Abstract
The prevalence of adult tobacco users who utilize the emergency department as patients or parents is disproportionately higher than the national average rates of tobacco use. Thus, it is advised that the emergency department be utilized as a venue for providing tobacco cessation counseling to adult tobacco users. Using a randomized control trial design, this pilot study evaluated the effect of a brief tobacco cessation intervention for tobacco using parents of children brought to a pediatric emergency department. Participants received either usual care or a brief tobacco cessation intervention based on the first 2 of the 5A's of the Clinical Practice Guidelines and fax referral to the Quitline. The primary outcome was self-reported repeated point prevalence of tobacco use at 6 weeks and 3 months following the intervention. Secondary aims included number of quit attempts, increases in readiness to quit, comparisons of participants who were successfully retained, and contact rates by Quitline counselors. At 3-month follow-up, compared to the Usual Care Control group, intervention participants were more likely to have made at least one quit attempt (59% vs. 34%; p<.01), be seriously thinking about quitting (68% vs. 37%; p<.001), and have higher Ladder scores (6.2 vs. 5.3; p<.05). Study personnel were able to contact 68% and 52%, respectively, of participants at 6-week and 3-month follow-up. Quitline counselors were unable to reach 54% of participants. Our results reveal increased intentions to quit and trends toward quitting, however we experienced difficulties with participant retention. Suggestions for improvements in point prevalence and retention are given.
Introduction
More than 30 million pediatric patients are treated annually in U.S. emergency departments (McCaig & Ly, 2002). Parents of pediatric emergency department and adult emergency department patients have a disproportionately high rate of smoking, with estimates up to 48% (Baker, Stevens, & Brook, 1994; Lowenstein, Koziol-McLain, & Thompson, 1998; Mahabee-Gittens, 2002; O'Brien et al., 1997). Recently, the American College of Emergency Physicians recommended that the emergency department be utilized as a venue to launch tobacco cessation efforts (Bernstein, et al., 2006). When children are brought to the emergency department, there is an opportunity for a “teachable moment” in which to give tobacco cessation advice to parents who may be more motivated to quit smoking in order to improve their child's health (Winickoff et al., 2003). In addition, studies have shown that adult emergency department patients are interested in quitting and are willing to engage in a brief tobacco cessation intervention (Bock et al., 2001; Klinkhammer, Patten, Sadosty, Stevens, & Ebbert, 2005).
Health care providers have been encouraged to utilize the Public Health Service-sponsored Clinical Practice Guideline, Treating Tobacco Use and Dependence (Fiore, et al., 2000) as a framework for providing tobacco interventions to tobacco-using patients. However, emergency department practitioners cite numerous barriers to implementing this type of intervention, including lack of time, lack of confidence in their ability to give smoking-cessation advice, and difficulties with emergency department follow-up (Prochazka, Koziol-McLain, & Tomlinson, 1995; Zapka et al., 2000).
Referral of smokers by emergency department staff to a tobacco Quitline may help to overcome some of these barriers. Telephone counseling has been shown to be an effective intervention for smoking cessation (Fiore, et al., 2000; Lichtenstein, Glasgow, Lando, Ossip-Klein, & Boles, 1996; Ossip-Klein & McIntosh, 2003; Stead, Lancaster, & Perera, 2004; Zhu, Anderson, & Tedeschi, 2002), and the use of “proactive referral” (faxing of a completed Quitline enrollment form by the healthcare provider) to a tobacco Quitline involves minimal effort by the provider. In addition, tobacco Quitline counselors may aid in achieving higher rates of follow-up in an inner city emergency department population which is historically difficult to track and retain due to factors such as low social support, frequent changes of address and high geographic mobility, lack of telephones, increased caretaker stress, and lower socioeconomic status (Richman et al., 2000; Senturia et al., 1998). Although the effectiveness of fax referrals from the emergency department in contacting smokers and assisting in quit attempts has not been examined, a recent study demonstrated that fax referrals from the dental care setting resulted in higher quit rates than those who received usual care; however, overall low numbers of participants had received counseling from the Quitline (Gordon, Andrews, Crews, Payne, & Severson, 2007).
