Abstract
The concept of visual restoration via retinal prosthesis arguably started in 1992 with the discovery that some of the retinal cells were still intact in those with the retinitis pigmentosa disease. Two decades later, the first commercially available devices have the capability to allow users to identify basic shapes. Such devices are still very far from returning vision beyond the legal blindness. Thus, there is considerable continued development of electrode materials, and structures and electronic control mechanisms to increase both resolution and contrast. In parallel, the field of optogenetics—the genetic photosensitization of neural tissue holds particular promise for new approaches. Given that the eye is transparent, photosensitizing remaining neural layers of the eye and illuminating from the outside could prove to be less invasive, cheaper, and more effective than present approaches. As we move toward human trials in the coming years, this review explores the core technological and biological challenges related to the gene therapy and the high radiance optical stimulation requirement.
Keywords: Optogenetics, Visual prosthesis, Retinal prosthesis, Bionics, Visual restoration
Introduction
Treatments of blindness include pharmaceuticals, gene therapy, stem cells, and visual assistive devices. Pharmaceutical treatment strategies such as anti-vascular endothelial growth factor (VEGF) drugs for wet-age-related macular degeneration (AMD) are becoming increasingly available. Such treatments are also becoming increasingly effective in treating glaucoma, for example, prostaglandin analogs (Tomic et al., 2013), beta-adrenergic receptor antagonists (Himber et al., 1987), alpha2-adrenergic agonists (Wheeler & Woldemussie, 2001), alpha agonists (Arthur & Cantor, 2011), carbonic anhydrase inhibitors (Gugleta, 2010), and physostigmine (Gburkowa & Pojda, 1965). Nevertheless, such approaches cannot treat conditions where the underlying cause is genetic and cannot restore lost vision.
For retinal degenerations caused by mutations in a single gene, genetic therapies have shown promise in preclinical studies and early stage clinical trials (for review, see e.g., Cepko, 2012; Boye et al., 2013; Sahel & Roska, 2013 and the article on gene therapies in this issue). However, this only works in cases where the underlying gene is known and retinal dystrophies can arise due to mutations in hundreds of different genes (Daiger et al., 2013). It the long term, it may even be possible to regrow an entire new eye utilizing stem cell approaches as demonstrated in principle by Eiraku and Sasai (2012). However, these may be limited to certain conditions, and will take some time to become clinically available. As such, it is very important that we also explore prosthetic restorative strategies to our most important sensory system.
Bionic solutions to blindness have been considered for almost a century, since Förster (1929) discovered electrical stimulation of the visual cortex could elicit the perception of phosphenes. Pioneering work on visual cortical prosthesis was carried out in the 1960s by Brindley and Lewin (1968) and extended by Dobelle et al. (1974). However, the discovery of inner retinal preservation in the 1990s (Stone et al., 1992; Santos et al., 1997), combined with the relative accessibility of the eye, led to a shift in research emphasis to retinal prostheses. In addition to this article, readers may want to consider the reviews on electronic retinal prosthesis by Shepherd et al. (2013) and Picaud and Sahel (2014).
Retinal prostheses are only appropriate for photoreceptor degenerations where there is still a functional neural link to the visual cortex. Current generations of prostheses have returned limited vision and have thus only been implanted in those with late stage retinitis pigmentosa (RP) (prevalence 1:3500), who have bare light perception (Ahuja & Behrend, 2013). In the longer term, other retinopathies such as AMD, are also of interest to the prosthetic community as these are much larger communities (Weiland et al., 2011). These can be classed into nonvascular conditions such as Stargardt (Liutkeviciene et al., 2012) and dry-AMD (van Lookeren Campagne et al., 2014), and vascular conditions such as wet-AMD (de Amorim Garcia Filho et al., 2012) and diabetic retinopathies (Simo & Hernandez, 2014). The latter can now be treated with anti-VEGF pharmaceutical agents (de Amorim Garcia Filho et al., 2012; Holz et al., 2014). The former, while untreatable, rarely leads to a total loss in vision. Thus, in the majority of cases, patients may be legally blind, but still have navigation function and can use adaptive technologies to help with other activities of daily living. Any prosthetic treatment for these conditions would thus have to restore highly functional vision without damaging what currently remains. As such, RP currently remains the priority target for retinal prosthesis.
Where the retinal ganglion cells (RGCs) are destroyed, as in optic neuropathies such as glaucoma, it is no longer possibly to communicate from the eye and a deeper visual prosthesis is required. This may be in the lateral geniculate nucleus (Pezaris & Reid, 2007) or in area V1 of the visual cortex (Normann et al., 2009).
Optogenetic approaches to neuron stimulation
Classically, the electrical based neurological therapies date back almost two millennia, as Scribonius Largus used electrical shocks from torpedo fish to provide pain relief (Nutton, 1995). Many centuries later, Galvani was the first to demonstrate electrical nerve control in 1790s. But with the advent of precise electronics in the 20th century, clinical neuroprostheses became possible. The first was the heart pacemaker in 1950, followed by commercial availability of cochlear implants in the 1980s and deep brain pacemakers in the 1990s. These devices utilize electrodes which impart electrical charge into medium near nerve cells to open up electrically gated ion channels on neuron cell membranes—and thus enable information transfer or pacemaking.
Other methods of nerve control have been explored. Fork first demonstrated optical stimulation of the sciatic nerve of a rat with high power infrared lasers in 1971 (Fork, 1971). This effect could be the result of thermal activation of transient receptor potential (TRP) channels (Albert et al., 2012) or perhaps simply temperature increases changing the intermembrane diffusion relations (Li et al., 2013). Another approach is the physical release (Finlayson & Iezzi, 2010) or uncaging (Shoham et al., 2005) of neurotransmitters to create chemical or optochemical prosthesis.
In all of the above cases, there is no modification of the nervous system, only the introduction of some form of optical, chemical, or electrical stimulus. Optogenetics, in contrast, involves the genetic modification of nerve cells to become sensitive to certain wavelengths of light. There are four different methods for doing this, each with their own characteristics:
-
1.
Light sensitive ion channels
-
2.
Light sensitive charge pumps
-
3.
Light sensitive signal transduction pathways
-
4.
Genetically modified receptors to which an optically activated ligand is chemically attached.
Light sensitive proteins have been studied for many years. For example, bacteriorhodopsin, a light sensitive proton pump, was documented in 1973 (Oesterhe & Stoecken, 1973). However, the advent of neural optogenetics arguably started with the identification and expression in animal cells of channelrhodopsin-2 (ChR2) in 2003 (Nagel et al., 2003), followed by expression in neurons in 2005 (Boyden et al., 2005). The key difference was that, as ChR2 is a light sensitive cation channel, it could be used to depolarize nerve cells and thus generate action potentials.
