Abstract
Background
Despite evidence that electronic medical records (EMR) information technology innovations can enhance the quality of trauma center care, few investigations have systematically assessed United States (US) trauma center EMR capacity, particularly for screening of mental health comorbidities.
Study Design
Trauma programs at all US Level I and II trauma centers were contacted and asked to complete a survey regarding health information technology (IT) and EMR capacity.
Results
Three hundred and ninety one of 525 (74%) US Level I and II trauma centers responded to the survey. More than 90% of trauma centers report the ability to create custom patient tracking lists in their EMR. Forty-seven percent of centers were interested in automating a blood alcohol content (BAC) screening process, while only 14% report successfully using their EMR to perform this task. Marked variation was observed across trauma center sites with regard to the types of EMR systems employed as well as rates of adoption and turnover of EMR systems.
Conclusions
Most US Level I and II trauma centers have installed EMR systems, however marked heterogeneity exists with regard to EMR type, available features, and turnover. A minority of centers have leveraged their EMR for screening of mental health comorbidities among trauma inpatients. Greater attention to effective EMR use is warranted from trauma accreditation organizations.
Introduction
Each year in the United States (US), approximately 2 million Americans are admitted to trauma centers and other hospitals after incurring traumatic physical injuries.1-4 Among these injured patients, mental health and substance related disorders, including alcohol use problems and posttraumatic stress disorder (PTSD) symptoms, are very common – reaching 79% prevalence in some studies.5-9
The American College of Surgeons' Committee on Trauma (ACS/COT) is the leading US agency responsible for establishing trauma center requirements.10,11 This agency helps trauma systems put evidence into practice by periodically reviewing and revising accreditation requirements.11 Among the evidence-based interventions that improve trauma care quality and reduce readmissions after traumatic injuries is alcohol screening, which is now mandatory for ACS-verified Level I and II trauma centers. Level I trauma centers are also required to have the capacity to provide an intervention for those patients who screen positive. Although no current ACS/COT mandates exist for PTSD screening and intervention, recent evidence and advances in PTSD screening and intervention suggest that clinical practice guidelines from the College could improve outcomes for patients with this disorder.12-14
Widespread screening for mental health and substance abuse symptoms at US trauma centers would require dedicated trained personnel or integration of a new computerized screening system to existing electronic medical record (EMR) installations. Such work is a logistical challenge but may represent an opportunity for pragmatic informatics solutions that simultaneously support both patient care and the intent of the Health Information Technology for Economic and Clinical Health (HITECH) Act.15 The HITECH Act, part of the American Recovery and Reinvestment Act of 2009, allocated $25.9 billion to expand adoption of health information technology in the US. It established a certification program for EMR systems, defined how facilities and providers must use an EMR in order to demonstrate “Meaningful Use” of EMR technologies, and under the Act, facilities and providers that satisfied the Meaningful Use criteria earned incentive payments.16 Teams of trauma surgical researchers and mental health clinical investigators have begun to develop electronic medical record tools that perform population-based automated screening for alcohol, PTSD, and related comorbid conditions.9,17 Approaches to screening have ranged from aggregation of previously collected data from within the EMR such as blood alcohol concentrations,9 to the development of risk prediction tools for PTSD that draw from multiple EMR domains.17 These novel screening approaches should improve the ability of trauma centers to apply clinically effective care protocols in daily practice, but they all rely on advanced EMR technical capacity.
Previously, studies in non-trauma hospitals have systematically assessed the availability of advanced EMR capacity, and linked enhanced function with improved patient outcomes.18-21 While advanced EMR capacity has the potential to enhance trauma center screening and intervention, our literature review found limited investigations that have systematically assessed current trauma center information technology (IT) or availability of advanced EMR capacity.
