Abstract
The history of pollinosis in Japan before the discovery of Japanese cedar pollinosis was presented in part I in this paper. Until early 1960s, it was believed that there was no pollinosis in Japan except one case of ragweed pollinosis.
The summary of how the Japanese cedar pollinosis was discovered and named was presented in part II, by referring to the paper in which we reported the presence of Japanese cedar pollinosis for the first time.
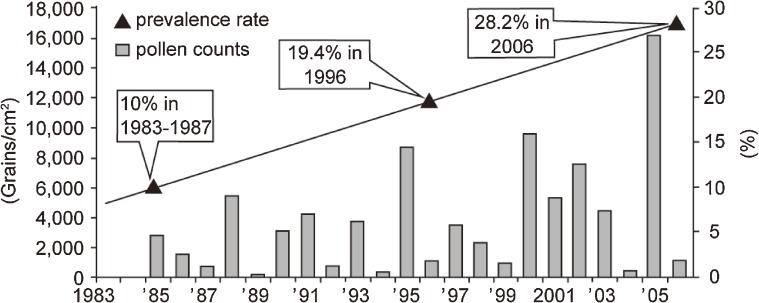
The epidemiology after the discovery of Japanese cedar pollinosis was presented in part III. The number of the patients suffering from Japanese cedar pollinosis gradually increased since the 1970s. The annual incidence rate of the pollinosis had correlations with the dispersed pollen count per year. The prevalence rate of the patients with Japanese cedar pollinosis increased from 16.2% in 1998 to 26.5% in 2008 by the nationwide survey. The prevalence rate of the patients with Japanese cedar pollinosis in Tokyo metropolitan area was 10% from 1983 to 1987, 19.4% in 1996, and 28.2% in 2006.
The prospects of current research and future studies were discussed in parts IV and V.
Keywords: Japanese cedar, pollinosis, Japanese cedar pollinosis
Part I. Pollinosis in Japan before the discovery of Japanese cedar pollinosis
In 1828, Bostock1) published the first report on the hay fever. Subsequently, Blackley2) demonstrated in 1873 that the hay fever is caused by the pollen of Gramineae grasses. Thus, hay fever has been a well-known disease for a long time in Europe and the United States, although it was not recognized in Japan until the 1930s. When I wrote the first review article entitled “Pollinosis in Japan”,3) only a few reports could be cited in the references. The report by Misawa,4) which was one of those cited in my review, indicated that some Japanese living in the U.S. often developed hay fever. Hara,5) a second-generation Japanese-American living in Los Angeles, conducted research on airborne pollens in Sapporo, Tokyo, and Kobe.5) He reported that many pollens were detected in the air, but very few of these pollens were known to cause hay fever. Airborne Japanese cedar pollen was not described in the report.
After World War II, Alford (a U.S. military doctor) published a brief report entitled “Allergy in Japan” 6) regarding allergic diseases that he saw and heard about in Japan. Since hay fever caused by ragweed was a serious problem in the U.S. at that time, but was not found in Japan, Alford speculated that pollens released from ragweed and Gramineae grasses did not appear to act as allergens in Japan probably because of the local climate.
In a brief report titled “Ragweed in Japan” 7) Durham (a botanist) cited the above-mentioned report by Hara5) on the airborne pollens, and stated that ragweed was uncommon in Japan, and therefore that airborne ragweed pollen did not cause any problem. It was thought for a long time in Europe and the U.S. that there was no problem of the pollinosis-type allergy in Japan. Around that time in Japan, Ueno (a botanist) reported on the status of pollinosis in the U.S. and emphasized the importance of studying pollinosis.8) Ikuse et al. (botanists) also considered that the study of airborne pollens was important.9)
The first review article on the pollinosis in Japan “Pollen allergy” 10) was published by Ishizaki in 1957, and the first systematic study of pollinosis in Japan was carried out on ragweed pollinosis by Araki in 1960–61.11,12) He performed two-year survey on airborne pollens (mainly in Tokyo) to assess the seasonal variation of Cryptomeria japonica (Japanese cedar), Pinus, and ragweed pollens. In this paper, he also described one patient suffering from ragweed pollinosis. Subsequent investigation on pollinosis in Japan has been based on these studies conducted by the above-mentioned forerunners. It should be noted that Japanese cedar pollinosis, which is the primary subject of the present review, was discovered with much assistance from the findings of these forerunners.
