Abstract
To evaluate the importance of achieving a CCyR for CML patients failing imatinib and treated with 2nd generation TKI’s, we studied the effect of CCyR on OS in 123 CP CML patients failing frontline imatinib treatment. We found that achieving CCyR at 3 months is the only predictive factor of good outcomes (EFS and OS).
Background
We assessed whether the achievement of a 3-month complete cytogenetic response (CCyR) in 123 patients with chronic myeloid leukemia (CML) in the chronic phase, which was treated with second-generation tyrosine kinase inhibitors (2nd-TKI) after imatinib failure could predict for survival.
Patients and Methods
In a multivariate analysis, the lack of a 3-month CCyR to 2nd-TKI therapy was selected as the only independent factor associated with poor event-free survival (hazard ratio [HR] 4.5; P < .001) and overall survival (5.4; P = .03).
Results
The 3-year event-free survival and overall survival rates were 74% and 43%, respectively, for patients with 3-month CCyR, and were 98% and 79%, respectively, for patients without 3-month CCyR. In a multivariate analysis, high hemoglobin level, previous major cytogenetic response to imatinib therapy, and ≤90% Philadelphia-positive metaphases were associated with the achievement of a 3-month CCyR.
Conclusion
The achievement of a 3-month CCyR is the only predictor of outcome in patients treated with 2nd-TKI therapy after imatinib failure. Patients with <3-month CCyR may not obtain long-term benefit and should be followed-up closely.
Keywords: Chronic myeloid leukemia, Cytogenetic response, Tyrosine kinase inhibitor, Prognosis
Introduction
The introduction of the tyrosine kinase inhibitors (TKI) has revolutionized the outcome of chronic myeloid leukemia (CML).1 Imatinib therapy induced high rates of complete cytogenetic and major molecular responses, and improved survival in CML.2–6 Despite the benefit of imatinib over prior treatments, some patients may develop resistance,7 with a reported annual resistance rate of 2% to 4% in newly diagnosed patients in the chronic phase (CP), and the incidence decreases over time.8 Second-generation TKIs (2nd-TKI) dasatinib and nilotinib are approved for the treatment of such patients, which induces a complete hematologic response (CHR) in 77% to 91% and a complete cytogenetic response (CCyR) in 41% to 53%.9,10
The achievement of a CCyR is now generally accepted as a surrogate marker for survival. The association between early cytogenetic response and long-term survival has been clearly demonstrated for patients treated with interferon or TKI.5,11,12 We recently showed that early achievement of CCyR by 3 to 6 months of therapy with 2nd-TKI used as initial therapy correlated with significant improvement of outcome.13 The aim of this study was to assess the impact of an early CCyR on survival of patients with CML-CP who were treated with 2nd-TKI after imatinib failure.
Patients and Methods
A total of 123 consecutive patients with CML-CP after imatinib failure were treated with 2nd-TKIs in phase II pivotal trials. Entry criteria were similar for both trials. Seventy-eight (63%) patients were treated with dasatinib and 45 (37%) with nilotinib. CML-CP was as previously defined.14 The definitions of imatinib failure have been previously described15,16 and generally are aligned with those later proposed by the European LeukemiaNet.17 The patients were treated by using institutional review board–approved protocols. Informed consent was obtained in accordance with the Declaration of Helsinki.
