Abstract
Background
Key factors limiting patients with lower extremity amputations to achieve maximal functional capabilities are falls and fear of falling. A task-specific fall prevention training program has successfully reduced prospectively recorded trip-related falls that occur in the community by the elderly. However, this program has not been tested in amputees.
Questions/purposes
In a cohort of unilateral transtibial amputees, we aimed to assess effectiveness of a falls prevention training program by (1) quantifying improvements in trunk control; (2) measuring responses to a standardized perturbation; and (3) demonstrating retention at 3 and 6 months after training. Second, we collected patient-reported outcomes for balance confidence and falls control.
Methods
Fourteen male military service members (26 ± 3 years) with unilateral transtibial amputations and who had been walking without an assistive device for a median of 10 months (range, 2–106 months) were recruited to participate in this prospective cohort study. The training program used a microprocessor-controlled treadmill designed to deliver task-specific postural perturbations that simulated a trip. The training consisted of six 30-minute sessions delivered over a 2-week period, during which task difficulty, including perturbation magnitude, increased as the patient’s ability progressed. Training effectiveness was assessed using a perturbation test in an immersive virtual environment. The key outcome variables were peak trunk flexion and velocity, because trunk kinematics at the recovery step have been shown to be a determinant of fall likelihood. The patient-reported outcomes were also collected using questionnaires. The effectiveness of the rehabilitation program was also assessed by collecting data before perturbation training and comparing the key outcome parameters with those measured immediately after perturbation training (0 months) as well as both 3 and 6 months posttraining.
Results
Mean trunk flexion angle and velocity significantly improved after participating in the training program. The prosthetic limb trunk flexion angle improved from pretraining (42°; 95% confidence interval [CI], 38°–47°) to after training (31°; 95% CI, 25°–37°; p < 0.001). Likewise, the trunk flexion velocity improved from pretraining (187°/sec; 95% CI, 166°–209°) to after training (143°/sec; 95% CI, 119°–167°; p < 0.004). The results display a significant side-to-side difference for peak trunk flexion angle (p = 0.01) with perturbations of the prosthetic limb resulting in higher peak angles. Prosthetic limb trips also exhibited significantly greater peak trunk flexion velocity compared with trips of the prosthetic limb (p = 0.005). These changes were maintained up to 6 months after the training. The peak trunk flexion angle of the subjects when the prosthetic limb was perturbed had a mean of 31° (95% CI, 25°–37°) at 0 month, 32° (95% CI, 28°–37°) at 3 months, and 30° (95% CI, 25°–34°) at 6 months. Likewise, the peak trunk flexion velocity for the prosthetic limb was a mean of 143°/sec (95% CI, 118°–167°) at 0 months, 143°/sec (95% CI, 126°–159°) at 3 months, and 132° (95% CI, 115°–149°) at 6 months. The peak trunk flexion angle when the nonprosthetic limb was perturbed had a mean of 22° (95% CI, 18°–24°) at 0 months, a mean of 26° (95% CI, 20°–32°) at 3 months, and a mean of 23° (95% CI, 19°–28°) at 6 months. The peak trunk flexion velocity for the nonprosthetic limb had a mean of 85°/sec (95% CI, 71°–98°) at 0 months, a mean of 96° (95% CI, 68°–124°) at 3 months, and 87°/sec (95% CI, 68°–105°) at 6 months. There were no significant changes in the peak trunk flexion angle (p = 0.16) or peak trunk flexion velocity (p = 0.35) over time after the training ended. The skill retention was present when either the prosthetic or nonprosthetic limb was perturbed. There were side-to-side differences in the trunk flexion angle (p = 0.038) and trunk flexion velocity (p = 0.004). Perturbations of the prosthetic side resulted in larger trunk flexion and higher trunk flexion velocities. Subjects prospectively reported decreased stumbles, semicontrolled falls, and uncontrolled falls.
Conclusions
These results indicate that task-specific fall prevention training is an effective rehabilitation method to reduce falls in persons with lower extremity transtibial amputations.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The US military is currently fitting patients who have amputations with state-of-the-art prosthetic devices. However, some patients and their care providers learn that advanced technology does not always lead to high function. Key factors that limit the ability of individuals with amputations to achieve maximal functional capabilities are falls and fear of falling. People with a leg amputation have a greater risk of falling than the general public. The reported incidences of falls are 20% to 32% during rehabilitation [10, 34] and 52% within the community [29]. The increased rate of falling in individuals with lower limb amputations is not surprising because they tend to perform very poorly on balance-related functional tests [7, 8, 49]. Furthermore, 65% of individuals with lower limb amputation have reduced balance confidence [30]. As a result of the reduced balance confidence, up to 76% of these individuals with lower limb amputations avoid activities as a direct result of the lack of confidence [28].
Falls are also an issue for older adults. Approximately one-third of ambulatory, community-dwelling older adults fall each year [14]. These falls reduce balance confidence and increase the fear of falling [18], which in turn leads to a loss of mobility [50] physical activity [47], and balance control [23], further increasing fall risk. Trips and slips account for 59% of older adult falls [3]. Failed compensatory steps have been observed in 45% of older adult falls in the free-living environment [17]. Although compensatory stepping is impaired with older age [13, 24, 26, 33, 39], it is a modifiable skill that improves with practice [4, 11, 40, 46]. A task-specific fall prevention training program has been developed based on compensatory step training that has successfully reduced trip-related falls by the elderly after laboratory-induced trips [11] and prospectively reported trip-related falls that occur in the community [41].