The primary aim of this study was to examine the efficacy of a brief emergency department-based tobacco cessation intervention for tobacco-using parents of pediatric patients in combination with fax referral to a state tobacco Quitline. Participants were randomized to one of two conditions: (1) Intervention, in which participants were given a brief tobacco cessation intervention based on the first 2As (Ask and Advise) of the 5As of the Clinical Practice Guideline, and offered a faxed referral to the telephone tobacco Quitline, or (2) Usual Care Control. The primary outcome was self-reported, repeated point prevalence of tobacco use at 6 weeks and 3 months following the intervention. Secondary aims included number of quit attempts, level of readiness to quit in the next 30 days, number of cigarettes smoked daily, characteristics of participants who were successfully followed up by study personnel, and contact rates by Quitline counselors.
Method
Participants
Participants were recruited between September 2005 and August 2006 from the emergency department of Cincinnati Children's Hospital Medical Center. This emergency department has an annual patient census of more than 85,000 visits. All parents/legal guardians of children 18 years of age and younger triaged to the non-urgent category who reported current tobacco use by answering “yes” to one or both of the following questions, (1) “Have you smoked at least one cigarette in the previous week?” and (2) “Do you currently use chewing tobacco or snuff (took even one dip in the last 7 days)?” were eligible for participation in the study. Exclusion criteria included current enrollment in a smoking cessation program, use of nicotine replacement or other pharmacologic smoking cessation treatment, non-English speaking (due to lack of resources for translation of study materials), no working telephone number, and no permanent mailing address (or plans to move within 4 months after enrollment).
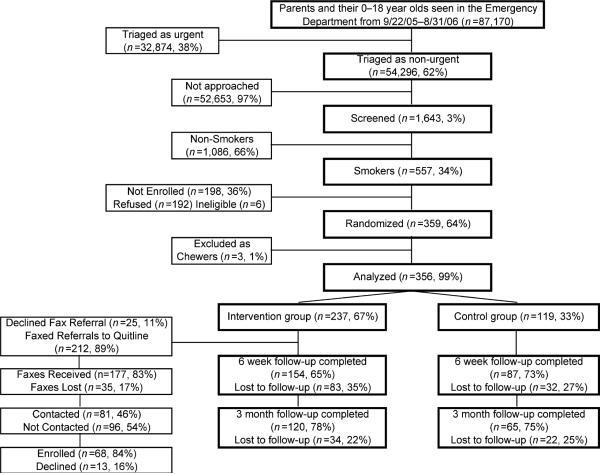
All potential participants completed a brief questionnaire including basic sociodemographic information and smoking status. A total of 1,643 adults were screened, and 557 (34%) were current smokers. Of these, 359 (64%) consented to participate in the study and were block randomized to achieve a 2:1 ratio of participants in the Intervention (n=239) versus the Usual Care Control condition (120). Participant flow is shown in Figure 1. All participants provided written informed consent, and the study was approved by the Cincinnati Children's Hospital Medical Center Institutional Review Board.
Figure 1.
Participant flow.
Assessments
The baseline assessment included sociodemo-graphics, current smoking status and history, and motivation to quit tobacco use using the Contemplation Ladder (Biener & Abrams, 1991), and intentions to quit tobacco use. Phone follow-up interviews assessing participants’ readiness to quit, quit attempts, and abstinence (e.g., “During the last 7 days, I haven't smoked at all, not even a puff” or “During the last 7 days I haven't used chew/snuff at all, not even one chew or dip”), were conducted by personnel blinded to study group assignment at 6 weeks and 3 months after the initial assessment. The primary outcome measure was repeated point prevalence at 6 weeks and 3 months post intervention (which was defined as abstinence from smoking at both 6 weeks and 3 months).
