Abstract
Objective: To determine patient experience of pain during treatment with fixed orthodontic appliances, expectations of pain during debond and whether biting on a soft acrylic wafer during debond decreases pain experience.
Design: Multicentre randomized controlled trial.
Setting: Three UK hospital based orthodontic departments: Mid-Staffordshire NHS Foundation Trust, Birmingham Dental Hospital and University Hospital of North Staffordshire.
Materials and methods: Ninety patients were randomly allocated to either the control (n = 45) or wafer group (n = 45). A visual analogue scale-based questionnaire was completed pre-debond to determine pain experience during treatment and expectations of pain during debond. The appliances were debonded and those in the wafer group bit on a soft acrylic wafer. A second questionnaire was completed post-debond to assess the pain experienced.
Results: Biting on an acrylic wafer significantly reduced the pain experienced when debonding the posterior teeth (P≤0·05). Thirty-nine per cent found the lower anterior teeth the most painful. The expected pain was significantly greater than that actually experienced (P≤0·0001). Greater pain during treatment correlated with increased expectations and increased actually experienced pain (P≤0·0001).
Conclusions: Biting on a soft acrylic wafer during debond of the posterior teeth reduces the pain experienced. The lower anterior teeth are the most painful. The pain expected is significantly greater than actually experienced. Patients who had greater pain during treatment expected and experienced greater pain at debond.
Keywords: Pain, debond, fixed appliances
Introduction
Pain is defined by the International Association for the Study of Pain (1994) as an ‘unpleasant sensory and emotional experience associated with actual or potential tissue damage’. It is a subjective experience, with great individual variation and is dependent upon various factors such as age, gender, emotional state, culture and previous pain experience. Pain or discomfort is experienced by up to 95% of patients during orthodontic treatment and has been cited as a reason for discontinuing treatment.1,2
Pain is caused by tissue damage that results in cell death and subsequent release of intracellular factors such as histamine, substance P, bradykinin, prostaglandins and serotonin that stimulate nociceptors and cause depolarisation of local pain nerve fibres. Orthodontic forces create zones of pressure and tension in the periodontal ligament space, resulting in an inflammatory reaction within the periodontium and pulp along with the release of inflammatory mediators. It is thought that the perception of pain is influenced by changes in blood flow and is correlated with the release of mediators such as prostaglandins, leukotrienes, histamine, serotonin and substance P, which elicit a hyperalgesic response. The increase of these mediators following the application of force is well documented in the dental and orthodontic literature.3,4 Burstone5 described an immediate and a delayed pain response to orthodontic forces. The immediate response was due to compression of the periodontal ligament and the delayed response due to hyperalgesia of the periodontal ligament.
As part of the informed consent process, patients should be advised of all of the risks and benefits of treatment including the potential for pain at all stages. Previous research has investigated levels of pain experienced during and after various procedures, such as the placement of separators,6,7 activation of archwires8–10 and the use of different bracket systems,11–14 along with methods of pain reduction. However, pain experienced during the debond of fixed appliances is currently poorly quantified in the published literature. Further investigation is therefore required, not only for consent, but to enable review of potential methods for minimizing discomfort.
Williams and Bishara15 conducted a pilot study of 15 subjects to investigate the level and direction of force that could be tolerated at debond. Torsional forces were very poorly tolerated and less than 100 g of force could be applied before discomfort was experienced, while intrusional forces were relatively well tolerated, with a discomfort threshold of 934 g. Mobility of the teeth reduced the discomfort threshold. The periodontal structures are designed to withstand intrusive forces during mastication and it is logical that intrusive forces would be best tolerated. They suggested that stabilizing the teeth by asking the patient to bite on a cotton wool roll during debond may reduce the discomfort experienced.
This study aims to determine: (1) pain experience during orthodontic fixed appliance treatment; (2) expectations of pain during the debonding of orthodontic fixed appliances; and (3) whether biting on a soft acrylic wafer reduces pain experience during the debonding of orthodontic fixed appliances.