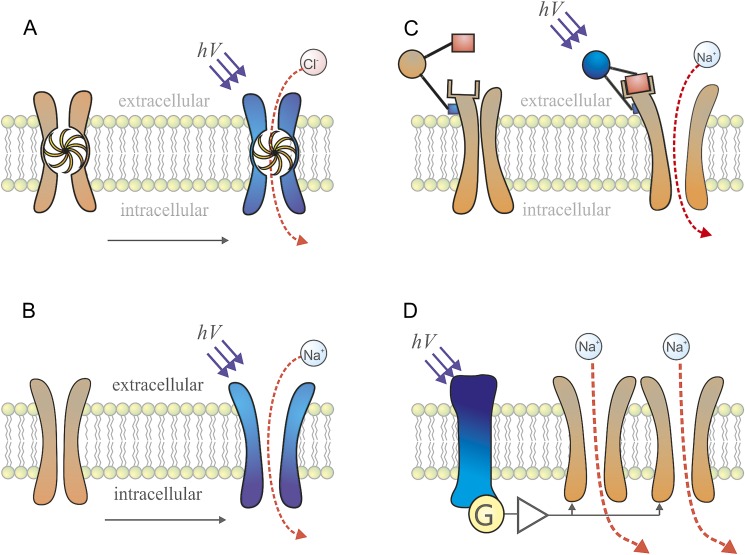
In the same period, melanopsin—a light-activated, depolarizing transduction pathway was demonstrated to optically activate mammalian cells (Barnard et al., 2004; Melyan et al., 2005). Such G-protein coupled receptor approaches are very sensitive but very slow, with response times in multiple seconds. As such, their use is now being explored for non-neuronal systems (Koyanagi et al., 2013). In 2004, the first paper demonstrating chemically assisted optogenetics was published (Banghart et al., 2004). In this case, a potassium channel was genetically modified to make it susceptible to binding to a photosensitive ligand with a plug. The channel would then remain open until light activation would extend the ligand and plug the channel. Work in this field is ongoing, but is complicated in requiring both chemical and genetic modifications. In 2007, the optogenetic repertoire was expanded with the addition of halorhodopsin (HR) (Han & Boyden, 2007), a light sensitive chloride pump. This allowed for both optical stimulation and inhibition, determined by wavelength. These different forms of optogenetics are summarized in the cartoon in Fig. 1.
Fig. 1.
Different forms of optogenetic photosensitization in conceptual form: (A) optically sensitive ion pumps such as halorhodopsin (HR); (B) optically sensitive ion channels such as channelrhodopsin-2 (ChR2); (C) ion channels genetically engineered to allow attachment of optically active chemical groups; (D) optically sensitive signal transduction pathways such as melanopsin.
Since its inception, the field of optogenetics has exploded, being adopted by neuroscience laboratories around the world to study a variety of basic science questions in numerous species. Many review articles describing the development and application of optogenetics have been published (e.g., Bernstein & Boyden, 2011; Fenno et al., 2011; Zhang et al., 2011; Mei & Zhang, 2012; Packer et al., 2013). In 2010, optogenetics was chosen as the “Method of the Year” across all fields of science and engineering by the interdisciplinary research journal Nature Methods (Nat.Meth.Editorial, 2012).
From the perspective of visual prosthesis, one of the key advantages of optogenetic approaches is the ability to achieve targeted delivery to key subcircuits. Of particular pertinence to retinal prosthesis is the specific targeting of ON bipolar cells (Lagali et al., 2008). The clinically relevant method for achieving this is via a viral expression system (Kamimura et al., 2011). Serotypes of lenti or adeno-associated viral vectors with good expression in target cells can be incorporated with genes to express particular combinations of opsins and promoters to improve cellular specificity. The most promising approaches use variants of ChR2 or HR to depolarize and hyperpolarize target cells, respectively.
Once transfected, optogenetically encoded cells require a high irradiance in order to be activated. The specific irradiance depends on expression levels, the biophysics of the opsin used and the dynamic range of signal required (Grossman et al., 2011). This requirement could impact on tissue safety—i.e., high levels of blue light could cause photochemical damage (Degenaar et al., 2009). It also limits the range of optoelectronic stimulator options to those that can provide sufficient light intensity (Grossman et al., 2010; Reutsky-Gefen et al., 2013). As will be discussed later, there are continuing efforts to improve opsin sensitivities with, for example, over 103 different opsin variants available from the Deisseroth lab, a review of which can be seen in Zhang et al. (2011). A review of the invertebrate and small mammal implementations has been given by Kos et al. (2013) CatCh-ChR2, in particular, appears to reduce the light requirement by over an order of magnitude (Kleinlogel et al., 2011).
Optogenetic photosensitization of the human eye
Much can be learned from the last two decades of effort into developing electronic retinal prostheses and it is worth highlighting their successes and challenges. Two systems have effectively been brought to market by the 2nd Sight and Retina Implant AG companies (Dorn et al., 2013; Stingl et al., 2013). But it has taken 2 decades of science and engineering research to achieve this. Key issues include:
-
•
Electrical stimulus can excite but not inhibit neurons.
-
•
Electrodes are typically larger than individual cells, and thus it is challenging to target individual cells and thus specific information pathways.
-
•
As stimulation arrays get larger, the electrodes get smaller and new materials are required to reduce electrolytic degradation and thus improve device lifetimes.
-
•
A considerable effort has been required to create an implantable package with sufficient power and information transfer.
Perhaps fundamental to all of these issues is that electronic retinal prostheses need to be implanted. They must thus be durable over many years and not cause functional loss to the surrounding tissue, and this significantly increases cost. As all healthcare providers will perform cost-benefit analyses on new products, such systems will need to provide some functional vision in return for their significant cost. It would be difficult to argue that current prostheses return truly functional vision.
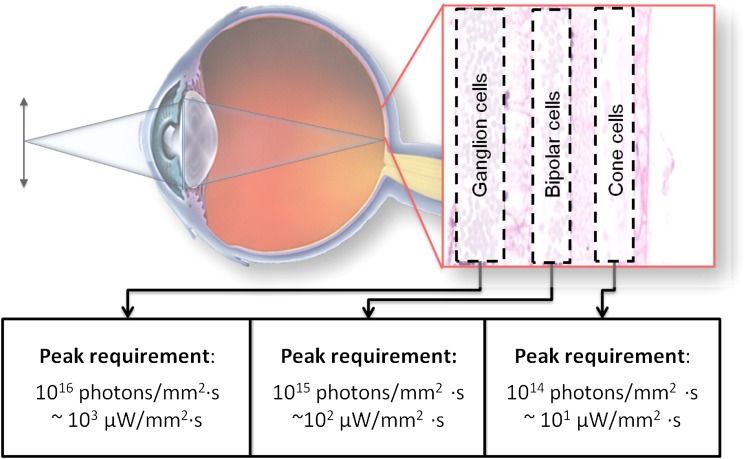
Optogenetic retinal prostheses are fundamentally different, as can be seen in Fig. 2. Clinically it would involve the injection of a viral vector to make specific cells in a target area of the remaining retina light sensitive. Then, given that the eye is transparent, the patient could wear an adapted virtual/augmented reality (AR) headset which can transmit appropriate pulses of light. No invasive surgery is required (though brain level visual prosthesis would need implantable optoelectronics). As such, the optoelectronics do not require the same level of biocompatibility and thus complex engineering as their implantable electronic counterparts. Optogenetic prosthesis should therefore be more straightforward to develop and cheaper to implement. Many of the durability problems and cellular targeting could also be overcome. Obtaining high resolution should simply be a matter for increasing the resolution of a high brightness display and developing appropriate optics.
Fig. 2.
