Abstract
Background
Patients with severe lower extremity trauma have significant disability 2 years after injury that worsens by 7 years. Up to 15% seek late amputation. Recently, an energy-storing orthosis demonstrated improved function compared with standard orthoses; however, the effect when integrated with rehabilitation over time is unknown.
Questions/purposes
(1) Does an 8-week integrated orthotic and rehabilitation initiative improve physical performance, pain, and outcomes in patients with lower extremity functional deficits or pain? (2) Is the magnitude of recovery different if enrolled more than 2 years after their injury versus earlier? (3) Does participation decrease the number considering late amputation?
Methods
We prospectively evaluated 84 service members (53 less than and 31 > 2 years after injury) who enrolled in the initiative. Fifty-eight sustained fractures, 53 sustained nerve injuries with weakness, and six had arthritis (there was some overlap in the patients with fractures and nerve injuries, which resulted in a total of > 84). They completed 4 weeks of physical therapy without the orthosis followed by 4 weeks with it. Testing was conducted at Weeks 0, 4, and 8. Validated physical performance tests and patient-reported outcome surveys were used as well as questions pertaining to whether patients were considering an amputation.
Results
By 8 weeks, patients improved in all physical performance measures and all relevant patient-reported outcomes. Patients less than and greater than 2 years after injury improved similarly. Forty-one of 50 patients initially considering amputation favored limb salvage at the end of 8 weeks.
Conclusions
We found this integrated orthotic and rehabilitation initiative improved physical performance, pain, and patient-reported outcomes in patients with severe, traumatic lower extremity deficits and that these improvements were sustained for > 2 years after injury. Efforts are underway to determine whether the Return to Run clinical pathway with the Intrepid Dynamic Exoskeletal Orthosis (IDEO) can be successfully implemented at additional military centers in patients > 2 years from injury while sustaining similar improvements in patient outcomes. The ability to translate this integrated orthotic and rehabilitation program into the civilian setting is unknown and warrants further investigation.
Level of Evidence
Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Extremity injuries account for the majority of injuries sustained in combat [14] and are responsible for the majority of in-hospital costs and associated long-term disabilities [3, 13]. Patients who sustain high-energy limb-threatening trauma are often faced with the decision between amputation and limb salvage. In the largest study evaluating outcomes after limb salvage or amputation for high-energy lower extremity trauma in a civilian population, patients had equivalent patient-reported functional outcomes [2, 11]. However, regardless of whether a patient underwent amputation or limb salvage, patients remained severely disabled both at 2 and 7 years after injury [2, 12]. Additionally, a recent retrospective study evaluating patient-reported outcomes in a military combat-wounded population also found service members who underwent limb salvage had high levels of disability that were more significant than the service members who had undergone bilateral lower extremity amputations [5].
Before injury, service members typically run, jump, and perform energy-intensive, high-impact tasks necessary for combat readiness. Although not all of these tasks may be possible after injury, many service members view the ability to run as a surrogate for returning to normal life activities. Continued activity limitation, weakness, and pain are three primary factors that play a role in a patient’s decision to abandon the limb salvage pathway and undergo late amputation (defined as > 90 days from injury) at a rate of up to 15% [10, 21].
The Return to Run clinical pathway is a dynamic high-intensity rehabilitation program designed to return military patients undergoing limb salvage to high-level physical function with the additional goal of decreasing the likelihood patients will opt for late amputation [16, 17]. The program combines high-intensity physical therapy with the Intrepid Dynamic Exoskeletal Orthosis (IDEO). The IDEO is a customized, carbon fiber energy storage and return orthosis that returns the energy stored during the stance phase of gait to help power pushoff. It consists of a proximal patellar tendon-bearing ground reaction cuff connected by carbon fiber posterior struts to a distal supramalleolar ankle-foot orthosis (Fig. 1). The IDEO has been shown in a small cohort of patients undergoing limb salvage to result in better functional performance and to decrease the number of patients undergoing limb salvage who were considering amputation [18]. However, this study occurred at a single time point and data on validated, patient-reported outcomes were not collected.
Fig. 1.

The IDEO is shown.
The purpose of this study was to determine if 8 weeks of participation in the Return to Run clinical pathway resulted in improvement in validated patient-reported functional outcomes and objective physical performance measures in patients with lower extremity functional deficits or pain that limits their activities. We also determined if the magnitude of recovery differed between patients who enrolled > 2 years after injury, late-entry patients, compared with those who enrolled < 2 years after injury, early-entry patients. Finally, we sought to determine whether participation in this initiative decreases patients’ willingness to consider late amputation.