The purpose of this investigation was to assess the availability of advanced EMR capacity for all US Level I and II trauma centers that is used in, or could be applied to, mental health comorbidity in trauma care. The investigation hypothesized that current trauma center EMR capacity to create systems for screening and tracking of defined trauma populations would be characterized by marked heterogeneity. We anticipated that trauma centers would vary in EMR software systems, as well as in the sophistication of information technology.
Methods
Identification and Characterization of US Level I and II Trauma Centers
This investigation was part of a larger effort to examine alcohol screening and brief intervention procedures in the wake of the ACS/COT mandate.11 All US Level I and II trauma centers were identified through a review of the American College of Surgeons' listing of verified trauma programs, the American Trauma Society's Information Exchange information system, and other web-based searches.22,23 Informational data on hospital accreditation, academic affiliation and residency training programs, and bed number were obtained from American Hospital Directory listings and through review of individual hospital web pages. These public information data sources were utilized in conjunction with hospital web-sites to identify potential trauma program survey responders. Because the survey aimed to assess both general hospital compliance with American College of Surgeons' alcohol screening and intervention mandate procedures and specific information about technology resources at trauma centers, trauma center staff - such as trauma program coordinators - were identified as primary survey contacts.22 Trauma program staff had the option of completing web-based, hard copy, or telephone interview questionnaires. Providers were reimbursed $30 after completion of the questionnaire. The University of Washington Institutional Review Board approved all study procedures prior to protocol implementation.
Development of the Trauma Center Organizational Information Technology Capacity Survey
A questionnaire was developed to assess Level I and II trauma center alcohol screening and brief intervention practices and EMR and information technology capacity (see Appendix online only). Selected items were adapted from an instrument previously developed by the investigative group to assess nationwide alcohol screening and brief intervention practices in the wake of the ACS/COT mandate.22 Additional items were developed to capture current hospital EMR and information technology capacity and practice.24 For each hospital, the survey assessed what EMR system was currently in place, and the capacity for system management of clinical documentation, nursing observations, pharmacy information, patient alerts, laboratory data, diagnostic test results, clinician orders, clinical decision support and for tracking patient-clinician team relationships. When hospitals endorsed no tracking system in place, additional items queried anticipated future changes in EMR systems/capacity. Additional items were developed to assess the global sophistication/refinement of hospital based EMR systems. These items queried whether or not the trauma center currently had the capacity to perform automated alcohol screening that aggregated patients with positive blood alcohol concentrations, and whether the respondent believed the trauma center was capable of locally developing IT applications to support trauma quality improvement, such as alcohol screening. Trauma centers were also asked to endorse the presence of barriers to IT system implementation that included inadequate funds, concerns about IT maintenance costs, lack of technical support staff, and provider/organizational resistance to the implementation of IT innovations. Trauma centers were also asked whether they experienced support from their EMR vendors surrounding IT quality improvement. Finally, because we were aware that trauma program coordinators may rely on individuals with greater IT expertise, we asked trauma centers to identify individuals with more extensive EMR knowledge and technical support capacity.
Data Analyses
We first examined the frequencies and distributions of organizational characteristics for all US Level I and level II trauma centers. We used χ2, t-tests and Fisher's exact test statistics to compare the characteristics of responding and non-responding sites. We then examined the frequencies and distributions of survey items. Generic trauma center organizational characteristics assessed included ACS verification, geographic location (region of the county and rural status), teaching status (teaching hospital status, membership in council of teaching hospitals, number of interns/residents), population served (adult, pediatric or combined), and numbers of hospital beds and injury admissions per year. We used the χ2, t-tests and Fisher's exact test statistics to compare the organizational characteristics of centers that endorsed versus did not endorse capacity indicators. We also report the demographic and clinical characteristics of trauma program survey respondents.
