Abstract
Introduction: Postpartum depression is a common disorder. Systematic reviews emphasized the need to conduct more trials about interventions to prevent postpartum depression. The aim of this study was to determine the effect of postpartum telephone support on maternal depression. Methods: 366 postpartum women with no history of known depression were randomly assigned into control (244 subjects) and intervention (122 subjects) groups. The control group received only routine postpartum care. In the intervention group, telephone support was provided twice in the first week and once a week during the second to sixth week of postpartum by a trained midwife in addition to the routine care. In order to meet their unpredicted needs, the mothers could contact the consultant 24 hours a day. Postpartum depression was assessed using the self-administered Edinburgh Depression Scale at 60 to 65 days of postpartum. Mothers with scores of 13 and above were considered to have depression. Logistic regression and Student's t-test were used for the data analysis. Results: There was no significant difference regarding frequency of depression between the intervention and control groups (29.9% vs. 31.6%; Odds ratio 0.91, 95% CI 0.56 to 1.49). Mean of depression score was not significantly different between the groups [9.2 (6.1) vs. 10.4 (5.8); mean difference -1.19, 95%CI -2.5 to 0.13]. Conclusion: This study did not provide evidence to show that telephone support of a midwife during postpartum period have a preventive effect on postpartum depression.
Keywords: Postpartum depression, Support, Telephone, Midwife
Introduction
Postpartum depression is one of the most common disorders following child birth that affects more than 10% of women in the postpartum period.1 The prevalence of postpartum symptomatic depression is at the highest level in Asian countries.2 In different studies in Iran, it was reported to be between 15% and 32%. 3- 7 The postpartum depression symptoms persist in considerable percent of women for months or years after child birth.8
Postpartum depression may cause many problems for the woman, her child and family. A study indicated that the functional level (personal responsibilities, household, and social functions) of women with postpartum depression is 12 times less than women without depression.9 This disorder is an independent predictor of breastfeeding outcome that reduces breastfeeding initiation ratio, duration and exclusivity; and increases breastfeeding problems and early weaning.10-12 A review showed that infants of depressed mothers are more likely to suffer from malnutrition and stunting at the age of six months.13 The children display more behavioral problems and lower cognitive functions compared with children of not depressed mothers.14
Given the high prevalence of postpartum depression and its broad adverse effects, measures for prevention of this disorder are very important. However, most interventions have not succeeded to prevent it. A review on 22 trials showed that although there were wide variety of support interventions during postpartum period for women at low risk, but the maternal outcomes including maternal mental health and postpartum depression did not change.15 A meta-analysis of 15 trials published from 1995 until 2003 on the effect of psychosocial and physiological interventions for prevention of postpartum depression also showed that the only intervention that had a statistically significant preventive effect on postpartum depression was intensive support by a health professional in the postpartum period.16
Social support has been known as one of the important predictors of postpartum depression, and low social support or lack of it, especially in the postpartum period, is associated with risk of mental health problems including depression.17,18 One of the social support sources are the health care staffs. In a study on the anxiety of primiparous mothers in Iran, those who were supported by a midwife after a traumatic delivery had less anxiety than the control group.19 In another study in Canada, mothers with symptoms of postpartum depression expressed their preference for emotional and informational one to one support, preferably by telephone with an organized schedule.20
A systematic review of 14 trials on telephone support for women during pregnancy and postpartum period showed that the telephone support as primary proactive intervention (where calls are initiated by a trained supporter) may assist in preventing smoking relapse and low birth weight, increasing breastfeeding duration, and reducing postpartum symptomatic depression.21 Furthermore, in another review, it was identified that using telephone delivered interventions is effective for promoting preventive behaviours such as cancer screening, risk factor screening for heart disease, and immunization.22
The reviews conducted recommend that further trials are needed for rigorous evaluation of preventive interventions for postpartum depression16 and also evaluation of telemedicine applications (such as telephone support which is a simple telemedicine technology).23,24 In Iran, findings of some studies showed positive effect of telephone counselling or telephone follow-up on increasing mean quality of life score (on both physical and psychological aspects) in women during postpartum period25 and in patients after pacemaker implantation.26
Although telephone support after delivery is a common practice in postpartum care in many countries, it is not used in health care system in Iran. To our knowledge, no randomized trial has been done on effect of telephone support on postpartum depression in Iran. Such interventions may have different effect on Iranian mothers due to the strong support of close relatives of newly delivered mothers. The aim of this study was to determine the effect of postpartum telephone support on maternal depression and exclusivity of breastfeeding 60 to 65 days after delivery. In this article, results of the first outcome are reported.