Part II. Discovery and nomenclature of Japanese cedar pollinosis
Japanese cedar pollinosis is the first pollinosis which is caused by the plant indigenous to wide regions of Japan. Our first case report published in 1964 was only three pages long and was entitled “Japanese cedar pollinosis in Nikko, Japan”.13) The first author of the report was our professor Dr. Horiguchi, who supervised our study. Here, I will summarize that report and review the discovery and nomenclature of Japanese cedar pollinosis.
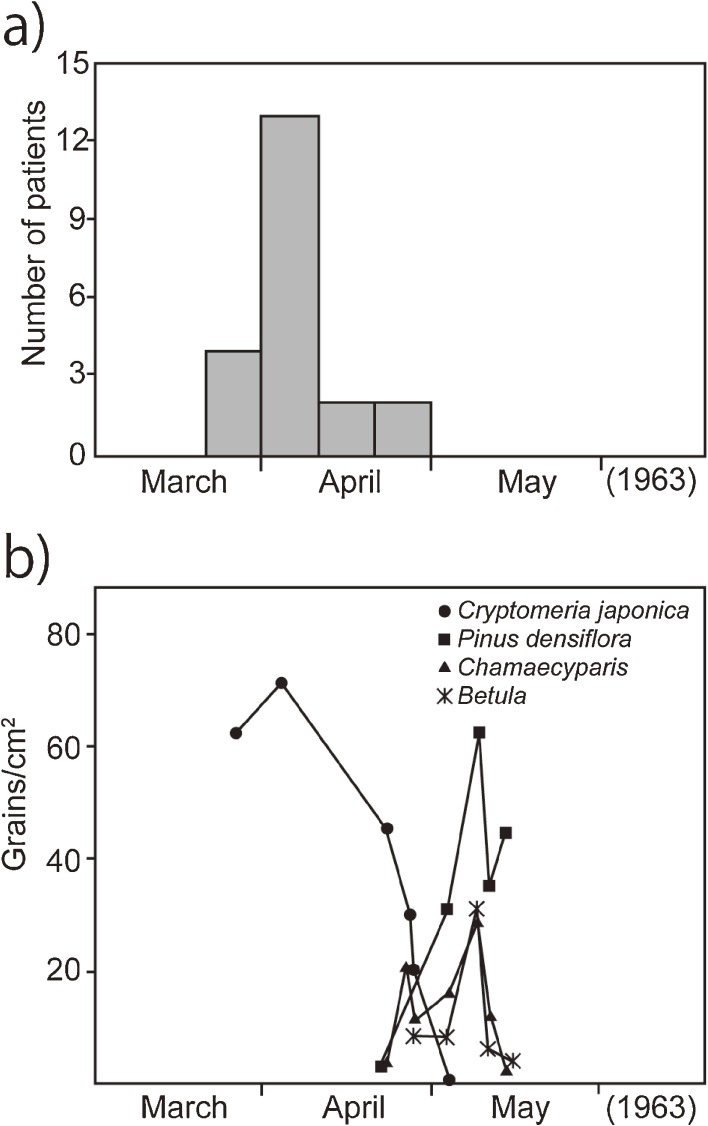
In the spring of 1963, I was working in the otolaryngology department of the former Nikko Denki Seidosho Hospital (Furukawa Electric Co., Ltd.) in Nikko (Tochigi Prefecture) immediately before completion of my graduate course. In March and April of the year, I encountered 21 patients who complained for allergic symptoms affecting the nose, eyes, and throat (Fig. 1a). This experience was the prelude to the discovery of Japanese cedar pollinosis. The main symptoms of these patients were intranasal itching, paroxysmal sneezing, watery rhinorrhea, nasal obstruction, pharyngeal itching, and conjunctival itching. They claimed that they had these symptoms from late March to late April every year, but did not have such symptoms during the rest of the year. Upon examination, the nasal mucosa of the patients showed edematous swelling. They also had watery rhinorrhea, and the nasal smear test revealed eosinophilia in the rhinorrhea. Histopathological examination of biopsy specimens from the nasal turbinate mucosa was performed in some patients. The results showed exfoliation of epithelial cells and prominent infiltration of eosinophils in the lamina propria of the mucous membrane.13)
Figure 1.