Study conditions
Participants randomized to the Intervention group were given a brief (10- to 15-minute) counseling session by the principal investigator or trained clinical research coordinator while their child was waiting to be evaluated by the emergency department physician. Participants were encouraged to quit smoking and assessed for level of readiness to quit. Participants responding positively to the question: “Would you seriously consider quitting in the next 6 months?” were given a brief description of the Ohio Quitline, and then asked about their interest in being referred to the Quitline. This time period was chosen to encourage as many participants as possible to speak with Quitline counselors trained in increasing motivation to quit.
For those participants not ready to quit in the next 6 months, study personnel used the 5Rs counseling technique to increase motivation (Fiore, et al., 2000). Then study personnel described the services offered by the Quitline and offered participants the opportunity for faxed Quitline referral. All participants not wishing to be contacted by the Quitline were offered written Ohio Quitline tobacco cessation brochures.
Usual Care Control Group participants completed the informed consent form and survey, but were not given any specific information regarding tobacco cessation. Participants in both conditions received department store gift cards at baseline (US$5), and at 6-week ($5) and 3-month follow-ups ($10) for completing the assessments.
Ohio Quitline protocol
All intervention participants agreeing to be contacted by the Quitline completed a form that was faxed by study staff to the Ohio Quitline. Counselors at the Quitline attempted to contact participants up to three times over a 7–10 day period. Contacted participants were screened for basic demographic and tobacco use information, assessed for readiness to quit, and provided stage-appropriate information and/or counseling.
The Quitline recorded the following information and provided it to the principal investigator: the number of forms received from the study; number of participants contacted; number of participants who set a quit date; number of attempts to quit; reported receipt of mailed materials; and self-reported quitting.
Analyses
Fisher's exact tests were used to compare the intervention with the usual care control group or retained vs. non-retained participants on dichotomized variables, and Student's t-tests were used to compare means for continuously scaled variables. In our primary analyses of follow-up results (quitting), we used both complete case analysis and an intention-to-treat model, with any of the original 359 participants lost to follow-up classified as smokers. Because intervention and usual care control participants differed significantly at baseline on two of our secondary outcome measures, comparisons of the groups on those measures at the 3-month follow-up were adjusted for participant's baseline measures. All significance tests were two-tailed, with an alpha of .05.
Results
Baseline characteristics
Due to the extremely low prevalence of smokeless tobacco use, our analyses were restricted to only the 356 of our original 359 participants who were smokers. We excluded the three participants (two intervention and one usual care control) who used only chew/snuff. Participants were on average 31.9 years old (SD 9.2); 281 (79%) were female, 176 (49%) were African American, 165 (46%) were Caucasian, and 18 (5%) were Asian, American Indian, or unspecified. The majority of participants (71%) had an annual income of ≤$25,000, and 26% had not completed high school. The mean score on the Contemplation Ladder was 6.1 (SD 2.3), representing the response: “I am thinking about cutting down or quitting.” The majority of participants (58%) were seriously thinking about quitting in the next 30 days, 63% had made a serious quit attempt in the past year, and 51% had been advised to quit by their physician or other health care worker. The intervention and usual care control groups did not differ significantly on any demographic variables, but did differ on two baseline measures of readiness to quit smoking. Intervention participants were more likely to report at baseline that they were seriously thinking about quitting smoking (62% vs. 48%; p=.01) and they scored higher on the baseline contemplation ladder (6.3 vs. 5.7; p=.02).
Primary outcome
Intervention participants had higher rates of quitting than did those in the usual care control group using both complete case and intent-to-treat analyses (Table 1), with the differences approaching significance for intervention participants successfully followed up at 3 months (22.5% vs. 10.8%; p<.07). In the followed sample, 6.7% of the intervention group participants had quit at both time periods, vs. 2.3% of the usual care control group participants (p=.22). In the intent to treat sample, the quit rates were 4.2% and 1.7% (p=.35).
Table 1.