The primary null hypothesis was that biting on a soft acrylic wafer during debonding of fixed appliances does not reduce pain experienced and the secondary null hypothesis was that there is no difference between expected and perceived levels of pain during the debonding of fixed appliances.
Materials and methods
This prospective randomized controlled trial recruited patients from the orthodontic departments of the Mid-Staffordshire NHS Foundation Trust, Birmingham Dental Hospital and University Hospital of North Staffordshire.
Ethical approval was gained from the Northern and Yorkshire Research Ethics Committee, reference number: 09/H0903/6. Local NHS Research and Development approval was gained for the three sites.
The sample size calculation was based on a clinically significant difference of 13 mm on a visual analogue scale (VAS) (100 mm long) with a standard deviation of 20 mm, a significance level of 0·05 and a power of 80%. This gave a required sample size of 39 subjects per group with a total of 78 subjects. A 13 mm reduction in pain score was deemed to be clinically significant by research previously carried out in accident and emergency departments on children aged 5–16 years in acute pain.16 To date, there have been no studies determining clinically significant reduction in pain scores for orthodontic patients.
All eligible patients were given verbal and written information describing the trial and the opportunity to ask further questions. Inclusion criteria for the study were:
informed consent gained from patients and parents;
patients aged 12–18 years;
patients with full orthodontic fixed appliances in both arches with either Victory or SmartClip brackets (both 3M Unitek) precoated with APC adhesive.
Exclusion criteria included:
patients who had completed a previous course of orthodontic treatment;
patients who were unable to comprehend or complete the questionnaire;
patients with craniofacial syndromes.
Randomization was carried out using Minitab computer software. Sealed opaque envelopes were used to conceal the allocation and they were opened independently upon patient recruitment. Informed consent was obtained and the patients were randomly allocated to one of two groups, the control group (group 1) or the wafer group (group 2). Both groups completed the first VAS-based questionnaire investigating their overall pain experience during fixed appliance treatment, their anxiety levels before the debond and their expectations of pain during the removal of their appliances. The VAS consisted of a 100 mm line labelled at the extremes with ‘no pain’ and a happy face and ‘worst pain imaginable’ and a sad face. The investigator was present while the questionnaires were answered to supervise and provide further information, if required.
Following completion of the first questionnaire the fixed appliances were debonded using a standardized procedure. Debonding pliers, with right-angled beaks, were used, beginning with the upper right quadrant and working around to the upper left quadrant, followed by the lower right quadrant around to the lower left quadrant. The archwire was left in-situ during the debond. Those in the wafer group bit into a soft acrylic wafer as their appliances were debonded (Figure 1) and the control group stayed open with their teeth out of occlusion. On completion of the debond, the patients completed the second questionnaire to determine the actual amount of pain experienced during the debond.
Figure 1.
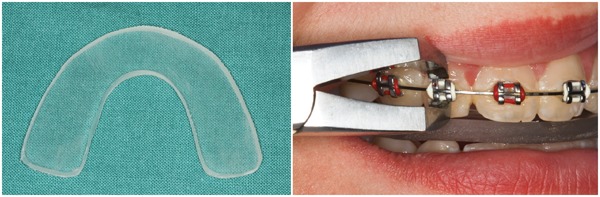
The soft acrylic bite wafer and the wafer in use during the debond
The soft acrylic bite wafers were manufactured by the orthodontic laboratory at Birmingham Dental Hospital. They were constructed from 3 mm transparent Drufosoft material (Dreve GmbH) (Figure 1).
The questionnaires were analysed by one operator who was blinded to the group allocation. Digital callipers were used to measure the visual analogue scale scores and intra-examiner reliability for the measurements was tested by re-measuring 15 questionnaires 1 month later.
Statistical analysis
The Predictive Analytics SoftWare (PASW 18·0) statistical program was used for the statistical analysis of data. The results were not normally distributed so a logarithmic transformation was applied to all the VAS pain scores, before carrying out the analyses to enable the use of parametric statistical tests.