We described EMR characteristics and capacity of responding Level I and II trauma centers. Included in our description were the EMR system vendor, EMR characteristics, and barriers to implementation of more advanced EMR systems. Finally, we used multivariate regression models to assess associations between trauma center characteristics and advanced EMR capacity (i.e., self-assessed capacity for automated alcohol screening and real-time clinical data feeds). Organizational characteristics positively associated with IT quality indicators at the p < 0.05 level are reported. When two or more organizational characteristics were significantly associated with IT quality indicators, logistic regression with simultaneous entry of variables significant at the p < 0.05 level was used to assess for significant independent associations.
Results
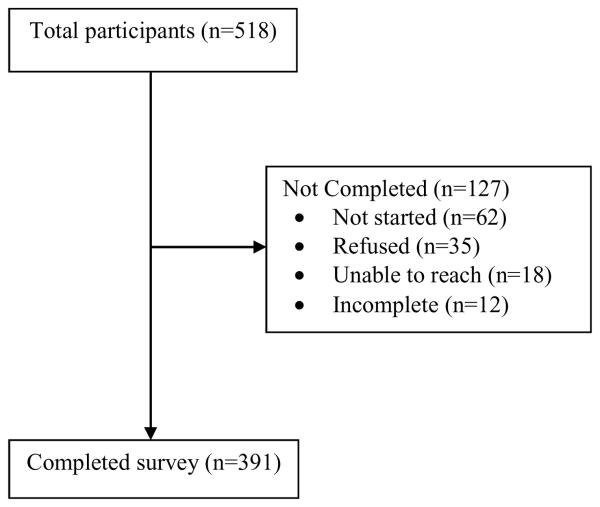
Of the 518 Level I and II trauma centers identified 391 (74%) responded and completed all surveys (Figure 1). Responding centers did not significantly differentiate from non-responding centers with regard to ACS accreditation, rural status, adult or pediatric population served, number of hospital beds, teaching hospital status and university affiliation. The only characteristics that were significantly different were: Midwest centers were more likely to be survey responders (39.9% vs 29.1%, p=0.03); and centers with greater numbers of inpatient admissions were more likely to respond (average number of admissions 22,615 vs 20,031, p=0.05). About half of responding sites were ACS accredited (Table 1). More than 80% of responding centers were from major metropolitan areas and only 17% were from rural areas. Approximately 70% of trauma centers were teaching hospitals and more than 80% had university affiliations. The majority of trauma center survey respondents described themselves as nurses (91%) and were women (82%). Respondents were 91% white, 3.6% Hispanic, 1.8% Asian, 1.5% African American, and 0.5% as American Indian.
Figure 1. Trauma center flow through protocol.
Table 1. Organizational Characteristics of United States Level I & II Trauma Centers (N = 391).
| Characteristic | n | % |
|---|---|---|
| ACS accredited | 184 | 47.1 |
| ACS accredited | 184 | 47.1 |
| Region of country | ||
| Midwest | 156 | 39.9 |
| South | 25 | 6.4 |
| Northeast | 86 | 22.0 |
| West | 90 | 23.0 |
| Southeast | 19 | 4.9 |
| Central | 15 | 3.8 |
| Rural location | 68 | 17.4 |
| Population served | ||
| Adult | 275 | 70.3 |
| Adult & pediatrics | 85 | 21.7 |
| Pediatrics | 29 | 7.4 |
| Missing | 2 | 0.5 |
| Teaching hospital | 274 | 70.1 |
| Member of council of teaching hospitals | 161 | 41.2 |
| University affiliation | 319 | 81.6 |
| Mean | SD | |
| Number of interns/residents | 173 | 219 |
| Number of hospital beds | 460 | 265 |
| Number of annual injury admissions | 1532 | 2122 |
More than 90% of trauma centers endorsed having currently available EMR custom patient tracking lists. Trauma centers demonstrated variability in the use of other common EMR features, such as computerized provider order entry and clinical decision support tools. Availability of these features ranged from 62% to 93% of trauma centers (Table 2). Among sites that lacked one or more common EMR features, the range of those planning to implement a given feature within the next 12 months was 3% to 28%.
