Abstract
Objective
To investigate the psychometric properties of the Bipolar Prodrome Symptom Interview and Scale–Prospective (BPSS-P), the first specific interview for emerging bipolar disorder (BD) symptoms.
Methods
A total of 205 youth aged 12–23 years and/or their caregivers underwent BPSS-P interviews: 129 patients with mood-spectrum disorders [depression-spectrum disorder (n = 77), mood disorder not otherwise specified (NOS) (n = 27), BD-NOS (n = 14), bipolar I disorder (BD-I)/bipolar II disorder (BD-II)/cyclothymia (n = 11), 34 with non-mood-spectrum disorders, and 42 healthy controls (HCs)]. We used Cronbach’s α to assess internal consistency; intra-class correlation (ICC) for inter-rater reliability; Spearman’s rho for convergent validity with the Young Mania Rating Scale (YMRS), General Behavior Inventory–10-item Mania Form (GBI-M-10), and Cyclothymic–Hypersensitive Temperament (CHT) scale; and ANOVAs for discriminatory power between diagnostic groups.
Results
Internal consistency was good to very good for the BPSS-P Mania (Cronbach’s α = 0.87), Depression (Cronbach’s α = 0.89), and General Symptom indices (Cronbach’s α = 0.74). Inter-rater reliability was high for the BPSS-P Total score (ICC = 0.939), and BPSS-P Mania (ICC = 0.934), Depression (ICC = 0.985), and General (ICC = 0.981) indices. Convergent validity was large (rho ≥ 0.50) between the BPSS-P Mania Index and YMRS, GBI-M-10, and CHT; BPSS-P Depression Index and MADRS and CHT; and BPSS-P General Index and GBI-M-10 and CHT. Expectedly, convergent validity was small (rho = 0.10 to < 0.30) between the BPSS-P Mania Index and MADRS, and BPSS-P Depression Index and YMRS. Furthermore, the BPSS-P and its subscales discriminated each patient group from HCs and from non-mood spectrum patients (except for the BPSS-P General Index). Moreover, the BPSS-P Total score discriminated BD-I/BD-II/cyclothymia from depression-spectrum patients, and the BPSS-Mania Index differentiated all three bipolar-spectrum groups from depression-spectrum patients.
Conclusions
The BPSS-P has good to excellent psychometric properties. Its use across multiple settings and predictive validity requires further investigation.
Keywords: adolescents, bipolar disorder, children, clinical high risk, early recognition, mania, pediatric, prevention, prodrome
Prediction, early intervention, and prevention of bipolar disorder (BD), a chronic, relapsing, and highly debilitating illness, are preeminent clinical and research goals (1-10). In BD, familial high-risk research has a relatively long tradition (11-21). However, different from psychosis high-risk research (22, 23), clinical high-risk approaches in BD have only more recently gained strong attention (2, 4-10, 24-30). Since the first illness manifestations of BD seem to emerge before the age of 18 in up to two-thirds of patients with BD (31, 32), early recognition and intervention efforts have also focused specifically on youth (1, 5-8, 33-35).
However, different from the psychosis high-risk arena where presence of a psychotic prodrome has been validated with criteria that have yielded transition rates to psychosis within six months to three years of 10–40% (23) and where targeted intervention trials have been successful (22), the existence of a sufficiently specific prodrome to BD that would allow targeted intervention is much less clear (2, 5-10, 25, 26). Identification of a symptomatic high-risk BD phase is complicated by the complex nature and definition of BD in general as well as by its potential different symptom presentations in children and adolescents.
Critical differences from the clinical high-risk state for psychosis include the potentially shorter and more complex time course of the symptom development, episodicity of subsyndromal symptoms and episodes, and the greater number of sub- or suprathreshold symptoms allowed before a syndromal BD diagnosis is made. For example, while the onset of non-affective psychotic disorders is predominantly insidious (36), the onset of BD, even of depressive episodes (37), may be more abrupt. Moreover, whereas the course of attenuated positive and negative symptoms usually fluctuates relatively little, subsyndromal mood symptoms are typically intermittent and episodic. Furthermore, importantly, one attenuated positive psychotic symptom and one full syndromal positive psychotic symptom, each, suffice to fulfill criteria for the psychosis prodrome and for transition to full psychosis, respectively (22). Conversely, for full mania, irritability plus at least four B criteria or mood elevation and at least three B criteria are required (38). This leaves room for a number of combinations of sub- and suptrathreshold symptomatology that may be part of a high-risk status or trajectory toward BD transition. In addition, different from psychosis, several conditions that are frequently comorbid with BD or that may develop and exist separately, such as attention-deficit hyperactivity disorder (ADHD), oppositional defiant disorder, or borderline personality disorder, present with symptoms that can be (co-)rated as mania symptoms. Finally, a major depressive episode that often precedes schizophrenia-spectrum disorders as a separate diagnostic entity can already be part of BD, either preceding a first manic episode or being part of a developing mixed episode (35). One related problem in youth is that irritability, which cuts across a whole host of pediatric psychiatric disorders, appears to predominate over classic elated mood states in early onset BD, particularly in pre-pubertal individuals (39). Additionally, in children and adolescents, irritability is both an A criterion for depression and for BD (38), and mixed episodes are frequent in youth (40).
Given these complexities, an important limitation to reliably identifying high-risk BD individuals has been the lack of specific rating scales and rating scale-based criteria for defining clinical high-risk states for BD. The problem of lacking specific BD risk rating instruments is highlighted by the findings of a prospective study of 147 adolescents fulfilling clinical high-risk criteria for schizophrenia-spectrum psychoses by having attenuated positive or negative symptoms (41). In this cohort, eight adolescents who eventually developed bipolar-spectrum disorders did not differ significantly on any baseline symptoms and neurocognitive measures compared to 24 adolescents who developed schizophrenia-spectrum disorders, while both groups differed significantly from the 115 non-converters (41). That a tool for the assessment of attenuated or emerging mania-like symptoms is needed is further indicated by three recent studies. In a large German community sample (n = 3,206), that underwent three follow-up interviews, the predictive value of the number and persistence of mania-like symptoms for bipolar I disorder (BD-I) or bipolar II disorder (BD-II) development was assessed prospectively in a risk sample of 1,565 subjects aged 14–21 years at baseline who were followed for 10 years (42). The authors found a significant dose-response relationship for persistence and number of both manic and depressive symptoms. Moreover, in 30–40% of individuals converting to BD-I/BD-II the symptom progression could be traced back to subthreshold manic and depressive symptoms (42). Furthermore, in an 18-month study of youth aged 8–11 years old with mood disorders, 48% of 37 children with depression-spectrum disorders and transient manic symptoms converted to bipolar-spectrum disorders [BD-I, BD-II, and bipolar disorder not otherwise specified (NOS)] compared to 12% of 13 youth with depression-spectrum disorders (43). Finally, based on retrospective chart review data, Bechdolf and colleagues (3) proposed a constellation of three BD risk domains, coined Bipolar at Risk (BAR) criteria: (i) sub-threshold mania symptoms, (ii) depression plus cyclothymic features, and (iii) depression plus genetic risk. Importantly, these BAR criteria were recently validated in a prospective study of youth and young adults aged 15–24 years (44), finding the greatest predictive value in attenuated mania-like symptoms, further calling for a specific and validated instrument that can be used to elicit and rate attenuated mania-like as well as other symptoms that may predict the development of BD.
Using symptom ratings for a BD risk definition is not new. For example, the self-report or parent-reported General Behavior Inventory (GBI) (45) was developed to look for subsyndromal and prodromal presentations of mood disorders, and several decades of research from multiple groups found evidence that the GBI identifies patients with BD, correlates plausibly with biomarkers, differentiates patients with BD from other psychiatric populations or healthy controls, predicts BD development prospectively, and predicts concurrent diagnoses of cyclothymia and dysthymia (46-59). Recently, prospective data from the ongoing Longitudinal Assessment of Mania Study (LAMS) (60, 61) revealed that manic-like symptoms, measured with the Parent General Behavior Inventory–10-item Mania Form (GBI-M-10) (62), significantly decreased over the two-year follow-up period in the 621 children whose parents/guardians’ ratings scored ≥ 12 on the GBI-M-10 and in the matched random sample of 86 children whose GBI-M-10 scores were ≤ 11 (63). Altogether, 85% of the cohort experienced decreases in manic symptoms, whereas approximately 15% either had high and rising, or unstable manic symptoms using the GBI. Importantly, the two latter patterns were associated with the highest rates of diagnostic conversion to BD (63).
Conversely, although a meta-analytic review of seven studies using the Child Behavior Checklist (CBCL) (64) led to the proposal of a constellation of problems with attention, aggression and anxiety/depression as defining a pediatric BD phenotype, this possibility was rejected after the majority of subsequent cross-sectional and longitudinal studies (65-71) did not support the CBCL or the pediatric BD subscale sum score as standardized measures enabling the differentiation of BD from other psychopathology.
Finally, a number of studies employed a combination of mania and depression interviews using psychopathology-based ratings of mild to moderate symptom levels to define at-risk populations for BD. This approach capitalizes on the dimensional nature of mood ratings that have been found to be superior to categorical approaches in predicting for example major depressive disorder (72, 73). Likewise, studies that used composite definitions combining moderate scores on the Young Mania Rating Scale (YMRS) (80) and Children’s Depression Rating Scale (CDRS), sometimes with additional criteria such as functional impairment or family history, found reasonable high rates of progression to bipolar-spectrum disorders (16, 43, 63). However, since the YMRS, CDRS, and other mania or depression scales do not cover all DSM symptoms and use inconsistent anchors and weighting within the same instrument, availability of an interview that comprehensively covers depressive and hypo-/manic and that may predict development of bipolar-spectrum disorders would be valuable.
Taken together, the successful application of the clinical high-risk approach in the psychosis risk arena (22, 23) through the use of validated rating scales for attenuated positive, negative, general and basic symptoms (74-76), and the results from the reviewed studies that point to the relevance of mania-like symptoms for conversion to BD underscore the need for a validated interview and rating scale for symptoms that may be present prior to the onset of a first full mania episode and that can be used as a clinical risk prediction tool. Such an interview would be complementary to the GBI that is a self-rating instrument. Therefore, as the next step after working with our Bipolar Prodrome Symptom Scale–Retrospective (BPSS-R) (25), we developed and tested the psychometric properties of the Bipolar Prodrome Symptom Interview and Scale–Prospective (BPSS-P) in a group of adolescents and young adults diagnosed with mood-spectrum and non-mood spectrum psychiatric disorders as well as in healthy control subjects.
Methods
Participants
Altogether, 205 participants were drawn from two independent samples for this validation study. The research protocol for the two studies from which the patients were drawn was approved by the Institutional Review Board at North Shore–Long Island Jewish Health System (NS-LIJHS). Written, informed consent was obtained from the patient if they were 18 years or older, or from their parent (with patient’s written assent) if the patient was under 18 years of age.