Patients and Methods
We conducted a prospective, longitudinal, observational dual-cohort study. Testing the patients before and after the intervention allowed the patients to act as their own controls. This is a short-term followup report of the first 84 patients enrolled between January 30, 2012, and December 20, 2012. Patients were selected based on the following inclusion criteria: active-duty men and nonpregnant women 18 years or older who had a functional deficit of the lower extremity as well as muscle weakness, nerve injury, volumetric muscle loss, or significant pain precluding normal function and full rehabilitation participation; able to bear full weight on bilateral lower extremities; who had completed definitive surgical treatment; and were beginning their participation in the Return to Run clinical pathway. Although this work focused on lower extremity trauma, this study included three patients with injuries at the level of the spine that affected the lower extremity making them functionally similar to the remainder of the cohort. Additionally, a healthy contralateral limb was not required for inclusion.
One hundred eight patients were eligible for the study. A total of 24 patients (22%) were excluded: 21 patients were lost to followup, two withdrew consent, and one withdrew for medical reasons. There was a small subset of patients who did not complete the testing at Week 0 as a result of the physical inability to do so and a small subset at the beginning of the study that did not complete testing at the end of Week 4; however, all patients included for the final analysis had full data for Week 8. The final study group consisted of 84 patients with a broad range of injury diagnoses including lower extremity fractures, nerve and other soft tissue injuries, and posttraumatic or degenerative osteoarthritis (Table 1). The majority of the patients had symptoms from multiple injury categories including mechanical pain, neuropathic pain, weakness, stiffness, and muscle loss with an average of 3.1 injury categories per patient (range, 1–5 categories) (Table 2). Patients began participation in the Return to Run an average of 3 years after injury. Thirty-one patients started the Return to Run clinical pathway > 2 years after their injury (late-entry cohort) and 53 patients started within 2 years after injury (early-entry cohort).
Table 1.
Clinical characteristics
| Demographic and injury factors | Values |
|---|---|
| Sex | 79 male, 5 female |
| Laterality | 10 bilateral, 35 left, 38 right |
| Time from date of injury at enrollment | 3.04 years (range, 0.25–22.4 years) |
| Early entry (enrolled < 2 years after injury) | 53 patients |
| Late entry (enrolled > 2 years after injury) | 31 patients |
| Mechanism of injury | 82% high energy (explosion, fall from |
| height, GSW, MVC) | |
| 18% low energy sports-related/degenerative | |
| Tobacco users | 23 |
| History of TBI | 29 (23 mild, 5 moderate, 1 severe) |
| Lower extremity injury diagnoses | |
| Fractures | 58 (69%) patients |
| Femur | 2 (2%) |
| Tibia (diaphyseal) | 20 (24%) |
| Tibial plafond/ankle | 23 (27%) |
| Hindfoot (talus/calcaneus) | 29 (35%) |
| Forefoot/midfoot | 12 (14%) |
| Nerve injury | 53 (63%) patients |
| Proximal to the knee | 8 (15%) |
| Distal to the knee | 45 (85%) |
| Osteoarthritis | 6 (7%) patients |
| Posttraumatic | 5 (6%) |
| Degenerative | 1 (1%) |
TBI = traumatic brain injury; GSW = gunshot wound; MVC = motor vehicle collision.
Table 2.
Symptom-related injury categories
| Injury category | Number of patients |
|---|---|
| Lower extremity weakness | 73 (87%) |
| Mechanical pain | 67 (80%) |
| Stiffness | 54 (64%) |
| Neuropathic pain | 43 (52%) |
| Muscle loss | 21 (25%) |
The Return to Run clinical pathway has previously been described [15–17]. Briefly, the Return to Run program is a sports medicine-style rehabilitation program that incorporates a strength training program, plyometrics, and agility training. Once the IDEO is received, the program focuses on running, cutting, jumping, and military-specific training while using the energy-storing orthosis. For this study, patients initially completed a 4-week physical therapy program focused on strength training, functional movement, and core muscle strengthening to improve their force-generating ability. For the majority of patients, this portion of therapy was home-based. The patients were then fit with the IDEO and underwent an additional 4 weeks of physical therapy focused on proper use of the device to maximize energy storage and return during both low- and high-impact activities.
Patient demographics and injury data were collected at the patient’s initial visit for enrollment into the study (Week 0). Physical performance evaluations and validated patient-reported outcomes questionnaires, as described subsequently, were completed at Week 0, the end of Week 4 before receiving the IDEO, and at Week 8 after completing the physical therapy training in the IDEO. A patient questionnaire was also completed at Week 0 and Week 8 to determine the prevalence of patients who were considering amputation at the start of the program and the number who still were considering amputation at the end of the program.