Proportion of participants who reported tobacco-use cessation (point prevalence) at each assessment using intent-to-treat analysis and complete case analyses.
| Intent-to-treat analysis | |||
|---|---|---|---|
| Assessment point | Usual care control group n (%) | Intervention group n (%) | Odds ratio (95% CI) |
| 6 weeks | 4/119 (3.4) | 16/237 (6.8) | 2.08 (.68–6.4) |
| 3 months | 7/119 (5.9) | 27/237 (11.4) | 2.06 (.87–4.9) |
| 6 weeks and 3 months | 2/119 (1.7) | 10/237 (4.2) | 2.58 (.56–12.0) |
| Complete case analysis | |||
| 6 weeks | 4/87 (4.6) | 16/154 (10.4) | 2.41 (.78–7.4) |
| 3 months | 7/65 (10.8) | 27/120 (22.5) | 2.41 (.98–5.9) |
| 6 weeks and 3 months | 2/87 (2.3) | 10/150 (6.7) | 3.04 (.65–14.2) |
Secondary outcomes
Continuing smokers in the intervention group reported significantly higher rates of attempting to quit and thinking seriously about quitting, higher scores on the contemplation ladder, and fewer cigarettes smoked at 3 months than those in the usual care control group (see Table 2). Because the two groups differed at baseline on “Seriously thinking about quitting” and on the contemplation ladder, the groups were also compared at 3 months adjusting for baseline scores. In that case the difference between the groups on the contemplation ladder was reduced by 36% and became non-significant (p=.16), while the OR for “Seriously thinking about quitting” was reduced by 21% and was still significant (p=.005)
Table 2.
Secondary outcomes for participants at 3-month follow-up.
| OUTCOME | Usual care control group n (%) | Intervention group n (%) |
|---|---|---|
| At least 1 quit attempta | 20/58 (34.5%) | 55/93 (59.1%)** |
| Seriously thinking about quitting in the next 30 daysb,c | 21/57 (36.8%) | 60/88 (68.2%)† |
| Contemplation Ladder Scored (mean, SD)e | 5.30 (2.37) (n=56) | 6.2 (2.65) (n=91)* |
| Number of cigarettes smoked on a typical day | 12.8 (8.5) (N=58) | 10.1 (8.1) (N=94)* |
Note.
p<.05
p<.01
p<.001.
Denominators (58 and 93) are the numbers of usual care control and intervention subjects, respectively, completing the 3-month follow-up and who were non-quitters.
Denominators (57 and 88) are the numbers of usual care control and intervention subjects, respectively, completing the 3-month follow-up, who were non-quitters, and who responded to the query “I am seriously thinking about quitting in the next 30 days.”
After adjusting for baseline values, OR reduced 21% from 3.7 to 2.9, p=.005.
The Contemplation Ladder is a 10-point scale with higher score indicating more readiness to quit.
After adjusting for baseline value of the predictor, difference between groups dropped 36%, from 0.9 to 0.58, p=.16.
Participant retention
Study personnel were able to contact and collect completed 6-week questionnaires from approximately 68% (241) of participants at 6-week follow-up, and 52% (185) at 3-month follow-up, with the remaining lost to follow-up. The two primary reasons for being unable to reach participants by telephone were no answer, or the wrong telephone number given at baseline. Analyses indicated that at 6 weeks, those who were successfully followed vs. those who were lost to follow-up did not differ significantly on any demographic or baseline measures. However, at 3 months, the groups differed significantly on age and number of years of smoking, with those who were successfully followed being older and smoking longer than those lost to follow-up (Table 3).
Table 3.
Characteristics of participants who were and were not contacted at 6 weeks and 3 months.