The first sample (n = 134) consisted of 92 patients at clinical high-risk (CHR) for psychosis and 42 healthy control subjects (HCs) with available BPSS-P data. Subjects were recruited to the Zucker Hillside Hospital Recognition and Prevention (RAP) Program from 2006–2010. The RAP Program is a longitudinal research program for adolescents and young adults considered to be at CHR for schizophrenia. Patients were referred to the program from the outpatient and inpatient services at The Zucker Hillside Hospital, a semi-urban, tertiary care psychiatric hospital, schools, community professionals, and concerned family members. Patients aged 12–25 years old were included in the RAP program if they met criteria for one of two CHR categories that were based on scores from the Scale of Prodromal Symptoms (SOPS) (75). Patients were classified as CHR Negative (CHR−) if they had a score of moderate or higher (score of 3–6) on any negative symptom (and no attenuated positive symptoms) or as CHR Positive (CHR+) if they had attenuated positive symptoms, defined by a score of moderate to severe (score of 3–5) on any SOPS positive symptom item. Patients were excluded from the study if they met DSM-IV (38) criteria for an Axis I schizophrenia-spectrum disorder (i.e., schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, or psychotic disorder NOS), major depressive disorder (MDD) with psychotic features, or a bipolar-spectrum disorder (i.e., BD-I, BD-II) with psychotic features at baseline. Additionally, patients were excluded if they were non-English speaking, had a medical or neurological disorder that could affect brain functioning, drug or alcohol dependence within the past six months, or had an estimated IQ < 70. HCs had to meet the same criteria, with the exception that they could not meet criteria for any high-risk category and that they must not have a first-degree relative with a psychotic disorder. HCs could not have had any lifetime history of psychiatric diagnoses or psychotropic prescriptions. However, if disruptive behavior disorders and anxiety disorders were diagnosed during the HC assessment in these non-help-seeking subjects, these diagnoses were allowed in order to avoid the ascertainment of supernormal controls.
The second sample consisted of 71 patients with available BPSS-P data who were drawn from the first 103 subjects who were recruited into the ongoing Adolescent Mood Disorder and Psychosis Study (AMDS) between September 2009 and February 2012. AMDS is a longitudinal cohort study aiming to characterize the early, pre-syndromal stages of mood and psychotic disorders in adolescents and young adults. Enrolled are patients aged 12–18 years with clinical chart diagnoses of mood-spectrum and psychosis-spectrum disorders, including BD-I, BD-II, BD-NOS, cyclothymia, MDD, depressive disorder NOS, dysthymia or mood disorder NOS, schizophrenia, schizoaffective disorder, schizophreniform disorder, or psychotic disorder NOS. Excluded were subjects unable or unwilling to sign consent (if age 18) or assent (if younger than age 18), or if the legal guardian did not sign informed consent if patients were < 18 years old, those non-English speaking, with an estimated IQ < 70, meeting DSM-IV criteria for pervasive developmental disorder, autism spectrum disorders, or current substance dependence, and patients with a medical condition known to affect the brain. In addition, for these analyses, patients with an Axis I schizophrenia-spectrum disorder (i.e., schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, or psychotic disorder NOS) were also excluded because too few such patients were available.
BPSS-P interviews in the RAP sample were conducted only in patients or healthy control adolescents, respectively. In the AMDS sample, both patients and primary caregivers were interviewed whenever possible (patient and caregiver: n = 38, patient only: n = 32, caregiver only: n = 1). Interviews of both patients and primary caregivers were preferred in order to further enhance the accuracy of the ratings, using the higher score in case of incongruent ratings, following the convention that symptoms are more likely minimized or forgotten than embellished or invented (12, 77).
Clinical assessments
All interviews for the RAP and AMDS studies were administered by a trained masters- or doctoral-level psychologist (RAP) and/or medical doctor (AMDS). Axis I diagnoses were assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/CV) (78), with added components from the Kiddie-Schedule for Affective Disorders and Schizophrenia (79) for childhood disorders not contained in the SCID (e.g., oppositional defiant disorder, conduct disorder, autism spectrum disorders), interviewing both the patient and the caregiver separately, integrating the results from the two separate interviews.
The BPSS-P (Correll CU, Auther AM, Cornblatt BA. The Bipolar Prodrome Symptom Interview and Scale–Prospective, unpublished manual.) is a semi-structured interview that was developed based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (38) criteria for BD and MDD, as well as established rating scales for mania, depression and other psychopathology. In addition, the BPSS-P development was informed by a review of existing literature regarding risk factors and early symptoms of BD (1), published scales and interviews for the assessment of the psychotic prodrome and character traits, input from experts in the areas of the schizophrenia prodrome and BD, and open questioning of youth with BD and their caregivers regarding emerging subthreshold symptoms prior to the onset of a first syndromal bipolar manic, mixed and major depressive episode. Finally, the identified items were used to develop the semi-structured Bipolar Prodrome Symptom Interview and Scale–Retrospective (BPSS-R) (25). The use of the BPSS-R in clinical samples of youth and young adults with established BD-I and BD-II further informed the final BPSS-P development.
The BPSS-P assesses the onset and severity of prodromal symptoms and is divided into three sections: Mania, Depression, and General Symptom Index (see Appendix A). The format of the BPSS-P was modeled after the Scale of Prodromal Symptoms (SOPS) (74), such that each symptom is rated on the following ordinal scale: 0 = absent, 1 = questionably present, 2 = mild, 3 = moderate, 4 = moderately severe, 5 = severe, and 6 = extreme. Each symptom is assessed by specific probes and anchors for accurate ratings. The severity of the symptoms is assessed for the past month and the past year. Administration of the BPSS-P takes about one hour in HCs and 1.5–2.5 hours in psychiatric patients or their caregivers, depending on the extent and severity of past and current psychopathology.
To test inter-rater reliability, four raters/interviewers at the Masters (n = 1: SS), Ph.D. psychology (n = 2: AMA, MH), or medical doctor level (n = 1: TK) rated six reliability video tapes of a patient interview conducted by one of the four expert interviewers (one interview only contained the ten BPSS-P mania items plus mood lability, a general psychopathology item). These four raters had been trained on the BPSS-P, using three training videos and had at least two years (range: 2–6 years) of BPSS-P interview and rating experience.
The YMRS (80) was used to measure interviewer-rated manic symptoms. The Montgomery–Åsberg Rating Scale (MADRS) (81), which was administered in a subgroup of the AMDS sample (n = 61), was used to measure interviewer-rated depressive symptoms. The General Behavior Inventory-10-item Mania Form (GBI-M-10) (62) parent and respective patient self-report, which was added later to the assessment battery of the AMDS sample (n = 31), was used to measure self-reported mania-like symptoms. Temperament was measured with the Cyclothymic–Hypersensitive Temperament questionnaire (CHT) (82) of the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego–Autoquestionnaire (TEMPS-A) (83).
Statistical analyses
For the comparison of the diagnostic groups regarding demographic, illness, and treatment variables univariate ANOVA with group as the between-subjects factor was conducted for continuous variables and chi square of Fisher’s Exact test analysis were used for categorical variables. For the psychometric analyses, the following statistical tests were performed. Cronbach’s α was used to determine internal consistency of the BPSS Mania, Depression, and General Index. A Cronbach’s α above 0.70 is considered to be an acceptable cutoff (84), with a maximum of 0.90 to prevent redundancy (85). The Spearman’s rank correlation coefficient (rho) was used to determine convergent validity between the BPSS subscales and four clinical measures: the YMRS, GBI-M-10, MADRS, and CHT. Since convergent validity between the BPSS-P Mania Index score and the YMRS versus the GBI-M-10 is of special interest due to the latter two instruments’ current use in the detection of at-risk individuals, we also calculated the Spearman’s rho coefficient for the correlation between the BPSS-P Mania Index and the YMRS excluding healthy controls, as the GBI-M-10 was only administered to a subgroup of the psychiatric patients. Besides a more equal comparison, this approach has the advantage of avoiding the possibility of an artificial inflation of the correlation, as healthy controls are likely to all have low scores in the used instruments. Moreover, these instruments will be used for early risk detection in clinical samples and not in healthy control individuals. Inter-rater reliability was assessed using the intra-class correlation (ICC) coefficient as a two-way mixed model with absolute agreement. ICC coefficients reflect the consistency of a measure taking into account variance related to the time of testing (86). A two-way random model was utilized for consistency between scores. Scores are interpreted as excellent (ICC ≥ 0.75), fair to good (ICC = 0.40–0.74), and poor (ICC < 0.40) agreement (86). Finally, for the assessment of the discriminant validity of the BPSS-P Total score and Mania, Depression, and General subscores, as well as for YMRS and CHT, univariate ANOVA with group as the between-subjects factor was conducted. This was followed by post-hoc pair-wise comparisons, using Tukey–Kramer statistics adjusting for multiple testing. There were insufficient numbers of patients with data on the GBI-M-10 and MADRS, which had only been administered to a subsample to do the same for these instruments.
All test were two-sided with alpha set at 0.05, using the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL, USA, Version 16.0) or JMP5 (1998–2003 SAS Institute, Inc.,).
Results
Sample characteristics
Demographic, illness, and treatment characteristics of the 163 psychiatric patients [mean age: 16.0 ± 1.9 years (range: 12–23 years), 57.5% male, 63.2% White] and 42 HCs (mean age: 17.3 ± 2.4 years, 40.5% male, 57.1% White) included in the analyses of the psychometric properties of the BPSS-P are displayed in Table 1. Psychiatric patients were approximately one year younger than HC subjects and contained also 15–25% more males. In addition, per design, psychiatric patients had significantly more psychiatric diagnoses and received significantly more psychotropic medications than HCs.
Table 1.