Materials and Methods
In this randomized controlled trial with two parallel arms, we recruited women hospitalized at the postpartum ward in Akbar-Abadi academic hospital, affiliated to Tehran University of Medical Sciences, Tehran, Iran, from August to November 2011. This public center, known as baby-friendly hospital, provides services mostly to mothers and infants in a deprived urban area. At this hospital, about 11000 mothers deliver annually. The mothers are usually discharged within 24 hours after normal delivery and 48 hours after caesarean section. Telephone support is not performed as a routine procedure of postpartum care.
Women were excluded from study if they reported any of the following characteristics: Not resident in Tehran, divorced or widowed, no access to telephone, unwilling to have exclusive breastfeeding, having lower than six years formal education, speaking or hearing problems, smoking and drug addiction, having a high risk infant (5-minute Apgar score less than 7, premature, low birth weight or twin). Moreover, women with systematic disease causing depressive symptoms (such as hypothyroidism, kidney disease, cardiac disease, chemotherapy, and radiation) were excluded as well as those with chronic diseases (such as bipolar disorder, diabetes, hypertension, thyroid disorder, and asthma), consumption of drugs causing the symptoms of depression (except contraceptive drugs), history of postpartum depression, history of stillbirth or neonatal death, or need for postpartum intensive care.
Sample size was calculated using STATA software version 9.2. Considering depression prevalence of 35% at 60 to 65 days after delivery in control group,27 reduction of the prevalence at least by two quintiles in the intervention group (P2 = 21%), a one-sided significance level of 0.05, power of 0.08, allocation ratio of 2:1 and 10% possibility of lost to follow up, sample size was calculated as 244 in the control group and 122 in the intervention group.
After getting informed written consent, demographic and obstetric information of the participants was gathered by interview with the mothers at the postpartum ward within the first day after delivery. To prevent the risk of lost to follow up, besides obtaining the participants' phone numbers and address, contact number of one of her relatives was also obtained.
The participants were randomized into the control and intervention groups using a computerized random number and block randomization with block sizes of 6 and 9. Allocation sequence was prepared by a person who was not involved in data collection and analysis. To conceal the allocation, opaque sealed consequently numbered envelops were used. Due to the nature of the study, it was not possible to blind the subjects about the type of intervention received. However, the subjects were not aware of the aim of the study, and only received general information about telephone support during postpartum. The support was covered all the issues about mothers and infants, and the outcome was evaluated by a blind research assistant.
In both groups, mothers received routine postpartum care and education by the hospital personnel (with no interference from the study staff). The researcher reminded both groups to refer to public health centers twice within the following two months (on days 10 to 15 and 42 to 60)28 to receive routine maternal and child care and refer to the hospital 60 to 65 days after delivery for an assessment.
The control group did not receive any further intervention during the study period. The intervention group received telephone support provided by a midwifery master student (the corresponding author who had passed a special short-term course on communication skills besides formal university education).
For each mother (in the intervention group), seven 15-minutes telephone calls during working days were designed over 6 weeks after delivery. First call was made within 48 hours after discharge from hospital, continuing twice during the first week and once during the second to sixth week. Sometimes, some changes were occurred in the scheduled interval based on individual needs of the mothers.
Furthermore, mother could call the midwife in order to get response to their unforeseen needs. For convenient access to the midwife, a special phone line was dedicated for their contact. Contacting the midwife was free of charge. They were told to send a text message or a single call to announce their need for contact with the midwife and she called them within five minutes.
The contents of the phone conversations were based on a mother and infant care guide and a support booklet. This booklet had been prepared by the research team based on the World Health Organization midwifery guideline29 and some other scientific literature,1,30 and had been confirmed by eight experts.