| Contacted at 6 wks (n=241) | Unable to contact at 6 wks (n=115) | Contacted at 3 months (n=185) | Unable to contact at 3 months (n=171) | |
|---|---|---|---|---|
| Intervention group | 63.9% | 72.2% | 64.9% | 68.4% |
| Age (mean, SD) | 32.1 (9.6) | 31.4 (8.2) | 32.8 (10.0)* | 30.9 (8.1) |
| Female | 80.9% | 74.8% | 82.7% | 74.9% |
| Race | ||||
| White | 45.4% | 50.9% | 48.4% | 45.8% |
| Black | 52.5% | 45.5% | 50.0% | 50.6% |
| Married | 38.2% | 41.7% | 38.4% | 40.4% |
| Educ (H.S. graduate) | 71.9% | 77.4% | 72.5% | 74.9% |
| Income more than $25,000 | 27% | 33.6% | 28.2% | 30.4% |
| Years smoked (mean, SD) | 12.9 (9.2) | 11.7 (7.5) | 13.6 (9.6)* | 11.4 (7.4) |
| Cigarettes/day (mean, SD) | 16.4 (10.8) | 14.7 (11.3) | 15.9 (10.2) | 15.8 (11.8) |
| Smoke within 5 minutes of waking | 26.8% | 26.6% | 28.3% | 25.0% |
| Cravings (mean, SD)a | 3.4 (1.1) | 3.3 (1.1) | 3.4 (1.1) | 3.3 (1.1) |
| Advised to quit | 53.8% | 43.9% | 54.9% | 45.9% |
| Contemplation Ladder Score (mean, SD)b | 6.1 (2.3) | 6.1 (2.4) | 6.3 (2.2) | 5.9 (2.4) |
| Thinking about quitting | 40.6% | 46.4% | 38.3% | 47.0% |
| At least one quit attempt | 64.9% | 62.3% | 63.6% | 64.5% |
Note.
Strong cravings to smoke (1) never, (2) seldom, (3) sometimes, (4) often, (5) always.
The Contemplation Ladder is a 10-point scale with higher score indicating more ready to quit.
p<.05.
Of the referrals faxed to the Quitline, 83% (177) were received. From those received referrals, 54% (96) of participants were unreachable and 16% (13) declined enrollment. Of those contacted, 84% (68) enrolled with the Quitline, with 42 (62%) participants who requested mailed information only, and only 26 (38%) participants who enrolled in counseling from a Quitline counselor. Of those enrolled in counseling, five (19.2%) quit at 6-month follow-up by the Quitline.
Discussion
Smoking cessation counseling is one of the five preventive services that are considered inexpensive and potentially feasible in the emergency department setting; thus the Society of Academic Emergency Medicine's Public Health Task Force recommended that smoking cessation counseling be implemented in the emergency department (Irvin, Wyer, & Gerson, 2000). To our knowledge, this is the first study to assess the effectiveness of a parental tobacco cessation intervention in a pediatric emergency department setting. The quit rates in our study compare favorably to those in adult emergency department-based and pediatric outpatient trials (Richman et al., 2000; Schiebel & Ebbert, 2007; Severson, Andrews, Lichtenstein, Wall, & Akers, 1997). One randomized controlled study investigated the effectiveness of a brief tobacco cessation intervention and found equivalent quit rates of 10% in both their intervention and control groups at 3-month follow-up (Richman et al., 2000). These rates were lower than those in our complete case analysis at 3 months (10.8% vs. 22.5%; usual care control vs. intervention, respectively). Other randomized, controlled trials conducted in the pediatric outpatient setting have found significant increases in cessation rates and quit attempts compared to controls (Severson et al., 1997, Yilmaz et al., 2006).
The emergency department appears to be a viable venue for recruiting smokers. We found that a high proportion of parental smokers were very interested in quitting, with 63% reporting that they had made a serious quit attempt in the past year, and 58%, indicating that they were seriously thinking about quitting in the next 30 days. These results closely parallel other studies that examined the interest of adult emergency department patients in tobacco cessation (Boudreaux, Baumann, Friedman, & Ziedonis, 2005; Klinkhammer et al., 2005). In addition, our study population had similar Contemplation Ladder scores as compared to other studies of adult emergency department smokers (Klinkhammer et al., 2005; Bernstein & Cannata, 2006).