The effect of the intervention (control or wafer group) was assessed using multiple linear regression analysis and the model was adjusted for age, gender, type of molar attachment and the expected pain at debond. To facilitate interpretation of the multiple linear regression β coefficients, based on a log-transformed outcome, they are reported as the percentage difference in pain, calculated using the formula: [exp (β)−1]×100%.
The difference between the expected and actual pain scores was determined using Wilcoxon signed-rank analysis. Spearman’s Rank correlations were determined between the overall pain experienced during the fixed appliance treatment, the level of anxiety about the debond, the overall pain expected during the debond and the actual pain experienced at debond. Descriptive statistics were used to determine the most painful sextant during the debond.
The intra-examiner reliability for the measurement of the VAS was performed using intra-class correlation following re-measurement of 15 subject questionnaires. The intra-class correlation coefficient was 0·984, indicating good intra-examiner reliability for the measurement of the VAS.
Results
A consort diagram showing the flow of patients through the study is shown in Figure 2.
Figure 2.
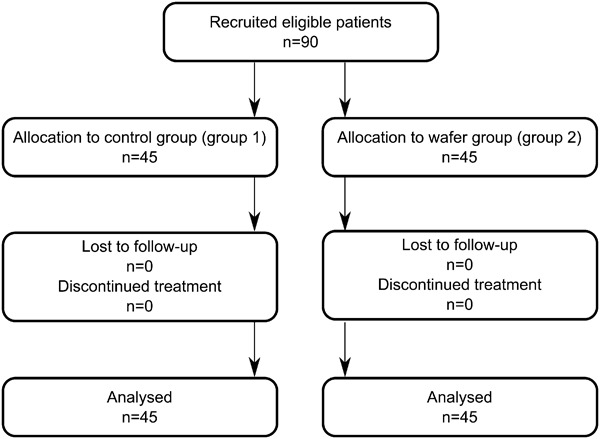
Consort flow diagram
Baseline data
Ninety patients participated with 45 in each group. There were 51 females and 39 males with a mean age of 16 years (SD: 1·5 years). The control group comprised 23 females and 22 males with a mean age of 15·9 years (SD: 1·5 years), while the wafer group had 28 females and 17 males with a mean age of 16 years (SD: 1·6 years).
The duration of fixed appliance treatment ranged from 12–48 months with a mean of 26·9 months. Satisfaction with the overall treatment result was generally high with a median VAS score of 98·3 (Table 1).
Table 1. Baseline data: patient demographics and the VAS scores for the expectations of pain during the debond.
| Group 1 — control | Group 2 — wafer | Total | ||
| Subjects | Number | 45 | 45 | 90 |
| Males (%) | 22 (48·9) | 17 (37·8) | 39 (43·3) | |
| Females (%) | 23 (51·1) | 28 (62·2) | 51 (56·7) | |
| Age (years) | Mean (SD) | 15·9 (1·5) | 16·0 (1·6) | 16·0 (1·5) |
| Treatment duration (months) | Mean (SD) | 26·1 (7·3) | 27·7 (9·8) | 26·9 (8·6) |
| Range | 12–41 | 12–48 | 12–48 | |
| Satisfaction with treatment result | Mean (SD) | 91·6 (14·0) | 94·8 (8·8) | 93·2 (11·7) |
| Median | 98·5 | 98·2 | 98·3 | |
| Range | 48·8–100 | 49·2–100 | 48·8–100 | |
| Expectations of pain | ||||
| Anxiety about debond | Median | 13·2 | 11·4 | 11·4 |
| Range | 0–89·9 | 0–100 | 0–100 | |
| Pain overall | Median | 25·9 | 33·6 | 33·1 |
| Range | 0–76·0 | 0–99·4 | 0–99·4 | |
| Upper posterior teeth | Median | 29·4 | 30·4 | 30·2 |
| Range | 0–88·1 | 0 – 100 | 0–100 | |
| Upper anterior teeth | Median | 33·2 | 34·8 | 33·7 |
| Range | 0–85·7 | 0–87·7 | 0–87·7 | |
| Lower posterior teeth | Median | 22·3 | 23·6 | 23·0 |
| Range | 0–83·8 | 0–89·6 | 0 89·6 | |
| Lower anterior teeth | Median | 26·0 | 27·9 | 27·8 |
| Range | 0–75·7 | 0–95·7 | 0–95·7 | |
| Composite removal | Median | 29·6 | 21·5 | 23·8 |
| Range | 0–92·4 | 0–88·4 | 0–92·4 |
Expectations of pain during the debond process
The expectations of pain during debond are shown in Table 1. Both groups had a similar level of anxiety about the debond and similar expectations of pain, with a full range of scores given (0–100).