At each call, mothers were asked about own and infant's problems according to an assessment checklist and in case of a problem, the midwife explained about the proper management. The other part of the conversation was about giving information on maternal and child care, emphasizing on breastfeeding and the natural course of maternity blues and postpartum depression and their symptoms along with general recommendations for their prevention. Before the termination of any telephone call, the mothers were once again invited to ask their questions.
Contacting family members to motivate them for more maternal support (including emotional and mental support, help with household chores) was done only in case of mother request. During the next call, the same process was repeated in addition to follow-up of the problems and concerns identified in the previous calls.
In the eighth week after delivery, the researcher reminded the both groups to be present at the hospital for an interview on days 60 to 65 after their delivery. During this visit, the mothers were asked to mention their main support after delivery and fill in the Edinburgh Depression Scale.
The Edinburgh scale is a 10-item self-report measure with a possible range score of 0 to 30. It is a valid screening test that is also validated in Persian language and has been used in many studies in Iran. However, to determine its external reliability, both the Edinburgh and Beck Depression Scales were filled in by 13 mothers who referred to the hospital for vaccination of their two-month old infants; and their correlation was calculated from the Pearson test which was 0.79. Its internal reliability was 0.77 using Cronbach's alpha.
Mothers with scores of 13 and above were considered to have depression. The data were analyzed using the statistical software SPSS ver. 13 (SPSS, Inc., Chicago, IL, USA). Chi-square, Fisher's exact, independent Student's t-test, and logistic regression tests were used for the group comparisons.
The ethical permission for this study was obtained from the Ethics Committee of Tabriz University of Medical Sciences. Subject recruitment was started after study registration in www.irct.ir.
Results
Out of 366 recruited mothers (122 in the intervention group and 244 in the control group), 33 subjects (9%) did not attend at the outcome assessment visit (3 from the intervention and 29 from the control group). In the intervention group, one case was excluded from the study because of infant death due to respiratory distress (Figure 1). Because of relatively high loss to follow up in the control group, we compared the people who did and who did not attend the final visit and therefore were excluded from analysis. They were similar regarding demographic and obstetric characteristics.
Figure 1.
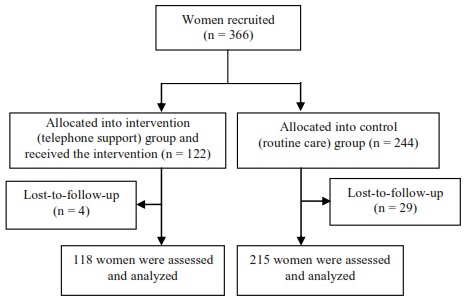
Flow diagram of the study
The two control and intervention groups were similar regarding demographic and obstetric characteristics such as age, education, occupation, being immigrant, property ownership, number and type of delivery, history of abortion and stillbirth and birth weight (Table 1).
Table 1. Baseline characteristics of the participants by study group.
