Abstract
Background
Medialization of the cup with a respective increase in femoral offset has been proposed in THA to increase abductor moment arms. Insofar as there are potential disadvantages to cup medialization, it is important to ascertain whether the purported biomechanical benefits of cup medialization are large enough to warrant the downsides; to date, studies regarding this question have disagreed.
Questions/purposes
The purpose of this study was to quantify the effect of cup medialization with a compensatory increase in femoral offset compared with anatomic reconstruction for patients undergoing THA. We tested the hypothesis that there is a (linear) correlation between preoperative anatomic parameters and muscle moment arm increase caused by cup medialization.
Methods
Fifteen patients undergoing THA were selected, covering a typical range of preoperative femoral offsets. For each patient, a finite element model was built based on a preoperative CT scan. The model included the pelvis, femur, gluteus minimus, medius, and maximus. Two reconstructions were compared: (1) anatomic position of the acetabular center of rotation, and (2) cup medialization compensated by an increase in the femoral offset. Passive abduction-adduction and flexion-extension were simulated in the range of normal gait. Muscle moment arms were evaluated and correlated to preoperative femoral offset, acetabular offset, height of the greater trochanter (relative to femoral center of rotation), and femoral antetorsion angle.
Results
The increase of muscle moment arms caused by cup medialization varied among patients. Muscle moment arms increase by 10% to 85% of the amount of cup medialization for abduction-adduction and from −35% (decrease) to 50% for flexion-extension. The change in moment arm was inversely correlated (R2 = 0.588, p = 0.001) to femoral antetorsion (anteversion), such that patients with less femoral antetorsion gained more in terms of hip muscle moments. No linear correlation was observed between changes in moment arm and other preoperative parameters in this series.
Conclusions
The benefit of cup medialization is variable and depends on the individual anatomy.
Clinical Relevance
Cup medialization with compensatory increase of the femoral offset may be particularly effective in patients with less femoral antetorsion. However, cup medialization must be balanced against its tradeoffs, including the additional loss of medial acetabular bone stock, and eventual proprioceptive implications of the nonanatomic center of rotation and perhaps joint reaction forces. Clinical studies should better determine the relevance of small changes of moment arms on function and joint reaction forces.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3787-3) contains supplementary material, which is available to authorized users.
Introduction
The classic technique of THA as described by Charnley [6] and Müller [13] includes medialization of the acetabular cup to the medial acetabular wall. To keep the global offset (ie, the sum of the acetabular and femoral offset) anatomic, the femoral offset is increased by the same distance by which the acetabular offset is decreased (Fig. 1). This concept is based on a two-dimensional analysis of lever arms, which leads to the conclusion that the more medial the center of rotation, the more favorable the moment arms.
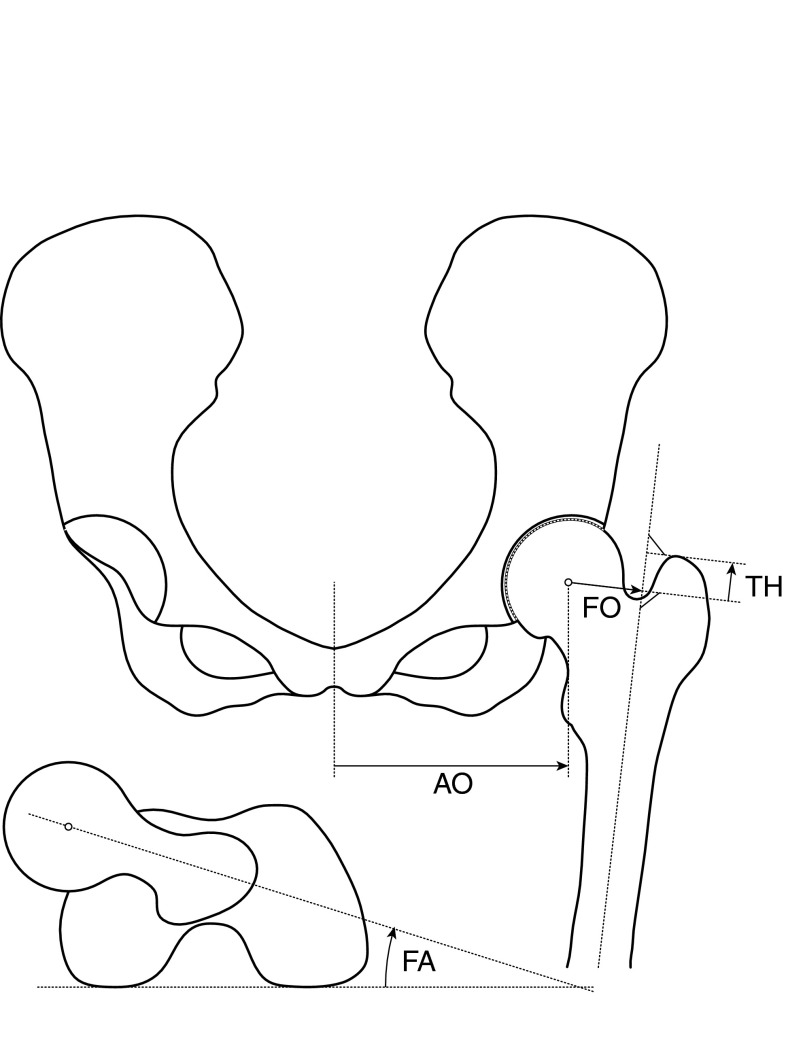
Fig. 1.