In the current military and healthcare environment, it is essential to focus on rapid, safe, and maximum improvement of functional skills with a goal of prompt discharge from rehabilitation and return to active duty or civilian life. Therefore, the purpose of this study was to extend a task-specific fall prevention training technique to the rehabilitation of active-duty service members who have sustained trauma-related limb loss and amputation. We aimed to assess training effectiveness by (1) quantifying improvements in trunk flexion angle and velocity; (2) measuring responses to a standardized perturbation; and (3) demonstrating retention at 3 and 6 months after training. Second, we collected patient-reported outcomes for balance confidence and falls control. We hypothesized that task-specific training would reduce fall risk in military patients with amputations.
Patients and Methods
This prospective cohort study compared changes in outcome variables after trip-specific perturbation training. Between September 2011 and March 2013, participants who were active-duty members of the US military were recruited from the Comprehensive Combat & Complex Casualty Care (C5) program at the Naval Medical Center San Diego (NMCSD). Inclusion criteria were traumatic unilateral transtibial amputation, between the ages of 18 and 40 years who were ambulating without an assistive device, medically cleared for high-level functional activities, and able to walk easily for more than 15 minutes. Subjects were excluded if they had traumatic brain injury, vestibular dysfunction, significant traumatic injury of the contralateral limb, pain, or neuromuscular problems. The experimental protocol was approved by the NMCSD, Naval Health Research Center (NHRC), and Mayo Clinic institutional review board as well as the Human Research Protection Office, US Army Medical Research and Materiel Command. Subjects provided written informed consent before participating in the study.
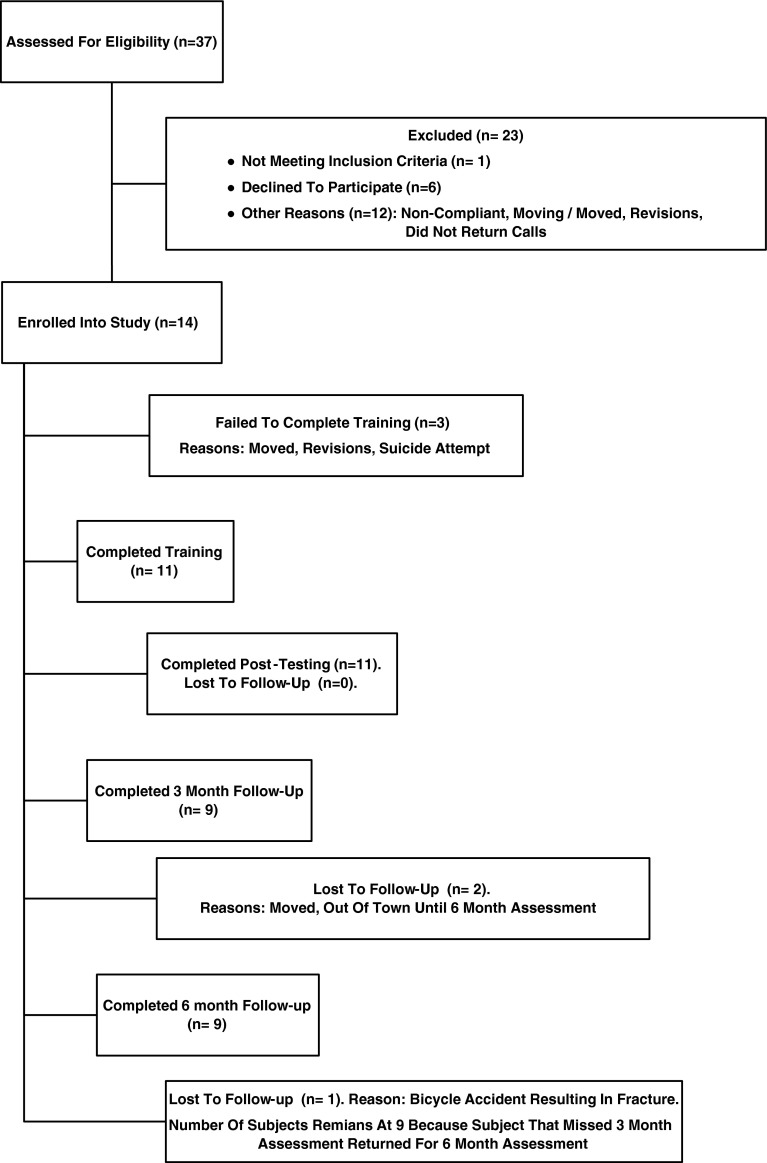
Thirty-seven charts were examined for eligibility (Fig. 1). Twenty-three subjects were excluded. Individuals did not participate because of contralateral limb involvement, time commitment/time conflict (could not or would not dedicate the time as a result of work, school, or therapies), socket-fit issues, residual limb issues such as infections and heterotopic ossification, moving from the area before participation could be completed, or mental health/posttraumatic stress disorder issues. Fourteen male subjects (mean [± SD] age, 26 ± 3 years; body mass index, 23 ± 3 kg/m2) enrolled in this study. The subjects studied had a radiographic residual limb length of 48 ± 8% (range, 29%–58%) of the intact limb measured from the medial joint line to the medial malleolus. Subjects were enrolled a median of 12 months (range, 5–113 months) after amputation and a median of 10 months (range, 2–106 months) after they became able to walk without assistive devices. All subjects were highly functional (Medicare Functional Classification Level K3 or K4). All subjects had custom sockets made by one of two in-house prosthetists. All subjects wore carbon fiber-type feet (Re-Flex Shock™, Vari-Flex™, or Re-Flex Rotate™; Össur, Reykjavik, Iceland). The high functionality of the participants in the study is reflected by the fact that their Activities-Specific Balance Confidence (ABC) Scale score was 90 ± 9 (95% confidence interval [CI], 86–95) before training and did not change significantly after training (p = 0.86). Three subjects did not finish training: one dropped out as a result of a needed revision of his residual limb, one had mental health issues and could not continue, and one moved out of the area. None of the dropouts were related to the training program. Of the 14 subjects who started the study, 11 completed the training, the initial posttraining assessment, and the 3-month and 6-month assessments.
