Note: Digit at the end abbreviations indicates wave of assessment; MDD = major depression; DYS = dysthymia; GAD = generalized anxiety disorder; SPP = specific phobia; SOC = social phobia; AGP = agoraphobia and or panic disorder; APD = antisocial personality disorder; TOB = tobacco dependence; ALC = alcohol dependence; SUB = other substance dependence; tetrachoric correlations for homotypic associations are in bold.
P < .05;
P < .01;
P < .001;
P < .0001
The results presented in Table 3 also revealed less consistent, but still widespread heterotypic continuities from diagnoses in one second-order domains to diagnoses in different second-order domains, even when homotypic continuity and the heterotypic associations of all other wave 1 diagnoses were controlled. There was a notable pattern to these cross-domain heterotypic continuities: The significant independent heterotypic associations more commonly involved distress diagnoses as either the predictor or as the predicted diagnosis. The three wave 1 distress diagnoses accounted for significant independent variance in the prediction of wave 2 fear diagnoses in seven of nine tests of association. Similarly, wave 1 fear diagnoses were found to independently predict wave 2 distress diagnoses in six of nine tests, and wave 1 externalizing diagnoses predicted wave 2 distress diagnoses in six of twelve tests. In contrast, the wave 1 fear diagnoses only accounted for significant independent variance in wave 2 externalizing diagnoses in two of twelve tests.
Given this conservative evidence of widespread heterotypic continuity during adulthood, we tested the prediction derived from hierarchical-dimensional models of psychopathology that the varying magnitudes of bivariate heterotypic continuities from wave 1 to wave 2 will mirror the extents of cross-sectional correlations among the wave 1 disorders. Note that the heterotypic associations of diagnoses X and Y across waves generates two heterotypic correlations for each pair of disorders (X1 with Y2 and Y1 with X2), in contrast to the single cross-sectional correlation of X1 and Y1. The rank-order correlation of the cross-sectional tetrachoric correlations adjusted for age and sex for cross-sectional associations among wave 1 diagnoses with the heterotypic tetrachoric correlations adjusted for age and sex for predictions from wave 1 to wave 2 diagnoses was ρ (90) = 0.86, P < .0001 (see Figure 1).
Figure 1.
Scatter-plot and Spearman rank correlation of bivariate cross-sectional age and sex adjusted tetrachoric correlations among wave 1 diagnoses with bivariate heterotypic age and sex adjusted tetrachoric correlations from wave 1 to wave 2 diagnoses in the NESARC sample.
DISCUSSION
The present findings reveal widespread heterotypic continuity among mental disorders in a representative sample of adults, even when homotypic continuity is controlled. The tests of heterotypic continuity reported in Table 3 were highly conservative, controlling not only for homotypic continuity but for heterotypic continuity with every other wave 1 diagnosis. The results of these strict tests are important in two ways. First, they reveal that widespread heterotypic prediction of future diagnoses is not an artifact of uncontrolled homotypic continuity. Second, these tests reveal that each wave 2 diagnosis is independently predicted by multiple wave 1 diagnoses. For example, agoraphobia/panic disorder in wave 2 is not only significantly predicted by the same diagnosis in wave 1, it also is independently predicted by six other wave 1 diagnoses, each of which explained from 1.0 to 3.6% of the residual variance in wave 2 agoraphobia/panic disorder, after controlling all other predictors. Thus, a network of multiple significant homotypic and heterotypic continuities allows agoraphobia/panic disorder in wave 2 to be predicted based on knowledge of all wave 1 diagnoses. To varying degrees the same is true of all other wave 2 diagnoses.
The present findings also confirmed a key prediction derived from hierarchical-dimensional models of psychopathology.22, 24, 25, 44 The relative magnitudes of heterotypic associations among different diagnoses from time 1 to time 2 clearly recapitulate the magnitudes of their cross-sectional associations at time 1. These findings are consistent with the hypothesis that the same shared etiologic factors that give rise to patterned correlations among multiple mental disorders at time 1 also give rise to heterotypic continuities over time.