Table 2. Trauma Center Use of Common EMR Features (N = 391).
| Feature | n | % |
|---|---|---|
| Custom patient-tracking lists | 364 | 93.1 |
| Computerized clinician documentation | 324 | 82.9 |
| Computerized nursing observations | 338 | 86.5 |
| Pharmacy information | 355 | 90.8 |
| Patient alerts | 330 | 84.4 |
| Laboratory data | 366 | 93.6 |
| Diagnostic test results | 363 | 92.8 |
| Computerized Provider Order Entry | 300 | 76.7 |
| Clinical decision support | 299 | 76.5 |
| Patient-clinician team relationship tracking | 243 | 62.2 |
Marked heterogeneity was observed with regard to the type, number, and number of years in service of trauma center EMR systems. Overall, trauma centers reported currently using 17 distinct EMR systems. The four most frequently endorsed systems were Epic (n = 94, 24.0%), Cerner (n = 69, 17.6%), McKesson (n = 44, 11.3%) and Meditech (n = 41, 10.5%). Thirty-one (7.9%) trauma centers endorsed using more than one EMR system and 21 (5.4%) centers anticipated upcoming changes or upgrades to their systems. About half (54%) of sites reported that they felt their vendors supported IT innovation and quality improvement. Only 14% of sites reported the capacity for automated blood alcohol content (BAC) screening. However 47% of sites endorsed an interest in implementing such automated screening procedures.
Forty five percent of sites endorsed having the capacity to create real-time clinical data feeds. Barriers cited by centers to real-time data feed implementation were inadequate funds (28%), concerns about IT maintenance costs (25%), lack of information technologies support staff (22%), and resistance on the part of the clinical staff (11%). In multivariate analysis, the only significant organizational factor associated with increased capacity to create an automated EMR alcohol screening process was teaching hospital status, with a relative risk of 2.19 (95% CI: 1.24-3.89). Of note, 45% of respondents could identify an individual with greater IT knowledge on site at their trauma center.
Discussion
Advanced EMR systems can be leveraged to improve application of evidence-based preventive care interventions among hospitalized patients, using computerized decision support tools to drive physician alerts.25 Some trauma centers report using custom patient tracking lists, real-time feeds of clinical data, and automated BAC screening as examples of leveraging their EMR to improve trauma patient screening as part of high-quality trauma care. The results of the current investigation suggest that despite advanced EMR capacity at many trauma center sites, there is marked heterogeneity in innovative applications in their EMR systems. An important drawback to EMR implementation today is that the underlying data models are different among different hospital EMR systems, even among systems from the same vendor. This heterogeneity sharply restricts both seamless connection to existing patient data systems, as well as implementation of innovative clinical systems that rely on EMR data.26
There are many factors about advanced EMR systems that limit their widespread use for trauma care improvement: (1) many published EMR benefits are described by only a handful of innovative institutions, and there are no studies that prove the results are generalizable or are provided by commercially available EMR systems;27 (2) there is substantial variability in the definition of an EMR, the amount of patient data entered to a given institution's EMR, and the installation of EMR features to drive electronic clinical decision support algorithms – a finding confirmed by our analysis;28,29 (3) intense competition among EMR vendors has led to substantial heterogeneity in types and capabilities of EMR systems across the US – also confirmed by our analysis – and this prevents development and distribution of standardized, proven screening and reminder tools for trauma patients.30 Therefore, in order to understand whether the recent intense investment in EMR technology spurred by the HITECH Act has produced functional EMR systems capable of detecting trauma patients suitable for interventions to treat alcohol abuse, PTSD, and other conditions, we first need to understand the capacity of US trauma centers to install or build such tools.