The patient-reported outcomes included the Short Musculoskeletal Function Assessment (SMFA), the Veterans Rand 12 item health Survey (VR-12), and the visual analog pain scale (VAS). The SMFA is designed to detect differences in patient function and how bothersome the patient perceives their injury to be [6]. The VR-12 is a 12-question health survey based on the SF-12 that assesses physical functioning, role limitations resulting from physical problems, bodily pain, general health perceptions, vitality, social functioning, role limitations resulting from emotional problems, and mental health [9]. The VR-12 is used to compute two scores: a physical and mental component score. The VAS was used to assess the patient’s average level of pain while wearing the IDEO.
Patients enrolled in this study were all active-duty service members and at preinjury baseline were highly functioning, physically fit individuals. This study assessed four physical performance measures: the four square step test, the timed stair ascent, self-selected walking velocity [22], and the 20-m shuttle run at each time point. All of the measures except the 20-m shuttle run have been previously validated in young, healthy active-duty service members [22]. At the beginning of this study, 30 healthy subjects underwent testing for the 20-m shuttle run. They completed three trials of the measure on 2 separate days. Patients completed three trials of each measure. Each patient was timed by one of six research assistants (SG, KA, DL, MF, DM, AG) who had been trained in the testing method. The four square step test is a test of balance and agility [4]; the patient must change directions quickly while maintaining balance. A 1-inch high obstacle in the shape of a Maltese cross is placed on the floor. The patient was instructed to begin in the back, left quadrant and then to move (1) forward; (2) sideways right; (3) backward; then (4) sideways left and then to move in the reverse direction back to the original square. They were to move as fast as possible with one foot at a time but each foot had to touch the floor in each square. The timed stair ascent is a test of power. The patient was instructed to ascend 12 stairs as fast as possible while touching each stair with alternating feet and without using the handrail. Time started on the command “go” and ended when both feet reached the 12th step. Self-selected walking velocity is a test of general physical mobility and overall disability [8]. Patients were instructed to walk 25 m at a comfortable pace and the middle 15 m was timed to calculate the patient’s speed. The 20-m shuttle run assesses power, deceleration, and ability to change pace. Patients were instructed to move to a cone 10 m away and then return to the start point as fast as possible. They were allowed to rest for 5 minutes among each of the three trials.
A questionnaire pertaining to amputation was included at 8 weeks. The initial question asked, “Have you ever considered amputation of your injured leg?” It then asked the reasons why (pain, weakness, inability to run/jump). The next question was “Are you now favoring keeping your injured leg?” The answers to these questions were used to determine who was considering amputation and the number of patients favoring limb salvage after 8 weeks of the Return to Run clinical pathway.
A one-way analysis of variance (ANOVA) with repeated measures was used to examine the change in each of the physical performance measures and patient-reported outcomes during the course of the study (Week 0, Week 4, and Week 8) in both the full 84-patient cohort and the 31-patient late entry group. A two-way ANOVA with repeated measures and the Tukey-Kramer adjustment for multiple comparisons were used to determine if there were differences in the rate and magnitude of improvement in the scores in each of the physical performance measures and questionnaire scores between the early-entry and late-entry groups of patients. If the overall magnitude of change or rate of change was found to be statistically significant, the individual week p values were listed at the bottom of the table. The effect size was determined using the difference of the means. SAS 9.2 (SAS Institute Inc, Cary, NC, USA) was used for all statistical analysis. Statistical significance was set at p < 0.05.
Results
Physical Performance, Pain, and Patient-reported Outcomes
Improvements were seen in each of the four physical performance measures from Week 4 to Week 8 and in the four square step test, self-selected walking velocity, and timed stair ascent from Week 0 to Week 8 (effect size range, 24%–166%). No improvements were found for Week 0 to Week 4 (Fig. 2A–D). Despite instructions to walk at a comfortable pace during the self-selected walking velocity test, 17 patients completed the test in a manner inconsistent with the instruction (eg, walking very rapidly). Previously published data from young, healthy active-duty individuals suggest a mean self-selected walking velocity of 1.5 m/s. To prevent overestimation of treatment effect, the 17 patients who walked at a pace greater than the highest velocity in the healthy population (> 1.93 m/s) were excluded from the self-selected walking velocity test analysis [22].
Fig. 2A–D.
