Abstract
Background:
Immunization against childhood diseases is one of the most important ways of preventing childhood morbidity and mortality.
Aims:
The objective of this study is to review the dropout rates of immunization of children in a health center using a single dose of diphtheria-pertussis-tetanus (DPT1) and three doses of diphtheria-pertussis-tetanus (DPT3) vaccine.
Subjects and Methods:
This is a cross sectional study where immunization dropout rate of children less than 1 year in a health center was ascertained. Data was analyzed by Statistical Package for the Social Sciences version 17 (Chicago, IL, USA). Data presentation was in the form of tables and charts. The P values and confidence intervals were calculated using Chi-square. The mean and ranges of all the variables were calculated. The level of significance was set at P ≤ 0.05.
Results:
Out of 972 children who are within 1 year, 63% (613/972) were immunized for DPT3 while 63.7% (619/972) were immunized for DPT1 with an overall dropout rates and percentage of 6 and 1% (6/613) respectively. Immunization coverage for 2012 was also stratified into intervals of 4 months: From January to April 2012, 168 children received DPT1 while 166 received DPT3. Between May and August 2012, 222 children received DPT1 while 226 received DPT3. The last 3rd of the year showed that 223 children received DPT1 while 227 received DPT3.
Conclusions:
Though the total immunization coverage for DPT in this rural health center is poor, they have a very low dropout rate.
Keywords: Coverage, Health center, Immunization, Single dose of diphtheria-pertussis-tetanus, Three doses of diphtheria-pertussis-tetanus
Introduction
Immunization of children against the killer diseases has proven effective in reducing the morbidity and mortality from those diseases. For this reason, World Health Organization (WHO) recommends that all children receive one dose of bacille Calmette-Guérin vaccine, three doses of diphtheria-tetanus-pertussis vaccine (DTP), three doses of either oral polio vaccine or inactivated polio vaccine, three doses of hepatitis B vaccine and one dose of a measles virus-containing vaccine, either anti-measles alone or in combination with other antigens.[1,2,3,4] It also recommends three doses of vaccine against infection with Haemophilus influenza type B.[5] To boost immunity at older ages, additional immunizations are recommended for healthcare workers, travellers, high-risk groups and people in areas where the risk of specific vaccine-preventable diseases is high.[1]
In Nigeria, who has a population of approximately 140 million, vaccine preventable diseases account for approximately 22% of child deaths in the country; amounting to over 200,000 deaths/year.[6] The expanded program on immunization (EPI), responsible for routinely delivering immunization, started in the late 1970s. In 1990, reported three doses of diphtheria-pertussis-tetanus (DPT3) coverage in infants (<12 months of age) reached an estimated 56%.[6] During the years following the global Universal Childhood Immunization efforts that culminated in 1990, immunization coverage rates in Nigeria declined significantly. Preliminary results of a 2006 national coverage survey reported 36% DPT3 coverage and only 18% of children fully immunized (aged 12-23 months at survey time, using the card and recall).[6] The survey results revealed significant differences across zones ranging from 0% to 40% of fully immunized children.