Demographic illness and treatment characteristics of the healthy control and psychiatric disorders groups
| HCs (n = 42) | All psychiatric subjects (n = 163) | Mood spectrum disorder (n = 129) | Non-mood spectrum disorder (n = 34) | All psychiatric subjects versus HCs p-value | Mood disorder patients versus HCs p-value | Non-mood disorder patients versus HCs p-value | Mood disorder versus non-mood disorder groups p-value | |
|---|---|---|---|---|---|---|---|---|
| Demographics | ||||||||
| Age, years, mean ± SD | 17.3 ± 2.4 | 16.0 ± 1.9 | 16.0 ± 1.9 | 16.0 ± 1.6 | < 0.0001 | < 0.0001 | 0.011 | 0.84 |
| Gender, male, n (%) | 17 (40.5) | 94 (57.5) | 68 (52.7) | 26 (76.5) | 0.046 | 0.17 | 0.002 | 0.013 |
| Race, n (%) | 0.39 | 0.30 | 0.72 | 0.54 | ||||
| Caucasian | 24 (57.1) | 103 (63.2) | 85 (65.9) | 18 (52.9) | ||||
| African American | 8 (19.0) | 26 (16.0) | 19 (14.7) | 7 (20.6) | ||||
| Other | 7 (16.7) | 13 (8.0) | 9 (7.0) | 4 (11.8) | ||||
| Asian | 3 (7.1) | 19 (11.7) | 15 (11.6) | 4 (11.8) | ||||
| Native American | 0 (0) | 2 (1.2) | 1 (8.0) | 1 (2.9) | ||||
| Ethnicity, Hispanic, n (%) | 46 (22.4) | 11 (26.2) | 26 (20.2) | 9 (26.5) | 0.51 | 0.41 | 0.98 | 0.43 |
| No. of DSM-IV diagnoses, mean ± SD | 0.1 ± 0.3 | 2.2 ± 1.3 | 2.4 ± 1.3 | 1.5 ± 1.0 | < 0.0001 | < 0.0001 | < 0.0001 | 0.0002 |
| DSM-IV diagnoses, n (%) | ||||||||
| Depressive spectrum disordersa | 0 (0) | 83 (50.9) | 83 (64.3) | 0 (0) | < 0.0001 | < 0.0001 | 1.0 | < 0.0001 |
| Major depressive disorder | 0 (0) | 54 (33.1) | 54 (41.9) | 0 (0) | < 0.0001 | < 0.0001 | 1.0 | < 0.0001 |
| Depressive disorder NOS | 0 (0) | 18 (11.0) | 18 (14.0) | 0 (0) | 0.027 | 0.007 | 1.0 | 0.015 |
| Dysthymic disorder | 0 (0) | 10 (6.1) | 10 (7.8) | 0 (0) | 0.22 | 0.12 | 1.0 | 0.12 |
| Adjustment disorder with depressed mood | 0 (0) | 5 (3.1) | 5 (3.9) | 0 (0) | 0.59 | 0.34 | 1.0 | 0.59 |
| Bipolar spectrum disorders | 0 (0) | 51 (31.3) | 51 (39.5) | 0 (0) | < 0.0001 | < 0.0001 | 1.0 | < 0.0001 |
| Mood disorder NOS | 0 (0) | 27 (16.6) | 27 (20.9) | 0 (0) | 0.002 | < 0.0001 | 1.0 | 0.001 |
| Bipolar disorder NOS | 0 (0) | 14 (8.6) | 14 (10.9) | 0 (0) | 0.079 | 0.023 | 1.0 | 0.043 |
| Bipolar I disorder | 0 (0) | 9 (5.5) | 9 (7.0) | 0 (0) | 0.21 | 0.12 | 1.0 | 0.21 |
| Bipolar II disorder | 0 (0) | 1 (0.6) | 1 (0.8) | 0 (0) | 1.0 | 1.0 | 1.0 | 1.0 |
| Cyclothymic disorder | 0 (0) | 1 (0.6) | 1 (0.8) | 0 (0) | 1.0 | 1.0 | 1.0 | 1.0 |
| Anxiety disorders | 2 (4.8) | 68 (41.7) | 50 (38.8) | 18 (52.9) | < 0.0001 | < 0.0001 | < 0.0001 | 0.14 |
| Social phobia | 0 (0) | 23 (14.1) | 20 (15.5) | 3 (8.8) | 0.005 | 0.004 | 0.085 | 0.41 |
| Other anxiety disorders | 2 (4.8) | 20 (12.3) | 10 (7.8) | 10 (29.4) | 0.26 | 0.73 | 0.004 | 0.001 |
| Generalized anxiety disorder | 0 (0) | 15 (9.2) | 13 (10.1) | 2 (5.9) | 0.044 | 0.040 | 0.20 | 0.74 |
| Panic disorder | 0 (0) | 13 (8.0) | 12 (9.3) | 1 (2.9) | 0.075 | 0.040 | 0.45 | 0.31 |
| Specific phobia | 0 (0) | 12 (7.4) | 8 (6.2) | 4 (11.8) | 0.13 | 0.20 | 0.036 | 0.27 |
| Obsessive compulsive disorder | 0 (0) | 8 (4.9) | 4 (3.1) | 4 (11.8) | 0.37 | 0.57 | 0.036 | 0.060 |
| Agoraphobia | 0 (0) | 5 (3.1) | 5 (3.9) | 0 (0) | 0.59 | 0.34 | 1.0 | 0.59 |
| Posttraumatic stress disorder | 0 (0) | 4 (2.5) | 2 (1.6) | 2 (5.9) | 0.58 | 1.0 | 0.20 | 0.19 |
| Substance use disorders | 0 (0) | 17 (10.4) | 13 (10.1) | 4 (11.8) | 0.026 | 0.040 | 0.036 | 0.66 |
| Substance abuse | 0 (0) | 11 (6.7) | 8 (6.2) | 3 (8.8) | 0.13 | 0.12 | 0.085 | 0.70 |
| Substance dependence | 0 (0) | 6 (3.7) | 5 (3.9) | 1 (2.9) | 0.35 | 0.34 | 0.45 | 1.0 |
| Disruptive behavior disorders | 2 (4.8) | 67 (41.1) | 55 (42.6) | 12 (35.3) | < 0.0001 | < 0.0001 | 0.001 | 0.44 |
| ADHD | 1 (2.4) | 41 (25.2) | 34 (26.4) | 7 (20.6) | < 0.0001 | < 0.0001 | 0.019 | 0.66 |
| Oppositional defiant disorder | 1 (2.4) | 27 (16.6) | 21 (16.3) | 6 (17.6) | 0.020 | 0.017 | 0.041 | 0.85 |
| Otherb | 0 (0) | 18 (11.0) | 13 (10.1) | 5 (14.7) | 0.027 | 0.040 | 0.015 | 0.44 |
| Conduct disorder | 0 (0) | 13 (8.0) | 10 (7.8) | 3 (8.8) | 0.075 | 0.12 | 0.085 | 0.74 |
| Disruptive behavior disorder NOS | 0 (0) | 9 (5.5) | 9 (7.0) | 0 (0) | 0.21 | 0.12 | 1.0 | 0.21 |
| Psychotropic medications, n (%)c | ||||||||
| None | 42 (100) | 52 (32.5) | 36 (28.6) | 16 (47.1) | < 0.0001 | < 0.0001 | < 0.0001 | 0.041 |
| Antipsychotics | 0 (0) | 81 (50.6) | 65 (51.6) | 16 (47.1) | < 0.0001 | < 0.0001 | < 0.0001 | 0.64 |
| Antidepressants | 0 (0) | 42 (26.3) | 40 (31.8) | 2 (5.9) | < 0.0001 | < 0.0001 | 0.11 | 0.0017 |
| Mood stabilizers | 0 (0) | 35 (21.9) | 30 (23.38) | 5 (14.7) | 0.0002 | 0.0001 | 0.015 | 0.35 |
| Anxiolytics | 0 (0) | 21 (13.1) | 19 (15.1) | 2 (5.9) | 0.0089 | 0.0041 | 0.11 | 0.25 |
| Stimulants | 0 (0) | 13 (8.3) | 9 (7.1) | 4 (11.8) | 0.074 | 0.075 | 0.036 | 0.48 |
Bolded p-values: p < 0.05. HCs = healthy controls; SD = standard deviation; NOS = not otherwise specified; ADHD = attention-deficit hyperactivity disorder.
Depressive spectrum disorders included: major depressive disorder (n = 51), depressive disorder not otherwise specified (n = 18), dysthymic disorder (n = 4), and adjustment disorder with depressed mood (n = 4).
Other disorders included: unspecified mental disorder (n = 1), intermittent explosive disorder (n = 2), learning disorder (n = 3), pain disorder (n = 1), parent–child relational problem (n = 1), pervasive developmental disorder (n = 3), communication disorder (n = 1), alcohol use disorder (n = 1), reading disorder (n = 1), bulimia (n = 2), and body dysmorphic disorder (n = 1).
Medication information missing for three patients with mood spectrum disorder.
Among the 163 psychiatric patients, 129 (79.1%) had a primary mood spectrum disorder, and 34 (20.9%) had a primary non-mood spectrum disorder. These two groups differed on few variables in addition to the diagnoses that depended on the grouping by design. These significant differences included a higher proportion of males and lower mean number of psychiatric diagnoses in the non-mood disorder group. Moreover, more non-mood disorder patients were not on any psychotropic medications at the time of the assessment. While non-psychotic non-mood disorder patients received significantly less antidepressants, the prescription of antipsychotics, mood stabilizers, anxiolytics, and stimulants did not differ significantly from those in mood-spectrum disorder patients.
Demographic, illness and treatment characteristics of the 129 mood-spectrum disorder patients [mean age: 16.1 ± 1.9 years (range: 13–23 years), 51.5% male, 65.90% White] are displayed and compared in Table 2. Most patients had a primary depressive-spectrum diagnosis (59.7%), followed by mood disorder NOS (20.9%), BD-NOS (10.9%), and then BD-I, BD-II, and cyclothymia (8.5%). There were no differences across the mood-spectrum disorder groups in addition to the diagnostic differences due to grouping, except for the proportion of patients diagnosed with disruptive behavior disorders (DBDs) and those receiving mood stabilizers. In post-hoc analyses, only a higher proportion of DBDs in patients with mood disorder NOS than those with depressive disorders remained significant.
Table 2.