Fig. 1.
The diagram shows the recruitment and flow of subjects in the study.
The trip-specific fall prevention training program used an ActiveStep Treadmill™ (Symbex, Lebanon, NH, USA). This microprocessor-controlled treadmill was designed to deliver bidirectional (forward and backward) postural disturbances ranging from benign to extremely challenging. Three types of perturbations (static perturbation, static walk, and e-trip) were used during each of six 30-minute training sessions that were delivered over a 2-week period. The perturbation intensity, ie, treadmill belt acceleration, was increased each visit according to the subject’s ability. The static perturbation was delivered while the patient was standing on the treadmill and the belt was initially stationary. The subject was instructed to avoid falling by using a single forward recovery step after the onset of treadmill belt motion. The static walk was similar to the static perturbation, but after the initial recovery step, the subject continued walking until the treadmill belt motion stopped. These disturbances were more challenging as a result of their larger acceleration and longer treadmill belt displacement. Finally, during the e-trip disturbance, the perturbation was delivered randomly while the subject was walking on the treadmill. This perturbation required a stepping response consisting of multiple forward steps. The progression of the perturbations involved increasing the task difficulty as the patient’s ability to avoid falling improved. The subject wore a safety harness, which encompassed the trunk and could support the subject’s full weight. The harness was tethered to an instrumented safety system (Interface Inc, Scottsdale, AZ, USA). The tether length was set so that the subject’s hands and knees would not contact the treadmill belts in the event of a fall. The tether did not interfere with normal walking.
Assessment of the training program effectiveness was also performed using a Computer-Assisted Rehabilitation Environment (CAREN) extended version (Motek Medical BV, Amsterdam, The Netherlands). This fully immersive virtual environment consists of a six degrees of freedom motion platform (Moog Inc, East Aurora, NY, USA) with a 1.7-m dual belt (side-by-side) instrumented treadmill (Forcelink, BV, Culemborg, The Netherlands) capable of accelerations up to 15 m/sec2. The platform is surrounded by a 180° screen. Visual inputs were synchronized with the subject’s treadmill walking speed to simulate walking on an endless pastoral path (Fig. 2). The walking speed for each subject was controlled for leg length by normalizing to a Froude number (FR) of 0.2, where FR = v2/gl, v is the walking speed, g is the gravitational constant, and l is the leg length [1]. The speed was based on the overground self-selected walking speed of subjects with amputation previously studied in the NMCSD Motion Analysis Laboratory [44]. In addition, the speed was approximately 2% slower than their self-selected walking speed to increase the likelihood that subjects could maintain a constant speed for the duration of the perturbation trial (approximately 15 minutes) without fatigue. Walking speeds ranged from 1.0 to 1.5 m/sec.
Fig. 2.

Photograph of a subject walking within the CAREN at the NHRC in San Diego.
The protocol allowed for a warm-up period of walking for 10 minutes at the normalized walking speed before the perturbation testing to acclimate the subjects with the treadmill environment. After the warm-up period, while subjects walked for 5 to 6 minutes at their normalized velocity [44], six perturbations (three prosthetic, three nonprosthetic) were delivered in a randomized order.
During the perturbation testing, motion capture data were recorded from 34 retroreflective markers placed on the subject using a modified Helen Hayes marker set configuration [19]. The marker trajectories were tracked with a 12-camera motion capture system (Motion Analysis Corp, Santa Rosa, CA, USA) operating at 120 Hz. Marker data were filtered using a fourth-order bidirectional recursive Butterworth filter with a cutoff frequency of 9 Hz (Visual3D™; C-Motion, Inc, Germantown, MD, USA). A 13-segment rigid body model was created using the marker data.
To reduce changes resulting from the learning effects of the perturbation recovery, the first trial was dropped and only the last two perturbation trials on each limb were analyzed for each visit. The key outcome variables were peak trunk flexion and velocity. These variables have been shown to be determinants of the likelihood of a fall [5, 32]. Trunk flexion angle was defined as the angle of the trunk segment with respect to vertical. Trunk flexion velocity was computed as a derivative of the trunk flexion angle time series. The maximum values were determined during the timeframe from perturbation of the target limb to the moment of foot contact during the recovery step of the perturbed limb. Higher flexion values and velocities are indicative of less trunk flexion control.