It is gratifying to note that the Government of Nigeria has recently accelerated efforts to revive immunization services. EPI officials developed a blue print with a multi-year plan including activities for improving routine immunization coverage.[6] They adapted the global Reaching Every District strategy into a Reaching Every Ward approach which is in the process of being implemented across the 37 states. Moreover, in April 2006, the National Program on Immunization developed an approach of integrating other antigens and child survival interventions with the polio eradication campaigns.[6]
Routine immunization against DPT, measles, polio and tuberculosis is proven to be one of the most cost-effective interventions for reducing childhood illness and mortality, especially with the addition of other vaccines such as yellow fever in endemic areas and tetanus toxoid (injections for the pregnant women.[7] Not withstanding national coverage in Nigeria for full immunization is less than 13%, one of the lowest rates in the world, even lower than many countries in conflict, such as Democratic Republic Of Congo DRC. Some states in Northern Nigeria have coverage rates below 1% and the average for the whole North West Zone is just 4%. These coverage figures are much worse than in the neighboring countries of Benin, Niger, Chad and Cameroon.[7]
WHO has used a variety of coverage survey data for identifying firm points for 1993, 1998, 1999 and 2002.[8] It was noted that between the Demographic and Health Surveys for 1999 and 2003, the percentage of children aged between 12 and 23 months who received at least one dose of the traditional vaccines by their first birthday rose from 60.9% to 69.4%, indicating that access and uptake had improved.[9] Yet the percentage fully immunized with all doses before 12 months of age fell from 14.3% in 1999 to 11.3% in 2003 and dropout between first and third dose of DPT increased from 45.7% to 48.1%, indicating growing problems with the continuity of immunization services.[9]
Estimated global DTP3 coverage among children aged <12 months in 2011 was 83%, ranging from 71% in the African Region to 96% in the Western Pacific Region and representing 106.8 million vaccinated children.[10] During 2011, 130 (67%) countries achieved ≥90% national DTP3 coverage and 46 (24%) achieved the global immunization vision and strategy goal of ≥80% DTP3 coverage in every district or equivalent administrative unit. DTP3 coverage was 80-89% in 32 (17%) countries, 70-79% in 13 (7%) countries and <70% in 19 (10%) countries.[10]
Among the 22.4 million children's who did not receive three DTP doses during the 1st year of life, 11.8 million (53%) lived in three countries, India (32%), Nigeria (14%) and Indonesia (7%) and 16.2 million (72%) lived in 10 countries.[11] Nearly 14 million (62%) of these children did not receive the first dose of DTP, whereas 8.4 million (38%) started, but did not complete the three dose DTP series. In 2011, nearly 107 million infants (83%) world-wide received at least three doses of DTP vaccine; however, approximately 22.4 million failed to receive three doses, leaving large numbers of children susceptible to vaccine-preventable diseases and death.[11]
Dropout rate is assessed by the number of DPT1 and DPT3 that was given to the child over a year. The study is aimed at determining the coverage rate of immunization services in a health center over a year using DPT1 and DPT3. This will go a long way to determine the impact of these services in rural areas. In addition, this study would also help in establishing baseline values of DPT coverage rates in this locale and will assist the health worker and government to improve the immunization service in the area if the coverage rate is low.
Besides, this would also form a database upon which further studies can be carried out.
Subjects and Methods
Study area
The study was carried out in a health center in a remote village over a 1 year period. Ihe is a town in Awgu Local Government Area in Enugu State of Nigeria. It has a population of 24,431 people according to National Population census.[8] Enugu state is in the South East geographic zone of Nigeria. It lies in the rainforest zone with two major seasons (rainy and dry) and a temperature of about 28-33°C. It has a population of 3.5 million people according to the National population census.[8]
Study procedure
Using the immunization monitoring chart provided by the National Immunization Program, immunization dropout rates were evaluated among children who are less than 1 year old in Ihe, Awgu local government area over a year period. Children who moved out of the area or who went elsewhere for health-care service were excluded.
The health center had data where list of eligible children who were vaccinated in the local health center were recorded. Drop our rates were calculated using DPT1-DPT3 while the dropout percentage was calculated using DPT1-DPT2/DPT3.
Ethical consideration and consent
Informed consent was sought and obtained from the chief community health officer of Ihe health center, Owelle court, Awgu. Ethical clearance was also obtained from from the chiefcommunity health officer of Ihe health center, Owelle court, Awgu.
Data was analyzed by statistical package for the social sciences version 17 (Chicago Il, USA). Data presentation was in the form of tables and charts. The P values and confidence intervals were calculated using Chi-square. An initial frequency count of all variables was done and represented in tables. The mean and ranges of all the variables were calculated. The level of significance was set at P ≤ 0.05.
Results
Out of 972 children who are within 1 year who are residents in this health center in 2012, 63% (613/972) were immunized for DPT3 while 63.7% (619/972) were immunized for DPT1. This gives an overall dropout rates and percentage of 6 and 1% (6/613) respectively.