Demographic illness and treatment characteristics of individual mood spectrum disorder groups
| All mood spectrum disorders (n = 129) | Depression spectrum disorders (n = 77) | Mood disorder NOS (n = 27) | BD-NOS (n = 14) | BD-I/BD-II/cyclothymia (n = 11) | Omnibus p-value | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, years, mean ± SD | 16.0 ± 1.9 | 16. 0 ± 2.1 | 15.4 ± 1.4 | 16.8 ± 1.9 | 16.2 ± 1.7 | 0.22 |
| Gender, male, n (%) | 53 (51.5) | 27 (52.9) | 14 (51.9) | 8 (57.1) | 4 (36.4) | 0.71 |
| Race, n (%) | 0.15 | |||||
| Caucasian | 85 (65.9) | 45 (58.4) | 23 (85.2) | 9 (64.3) | 8 (72.7) | |
| African American | 19 (14.7) | 13 (16.9) | 2 (7.4) | 3 (21.4) | 1 (9.1) | |
| Asian | 15 (11.6) | 12 (15.6) | 1 (3.7) | 1 (7.1) | 1 (9.1) | |
| Other | 9 (7.0) | 7 (9.1) | 1 (3.7) | 0 (0) | 1 (9.1) | |
| Native American | 1 (0.8) | 0 (0) | 0 (0) | 1 (7.1) | 0 (0) | |
| Ethnicity, Hispanic, n (%) | 26 (20.2) | 21 (27.3) | 2 (7.4) | 1 (7.1) | 2 (18.2) | 0.084 |
| No. of DSM-IV diagnoses, mean ± SD | 2.4 ± 1.3 | 2.5 ± 1.4 | 2.6 ± 1.2 | 2.1 ± 1.0 | 2.0 ± 1.0 | 0.48 |
| DSM-IV diagnoses, n (%) | ||||||
| Depressive disorders | 83 (64.3) | 77 (100) | 0 (0) | 5 (35.7) | 1 (9.1) | < 0.0001 |
| Major depressive disorder | 54 (41.9) | 51 (66.2) | 0 (0) | 3 (21.4) | 0 (0) | < 0.0001 |
| Depressive disorder NOS | 18 (14.0) | 18 (23.4) | 0 (0) | 0 (0) | 0 (0) | 0.0027 |
| Dysthymic disorder | 10 (7.8) | 8 (10.4) | 0 (0) | 2 (14.3) | 0 (0) | 0.19 |
| Adjustment disorder with depressed mood | 5 (3.9) | 4 (5.2) | 0 (0) | 0 (0) | 1 (9.1) | 0.40 |
| Bipolar spectrum disorders | 52 (40.3) | 0 (0) | 27 (100) | 14 (100) | 11 (100) | < 0.0001 |
| Mood disorder NOS | 27 (26.2) | 0 (0) | 27 (100) | 0 (0) | 0 (0) | < 0.0001 |
| BD-NOS | 14 (10.9) | 0 (0) | 0 (0) | 14 (100) | 0 (0) | < 0.0001 |
| BD-I | 9 (7.0) | 0 (0) | 0 (0) | 0 (0) | 9 (81.8) | < 0.0001 |
| BD-II | 1 (0.8) | 0 (0) | 0 (0) | 0 (0) | 1 (9.1) | 0.013 |
| Cyclothymic disorder | 1 (0.8) | 0 (0) | 0 (0) | 0 (0) | 1 (9.1) | 0.013 |
| Anxiety disorders | 50 (38.8) | 35 (45.5) | 10 (37.0) | 1 (7.4) | 4 (36.4) | 0.060 |
| Social phobia | 20 (15.5) | 15 (19.5) | 2 (7.4) | 0 (0) | 3 (27.3) | 0.11 |
| Generalized anxiety disorder | 13 (10.1) | 9 (11.7) | 2 (7.4) | 0 (0) | 2 (18.2) | 0.42 |
| Panic disorder | 12 (9.3) | 9 (11.7) | 2 (7.4) | 0 (0) | 1 (7.1) | 0.56 |
| Other anxiety disorder | 10 (7.8) | 7 (9.1) | 3 (11.1) | 0 (0) | 0 (0) | 0.44 |
| Specific phobia | 8 (6.2) | 6 (7.8) | 2 (7.4) | 0 (0) | 0 (0) | 0.56 |
| Agoraphobia | 5 (3.9) | 5 (6.5) | 0 (0) | 0 (0) | 0 (0) | 0.32 |
| Obsessive compulsive disorder | 4 (3.1) | 4 (5.2) | 0 (0) | 0 (0) | 1 (9.1) | 0.56 |
| Posttraumatic stress disorder | 2 (1.6) | 1 (1.3) | 0 (0) | 1 (7.1) | 0 (0) | 0.32 |
| Substance use disorders | 13 (10.1) | 9 (11.7) | 3 (11.1) | 1 (7.1) | 0 (0) | 0.66 |
| Substance abuse | 8 (6.2) | 5 (6.5) | 3 (11.1) | 0 (0) | 0 (0) | 0.43 |
| Substance dependence | 5 (3.9) | 4 (5.2) | 0 (0) | 1 (7.1) | 0 (0) | 0.51 |
| Disruptive behavior disorders | 55 (42.6) | 26 (33.8) | 18 (66.7) | 7 (50.0) | 4 (36.4) | 0.025 |
| Attention-deficit hyperactivity disorder | 34 (26.4) | 17 (22.1) | 12 (44.4) | 3 (21.4) | 2 (18.2) | 0.12 |
| Oppositional defiant disorder | 21 (16.3) | 10 (13.0) | 8 (29.6) | 1 (7.1) | 2 (18.2) | 0.17 |
| Othera | 13 (10.1) | 11 (14.3) | 2 (7.4) | 0 (0) | 0 (0) | 0.21 |
| Conduct disorder | 10 (7.8) | 4 (5.2) | 5 (18.5) | 1 (7.1) | 0 (0) | 0.11 |
| Disruptive behavior disorder NOS | 9 (7.0) | 5 (6.5) | 1 (3.7) | 3 (21.4) | 0 (0) | 0.12 |
| Psychotropic medications, n (%)b | ||||||
| None | 36 (28.6) | 24 (31.6) | 7 (26.9) | 4 (30.8) | 1 (9.1) | 0.48 |
| Antipsychotics | 65 (51.6) | 24 (47.1) | 11 (40.7) | 7 (50.0) | 9 (81.8) | 0.17 |
| Antidepressants | 40 (31.8) | 27 (35.5) | 8 (30.8) | 2 (14.4) | 3 (27.3) | 0.53 |
| Mood stabilizers | 30 (23.8) | 11 (18.4) | 8 (30.8) | 2 (14.4) | 6 (54.6) | 0.043 |
| Anxiolytics | 19 (15.1) | 13 (17.1) | 3 (11.5) | 1 (7.7) | 2 (18.2) | 0.77 |
| Stimulants | 9 (7.1) | 4 (5.3) | 3 (11.5) | 0 (0) | 2 (18.2) | 0.24 |
Bolded p-values: p < 0.05. NOS = not otherwise specified; BD-NOS = bipolar disorder not otherwise specified; BD-I = bipolar I disorder; BD-II = bipolar II disorder; SD = standard deviation.
Other disorders included: unspecified mental disorder (n = 1), intermittent explosive disorder (n = 2), learning disorder (n = 3), pain disorder (n = 1), parent–child relational problem (n = 1), pervasive developmental disorder (n = 3), communication disorder (n = 1), alcohol use disorder (n = 1), reading disorder (n = 1), bulimia (n = 2), and body dysmorphic disorder (n = 1).
Medication information missing for three patients with mood spectrum disorder.
Psychometric properties of the BPSS-P
Internal consistency
Cronbach’s α was used to determine internal consistency within each of the subscales of the BPSS-P. Internal consistency estimates were high for the BPSS-P Mania (Cronbach’s α = 0.87), Depression (Cronbach’s α = 0.89), and General Symptom Index (Cronbach’s α = 0.74).
Convergent validity
Table 3 presents Spearman’s rho and p-values for the convergent validity between the BPSS-P subscales and the YMRS, GBI-M-10, MADRS and CHT. Correlations were large (r ≥ 0.50) between the BPSS-P Mania Index and the YMRS, GBI-M-10, and CHT; BPSS-P Depression Index and MADRS and CHT; and BPSS-P General Index and GBI-M-10 and CHT. Correlations were medium (rho = 0.30 to < 0.50) between the BPSS-P Depression Index and the GBI-M-10, and between the BPSS-P General Index and both the YMRS and MADRS. Correlations were small (rho = 0.10 to < 0.30) between the BPSS-P Mania Index and MADRS, and BPSS-P Depression Index and the YMRS. Reanalyzing the correlation between the BPSS-P Mania Index score and the YMRS in psychiatric patients only (excluding healthy controls), yielded a medium correlation (rho = 0.35, p < 0.0001, n = 159), which was smaller than the large correlation with the GBI-M-10 (rho = 0.54, p = 0.0045, n = 31).
Table 3.
Spearman’s rank correlation coefficients (rho) for the BPSS-P subscales and the YMRS, GBI-M-10, MADRS, and the CHT
| BPSS-P Mania Index | BPSS-P Depression Index | BPSS-P General Index | YMRS | GBI-M-10 | MADRS | CHT | |
|---|---|---|---|---|---|---|---|
| BPSS-P Mania Index | – | 0.50a | 0.65a | 0.52a | 0.54c | 0.14 | 0.56a |
| BPSS-P Depression Index | – | – | 0.72a | 0.27a | 0.39e | 0.69a | 0.50a |
| BPSS-P General Index | – | – | – | 0.45a | 0.56c | 0.42b | 0.55a |
| YMRS | – | – | – | – | 0.31 | –0.24 | 0.42a |
| GBI-M-10 | – | – | – | – | – | 0.22 | 0.48d |
| MADRS | – | – | – | – | – | – | 0.10 |
| CHT | – | – | – | – | – | – | – |
BPSS-P = Bipolar Prodrome Interview and Symptoms Scale–Prospective; YMRS = Young Mania Rating Scale; GBI-M-10 = General Behavior Index–Mania-10 Item Form; MADRS = Montgomery-Åsberg Depression Rating Scale; CHT = Cyclothymic–Hypersensitive Temperament.
p < 0.0001;
p < 0.001;
p < 0.005;
p < 0.01;
p < 0.05.
Inter-rater reliability
Inter-rater reliability was very high for the BPSS-P Total score (ICC = 0.939), as well as for the BPSS-P Mania (ICC = 0.934), Depression (ICC = 0.985), and General Symptom Index (ICC = 0.981).
Discriminant validity of the BPSS-P across diagnostic groups
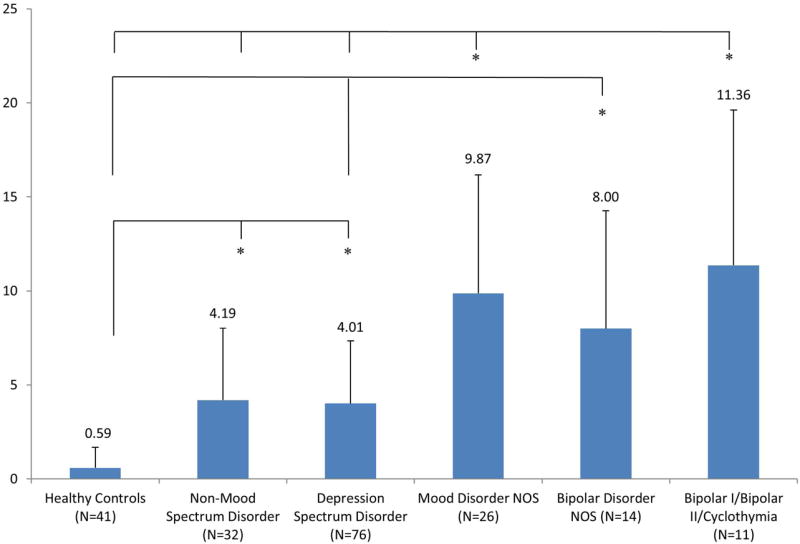
BPSS-P Total scores were significantly different among the diagnostic groups [F(5,195) = 55.73, p < 0.0001] (Fig. 1A). Post-hoc analyses revealed that BPSS-P Mania Index scores were significantly higher in each of the four individual mood-spectrum disorder groups compared to both the non-mood spectrum and HC groups. In addition, the BD-I/BD-II/cyclothymia group had significantly higher BPSS-P Total scores than the depression-spectrum group, and the non-mood spectrum had higher scores than HCs.
Fig. 1.