As has been seen in other clinical arenas, making evidence-based interventions available to EMR owners is insufficient to drive advanced EMR utilization. While some technologists believe that clinically advantageous innovations will sell themselves, that benefits in care because of a new idea will be widely utilized by potential adopters, and that the innovation will therefore diffuse rapidly, this is rarely the case. Most innovations, such as protocol-driven improvements in clinical care, in fact, diffuse at a disappointingly slow rate.31 Innovations that have only a software component, such as EMR-driven care processes, have a relatively lower degree of observability and thus a slower rate of adoption.31 Successful adoption requires a connection between an institution that has experience with a new innovation and another institution capable of adopting, but it does not yet have experience with the innovation. In the case of EMR-based screening tools for improved trauma care, the specific technical capabilities that make another institution “capable of adopting” often requires investment of time and money by that institution. Communicating these innovations, demonstrating their benefits, and ensuring development of the capability to adopt them will likely require policy-level intervention by the College as a driving stimulus. However, without aligning the innovations to other desired outcomes, such as reduction in recidivism and rate of readmission, the opinion leaders in the community that could adopt the innovation may not be able or ready to devote resources to such an undertaking, even if mandatory. Therefore, the benefits of the intervention and improvement in EMR must be proven and shown to be generalizable to the larger community. The American College of Surgeons, through its Committees on Trauma and Health Information Technology, could extend its leadership role in this area. Examples include more study into the impact on trauma outcomes of interventions for substance abuse, PTSD and depression. Also, support for the investigation of EMR tools and processes that can be integrated to the clinical workflow across trauma centers to improve care of the injured patient, to track interventions for substance abuse, PTSD, depression, and other comorbid conditions associated with physical trauma. Documentation of benefit and confirmation of cross utilization potential among trauma centers will be critical to further advances in this field.
There are a number of important limitations in considering the results of this investigation. First, trauma program coordinators may not have been the most knowledgeable trauma center providers with regard to EMR capacity (although fewer than half could identify someone who was more knowledgeable). Second, survey items did not provide an in-depth understanding of what was contained within each trauma center EMR. Finally, the survey may have only begun to capture the rapidly changing EMR context at trauma centers, and therefore may underestimate EMR evolution and turnover.
Beyond these considerations, this study contributes to an evolving literature on EMR capacity at US trauma centers. The investigation documents that most US Level I and II trauma centers have installed EMR systems, however marked heterogeneity exists with regard to EMR type and vendor turnover. This is of particular interest because of increasing reliance upon advanced EMR systems for powering institutional understanding of patient population-level statistics, care quality metrics, and assurance of execution of best-practices in the delivery of high quality trauma care. Standardized third-party systems do not yet exist for providing these kinds of data in the effort to improve care quality delivery, reduce readmissions, and ensure delivery of evidence-based processes of trauma care. Ultimately, US trauma care systems may be capable of real-time, workflow-integrated automated screening, intervention and screening procedures.21
Précis.
Few investigations have assessed US trauma center EMR capacity; 391 of 525 (74%) of US Level I-II trauma centers completed a health information technology survey. Marked variation was observed regarding EMR type, available features, and turnover. A minority of trauma centers have leveraged their EMR for screening of mental health comorbidities.
Acknowledgments
Supported by a grant from the NIH.
Abbreviations
- EMR
electronic medical records
- US
United States
- IT
information technology
- PTSD
posttraumatic stress disorder
- ACS/COT
American College of Surgeons' Committee on Trauma
- HITECH
Health Information Technology for Economic and Clinical Health
- BAC
Blood Alcohol Content
Appendix. EMR characteristics section of the Trauma Program Coordinator Survey
Managing patient information. Most US hospitals have, or are implementing, Electronic Medical Records systems. These systems can be built one piece at a time. The following questions ask what kinds of information are managed in an Electronic Medical Records system at your trauma center at this time.