Event-free survival (EFS) was measured from the start of treatment to the date of any of the following events while on therapy: death from any cause, loss of CHR or CCyR, discontinuation of therapy for toxicity or lack of efficacy as per the European LeukemiaNet criteria, or progression to accelerated or blast phases. Overall survival (OS) was measured from the date of the start of therapy until death. Survival probabilities were estimated by the Kaplan-Meier method and were compared by using the log-rank test. Differences among variables were evaluated by the χ2 test and the Mann-Whitney U test for categorical and continuous variables, respectively. Univariate and multivariate analyses were performed to identify potential prognostic factors associated with response and survival. These factors included age; performance status; the presence of splenomegaly, anemia, thrombocytopenia, and hyperleukocytosis; the percentage of basophils and blasts in the blood and marrow; the presence of clonal evolution; the mutation status; the presence of a CHR; and the percentage of Philadelphia (Ph) positive metaphases at the start of 2nd-TKI therapy, in addition to the CML duration and the cytogenetic response to previous imatinib therapy. The 3-month cytogenetic response to 2nd-TKIs was also included. All but 3 patients were not evaluable for 3-month cytogenetic response, and they were removed from the total denominator. Multivariate analysis of response used a logistic regression model, and survival analysis used the Cox proportional hazard model.18–20
Results
Baseline patient characteristics for the 123 patients treated were as follows: median age of 56 years (range, 21–83 years) and median duration of CP (CML diagnosis to the start of 2nd-TKI therapy) of 67 months (range, 2–268 months). The best response to imatinib was CHR only in 30 patients (24%), and cytogenetic response in 77 (63%) patients: 34 (28%) patients complete, 21 (17%) patients partial, 22 (18%) patients minor. Among the others, 2 (2%) patients were refractory to imatinib, 6 (5%) had an unknown response, and 8 (7%) were intolerant.