Immunization coverage for 2012 was also stratified into intervals of 4 months: From January to April 2012, 168 children received DPT1 while 166 received DPT3. This gives a dropout rate and percent of 2 and 0.6% (2/166) respectively.
Between May and August 2012, 222 children received DPT1 while 226 received DPT3. Dropout rate and percentage of −4 and −1.8% (−4/222) were obtained respectively.
The last third of the year (September to December 2012) showed that 223 children received DPT1 while 227 received DPT3. This gave dropout rate and percentage of −4 and −1.8% (−4/223) were obtained respectively.
The average number of children immunized for DPT1 and DPT3 per month is 61.3 and 60.7 respectively. When immunization of DPT1 and DPT 3 were compared at 4 months intervals, the dropout rate is not statistically significant (P = 0.75 and 95% confidence interval of 63 (1.86%) [Table 1].
Table 1.
Immunization coverage using DPT
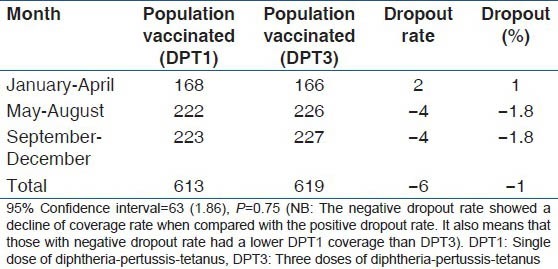
Figure 1 shows a step lather increase in immunization coverage (using DPT) from January to December 2012.
Figure 1.
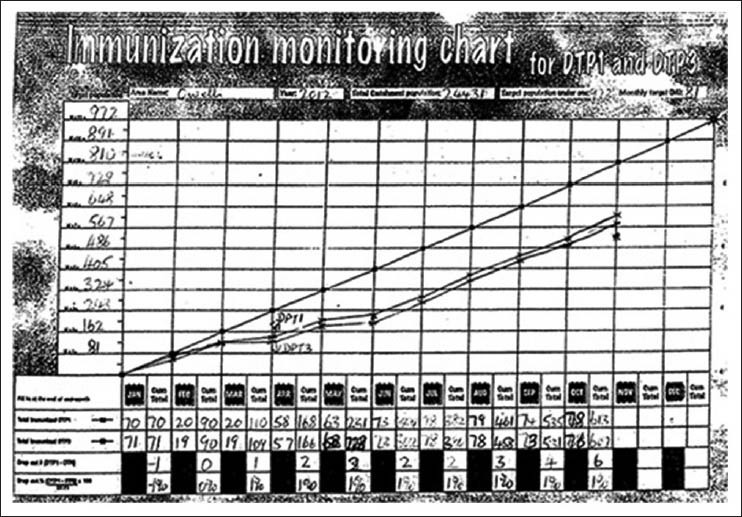
A graphical representation of immunization coverage rate over 1 year period
Discussion
Immunization coverage rate for DPT3 is the proportion of surviving infants who received three doses of DPT (diphtheria, pertussis and tetanus) vaccine before their first birthday. This study clearly depicts the level of immunization coverage in a rural setting in Nigeria. The 63% coverage obtained in this study is less than that (70%) obtained in a particular center in Nigeria.[3,12] The reason for this low value could probably be that the health facility is located in a rural area. Obstacles ranging from bad road conditions, concentration of health workers in cities and lack of extension of government immunization policies in the rural areas could explain this low coverage rates.
Painfully, the low values obtained in this study is even higher than that in two hospitals in northern Nigeria where coverage rates of 32% and 35% were obtained respectively.[9,13]
Reasons adduced for this low value varies from non-acceptance of immunization in the Northern area because of religio-cultural beliefs. Other reasons for low coverage here could be resistance from parents. It was revealed that when parents resist vaccination, it is because they want to protect their children from harm.[14,15] In 2003, political and religious leaders in three Northern Nigerian states boycotted a WHO polio vaccination campaign, claiming that the vaccine can caused sterility and acquired immunodeficiency syndrome.[16]
It is noted that in 1980, fewer than 10% of the world's children lived in 20 of the 167 countries with DTP3 coverage levels greater than 80%; 84% of the world's children lived in countries where coverage was less than 50%. By 1990, 108 countries (43% of all children) had DTP3 coverage levels greater than 80% and fewer than 10% of children lived in countries with under 50% coverage.