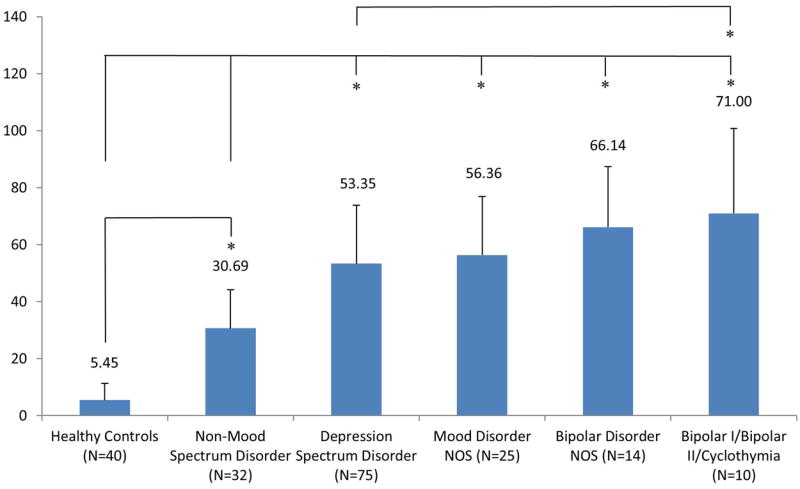
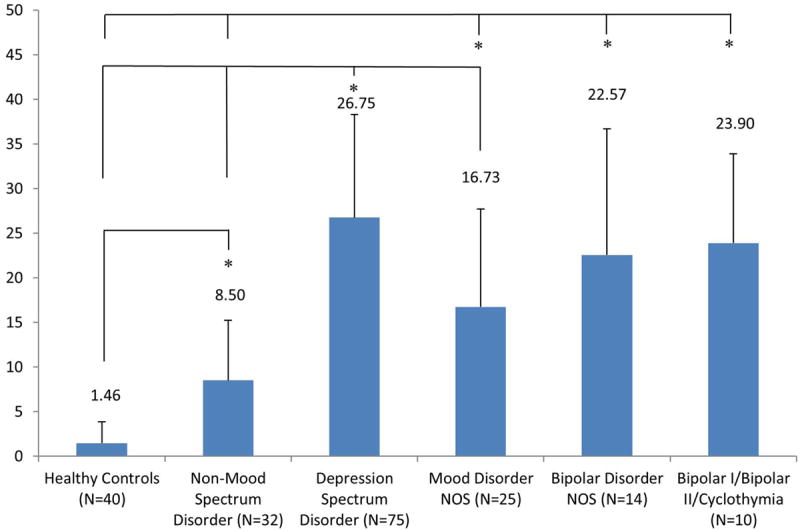
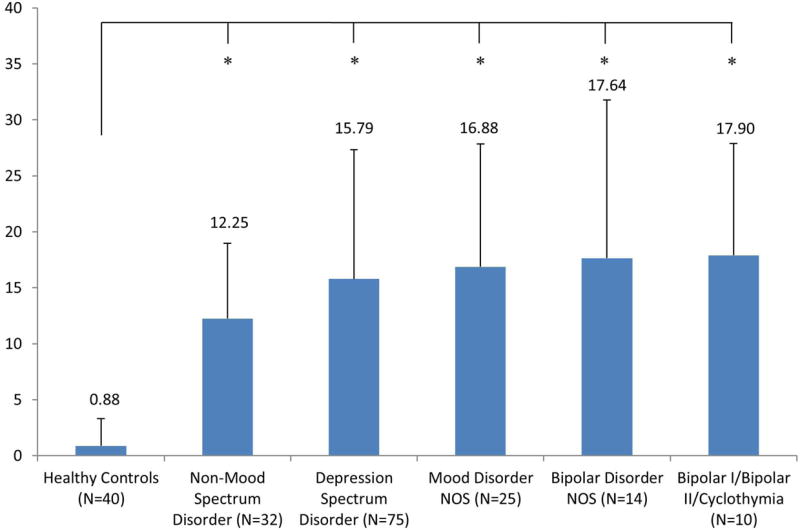
Bar graphs of mean ± standard deviation in the Bipolar Prodrome Symptom Interview and Scale–Prospective (BPSS-P) Total score (A), BPSS-P Mania Index score (B), BPSS-P Depression Index score (C), and BPSS-P General Symptom Index score (D) across diagnostic groups. NOS = not otherwise specified. *p < 0.05 for greater value in post-hoc pair-wise comparisons adjusted for multiple testing.
BPSS-P Mania Index scores were significantly different among the diagnostic groups [F(5,204) = 51.20, p < 0.0001] (Fig. 1B). Post hoc analyses revealed that BPSS-P Mania Index scores were significantly higher in each of the three individual bipolar-spectrum groups (i.e., BD-I/BD-II/cyclothymia, BD-NOS, and mood disorder NOS) compared to the depression-spectrum, non-mood spectrum and HC groups. In addition, the depression-spectrum and non-mood spectrum groups held a middle position, having significantly higher BPSS Mania Index scores than HCs.
BPSS-P Depression Index scores were significantly different among the diagnostic groups [F(5,201) = 44.00, p < 0.0001] (Fig. 1C). Post-hoc analyses revealed that BPSS-P Depression Index scores were highest in the depression-spectrum disorder group, with significantly higher scores than the mood disorder NOS as well as the non-mood spectrum and HC groups. In addition, BPSS-P Depression Index scores were significantly higher in each of the three individual bipolar-spectrum groups (i.e., BD-I/BD-II/cyclothymia, BD-NOS, and mood disorder NOS) compared to the non-mood spectrum and HC groups. Finally, the non-mood spectrum disorder group had significantly higher BPSS-P Depression scores than HCs.
BPSS-P General Index scores were also significantly different among the diagnostic groups [F(5,195) = 37.04, p < 0.0001] (Fig. 1D). However, this was solely driven by differences between each of the psychiatric groups and HCs without any significant differences between psychiatric groups.
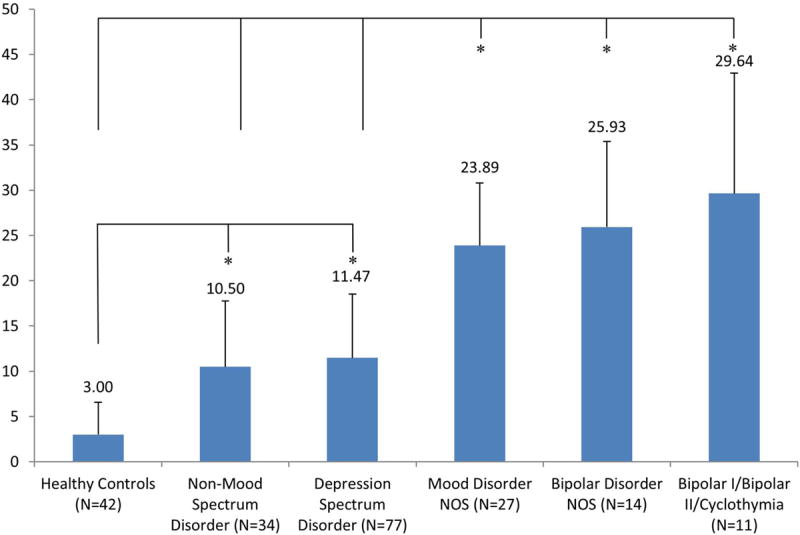
Distribution of the YMRS and CHT questionnaire scores across the diagnostic groups
YMRS total scores were significantly different among the diagnostic groups [F(5,199) = 22.86, p < 0.0001]. Post-hoc analyses indicated that all five psychiatric groups had significantly higher YMRS scores than the HC group (Fig. 2A). Moreover, the BD-I/BD-II/cyclothymia and mood disorder NOS groups had significantly higher scores that the depression-spectrum and non-mood disorder spectrum groups, while the BD-NOS group ad higher scores than the depression-spectrum group only.
Fig. 2.
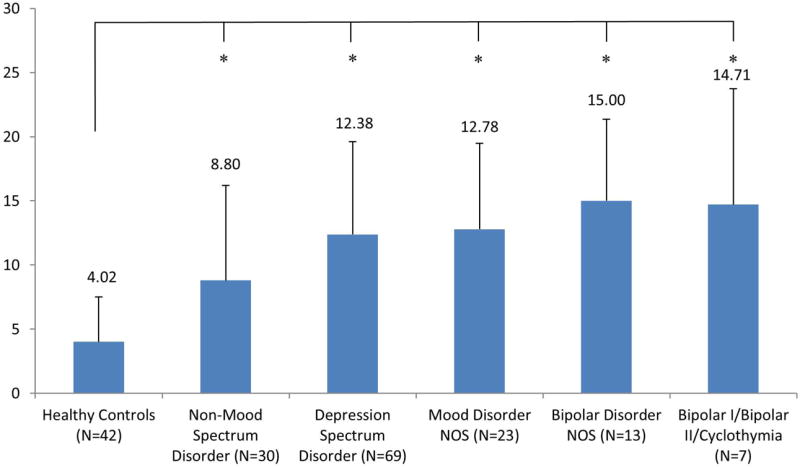
Bar graph of mean ± standard deviation of the Young Mania Rating Scale score (A) and the Cyclothymic–Hypersensitive Temperament score (B) across diagnostic groups. NOS = not otherwise specified. *p < 0.05 for greater value in post-hoc pair-wise comparisons adjusted for multiple testing.
Finally, CHT total scores were also significantly different among the groups [F(5,183) = 12.07, p < 0.0001] (Fig. 2B). Again, post-hoc analyses indicated that five psychiatric groups had significantly higher CHT scores than the HC group. However, none of the psychiatric groups differed from each other.
Discussion
This study in 163 psychiatrically ill adolescents with mood-spectrum disorders (n = 129) and non-psychotic, non-mood spectrum disorders (n = 34), as well as 42 healthy control subjects suggests that the BPSS-P has good to excellent psychometric properties. This includes very high internal consistency (Cronbach’s α = 0.87 and 0.89 for the BPSS-P Mania and Depression Indices), inter-rater reliability (ICC = 0.934–0.985), and convergent validity (r ≥ 0.50 between the BPSS-P Mania Index and the YMRS, GBI-M-10, and CHT; and between the BPSS-P Depression Index and MADRS and CHT). Moreover, in the psychiatric population, the correlation was greater between the BPSS-P Mania Index and the self-reported GBI-M-10, which has been used successfully in the risk detection for BD, than between the BPSS-P Mania Index and the YMRS. In addition, the BPSS-P had good discriminatory power not only regarding healthy control subjects, but also regarding depression-spectrum disorder patients as well as in relationship to youth with a variety of non-mood spectrum psychiatric disorders.
We deliberately included a psychiatric sample consisting of patients with diverse mood and non-mood, but non-schizophrenia spectrum disorders in order to increase generalizability of the findings and to test discriminant validity of the BPSS-P and its subscales. In general, the BPSS-P Total score and each of the subscores were significantly different between each of the psychiatric groups and HCs, but differences emerged also between psychiatric groups for the BPSS-P Total and the BPSS-P Mania and Depression Index scores. The BPSS-P Total score was highest in the syndromal mania/hypomania group, with discrimination from the depressive-spectrum disorder group despite the low number of subjects in the former group. Further, the BPSS-P Total score discriminated all mood disorder groups from the non-mood disorder psychiatric patients. The BPSS-P Mania Index discriminated each of the three bipolar-spectrum groups from the depression and non-mood disorder groups. All mood disorder groups separated on the BPSS-P Depression Index from the non-mood disorder patients. Although the BPSS-P Depression Index scores were highest in the depressive spectrum disorder group, the scores only separated from the mood disorder NOS group. This indicates that depression cuts across unipolar and bipolar spectrum groups, but one also needs to bear in mind that the number of subjects in the BD-NOS and BD-I/BD-II/cyclothymia groups was quite small, reducing the power to detect significant differences.