| Characteristics |
Intervention
(n = 122) |
Control
(n = 244) |
| Age (years) | 26.4 (5.5) | 26.7 (5.6) |
| Spouse age (years) | 30.7 (5.6) | 31.1 (5.9) |
| Education (years) | ||
| 6 – 8 | 48 (39.3%) | 107 (43.9%) |
| 9 – 12 | 65 (53.3%) | 116 (47.5%) |
| 13 + | 9 (7.4%) | 21 (8.6%) |
| Employed | 5 (4.1%) | 7 (2.9%) |
| Born in Tehran | 61 (50.0%) | 97 (39.8%) |
| Spouse education (years) | ||
| 0 – 8 | 76 (62.3%) | 138 (56.6%) |
| 9 – 12 | 75 (36.9%) | 87 (35.7%) |
| 13 + | 1 (0.8%) | 19 (7.8%) |
| Rented residence | 90 (73.8%) | 182 (74.6%) |
| First delivery | 60 (49.2%) | 136 (55.7%) |
| History of abortion or stillbirth | 25 (20.5%) | 42 (17.2%) |
| Unwanted pregnancy | 56 (45.9%) | 78 (32.0%) |
| Vaginal delivery | 69 (56.6%) | 130 (53.3%) |
| Infant gender (boy) | 61 (50.0%) | 127 (52.0%) |
| Birth weight (g) | 3170 (354) | 3190 (402) |
| Being desirable of the infant gender | ||
| Yes | 46 (37.7%) | 97 (39.8%) |
| No | 16 (13.1%) | 36 (14.8%) |
| No difference | 60 (49.2%) | 111 (45.5%) |
| Livelihood status | ||
| Comfortable | 6 (4.9%) | 11 (4.5%) |
| Relatively comfortable | 82 (67.2%) | 155 (63.5%) |
| Sometimes hard | 54 (22.1%) | 28 (23.0%) |
| Hardly | 6 (4.9%) | 24 (9.8%) |
The data are given as number (%) or mean (SD)
The mean age of the mothers was 26.5 (SD 5.5) and their spouses was 30.9 (SD 5.8) years. Only 8.2% of the women had university education. About half (57%) of them had their first delivery. The vast majority (97%) of the mothers were housewives. Nearly three quarters of them lived in rental houses and about more than half (57%) were born outside of Tehran. More than one third (37%) of the mothers had unwanted pregnancy. 46% of them were delivered by cesarean section.
According to the mothers, the most common source of their support after delivery was their husbands and mothers. Neither of the women mentioned the health professionals working at health care centers as their primary support source. Only 7 in the control group (0.03%) mentioned it as one of their three important support sources. In the intervention group, 18% reported the midwife telephone support as the first priority, and 87% mentioned it as one of the three important sources (Table 2). There was no significant difference between the groups regarding the frequency of sources of support, except the midwife phone support.
Table 2. The most important sources of support for the mothers after delivery mentioned by the mothers 60 to 65 after delivery.
| Support sources | First priority | One of the three priorities | ||
| Intervention | Control | Intervention | Control | |
| Spouse | 39 (33.1) | 89 (42.2) | 73 (61.9) | 139 (64.7) |
| Mother | 43 (36.4) | 72 (34.1) | 73 (62.9) | 130 (60.5) |
| Health care centers | 0 (0) | 0 (0) | 0 (0) | 7 (0.03) |
| Midwife telephone support | 21 (17.8) | 0 (0) | 103 (87.3) | 0 (0) |
| Others (mother-in-law, sister, etc.) | 15 (12.7) | 50 (23.7) | 45 (38.1) | 166 (77.2) |
The data are given as number (%)
Although the mean score of Edinburg Depression Scale in the intervention group was lower than the control group, but this difference was not statically significant [9.2 (6.1) vs. 10.4 (5.8), p = 0.08). There was no statistically significant difference between the groups regarding depression prevalence (29.9% vs. 31.6%, p = 0.71) (Table 3).
Table 3. Postpartum depression in days 60 to 65 after delivery.
| Outcome |
Intervention
n = 118 |
Control
n = 215 |
Effect size
(95% CI) |
P |
| Postpartum depression, n (%) | 35 (29.9%) | 68 (31.6%) | Odds ratio: 0.91 (0.59,1.49) | 0.71 |
| Edinburg depression test score, mean (SD) | 9.2 (6.1) | 10.4 (5.8) | Mean difference: -1.19 (-2.5,0.13) | 0.08 |
SD: Standard deviation; CI: Confidence interval
Discussion
In this study, there was no statistically significant difference in terms of postpartum depression between the group receiving 2-month postpartum telephone support by a midwife and the control group getting only routine care. The telephone support was probably not professional enough or lacked high quality. High number of calls (about 15 calls a day) was done by the midwife who provided support and this could have affected the quality of the supportive intervention. During the relatively short calls, she was expected to provide information and emotional support and give recommendations for prevention of postpartum depresssion. Along this communication, other aspects such as breastfeeding issues were also educated, and the mothers could talk about other matters besides depression and the midwife had to answer all their questions.