A schematic of the pelvis shows the measurements taken from the patients’ CT scans. Femoral offset (FO) is the distance between the axis of the proximal third of the femoral diaphysis and the femoral center of rotation. Femoral antetorsion (FA) is based on the posterior condyles. The height of the greater trochanter (TH) is the vertical distance between the femoral center of rotation and the tip of the greater trochanter. The acetabular offset (AO) is the distance between the acetabular center of rotation and the sagittal pelvic plane.
The downside of cup medialization is threefold. First, a variable amount of bone on the medial aspect of the acetabulum has to be removed. This loss of bone stock might pose a problem in the case of revision surgery, in which cup fixation might be hampered. In addition, in patients with severe osteoporosis, subchondral sclerotic bone might be removed with a negative effect on primary cup stability (ie, press-fit). Second, by moving the center of rotation away from its anatomic position, joint reaction forces are altered with a possible effect on the longevity of the implants. Third, the amplitude of the working length of muscle fibers is altered by changing the offsets and the center of rotation away from an anatomic situation, an effect that might be particularly relevant for the abductor muscles.
Clinically, some studies suggest that a loss of femoral offset is associated with abductor dysfunction. For example, McGrory et al. [12] analyzed 86 THAs at 1 year. Their results suggest that an increased femoral offset improves abductor strength. Asayama et al. [3] observed in a clinical series that a loss of femoral offset by 20% is associated with a significant limp.
Several finite element models have been developed to evaluate the effects of nonanatomic reconstruction on the biomechanics of the hip. Bonnin et al. [5] used a three-dimensional (3-D) finite element model of the femur, pelvis, and bundles of the gluteus minimus and medius. They observed an 8% decrease of the joint force with 5 mm medialization. Delp et al. [7] used a 3-D numerical musculoskeletal model of the hip to evaluate geometric THA parameters. They observed that a center of rotation 2 cm superior relative to its anatomic position with compensatory neck lengthening decreases the abductor moment arm by less than 10%. The model by Delp et al. [7] was later extended by representing muscle as 3-D volumes instead of cables [4]. However, despite numerous clinical and biomechanical studies, the effect of cup medialization on moment arms of the abductor muscles remains unclear. In addition, it remains elusive whether there are pelvic and femoral geometries more susceptible or resistant to biomechanical effects of cup medialization. This lack of biomechanical insight often complicates the choice of the optimal surgical strategy. This decision-making might be facilitated if anatomic parameters predicting a benefit of cup medialization would be identified.
Therefore, the purpose of this project was to quantify the effect of cup medialization with a compensatory increase in femoral offset compared with anatomic reconstruction. We first evaluated the variability of the effect of cup medialization among 15 patients. Then we tested the hypothesis that there is a (linear) correlation between preoperative anatomic parameters and muscle moment arm increase caused by cup medialization. To answer this question, we developed a finite element model of the hip based on preoperative CT scans of patients undergoing THA.