Pain experienced during fixed appliance treatment
Figure 3 shows the pain experienced overall during the fixed appliance treatment along with the pain during adjustment of the appliances and the pain 24 h after adjustment. Patients reported that the pain 24 h after adjustment of their appliances was greater than that overall or during the actual adjustment.
Figure 3.
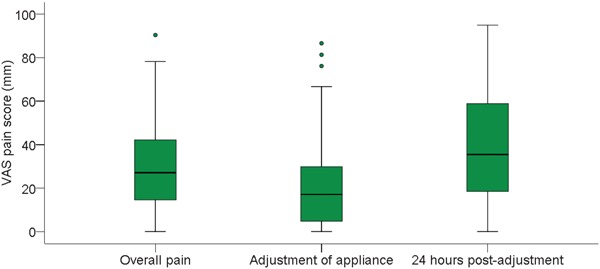
Box and whisker plot of the pain experienced during fixed appliance treatment
The actual pain experienced at debond
The pain experienced at debond is shown in Figure 4. The overall pain experienced and that experienced for all quadrants, except the lower anterior teeth, was lower in the wafer group than in the control group. Debond of the lower anterior teeth was reported as the most painful by both groups. Debond of the lower posterior teeth was the second most painful, followed by the upper anterior teeth with the upper posterior teeth being the least painful.
Figure 4.
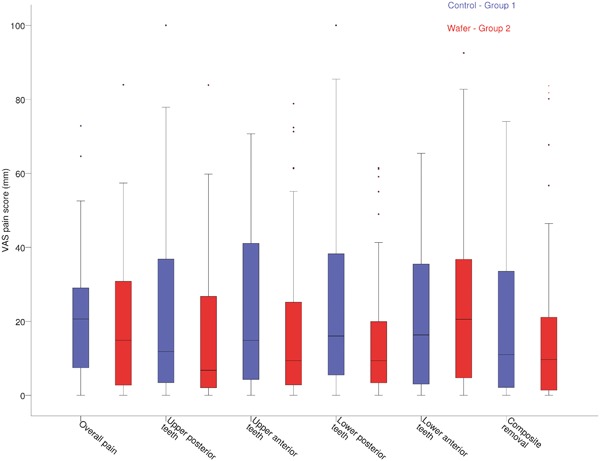
Box and whisker plot of the pain experienced during debond for the control and wafer group
The median pain score for composite removal was less than that of the overall pain experienced during the debond. The lower anterior teeth were chosen as the most painful sextant by 39%, followed by the upper right sextant (18%) (Figure 5).
Figure 5.
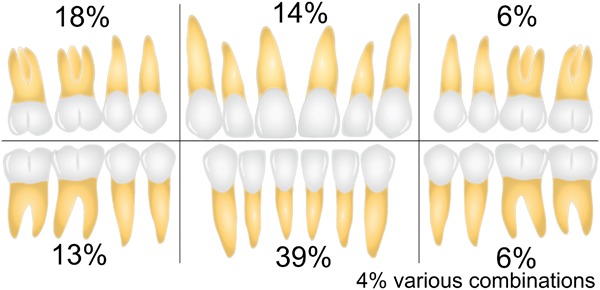
The most painful sextant during the debond, as reported by the patients
Multiple linear regression analysis was used to examine the effect of the intervention and the results are shown in Table 2. The wafer group had lower pain scores overall, for the posterior teeth and the upper anterior teeth with up to a 36% reduction in the pain scores, for the lower posterior teeth; however, this did not reach statistical significance (P = 0·107).