The findings of this study showed that mothers and other relatives such as mother in law and sister were important sources of support for most of the women during puerperium. In most Iranian families, one of the close relatives would stay with the mother during puerperium to support her, especially for mothers with their first child that held true in about half of the subjects in this study, and new mothers are expected to follow their recommendations.
There are some incorrect health beliefs regarding mother and infant care in the community. The inconsistency between the health provider and the relatives' recommendations may have caused conflicts and have prevented the intervention to be effective for postpartum depression.
Although in this study there were some contacts with the relatives for more support and the mothers were told that the members of their family also could contact with the researcher, but proactive intervention in this regard had not been planned and the number of such contacts was actually very low (25 cases).
In some studies, functional social and emotional support were associated with reducing postpartum depression.31 Perhaps, one of the reasons for the failure to find positive effect of telephone support in this study was that family support is more important than the support of a health expert. In a study on women from Taiwan, mothers had less postpartum depression when they stayed in their parents' home and had their own mothers take care of them.32 In terms of different dimensions of social support, in a qualitative study interviewing 62 new mothers in their sixth week after delivery, the mothers reported a tremendous need for material support.33
Other clinical trials in different countries have also had similar results as the present study.34-36 Some reviews also showed that different interventions (such as home visits, training classes, continuous care model, psychological sessions, early follow-up in postpartum period, etc.) did not have any positive effect in preventing postpartum depression, and they only helped to identify high risk women.16,37 For example, in a study new mothers were randomized into three groups: A group had call visits by a public health nurse, another group was called by health staff as a reminder to attend at mother-infant friendly group, and the control group. Ten days after hospital discharge, an information package about child care, safety and nutrition was emailed to each group. The depression scores of the group which had the call visits did not have a significant difference compared to the other two groups.36
On the other hand, Milgrom et al.38 used weekly phone support by a psychologist or assistant psychologist and a self-help booklet entitled ‘towards parenthood', for the intervention group consisted of 20 to 32 weeks pregnant women. At week 12 after delivery, the amount of postpartum depression in the intervention group was significantly low.38 Possible reasons for the different results could be due to using the self-help booklet along the phone call, providing the telephone supports by psychologists, starting the intervention during pregnancy and /or the long period of intervention.
In some studies in which supportive interventions were effective on postpartum depression, subjects were women at risk for postpartum depression (women with Edinburg score higher than 9 or with depressive signs).16,39,40 The participants of this study were women at low risk for depression, and according to their report they did not have any history of depression during their life. This may also explain the lack of effect of the intervention in this study.
In this study, due to the relatively small sample size, it was not possible to identify possible small effects of the intervention. Another possible limitation of this study was higher number of lost to follow-up in the control group compared to the intervention group. However, since the lost to follow up subjects did not have any difference with the remaining participants, this should not have affected the findings.
This study did not provide evidence that 2-month postpartum telephone support by a midwife for low risk mothers prevents postpartum depression. Further studies are recommended on the effects of such interventions with starting support from first half of pregnancy, adding direct education for supporters of the new mothers, focusing on women at risk, and using skilled psychologists for such supports to prevent postpartum depression.
Ethical issues
None to be declared.
Conflict of Interest
The authors declare no conflict of interest in this study.
Acknowledgments
This article was extracted from the corresponding author's thesis; which was approved on 4 May 2011 by Tabriz University of Medical Sciences. Appreciation goes to the deputy of research of Tabriz University of Medical Sciences for their financial support. The authors would like to thank Tehran University of Medical Sciences, personnel of Akbar-Abadi Hospital and the participating mothers for their cooperation.