a) The first visit of 21 patients with Japanese cedar pollinosis in 1963. Each column represents the number of patients during 10-days period. b) Airborne pollen grains collected in 24 hours on one square centimeter of the slide glass, from March to May in 1963 (Modified from ref. 13).
As a possible common allergen for these patients, I suspected pollens because the patients had seasonal symptoms. Therefore, I conducted a field study of pollens of anemophilous flowers and plants that bloom during March and April in Nikko, and identified Cryptomeria japonica (Japanese cedar), Chamaecyparis (Japanese cypress), Betula, and Pinus densiflora. In addition, an investigation of airborne pollens was conducted by the gravity slide method (Fig. 1b). This study revealed the presence of high levels of Japanese cedar pollen grains in the air in March to April. The peak of Japanese cedar pollen dispersal corresponded to the peak of new patients suffering from allergy symptoms (Fig. 1a and 1b). Since the allergen extract from Japanese cedar pollen (Torii Pharmaceutical Co., Ltd.) was available, intracutaneous reaction test was carried out using the allergen extract of Japanese cedar pollen. Positive reactions to the allergen extract were obtained in 18 of the 21 patients (85.7%), while negative reaction was seen in all of the 73 healthy volunteers. In 2 of the 21 patients presenting allergic symptoms, the Prausnitz-Küstner (P-K) skin test (which detects reagins in patient serum based on the skin reaction) was performed and the results showed positive reactions to Japanese cedar pollen. Although IgE had not been discovered at that time, the P-K reaction demonstrated the presence of reagin specific for the Japanese cedar pollen antigens in their serum.
In the nasal mucosa provocation test, in which a tiny amount of Japanese cedar pollen was administered into the nasal cavity (sniff test), violent allergic symptoms were induced in all of the 21 patients (100%). In the conjunctival tests, in which a tiny amount of Japanese cedar pollen was placed on the conjunctiva at the inner canthus, caused itching, hyperemia, and/or edema in 18 of the 21 patients (85.7%).
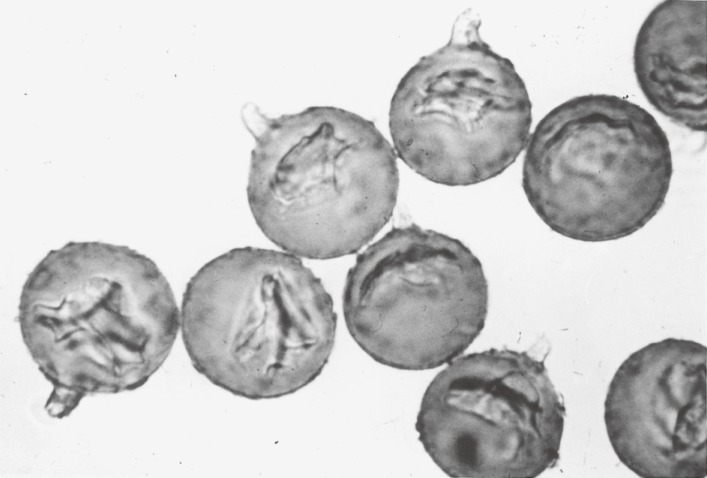
Based on the results of the clinical allergological, immunoserological, and palynological examinations, I concluded that the 21 patients had pollinosis, with the causative allergen being pollen of Cryptomeria japonica D. Don (Japanese cedar) (Fig. 2). Thus, we named this disease as “Japanese cedar pollinosis”.