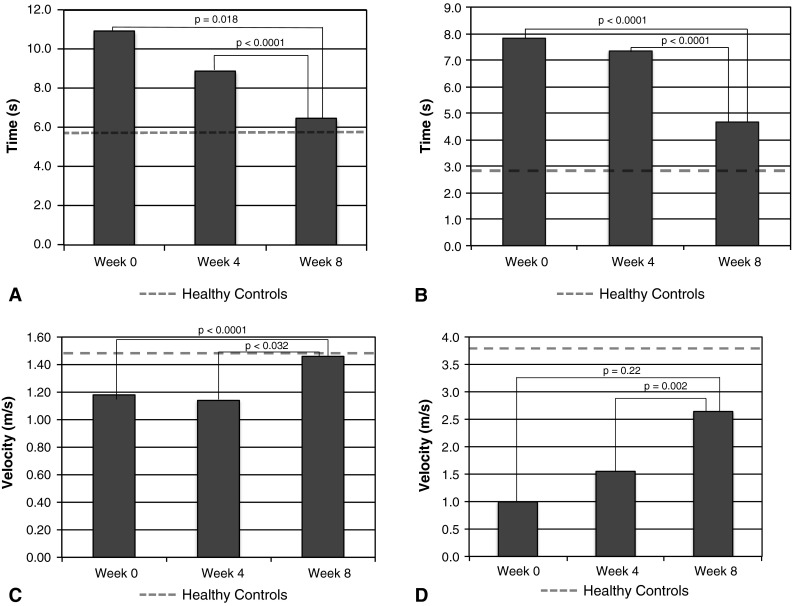
The graphs show the change in the (A) time for the four square step test (effect size 4.5 seconds, 41%); (B) time for the timed stair ascent (effect size 3.2 seconds, 40%); (C) speed for the self-selected walking velocity (effect size 0.3 m/s, 24%); and (D) speed for the 20-m shuttle run (effect size 1.6 m/s, 165%).
Patients with lower extremity disability improved in the VAS pain scores and SMFA scores except in the function of the arm and hand subcategory (effect sizes range, 23%–35% improvement, all p < 0.0001). Physical health VR-12 scores improved from Week 0 to Week 8 and Week 4 to Week 8 (p < 0.0001). The mental health VR-12 score demonstrated improvement from Week 0 to Week 8 only (p < 0.013) (Table 3).
Table 3.
Patient-reported outcome measures for the combined cohort (n = 84)
| Outcome measure | Week 0 | Week 4 | Week 8 | p value | p value | p value | Effect size |
|---|---|---|---|---|---|---|---|
| Week 0 to > 4 | Week 0 to > 8 | Week 4 to > 8 | Week 0 to > 8 | ||||
| Short Form Musculoskeletal Assessment | |||||||
| Daily activities | 36 | 35 | 23 | 0.97 | < 0.0001 | < 0.0001 | 35% |
| Emotional status | 48 | 46 | 37 | 0.28 | < 0.0001 | < 0.0001 | 23% |
| Mobility | 42 | 42 | 30 | 0.99 | < 0.0001 | < 0.0001 | 30% |
| Function | 33 | 32 | 23 | 0.86 | < 0.0001 | < 0.0001 | 29% |
| Bothersome | 36 | 35 | 23 | 0.73 | < 0.0001 | < 0.0001 | 37% |
| Arm | 5 | 5 | 5 | 0.71 | 0.36 | 0.94 | |
| Visual analog pain scale | |||||||
| Pain scale rating | 3.9 | 3.8 | 2.7 | 0.96 | < 0.0001 | < 0.0001 | 31% |
| Veteran Rand 12-item Health Survey | |||||||
| Mental component score | 48 | 48 | 51 | 0.8 | 0.013 | 0.58 | |
| Physical component score | 27 | 29 | 37 | 0.2 | < 0.0001 | < 0.0001 | 34% |
Influence of Early versus Late Enrollment in the Program
The late-entry patients improved in all physical performance measures and all patient-reported outcomes from Weeks 0 and 8 (effect size ranges, 16%–45% and 27%–38% improvement, respectively, p value range 0.002 to < 0.0001) and Weeks 4 and 8 except the arm and hand function subcategory of the SMFA and the mental health VR-12 score (Table 4). There were similar rates of improvement between the early-entry and late-entry groups in all physical performance measures (p > 0.097). For all physical performance measures, except the timed stair ascent, the magnitudes of improvement were similar (p values listed Table 5). In the timed stair ascent, the early-entry group started out slower but the groups were similar at Week 8 (Table 5).
Table 4.