References
- 1.Ricci S, Kyle T. Maternity and pediatric nursing. Philadelphia: Wolters kluwer /Lippincott williams & wilkins; 2009. [Google Scholar]
- 2.Affonsoa DD, Deb AK, Horowitzc JA, Mayberry LJ. An international study exploring levels of postpartum depressive symptomatology. J Psychosom Res. 2000;49(3):207–16. doi: 10.1016/s0022-3999(00)00176-8. [DOI] [PubMed] [Google Scholar]
- 3.Shobeyri F, Farhadinasab AA, Nazari M. Detecting postpartum depression in referents to medical and health centers in Hamadan city. Scientific Journal of Hamadan University of Medical Sciences . 2007;14(3):24–8. (Persian) [Google Scholar]
- 4.Foruzande N, Dashtbozorgi B. Prevalence and predisposing factors of post-partum depression among women refferred to the health care center of Shahrehord, 1996. Journal Sharekord University of Medical Sciences. 2000;2(1):43–51. (Persian) [Google Scholar]
- 5.Khorramirad A, lotfi MM, Bidgoli AS. Prevalence of postpartum depression and related factors in Qom. Pejouhandeh. 2010;15(2):62–6. (Persian) [Google Scholar]
- 6.Lolati HA, Danesh MM, Hosseini SH, Khalilian A, Zarghami M. Postpartum depression in clients at health care centers in Sari. Iranian journal of psychiatry and clinical psychology. 2005;11(1):31–42. (Persian) [Google Scholar]
- 7.Bagherzadeh R, Zahmatkeshan N, Moatamed N, Khorramroudi R, Ganjoo M. Prevalence of maternal blues, postpartum depression and their correlation with premenstrual syndrome in women refferred to health centers affiliated to Bushehr university of medical sciences. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2009;12(3):9–16. (Persian) [Google Scholar]
- 8.Goodman JH. Postpartum depression beyond the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2004;33(4):410–20. doi: 10.1177/0884217504266915. [DOI] [PubMed] [Google Scholar]
- 9.Posmontier B. Functional status outcomes in mothers with and without postpartum depression. J Midwifery Womens Health. 2008;53(4):310–8. doi: 10.1016/j.jmwh.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn S, Davies B, McCleary L, Edwards N, Gaboury I. The relationship between vulnerability factors and breastfeeding outcome. J Obstet Gynecol Neonatal Nurs. 2006;35(1):87–97. doi: 10.1111/j.1552-6909.2006.00005.x. [DOI] [PubMed] [Google Scholar]
- 11.Thome M, Alder EM, Ramel A. A population-based study of exclusive breastfeeding in Icelandic women: is there a relationship with depressive symptoms and parenting stress? Int J Nurs Stud. 2006;43:11–20. doi: 10.1016/j.ijnurstu.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Dennis C-L, McQueen K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics. 2009;123(4):e736–51. doi: 10.1542/peds.2008-1629. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Maternal mental health and child health and development in resource-constrained settings. Report of a UNFPA/WHO international meeting: The interface between reproductive health and mental health. WHO. 2009.
- 14.Beck CT. The effects of postpartum depression on child development: A meta-analysis. Arch Psychiat Nurs. 1998;XII(1):12–20. doi: 10.1016/s0883-9417(98)80004-6. [DOI] [PubMed] [Google Scholar]
- 15.Shaw E, Levitt C, Wong S, Kaczorowski J. Systematic review of the literature on postpartum care: Effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. 2006;33(3):210–20. doi: 10.1111/j.1523-536X.2006.00106.x. [DOI] [PubMed] [Google Scholar]
- 16.Dennis C-L. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ. 2005;331:1–8. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Webster J, Nicholas C, Velacott C, Cridland N, Fawcett L. Quality of life and depression following childbirth: impact of social support. Midwifery. 2011;27(5):745–9. doi: 10.1016/j.midw.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Xie RH, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. 2009;19(9):637–43. doi: 10.1016/j.annepidem.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Azizi M, Faghihzade S, Nematollahzade M, Lamyian M. The effect of counseling on anxiety after traumatic childbirth in nulliparous women; a single blind randomized clinical trial. Behbood Journal. 2010;14(3):219–27. (Persian) [Google Scholar]
- 20.Letourneau N, Duffett-Leger L, Stewart M, Hegadoren K, Dennis C-L, Rinaldi CM. et al. Canadian mothers' perceived support needs during postpartum depression. J Obstet Gynecol Neonatal Nurs. 2007;36(5):441–9. doi: 10.1111/j.1552-6909.2007.00174.x. [DOI] [PubMed] [Google Scholar]