At the start of 2nd-TKI therapy, 84 (68%) patients were not in CHR: 23% had clonal evolution, and 70% had >90% Ph-positive metaphases. Kinase domain sequencing was performed before the start of therapy in 80 (65%) patients. Mutations were detected in 53 (43%) of these patients: 23 (19%) had mutations sensitive to dasatinib and nilotinib, and 12 (10%) had mutations with intermediate sensitivity. Patients with the T315I mutation were excluded from this analysis because this T315I mutation is universally resistant to all available TKIs.
The median follow-up was 76 months (range, 25–109 months) for all patients from the start of the 2nd-TKI therapy. The CHR and major cytogenetic response (MCyR) rates were 85% and 63% (complete in 59%), respectively. The rates of CCyR at 3-, 6- and 12-month were 33%, 39% and 43%, respectively. The 3-year EFS and OS rates were 53% and 84%, respectively. In a second step, we assessed the impact of a 3-month response by using the transcript levels in 71 patients with available samples. Of these 71 patients, 42 (60%) had a transcript level ≤1% on the International Scale, 14 (20%) had a transcript level superior to 1% and <10%, and 15 (20%) had a transcript level above 10%. The patients with a transcript level below 1% had significantly better EFS and OS. The 3-year EFS rates were 68%, 54%, and 29% (P = .02) and the 3-year OS rates were 93%, 79%, and 73% (P = .02), respectively. At the time of the last follow-up, 94 (76%) of the 123 patients were alive, 20 (16%) had progressed to accelerated or blast phase, 46 (37%) remained in CP while on study when receiving 2nd-TKI therapy.
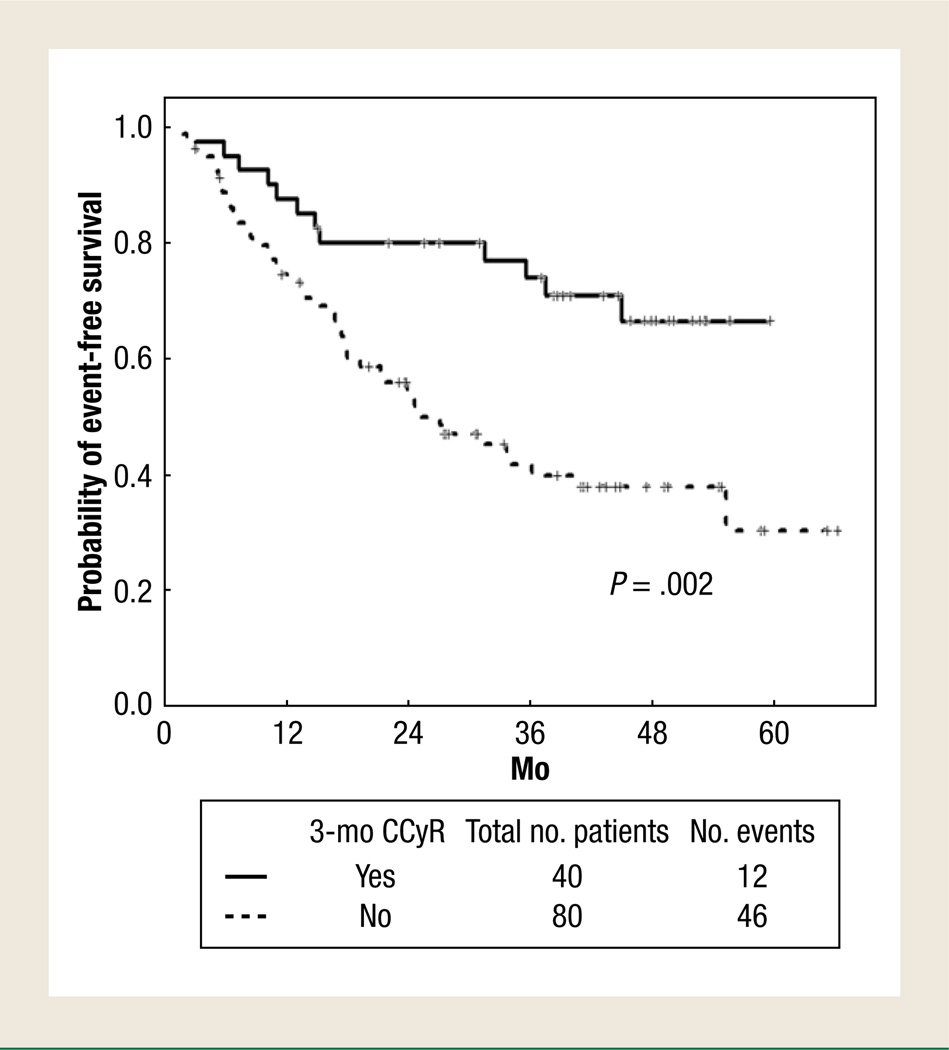
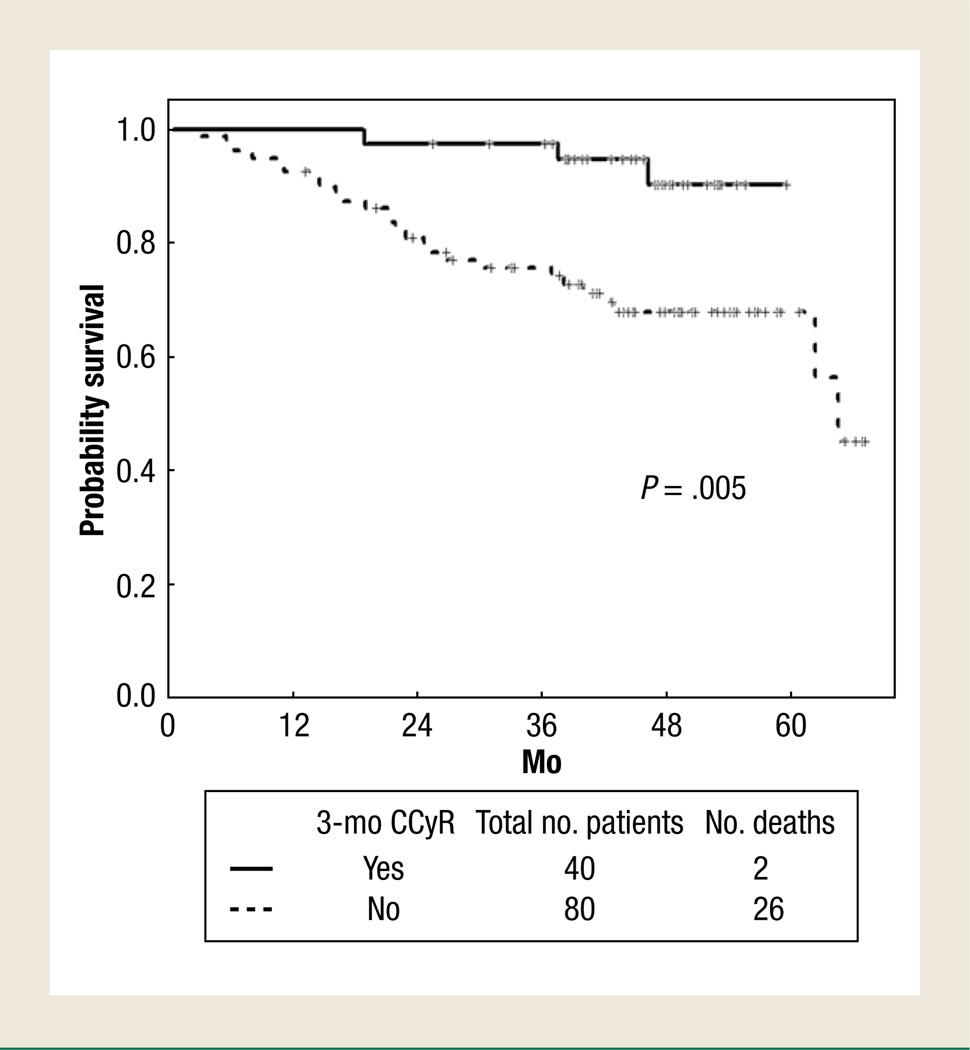
Factors associated with poor EFS in the univariate analysis were older age (>55 years), lack of any cytogenetic response to previous imatinib therapy, performance status, more than ≥90% Ph-positive metaphases at the start of 2nd-TKI therapy, and the lack of a 3-month CCyR to 2nd-TKI therapy (Table 1). In a multivariate analysis, the lack of a 3-month CCyR to 2nd-TKI therapy (hazard ratio [HR] 4.5 [95% CI, 2.12–11.66]; P < .01) was the only independent factor associated with poor EFS, with 3-year EFS rates of 74% and 43% (P = .002) (Figure 1) for patients with and without 3-month CCyR, respectively. Factors associated with poor OS in the univariate analysis were older age (>55 years), increasing peripheral blood blasts, a lack of any cytogenetic response to previous imatinib therapy, performance status, and lack of a 3-month CCyR to 2nd-TKI therapy (Table 1). In a multivariate analysis, only a lack of a 3-month CCyR