Optogenetic visual prosthesis concept. One of the remaining layers of the retina is photosensitized, and a high radiance image is projected via the eye’s optics. The photon peak requirements for RGCs have been taken from Bi et al. (2006), for bipolar cells from Lagali et al. (2008), and for cone cells from Busskamp et al. (2010). The requirement was taken as the intensity 256 (8-bit) times the minimum effective threshold turn on, so as to give grayscale dynamic range to normal display technology.
As with any new technique, optogenetics is not without its own challenges. There are two major ethical and safety hurdles to overcome. There are the ethical issues surrounding human genetic engineering and the possible toxicity of the viral vectors used. Preclinical and early-stage clinical trials of gene therapies for various retinal disorders have largely not reported any adverse effects of retinal transfection (Boye et al., 2013). Two groups have shown long-term (over one year) expression of ChR2 in rodent retinas without serious adverse effects (Ivanova & Pan, 2009; Sugano et al., 2011). Taken together, these findings are encouraging for the safety of optogenetic retinal prostheses, although safety data from larger mammals, particularly nonhuman primates, are still lacking. Moreover, one study in mice found (Sugano et al., 2011) abnormal morphology and connectivity associated with long-term, high-level expression of ChR2 in the cortex (Miyashita et al., 2013). However, viral transfection—as would be used in clinical application—was associated with lower rates of abnormalities and the functional consequences of these abnormalities, if any, are unknown at present. If long-term optogene expression has similar consequences in the retina, it may not be an issue given the extensive remodeling that takes place in the degenerating retina anyway (Marc et al., 2003), but it emphasizes the necessity of ensuring transgene expression is restricted to the retina and, particularly in the case of RGC targeting prosthetics, that it does not spread to higher brain areas.
Assuming that in the coming years the fundamental ethical and safety challenges can be overcome, there are three major technical challenges. The opsins need to be improved to provide better photosensitivity—thus reducing the light requirement (Grossman et al., 2011). Vectors need to be developed to target key layers and cells of the retina. Finally, an efficient optoelectronic headset is required with a high radiance.
The earliest attempt at an optogenetic retinal prosthesis was by Bi et al. (2006), wherein they transfected rd1 mouse retinas with ChR2. Expression was retina-wide, although primarily in the RGCs, and they were able to elicit action potentials and visual-evoked potentials (VEPs) in the cortex. These results were extended to the Royal College of Surgeons rat by Tomita et al. (2007), who were also able to record VEPs as well as optomotor responses (Tomita et al., 2009, 2010). Since then, a number of other groups have achieved similar results in various models of retinal degeneration using a variety of different opsins, promoters, and expression techniques (Lagali et al., 2008; Lin et al., 2008; Zhang et al., 2009; Busskamp et al., 2010; Thyagarajan et al., 2010; Doroudchi et al., 2011; Nirenberg & Pandarinath, 2012). These approaches can be separated based on a number of key decisions, two of which in particular are described in more detail below.
Choice of target cell population
The retina is a layered structure and visual information flows from the photoreceptors in the outermost layer, through the inner retina where it undergoes various processing, before finally reaching the ganglion cell layer, where RGCs encode information and pass it along to higher visual areas. In principle, it would be best to intervene as early as possible in the visual pathway, i.e., in the photoreceptors. RP—the key target of retinal prosthesis—causes inactivation and degeneration of the rod cells. This in turn causes degeneration of cone cells (Santos et al., 1997). However, these cone cells are not necessarily completely destroyed. They lose their outer segments and survive until very late stages of the condition.
In 2010, Busskamp et al. (2010) demonstrated photosensitization of mouse cone cell inner segments by transfecting them with HR. HR is a better choice than ChR2 as the cones are normally depolarized in the dark and hyperpolarize in response to light. Photon fluxes of around 1014 photons/mm2 s (10 µW/mm2) for 5–10 ms were required to evoke strong responses.
The chief drawback of targeting the photoreceptors is the low number of surviving cells to transfect (Stone et al., 1992; Santos et al., 1997). In late stages of RP in particular, the surviving cones are primarily in the macula (Milam et al., 1998). As such, high resolution vision can be restored, but it will be restricted to tunnel vision akin to mid-stage RP. Additionally, in late stages of other retinal dystrophies there may be no surviving photoreceptors detectable via optical coherence tomography (which is likely to be an important diagnostic tool for determining patients' suitability for optogenetic prostheses), whereas the inner retina is largely intact (Jacobson et al., 2013).
Given the relative preservation of the inner retina and in keeping with the idea of intervening as far upstream as possible, the next best cell population to target is the bipolar cells. These cells are important in creating the centre–surround spatial organization of retinal receptive fields. Thus bipolar cells come in ON and OFF varieties, respectively depolarizing and hyperpolarizing in response to light. Expressing the same opsin in both populations would cause conflicting responses to visual stimulation and so may not elicit useful percepts. Two groups have attempted to circumvent this problem by targeted expression of ChR2 only to ON bipolar cells in rd1 (Lagali et al., 2008) as well as rd6 and rd10 (Doroudchi et al., 2011) mice, with encouraging results. In the case of the former, with wild type ChR2, 1015 photons/mm2 s (100 µW/mm2) were required to elicit strong responses. However, with advanced forms of ChR2 such as CatCh (Kleinlogel et al., 2011), and perhaps better expression, this could be brought down significantly.
A key issue with the inner layers of the retina is the anatomical remodeling and physiological dysfunction that occurs subsequent to photoreceptor loss in retinal degenerations (Marc et al., 2003; Stasheff, 2008; Stasheff et al., 2011). In particular, extensive pathological connectivity arises and strong oscillatory field potentials develop, accompanied by spontaneous bursting activity. It seems unlikely that normal retinal processing would remain intact in the presence of such remodeling and the signal-to-noise ratio of any signal passing through the retina will be diminished by the spontaneous activity (Toychiev et al., 2013). Previous work suggests that certain features of retinal processing, such as centre–surround receptive field organization and direction selectivity, are relatively preserved despite the remodeling, at least for simple stimuli (Lagali et al., 2008; Busskamp et al., 2010). Whether these results hold for more sophisticated stimuli remains to be seen.
Alternatively, it is possible to bypass the degenerated inner retina and target the RGCs directly (Thyagarajan et al., 2010; Tomita et al., 2010; Nirenberg & Pandarinath, 2012). Thyagarajan et al. (2010) found poor results with nonselective expression of ChR2 in RGCs, perhaps because their approach abolishes the distinction between ON and OFF pathways (Doroudchi et al., 2011). Another possibility is that the visual scene has already undergone considerable processing before reaching the RGCs, so to effectively stimulate the retina using this approach requires replicating this processing prior to stimulation. To test this, Nirenberg and Pandarinath (2012) stimulated blind mouse retinas expressing ChR2 under the same promoter used by Thyagarajan et al. (2010) with natural images processed by a simple computational model of retinal encoding. They also presented the same images, without preprocessing, to wild-type retinas and trained a decoder to match retinal population responses to images. The decoder achieved nearly identical performance when tested on wild-type RGC responses and on RGC responses evoked by their optogenetic system.