Table 2. Multiple linear regression analysis for the effect of the intervention, adjusted for age, gender, type of molar attachment and the expected level of pain at debond. Percentages are used to give meaning to the logarithmically transformed data.
| Control/wafer | Age/gender adjusted | Age, gender, molar attachment adjusted | Age, gender, molar attachment, expected pain adjusted | ||
| Overall | B | −0·31 | −0·35 | −0·33 | −0·44 |
| % difference in pain | −27% | −30% | −28% | −36% | |
| 95% confidence interval | −56%, 22% | −59%, 22% | −55%, 22% | −59%, 11% | |
| P-value | 0·236 | 0·183 | 0·204 | 0·079 | |
| Upper posterior teeth | B | −0·4 | −0·46 | −0·45 | −0·58 |
| % difference in pain | −33% | −37% | −36% | −44% | |
| 95% confidence interval | −63%, 22% | −63%, 11% | −63%, 11% | −67%, 0% | |
| P-value | 0·161 | 0·107 | 0·118 | 0·037 | |
| Upper anterior teeth | B | −0·22 | −0·29 | −0·28 | −0·45 |
| % difference in pain | −20% | −25% | −24% | −36% | |
| 95% confidence interval | −55%, 35% | −55%, 35% | −55%, 35% | −63%, 11% | |
| P-value | 0·427 | 0·292 | 0·319 | 0·078 | |
| Lower posterior teeth | B | −0·44 | −0·49 | −0·47 | −0·58 |
| % difference in pain | −36% | −39% | −37% | −44% | |
| 95% confidence interval | −63%, 11% | −63%, 11% | −63%, 101% | −67%, −10% | |
| P-value | 0·107 | 0·70 | 0·086 | 0·031 | |
| Lower anterior teeth | B | 0·095 | 0·03 | 0·03 | −0·18 |
| % difference in pain | 10% | 3% | 3% | −16% | |
| 95% confidence interval | −39%, 101% | −39%, 82% | −45%, 82% | −50%, 35% | |
| P-value | 0·742 | 0·912 | 0·933 | 0·496 |
Once the multiple linear regression model had been adjusted the wafer group had significantly less pain during debond of the upper posterior teeth (P = 0·037) and the lower posterior teeth (P = 0·031).
The expected pain scores were significantly greater than the experienced scores overall, for all quadrants and for the composite removal (P≤0·001) (Table 3).
Table 3. The Wilcoxon signed-rank test to compare the expected pain scores with the actually experienced pain scores. Z is the Wilcoxon signed-rank test result.
| Overall pain | Upper posterior teeth | Upper anterior teeth | Lower posterior teeth | Lower anterior teeth | Composite removal | |
| Z | −4·194 | −4·053 | −5·349 | −3·569 | −4·159 | −3·274 |
| Significance P-value | <0·0001 | <0·0001 | <0·0001 | <0·0001 | <0·0001 | 0·001 |
Table 4 shows the correlations between expected and actually experienced pain scores. There were correlations between the level of pain experienced during the course of fixed appliance treatment and the anxiety about the debond (correlation coefficient r = 0·215, P = 0·041), the expected level of pain at debond (r = 0·373, P≤0·0001) and the pain experienced during the debond (r = 0·408, P≤0·0001). The level of anxiety about the debond correlated with the expected pain (r = 0·617, P≤0·0001) and with the actually experienced pain (r = 0·249, P = 0·018). The expected pain scores correlated with the actually experienced pain scores (r = 0·340, P = 0·001).