to 2nd-TKI therapy (HR 5.4 [95% CI, 1.27–10.87]; P = .03) was independently associated with a lower probability of survival; the 3-year OS rates were 98% and 79%, respectively (P = .005) (Figure 2) (Table 2). The achievement of a 3-month CCyR predicts for significantly better EFS and OS than any other 3-month cytogenetic response (eg, partial, minor, and lack of any cytogenetic response).
Table 1.
Patients and Disease Characteristics Associated with 3-Year Survival Outcomes
| Parameter and Category | % 3-Y Patient Survival | |||
|---|---|---|---|---|
| EFS | P | OS | P | |
| Age | .007 | .01 | ||
| ≤55 y | 62 | 87 | ||
| >55 y | 40 | 80 | ||
| Splenomegaly | .07 | .44 | ||
| No | 52 | 85 | ||
| Yes | 0 | 57 | ||
| Hemoglobin | .48 | .08 | ||
| <10 g/dL | 36 | 60 | ||
| 10–11 g/dL | 48 | 93 | ||
| ≥12 g/dL | 53 | 86 | ||
| WBC | .40 | .08 | ||
| <10 × 109/L | 54 | 88 | ||
| ≥10 × 109/L | 48 | 80 | ||
| Platelets | .28 | .94 | ||
| ≤450 × 109/L | 55 | 88 | ||
| >450 × 109/L | 42 | 80 | ||
| Peripheral Basophils | .27 | .85 | ||
| <2% | 56 | 86 | ||
| 2–6% | 38 | 81 | ||
| ≥7% | 54 | 83 | ||
| Peripheral Blasts | .14 | .02 | ||
| 0% | 54 | 86 | ||
| 1–2% | 41 | 84 | ||
| ≥3% | 15 | 56 | ||
| Marrow Basophils | .39 | .10 | ||
| <2% | 56 | 89 | ||
| 2–4% | 44 | 74 | ||
| >4% | 39 | 86 | ||
| Marrow Blasts | .79 | .21 | ||
| 0% | 49 | 83 | ||
| 1–2% | 48 | 96 | ||
| 3–4% | 56 | 71 | ||
| ≥5% | 39 | 60 | ||
| Clonal Evolution | .35 | .37 | ||
| No | 51 | 87 | ||
| Yes | 49 | 71 | ||
| CML Duration | .42 | NA | ||
| 0–3 y | 41 | 84 | ||
| 4–y | 56 | NA | ||
| ≥6 y | 55 | NA | ||
| CHR at the Start of 2nd-TKI | .82 | .16 | ||
| No | 53 | 84 | ||
| Yes | 48 | 83 | ||
| Best Response to Imatinib | .02 | .02 | ||
| Intolerant | 50 | 100 | ||
| MCyR | 66 | 87 | ||
| mCyR | 54 | 82 | ||
| No CyR | 26 | 81 | ||
| No data | 20 | 50 | ||
| Performance Status | .04 | ≤.001 | ||
| 0 | 53 | 91 | ||
| ≥1 | 39 | 59 | ||
| Ph at the Start at the Start of 2nd-TKI | .02 | .31 | ||
| ≤90% | 67 | 81 | ||
| >90% | 41 | 80 | ||
| Prior IFN | .46 | .56 | ||
| No | 55 | 77 | ||
| Yes | 47 | 87 | ||
| Mutation Status | .06 | .06 | ||
| None | 52 | 81 | ||
| Low IC50 | 39 | 87 | ||
| Int IC50 | 25 | 50 | ||
| Not done | 65 | 95 | ||
| 3-mo CyR | .001 | .001 | ||
| CCyR | 75 | 97 | ||
| PCyR | 62 | 74 | ||
| mCyR | 40 | 86 | ||
| None | 23 | 84 | ||