Choice of opsin and promoter
As discussed previously, there are a variety of optogenetic proteins available. One major distinction is between excitatory proteins, such as ChR2, and inhibitory proteins such as HR and ArchR. The decision whether to use an excitatory or inhibitory opsin is driven largely by what type of activity one wishes to evoke, for example, ChR2 for ON responses and HR for OFF responses (or photoreceptor responses, as described above). One or multiple opsins could be expressed in distinct cell populations or two opsins could be evoked in the same cells and different wavelengths of light used to evoke ON, OFF, and ON-OFF responses (Zhang et al., 2009). This latter approach could in principle provide color opponency using ambient light or luminance information using a stimulator that takes the derivative of the incoming image and passes information about light increments in the blue (ChR2) channel and decrements in the red (HR) channel.
An even more sophisticated approach targets ChR2 and HR separately to the soma and dendrites of RGCs (or vice versa) in order to recreate the centre–surround organization of healthy RGCs (Greenberg et al., 2011). Innovative though these approaches are, so far neither group has presented behavioral data to show they are superior to simpler approaches involving a single opsin and promoter.
Most previous work in retinal optogenetics has used classic versions of the relevant opsins, but since their initial discovery, a multitude of new varieties with altered kinetics, mechanisms of action, and spectral sensitivities have been engineered (see above). ChR2 can be modeled in terms of light and dark adaptation with lower performing and inactive states in the light adapted form (Nikolic et al., 2009). Increasing stimulation reduces those channels available for further stimulation and it is thus difficult to achieve neural firing frequencies beyond 40 Hz (Grossman et al., 2011). Attempting to drive encoded neurons faster would simply lead to dropped action potentials. Faster ChR2 variants such as ChIEF (Lin et al., 2009) and ChETA (Gunaydin et al., 2010) allow for firing rates up to 200 Hz. Such improved frequency response could enable more precise control of retinal activity with higher temporal resolution, which would be particularly useful for RGC-targeting prostheses that attempt to mimic natural retina spiking patterns (Nirenberg & Pandarinath, 2012).
Another problem with classic optogenetic proteins, especially ChR2, is their relative insensitivity to light. Furthermore, the frequency studies above showed a strong correlation between irradiance and frequency response. Thus, irradiance significantly beyond threshold is required to achieve full dynamic range. This in turn makes it challenging for the optoelectronics and can surpass phototoxicity safety limits in the eye (Degenaar et al., 2009).
Altering the channel permeability to permit Ca2+ ion flux as well as monovalent cations, as in CatCh (Kleinlogel et al., 2011), greatly improves the light sensitivity without sacrificing speed. However, detailed studies will need to be made to check for any long term calcium-mediated excitotoxicity to cells during prolonged stimulation. An alternative strategy for dealing with light insensitivity is to use red-shifted channelrhodopsin variants such as VChR and C1V1. Photochemical toxicity falls exponentially with decreasing photon energy (i.e., longer wavelengths). As such, changing the stimulation wavelength from 470 nm (2.64 eV) to 590 nm (2.11 eV) changes the safe irradiance limit by two orders of magnitude (Degenaar et al., 2009). Early red-shifted variants (Mattis et al., 2012) were not as sensitive as some advanced blue variants, but both the sensitivity and response kinetics have improved with more recent red-shifted variants such as ReaChR (Lin et al., 2013).
In summary, the variety of optogenetic tools available allows considerable scope for improving existing optogenetic retinal prosthetic approaches, but each comes with its own caveats and trade-offs. It could be that the challenges in developing fast and efficient opsins may also face challenges with immune rejection. As such, melanopsin—a light sensitive signaling transduction cascade could offer an alternative. As most prior work in this area has used wild-type variants, it remains to be seen whether and how novel opsins can lead to improved retinal prosthetic strategies. Some demonstrations on animal models have been achieved (Lin et al., 2008), but they would need significant fundamental alteration to speed up their kinetics from multiple seconds to milliseconds. Nevertheless, as their TRP channels already exist on the membrane of cells in the human retina, a long-term immune response would not be expected from their use.
The optoelectronic headset
In the late 1960s, virtual reality systems were created for the American airforce. These consisted of headsets which projected a virtual world into the user's eyes. In the 1990s, consumer versions were made, though with little commercial success. Now, with developments in various mobile technologies, there has been a resurgence in the field with major companies such as Google creating systems. The particular interest is in AR—projecting synthetic information over the real visual scene. Such AR is actually very similar to what is required for optogenetic retinal prosthesis. There needs to be an image acquisition system (camera), some form of image and retinal processing, a high intensity display, and an optical projection system to the retina. It all needs to fit into a wearable headset and operate under battery power for the course of a day. Much can be taken from existing commercial systems, but the display radiance and processing requirements are significantly different from existing AR systems.
Light stimulation systems
The in vivo studies in recent years described above give a requirement of 1012/mm2 photons or 0.4 µJ/mm2 over a period of 10 ms. This is less than the original in vitro requirement of 10 µJ/mm2 but still challenging for current display systems. When optical efficiencies are taken into account, display brightness' of 100–500,000 cd/m2 are required, when typical liquid crystal (LCD) or organic light emitting diode displays emit around 1000 cd/m2 (Degenaar et al., 2009). Realizing what is in effect a high brightness display can be achieved by either creating a singular intense beam which is then spatially patterned, raster scanning beam of light across the target, or by creating an array of microemitters.
Spatial light modulation is common in consumer projection systems for presentations. Typically, many will have a high brightness tungsten lamp with light shining through a liquid crystal screen (LCD), or reflected off either micromirror array (DLP—digital light processing) or reflective liquid crystal array (LCoS—liquid crystal on silicon). The light is then imaged onto the final target. Bright regions are simply those that have allowed all the light through, whereas dark regions have had their pixels attenuated. Some researchers have also adapted such displays for in vitro optical neural stimulation. As tungsten lamps are very inefficient, and most light is wasted by the attenuation system, such systems are not directly scalable to battery-powered retinal prosthesis headsets. Compact laser or high luminance light emitting diode (LED) systems can significantly reduce the energy cost and can be combined into compact packages for head-mounted displays. But there is still an issue with light wastage and thus battery life.
Laser scanning is akin to the old style CRT televisions where an electron beam was scanned across a phosphor surface to create an image. In the case of a laser, mechanical or electro-optical modulators can be used to scan the beam and deflect it off the image for dark areas. The efficiency is thereby the same as for LED/laser-DLP systems. An alternative approach involves computer generated holography that recently has been successfully used for in vitro patterned neuronal stimulation (Reutsky-Gefen et al., 2013). Holography should in theory be considerably more efficient than DLP projection, as it should utilize most of the light, although the processing requirement is increased in order to perform real-time hologram computation.
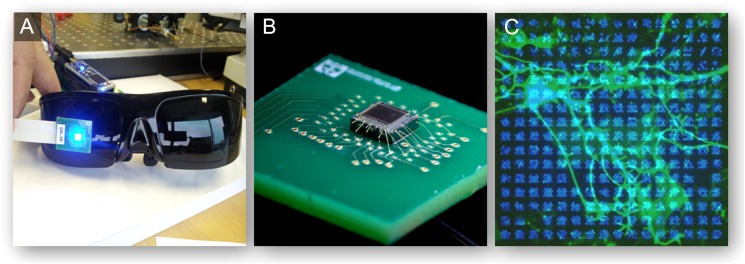
The alternative to laser projection is to utilize high power LED arrays as shown in Fig. 3. Light in LEDs is produced when positive and negative charge carriers combine to form a photon. Increasing the charge carrier concentration can therefore increase the light output. However, there are limits for given architectures and semiconductor materials. As such, gallium nitride is presently the platform of choice for much of the present white and blue high brightness LED light sources. For the purpose of retinal prosthesis, these high brightness LEDs can be patterned into arrays of µLEDs to form a display. Such systems have been demonstrated in papers by our team (Grossman et al., 2010), incorporating CMOS controllers, gallium nitride µLEDs (McGovern et al., 2010), and microlenses (Chaudet et al., 2013), and can be seen in Fig. 3. The advantage of such systems is that they are directly emissive, only producing the required light and each pixel directly correlating to required stimulus point. The challenge is that such technology is not as mature as for DLP systems and still needs development.