Immunization coverage levels can “mask” some rural areas where coverage is much lower as depicted in our study. For instance, in 2006, despite the 80% world DTP3 coverage; approximately 26.3 million children who reached their first birthday still did not receive DTP3 and 16.2 million (62%) of them lived in rural China, India, Indonesia or Nigeria.[17]
The dropout rates obtained in this study are very minimal. These low levels can be explained. It is seen that these villagers live in clans and those who came for immunization are well communicated to, on the need to comply with subsequent immunization schedules. They use jingles, town crier, village square meetings to achieve these aims. As part of a complete immunization program, communication efforts should be totally linked to and complement the other immunization technical components, including the provision and quality of services, health worker capacity-building and skills and disease reporting and surveillance.[18] Communication activities that are sufficiently planned, funded and integrated with service delivery can help facilitate immunization program.[19,20] It has been documented that dropout rates are higher in studies carried in three states in Nigeria where rates higher than 10% were obtained.[3]
The WHO standard is that a dropout rate greater than 10% is unacceptable.[21,22] In none of these two hospitals from Northern states for which data are presented were dropout rates within that allowable maximum.[18] Indeed, an inspection of dropout rates from DPT1 to DPT3 is very vital to indicate coverage and compliance in a given area.[3]
Immunization coverage for children, in this study, improved in the last half of the year when compared to the first half. This could be due to the fact that the first half of the year is usually a farming season and as such a parents and care givers of these children will prefer giving more time for farm work to visit the health facility.
Finally, it is important to note that there is no significant difference between dropout rates for 2012 and part of 2013. This is a clarion call for the government to intensify efforts at reducing the dropout rates to the barest minimum. The dropout rate for both years however, is significant when compared with the 10% WHO standard.
Although childhood vaccination prevents 2 million deaths/year world-wide and is widely considered to be “overwhelmingly good” by the scientific community.[1] However, about 2.5 million deaths/year continue to be caused by vaccine-preventable diseases, mainly in Africa and Asia among children less than 5 years old.[1] Vaccination coverage is dwindling in many developing countries and even where good coverage has been attained, reaching children not yet vaccinated has proved difficult. There is an urgent need to increase vaccination coverage. It is also important to encourage parents to have their children vaccinated.
Conclusion
Though the total immunization coverage in this rural health center is poor, they have a very low dropout rate.
Limitation
Immunization coverage rates in all health centers in Awgu Local Government Area were not ascertained due to lack of good road network. This would have made this work better.
Recommendation
This study goes to portend the need for the government to intensify effort to improve immunization coverage, especially in rural areas.