Participant follow-up and retention is challenging, but not an insurmountable barrier, for conducting cessation research with an emergency department population. Our overall 6-week follow-up of 68% was consistent with an adult emergency department tobacco cessation intervention that had a 3-month follow-up rate of 68% (Richman et al., 2000). Emergency department populations have been historically difficult to follow due to factors such as low social support, frequent changes of address and high geographic mobility, lack of telephones, increased caretaker stress, and lower socioeconomic status (Richman et al., 2000; Senturia et al., 1998). Factors that may result in improved contact rates in such populations may include obtaining many alternate telephone numbers and addresses for follow-up, frequent written and telephone contact with short intervals between follow-up, adequate participant reimbursement, and multiple call attempts for follow-up done at flexibly scheduled times (Janson, Alioto, & Boushey 2001; Senturia et al., 1998). Although it has been suggested that recruiting tobacco-using participants who are highly motivated to quit or who have tobacco-related illnesses may increase follow-up and cessation rates (Bock et al., 2001; Boudreaux, Baumann, Friedman, & Ziedonis, 2005; Klinkhammer et al.,), this has not been investigated in randomized controlled trials.
The state Quitline follow-up rate was lower than expected due in part to the following: (1) Quitline counselors tried only three times to contact participants, in contrast to our research coordinators who made up to 10 attempts at phone follow-up; (2) during the first few months of our study, we experienced problems with the fax referral process, and it is unclear if all faxes were properly transmitted and/or received. Once we realized that there was a discrepancy in the number of faxes we sent versus those that were received, we instituted a procedure to verify that each fax was received by the Quitline; (3) this study did not assess feasibility of conducting a 10–15 minute smoking cessation intervention in a “real world” Emergency Department setting where physicians or other health care providers, and not clinical research coordinators, would be called upon to deliver the intervention; (4) this emergency department study population is highly mobile, and Quitline counselors most commonly received no answer or reached disconnected phone numbers; and 5) we assessed readiness to quit very broadly (i.e., ready to quit within the next 6 months), and perhaps recruiting more motivated smokers (e.g., those ready to quit in the next 2 weeks or next 30 days) would have allowed Quitline staff to locate these participants more easily. However, the Quitline was able to reach 46% of faxed referrals, and 84% were willing to enroll with the Quitline. Of these participants, 62% were interested in receiving mailed information, and 38% enrolled in Quitline counseling. These rates are higher than the contact rates of 2%–3% reported for smokers who are self-referred to a Quitline (McAfee, 2002; Zhu, Cummins, & Anderson, 2002), and the rate of 6% found in the dental setting (Gordon et al., 2007). It has been demonstrated that higher reach rates by Quitline counselors can be achieved by an increased number of telephone call attempts (up to 10 times), which may be effective in reaching smokers referred from the emergency department setting as well (Gordon et al., 2007).
Our study has several potential limitations: (1) Thirty-six percent of eligible participants refused to participate, which may indicate that they did not want to participate because they did not want to quit smoking. Thus, the observed cessation rate in our study may have been higher than the true rate for all emergency department smokers. (2) Due to the low socioeconomic status of our emergency department population, we experienced a high attrition rate at follow-up. However, our attrition analyses suggest that those who did not respond did not differ from those who did on baseline variables known to be associated with tobacco-use cessation. (3) We used self-report of smoking status and not biochemically validated abstinence. (4) The study population was a convenience sample collected in a Midwestern, tertiary care, pediatric emergency department, and the majority of participants had a low socioeconomic status, which may limit the generalizability of our results.
In conclusion, the results of our pilot study suggest that further research in this area is warranted. Although the intervention model was viable, there was limited effectiveness, as quit rates only approached statistical significance in our intervention group for the full case analysis. This may have been due, in part, to low contact rates, and only a small percentage of participants received counseling from the Quitline. Even though quit rates were lower than expected, our secondary outcomes suggest that the intervention was effective in increasing quit attempts and readiness to quit. It appears that using the pediatric emergency department setting to provide tobacco cessation counseling may be most effective in helping parents to quit by regularly providing the 5As plus proactively referring only those parents who are highly motivated to be contacted by a Quitline for more intensive counseling. An estimated 7.5 million parents or guardians who smoke visit pediatric emergency departments annually (McCaig & Ly, 2002). Even with a modest cessation rate such as that reported in our intervention, the public health impact of a brief tobacco-use cessation intervention could be significant.