Abbreviations: CCyR = complete cytogenetic response; CHR = complete hematologic response; CML = chronic myeloid leukemia; CyR = cytogenetic response; EFS = event-free survival; IC = inhibitory concentration; Int = intermediate; IFN = interferon alfa; MCyR = major cytogenetic response; mCyR = minor cytogenetic response; NA = not available; OS = overall survival; PCyR = partial cytogenetic response; Ph = Philadelphia chromosome; 2nd-TKI = second-generation tyrosine kinase inhibitor therapy; WBC = white blood cells.
Figure 1.
Event-Free Survival by 3-Month Complete Cytogenetic Response (CCyR)
Figure 2.
Overall Survival by 3-Month Complete Cytogenetic Response (CCyR)
Table 2.
Multivariate Analysis for Survival
| Adverse Feature | HR | P Value | 95% CI |
|---|---|---|---|
| For Overall Survival: No CCyR at 3 months | 5.4 | .03 | 1.27–10.87 |
| For Event-Free Survival: No CCyR at 3 months | 4.5 | <.001 | 2.12–11.66 |
Abbreviations: CCyR = complete cytogenetic response; HR = hazard ratio.
We then analyzed the factors associated with achievement of CCyR at 3 months. In the univariate analysis, high hemoglobin level, previous MCyR to imatinib therapy, and ≤90% Ph-positive metaphases were associated with 3-month CCyR. In the multivariate analysis for response, these 3 factors remained as independent poor predictive factors for 3-month CCyR.
Discussion
Our study has shown that the achievement of a 3-month CCyR is the only predictor of outcome in patients treated with 2nd-TKI after imatinib failure. We and other researchers have shown that the achievement of an early CCyR is the major surrogate endpoint for long-term outcome in patients with CML treated with imatinib as well as with the 2nd-TKI therapy.12,13,21 Furthermore, we recently reported that the achievement of a 3-month CCyR was associated with optimal outcome in patients with early CP treated with 2nd-TKI therapy.13 Our findings in the setting of post-imatinib failure are in line with our previous report in the frontline setting. Importantly, the pivotal phase II trials showed that the median time to MCyR was 2.8 months.15,16 Finally, as with the results reported by Milojkovic et al,22 and more recently by Branford et al,23 our findings confirm the importance of the achievement of an early response (molecular or cytogenetic) as a major surrogate endpoint in predicting survival, which trumped all other factors.