Fig. 3.
High brightness gallium nitride micro-LED arrays for retinal prosthesis. (A) Modules which are scalable to an existing head-mounted display system; (B) the electronic module; (C) an illuminated array on in vitro culture.
Processing requirements
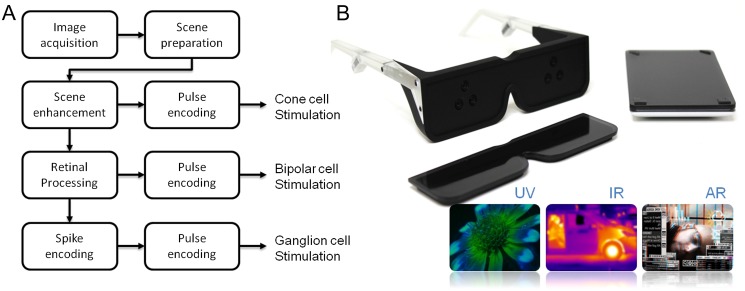
The holy grail of optogenetic retinal prosthesis research would be a particular combination of opsins and promoters that, when transfected, restores normal or near-normal vision using only ambient light. However, between cell death, inner retinal remodeling, imperfect transgenic expression, reaching this goal at least in the initial iterations of retinal prosthesis is unlikely. Hence, there will be a need to modify the visual information to maximize the useful information content transmitted to the patient. Furthermore, depending on the target cell population, some form of retinal processing will be required in addition to standard display encoding and pulse modulation. This is summarized in Fig. 4.
Fig. 4.
Visual prosthesis coding stream. (A) The visual encoding requirement depending on which cell type is being stimulated (adapted from Al-Atabany et al. (2013)); (B) in the future it may also be possible to explore imaging of additional wavelengths and integration of AR concepts (taken from Song of the Machine (Jain et al., 2011)).
The first stage is the same for any AR system. A camera acquisition system needs to send visual information to the display at high speed without significant lag. Furthermore, automatic gain control, contrast and basic image enhancement techniques that exist in most mobile camera systems need to be performed. One of the problems that plagued early virtual reality was induced motion sickness (LaViola, 2000; Nichols and Patel, 2002). Initially, it was thought that it correlated to significant time lags between the head position and the display position, coupled with motion blur. More recent studies however indicate that users can adapt to time lags of up to 200 ms (Moss et al., 2011), though this would be undesirable from an aesthetic perspective. To reduce motion blur, the commonly accepted video rate is 25 frames per second. High end displays are considerably faster, up to hundreds of Hertz, but acquiring data from imaging chips at such high speeds reduce their signal-to-noise ratio. This can affect performance under poorer lighting.
The second stage is to enhance the useful information provided to the user. If the target cell group to be photosensitized is the degenerated cone cells, then the returned sight will be a tunnel vision. If bipolar cells or RGCs are targeted, then (without a fovea) contrast sensitivity and resolution may be poor. The returned sight could therefore be akin to that of someone with mid-stage RP or AMD, respectively. For tunnel vision, dynamic scene compression techniques could be used to nonlinearly spatially compress the visual scene such that non-important features are compressed leaving important features the same size (Al-Atabany et al., 2010b; Al-Atabany et al., 2013). For poor visual acuity and contrast sensitivity, cartoonization of the visual scene whereby non-important textures are compressed could improve the contrast and thus the clarity of the transmitted scene (Al-Atabany et al., 2010a; Al-Atabany et al., 2013).
The third stage is to take into account any retinal processing which is bypassed by the prosthesis and the effects of any remodeling. The retina is not simply a camera. It is the first stage in a system to understand the world and as such extracts particular stimulus features (Gollisch & Meister, 2010), which are sent to the visual cortex for higher level analysis. As a computational system it is particularly tractable for analysis and modeling (Meister & Berry Ii, 1999). Consequently, there is a vast literature on computational models of retinal processing and encoding. These range from the extremely simple, such as the classic difference-of-Gaussians (DoG) model of the RGC receptive field (Rodieck, 1965) to highly detailed compartmental models of specific retinal circuits (for example, see Escobar et al., 2013 for a review of such models pertaining specifically to direction selectivity). Lying somewhere in between these is the linear–nonlinear (LN) model employed by Nirenberg and Pandarinath (2012), which comprises a linear filter kernel followed by a static nonlinearity (Chichilnisky, 2001; Paninski, 2004; Paninski et al., 2007) and is considered in some circles as a ‘standard model’ of retinal computation (Carandini et al., 2005). Such models become increasingly important with increasing resolution as transferred images move from simple lines and shapes to complex features.
The key issue with all of these models is the trade-off between quality and accuracy and computational complexity. Too complex, and the required processing could no longer be performed in real time by portable processing units. Models like the DoG can be implemented using computationally cheap convolution methods and are often employed by the retinomorphic engineering community (e.g., Mead & Mahowald, 1988; Banks et al., 2005; Martínez et al., 2009). Models like the LN cascade (Nirenberg & Pandarinath, 2012) could be calculated efficiently if tight constraints are placed on the processing boundaries. Otherwise the complexity scales linearly with the number of neurons simulated.
Finally, a pulse encoding scheme is required to emulate signal intensity. In many display systems, it is problematic to implement analog range controls per pixel. Mismatch between transistor properties would inevitably lead to large variations in intensity. Also in some systems (e.g., DLP), the light beam either points to its target or is deflected away. Thus, intensity modulation is via pulses of light of a fixed intensity. The longer the pulse, the greater the intensity. Such pulse width modulation could be combined with the biophysics of the channelrhodopsin, i.e., if dark adapted a shorter pulse may be sufficient and vice versa for light adapted (Grossman et al., 2011).
Since the late 1980s the neuromorphic community has suggested silicon chips with fixed retinal architectures as a solution to achieve high speed processing at ultra low power (Mead & Mahowald, 1988; Banks et al., 2005). These may even be combined with the optoelectronic stimulator in a single pipelined chip (Huang et al., 2009). In more recent years, the power of mobile graphics processors is increasingly allowing the powerful computation required for retinal prosthesis, with battery life measured in hours. Such systems have the added benefit of being programmable and thus being adjustable and responsive to the individual's preference. They will continuously improve in the coming years with the increasing interest in AR.