22. Does your trauma center have an electronic system for tracking:
22a. Admit/Discharge/Transfer information, such as dates of admission and discharge, demographic patient characteristics like age and gender, admitting medical service and unit?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22b. Clinician documentation, such as inpatient clinician notes, consult notes, procedure reports, and discharge summaries?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22c. Nursing observations, such as vital signs, shift summaries, patient assessments and therapies?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22d. Pharmacy information, such as medication allergies, medication orders, and medication administration records?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22e. Patient alerts, such as advance directives, care plan alerts, and allergy alerts?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22f. Laboratory data, such as serum chemistry values, toxicology reports, and microbiology results?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22g. Diagnostic test results, such as radiology reports, vascular testing reports, and echocardiogram reports?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22h. Clinician orders, such as consult requests, medication orders, therapy orders, and nursing orders?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22i. Clinical decision support, such as clinical reminders, drug interaction alerts, clinical uidelines, and drug dose-range checking?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
22j. Patient-clinician team relationships, such as a medical team electronic list system that provides information during rounds and supports patient care handovers?
□ Yes □ No (if no, are there plans to implement in the next 6 to 12 months? □ Yes □ No)
Some trauma centers have begun to use electronic systems to conduct screening procedures and quality improvement. For example, after blood alcohol concentrations are drawn an automated screening program would generate a computerized report listing all traumatically injured inpatients who were blood alcohol positive. The following questions ask about your trauma center's experience with automated systems to support such procedures.
23. Does your trauma center currently use an automated alcohol screening program that generates a computerized list of all trauma patients with positive blood alcohol tests?
∎ Yes (If yes skip to 24) ∎ No
23a. Would such an automated screening procedure be of interest to you/your trauma center?
∎ Yes ∎ No
24. Does your trauma center have the capacity to use real-time clinical data feeds for local development of electronic quality improvement tools, such as the alcohol screening program above?
∎ Yes (if yes, skip to 25) ∎ No
If no, Which of the following are barriers to implementing systems at your institution that use real-time clinical data feeds for local/electronic quality improvement?
24a. Inadequate funds to purchase required information technologies
∎ Yes ∎ No
24b. Concerns about information technologies maintenance costs
∎ Yes ∎ No
24c. Lack of adequate information technologies support staff
∎ Yes ∎ No
24d. Resistance on the part of clinical staff to use new information technologies
∎ Yes ∎ No
25. If you have an Electronic Medical Records system, what company made it?
Open ended response:
25a. Do you believe the manufacturer of your institution's electronic medical records system is supportive toward building local tools for patient screening and quality improvement?
∎ Yes ∎ No ∎ We don't have an electronic medical record system
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
References
- 1.McCaig LF, Nawar EW. National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Advance Data. 2006 Jun 23;(372):1–29. [PubMed] [Google Scholar]
- 2.Bonnie RJ, Fulco CE, Liverman CT, editors. Reducing the burden of injury: Advancing prevention and treatment. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention. CDC Injury Fact Book. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 4.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. Jama. 2003 Mar 26;289(12):1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 5.Soderstrom CA, Smith GS, Dischinger PC, et al. Psychoactive substance use disorders among seriously injured trauma center patients. Jama. 1997;277(22):1769–1774. [PubMed] [Google Scholar]
- 6.Ramchand R, Marshall GN, Schell TL, et al. Alcohol abuse and illegal drug use among Los Angeles County trauma patients: Prevalence and evaluation of single item screener. J Trauma. 2009 May;66(5):1461–1467. doi: 10.1097/TA.0b013e318184821d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih RA, Schell TL, Hambarsoomian K, Belzberg H, Marshall GN. Prevalence of posttraumatic stress disorder and major depression after trauma center hospitalization. J Trauma. 2010 Dec;69(6):1560–1566. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zatzick D, Rivara FP, Nathens AB, et al. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol Med. 2007 Oct;37(10):1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- 9.Zatzick D, Donovan D, Dunn C, et al. Substance use and PTSD in trauma center patients receiving mandated alcohol SBI. Journal of substance abuse treatment. 2012;43(4):410–417. doi: 10.1016/j.jsat.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shafi S, Nathens AB, Cryer HG, et al. The Trauma Quality Improvement Program of the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2009;209(4):521–530. doi: 10.1016/j.jamcollsurg.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 11.American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient: 2006. Chicago: American College of Surgeons Committee on Trauma; 2006. [Google Scholar]
- 12.Coimbra R. Posttraumatic stress disorder (PTSD) screening and early intervention after physical injury: are we there yet? Ann Surg. 2013 Mar;257(3):400–402. doi: 10.1097/SLA.0b013e31828352c2. [DOI] [PubMed] [Google Scholar]
- 13.Zatzick D, Jurkovich G, Rivara FP, et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013;257(3):390–399. doi: 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zatzick D, Jurkovich G, Rivara F, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after injury hospitalization. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 15.Medicare and Medicaid programs; electronic health record incentive program. Final rule. Fed Regist. 2010 Jul 28;75(144):44313–44588. [PubMed] [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. Medicare and medicaid EHR incentive program. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html.