In addition, our study has identified that tumor burden (≥90% Ph-positive metaphases) and mainly a previous MCyR to imatinib therapy was independently predictive for the achievement of a 3-month CCyR. This is consistent with the finding of the Hammer-smith group who identified best cytogenetic response to imatinib as being predictive for response to 2nd-TKI therapy.24,25 Thus, patients with poor cytogenetic response to imatinib have a low likelihood of achieving a 3-month CCyR after 2nd-TKI therapy. This observation may have important practical consequences and should prompt the discussion as to what the definitions should be for the patients treated with 2nd-TKI therapy after imatinib failure. Therefore, we propose that, for patients treated with 2nd-TKI therapy after imatinib failure, who achieved a CCyR by 3 months of therapy should be considered an optimal response; patients with <3-month CCyR should be followed-up closely and might be considered for alternative treatment options provided that these options can realistically be expected to offer a better long-term outcome. Such patients could be evaluated concurrently for transplantation eligibility.26
Conclusion
In summary, the achievement of a 3-month CCyR is the only predictor of outcome in patients treated with 2nd TKI therapy after imatinib failure. The patients with a high tumor burden and who had not achieved MCyR while on imatinib therapy have a low likelihood of achieving 3-month CCyR to 2nd-TKI therapy and, therefore, might be offered additional options.
Clinical Practice Points.
Achievement of a CCyR is now generally accepted as a surrogate marker for survival. The achievement of a 3-month CCyR predicts for significantly better EFS and OS than any other 3-month cytogenetic response for patients treated with 2nd-TKI therapies after imatinib failure.
We propose that, for patients treated with 2nd-TKI therapy after imatinib failure, achieving a CCyR by 3 months of therapy should be considered an optimal response.
Patients with less than CCyR by 3 months should be considered for alternative treatment options provided these can realistically be expected to offer a better long-term outcome.
Acknowledgments
E. Jabbour has received honoraria from BMS and Novartis. H. Kantarjian and J. Cortes received research grants from Novartis and BMS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure
The remaining authors have stated that they have no conflicts of interest.
References
- 1.Jabbour E, Cortes JE, Giles FJ, et al. Current and emerging treatment options in chronic myeloid leukemia. Cancer. 2007;109:2171–2181. doi: 10.1002/cncr.22661. [DOI] [PubMed] [Google Scholar]
- 2.Kantarjian H, Sawyers C, Hochhaus A, et al. Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med. 2002;346:645–652. doi: 10.1056/NEJMoa011573. [DOI] [PubMed] [Google Scholar]
- 3.O’Brien SG, Guilhot F, Larson RA, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348:994–1004. doi: 10.1056/NEJMoa022457. [DOI] [PubMed] [Google Scholar]
- 4.Cortes J, Talpaz M, O’Brien S, et al. Molecular responses in patients with chronic myelogenous leukemia in chronic phase treated with imatinib mesylate. Clin Cancer Res. 2005;11:3425–3432. doi: 10.1158/1078-0432.CCR-04-2139. [DOI] [PubMed] [Google Scholar]
- 5.Kantarjian HM, Talpaz M, O’Brien S, et al. Survival benefit with imatinib mesylate versus interferon-α-based regimens in newly diagnosed chronic-phase chronic myelogenous leukemia. Blood. 2006;108:1835–1840. doi: 10.1182/blood-2006-02-004325. [DOI] [PubMed] [Google Scholar]
- 6.Deininger M, O’Brien SG, Guilhot F, et al. International randomized study of interferon vs. STI571 (IRIS) 8-year follow up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) treated with imatinib. Blood. 2009;114 abstract 1126. [Google Scholar]
- 7.Shah NP. Loss of response to imatinib: mechanisms and management. Hematology Am Soc Hematol Educ Program. 2005:183–187. doi: 10.1182/asheducation-2005.1.183. [DOI] [PubMed] [Google Scholar]
- 8.Hochhaus A, Hughes T. Clinical resistance to imatinib: mechanisms and implications. Hematol Oncol Clin North Am. 2004;18:641–656. doi: 10.1016/j.hoc.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Talpaz M, Shah NP, Kantarjian H, et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med. 2006;354:2531–2541. doi: 10.1056/NEJMoa055229. [DOI] [PubMed] [Google Scholar]