Patients and Methods
Fifteen patients undergoing THA were selected from a series of 50 consecutive patients to account for a broad range of anatomic variability (Table 1). It was ensured that patients with large, medium, and small femoral offsets were included in this study. The study was approved by the institutional review board at our institutions. The following procedure was applied to all of these patients. A preoperative CT scan that included the entire pelvis and the proximal and distal femur was obtained. Using 3-D surgical planning software (Hip-Plan; Symbios Inc, Yverdon, Switzerland), femoral offset, femoral antetorsion (anteversion), height of the greater trochanter relative to the femoral center of rotation (reflecting the degree of varus-valgus anatomy), and acetabular offset were measured. Using the same scan, the pelvis, femur, gluteus medius, gluteus minimus, and gluteus maximus were segmented with the imaging software Amira® (FEI Visualization Sciences Group, Bordeaux, France). Based on this segmentation, we built a surface model of each anatomic structure using Geomagic® software (Geomagic, Research Triangle Park, NC, USA). The THA then was simulated on this geometric model using the software package CATIA (Dassault Systèmes Simulia Corp, Providence, RI, USA). Two types of reconstruction were tested: (1) a strictly anatomic reconstruction with preservation of the center of rotation and the femoral and acetabular offset; and (2) a reconstruction with arbitrary cup medialization of 5 mm and compensatory increase of the femoral offset by 5 mm. This constant distance was chosen because it reflects our estimation of the average capacity of medialization given by the acetabular anatomy. In addition, a constant value allows for more consistent comparisons among patients. The THA was simulated by defining the femoral and acetabular center of rotation, rather than by implantation of a prosthesis. Reconstruction therefore was independent of implant types and sizes, which is important for this theoretical study.
Table 1.
Patients with the four preoperative parameters
| Patient number | Age (years) | Sex | Femoral offset (mm) | Acetabular offset (mm) | Trochanteric height (mm) | Femoral antetorsion (degrees) |
|---|---|---|---|---|---|---|
| 1 | 65 | F | 39 | 93 | 12 | 25 |
| 2 | 61 | M | 46 | 85 | 14 | 34 |
| 3 | 68 | M | 53 | 90 | 15 | 35 |
| 4 | 77 | M | 45 | 88 | 18 | 27 |
| 5 | 74 | F | 39 | 93 | 9 | 42 |
| 6 | 73 | M | 55 | 87 | 18 | 24 |
| 7 | 60 | F | 45 | 88 | 19 | 23 |
| 8 | 72 | F | 47 | 93 | 9 | 19 |
| 9 | 71 | F | 43 | 91 | 14 | 18 |
| 10 | 39 | M | 51 | 88 | 11 | 13 |
| 11 | 47 | F | 31 | 83 | 6 | 34 |
| 12 | 36 | M | 40 | 82 | 10 | 14 |
| 13 | 52 | M | 39 | 86 | 9 | 8 |
| 14 | 57 | M | 39 | 84 | 11 | 33 |
| 15 | 39 | F | 32 | 89 | 1 | 12 |
F = female; M = male.