We previously reported independent evidence based on cross-sectional twin data that phenotypic correlations among common dimensions of psychopathology in children and adolescents at one point in time are primarily due to highly pleiotropic genetic influences, whereas environmental influences are mostly specific to each dimension of psychopathology.25 By adding the dimension of time, the present prospective analyses suggest the further hypothesis that the underlying pleiotropic liabilities are relatively unchanging, but often give rise to changing symptomatic manifestations over time, perhaps due to changing environmental influences.
An incidental finding regarding the relative magnitudes of homotypic and heterotypic predictions of some wave 2 diagnoses is notable in this context. Although we did not conduct formal statistical tests, tables 2 and 3 shows that bivariate heterotypic continuities are generally smaller than homotypic continuities for the same wave 2 diagnosis. In the distress domain, however, bivariate heterotypic continuities rival the homotypic continuities. Indeed, generalized anxiety disorder in wave 1 predicts dysthymia wave 2 heterotypically as well as it predicts itself homotypically. These findings suggest substantial shifting across diagnostic boundaries among distress diagnoses over time, perhaps more than among diagnoses in other domains.
The robust pattern of widespread heterotypic continuity observed in the present analyses supports future studies of hierarchical-dimensional models22, 24, 25, 44 and other models that view psychopathology as subject to change from one form of psychopathology to another over time.4, 5 These models have strong implications for how shared and disorder-specific aspects of etiology and psychobiological mechanisms should be studied,25 and argue for further study of transdiagnostic approaches to the treatment of psychopathology, which focus less on the specific presenting symptoms and more on broad domains of dysfunction hypothesized to underlie changing symptoms.5, 45
Limitations
Like nearly all studies of adult psychopathology in population-based samples, the structured diagnostic interview in NESARC used skip patterns to route the interview from questions about symptoms of a disorder as soon as it was impossible for the individual to meet diagnostic criteria for that disorder. For example, individuals who did not report either dysphoria or anhedonia were not asked about other symptoms of major depression.46 This means that full counts of all symptoms of each disorder could not be used in these analyses instead of categorical diagnoses. Because persons with subthreshold symptoms of at least some disorders are at increased risk for the same and other mental disorders in the future,47–49 it would have been preferable to study symptom counts. Although this may have changed the estimates of homotypic and heterotypic continuity somewhat, it seems unlikely that it would have changed the pattern of findings. Nonetheless, longitudinal studies of large population-based samples of adults using instruments that can yield full symptom counts are needed to fully understand the structure of psychopathology over time.
Future Directions
Although sex and age were controlled in all analyses, we did not test for the possible moderation of homotypic and heterotypic continuity by demographic factors. Because previous studies of youth found evidence for moderation of continuity by sex,50, 51 this is an important topic for future research.