Acknowledgments
We acknowledge the Almighty God whose assistance and ideas through the course of this work were priceless. We are also grateful to the community health extension health workers and district officers in Ihe health center whose help in this study is priceless.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Burton A, Monasch R, Lautenbach B, Gacic-Dobo M, Neill M, Karimov R, et al. WHO and UNICEF estimates of national infant immunization coverage: Methods and processes. Bull World Health Organ. 2009;87:535–41. doi: 10.2471/BLT.08.053819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geneva: World Health Organization; 2005. [Last accessed on 2013 Aug 12]. Global Immunization Vision and Strategy 2006-2015. Available from: http://whqlibdocwhoint/hq/2005/WHO_IVB_05.05.pdf . [Google Scholar]
- 3.WHO. Geneva: World Health Organization; 2005. [Last accessed on 2013 Aug 12]. Vaccine Introduction Guidelines: Adding a Vaccine to a National Immunization Program, Decision and Implementation. WHO/IVB/0518. Available from: http://whqlibdoc.who.int/hq/2005/WHO_IVB_0518.pdf . [Google Scholar]
- 4.Griffiths UK, Wolfson LJ, Quddus A, Younus M, Hafiz RA. Incremental cost-effectiveness of supplementary immunization activities to prevent neonatal tetanus in Pakistan. Bull World Health Organ. 2004;82:643–51. [PMC free article] [PubMed] [Google Scholar]
- 5.WHO-UNICEF. Geneva: WHO; 2005. [Last accessed on 2014 July 07]. Global immunization vision and strategy: Strategic framework for 2006-2015. Available at http://www.who.int/vaccines/GIVS/ [Google Scholar]
- 6.Keja K, Chan C, Hayden G, Henderson RH. Expanded programme on immunization. World Health Statistics. 1988;41:59–63. [PubMed] [Google Scholar]
- 7.WHO and UNICEF estimates of national infant immunization coverage. [Last assesed on 2014 July 07]. Obtainable from http://www.who.int/bulletin/volumes/87/7/08-053819/en/
- 8.World Health Organization, UNICEF. Geneva, Switzerland: World Health Organization; 2005. [Last accessed on 2013 Aug 7]. Global Immunization Vision and Strategy 2006-2015. Available from: http://www.who.int/vaccines-documents/docspdf05/givs_final_en.pdf . [Google Scholar]
- 9.Lagos: BASICS II/USAID; 2003. BASICS II/Nigeria. Report of the Integrated Child Health Cluster Survey (ICHCS) [Google Scholar]
- 10.World Health Organization. Geneva, Switzerland: World Health Organization; 2005. [Last accessed on 2013 Jun 12]. United Nations Children's Fund. Global Immunization Vision and Strategy 2006-2015. Available from: http://www.who.int/vaccines-documents/docspdf05/givs_final_en.pdf . [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC). Global routine vaccination coverage, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1520–2. [PubMed] [Google Scholar]
- 12.National population commission 2006 provisional census figures. Census News. 31:14. [Google Scholar]
- 13.Chizoba W, Cecily S, Muyi A, Gbolahan O, Tope O, Muhammad AP, et al. Landscape analysis of routine immunization in Nigeria. International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. 2012. [Last accessed on 2013 Aug 07]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21653952 .
- 14.Nichter M. Vaccination in South Asia: False expectations and commanding metaphors. In: Coreil J, editor. Anthropology and Primary Health Care. Oxford: Westview Press; 1990. pp. 196–221. [Google Scholar]
- 15.Streefland PH. Public doubts about vaccination safety and resistance against vaccination. Health Policy. 2001;55:159–72. doi: 10.1016/s0168-8510(00)00132-9. [DOI] [PubMed] [Google Scholar]
- 16.Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4:73. doi: 10.1371/journal.pmed.0040073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NewYork, NY: UNICEF; 2008. [Last accessed on 2013 Aug 7]. State of the World's Children 2007: Women and Children, The Double Divide of Gender Equality. Available from: http://www.unicef.org/sowc07/docs/sowc07.pdf . [Google Scholar]
- 18.Seattle: CVP, PATH; 2001. [Last accessed on 2013 Aug 12]. Children's Vaccine Program at the Program for Appropriate Technology in Health. Advocacy for Immunization: How to Generate and Maintain Support for Vaccination Programs. Available from: http://rho.org.whsites.net/files/Vaccine_24_S3_ch25.pdf . [Google Scholar]
- 19.Communication Handbook for Polio Eradication and Routine EPI. New York: UNICEF; 2000. United Nations Children's Fund. World Health Organization. Collaboration with polio partners and ministry of health representatives. [Google Scholar]
- 20.World Health Organization. Immunization coverage cluster survey reference manual. [Last accessed on 2013 Jun 12]. Available from: http://www.who.int/immunization_monitoring/routine/immunization_coverage/en/index2.html .
- 21.World Health Organization. Geneva: WHO; 2002. United Nations Children's Fund, United States Agency for International Development (BASICS and CHANGE projects). Communication for Polio Eradication and Routine Immunization: Checklists and Easy Reference Guides. [Google Scholar]
- 22.World Health Organization: The EPI Coverage Survey. Training for Mid-level Managers WHO. 2008 [Google Scholar]