Change over time for the greater than 2 years after injury cohort (n = 31)
| Week 0 | Week 4 | Week 8 | p value Week 0 to > 4 |
p value Week 0 to > 8 |
p value Week 4 to > 8 |
Effect size Week 0 to > 8 |
|
|---|---|---|---|---|---|---|---|
| Patient-reported outcomes | |||||||
| Short Form Musculoskeletal Assessment | |||||||
| Daily activities | 32 | 31 | 21 | 0.88 | 0.0002 | 0.001 | 34% |
| Emotional status | 51 | 47 | 37 | 0.25 | < 0.0001 | 0.001 | 27% |
| Mobility | 42 | 41 | 28 | 0.94 | < 0.0001 | < 0.0001 | 31% |
| Function | 31 | 30 | 22 | 0.71 | < 0.0001 | < 0.0001 | 33% |
| Bothersome | 35 | 33 | 20 | 0.86 | < 0.0001 | < 0.0001 | 31% |
| Arm | 3 | 2 | 2 | 0.37 | 0.21 | 0.93 | |
| Visual analog pain scale | |||||||
| Pain scale rating | 4.8 | 4.5 | 3.2 | 0.66 | < 0.0001 | 0.002 | 33% |
| Veteran Rand 12-item Health Survey | |||||||
| Mental component score | 48 | 49 | 52 | 0.79 | 0.0874 | 0.08 | |
| Physical component score | 27 | 30 | 37 | 0.13 | < 0.0001 | 0.002 | 38% |
| Physical performance measures | |||||||
| Four square step test (seconds) | 8.8 | 8.3 | 6.3 | 0.39 | < 0.0001 | < 0.0001 | |
| Time stair ascent (seconds) | 6.2 | 6.0 | 4.2 | 0.55 | 0.0004 | 0.001 | |
| Self-selected Walking Velocity (m/s) | 1.27 | 1.30 | 1.50 | 0.35 | 0.0008 | 0.006 | |
| 20-m shuttle run (m/s) | 1.8 | 1.9 | 2.6 | 0.74 | < 0.0001 | < 0.0001 | |
Table 5.
Magnitude of change comparison of physical performance measures in early entry (n = 53) versus late entry (n = 31) patients
| Measure | Time after injury | Week 0 | Week 4 | Week 8 | Magnitude of improvement p value |
|---|---|---|---|---|---|
| Four square | Early entry | 12.1 | 9.2 | 6.6 | 0.28 |
| step test (s) | Late entry | 8.8 | 8.5 | 6.3 | |
| Timed stair | Early entry | 8.2 | 8.3 | 4.9 | 0.013* |
| ascent (s)* | Late entry | 6.2 | 5.9 | 4.2 | |
| Self-selected walking | Early entry | 1.15 | 1.06 | 1.43 | 0.06 |
| velocity (m/s) | Late entry | 1.33 | 1.33 | 1.54 | |
| 20-m shuttle | Early entry | 0.8 | 1.3 | 2.6 | 0.34 |
| run (m/s) | Late entry | 1.8 | 1.9 | 2.6 |
* Timed stair ascent: Week 0 p = 0.006, Week 4 p = 0.055, Week 8 p = 0.08.
There were similar magnitudes and rates of improvement (p > 0.3) for all patient-reported outcomes except VAS between the early-entry and late-entry groups as well (magnitudes; Table 6). The late-entry group had a higher VAS score at Week 0 (4.9 versus 3.3, p = 0.001) that remained higher at Week 8 (3.3 versus 2.3, p = 0.04). However, the rate of improvement of change was similar between the late-entry and early-entry groups (p = 0.3) (Table 6).
Table 6.
Magnitude of change comparison of patient-reported outcomes in early entry (n = 53) versus late entry (n = 31)
| Measure | Time after injury | Week 0 | Week 4 | Week 8 | Magnitude of improvement p value |
|---|---|---|---|---|---|
| Short Musculoskeletal Function Assessment | |||||
| Daily | Early entry | 38 | 38 | 24 | 0.12 |
| Late entry | 31 | 31 | 21 | ||
| Emotional | Early entry | 46 | 45 | 36 | 0.55 |
| Late entry | 50 | 47 | 37 | ||
| Mobility | Early entry | 43 | 43 | 30 | 0.60 |
| Late entry | 42 | 41 | 28 | ||
| Function | Early entry | 33 | 33 | 24 | 0.35 |
| Late entry | 31 | 30 | 22 | ||
| Bothersome | Early entry | 37 | 36 | 25 | 0.31 |
| Late entry | 35 | 33 | 20 | ||
| Arm | Early entry | 6 | 6 | 6 | 0.15 |
| Late entry | 3 | 2 | 2 | ||
| Visual analog pain scale (VAS)* | |||||
| Early entry | 3.3 | 3.5 | 2.3 | 0.005* | |
| Late entry | 4.9 | 4.7 | 3.3 | ||
* VAS: Week 0 p = 0.002, Week 4 = 0.02, Week 8 p = 0.04.
Does Participation Decrease the Number of Patients Considering Late Amputation?
At enrollment into the program, 50 patients had considered an amputation. The most common reasons were an inability to run/jump (44 [88%]) followed by mechanical pain (43 [86%]), weakness (34 [68%]), and neuropathic pain (27 [54%]). At the conclusion of the 8 weeks in the study, 41 (82%) of those 50 patients now favored limb salvage.