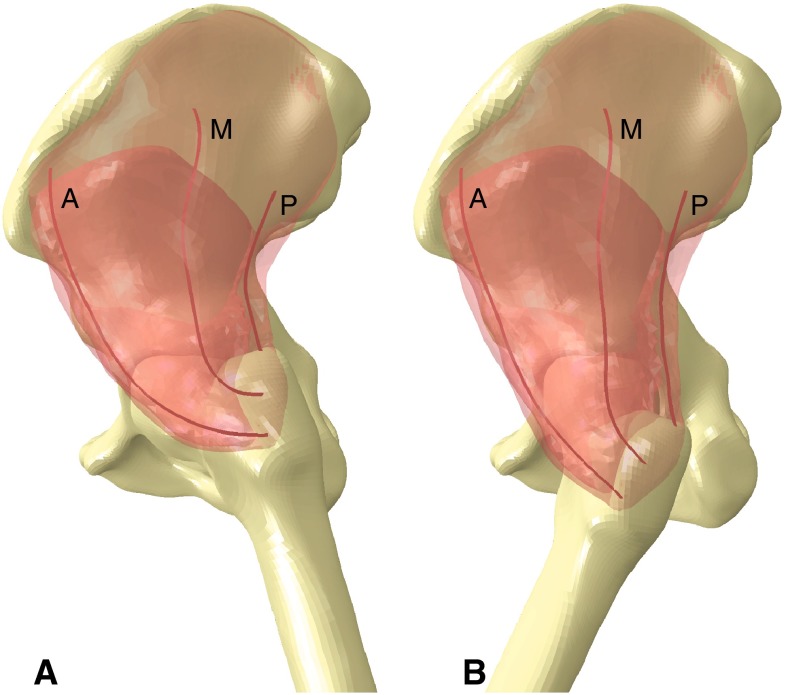
A coordinate system around the pelvis and femur was defined according to Wu et al. [15]. Passive hip motion was simulated in the range of a normal gait cycle [10]; adduction was performed in the coronal plane, from 6° abduction to 6° adduction. Flexion was performed in the parasagittal plane, from 5° extension to 38° flexion. The muscle deformation associated with the passive motion was simulated by the finite element method (Appendix 1. Supplemental material is available with the online version of CORR®). The muscle moment arms were calculated on three fibers in the 3-D volume of the deformable muscles. Three fibers of the gluteus minimus and gluteus medius were selected: a middle fiber in the center of the muscle and an anterior and posterior fiber at one-fifth of the AP width from the anterior and, respectively, posterior border of the muscle (Fig. 2). Moment arms of the three fibers were calculated for each of the two muscles, with and without cup medialization, using the tendon excursion method [2]. Then, the difference of moment arms for each fiber was calculated throughout the gait cycle. This difference was normalized to the maximal theoretical value of 5 mm (100%), because it is impossible that the moment arms of the abductor muscles increase by more than the distance of cup medialization (ie, 5 mm in our model). An average value of this relative difference was calculated separately for abduction and flexion.
Fig. 2A–B.
Sagittal views of the 3-D model show the deformed gluteus medius with the embedded anterior (A), middle (M), and posterior fibers (P) in (A) extended and (B) flexed positions.
We tested the hypothesis that the relative increase of muscle moment arm is linearly correlated with the four preoperative anatomic parameters (actabular and femoral offset, trochanteric height and femoral anteversion). For each parameter we calculated the coefficient of determination (R2) and we tested the null hypothesis that the slope of the correlation is zero. Statistical analysis was done with the Statistics Toolbox™ of MATLAB® (MathWorks, Natick, MA, USA).
Results
For abduction-adduction, the effect of cup medialization on moment arms was consistently positive, ranging from 10% to 85% (Fig. 3). For flexion-extension, the effect was not always positive (Fig. 3). In some cases, cup medialization even decreased the moment arms considerably (eg, Patient 2 by −34%). The effect of cup medialization on moment arms varied among patients and with the two movements, but also between the three fibers. For example, in Patient 5 (Table 1), cup medialization increased the moment arms of the three fibers of the gluteus medius during abduction and flexion (Supplemental Fig. 1. Supplemental material is available with the online version of CORR®). The maximal increase most often was observed in the middle fiber of the gluteus medius: in three of 15 cases in the anterior, in eight of 15 in the middle, and in four of 15 in the posterior fibers (Supplemental Figs. 1–3. Supplemental material is available with the online version of CORR®). In the gluteus minimus it was observed in six of 15, seven of 15, and two of 15 in the anterior, middle, and posterior fibers, respectively.
Fig. 3A–D.