Future perspectives
In the coming few years, we will see the first human optogenetic trials. It is no coincidence that this will be performed for retinal prosthesis prior to other conditions. The human eye is transparent, removing requirements for implantation. In addition, should there be an immune response, the removal of the eye of a blind individual will not cause any further functional loss. Nevertheless, there are serious challenges. RGCs project to the brain, so in the first instance, these are unlikely to be targeted, lest there is an immune response in the brain itself. Should there be such a response, it might considerably delay progress in the field until non-immunogenic alternatives are found. Despite these unknowns, optogenetic approaches to retinal prosthesis hold the potential to bring back significantly improved vision—in particular foveal vision (not possible with electronic approaches). It can also be implemented at significantly lower cost compared to electronic approaches. If we consider the cost of intravitreal injections for macular degeneration, and the cost of AR headwear, then perhaps such systems could be at least an order of magnitude less expensive than their implantable counterparts.
Finally, as systems become more advanced and commonplace, but not yet returning full vision, there will be scope for user interface development. Visual enhancement techniques, utilizing potentially even infrared and UV wavelengths beyond normal vision, could provide benefit. The effect of popular culture interestingly is also playing a part. The success of the 2009 Avatar film revitalized interest in 3D head-mounted displays and the success of smartphone technology did the same for AR. Advances in both technologies, largely driven by consumer interests rather than academic research, will in turn spur improvements in optogenetic prosthesis headset design.
References
- Ahuja A.K. & Behrend M.R. (2013). The Argus (TM) II retinal prosthesis: Factors affecting patient selection for implantation. Progress in Retinal and Eye Research 36, 1–23 [DOI] [PubMed] [Google Scholar]
- Al-Atabany W., McGovern B., Mehran K., Berlinguer-Palmini R. & Degenaar P. (2013). A processing platform for optoelectronic/optogenetic retinal prosthesis. IEEE Transactions on Biomedical Engineering 60, 781–791 [DOI] [PubMed] [Google Scholar]
- Al-Atabany W.I., Memon M.A., Downes S.M. & Degenaar P.A. (2010a). Designing and testing scene enhancement algorithms for patients with retina degenerative disorders. Biomedical Engineering Online 9, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Atabany W.I., Tong T. & Degenaar P.A. (2010b). Improved content aware scene retargeting for retinitis pigmentosa patients. Biomedical Engineering Online 9, 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert E.S., Bec J.M., Desmadryl G., Chekroud K., Travo C., Gaboyard S., Bardin F., Marc I., Dumas M., Lenaers G., Hamel C., Muller A. & Chabbert C. (2012). TRPV4 channels mediate the infrared laser-evoked response in sensory neurons. Journal of Neurophysiology 107, 3227–3234 [DOI] [PubMed] [Google Scholar]
- Arthur S. & Cantor L.B. (2011). Update on the role of alpha-agonists in glaucoma management. Experimental Eye Research 93, 271–283 [DOI] [PubMed] [Google Scholar]
- Banghart M., Borges K., Isacoff E., Trauner D. & Kramer R.H. (2004). Light-activated ion channels for remote control of neuronal firing. Nature Neuroscience 7, 1381–1386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks D.J., Degenaar P. & Tournazou C. (2005). Distributed current-mode image processing filters. Electronics Letters 41, 1201–1202 [Google Scholar]
- Barnard A.R., Appleford J.M., Sekaran S., Chinthapalli K., Jenkins A., Seeliger M., Biel M., Humphries P., Douglas R.H., Wenzel A., Foster R.G., Hankins M.W. & Lucas R.J. (2004). Residual photosensitivity in mice lacking both rod opsin and cone photoreceptor cyclic nucleotide gated channel 3 α subunit. Visual Neuroscience 21, 675–683 [DOI] [PubMed] [Google Scholar]
- Bernstein J.G. & Boyden E.S. (2011). Optogenetic tools for analyzing the neural circuits of behavior. Trends in Cognitive Sciences 15, 592–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi A., Cui J., Ma Y.P., Olshevskaya E., Pu M., Dizhoor A.M. & Pan Z.H. (2006). Ectopic expression of a microbial-type rhodopsin restores visual responses in mice with photoreceptor degeneration. Neuron 50, 23–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyden E.S., Zhang F., Bamberg E., Nagel G. & Deisseroth K. (2005). Millisecond-timescale, genetically targeted optical control of neural activity. Nature Neuroscience 8, 1263–1268 [DOI] [PubMed] [Google Scholar]
- Boye S.E., Boye S.L., Lewin A.S. & Hauswirth W.W. (2013). A comprehensive review of retinal gene therapy. Molecular Therapy 21, 509–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brindley G.S. & Lewin W.S. (1968). The sensations produced by electrical stimulation of the visual cortex. Journal of Physiology 196, 479–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busskamp V., Duebel J., Balya D., Fradot M., Viney T.J., Siegert S., Groner A.C., Cabuy E., Forster V., Seeliger M., Biel M., Humphries P., Paques M., Mohand-Said S., Trono D., Deisseroth K., Sahel J.A., Picaud S. & Roska B. (2010). Genetic reactivation of cone photoreceptors restores visual responses in retinitis pigmentosa. Science 329, 413–417 [DOI] [PubMed] [Google Scholar]
- Carandini M., Demb J.B., Mante V., Tolhurst D.J., Dan Y., Olshausen B.A., Gallant J.L. & Rust N.C. (2005). Do we know what the early visual system does?. The Journal of Neuroscience 25, 10577–10597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepko C.L. (2012). Emerging gene therapies for retinal degenerations. The Journal of Neuroscience 32, 6415–6420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudet L., Neil M., Degenaar P., Mehran K., Berlinguer-Palmini R., Corbet B., Maaskant P., Rogerson D., Lanigan P., Bamberg E. & Roska B. (2013). Development of optics with micro-LED arrays for improved opto-electronic neural stimulation. Proceedings of the SPIE 8586, Optogenetics: Optical Methods for Cellular Control,85860R [Google Scholar]
- Chichilnisky E.J. (2001). A simple white noise analysis of neuronal light responses. Network 12, 199–213 [PubMed] [Google Scholar]
- Daiger S.P., Sullivan L.S. & Bowne S.J. (2013). RetNet
- de Amorim Garcia Filho C.A., Penha F.M. & de Amorim Garcia C.A. (2012). Wet-amd treatment: A review in the anti-vegf drugs. Revista Brasileira De Oftalmologia 71, 63–69 [Google Scholar]
- Degenaar P., Grossman N., Memon M.A., Burrone J., Dawson M., Drakakis E., Neil M. & Nikolic K. (2009). Optobionic vision—a new genetically enhanced light on retinal prosthesis. Journal of Neural Engineering 6, 035007. [DOI] [PubMed] [Google Scholar]
- Dobelle W.H., Mladejovsky M.G. & Girvin J.P. (1974). Artificial vision for the blind: Electrical stimulation of visual cortex offers hope for a functional prosthesis. Science 183, 440–444 [DOI] [PubMed] [Google Scholar]