Patient-reported outcomes were also collected. Subjects completed the ABC Scale [37] and the Prosthesis Evaluation Questionnaire Addendum (PEQ-A) [12]. The 16-item ABC Scale, a reliable, valid, and responsive instrument for assessing individuals who have a unilateral lower limb amputation [27], was used to assess the subject’s perceived balance confidence. Subjects rated their balance confidence on a scale from 0% (no confidence) to 100% (very confident) that they would not lose their balance when performing specific activities such as reaching overhead, bathing, and climbing stairs [37]. The PEQ-A consists of 14 questions regarding subject confidence, concentration, stumbles, and falls. For the questionnaire, a semicontrolled fall was defined as a loss of balance with awareness that a fall was occurring and resulting in the opportunity to brace for the fall or grasp something to not get hurt and/or land in a protected fashion. An uncontrolled fall was defined as a sudden loss of balance without any time to protect against a fall.
The effectiveness of the rehabilitation program was assessed by collecting data before perturbation training and comparing the key outcome parameters with those measured immediately after perturbation training (zero months) as well as at 3 and 6 months posttraining. Data were assessed for normality using the Anderson-Darling test. A two- factor repeated-measures analysis of variance was used to assess the effectiveness of the training program. The two independent variables were time and side (prosthetic limb, nonprosthetic limb). Statistical analyses were performed using SAS 9.2 software (SAS Institute Inc, Cary, NC, USA). Statistical significance was set at p ≤ 0.05.
Results
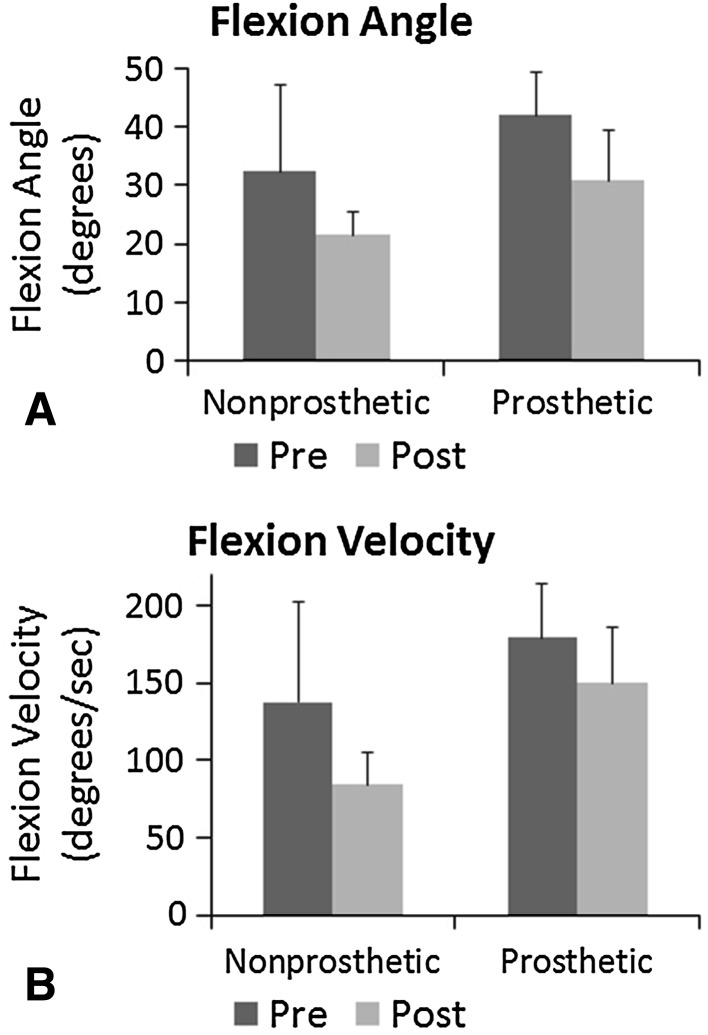
The training program resulted in decreases in perturbation-induced peak trunk flexion angle and trunk flexion velocity in both prosthetic and nonprosthetic limbs (Fig. 3). The prosthetic limb trunk flexion angle improved from pretraining (42°; 95% CI, 38°–47°) to after training (31°; 95% CI, 25°–37°; p < 0.001). Likewise, the trunk flexion velocity improved from pretraining (187°/sec; 95% CI, 166°–209°) to after training (143°/sec; 95% CI, 119°–167°; p < 0.004). The results display a significant side-to-side difference for peak trunk flexion angle (p = 0.01) with perturbations of the prosthetic limb resulting in higher peak angles. Prosthetic limb trips also exhibited greater peak trunk flexion velocity compared with trips of the prosthetic limb (p = 0.005).
Fig. 3A–B.
Mean peak (A) trunk flexion angle (degrees) and (B) velocity (degrees per second) before and after training. A trip-like perturbation was delivered to the prosthetic and nonprosthetic limb.
Before beginning the training program, a standard perturbation was administered without telling the subject which leg to use to avoid falling. A subject was considered to pass the standard perturbation if they recovered without assistance from the harness and considered to have failed if they fell and the harness had to catch them. In this pretest condition, 10 of 11 subjects (91%) failed and six of the 11 subjects (55%) elected to recover on the prosthetic limb. After training, the standard perturbation was administered again. Now all subjects passed the standard perturbation and seven of the 11 subjects (64%) chose to use the prosthetic limb to avoid falling. These results demonstrate a greatly increased ability to avoid a fall after a postural disturbance.