Discussion
Extremity injuries account for the majority of injuries sustained in combat [14] and are responsible for the majority of in-hospital costs and associated long-term disabilities [3, 13]. Previous studies of the Return to Run clinical pathway have demonstrated an improvement in physical performance and higher return to duty and deployment rates than described before initiation of this program [1, 18, 19]. To date, however, there has not been a prospective study to evaluate the effect of the Return to Run clinical pathway and use of the IDEO on patients’ physical performance over time and on validated patient-reported outcomes. The purpose of this study was to determine if 8 weeks of participation in the Return to Run clinical pathway resulted in improvements in patient-reported outcomes and validated physical performance measures. This study also sought to determine if the magnitude of recovery differed between patients who enrolled > 2 years after injury and those who enrolled < 2 years after injury and if the Return to Run clinical pathway affected patients’ willingness to consider a late amputation.
There were several limitations to this study. We did not have a control group that completed only physical therapy without the use of the IDEO for 8 weeks. A previous study at this institution found the IDEO improved patients’ physical performance on specific tasks more than two other commercially available ankle-foot orthoses and no brace [18]. Given the apparent clinical success of the Return to Run clinical pathway with the IDEO in returning patients to duty [1], the limited improvements with rehabilitation alone, as demonstrated by the lack of significant improvement in the first 4 weeks of this study when the IDEO was not worn, and we believe this issue had already been addressed by our prior study [18], we believe it would have been inappropriate to randomize the patients to rehabilitation with and without the IDEO.
This study was conducted solely in active-duty service members, the majority of whom sustained high-energy injuries in a combat environment. These are generally highly motivated patients who are physically fit before injury; it is unknown how civilian patients would respond to this program. However, the physical therapy portion of the Return to Run clinical pathway, as modified for this study, involved 4 weeks of home-based physical therapy to increase extremity and core strength and functional capacity before receiving the IDEO; it is not unlike other physical therapy programs used in the civilian sector. The IDEO combined with physical therapy may be useful in a subset of patients who are motivated and have exhausted other measures to improve functional capabilities and decrease distal lower extremity pain. Also, the severity of the injuries may differ between military and civilian patients, particularly blast injuries. The followup for this cohort was only 8 weeks. In light of growing concerns regarding the cost of medical care, a program capable of delivering positive results over a short period of time is advantageous. However, long-term followup will be necessary to determine whether these improvements can be maintained. Finally, of the 108 patients initially enrolled, 24 (22%) did not participate in the 8-week followup. A unique limitation of our population is the majority of service members in this study traveled to our institution from remote facilities for short periods of time and sometimes they may have been required to leave the training earlier than anticipated. This may have precluded them from completing full followup.
Finally, patients in this study had a wide complement of injuries and symptoms associated with those diagnoses resulting in a heterogeneous patient population (Tables 1, 2). Based on this, there were two challenges in this study with subgroup analysis. The first is the majority of the patients had multiple symptoms in their limb (average of 3.1 per patient) contributing to their lower extremity functional limitations, making division into subgroups challenging. Additionally, this cohort consisted of a relatively small number of patients for the number of diagnoses and would result in relatively small subgroups for analysis. A subgroup analysis or multivariable regression analysis would be appropriate in the future with a larger number of patients.
The Lower Extremity Assessment Project study group found worsening patient-reported outcomes between 2 and 7 years after injury in patients who had sustained high-energy lower extremity trauma and underwent limb salvage, which contradicted prior thought that continued recovery would occur during this late phase [2, 12]. Multiple small studies have shown similarly poor outcomes with respect to patient-reported outcomes in patients undergoing limb salvage [7, 20]. In contrast, this prospective study showed improvement from Week 0 to Week 8 in patient-reported outcomes both in the full cohort of patients and the cohort that was > 2 years from the time of injury. Likewise, there was an improvement in validated physical performance measures. Other than a preliminary study performed here on patients undergoing limb salvage [18], we are unaware of any other studies prospectively evaluating validated physical performance measures in patients undergoing limb salvage to quantify their improvement. Comparison to the normative data in an active-duty military population [22] reveals that after 8 weeks in the Return to Run clinical pathway, patients were able to return to a near normal self-selected walking velocity (1.46 m/s compared with 1.5 m/s) and approach a normal time for the four square step test (6.5 seconds compared with 5.7 seconds). However, in the more physically demanding tasks, the timed stair ascent and 20-m shuttle run, the patients improved but were not as fast as their uninjured peers. Further study is needed to determine if performance continues to improve with time.