Figure 2.
Japanese cedar pollen grains are almost globular, approximately 30 µm in diameter, provided with a single germ pore, consisting of a finger-like projection called papillae standing straight up from the surface and slightly bent at the top.
The abstract of the article reporting this research was presented at the 13th annual meeting of Japanese Society of Allergology (Kobe, October 1963) followed by publication of the original article in the Japanese Journal of Allergology Vol. 13 (Jan-Feb combined issue).13)
Since then, I investigated more patients of Japanese ceder pollinosis, and reported the results in Japan.14,15) However, I have not submitted any report to international journals. Consequently, the first article on Japanese cedar pollinosis in an international Journal was published in 1987 by Ishizaki et al.16) This article cited our work13) on Japanese cedar pollinosis and made the indigenous Japanese cedar pollinosis well-known in Europe and the U.S.
Part III. Epidemiological trends of Japanese cedar pollinosis
1. When the patients with Japanese cedar pollinosis began to increase?
1). Investigations by the pollinosis study group in the Ministry of Health and Welfare.
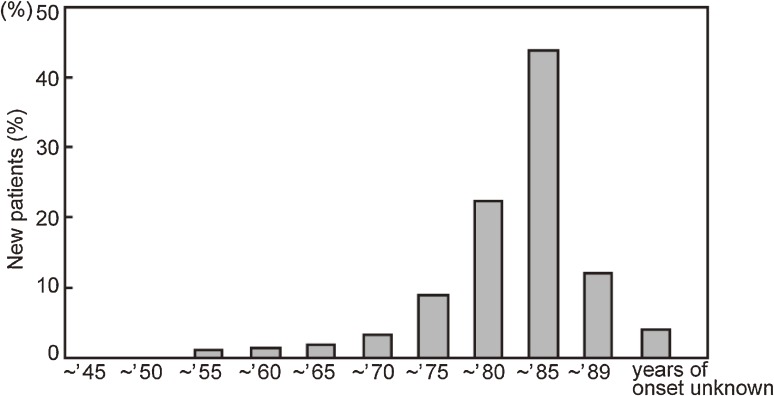
A three-year survey organized by the Ministry of Health and Welfare was performed in 1987–198917) to assess the timing of disease onset in 981 patients with Japanese cedar pollinosis (Fig. 3). The survey included the data obtained by the otolaryngology department of Tokyo Medical and Dental University to which I belonged. The results showed that Japanese cedar pollinosis patients started to appear in the 1950s and the number of the patients increased gradually since the 1970s. The peak period for the incidence rate of the pollinosis was 1981–1985 when 44.5% of the patients began to develop pollinosis. The next highest peak was observed in 1976–1980 (23.0%), followed by those in 1986–1989 (12.3%) and then in 1971–1975 (9.3%).
Figure 3.
Distribution of the onsets of Japanese cedar pollinosis in 981 patients from a survey conducted in 1987–1989 by the pollinosis study group of the Ministry of Health and Welfare. Each column represents the number of patients during a 5-years period (e.g., ∼’50 means 1946–1950) (Modified from ref. 17).
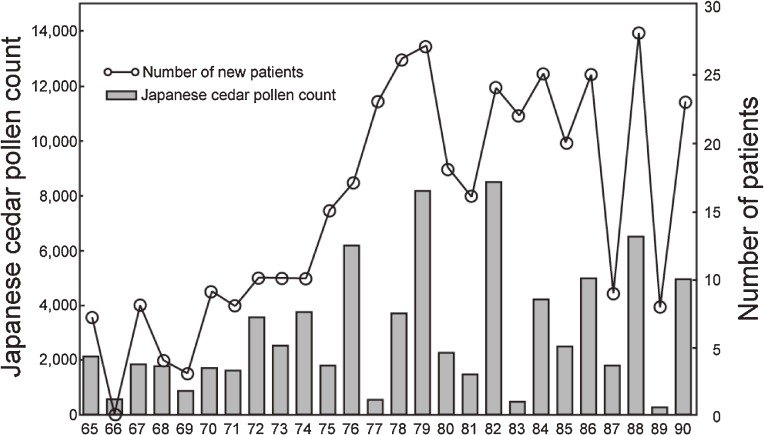
2). New pollinosis patients and the dynamics of airborne pollen.