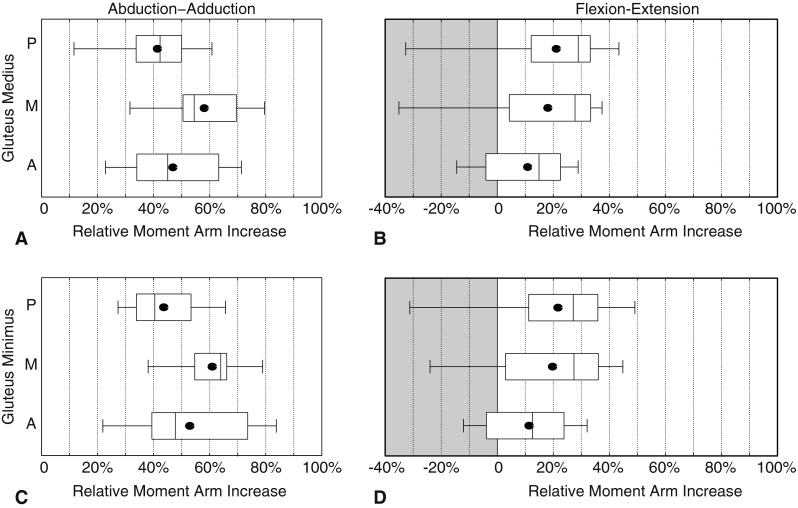
The relative increases of moment arm of the anterior (A), middle (M), and posterior (P) fibers of the gluteus medius during (A) abduction-adduction and (B) flexion-extension and of the gluteus minimus during (C) abduction-adduction and (D) flexion-extension are shown. A value of 0% means no increase and 100% corresponds to the maximum theoretical increase of 5 mm for a medialization of 5 mm. A negative value (gray area) corresponds to a decrease of moment arm. The box plots show the median, quartiles, minimum, maximum, and average (solid circle) of the 15 patients.
For abduction-adduction movements, an inverse correlation (R2 = 0.588, p = 0.001) was observed between cup medialization effect and femoral antetorsion (Fig. 4); that is, cup medialization was more efficient in increasing moment arm for patients with a small femoral antetorsion. However, we did not observe any linear correlation with femoral offset (R2 = 0.015, p = 0.659), acetabular offset (R2 < 0.001, p = 0.990), or height of the greater trochanter (R2 = 0.263, p = 0.051).
Fig. 4A–D.
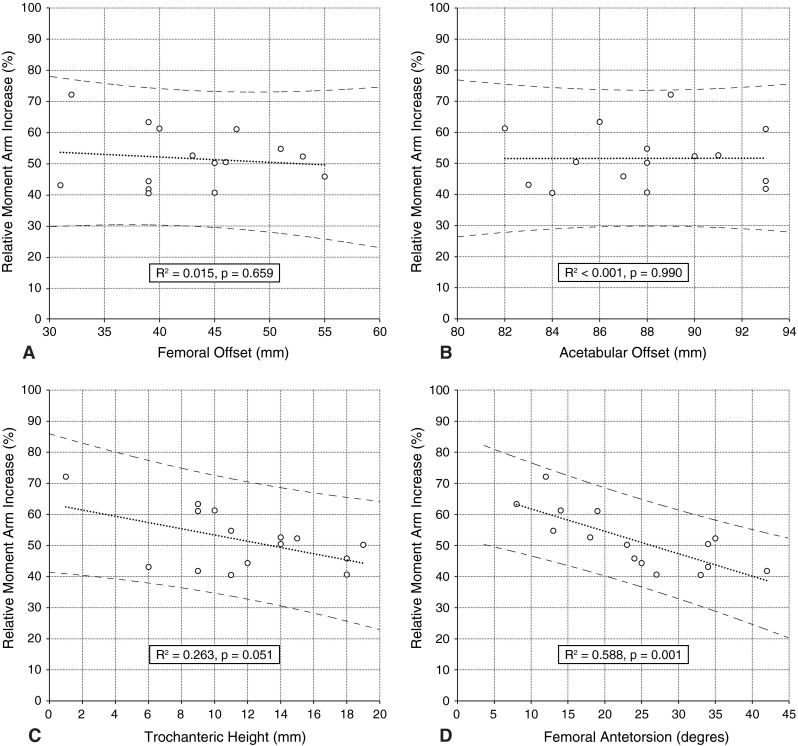
The scatterplots and linear correlations (with 95% CI) of the four preoperative anatomic parameters, (A) femoral offset, (B) acetabular offset, (C) trochanteric height, and (D) femoral antetorsion, with the relative moment arm increase are shown.