Table 4. Spearman’s rank correlations between the overall pain experienced during the fixed appliance treatment, the level of anxiety about the debond, the overall pain expected during the debond and the actual pain experienced at debond.
| Overall pain during fixed appliances | Anxiety about the debond | Overall pain expected | Overall pain experienced | ||
| Overall pain during fixed appliances | Correlation coefficient r | 1·000 | |||
| P-value | . | ||||
| Anxiety about the debond | Correlation coefficient r | 0·215 | 1·000 | ||
| P-value | 0·041 | . | |||
| Overall pain expected | Correlation coefficient r | 0·373 | 0·617 | 1·000 | |
| P-value | <0·0001 | <.0001 | . | ||
| Overall pain experienced | Correlation coefficient r | 0·408 | 0·249 | 0·340 | 1·000 |
| P-value | <0·0001 | 0·018 | 0·001 | . |
Discussion
This study showed that biting on a soft acrylic wafer during debond of the posterior teeth significantly reduced the pain experienced (P≤0·05). However, there was no statistically significant reduction in pain for the anterior teeth. The lower anterior teeth were reported by 39% of subjects to be the most painful sextant during debond, while the upper right posterior teeth were reported to be the most painful by 18%.
Pain is very subjective, with great individual variation. In this study, the large ranges of pain scores given both during treatment and during the debond mirror previous descriptions in the literature.7–10,12,14,17–19 Subjects who experienced more pain during treatment were more anxious about the debond and both expected and experienced more pain. The emotional state of the patient can modulate pain experience and increased anxiety can act to lower the pain threshold. Conversely, the motivation to wear appliances may serve to increase the pain threshold or filter out painful stimuli.20,21 Similarly, excitement about the often long-awaited debond, may reduce the pain experienced by raising the pain threshold or filtering painful stimuli.
Williams and Bishara15 in their pilot study of the force that could be tolerated at debond, found the lower incisors had the lowest threshold and that mobility of the teeth reduced the threshold further. The type of force applied affected the threshold for discomfort, with intrusive forces tolerated best and torsional forces very poorly tolerated. They concluded that providing an intrusive force on the teeth during debond may reduce the discomfort experienced. Our study showed that an intrusive bite force significantly reduced the pain experienced for the posterior teeth, but was not significant for the anterior teeth. This difference may be due to the ability of the posterior teeth to provide a greater biting force, which is distributed along the long-axis of the tooth. The wafer was repositioned when debonding the upper anterior teeth to ensure all teeth were in contact, but due to the small differences in the level of the incisal edges, the intrusive force may have been reduced and because of their inclination the force was not distributed along the long-axis. When debonding the lower anterior teeth, the patient bit into the wafer in an edge-to-edge incisor position. This ensured that there was sufficient space to accommodate the beaks of the debond pliers between the incisal edge of the bracket and the upper incisors. It is conceivable that this forward positioning of the mandible would reduce the biting force. Using a graduated wafer which is thicker anteriorly and made of a slightly softer material, may allow an even biting force to be applied to all teeth. Alternatively, biting on a firm cotton wool roll, which is smaller, easier to position and more readily available in most clinical settings, could provide a similar effective, intrusive, stabilizing force.
Strengths and weaknesses of the study
In this study, the use of a bite wafer ensured a standardized thickness and consistency, instead of cotton wool rolls which can vary significantly.
The use of multiple linear regression analysis enabled various confounding factors to be accounted for including gender, type of molar attachment (bonded tubes or bands) and the expectations of pain during the debond. Half of the subjects (51·1%) had bonded tubes on all four first molars, 16·7% had bands on all four first molars and 32·2% had a combination of bands and tubes. Those with bands on their molars could not occlude as the bands were debonded. The distribution of males to females was equal in the control group, but there were a greater proportion of females in the wafer group. As females are potentially more likely to report pain than males,7,10,20–22 the uneven gender distribution may have underestimated the effect of biting on the wafers and stratifying the groups for gender would have avoided this. The upper anterior teeth were expected to be the most painful during the debond. Potentially, this is because the upper anterior teeth had been felt to be the most painful during the course of treatment. This might be expected if the upper anterior teeth had been bodily retracted during treatment. However, neither the type of presenting malocclusion, extraction decision nor the most painful sextant during the fixed appliance treatment was recorded during the data collection to confirm this.
Implications for clinical practice: pain during fixed appliance treatment
Pain experience during and after the adjustment of appliances was variable with a wide range of scores given. It is usual to warn patients about pain following adjustment; however, we should also be mindful about the potential discomfort of the actual adjustment process.