I studied the relationship between the year of the incidence of Japanese cedar pollinosis and the change in the levels of airborne Japanese cedar pollen over time.18) As shown in Fig. 4, the first high cedar pollen count was seen in 1976 and the number of new patients increased dramatically in the year. In view of the above-mentioned findings of the pollinosis study group in the Ministry of Health and Welfare, one might notice that there were some (if not many) patients with Japanese cedar pollinosis before I discovered the patients of this disease in 1964 (see Fig. 3, columns before 1960).
Figure 4.
The airborne Japanese cedar pollen count and the number of new patients with Japanese cedar pollinosis over time. (a) ○: Number of new patients. Of 414 patients enrolled, 19 patients who developed pollinosis in 1964 or earlier were excluded, and the results of 395 patients are shown (data from Tokyo Medical and Dental University). (b) Each column represents a pollen count. Japanese cedar pollen counts from Sagamihara National Hospital (Director, Takao Shida) (Modified from ref. 18).
3). Background of the patients.
Based on the two investigations described above on the year of onset of Japanese cedar pollinosis, a rapid increase in the incidence rate appears to be directly correalated with the sudden increases of Japanese cedar pollen dispersal in the 1970s (cf. Fig. 4), and further increases occurred every few years since then. Why did Japanese cedar pollen levels increase so dramatically? To determine the cause of the increases in Japanese cedar pollen levels, we should consider about the Japanese cedar forests, which are the source of the pollen.
Regarding the increase of Japanese cedar forests since the Meiji era (1868∼), the area of these forests expanded dramatically during the period from 1957 to 1972, which is known as the expansive afforestation era in Japan. During this period, many trees of only one species (Cryptomeria japonica) were planted within a short period of time throughout Japan, except in Hokkaido and Okinawa. As the result, uniform Cryptomeria japonica forests currently account for 45% of all coniferous plantations, and the forests consist of Japanese cedars aged from 26 to 45 years, which are the optimum age for production of their pollen.
In the past, there were probably no uniform forests such as those currently growing in Japan. To my knowledge, there were no uniform forests in the Meiji era or later until the era for expansive afforestation of Cryptomeria japonica. Creating these uniform plantation forests has led to a “baby-boom” generation of Japanese cedars and has caused the explosion of Japanese cedar pollinosis since the 1970s. Due to the high cedar pollen levels, the new explosive outbreak of Japanese cedar pollinosis patients recurred every few years. Once a patient has developed this condition, it does not resolve naturally at an early stage, and the number of patients with Japanese cedar pollinosis continue to increase cumulatively (note 28.2% in 2006, as shown in Fig. 5).
Figure 5.
Time-course of prevalence rate of pollinosis according to three successive surveys and average Japanese cedar and Japanese cypress pollen counts in Tokyo during the survey periods. ▲ represents the prevalence rate of pollinosis, and each column represents a pollen count (Modified from ref. 21).
4). Seroepidemiological study.
Inouye et al.19) carried out a seroepidemiological study to investigate whether the prevalence of Japanese cedar pollinosis had increased during the 1970s to 1980s. They assayed the IgE antibody specific for Japanese cedar allergen by a fluorometric EIA in the sera collected in different time from adult populations (20–39 years of age) who were residing in Gunma Prefecture and kept stored at −40 ℃ in a serum bank. They found that the IgE prevalence increased over 4-fold from 8.7% (24/277) in 1973 to 36.7% (117/319) in 1984–5.