- Dorn J.D., Ahuja A.K., Caspi A., da Cruz L., Dagnelie G., Sahel J.A., Greenberg R.J. & McMahon M.J. (2013). The detection of motion by blind subjects with the epiretinal 60-electrode (Argus II) retinal prosthesis. JAMA Ophthalmology 131, 183–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doroudchi M.M., Greenberg K.P., Liu J., Silka K.A., Boyden E.S., Lockridge J.A., Arman A.C., Janani R., Boye S.E., Boye S.L., Gordon G.M., Matteo B.C., Sampath A.P., Hauswirth W.W. & Horsager A. (2011). Virally delivered channelrhodopsin-2 safely and effectively restores visual function in multiple mouse models of blindness. Molecular Therapy 19, 1220–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiraku M. & Sasai Y. (2012). Mouse embryonic stem cell culture for generation of three-dimensional retinal and cortical tissues. Nature Protocols 7, 69–79 [DOI] [PubMed] [Google Scholar]
- Escobar M.J., Pezo D. & Orio P. (2013). Mathematical analysis and modeling of motion direction selectivity in the retina. Journal of Physiology Paris 107, 349–359 [DOI] [PubMed] [Google Scholar]
- Fenno L., Yizhar O. & Deisseroth K. (2011). The development and application of optogenetics. Annual Review of Neuroscience 34, 389–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson P.G. & Iezzi R. (2010). Glutamate stimulation of retinal ganglion cells in normal and S334ter-4 rat retinas: A candidate for a neurotransmitter-based retinal prosthesis. Investigative Ophthalmology & Visual Science 51, 3619–3628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fork R.L. (1971). Laser stimulation of nerve cells in aplysia. Science 171, 907–908 [DOI] [PubMed] [Google Scholar]
- Förster O. (1929). Beiträge zur Pathophysiologie der Sehbahn und der Sehsphare. Journal für Psychologie und Neurologie 39, 463–485 [Google Scholar]
- Gburkowa A. & Pojda S.M. (1965). Clinical observations on the use of demecarium bromide in glaucoma. Pharmacologic properties of demecarium and physostigmine in experiments. Klinika Oczna 35, 207–212 [PubMed] [Google Scholar]
- Gollisch T. & Meister M. (2010). Eye smarter than scientists believed: Neural computations in circuits of the retina. Neuron 65, 150–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg K., Pham A. & Werblin F. (2011). Differential targeting of optical neuromodulators to ganglion cell soma and dendrites allows dynamic control of center-surround antagonism. Neuron 69, 713–720 [DOI] [PubMed] [Google Scholar]
- Grossman N., Nikolic K., Toumazou C. & Degenaar P. (2011). Modeling study of the light stimulation of a neuron cell with channelrhodopsin-2 mutants. IEEE Transactions on Biomedical Engineering 58, 1742–1751 [DOI] [PubMed] [Google Scholar]
- Grossman N., Poher V., Grubb M.S., Kennedy G.T., Nikolic K., McGovern B., Berlinguer Palmini R., Gong Z., Drakakis E.M., Neil M.A., Dawson M.D., Burrone J. & Degenaar P. (2010). Multi-site optical excitation using ChR2 and micro-LED array. Journal of Neural Engineering 7, 16004. [DOI] [PubMed] [Google Scholar]
- Gugleta K. (2010). Topical carbonic anhydrase inhibitors and visual function in glaucoma and ocular hypertension. Current Medical Research and Opinion 26, 1255–1267 [DOI] [PubMed] [Google Scholar]
- Gunaydin L.A., Yizhar O., Berndt A., Sohal V.S., Deisseroth K. & Hegemann P. (2010). Ultrafast optogenetic control. Nature Neuroscience 13, 387–392 [DOI] [PubMed] [Google Scholar]
- Han X. & Boyden E.S. (2007). Multiple-color optical activation, silencing, and desynchronization of neural activity, with single-spike temporal resolution. PLoS One 2, e299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himber J., Sallee V.L., Andermann G., Bouzoubaa M., Leclerc G. & De Santis L. (1987). Effects of topically applied falintolol: A new beta-adrenergic antagonist for treatment of glaucoma. Journal of Ocular Pharmacology 3, 111–120 [DOI] [PubMed] [Google Scholar]
- Holz F.G., Schmitz-Valckenberg S. & Fleckenstein M. (2014). Recent developments in the treatment of age-related macular degeneration. The Journal of Clinical Investigation 124, 1430–1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Drakakis E.M., Degenaar P. & Toumazou C. (2009). A CMOS image sensor with light-controlled oscillating pixels for an investigative optobionic retinal prosthesis system. Microelectronics Journal 40, 1202–1211 [Google Scholar]
- Ivanova E. & Pan Z-H. (2009). Evaluation of the adeno-associated virus mediated long-term expression of channelrhodopsin-2 in the mouse retina. Molecular Vision 15, 1680–1689 [PMC free article] [PubMed] [Google Scholar]
- Jacobson S.G., Sumaroka A., Luo X. & Cideciyan A.V. (2013). Retinal optogenetic therapies: Clinical criteria for candidacy. Clinical Genetics 84, 175–182 [DOI] [PubMed] [Google Scholar]
- Jain A., Arden J. & Degenaar P. (2011). Song of the Machine. http://vimeocom/22616192 [Google Scholar]
- Kamimura K., Suda T., Zhang G. & Liu D. (2011). Advances in gene delivery systems. Pharmaceutical Medicine 25, 293–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinlogel S., Feldbauer K., Dempski R.E., Fotis H., Wood P.G., Bamann C. & Bamberg E. (2011). Ultra light sensitive and fast neuronal activation with the Ca(2)+-permeable channelrhodopsin CatCh. Nature Neuroscience 14, 513–518 [DOI] [PubMed] [Google Scholar]
- Kos A., Loohuis N.F.O., Glennon J.C., Celikel T., Martens G.J.M., Tiesinga P.H. & Aschrafi A. (2013). Recent developments in optical neuromodulation technologies. Molecular Neurobiology 47, 172–185 [DOI] [PubMed] [Google Scholar]
- Koyanagi M., Takada E., Nagata T., Tsukamoto H. & Terakita A. (2013). Homologs of vertebrate Opn3 potentially serve as a light sensor in nonphotoreceptive tissue. Proceedings of the National Academy of Sciences of the United States of America 110, 4998–5003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagali P.S., Balya D., Awatramani G.B., Münch T.A., Kim D.S., Busskamp V., Cepko C.L. & Roska B. (2008). Light-activated channels targeted to ON bipolar cells restore visual function in retinal degeneration. Nature Neuroscience 11, 667–675 [DOI] [PubMed] [Google Scholar]
- LaViola J.J.J. (2000). A discussion of cybersickness in virtual environments. SIGCHI Bulletin 32, 47–56 [Google Scholar]
- Li X., Liu J., Liang S., Guan K., An L., Wu X., Li S. & Sun C. (2013). Temporal modulation of sodium current kinetics in neuron cells by near-infrared laser. Cell Biochemistry and Biophysics 67, 1409–1419 [DOI] [PubMed] [Google Scholar]
- Lin B., Koizumi A., Tanaka N., Panda S. & Masland R.H. (2008). Restoration of visual function in retinal degeneration mice by ectopic expression of melanopsin. Proceedings of the National Academy of Sciences of the United States of America 105, 16009–16014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J.Y., Knutsen P.M., Muller A., Kleinfeld D. & Tsien R.Y. (2013). ReaChR: A red-shifted variant of channelrhodopsin enables deep transcranial optogenetic excitation. Nature Neuroscience 16, 1499–1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J.Y., Lin M., Steinbach P. & Tsien R. (2009). Characterization of engineered channelrhodopsin variants with improved properties and kinetics. Biophysical Journal 96, 1803–1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liutkeviciene R., Lesauskaite V., Asmoniene V., Gelzinis A., Zaliuniene D. & Jasinskas V. (2012). Inherited macular dystrophies and differential diagnostics. Medicina-Lithuania 48, 485–495 [PubMed] [Google Scholar]