Ultimately, the patients gained enough improvement in the 8 weeks of the Return to Run clinical pathway that 41 of 50 patients (82%) who initially were considering amputation at Week 0 favored limb salvage after completing the 8 weeks of the program. A recent study in an active-duty military population found better patient-reported outcomes in amputees compared with patients undergoing limb salvage, even if the service member had undergone bilateral lower extremity amputation [5]. A key aspect of that study was that the injuries occurred between 2003 and 2007 before the development of the IDEO and the Return to Run clinical pathway. The lack of a standardized postinjury rehabilitation program and custom orthotic for the patients undergoing limb salvage likely contributed to their findings. The data in this current study suggest the IDEO may provide an advantage by combining the ability for energy storage and return similar to an energy-storing prosthetic. Furthermore, the proximal portion of the IDEO is modeled after a patella tendon-bearing prosthetic. This may allow enough off-loading of the lower leg to provide pain relief along with ground reaction propulsion.
Also with respect to amputation, we aimed to obtain data on how many patients enrolled in this intervention had pain or disability severe enough that they considered amputation. Likewise, we queried the effect this intervention had, at least in the short term, affected their feelings on amputation. We directly asked the patients in two dichotomous questions regarding their consideration of amputation surgery. Although the decision to pursue an amputation is a complex and multifactorial decision, we believe the patient’s perspective on this is one of the most important measures of this program. Also, the results were not shared directly with the treating clinicians to reduce the likelihood of participants biasing their answers to meet clinician preference. These questions were also intended to help guide our clinical recommendation of attempting 8 weeks of this intervention versus amputation. If patients in this study demonstrated improvements in pain and function but the majority still desired amputation after 8 weeks, our clinical recommendation of which patients should go through this intervention may need to include only those patients who do not initially consider amputation. However, as demonstrated in this population, 41 of 50 patients who initially considered amputation favored limb salvage at the end of 8 weeks. In the future, we hope to assess at long-term followup how many patients actually elect to have an amputation.
In conclusion, patients who completed 8 weeks of the Return to Run clinical pathway with the IDEO improved in terms of validated physical performance measures, patient-based outcomes, and decreased desire for amputation in a short timeframe. Importantly, improvements also occurred in the patients who began the Return to Run clinical pathway and enrolled in this study > 2 years after their injury, a patient population previously shown to become more disabled with time. The strengths of this study include the prospective assessment of patient-reported outcomes and physical performance measures at multiple time points before the Return to Run clinical pathway, before receiving the IDEO at the end of the intervention, allowing patient comparison over time. Additional study is necessary to determine if the documented benefits are sustained. Finally, efforts are underway to determine if the Return to Run clinical pathway with the IDEO can be successfully implemented at additional military centers and in patients > 2 years from injury while sustaining similar improvements in patient outcomes. The ability to translate this integrated orthotic and rehabilitation program into the civilian setting is unknown and warrants further investigation.
Acknowledgments
We thank Andrea Garza for her assistance as the research nurse overseeing this study. We also thank Socorro Garcia, Kerri Anguiano, Dennis Mann, Donna Lopez, and Mary Fan for assistance with carrying out the testing and Eduardo Anguiano for assistance with data management and John Jones for assistance with the statistics.
Footnotes
One of the authors (RVB) is the developer of the Intrepid Dynamic Exoskeletal Orthosis but does not have any financial interests, patent, or licensing agreements. One of the authors (JRH) is on the speakers’ bureau for Smith & Nephew (Memphis, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at San Antonio Military Medical Center, Fort Sam Houston, TX, USA. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Army, Department of Defense, or the US Government.
References
- 1.Blair JA, Patzkowski JC, Blanck RV, Owens JG, Hsu JR, Skeletal Trauma Research Consortium (STReC). Return to duty after integrated orthotic and rehabilitation initiative. J Orthop Trauma. 2013 Oct 10 [Epub ahead of print]. [DOI] [PubMed]