Discussion
With a THA, cup medialization with a compensatory increase of femoral offset often is recommended [6, 13] based on an assumed improvement of moment arms. However, there are tradeoffs associated with medialization of the center of rotation in THA, including potential negative effect on joint reaction forces or proprioception owing to the nonanatomic position of the center of rotation and loss of bone stock. It seems important to ascertain whether there are any reproducible benefits to medialization that might justify such potential disadvantages. In this study, we therefore sought to quantify the effect of cup medialization on moment arms. In addition, we tested the hypothesis that the increase in the moment arm of the gluteus minimus and gluteus medius is correlated to four preoperative anatomic parameters (acetabular and femoral offset, trochanteric height, and femoral anteversion). A patient-specific numerical model was developed and applied to 15 patients undergoing THA. The comparison of anatomic reconstruction of the acetabulum and femur with reconstruction including cup medialization revealed large variability of the moment increase after cup medialization. Specifically, we found that as medialization increased, abductor moment arms increased, albeit variably, whereas there was an inverse relationship between cup medialization and femoral antetorsion, such that the effect of cup medialization was more pronounced in patients with less femoral antetorsion. The femoral or acetabular offset or the height of the greater trochanter was not correlated to the gain of cup medialization.
The main limitation of our study is that a passive rather than an active movement was simulated. The deformation of the muscle is different when the muscle is contracted. However, we can assume that this difference in shape would produce only a weak effect on moment arms, particularly for our comparison of cup medialization. The main consequence of the passive simulation was that we could not estimate the muscle and joint forces. However, we can assume as a first approximation that muscle and joint force decrease as moment arms increase. For the sake of simplicity, the analysis was limited to the gluteus medius and minimus. The gluteus maximus was included in the model, but only to serve as mechanical support for deformation of the gluteus medius and minimus. We limited our study to these two muscles because of their importance in midstance support [1]. This is also the reason for limiting the study to the two movements tested. Preoperative CT scans of the patients were used for the bone and muscle reconstructions. Although muscle origins at the iliac wing are reliably detectable, their insertions on the greater trochanter were difficult to identify, and an approximation based on the anatomic description by Pfirrmann et al. had to be used [14]. In this study, we did not determine how an improved moment arm compares with drawbacks such as bone loss or changes in proprioception. The anatomic variability of the pelvis was not analyzed here, but we expect that our conclusions would be refined with such an analysis. This study was based on only 15 patients, which might seem limited for a statistical analysis. However, this represents the main strength of our study, to apply this validated model to 15 patients to test a specific hypothesis (Supplemental Figs. 1–3. Supplemental material is available with the online version of CORR®).
Quantification of the effect of cup medialization on moment arms in this series of 15 patients using the finite element model revealed that medialization resulted in an increase of abduction moment arms of the gluteus medius and minimus in all patients. On average, this increase was approximately 50% of the maximal theoretical increase corresponding to the medialization distance (ie, 5 mm in our model). The variability of the patients’ anatomy is reflected by the broad range of the observed moment arm increases. The difference between the highest and the lowest moment arm increases was approximately 50% of the maximal theoretical increase. Flexion moment arms also were increased on average. For eight of the 15 patients, cup medialization led to a moment arm decrease during flexion. The variability also was considerable in flexion, particularly for the posterior fiber of the gluteus medius and minimus. However, the gluteus medius and minimus are weak contributors to hip flexion and extension in normal gait. The effect of cup medialization appears clinically less important in this respect; however, relevant negative effects on proprioception cannot be excluded.
The moment arms predicted in this study are consistent with reported values [4, 8]. A 3-D straight-line model of a dry bone specimen provided moment arms of the gluteus medius for flexion-extension and abduction-adduction in three principal anatomic planes in a neutral joint position [8]. For this specific specimen, the moment arm of the gluteus medius was 43, 60, and 67 mm for the anterior, middle, and posterior fibers, respectively. At the neutral position, the average (minimum, maximum) values in our model were 30 (19, 40), 39 (20, 53), and 29 (20, 36) mm. The same trend was observed with the gluteus minimus. Blemker and Delp [4] developed a numerical 3-D model of the gluteus maximus and gluteus medius from MR images of one patient. Muscles were modeled in 3-D with embedded fibers. They evaluated muscle moment arms for movements of abduction-adduction and flexion-extension. For the ROM considered in our study, the moment arms of the gluteus medius ranged from approximately 20 to 50 mm for abduction-adduction and −20 to 20 mm for flexion-extension.