- 10.Kantarjian H, Giles F, Wunderle L, et al. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med. 2006;354:2542–2551. doi: 10.1056/NEJMoa055104. [DOI] [PubMed] [Google Scholar]
- 11.Tam CS, Kantarjian H, Garcia-Manero G, et al. Failure to achieve a major cytogenetic response by 12 months defines inadequate response in patients receiving nilotinib or dasatinib as second or subsequent line therapy for chronic myeloid leukemia. Blood. 2008;112:516–518. doi: 10.1182/blood-2008-02-141580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jabbour E, Kantarjian H, O’Brien S, et al. The achievement of an early complete cytogenetic response is a major determinant for outcome in patients with early chronic phase chronic myeloid leukemia treated with tyrosine kinase inhibitors. Blood. 2011;118:4541–4546. doi: 10.1182/blood-2011-04-348110. quiz 4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jabbour E, Kantarjian H, O’Brien S, et al. Front-line therapy with second-generation tyrosine kinase inhibitors in patients with early chronic phase chronic myeloid leukemia: what is the optimal response? J Clin Oncol. 2011;29:4260–4265. doi: 10.1200/JCO.2011.36.0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kantarjian HM, Talpaz M, O’Brien S, et al. Imatinib mesylate for Philadelphia chromosome-positive, chronic-phase myeloid leukemia after failure of interferonalpha: follow-up results. Clin Cancer Res. 2002;8:2177–2187. [PubMed] [Google Scholar]
- 15.Kantarjian HM, Giles F, Gattermann N, et al. Nilotinib (formerly AMN107), a highly selective bcr-abl tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood. 2007;110:3540–3546. doi: 10.1182/blood-2007-03-080689. [DOI] [PubMed] [Google Scholar]
- 16.Hochhaus A, Kantarjian HM, Baccarani M, et al. Dasatinib induces notable hematologic and cytogenetic responses in chronic-phase chronic myeloid leukemia after failure of imatinib therapy. Blood. 2007;109:2303–2309. doi: 10.1182/blood-2006-09-047266. [DOI] [PubMed] [Google Scholar]
- 17.Baccarani M, Cortes J, Pane F, et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol. 2009;27:6041–6051. doi: 10.1200/JCO.2009.25.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agresti A. Categorical Data Analysis. 2nd ed. Hoboken, NJ: John Wiley; 1990. [Google Scholar]
- 19.Kaplan EL, Maier P. Non-parametric estimation from incomplete observations. J Am Stat Assoc. 1965;53:457–481. [Google Scholar]
- 20.Cox DR. Regression models and life tables. J R Stat Soc. 1972;34:187–220. [Google Scholar]
- 21.Marin D, Milojkovic D, Olavarria E, et al. European LeukemiaNet criteria for failure or suboptimal response reliably identify patients with CML in early chronic phase treated with imatinib whose eventual outcome is poor. Blood. 2008;112:4437–4444. doi: 10.1182/blood-2008-06-162388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Milojkovic D, Apperley JF, Gerrard G, et al. Responses to second-line tyrosine kinase inhibitors are durable: an intention-to-treat analysis in chronic myeloid leukemia patients. Blood. 2012;119:1838–1843. doi: 10.1182/blood-2011-10-383000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Branford S, Kim DW, Soverini S, et al. Initial molecular response at 3 months may predict both response and event-free survival at 24 months in imatinib-resistant or -intolerant patients with Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase treated with nilotinib. J Clin Oncol. 2012;30:4323–4329. doi: 10.1200/JCO.2011.40.5217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milojkovic D, Nicholson E, Apperley JF, et al. Early prediction of success or failure of treatment with second-generation tyrosine kinase inhibitors in patients with chronic myeloid leukemia. Haematologica. 2010;95:224–231. doi: 10.3324/haematol.2009.012781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jabbour E, Kantarjian H, O’Brien S, et al. Predictive factors for outcome and response in patients treated with second-generation tyrosine kinase inhibitors for chronic myeloid leukemia in chronic phase after imatinib failure. Blood. 2011;117:1822–1827. doi: 10.1182/blood-2010-07-293977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jabbour E, Cortes J, Santos FP, et al. Results of allogeneic hematopoietic stem cell transplantation for chronic myelogenous leukemia patients who failed tyrosine kinase inhibitors after developing BCR-ABL1 kinase domain mutations. Blood. 2011;117:3641–3647. doi: 10.1182/blood-2010-08-302679. [DOI] [PMC free article] [PubMed] [Google Scholar]