In contrast to the BPSS-P Total score and the Mania and Depression Indices, the BPSS-P General Index only differentiated psychiatric groups from HCs, but not from each other. Although individual items on the BPSS-P General Index could potentially carry some predictive power for the development of mania and although these findings need to be replicated with larger numbers of patients in the bipolar-spectrum groups, these results seem to suggest that the BPSS-P General Index may be too non-specific to yield relevant discriminatory power. We will follow up on these results, but suggest keeping at least the mood lability item (6, 26, 87) in case the BPSS-P General Index will be dropped by some due to time constraints.
Clearly, long-term studies are needed to determine the predictive validity of the BPSS-P, its subscales and/or individual items. In this regard, if it is not feasible to administer the full BPSS-P scale, one could also consider administering only the 10 BPSS-P Mania Index items plus the BPSS-P General Index mood lability item, forming the BPSS-P-Abbreviated (BPSS-P-A), which we are currently testing in several settings. Notably, the BPSS-P Mania Index scores were not only highly correlated with the YMRS, but BPSS-P Mania Index scores were about three times as high as the YMRS scores in each of the five examined diagnostic groups. This suggests that the BPSS-P detects considerable symptomatology that is below the threshold of the syndromal YMRS ratings and anchors. These findings are reflective of the enrichment of the BPSS-P for attenuated mania-like symptoms.
Although the GBI (46-59, 63) and the combination of mania and depression symptom ratings (16, 43, 63) have been used successfully in order to identify individuals at risk for BD, there is a need for an interview that specifically targets symptoms that may emerge during a mania prodrome and that could complement these other approaches. Interestingly, although in one study (82), high ratings on the CHT were predictive of development of broadly defined bipolar-spectrum presentations in adolescents with MDD, in our sample, the CHT was unable to differentiate any of the 4 psychiatric groups from each other.
While the findings of this study are relevant and encouraging, the next important step will need to include longitudinal studies in clinical and familial high-risk individuals in order to assess the predictive validity of the BPSS-P, its subscales or individual items or clusters for the development of BD-I/BD-II/cyclothymia. Ideally, such studies should enrich samples for the presence of additional potential risk markers, including circadian rhythm abnormalities, imaging, electrophysiological and/or genetic markers (1, 5-10) in order to increase the likelihood of conversion to BD-I or BD-II in a reasonable time frame.
Moreover, prospective studies with sufficient numbers of individuals progressing to BD-I/BD-II are needed in order to establish high-risk criteria and thresholds on the BPSS-P for true BD high-risk individuals. While several groups developed theoretical and staging models for the BD prodrome (1, 3, 7-10), to date, few BD high-risk criteria have been proposed and tested. For example, following a large cohort of college students for over eight years, Lewinsohn et al. (88) defined a subsyndromal bipolar subgroup of youth (mean baseline age = 16.8 years) by “distinct period of abnormally and persistent elevated, expansive, or irritable mood, plus >1 manic symptom”. Using such broad criteria, the conversion rate to BD-I/BD-II after eight years was very low (i.e., 1/48 = 2.1%), whereas 40.9% developed MDD. As mentioned before, based on data from the Australian early identification program, Bechdolf and colleagues (44) were able to validate their BAR criteria prospectively, finding that attenuated mania-like symptoms had the greatest predictive value (44). However, a structured assessment of attenuated mania-like symptoms and of other potentially predictive, emerging symptomatology was not available to the authors.
More refined BD high-risk criteria are also hoped to allow for the successful and ethical testing of low-risk ameliorative and, potentially even, preventive interventions. For example, randomized early intervention studies, which have yielded inconclusive results, have largely been limited to high-risk samples of BD offspring with familial loading plus existing mood symptoms (33, 34, 89, 90). In these samples, the BD high-risk may not have been sufficiently imminent. By contrast, the only promising randomized trial mentioned above that tested Multi-Family Psychoeducational Psychotherapy for BD at-risk individuals was conducted in 165 children 8–11 years old with mood disorders in whom the high-risk status for BD was determined using presence of mania-like symptoms (43). This 18-month study followed 37 children with depression-spectrum disorders and transient manic symptoms, 13 youth with depression-spectrum disorders, and 115 with bipolar-spectrum disorders. Transient manic symptoms were defined as ≥ 1 DSM-IV mania criterion, except for irritability, that is distinguishable from ADHD, presence of 1–3 manic-like episodes of moderate to severe intensity lasting ≥ 4 hours, or presence of ≥ 2 brief episodes of 2–4 hours duration, evidence of functional impairment, and lack of a bipolar-spectrum disorder (i.e., BD-I, BD-II, cyclothymia, or BD-NOS). Patients were randomized to receive Multi-Family Psychoeducational Psychotherapy for the duration of the study or only for the last six months, i.e., after a one-year wait-list condition. At 18 months, poorer baseline functioning, as well as receiving the intervention only after one year, rather than immediately, was associated with transitioning to a bipolar-spectrum disorder (60% versus 16%). These findings are the first randomized results suggesting that a psychosocial intervention during a clinically identified high-risk state for BD may be effective in reducing conversion to bipolar-spectrum disorders. To enable an extension of these findings in larger studies and ultimately a clinical application, reliable, valid and practical interview and screening tools need to be developed and tested. We believe that the sound psychometric properties of the BPSS-P are one further step in this direction.
The results of our study need to be interpreted within its limitations. These include the small sample size of the individual bipolar-spectrum disorder groups and the non-mood disorder group, lack of test-retest data and lack of data on the predictive validity for subscales or items of the BPSS-P. The relatively small sample sizes in the psychiatric disorder groups and only partially available MADRS scores also precluded a multivariate examination of the degree to which the BPSS-P indices may add discriminatory power beyond the dimensional assessment of manic and depressive symptoms for distinguishing between mood and non-mood disorders and within mood disorders. Future studies should investigate these issues. Additional limitations include that all patients were help-seeking, that 50–70% received psychotropic medications at the time of the assessment and the diagnostic heterogeneity of the study cohort. However, we consider the focus on help-seeking individuals with a wide variety of psychopathology and psychotropic treatment a strength, as this reflects clinical reality in groups of patients who may be at potential risk for BD, increasing the generalizability and applicability of our findings. Since mood symptoms are more pervasive in the general population than sub/syndromal psychotic experiences, inclusion of diverse and enriched psychiatric control groups is highly desirable. Thus, a BD high-risk assessment instrument needs to be able to differentiate at-risk individuals not from healthy individuals, but rather from patients with a whole host of psychiatric disorders and comorbidities. In this regard the BPSS-P and/or its subscales performed well to excellent in differentiating bipolar-spectrum from depression spectrum and non-psychotic, non-mood spectrum disorder patients. Conduct of this study in only one center and region could be considered a further limitation. However, we believe that the findings have external validity, given the fact that The Zucker Hillside Hospital has a large catchment area of 3.5 million people, is located in a semi-urban location, drawing from more affluent Long Island population as well as urban Queens and Brooklyn, areas which are among the most diverse in the US. Moreover, patients in this study were adolescents or young adults aged 12–23 years old. Although additional data in patients with a broader age range should be collected, the BPSS-P was developed for youth and adults, and 39 adult caregivers were also interviewed about the youths’ symptoms using the informant version of the BPSS-P that is identical, except for asking about of someone else’s symptoms.
A further limitation is the possibility of criterion conflation, i.e., the fact that we cannot rule out that results from the diagnostic interview and the BPSS-R may have influenced each other. Although the scores of the BPSS-P were discussed as part of a consensus conference on an item-by-item fashion, independent of the results of the diagnostic interview, the results found in this study may represent a best case scenario. In order to avoid criterion contamination, future validation studies should consider having different people conduct the BPSS-P and a diagnostic interview. On the other hand, it is likely that the BPSS-P will be utilized together with a diagnostic interview and psychopathology assessments, at least in research settings. Whether parts of the BPSS-P could ultimately be used alone in clinical practice would be a later question after predictive validity of the total interview or item constellations has been established. An abbreviated, self-standing scale with predictive validity would be desirable, as the time needed to complete the entire interview (1.5–3.0 hours) is relatively long. Therefore, future studies are needed that ascertain the test-retest reliability and predictive validity of the BPSS-P as well as of the BPSS-P-A that contains only the 10 BPSS-P Mania items and the mood lability item from the BPSS-P General Symptom Index. Should the BPSS-P Mania Index be most predictive, then the research as well as clinical utility of the much shorter BPSS-P-A scale should be tested more widely. Moreover, we also recently developed a self-rating instrument of the BPSS-P-A, the BPSS-A-Screen in a patient and informant version, which we are currently testing and which may even have greater feasibility for use in clinical care.
In summary, we present the first semi-structured interview and rating scale for the clinical risk for BD, showing good to excellent psychometric properties, including discriminatory power compared to youth with depression-spectrum and non-mood spectrum disorders. Future, longitudinal studies in samples enriched for BD high-risk are needed to further assess the utility of the full BPSS-P and of its subscales in the early identification and risk stratification of help-seeking individuals with symptomatic mood presentations.
Acknowledgments
Supported in part by grant MH 61523-08 by the National Institute of Mental Health (NIMH) (BAC), The Feinstein Institute for Medical Research, and The Zucker Hillside Hospital NIMH Advanced Center for Intervention and Services Research for the Study of Schizophrenia (P30MH090590) (Dr. J.M. Kane).
CUC has received grant support from Bristol-Myers Squibb, the Feinstein Institute for Medical Research, Janssen/Johnson & Johnson, the National Institute of Mental Health (NIMH), the National Alliance for Research in Schizophrenia and Depression (NARSAD), and Otsuka; and has been a consultant and/or advisor to or has received honoraria from Actelion, Alexza, Bristol-Myers Squibb, Cephalon, Eli Lilly & Co., Genentech, Gerson Lehrman Group, IntraCellular Therapies, Lundbeck, Medavante, Medscape, Merck, Ortho-McNeill/Janssen/Johnson & Johnson, Otsuka, Pfizer, ProPhase, Roche, Sunovion, Takeda, Teva, and Vanda. TK has received grant support from the Byoutaitaisyakenkyukai Fellowship (Fellowship of Astellas Foundation of Research on Metabolic Disorders) and Eli Lilly Fellowship for Clinical Psychopharmacology; has received consultant fees from Dainippon Sumitomo, Novartis, and Otsuka; and has received speakers honoraria from Banyu, Eli Lilly & Co., Dainippon Sumitomo, Janssen, Novartis, Otsuka, and Pfizer.