Linear correlation of preoperative parameters (ie, acetabular and femoral offset, trochanteric height, and femoral anteversion) revealed that the increase in abductor moment arms by cup medialization with a compensatory increase in femoral offset inversely correlated with femoral antetorsion, while the other parameters appeared to be independent. In patients with a large femoral antetorsion, an increase in the femoral offset moves the insertion of the abductor muscles on the greater trochanter more posteriorly and less laterally compared with a patient with little femoral antetorsion. The contribution of the offset increase therefore is larger in a patient with little antetorsion. This concept is confirmed by our model.
Our study confirmed the assumption that the advantage of cup medialization depends on the individual anatomy and appears to be unrelated to preoperative femoral offset. In active patients with little femoral antetorsion, cup medialization might be considered. Anatomic parameters of the pelvis and femur predicting the advantage of cup medialization remain to be identified. Further studies are needed to facilitate decision making in this respect and to improve accuracy of implant positioning.
Electronic supplementary material
Acknowledgments
We thank Valérie Parvex MSc (Mechanical Engineering, Ecole Polytechnique Fédérale de Lausanne, Switzerland) for help in improving the figures of results.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Ecole Polytechnique Fédérale de Lausanne and the Centre Hospitalier Universitaire Vaudoisn, Lausanne, Switzerland.
References
- 1.Anderson FC, Pandy MG. Individual muscle contributions to support in normal walking. Gait Posture. 2003;17:159–169. doi: 10.1016/S0966-6362(02)00073-5. [DOI] [PubMed] [Google Scholar]
- 2.Arnold AS, Salinas S, Asakawa DJ, Delp SL. Accuracy of muscle moment arms estimated from MRI-based musculoskeletal models of the lower extremity. Comput Aided Surg. 2000;5:108–119. doi: 10.3109/10929080009148877. [DOI] [PubMed] [Google Scholar]
- 3.Asayama I, Naito M, Fujisawa M, Kambe T. Relationship between radiographic measurements of reconstructed hip joint position and the Trendelenburg sign. J Arthroplasty. 2002;17:747–751. doi: 10.1054/arth.2002.33552. [DOI] [PubMed] [Google Scholar]
- 4.Blemker SS, Delp SL. Three-dimensional representation of complex muscle architectures and geometries. Ann Biomed Eng. 2005;33:661–673. doi: 10.1007/s10439-005-1433-7. [DOI] [PubMed] [Google Scholar]
- 5.Bonnin MP, Archbold PH, Basiglini L, Selmi TA, Beverland DE. Should the acetabular cup be medialised in total hip arthroplasty. Hip Int. 2011;21:428–435. doi: 10.5301/HIP.2011.8582. [DOI] [PubMed] [Google Scholar]
- 6.Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970;72:7–21. [PubMed] [Google Scholar]
- 7.Delp SL, Wixson RL, Komattu AV, Kocmond JH. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;328:137–146. doi: 10.1097/00003086-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Dostal WF, Soderberg GL, Andrews JG. Actions of hip muscles. Phys Ther. 1986;66:351–361. doi: 10.1093/ptj/66.3.351. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson JA, Chi SW, Yang JP, Chen JS, Edgerton VR, Sinha S. Finite element modeling of passive material influence on the deformation and force output of skeletal muscle. J Mech Behav Biomed Mater. 2012;9:163–183. doi: 10.1016/j.jmbbm.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 11.Lu YT, Zhu HX, Richmond S, Middleton J. Modelling skeletal muscle fibre orientation arrangement. Comput Methods Biomech Biomed Eng. 2011;14:1079–1088. doi: 10.1080/10255842.2010.509100. [DOI] [PubMed] [Google Scholar]
- 12.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:865–869. [PubMed] [Google Scholar]
- 13.Müller ME. Total hip prostheses. Clin Orthop Relat Res. 1970;72:46–68. [PubMed] [Google Scholar]
- 14.Pfirrmann CW, Chung CB, Theumann NH, Trudell DJ, Resnick D. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae—MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221:469–477. doi: 10.1148/radiol.2211001634. [DOI] [PubMed] [Google Scholar]
- 15.Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion: Part II. shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.