- 21.Dennis C-L, Kingston D. A systematic review of telephone support for women during pregnancy and the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2008;37(3):301–14. doi: 10.1111/j.1552-6909.2008.00235.x. [DOI] [PubMed] [Google Scholar]
- 22.McBride CM, Rimer BK. Using the telephone to improve health behavior and health service delivery. Patient Educ Couns. 1999;37(1):3–18. doi: 10.1016/s0738-3991(98)00098-6. [DOI] [PubMed] [Google Scholar]
- 23.Car J, Sheikh A. Information in practice: telephone consultations. BMJ. 2003;326:966–9. doi: 10.1136/bmj.326.7396.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews. 2000;2:CD002098. doi: 10.1002/14651858.CD002098. [DOI] [PubMed] [Google Scholar]
- 25.Khakbazan Z, Tehrani SG, Payghambardoust R, Kazemnejad A. Effect of telephone counseling during post-partum period on women's quality of life. Hayat. 2010;15(4):5–12. (Persian) [Google Scholar]
- 26.Ali-Akbari F, Khalifehzadeh A, Parvin N. The effect of short time telephone follow-up on physical conditions and quality of life in patients after pacemaker implantation. Journal Sharekord University of Medical Sciences. 2009;11(3):23–8. (Persian) [Google Scholar]
- 27.Sehati Shafaei F, Ranjbar Kouchaksaraei F, Ghoujazadeh M, Mohammad Rezaei ZH. Study of relationship between some predisposing factors and postpartum depression. Journal of Ardabil University of Medical Sciences. 2008;8(1):54–61. (Persian) [Google Scholar]
- 28.Ministry of health and medical education, Bureau of population and family health- Maternal health unit. National program on safe motherhood: integrated care for mother health [internet]. 4xxsupthxysup ed. Tehran: Ministry of health and medical education 2010. [Cited 2012 Jan 27]. Available from: http://eazphcp.tbzmed.ac.ir/uploads/26/CMS/user/file/90/Booke%20Moragebat.pdf
- 29.World Health Organization, Maternal and Newborn. Postpartum care of the mother and newborn: a practical guide. Geneva: World Health Organization; 1998. [Google Scholar]
- 30.Gunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spang C. Willims Obstetrics. 23rd ed. New York: Mc Graw-Hill companies; 2010. [Google Scholar]
- 31.Leahy-Warren P, McCarthy G, Corcoran P. Postnatal depression in first-time mothers: prevalence and relationships between functional and structural social support at 6 and 12 weeks postpartum. Arch Psychiat Nurs. 2011;25(3):174–84. doi: 10.1016/j.apnu.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Heha S-S, Coombesb L, Bartlett H. The association between depressive symptoms and social support in Taiwanese women during the month. Int J Nurs Stud. 2004;41:573–9. doi: 10.1016/j.ijnurstu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27:237–42. doi: 10.1016/j.midw.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 34.Morrell C, Spiby H, Stewart P, Walters S, Morgan A. Costs and benefits of community postnatal support workers: a randomised controlled trial. Health Technol Assess. 2000;4(6):1–100. [PubMed] [Google Scholar]
- 35.Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H. et al. The social support and family health study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas. Health Technol Assess. 2004;8(32):iii, ix–x, 1. doi: 10.3310/hta8320. [DOI] [PubMed] [Google Scholar]
- 36.Edwards NC, Sims-Jones N. A randomized controlled trial of alternative approaches to community follow-up for postpartum women. Can J Public Health. 1997;88(2):123–8. doi: 10.1007/BF03403875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrell CJ. Review of interventions to prevent or treat postnatal depression. Clin Effect Nurs. 2006;9S2:e135–e61. [Google Scholar]
- 38.Milgrom J, Schembri C, Ericksen J, Ross J, Gemmill AW. Towards parenthood: An antenatal intervention to reduce depression, anxiety and parenting difficulties. J Affect Disord . 2011; 130(3):385–94. doi: 10.1016/j.jad.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 39.Dennis C-L, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE. et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ. 2009;338:a3064. doi: 10.1136/bmj.a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfeiffer PN, Heisler M, Piette JD, Rogers MA, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry. 2011;33:29–36. doi: 10.1016/j.genhosppsych.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