2. Changes in the prevalence of Japanese cedar pollinosis.
1). National epidemiological survey.
Baba et al.20) reported the results of annual epidemiological surveys of Japanese cedar pollinosis. The results of the surveys, in which otolaryngologists and their family members completed questionnaires, showed that the prevalence rate of Japanese cedar pollinosis increased from 16.2% in 1998 to 26.5% in 2008, so the rate increased by approximately 10% over the 10-years period.
2). Survey performed in Tokyo.
The Tokyo Metropolitan Government was the first local government to establish an action committee for pollinosis in 1983 and this committee still exists. I was involved in various projects of the committee, as the chairman, for 15 years until 1998. The first project of the study group was a survey of the prevalence rate of the Japanese cedar pollinosis in three communities in Tokyo (Ohta Ward, Chofu City, and Akiruno City), in which we employed questionnaires, pollen count and the measurement of IgE antibodies specific for the Japanese cedar pollen allergen in the serum of the residents.21) In this study, the pollen count included the number of Chamaecyparis (Japanese cypress) pollen, which shares common antigenic determinants with Japanese cedar pollen allergen. As expected, clinical role of Japanese cypress pollen as a cause of pollinosis was recently recognized.
The results of the study, shown in Fig. 5, indicated that the estimated prevalence rate of Japanese cedar pollinosis in Tokyo was 10.0% in 1983 to 1987, but the rate increased to 19.4% in 1996 and to 28.2% in 2006.21) Thus it appears that approximately 1 out of 3.5 residents in Tokyo were suffering from Japanese cedar pollinosis in 2006.
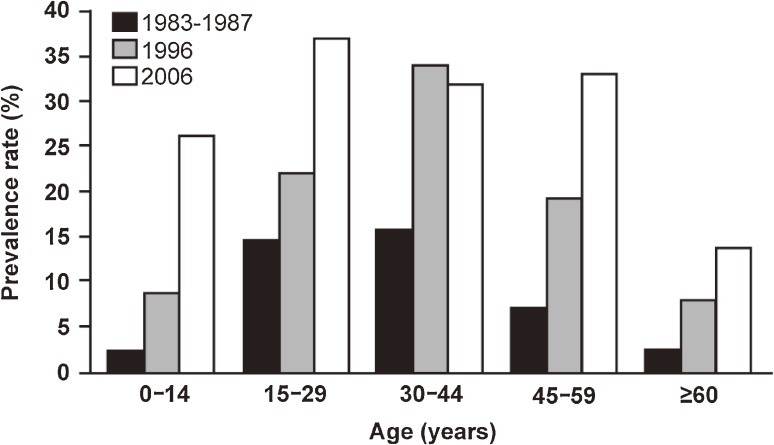
Figure 6 shows the estimated prevalence rate of the pollinosis in different age groups of the residents involved in the epidemiological studies. The results show a marked gap of the prevalence rate between the age 30–44 group and the age 45–59 group in the 1983–7 survey. In the 2006 survey, however, a gap was found between the age 45–59 group and the age over 60 group. Since the residents in both groups lived in the same area, and would have been exposed to comparable amounts of Japanese cedar pollen every year for more than 20 years, significant difference between the two age groups in their prevalence rate strongly suggests that the residents who were born before the end of the World War II, i.e., 1945, were protected from the development of Japanese cedar pollinosis, as compared with the residents, who were born after the war.
Figure 6.
Estimated prevalence rate of Japanese cedar pollinosis in different ranges of age in three target periods in 1983–1987, 1996, and 2006 (From ref. 21).
Several epidemiological studies in Europe indicated that modifications of the pattern of microbial exposure of children are critical factor for the prevalence of atopic diseases (hygiene hypothesis).22) Since the life style and the microbial environment in Japan suddenly changed after the end of the war, the big difference in the prevalence rate of Japanese cedar pollinosis between certain age groups described above may well be due to the changes in the microbial exposure of children, together with the westernized life style after war.