- 2.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347:1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 3.Cross JD, Ficke JR, Hsu JR, Masini BD, Wenke JC. Battlefield orthopaedic injuries cause the majority of long-term disabilities. J Am Acad Orthop Surg. 2011;19(Suppl 1):S1–S7. doi: 10.5435/00124635-201102001-00002. [DOI] [PubMed] [Google Scholar]
- 4.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83:1566–1571. doi: 10.1053/apmr.2002.35469. [DOI] [PubMed] [Google Scholar]
- 5.Doukas WC, Hayda RA, Frisch HM, Andersen RC, Mazurek MT, Ficke JR, Keeling JJ, Pasquina PF, Wain HJ, Carlini AR, MacKenzie EJ. The Military Extremity Trauma Amputation/Limb Salvage (METALS) study: outcomes of amputation versus limb salvage following major lower-extremity trauma. J Bone Joint Surg Am. 2013;95:138–145. doi: 10.2106/JBJS.K.00734. [DOI] [PubMed] [Google Scholar]
- 6.Engelberg R, Martin DP, Agel J, Swiontkowski MF. Musculoskeletal function assessment: reference values for patient and non-patient samples. J Orthop Res. 1999;17:101–109. doi: 10.1002/jor.1100170116. [DOI] [PubMed] [Google Scholar]
- 7.Georgiadis GM, Behrens FF, Joyce MJ, Earle AS, Simmons AL. Open tibial fractures with severe soft-tissue loss. Limb salvage compared with below-the-knee amputation. J Bone Joint Surg Am. 1993;75:1431–1441. doi: 10.2106/00004623-199310000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- 9.Kazis LE, Miller DR, Clark J, Skinner K, Lee A, Rogers W, Spiro A, 3rd, Payne S, Fincke G, Selim A, Linzer M. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 10.Krueger CA, Wenke JC, Ficke JR. Ten years at war: comprehensive analysis of amputation trends. J Trauma Acute Care Surg. 2012;73:S438–S444. doi: 10.1097/TA.0b013e318275469c. [DOI] [PubMed] [Google Scholar]
- 11.MacKenzie EJ, Bosse MJ. Factors influencing outcome following limb-threatening lower limb trauma: lessons learned from the Lower Extremity Assessment Project (LEAP) J Am Acad Orthop Surg. 2006;14:S205–S210. doi: 10.5435/00124635-200600001-00044. [DOI] [PubMed] [Google Scholar]
- 12.MacKenzie EJ, Bosse MJ, Pollak AN, Webb LX, Swiontkowski MF, Kellam JF, Smith DG, Sanders RW, Jones AL, Starr AJ, McAndrew MP, Patterson BM, Burgess AR, Castillo RC. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg Am. 2005;87:1801–1809. doi: 10.2106/JBJS.E.00032. [DOI] [PubMed] [Google Scholar]
- 13.Masini BD, Waterman SM, Wenke JC, Owens BD, Hsu JR, Ficke JR. Resource utilization and disability outcome assessment of combat casualties from Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma. 2009;23:261–266. doi: 10.1097/BOT.0b013e31819dfa04. [DOI] [PubMed] [Google Scholar]
- 14.Owens BD, Kragh JF, Jr, Wenke JC, Macaitis J, Wade CE, Holcomb JB. Combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma. 2008;64:295–299. doi: 10.1097/TA.0b013e318163b875. [DOI] [PubMed] [Google Scholar]
- 15.Owens JG. Physical therapy of the patient with foot and ankle injuries sustained in combat. Foot Ankle Clin. 2010;15:175–186. doi: 10.1016/j.fcl.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Owens JG, Blair JA, Patzkowski JC, Blanck RV, Hsu JR. Skeletal Trauma Research Consortium (STReC). Return to running and sports participation after limb salvage. J Trauma. 2011;71:S120–S124. doi: 10.1097/TA.0b013e3182219225. [DOI] [PubMed] [Google Scholar]
- 17.Patzkowski JC, Blanck RV, Owens JG, Wilken JM, Blair JA, Hsu JR. Can an ankle-foot orthosis change hearts and minds? J Surg Orthop Adv. 2011;20:8–18. [PubMed] [Google Scholar]
- 18.Patzkowski JC, Blanck RV, Owens JG, Wilken JM, Kirk KL, Wenke JC, Hsu JR. Skeletal Trauma Research Consortium (STReC). Comparative effect of orthosis design on functional performance. J Bone Joint Surg Am. 2012;94:507–515. doi: 10.2106/JBJS.K.00254. [DOI] [PubMed] [Google Scholar]
- 19.Patzkowski JC, Owens JG, Blanck RV, Kirk KL, Hsu JR, Skeletal Trauma Research Consortium (STReC) Deployment after limb salvage for high-energy lower-extremity trauma. J Trauma Acute Care Surg. 2012;73:S112–S115. doi: 10.1097/TA.0b013e3182606291. [DOI] [PubMed] [Google Scholar]
- 20.Sanders R, Pappas J, Mast J, Helfet D. The salvage of open grade IIIB ankle and talus fractures. J Orthop Trauma. 1992;6:201–208. doi: 10.1097/00005131-199206000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Stinner DJ, Burns TC, Kirk KL, Ficke JR. Return to duty rate of amputee soldiers in the current conflicts in Afghanistan and Iraq. J Trauma. 2010;68:1476–1479. doi: 10.1097/TA.0b013e3181bb9a6c. [DOI] [PubMed] [Google Scholar]
- 22.Wilken JM, Darter BJ, Goffar SL, Ellwein JC, Snell RM, Tomalis EA, Shaffer SW. Physical performance assessment in military service members. J Am Acad Orthop Surg. 2012;20(Suppl 1):S42–S47. doi: 10.5435/JAAOS-20-08-S42. [DOI] [PubMed] [Google Scholar]