Acknowledgments
Supported, in part, by the Fifth Third Bank/Charlotte R.Schmidlapp Women Scholars Program. The authors report having no competing interests. The authors are grateful to Cindy Haugland and Steven Wilson at the National Jewish Medical and Research Center in Denver, Colorado, for their help in facilitating, collecting, and analyzing the Quitline data.
Contributor Information
E. Melinda Mahabee-Gittens, Division of Emergency Medicine, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, OH
Judith S. Gordon, Oregon Research Institute, Eugene, OR
Matthew E. Krugh, Division of Emergency Medicine, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, OH
Brian Henry, Division of Emergency Medicine, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, OH.
Anthony C. Leonard, Department of Public Health Sciences, University of Cincinnati Medical Center, Cincinnati, OH.
References
- Babcock Irvin C, Wyer PC, Gerson LW. Preventive care in the emergency department, Part II: Clinical preventive services–an emergency medicine evidence-based review. Society for Academic Emergency Medicine Public Health and Education Task Force Preventive Services Work Group. Acad Emerg Med. 2000 Sep;7(9):1042–54. doi: 10.1111/j.1553-2712.2000.tb02098.x. [DOI] [PubMed] [Google Scholar]
- Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. The Journal of the American Medical Association. 1994;271:1909–1912. [PubMed] [Google Scholar]
- Bernstein SL, Boudreaux ED, Cydulka RK, Rhodes KV, Lettman NA, Almeida SL, et al. Tobacco control interventions in the emergency department: A joint statement of emergency medicine organizations. Annals of Emergency Medicine. 2006;48:e417–426. doi: 10.1016/j.annemergmed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- Bernstein SL, Cannata M. Nicotine dependence, motivation to quit, and diagnosis in emergency department patients who smoke. Addictive Behaviors. 2006;31:288–297. doi: 10.1016/j.addbeh.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Bock BC, Becker B, Monteiro R, Partridge R, Fisher S, Spencer J. Physician intervention and patient risk perception among smokers with acute respiratory illness in the emergency department. Preventive Medicine. 2001;32:175–181. doi: 10.1006/pmed.2000.0799. [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Baumann BM, Friedman K, Ziedonis DM. Smoking stage of change and interest in an emergency department-based intervention. Academic Emergency Medicine. 2005;12:211–218. doi: 10.1197/j.aem.2004.09.022. [DOI] [PubMed] [Google Scholar]
- Fiore MS, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Treating tobacco use and dependence. Clinical practice guideline. U.S. Department of Health and Human Services, Public Health Service; Rockville, MD: 2000. [Google Scholar]
- Gordon JS, Andrews JA, Crews KM, Payne TJ, Severson HH. The 5A's vs 3A's plus proactive quitline referral in private practice dental offices: Preliminary results. Tobacco Control. 2007;16:285–288. doi: 10.1136/tc.2007.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janson SL, Alioto ME, Boushey HA. Attrition and retention of ethnically diverse subjects in a multicenter randomized controlled research trial. Controlled Clinical Trials. 2001;22:S36S–S243. doi: 10.1016/s0197-2456(01)00171-4. [DOI] [PubMed] [Google Scholar]
- Klinkhammer MD, Patten CA, Sadosty AT, Stevens SR, Ebbert JO. Motivation for stopping tobacco use among emergency department patients. Academic Emergency Medicine. 2005;12:568–571. doi: 10.1197/j.aem.2004.11.027. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: Rationales and meta-analytic review of evidence. Health Education Research. 1996;11:243–57. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- Lowenstein SR, Koziol-McLain J, Thompson M. Behavioral risk factors in emergency department patients: A multisite survey. Academic Emergency Medicine. 1998;5:781–787. doi: 10.1111/j.1553-2712.1998.tb02504.x. [DOI] [PubMed] [Google Scholar]