Appendix A. Overview of the Bipolar Prodrome Symptom Interview and Scale–Prospective (BPSS-P) structure and items
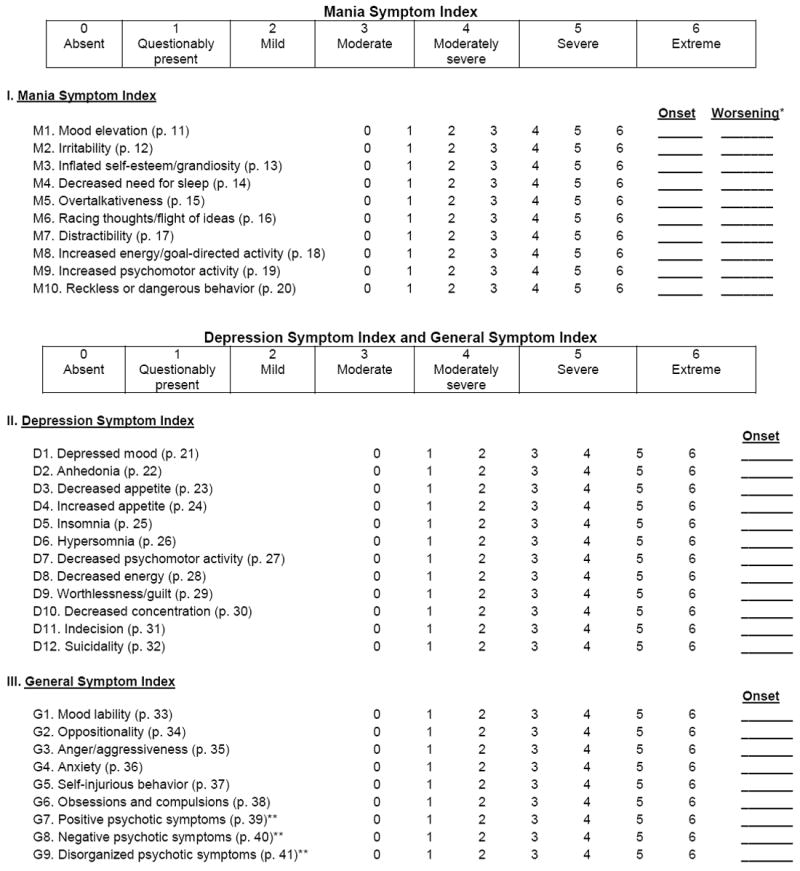
|
Worsening: Record most recent date when a symptom currently rated 3–5 experienced an increase in intensity by at least one rating point.
Optional items; rate only if not also using the SIPS/SOPS or CAARMS for a more-detailed assessment of prodromal psychotic symptoms.
Footnotes
Disclosures
DMO, AMA, MH, REC, SS, and BAC do not have any conflicts of interest to report.
References
- 1.Correll CU, Penzner JB, Lencz T, et al. Early identification and high-risk strategies for bipolar disorder. Bipolar Disord. 2007;9:324–338. doi: 10.1111/j.1399-5618.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 2.Bauer M, Juckel G, Correll CU, Leopold K, Pfennig A. Diagnosis and treatment in the early phase of bipolar disorders. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl. 5):50–54. doi: 10.1007/s00406-008-5009-z. [DOI] [PubMed] [Google Scholar]
- 3.Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord. 2010;127:316–320. doi: 10.1016/j.jad.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Conus P, Ward J, Lucas N, et al. Characterisation of the prodrome to a first episode of psychotic mania: results of a retrospective study. J Affect Disord. 2010;124:341–345. doi: 10.1016/j.jad.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 5.Luby JL, Navsaria N. Pediatric bipolar disorder: evidence for prodromal states and early markers. J Child Psychol Psychiatry. 2010;51:459–471. doi: 10.1111/j.1469-7610.2010.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skjelstad DV, Malt UF, Holte A. Symptoms and signs of the initial prodrome of bipolar disorder: a systematic review. J Affect Disord. 2010;126:1–13. doi: 10.1016/j.jad.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Pavuluri MN. Effects of early intervention on the course of bipolar disorder: theories and realities. Curr Psychiatry Rep. 2010;12:490–498. doi: 10.1007/s11920-010-0155-1. [DOI] [PubMed] [Google Scholar]
- 8.McNamara RK, Nandagopal JJ, Strakowski SM, DelBello MP. Preventative strategies for early-onset bipolar disorder: towards a clinical staging model. CNS Drugs. 2010;24:983–996. doi: 10.2165/11539700-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Leopold K, Ritter P, Correll CU, et al. Risk constellations prior to the development of bipolar disorders: rationale of a new risk assessment tool. J Affect Disord. 2012;136:1000–1010. doi: 10.1016/j.jad.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 10.Brietzke E, Mansur RB, Soczynska JK, Kapczinski F, Bressan RA, McIntyre RS. Towards a multifactorial approach for prediction of bipolar disorder in at risk populations. J Affect Disord. 2012;140:82–91. doi: 10.1016/j.jad.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 11.Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: a metaanalysis of risk for mental disorders. Can J Psychiatry. 1997;42:623–631. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- 12.Chang KD, Steiner H, Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. J Am Acad Child Adolesc Psychiatry. 2000;39:453–460. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 13.DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disord. 2001;3:325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 14.Chang K, Steiner H, Ketter T. Studies of offspring of parents with bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;123:26–35. doi: 10.1002/ajmg.c.20011. [DOI] [PubMed] [Google Scholar]
- 15.Egeland JA, Shaw JA, Endicott J, et al. Prospective study of prodromal features for bipolarity in well Amish children. J Am Acad Child Adolesc Psychiatry. 2003;42:786–796. doi: 10.1097/01.CHI.0000046878.27264.12. [DOI] [PubMed] [Google Scholar]
- 16.Findling RL, Youngstrom EA, McNamara NK, et al. Early symptoms of mania and the role of parental risk. Bipolar Disord. 2005;7:623–634. doi: 10.1111/j.1399-5618.2005.00260.x. [DOI] [PubMed] [Google Scholar]
- 17.Henin A, Biederman J, Mick E, et al. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry. 2005;58:554–561. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Hillegers MH, Reichart CG, Wals M, Verhulst FC, Ormel J, Nolen WA. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disord. 2005;7:344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 19.Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disord. 2007;9:828–838. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 20.Duffy A. The early course of bipolar disorder in youth at familial risk. J Can Acad Child Adolesc Psychiatry. 2009;18:200–205. [PMC free article] [PubMed] [Google Scholar]
- 21.Duffy A, Alda M, Hajek T, Sherry SB, Grof P. Early stages in the development of bipolar disorder. J Affect Disord. 2010;121:127–135. doi: 10.1016/j.jad.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 22.Correll CU, Hauser M, Auther AM, Cornblatt BA. Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol Psychiatry. 2010;514:390–431. doi: 10.1111/j.1469-7610.2010.02235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fusar-Poli P, Bonoldi I, Yung AR, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–229. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- 24.Berk M, Conus P, Lucas N, et al. Setting the stage: from prodrome to treatment resistance in bipolar disorder. Bipolar Disord. 2007;9:671–678. doi: 10.1111/j.1399-5618.2007.00484.x. [DOI] [PubMed] [Google Scholar]
- 25.Correll CU, Penzner JB, Frederickson AM, et al. Differentiation in the preonset phases of schizophrenia and mood disorders: evidence in support of a bipolar mania prodrome. Schizophr Bull. 2007;33:703–714. doi: 10.1093/schbul/sbm028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hauser M, Pfennig A, Ozgürdal S, Heinz A, Bauer M, Juckel G. Early Recognition of bipolar disorder. Eur Psychiatry. 2007;22:92–98. doi: 10.1016/j.eurpsy.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 27.Conus P, Ward J, Hallam KT, et al. The proximal prodrome to first episode mania – a new target for early intervention. Bipolar Disord. 2008;10:555–565. doi: 10.1111/j.1399-5618.2008.00610.x. [DOI] [PubMed] [Google Scholar]
- 28.Miklowitz DJ, Chang KD. Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Dev Psychopathol. 2008;20:881–897. doi: 10.1017/S0954579408000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bechdolf A, Ratheesh A, Wood SJ, et al. Rationale and first results of developing at-risk (prodromal) criteria for bipolar disorder. Curr Pharm Des. 2012;18:358–375. doi: 10.2174/138161212799316226. [DOI] [PubMed] [Google Scholar]
- 30.Howes OD, Lim S, Theologos G, Yung AR, Goodwin GM, McGuire P. A comprehensive review and model of putative prodromal features of bipolar affective disorder. Psychol Med. 2011;41:1567–1577. doi: 10.1017/S0033291710001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 32.Perlis RH, Miyahara S, Marangell LB, et al. STEP-BD Investigators: Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biol Psychiatry. 2004;55:875–881. doi: 10.1016/j.biopsych.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 33.DelBello MP, Adler CM, Whitsel RM, Stanford KE, Strakowski SM. A 12-week single-blind trial of quetiapine for the treatment of mood symptoms in adolescents at high risk for developing bipolar I disorder. J Clin Psychiatry. 2007;68:789–795. doi: 10.4088/jcp.v68n0520. [DOI] [PubMed] [Google Scholar]
- 34.Findling RL, Frazier TW, Youngstrom EA, et al. Double-blind, placebo-controlled trial of divalproex monotherapy in the treatment of symptomatic youth at high risk for developing bipolar disorder. J Clin Psychiatry. 2007;68:781–788. doi: 10.4088/jcp.v68n0519. [DOI] [PubMed] [Google Scholar]
- 35.Hauser M, Correll CU. The significance of at-risk or prodromal symptoms of bipolar I disorder in children and adolescents. Can J Psychiatry. 2013;58:22–31. doi: 10.1177/070674371305800106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Häfner H, an der Heiden W. The course of schizophrenia in the light of modern follow-up studies: the ABC and WHO studies. Eur Arch Psychiatry Clin Neurosci. 1999;249(Suppl. 4):14–26. doi: 10.1007/pl00014180. [DOI] [PubMed] [Google Scholar]
- 37.Hegerl U, Bottner AC, Holtschmidt-Täschner B, et al. Onset of depressive episodes is faster in patients with bipolar versus unipolar depressive disorder: evidence from a retrospective comparative study. J Clin Psychiatry. 2008;69:1075–1080. doi: 10.4088/jcp.v69n0705. [DOI] [PubMed] [Google Scholar]
- 38.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- 39.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160:430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 40.Geller B, Luby JL, Joshi P, et al. A randomized controlled trial of risperidone, lithium, or divalproex sodium for initial treatment of bipolar I disorder, manic or mixed phase, in children and adolescents. Arch Gen Psychiatry. 2012;69:515–528. doi: 10.1001/archgenpsychiatry.2011.1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olvet DM, Stearns WH, McLaughlin D, Auther AM, Correll CU, Cornblatt BA. Comparing clinical and neurocognitive features of the schizophrenia prodrome to the bipolar prodrome. Schizophr Res. 2010;123:59–63. doi: 10.1016/j.schres.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tijssen MJ, Van Os J, Wittchen HU, Lieb R, Beesdo K, Wichers M. Risk factors predicting onset and persistence of subthreshold expression of bipolar psychopathology among youth from the community. Acta Psychiatr Scand. 2010;122:255–266. doi: 10.1111/j.1600-0447.2010.01539.x. [DOI] [PubMed] [Google Scholar]
- 43.Nadkarni RB, Fristad MA. Clinical course of children with a depressive spectrum disorder and transient manic symptoms. Bipolar Disord. 2010;12:494–503. doi: 10.1111/j.1399-5618.2010.00847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bechdolf A, Ratheesh A, Cotton SM, et al. The predictive validity of bipolar at-risk (prodromal) criteria in help-seeking adolescents and young adults: a prospective study. Bipolar Disord. 2014 doi: 10.1111/bdi.12205. in press. [DOI] [PubMed] [Google Scholar]