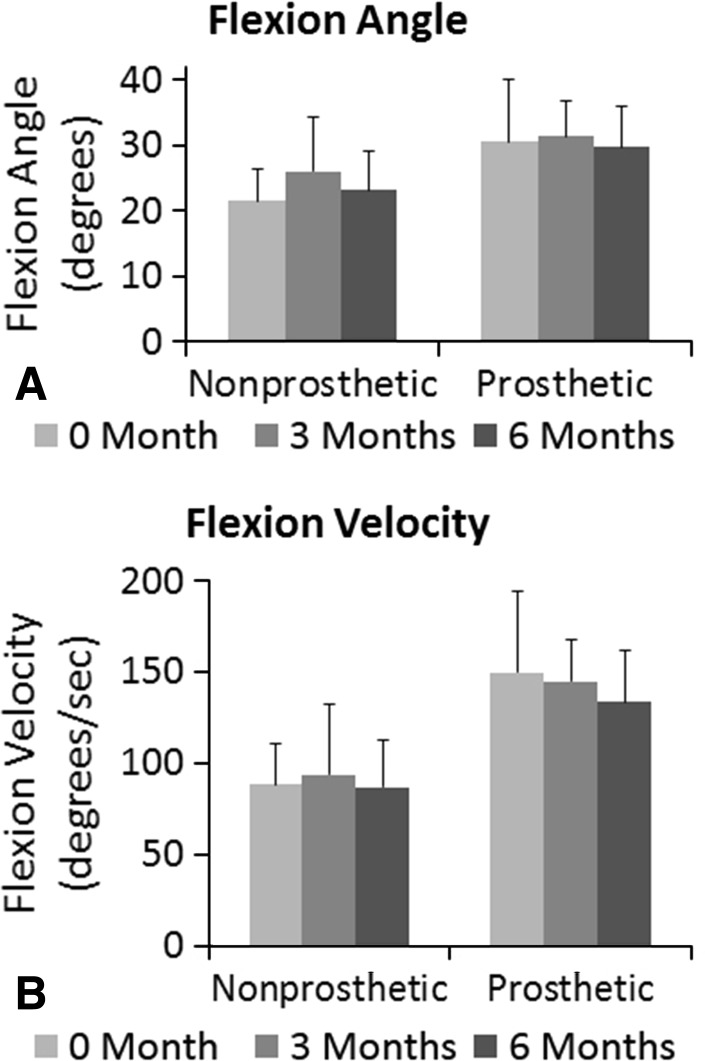
The skills acquired with the perturbation training were retained at 3 and 6 months after training (Fig. 4). The trunk flexion angle of the subjects when the prosthetic limb was perturbed had a mean of 31° (95% CI, 25°–37°) at 0 month, 32° (95% CI, 28°–37°) at 3 months, and 30° (95% CI, 25°–34°) at 6 months. Likewise, the trunk flexion velocity for the prosthetic limb was a mean of 143°/sec (95% CI, 118°–167°) at 0 month, 143°/sec (95% CI, 126°–159°) at 3 months, and 132°/sec (95% CI, 115°–149°) at 6 months. The peak trunk flexion angle when the nonprosthetic limb was perturbed had a mean of 22° (95% CI, 18°–24°) at 0 month, a mean of 26° (95% CI, 20°–32°) at 3 months, and a mean of 23° (95% CI, 19°–28°) at 6 months. The peak trunk flexion velocity for the nonprosthetic limb had a mean of 85°/sec (95% CI, 71°–98°) at 0 month, a mean of 96°/sec (95% CI, 68°–124°) at 3 months, and 87°/sec (95% CI, 68°–105°) at 6 months. There were no significant changes in the peak trunk flexion angle (p = 0.16) or peak trunk flexion velocity (p = 0.35) over time after the training ended. The skill retention was present when either the prosthetic or nonprosthetic limb was perturbed. There were side-to-side differences in the trunk flexion angle (p = 0.038) and trunk flexion velocity (p = 0.004). Perturbations of the prosthetic side resulted in larger trunk flexion and higher trunk flexion velocities.
Fig. 4A–B.
Mean peak (A) trunk flexion angle (degrees) and (B) velocity (degrees per second) at 0, 3, and 6 months after training. A trip-like perturbation was delivered to the prosthetic and nonprosthetic limbs.
Patient-reported outcomes confirmed the success of the training program. Their responses indicated increased confidence in their ability to recover from the postural perturbations in the community. Sixty percent of the subjects reported that the incidence of stumbles had decreased after the training program. Most of the subjects (80%) indicated that the number of semicontrolled falls had been reduced to zero after training. All subjects reported that the number of uncontrolled falls was zero after training. Reduction of stumbles and falls was maintained over time.
Discussion
US military men and women have been returning from combat with a higher percentage of amputations compared with other recent military conflicts [36]. The primary rehabilitation goal for these individuals has been to provide them with an expedited recovery and reintroduction into the civilian or active-duty population [2]. In the current military and healthcare environments, it is essential to focus on rapid but safe training of functional skills with a goal of early discharge from rehabilitation to active-duty or civilian life. Although the results of this study are promising, there are several limitations that need to be noted. First, a limited number of biomechanical variables were included in this investigation. Variables selected were based on previous studies, which have indicated these are the key outcome parameters to assess fall risk. Second, the current study only reported on patients with transtibial amputations. Further work is underway to investigate if outcomes are similar when patients with transfemoral amputations are trained with the same training method. Third, patients with significant comorbidities were excluded to eliminate confounding variables. It is unknown how these patients will respond to this training program. Fourth, this study was limited to young service members who had all sustained traumatic amputations. The efficacy of this training program for older individuals who had an amputation has not been demonstrated.