Further studies should be conducted annually to evaluate possible changes in the upward trend of the prevalence rate in the future and possible correlations between prevalence rate of pollinosis and airborne pollen levels. The Tokyo Metropolitan Government plans to conduct such surveys in the future.
Part IV. Increase of studies on Japanese cedar pollinosis — Studies presented at meetings of the Japanese Society of Allergology
To determine the trend of studies on Japanese cedar pollinosis, I investigated the chronological change of the number of free paper presentation relevant to Japanese cedar pollinosis as a percentage of all free papers presented at the spring clinical meetings and autumn annual meetings of the Japanese Society of Allergology. The percentage of presentations on Japanese cedar pollinosis was 0.8% of all papers during the period from 1963 (when we presented “Discovery of Japanese cedar pollinosis” orally at a meeting) to 1969, while the percentage in the decades after 1970 rose to 1.8% (1970–1979), 3.1% (1980–1989), and 5.5% (1990–1999), respectively. There was a further increase to 7.5% in 2000–2006, showing an upward trend. I am interested to follow this trend in the future.
Part V. Future prospects for Japanese cedar pollinosis
Because the Japanese cedar forests in Japan consist of many trees with limited age ranges and forest management remains poor, periodical heavy Japanese cedar pollen dispersal occurring every several years is likely to persist for a while. Unfortunately, a curative treatment for pollinosis may not be developed soon. Furthermore, once a patient develops Japanese cedar pollinosis, it does not resolve at an early stage. Therefore, the number of patients with Japanese cedar pollinosis will continue to increase for many years to come.
Conclusion
Given the current circumstances of Japanese cedar pollinosis, multidisciplinary research that involves various fields of medicine and science is required, and young researchers who are interested in allergology/immunology need to participate in the studies on this disease. Professor Ishizaka and his wife identified IgE antibodies in the serum of the patients with ragweed pollinosis and elucidated IgE-antibody-mediated mechanisms of allergy. Likewise, Japanese cedar pollinosis may be a treasure-box for research on allergology and immunology. I believe that studying Japanese cedar pollinosis will provide fruitful results in the future.
Profile
Yozo Saito was born in 1932 in Tokyo, Japan. He graduated from Tokyo Medical and Dental University, Faculty of Medicine, in 1958. After one year internship, he studied at the Department of Otorhinolaryngology (Director, Prof. Horiguchi, S.) of the same Faculty. He obtained M.D. from the same Faculty by studies on “clinical and exfoliative cytological studies on the healing process of epipharyngitis” in 1964. Since he discovered Japanese cedar pollinosis in 1964, he performed clinical and palynological studies on this disease. He became Associate Professor of the same Department in 1975 and retired in 1998. He was awarded the academic prize of Palynological Society of Japan in 2000 for studies on Japanese cedar pollinosis and pollen survey in Tokyo. Since 1998, he is the medical advisor of Kamio Memorial Hospital.
His life work is the research on Japanese cedar pollinosis.