Expectations of the debond process
The median anxiety score of 11·4 suggests a relatively low level of anxiety overall, but a full range of scores were given. Forty-six subjects listed specific concerns. The commonest was, ‘having white marks’ or, ‘discoloured teeth’ (47·8%), followed by pain (41·3%). Decalcification is a risk of orthodontic treatment and patients should be informed of this at the start of treatment. The extent of decalcification is often obvious before debond and reassurance can be given pre-debond which may help to alleviate some of this anxiety.
Debonding-fixed appliances
Theoretically biting on a soft acrylic wafer or a cotton wool roll equivalent reduces pain by applying an intrusive force to the teeth. The intrusion helps to stabilize the teeth and counteract the sheer/peel and torsional forces applied to the periodontal ligament during the debond. The additional pressure on the periodontal ligament may also provide a proprioceptive stimulus, helping to reduce the pain experienced, akin to the gate theory of pain control whereby rubbing an injured limb helps to take away pain. Occluding during debond also helps protect the airway by forcing a loose bracket towards the buccal sulcus, rather than potentially down the airway.
The lower anterior teeth were said to be the most painful by 39% and can be explained by the greater debond force per unit surface area of the root. Explanation of why the upper right posteriors were reported as the most painful by 18% is more difficult. It could be because this was the first sextant to be debonded and as such, was the most memorable. Additionally, the clinicians carrying out the debonds were right-handed and using a pair of right-angled debonding pliers. Operating on the right side requires a more rotated hand position causing a grip which has a greater chance of applying more painful torsional forces when debonding.
The results of this study suggest that biting on a safe, partially compressible material during debond, may make the process more comfortable and that spending time to alleviate anxiety about the expectations of pain during debond is likely to be worthwhile. The null hypothesis that biting on a soft acrylic wafer during debond does not reduce the pain experienced is therefore rejected for posterior teeth and accepted for anteriors. The null hypothesis that there is no difference between the expected and actual pain scores is also rejected.
Conclusions
Biting on a soft acrylic wafer during debond of the posterior teeth reduces the pain experienced.
The lower anterior teeth are the most painful during debond.
Patients who experience greater pain during their fixed appliances expect and actually experience greater pain during the debond.
Acknowledgments
The authors would like to thank all of the patients, parents and staff at Mid-Staffordshire NHS Foundation Trust, University Hospital of North Staffordshire and Birmingham Dental Hospital who were involved in the study.
References
- 1. doi: 10.1179/bjo.12.4.179. Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod 1985; 12: 179–88. [DOI] [PubMed] [Google Scholar]
- 2. doi: 10.1016/0889-5406(91)70073-6. Brown DF, Moerenhout RG. The pain experience and psychological adjustments to orthodontic treatment of preadolescents, adolescents and adults. Am J Orthod Dentofac Orthop 1991; 100: 349–56. [DOI] [PubMed] [Google Scholar]
- 3. doi: 10.1177/10454411910020040101. Davidovitch Z. Tooth movement. Crit Rev Oral Biol Med 1991; 2: 411–50. [DOI] [PubMed] [Google Scholar]
- 4. Davidovitch Z, Nicolay OF, Ngan PW, Shanfeld JL, Neurotransmitters, cytokines and the control of alveolar bone remodelling in orthodontics. Dent Clin N Am 1988; 32: 411–35. [PubMed] [Google Scholar]