- 17.Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry. 2013 Sep-Oct;35(5):485–491. doi: 10.1016/j.genhosppsych.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menachemi N, Chukmaitov A, Saunders C, Brooks RG. Hospital quality of care: does information technology matter? The relationship between information technology adoption and quality of care. Health Care Manage Rev. 2008 Jan-Mar;33(1):51–59. doi: 10.1097/01.HMR.0000304497.89684.36. [DOI] [PubMed] [Google Scholar]
- 19.Frimpong JA, Jackson BE, Stewart LM, Singh KP, Rivers PA, Bae S. Health information technology capacity at federally qualified health centers: a mechanism for improving quality of care. BMC Health Serv Res. 2013;13:35. doi: 10.1186/1472-6963-13-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med. 2009 Jan 26;169(2):108–114. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 21.Richesson RL, Hammond WE, Nahm M, et al. Electronic health records based phenotyping in next-generation clinical trials: a perspective from the NIH Health Care Systems Collaboratory. J Am Med Inform Assoc. 2013 Aug 16; doi: 10.1136/amiajnl-2013-001926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Terrell F, Zatzick DF, Jurkovich GJ, et al. Nationwide survey of alcohol screening and brief intervention practices at US Level I trauma centers. J Am Coll Surg. 2008 Nov;207(5):630–638. doi: 10.1016/j.jamcollsurg.2008.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zatzick D, Rivara F, Jurkovich G, et al. Enhancing the population impact of collaborative care interventions: Mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. Gen Hosp Psychiatry. 2011 Mar-Apr;33(2):123–134. doi: 10.1016/j.genhosppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. New England Journal of Medicine. 2009;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 25.Dexter PR, Perkins S, Overhage JM, Maharry K, Kohler RB, McDonald CJ. A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001 Sep 27;345(13):965–970. doi: 10.1056/NEJMsa010181. [DOI] [PubMed] [Google Scholar]
- 26.Klann JG, McCoy AB, Wright A, Wattanasin N, Sittig DF, Murphy SN. Health care transformation through collaboration on open-source informatics projects: integrating a medical applications platform, research data repository, and patient summarization. Interact J Med Res. 2013;2(1):e11. doi: 10.2196/ijmr.2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evid Rep Technol Assess (Full Rep) 2006 Apr;(132):1–71. doi: 10.23970/ahrqepcerta132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008 May;77(5):291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Kellermann AL, Jones SS. Health information technology: authors' reply. Health Aff (Millwood) 2013 Mar;32(3):629. doi: 10.1377/hlthaff.2013.0092. [DOI] [PubMed] [Google Scholar]
- 30.Jha AK, DesRoches CM, Kralovec PD, Joshi MS. A progress report on electronic health records in U.S. hospitals. Health Aff (Millwood) 2010 Oct;29(10):1951–1957. doi: 10.1377/hlthaff.2010.0502. [DOI] [PubMed] [Google Scholar]
- 31.Rogers EM. Diffusion of innovations. 4th. New York: The Free Press; 1995. [Google Scholar]