After training, the subjects were able to control their trunk to a greater degree. Trunk control is associated with reduced fall risk. The majority (59%) of adult falls are the result of trips and slips [3]. The ability to control balance is a critical condition for minimizing the risk of falls [38]. The skills necessary to recover from the treadmill-induced postural disturbances such as resisting trunk rotation and quickly executing long steps [6, 32, 43] are the same skills required to recover from trips [35] and slips [48]. The focus of the rehabilitation program was to increase the ability of the subjects to respond to large postural perturbations and perform the recovery steps necessary to avoid a fall. The training method used in this study allowed patients with amputations to learn how to perform a complex motor task in a safe environment and maintain gait stability despite the poor somatosensory feedback from their prosthesis and residual limb [9, 16, 20, 22]. This type of training is not addressed in most rehabilitation programs and, to our knowledge, has not previously been used to retrain persons with lower limb amputation. The rate at which these skills are acquired is multifactorial and includes the level of amputation, the patient’s motivation, and motor skills.
There was a dramatic difference in the response to a standardized postural disturbance before and after training. The novel methodology used in this training program focused on skill acquisition. The acquisition of motor skill is reinforced by the fact that all subjects, with one exception, fell during the pretest before training began, whereas none of the subjects fell during the posttest. This demonstrates that the success of the training program is not simply the result of time since amputation, but rather acquisition of motor skills. The foundational principle of the program is that of specificity of training [15], the premise of which is that the extent to which the conditions during which a motor skill is learned/practiced overlap with the conditions for which the learning/practice is intended dictates the degree to which the learned motor skill can be transferred. Practice of the modified motor task results in a new, readily available context-specific motor skill that can “bring about predetermined results with maximum certainty” (attributed to Knapp [21] by Ovens and Smith [31]). The results obtained in this study indicate that task-specific training is an effective rehabilitation method to reduce falls in individuals with unilateral transtibial amputation.
The posttraining improvement in the ability of the subjects to avoid falling was retained for 6 months. Traditionally, rehabilitation has focused on the design and function of the patient’s prosthesis rather than on the skills the person needs to acquire to use the prosthesis. Motor skill retention is consistent with the findings of previous studies. A key characteristic of the rehabilitation program was the induced, large perturbation-driven dynamic instability that required performance of a motor skill, ie, the stepping, or recovery response, in a repeatable and consistent manner. Constant training has been shown to result in better skill acquisition [25] and strong retention from day to day [45]. The training was distributed over several days, which has been shown to be the most important factor affecting learning and retention [42].
This article has introduced a novel and effective rehabilitation method that uses an innovative treadmill training technique. The training is aimed at increasing the ability of patients with lower limb amputations to rely on their prosthesis during challenging perturbations and thus improve their functional capabilities. The results obtained in this study also indicate that task-specific training can be an effective rehabilitation method to reduce falls in individuals with unilateral transtibial amputation.
Acknowledgments
We thank Jordan Sturdy, Trevor Kingsbury, Nancy Thesing, Katie Sharp, John-David Collins, Mandy Wong, Grant Myers, and Birgit Unfried for contributing to this research project.
Footnotes
This study was funded by the Department of Defense Grant Number W81X-WH-11-2-0058 (Log No. DM090896) and the Navy Bureau of Medicine and Surgery, Wounded, Ill, and Injured Program. Approved for public release; distribution is unlimited. This research was conducted in compliance with all applicable federal regulations governing the protection of human subjects (protocol NMCSD.2001.003 and Protocol NHRC.2001.0031). The institution of one or more of the authors (MDG) has a patent on technology (ActiveStep™; Symbex, Lebanon, NH, USA) noted in this manuscript. One of the authors (MDG) is an inventor of the ActiveStep™ system but has no conflicts of interest to declare with regard to the present study.
The views expressed are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Patients were recruited from the Comprehensive Combat & Complex Casualty Care (C5) program at the Naval Medical Center San Diego, San Diego, CA, USA.