- 5. Burstone CJ. The biomechanics of tooth movement. In Kraus BS, Riedel RA (eds.). Vistas in orthodontics. Philadelphia, PA: Lea & Febiger, 1962; 197–213. [Google Scholar]
- 6. doi: 10.1016/j.ajodo.2007.09.013. Bergius M, Broberg AG, Hakeburg M, Berggren U. Prediction of prolonged pain experiences during orthodontic treatment. Am J Orthod Dentofac Orthop 2008; 133: 339.e1–.e8. [DOI] [PubMed] [Google Scholar]
- 7. doi: 10.1034/j.1600-0722.2002.11193.x. Bergius M, Berggren U, Kiliaridis S. Experience of pain during an orthodontic procedure. Eur J Oral Sci 2002; 110: 92–8. [DOI] [PubMed] [Google Scholar]
- 8. doi: 10.1093/ejo/26.1.79. Erdinc AME, Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod 2004; 26: 79–85. [DOI] [PubMed] [Google Scholar]
- 9. doi: 10.1016/0889-5406(92)70054-e. Jones ML, Chan C. The pain and discomfort experienced during orthodontic treatment. A randomised controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop 1992; 102: 373–81. [DOI] [PubMed] [Google Scholar]
- 10. doi: 10.1093/ejo/18.4.349. Scheurer P, Firestone A, Burgin W. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod 1996; 18: 349–57. [DOI] [PubMed] [Google Scholar]
- 11. doi: 10.2319/121007-579.1. Fleming PS, DiBiase AT, Sarri Gm Lee RT. Pain experience during initial alignment with a self ligating and a conventional fixed orthodontic appliance system. Angle Orthod 2009; 79: 46–50. [DOI] [PubMed] [Google Scholar]
- 12. doi: 10.1093/ejo/cjm131. Scott P, Sherriff M, DiBiase AT, Cobourne MT. Perception of discomfort during initial orthodontic tooth alignment using a self-ligating or conventional bracket system: a randomised clinical trial. Eur J Orthod 2008; 30: 227–32. [DOI] [PubMed] [Google Scholar]
- 13. doi: 10.1016/j.ajodo.2007.08.032. Pringle AM, Petrie A, Cunningham SJ, McKnight M. Prospective randomised clinical trial to compare pain levels associated with 2 orthodontic fixed bracket systems. Am J Orthod Dentofac Orthop 2009; 136: 160–67. [DOI] [PubMed] [Google Scholar]
- 14. doi: 10.1093/ejo/cjp003. Tecco S, D’Attilio M, Tete S, Festa F. Prevalence and type of pain during conventional and self-ligating orthodontic treatment. Eur J Orthod 2009; 31: 380–84. [DOI] [PubMed] [Google Scholar]
- 15. doi: 10.1016/S0889-5406(05)80324-5. Williams OL, Bishara SE. Patient discomfort levels at the time of debonding: a pilot study. Am J Orthod Dentofac Orthop 1992; 101: 313–19. [DOI] [PubMed] [Google Scholar]
- 16. doi: 10.1016/s0196-0644(96)70238-x. Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med 1996; 27: 485–89. [DOI] [PubMed] [Google Scholar]
- 17. doi: 10.1016/0889-5406(89)90228-x. Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofac Orthop 1989; 96: 47–53. [DOI] [PubMed] [Google Scholar]
- 18. doi: 10.1016/s0889-5406(98)70201-x. Sergl HG, Klages U, Zenter A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod and Dentofacial Orthop 1998; 114: 684–69. [DOI] [PubMed] [Google Scholar]
- 19. Bondemark L, Fredriksson K, Ilros S. Separation effect and perception of pain and discomfort from two types of orthodontic separators. World J Orthod 2004; 5: 172–76. [PubMed] [Google Scholar]
- 20. doi: 10.1093/ejo/cjl081. Krishnan V. Orthodontic pain: from causes to management — a review. Eur J Orthod 2007; 29: 170–79. [DOI] [PubMed] [Google Scholar]
- 21. doi: 10.1007/BF01300354. Bergius M, Kiliardis S, Berggren U. Pain in orthodontics: a review and discussion of the literature. J Orofac Orthop 2000; 61: 125–312. [DOI] [PubMed] [Google Scholar]
- 22. doi: 10.1111/j.1600-0528.1987.tb00493.x. Kvam E, Bondevik O, Gjerdet NR. Traumatic ulcers and pain during orthodontic treatment. Comm Dent Oral Epidemiol 1989; 17: 154–57. [DOI] [PubMed] [Google Scholar]