- 45.Depue RA, Slater JF, Wolfstetter-Kausch H, Klein D, Goplerud E, Farr D. A behavioral paradigm for identifying persons at risk for bipolar depressive disorder: a conceptual framework and five validation studies. J Abnorm Psychol. 1981;90:381–437. doi: 10.1037//0021-843x.90.5.381. [DOI] [PubMed] [Google Scholar]
- 46.Depue RA, Krauss S, Spoont MR, Arbisi P. General behavior inventory identification of unipolar and bipolar affective conditions in a nonclinical university population. J Abnorm Psychol. 1989;98:117–126. doi: 10.1037//0021-843x.98.2.117. [DOI] [PubMed] [Google Scholar]
- 47.Klein DN, Depue RA. Continued impairment in persons at risk for bipolar affective disorder: results of a 19-month follow-up study. J Abnorm Psychol. 1984;93:345–347. doi: 10.1037//0021-843x.93.3.345. [DOI] [PubMed] [Google Scholar]
- 48.Klein DN, Depue RA, Slater JF. Cyclothymia in the adolescent offspring of parents with bipolar affective disorder. J Abnorm Psychol. 1985;94:115–127. doi: 10.1037//0021-843x.94.2.115. [DOI] [PubMed] [Google Scholar]
- 49.Klein DN, Depue RA, Slater JF. Inventory identification of cyclothymia. IX. Validation in offspring of bipolar I patients. Arch Gen Psychiatry. 1986;43:441–445. doi: 10.1001/archpsyc.1986.01800050043005. [DOI] [PubMed] [Google Scholar]
- 50.Reichart CG, van der Ende J, Wals M, et al. The use of the GBI in a population of adolescent offspring of parents with a bipolar disorder. J Affect Disord. 2004;80:263–267. doi: 10.1016/S0165-0327(03)00115-0. [DOI] [PubMed] [Google Scholar]
- 51.Youngstrom EA, Findling RL, Danielson CK, Calabrese JR. Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychol Assess. 2001;13:267–276. [PubMed] [Google Scholar]
- 52.Findling RL, Youngstrom EA, Danielson CK, et al. Clinical decision-making using the General Behavior Inventory in juvenile bipolarity. Bipolar Disord. 2002;4:34–42. doi: 10.1034/j.1399-5618.2002.40102.x. [DOI] [PubMed] [Google Scholar]
- 53.Reichart CG, van der Ende J, Wals M, et al. The use of the GBI as predictor of bipolar disorder in a population of adolescent offspring of parents with a bipolar disorder. J Affect Disord. 2005;89:147–155. doi: 10.1016/j.jad.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 54.Meyer B, Johnson SL, Carver CS. Exploring behavioral activation and inhibition sensitivities among college students at risk for bipolar spectrum symptomatology. J Psychopathol Behav Assess. 1999;21:275–292. doi: 10.1023/A:1022119414440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Danielson CK, Youngstrom EA, Findling RL, Calabrese JR. Discriminative validity of the general behavior inventory using youth report. J Abnorm Child Psychol. 2003;31:29–39. doi: 10.1023/a:1021717231272. [DOI] [PubMed] [Google Scholar]
- 56.Youngstrom EA, Findling RL, Calabrese JR, Gracious BL, et al. Comparing the diagnostic accuracy of six potential screening instruments for bipolar disorder in youths aged 5 to 17 years. J Am Acad Child Adolesc Psychiatry. 2004;43:847–858. doi: 10.1097/01.chi.0000125091.35109.1e. [DOI] [PubMed] [Google Scholar]
- 57.Youngstrom E, Meyers O, Demeter C, et al. Comparing diagnostic checklists for pediatric bipolar disorder in academic and community mental health settings. Bipolar Disord. 2005;7:507–517. doi: 10.1111/j.1399-5618.2005.00269.x. [DOI] [PubMed] [Google Scholar]
- 58.Fristad MA, Frazier TW, Youngstrom EA, et al. What differentiates children visiting outpatient mental health services with bipolar spectrum disorder from children with other psychiatric diagnoses? Bipolar Disord. 2012;14:497–506. doi: 10.1111/j.1399-5618.2012.01034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pendergast LL, Youngstrom EA, Merkitch KG, et al. Differentiating bipolar disorder from unipolar depression and ADHD: the utility of the General Behavior Inventory. Psychol Assess. 2014;26:195–206. doi: 10.1037/a0035138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Horwitz SM, Demeter CA, Pagano ME, et al. Longitudinal Assessment of Manic Symptoms (LAMS) study: background, design, and initial screening results. J Clin Psychiatry. 2010;71:1511–1517. doi: 10.4088/JCP.09m05835yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Findling RL, Youngstrom EA, Fristad MA, et al. Characteristics of children with elevated symptoms of mania: the Longitudinal Assessment of Manic Symptoms (LAMS) study. J Clin Psychiatry. 2010;71:1664–1672. doi: 10.4088/JCP.09m05859yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Youngstrom EA, Frazier TW, Demeter C, Calabrese JR, Findling RL. Developing a 10-item mania scale from the Parent General Behavior Inventory for children and adolescents. J Clin Psychiatry. 2008;69:831–839. doi: 10.4088/jcp.v69n0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Findling RL, Jo B, Frazier TW, Youngstrom EA, et al. The 24-month course of manic symptoms in children. Bipolar Disord. 2013;15:669–679. doi: 10.1111/bdi.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Achenbach TM. Integrative Guide to the 1991 CBCL/4-18, YSR, and TRF Profiles. Burlington: University of Vermont, Department of Psychology; 1991. [Google Scholar]
- 65.Ayer L, Althoff R, Ivanova M, et al. Child Behavior Checklist Juvenile Bipolar Disorder (CBCL-JBD) and CBCL Posttraumatic Stress Problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. J Child Psychol Psychiatry. 2009;50:1291–1300. doi: 10.1111/j.1469-7610.2009.02089.x. [DOI] [PubMed] [Google Scholar]
- 66.Biederman J, Petty CR, Monuteaux MC, et al. The Child Behavior Checklist-Pediatric Bipolar Disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. J Clin Psychiatry. 2009;70:732–740. doi: 10.4088/JCP.08m04821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Diler RS, Birmaher B, Axelson D, et al. The Child Behavior Checklist (CBCL) and the CBCL-bipolar phenotype are not useful in diagnosing pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2009;19:23–30. doi: 10.1089/cap.2008.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Holtmann M, Buchmann AF, Esser G, Schmidt MH, Banaschewski T, Laucht M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: a longitudinal analysis. J Child Psychol Psychiatry. 2011;52:139–147. doi: 10.1111/j.1469-7610.2010.02309.x. [DOI] [PubMed] [Google Scholar]
- 69.Meyer SE, Carlson GA, Youngstrom E, et al. Long-term outcomes of youth who manifested the CBCL-pediatric bipolar disorder phenotype during childhood and/or adolescence. J Affect Disord. 2009;113:227–235. doi: 10.1016/j.jad.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 70.Volk HE, Todd RD. Does the Child Behavior Checklist juvenile bipolar disorder phenotype identify bipolar disorder? Biol Psychiatry. 2007;62:115–120. doi: 10.1016/j.biopsych.2006.05.036. [DOI] [PubMed] [Google Scholar]
- 71.Youngstrom E, Youngstrom JK, Starr M. Bipolar diagnoses in community mental health: Achenbach Child Behavior Checklist profiles and patterns of comorbidity. Biol Psychiatry. 2005;58:569–575. doi: 10.1016/j.biopsych.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 72.Haslam N. Categorical versus dimensional models of mental disorder: the taxometric evidence. Aust N Z J Psychiatry. 2003;37:696–704. doi: 10.1080/j.1440-1614.2003.01258.x. [DOI] [PubMed] [Google Scholar]
- 73.Prisciandaro JJ, Roberts JE. A comparison of the predictive abilities of dimensional and categorical models of unipolar depression in the National Comorbidity Survey. Psychol Med. 2009;39:1087–1096. doi: 10.1017/S0033291708004522. [DOI] [PubMed] [Google Scholar]
- 74.Miller TJ, McGlashan TH, Rosen JL, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 75.Yung AR, Phillips LJ, McGorry PD, et al. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry Suppl. 1998;172:14–20. [PubMed] [Google Scholar]
- 76.Schultze-Lutter F, Ruhrmann S, Klosterkoetter J. Can schizophrenia be predicted phenomenologically? In: Johannessen JO, Martindale B, Cullberg J, editors. Evolving psychosis, Different Stages, Different Treatments. Routledge; London, New York: 2006. pp. 104–123. [Google Scholar]
- 77.Geller B, Zimerman B, Williams M, et al. Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry. 2001;40:450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- 78.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV–Clinical Version (SCID-I/CV) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 79.Kaufman J, Birmaher B, Rao U, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 80.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 81.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 82.Kochman FJ, Hantouche EG, Ferrari P, Lancrenon S, Bayart D, Akiskal HS. Cyclothymic temperament as a prospective predictor of bipolarity and suicidality in children and adolescents with major depressive disorder. J Affect Disord. 2005;85:181–189. doi: 10.1016/j.jad.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 83.Akiskal HS, Akiskal KK, Haykal RF, Manning JS, Connor PD. TEMPS-A: progress towards validation of a self-rated clinical version of the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord. 2005;85:3–16. doi: 10.1016/j.jad.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 84.Nunnally JC, Bernstein LH. Psychometric Theory. New York: McGraw-Hill; 1994. [Google Scholar]
- 85.Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80:99–103. doi: 10.1207/S15327752JPA8001_18. [DOI] [PubMed] [Google Scholar]
- 86.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 87.Ozgürdal S, van Haren E, Hauser M, et al. Early mood swings as symptoms of the bipolar prodrome: preliminary results of a retrospective analysis. Psychopathology. 2009;42:337–334. doi: 10.1159/000232977. [DOI] [PubMed] [Google Scholar]
- 88.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000;2:281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- 89.Geller B, Cooper TB, Zimerman B, et al. Lithium for prepubertal depressed children with family history predictors of future bipolarity: a double-blind, placebo-controlled study. J Affect Disord. 1998;51:165–175. doi: 10.1016/s0165-0327(98)00178-5. [DOI] [PubMed] [Google Scholar]
- 90.Chang KD, Dienes K, Blasey C, Adleman N, Ketter T, Steiner H. Divalproex monotherapy in the treatment of bipolar offspring with mood and behavioral disorders and at least mild affective symptoms. J Clin Psychiatry. 2003;64:936–942. doi: 10.4088/jcp.v64n0812. [DOI] [PubMed] [Google Scholar]