References
- 1.Alexander RM. Optimization and gaits in the locomotion of vertebrates. Physiol Rev. 1989;69:1199–1227. doi: 10.1152/physrev.1989.69.4.1199. [DOI] [PubMed] [Google Scholar]
- 2.Andersen R, Davis S, Scoville C. Rehabilitation of military amputees: from injury to independence. Orthopedics. 2008;31:100–1002. doi: 10.3928/01477447-20110525-05. [DOI] [PubMed] [Google Scholar]
- 3.Berg WP, Alessio HM, MIlls EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–268. doi: 10.1093/ageing/26.4.261. [DOI] [PubMed] [Google Scholar]
- 4.Bieryla KA, Madigan ML, Nussbaum MA. Practicing recovery from a simulated trip improves recovery kinematics after an actual trip. Gait Posture. 2007;26:208–213. doi: 10.1016/j.gaitpost.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 5.Crenshaw JR, Kaufman KR, Grabiner MD. Trip recoveries of people with unilateral transfemoral and knee disarticulation amputations. Gait Posture. 2013;38:500–506. doi: 10.1016/j.gaitpost.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 6.Crenshaw JR, Rosenblatt NJ, Hurt CP, Grabiner MD. The discriminant capabilities of stability measures, trunk kinematics, and step kinematics in classifying successful and failed compensatory stepping responses by young adults. J Biomech. 2012;45:129–133. doi: 10.1016/j.jbiomech.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch Phys Med Rehabil. 2007;88:109–114. doi: 10.1016/j.apmr.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Franchignoni F, Orlandini D, Ferriero G, Moscato TA. Reliability, validity, and responsiveness of the locomotor capabilities index in adults with lower-limb amputation undergoing prosthetic training. Arch Phys Med Rehabil. 2004;85:743–748. doi: 10.1016/j.apmr.2003.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Geurts ACH, Mulder TW, Nienhuis B, Rijken RA. Postural reorganization following lower limb amputation. Possible motor and sensory determinants of recovery. Scand J Rehabil Med. 1992;24:83–90. [PubMed] [Google Scholar]
- 10.Gooday HM, Hunter J. Preventing falls and stump injuries in lower limb amputees during inpatient rehabilitation: completion of the audit cycle. Clin Rehabil. 2004;18:379–390. doi: 10.1191/0269215504cr738oa. [DOI] [PubMed] [Google Scholar]
- 11.Grabiner MD, Bareither ML, Gatts S, Marone J, Troy KL. Task-specific training reduces trip-related fall risk in women. Med Sci Sports Exerc. 2012;44:2410–2414. doi: 10.1249/MSS.0b013e318268c89f. [DOI] [PubMed] [Google Scholar]
- 12.Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil. 2007;88:207–217. doi: 10.1016/j.apmr.2006.10.030. [DOI] [PubMed] [Google Scholar]
- 13.Hall CD, Jensen JL. Age-related differences in lower extremity power after support surface perturbations. J Am Geriatr Soc. 2002;50:1782–1788. doi: 10.1046/j.1532-5415.2002.50505.x. [DOI] [PubMed] [Google Scholar]
- 14.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 15.Henry FM. Specificity versus Generality in Learing Motor Skills. Englewood Cliffs, NJ, USA: Prentice Hall; 1968. [Google Scholar]
- 16.Hermodsson Y, Ekdahl C, Persson BM, Roxendal G. Standing balance in trans-tibial amputees following vascular disease or trauma: a comparative study with healthy subjects. Prosthet Orthot Int. 1994;18:150–158. doi: 10.3109/03093649409164400. [DOI] [PubMed] [Google Scholar]
- 17.Holliday PJ, Fernie G, Gryfe CI, Griggs GT. Video recording of spontaneous falls of the elderly. In: ASTM STP 1103. Slips, Stumbles, and Falls: Pedestrian Foorwear and Surfaces. Philadelphia, PA, USA: American Society for Testing and Materials; 1990:7–16.
- 18.Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A. Covariates of fear of falling and associated activity curtailment. Gerontologist. 1998;38:549–555. doi: 10.1093/geront/38.5.549. [DOI] [PubMed] [Google Scholar]
- 19.Kadaba M, Ramakrishnan H, Wootten M. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 20.Kavounoudias A, Tremblay C, Gravel D, Iancu A, Forget R. Bilateral changes in somatosensory sensibility after unilateral below-knee amputation. Arch Phys Med Rehabil. 2005;86:633–640. doi: 10.1016/j.apmr.2004.10.030. [DOI] [PubMed] [Google Scholar]
- 21.Knapp B. Skill in Sport–the Attainment of Proficiency. London, UK: Routledge & Kegan Paul PLC; 1963. [Google Scholar]
- 22.Liao KI, Skinner HB. Knee joint proprioception in below-knee amputees. Am J Knee Surg. 1995;8:105–109. [PubMed] [Google Scholar]
- 23.Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991;46:M123–M131. doi: 10.1093/geronj/46.4.M123. [DOI] [PubMed] [Google Scholar]
- 24.Mansfield A, Maki BE. Are age-related impairments in change-in-support balance reactions dependent on the method of balance perturbation? J Biomech. 2009;42:1023–1031. doi: 10.1016/j.jbiomech.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 25.Memmert D. Long-term effects of type of practice on the learning and transfer of a complex motor skill. Percept Mot Skills. 2006;103:912–916. doi: 10.2466/pms.103.3.912-916. [DOI] [PubMed] [Google Scholar]
- 26.Mille ML, Rogers MW, Martinez K, Hedman LD, Johnson ME, Lord SR, Fitzpatrick RC. Thresholds for inducing protective stepping responses to external perturbations of human standing. J Neurophysiol. 2003;90:666–674. doi: 10.1152/jn.00974.2002. [DOI] [PubMed] [Google Scholar]