- Mahabee-Gittens M. Smoking in parents of children with asthma and bronchiolitis in a pediatric emergency department. Pediatric Emergency Care. 2002;18:4–7. doi: 10.1097/00006565-200202000-00002. [DOI] [PubMed] [Google Scholar]
- McAfee T. Increasing the population impact of Quitline.. Paper presented at The North American Conference of Smoking Cessation Quitlines; Phoenix, AZ. May, 2002. [Google Scholar]
- McCaig LF, Ly N. National hospital ambulatory medical care survey: 2000 emergency department summary: Advance data from vital and health statistics: No. 326. National Center for Health Statistics; Hyattsville, MD: 2002. [Google Scholar]
- O'Brien GM, Stein MD, Zierler S, Shapiro M, O'Sullivan P, Woolard R. Use of the ED as a regular source of care: Associated factors beyond lack of health insurance. Annals of Emergency Medicine. 1997;30:286–291. doi: 10.1016/s0196-0644(97)70163-x. [DOI] [PubMed] [Google Scholar]
- Ossip-Klein DJ, McIntosh S. Quitlines in North America: Evidence base and applications. The American Journal of the Medical Sciences. 2003;326:201–205. doi: 10.1097/00000441-200310000-00010. [DOI] [PubMed] [Google Scholar]
- Prochazka A, Koziol-McLain J, Tomlinson D. Smoking cessation counseling by emergency physicians: Opinions, knowledge, and training needs. Academic Emergency Medicine. 1995;2:211–216. doi: 10.1111/j.1553-2712.1995.tb03201.x. [DOI] [PubMed] [Google Scholar]
- Richman PB, Dinowitz S, Nashed AH, Eskin B, Sylvan E, Allegra C, et al. The emergency department as a potential site for smoking cessation intervention: A randomized, controlled trial. Academic Emergency Medicine. 2000;7:348–353. doi: 10.1111/j.1553-2712.2000.tb02235.x. [DOI] [PubMed] [Google Scholar]
- Schiebel NE, Ebbert JO. Quitline referral vs. self-help manual for tobacco use cessation in the emergency department: A feasibility study. Biomed Central Emergency Medicine. 2007;14:7–15. doi: 10.1186/1471-227X-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senturia Y, McNiff-Mortimer K, Baker D, Gergen P, Mitchell H, Joseph C, et al. Successful techniques for retention of study participants in an inner-city population. Controlled Clinical Trials. 1998;19:544–554. doi: 10.1016/s0197-2456(98)00032-4. [DOI] [PubMed] [Google Scholar]
- Severson HH, Andrews JA, Lichtenstein E, Wall M, Akers L. Reducing maternal smoking and relapse: Long-term evaluation of a pediatric intervention. Preventive Medicine. 1997;26:120–130. doi: 10.1006/pmed.1996.9983. [DOI] [PubMed] [Google Scholar]
- Stead LF, Perera R, Lancaster T. Telephone counseling for smoking cessation. Cochrane Database of Systematic Reviews. 2006;(3) doi: 10.1002/14651858.CD002850.pub2. Art. No.: CD 002850. DOI: 10.1002/14651858. CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- Winickoff JP, Hillis VJ, Palfrey JS, Perrin JM, Rigotti NA. A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: The stop tobacco outreach program. Pediatrics. 2003;111:140–145. doi: 10.1542/peds.111.1.140. [DOI] [PubMed] [Google Scholar]
- Zapka JG, Fletcher K, Pbert L, Druker SK, Ockene JK, Chen L. The perceptions and practices of pediatricians: Tobacco intervention. Pediatrics. 1999;103:e65. doi: 10.1542/peds.103.5.e65. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Anderson CM, Tedeschi GJ. Evidence of real-world effectiveness of a telephone quitline for smokers. New England Journal of Medicine. 2002;347:1087–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Cummins SE, Anderson CM. Telephone quitlines for high-risk or hard-to-reach populations.. Paper presented at The 2002 National Conference on Tobacco or Health; San Francisco, CA.. Nov, 2002. [Google Scholar]