References
- 1).Bostock J. (1819) Case of a periodical affection of the eyes and chest. Med. Chir. Trans. X (part 1), 161–165 [PMC free article] [PubMed] [Google Scholar]
- 2).Blackley, C.H. (1873) Experimental researches on the causes and nature of catarrhus aestivus (hay-fever or hay-asthma), Balliere Tindall & Cox, reprinted in Dawson’s of Pall. Mall, London 1959. [Google Scholar]
- 3).Saito Y. (1968) Pollinosis in Japan. Nippon Jibiinkoka Gakkai Kaiho 71, 1036–1043(in Japanese) [PubMed] [Google Scholar]
- 4).Misawa T. (1937) Allergic diseases. J. Jpn. Soc. Int. Med. 25, 133–262(in Japanese) [Google Scholar]
- 5).Hara H.J. (1939) Hay fever among Japanese (III). Arch. Otolaryngol. 30, 525–535 [Google Scholar]
- 6).Alford R.I. (1948) Allergy in Japan. J. Allergy 19, 240–243 [DOI] [PubMed] [Google Scholar]
- 7).Durham O.C. (1961) Ragweed in Japan. JAMA 178 (1), 100 [Google Scholar]
- 8).Ueno J. (1953) Palynology and pollen disease. Kagaku no Jikken 4 (1), 23–25(in Japanese); [Google Scholar]; Ueno J. (1953) Palynology and pollen disease. Kagaku no Jikken 4 (2), 102–107(in Japanese) [Google Scholar]
- 9).Ikuse M., Ito A., Sado M. (1962) Airborne pollens. Shokubutsu Kenkyu Zasshi 37, 33–43(in Japanese) [Google Scholar]
- 10).Ishizaki, T. (1957) Pollen allergy. In Allergy (eds. Kimura, Y., Noguchi, Y. and Oshima, Y.) Kanehara & Co., Ltd., Tokyo, pp. 218–229 (in Japanese). [Google Scholar]
- 11).Araki H. (1960) Studies on pollinosis (I). Pollen Survey in Tokyo and its Neighbouing District. Jpn. J. Allergol. 9, 648–655(in Japanese with English abstract) [Google Scholar]
- 12).Araki H. (1961) Studies on pollinosis (II). Sensitization with pollens in Japan. Jpn. J. Allergol. 10, 354–370(in Japanese with English abstract) [PubMed] [Google Scholar]
- 13).Horiguchi S., Saito Y. (1964) Japanese cedar pollinosis in Nikko, Japan. Jpn. J. Allergol. 13, 16–18(in Japanese with English abstract) [PubMed] [Google Scholar]
- 14).Horiguchi S., Saito Y. (1965) Clinical observation on Japanese cedar polliosis. Nippon Jibiinkoka Gakkai Kaiho 68, 1224–1233(in Japanese) [Google Scholar]
- 15).Horiguchi S., Saito Y. (1967) Clinical observation on hay fever due to Japanese cedar pollen. Bull. Tokyo Med. Dent. Univ. 14, 141–155 [PubMed] [Google Scholar]
- 16).Ishizaki T., Koizumi K., Ikemori R., Ishiyama Y., Kushibiki E. (1987) Studies of the prevalence of Japanese cedar pollinosis among the residents in a densely cultivated area. Ann. Allergy 58, 265–270 [PubMed] [Google Scholar]
- 17).Kishikawa, R., Hirose, T. and Nishima, S. (1990) Report on the prevention and treatment of pollinosis. Ministry of Health and Welfare, pp. 43–48 (in Japanese). [Google Scholar]
- 18).Saito Y. (1991) Japanese cedar pollinosis. J. Therap. 73, 649–654(in Japanese) [Google Scholar]
- 19).Inouye S., Sakaguchi M., Mori H., Miyamura K., Ugiiye A., Sigehara S., Noguchi Y. (1986) Seroepidemiology of Sugi (Japanese Cedar) pollinosis. Igaku-no-Ayumi 138, 285–286(in Japanese) [Google Scholar]
- 20).Baba K., Nakae K. (2008) Epidemiological national survey of nasal allergy 2008 (compared with 1998) in otolaryngologists and their family members. Prog. Med. 28, 2001–2012(in Japanese) [Google Scholar]
- 21).Nishihata S., Murata T., Inoue S., Okubo K., Sahashi N., Takahashi H., Hirooka J., Hoshiyama Y., Murayama K., Mezawa A., Tokoyama T., Endo T., Saiga T., Saito Y. (2010) Prevalence of Japanese cedar pollinosis in Tokyo: a survey conducted by the Tokyo Metropolitan Government. Clin. Exp. Allergy Rev. 10, 8–11 [Google Scholar]
- 22).Strachan D.P. (1989) Hay fever, hygiene, and household size. BMJ 299, 1259–1260 [DOI] [PMC free article] [PubMed] [Google Scholar]