- 27.Miller WC, Deathe AB, Speechley M. Psychometric properties of the Activities-Specific Balance Confidence Scale among individuals with a lower limb amputation. Arch Phys Med Rehabil. 2003;84:656–661. doi: 10.1016/S0003-9993(02)04807-4. [DOI] [PubMed] [Google Scholar]
- 28.Miller WC, Deathe AB, Speechley M, Koval J. The influence of falling, fear of falling, and balance confidence on prosthetic mobility and social activity among individuals with a lower extremity amputation. Arch Phys Med Rehabil. 2001;82:1238–1244. doi: 10.1053/apmr.2001.25079. [DOI] [PubMed] [Google Scholar]
- 29.Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil. 2001;82:1031–1037. doi: 10.1053/apmr.2001.24295. [DOI] [PubMed] [Google Scholar]
- 30.Miller WC, Speechley M, Deathe AB. Balance confidence among people with lower-limb amputations. Phys Ther. 2002;82:856–865. [PubMed] [Google Scholar]
- 31.Ovens A, Smith W. Skill: making sense of a complex concept. Journal of Physical Education New Zealand. 2006;39:72–82. [Google Scholar]
- 32.Owings TM, Pavol MJ, Grabiner MD. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin Biomech. 2001;16:813–819. doi: 10.1016/S0268-0033(01)00077-8. [DOI] [PubMed] [Google Scholar]
- 33.Pai YC, Rogers MW, Patton J, Cain TD, Hanke TA. Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults. J Biomech. 1998;31:1111–1118. doi: 10.1016/S0021-9290(98)00124-9. [DOI] [PubMed] [Google Scholar]
- 34.Pauley T, Devlin M, Heslin K. Falls sustained during inpatient rehabilitation after lower limb amputation: prevalence and predictors. Am J Phys Med Rehabil. 2006;85:521–532. doi: 10.1097/01.phm.0000219119.58965.8c. [DOI] [PubMed] [Google Scholar]
- 35.Pavol MJ, Owings TM, Foley KT, Grabiner MD. Mechanisms leading to a fall from an induced trip in healthy older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M428–M437. doi: 10.1093/gerona/56.7.M428. [DOI] [PubMed] [Google Scholar]
- 36.Potter BK, Scoville CR. Amputation is not isolated: an overview of the US Army Amputee Patient Care Program and associated amputee injuries. J Am Acad Orthop Surg. 2006;14:S188–S190. doi: 10.5435/00124635-200600001-00041. [DOI] [PubMed] [Google Scholar]
- 37.Powell LE, Myers AM. The Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–M34. doi: 10.1093/gerona/50A.1.M28. [DOI] [PubMed] [Google Scholar]
- 38.Quai TM, Brauer SG, Nitz JC. Somatosensation, circulation and stance balance in elderly dysvascular transtibial amputees. Clin Rehabil. 2005;19:668–676. doi: 10.1191/0269215505cr857oa. [DOI] [PubMed] [Google Scholar]
- 39.Rogers MW, Hedman LD, Johnson ME, Cain TD, Hanke TA. Lateral stability during forward-induced stepping for dynamic balance recovery in young and older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M589–M594. doi: 10.1093/gerona/56.9.M589. [DOI] [PubMed] [Google Scholar]
- 40.Rosenblatt N, Marone J, Grabiner MD. Task-specific trainning decreases falls by older women in the community: 6 month prospective data. Gerontologist. 2010;50:412. [Google Scholar]
- 41.Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. J Am Geriatr Soc. 2013;61:1629–1631. doi: 10.1111/jgs.12428. [DOI] [PubMed] [Google Scholar]
- 42.Savion-Lemieux T, Penhune VB. The effects of practice and delay on motor skill learning and retention. Exp Brain Res. 2005;161:423–431. doi: 10.1007/s00221-004-2085-9. [DOI] [PubMed] [Google Scholar]
- 43.Schulz BW, Ashton-Miller JA, Alexander NB. Compensatory stepping in response to waist pulls in balance-impaired and unimpaired women. Gait Posture. 2005;22:198–209. doi: 10.1016/j.gaitpost.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 44.Sessoms PH, Wyatt M, Grabiner MD, Collins JD, Kingsbury T, Thesing N, Kaufman K. Method for evoking a trip-like response using a treadmill-based perturbation during locomotion. J Biomech. 2014;47:277–280. doi: 10.1016/j.jbiomech.2013.10.035. [DOI] [PubMed] [Google Scholar]
- 45.Shadmehr R, Brashers-Krug T. Functional stages in the formation of human long-term motor memory. J Neurosci. 1997;17:409–419. doi: 10.1523/JNEUROSCI.17-01-00409.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. 2004;83:493–499. doi: 10.1097/01.PHM.0000130025.54168.91. [DOI] [PubMed] [Google Scholar]
- 47.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53:M112–M119. doi: 10.1093/gerona/53A.2.M112. [DOI] [PubMed] [Google Scholar]
- 48.Troy KL, Donovan SJ, Marone JR, Bareither ML, Grabiner MD. Modifiable performance domain risk-factors associated with slip-related falls. Gait Posture. 2008;28:461–465. doi: 10.1016/j.gaitpost.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Velzen JM, Van Bennekom CAM, Polomski W, Slootman JR, Van Der Woude VHL, Houdijk H. Physical capacity of walking ability after lower limb amputation: a systematic review. Clin Rehabil. 2006;20:999–1016. doi: 10.1177/0269215506070700. [DOI] [PubMed] [Google Scholar]
- 50.Vellas BJ, Rubenstein LZ, Ousset PJ, Faisant C, Kostek V, Nourhashemi F, Allard M, Albarede JL. One-leg standing balance and functional status in a population of 512 community-living elderly persons. Aging (Milano). 1997;9:95–98. doi: 10.1007/BF03340133. [DOI] [PubMed] [Google Scholar]