A central hypothesis of our hierarchical-dimensional model of psychopathology is that correlations among different forms of psychopathology, both concurrently and across time, reflect shared etiologies and individual differences in central neural mechanisms that underlie multiple dimensions of psychopathology.25 More studies are needed both to test hierarchical-dimensional models of psychopathology using external validity criteria and to expand understanding of the relevant biological mechanisms. Furthermore, studies are needed to test the fundamental hypothesis of hierarchical-dimensional models that broadly shared (i.e., pleiotropic) influences on psychopathology of some molecular genetic variants are an important source of the hierarchical structure of psychopathology.25
It is important to note that studies of etiology and pathophysiology based on the hierarchical-dimensional model of psychopathology will inform the Research Domains Criteria (RDoC) initiative. RDoC is based on the assumption that nominal diagnostic categories are too heterogeneous biologically to study meaningfully.52 The hierarchical-dimensional model of psychopathology is consistent with RDoC: The hierarchical-dimensional model posits that some etiologic influences and mechanisms are specific to each first-order dimension of psychopathology, but other etiologic influences and mechanisms are shared across dimensions of psychopathology, resulting in substantial heterogeneity of etiologic influences within nominal categories of mental disorders.25 Consider genetic influences on the diagnosis of major depression as an example. Each individual who meets criteria for depression could be influenced by any combination of: genetic variants that are specifically associated with only major depression, genetic variants pleiotropically associated with risk for any internalizing disorder, and highly pleiotropic genetic variants associated with risk for any common form of psychopathology.25 As a result, this and other diagnostic categories are likely to be influenced by a heterogeneous mixture of these three (or more) sets of genetic influences, with different persons who meet diagnostic criteria for major depression being influenced by different combinations of these sets of genetic variants. There may well be intractable heterogeneity of genetic influences for studies that do not separate such putative hierarchical sets of genetic influences. The most informative etiologic studies, therefore, will examine genetic and environmental influences at multiple levels in the hierachical organization of psychopathology and link those influences to the specific functional domains identified in the RDoC model.52
Acknowledgement
Supported by grants R01 MH098098 and P50 MH94267.
Contributor Information
Benjamin B. Lahey, Departments of Health Studies and Psychiatry and Behavioral Neuroscience, University of Chicago, Chicago, Illinois
David H. Zald, Departments of Psychology and Psychiatry, Vanderbilt University, Nashville, Tennessee
Jahn K. Hakes, United States Census Bureau, Suitland, MD
Robert F. Krueger, Department of Psychology, University of Minnesota, Minneapolis, Minnesota
Paul J. Rathouz, Department of Biostatistics and Medical Informatics, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin
REFERENCES
- 1.Kagan J, Moss HA. Birth to maturity: A study in psychological development. New York: Wiley; 1962. [Google Scholar]
- 2.Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47:276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- 3.Angold A, Costello EJ. Nosology and measurement in child and adolescent psychiatry. Journal of Child Psychology and Psychiatry. 2009;50:9–15. doi: 10.1111/j.1469-7610.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- 4.Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annual Review of Psychology. 1997;48:371–410. doi: 10.1146/annurev.psych.48.1.371. [DOI] [PubMed] [Google Scholar]
- 5.Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology. Perspectives on Psychological Science. 2011;6:589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- 6.Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional defiant disorder and conduct disorder: Implications for the DSM-V. Journal of Abnormal Psychology. 2010;119:739–751. doi: 10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- 7.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 9.Lahey BB, Pelham WE, Loney J, et al. Three-year predictive validity of DSM-IV attention deficit/hyperactivity disorder in children diagnosed at 4–6 years of age. American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- 10.Ferdinand RF, Dieleman G, Ormel J, Verhulst FC. Homotypic versus heterotypic continuity of anxiety symptoms in young adolescents: Evidence for distinctions between DSM-IV subtypes. Journal of Abnormal Child Psychology. 2007;35:325–333. doi: 10.1007/s10802-006-9093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- 13.Bussing R, Mason DM, Bell L, Porter P, Garvan C. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:595–605. doi: 10.1016/j.jaac.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chronis-Tuscano A, Molina BSG, Pelham WE, et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewinsohn PM, Holm-Denoma JM, Small JW, Seeley JR, Joiner TE. Separation anxiety disorder in childhood as a risk factor for future mental illness. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:548–555. doi: 10.1097/CHI.0b013e31816765e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moffitt TE, Harrington H, Caspi A, et al. Depression and generalized anxiety disorder - Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 17.Roberson-Nay R, Eaves LJ, Hettema JM, Kendler KS, Silberg JL. Childhood separation anxiety disorder and adult onset panic attacks share a common genetic diathesis. Depression and Anxiety. 2012;29:320–327. doi: 10.1002/da.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson KA, Hayward C. A prospective evaluation of agoraphobia and depression symptoms following panic attacks in a community sample of adolescents. Journal of Anxiety Disorders. 2005;19:87–103. doi: 10.1016/j.janxdis.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Wickrama KAS, Conger RD, Lorenz FO, Martin M. Continuity and discontinuity of depressed mood from late adolescence to young adulthood: The mediating and stabilizing roles of young adults' socioeconomic attainment. Journal of Adolescence. 2012;35:648–658. doi: 10.1016/j.adolescence.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cicchetti D, Cohen DJ, editors. Developmental psychopathology. Second ed. New York: Wiley; 2006. [Google Scholar]
- 22.Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Watson D, O'Hara MW, Stuart S. Hierarchical structures of affect and psychopathology and their implications for the classification of emotional disorders. Depression and Anxiety. 2008;25:282–288. doi: 10.1002/da.20496. [DOI] [PubMed] [Google Scholar]
- 24.Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH. Conceptual backgroud, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety. 2010;27:882–890. doi: 10.1002/da.20735. [DOI] [PubMed] [Google Scholar]
- 27.Licinio J, Wong M-L. A novel conceptual framework for psychiatry: Vertically and horizontally integrated approaches to redundancy and pleiotropism that co-exist with a classification of symptom clusters based on DSM-5. Molecular Psychiatry. 2013;18:846–848. doi: 10.1038/mp.2013.90. [DOI] [PubMed] [Google Scholar]
- 28.Lahey BB, Rathouz PJ, Applegate B, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 29.Achenbach TM, Howell CT, Quay HC, Conners CK. National survey of problems and competences among 4 to 16 year-olds: Parents reports for normative and clinical samples. Monographs of the Society for Research in Child Development. 1991;56:R5–R119. [PubMed] [Google Scholar]
- 30.Cosgrove VE, Rhee SH, Gelhorn HL, et al. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. Journal of Abnormal Child Psychology. 2011;39:109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 32.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 33.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders - The NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 34.Eaton NR, Krueger RF, Markon KE, et al. The structure and predictive validity of the internalizing disorders. Journal of Abnormal Psychology. 2013;122:86–92. doi: 10.1037/a0029598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popper K. Conjectures and refutations. London: Routledge and Kegan Paul; 1963. [Google Scholar]
- 36.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders - Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 37.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 38.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, and disability of personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 40.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic Whites in them United States - Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 41.Kraemer HC. Reconsidering the odds ratio as a measure of 2×2 association in a population. Statistics in Medicine. 2004;23:257–270. doi: 10.1002/sim.1714. [DOI] [PubMed] [Google Scholar]
- 42.Kraemer HC. Correlation coefficients in medical research: From product moment correlation to the odds ratio. Statistical Methods in Medical Research. 2006;15:525–545. doi: 10.1177/0962280206070650. [DOI] [PubMed] [Google Scholar]
- 43.Muthén B, Muthén L. Mplus Version 6. Los Angeles: Muthén & Muthén; 2010. [Google Scholar]
- 44.Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behaviour Research and Therapy. 2002;40:485–499. doi: 10.1016/s0005-7967(02)00016-5. [DOI] [PubMed] [Google Scholar]
- 45.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 46.Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 48.Karsten J, Hartman CA, Smit JH, et al. Psychiatric history and subthreshold symptoms as predictors of the occurrence of depressive or anxiety disorder within 2 years. British Journal of Psychiatry. 2011;198:206–212. doi: 10.1192/bjp.bp.110.080572. [DOI] [PubMed] [Google Scholar]
- 49.Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE. Subthreshold conditions as precursors for full syndrome disorders: A 15-year longitudinal study of multiple diagnostic classes. Journal of Child Psychology and Psychiatry. 2009;50:1485–1494. doi: 10.1111/j.1469-7610.2009.02117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Costello EJ, Foley DL, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- 51.Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- 52.Insel T, Cuthbert B, Garvey M, et al. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]