- Marc R.E., Jones B.W., Watt C.B. & Strettoi E. (2003). Neural remodeling in retinal degeneration. Progress in Retinal and Eye Research 22, 607–655 [DOI] [PubMed] [Google Scholar]
- Martínez J.J., Toledo F.J., Fernández E. & Ferrández J.M. (2009). Study of the contrast processing in the early visual system using a neuromorphic retinal architecture. Neurocomputing 72, 928–935 [Google Scholar]
- Mattis J., Tye K.M., Ferenczi E.A., Ramakrishnan C., O'Shea D.J., Prakash R., Gunaydin L.A., Hyun M., Fenno L.E., Gradinaru V., Yizhar O. & Deisseroth K. (2012). Principles for applying optogenetic tools derived from direct comparative analysis of microbial opsins. Nature Methods 9, 159–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern B., Palmini R.B., Grossman N., Drakakis E., Poher V., Neil M.A. & Degenaar P. (2010). A new individually addressable micro-LED array for photogenetic neural stimulation. IEEE Transactions on Biomedical Circuits and Systems 4, 469–476 [DOI] [PubMed] [Google Scholar]
- Mead C.A. & Mahowald M.A. (1988) A silicon model of early visual processing. Neural Networks 1, 91–97 [Google Scholar]
- Mei Y. & Zhang F. (2012). Molecular tools and approaches for optogenetics. Biological Psychiatry 71, 1033–1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meister M. & Berry Ii M.J. (1999). The neural code of the retina. Neuron 22, 435–450 [DOI] [PubMed] [Google Scholar]
- Melyan Z., Tarttelin E.E., Bellingham J., Lucas R.J. & Hankins M.W. (2005). Addition of human melanopsin renders mammalian cells photoresponsive. Nature 433, 741–745 [DOI] [PubMed] [Google Scholar]
- Milam A.H., Li Z-Y. & Fariss R.N. (1998). Histopathology of the human retina in retinitis pigmentosa. Progress in Retinal and Eye Research 17, 175–205 [DOI] [PubMed] [Google Scholar]
- Miyashita T., Shao Y.R., Chung J., Pourzia O. & Feldman D. (2013). Long-term channelrhodopsin-2 (ChR2) expression can induce abnormal axonal morphology and targeting in cerebral cortex. Frontiers in Neural Circuits 7, 00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss J.D., Austin J., Salley J., Coats J., Williams K. & Muth E.R. (2011). The effects of display delay on simulator sickness. Displays 32, 159–168 [Google Scholar]
- Nagel G., Szellas T., Huhn W., Kateriya S., Adeishvili N., Berthold P., Ollig D., Hegemann P. & Bamberg E. (2003). Channelrhodopsin-2, a directly light-gated cation-selective membrane channel. Proceedings of the National Academy of Sciences of the United States of America 100, 13940–13945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nat.Meth.Editorial (2012). Method of the year 2011. Nature Methods 9, 1. [DOI] [PubMed] [Google Scholar]
- Nichols S. & Patel H. (2002). Health and safety implications of virtual reality: A review of empirical evidence. Applied Ergonomics 33, 251–271 [DOI] [PubMed] [Google Scholar]
- Nikolic K., Grossman N., Grubb M.S., Burrone J., Toumazou C. & Degenaar P. (2009). Photocycles of channelrhodopsin-2. Photochemistry and Photobiology 85, 400–411 [DOI] [PubMed] [Google Scholar]
- Nirenberg S. & Pandarinath C. (2012). Retinal prosthetic strategy with the capacity to restore normal vision. Proceedings of the National Academy of Sciences of the United States of America 109, 15012–15017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normann R.A., Greger B.A., House P., Romero S.F., Pelayo F. & Fernandez E. (2009). Toward the development of a cortically based visual neuroprosthesis. Journal of Neural Engineering 6, 035001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutton V. (1995). Scribonius Largus, the unknown pharmacologist. Pharmaceutical History 25, 5–8 [PubMed] [Google Scholar]
- Oesterhe D. & Stoecken W. (1973). Functions of a new photoreceptor membrane. Proceedings of the National Academy of Sciences of the United States of America 70, 2853–2857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packer A.M., Roska B. & Häusser M. (2013). Targeting neurons and photons for optogenetics. Nature Neuroscience 16, 805–815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paninski L. (2004). Maximum likelihood estimation of cascade point-process neural encoding models. Network 15, 243–262 [PubMed] [Google Scholar]
- Paninski L., Pillow J.W. & Lewi J. (2007). Statistical models for neural encoding, decoding, and optimal stimulus design. Progress in Brain Research 165, 493–507 [DOI] [PubMed] [Google Scholar]
- Pezaris J.S. & Reid R.C. (2007). Demonstration of artificial visual percepts generated through thalamic microstimulation. Proceedings of the National Academy of Sciences of the United States of America 104, 7670–7675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picaud S. & Sahel J-A. (2014). Retinal prostheses: Clinical results and future challenges. Comptes Rendus Biologies 337, 214–222 [DOI] [PubMed] [Google Scholar]
- Reutsky-Gefen I., Golan L., Farah N., Schejter A., Tsur L., Brosh I. & Shoham S. (2013). Holographic optogenetic stimulation of patterned neuronal activity for vision restoration. Nature Communications 4, 1509. [DOI] [PubMed] [Google Scholar]
- Rodieck R.W. (1965). Quantitative analysis of cat retinal ganglion cell response to visual stimuli. Vision Research 5, 583–601 [DOI] [PubMed] [Google Scholar]
- Sahel J-A. & Roska B. (2013). Gene therapy for blindness. Annual Review of Neuroscience 36, 467–488 [DOI] [PubMed] [Google Scholar]
- Santos A., Humayan M.S., de Juan E. Jr., Greenberg R.J., Marsh M.J., Klock I.B. & Milam A.H. (1997). Preservation of the inner retina in retinitis pigmentosa. A morphometric analysis. Archives of Ophthalmology 115, 511–515 [DOI] [PubMed] [Google Scholar]
- Shepherd R.K., Shivdasani M.N., Nayagam D.A.X., Williams C.E. & Blamey P.J. (2013). Visual prostheses for the blind. Trends in Biotechnology 31, 562–571 [DOI] [PubMed] [Google Scholar]
- Shoham S., O'Connor D.H., Sarkisov D.V. & Wang S.S.H. (2005). Rapid neurotransmitter uncaging in spatially defined patterns. Nature Methods 2, 837–843 [DOI] [PubMed] [Google Scholar]
- Simo R. & Hernandez C. (2014). Neurodegeneration in the diabetic eye: New insights and therapeutic perspectives. Trends Endocrinology and Metabolism 25, 23–33 [DOI] [PubMed] [Google Scholar]
- Stasheff S.F. (2008). Emergence of sustained spontaneous hyperactivity and temporary preservation of off responses in ganglion cells of the retinal degeneration (rd1) mouse. Journal of Neurophysiology 99, 1408–1421 [DOI] [PubMed] [Google Scholar]
- Stasheff S.F., Shankar M. & Andrews M.P. (2011). Developmental time course distinguishes changes in spontaneous and light-evoked retinal ganglion cell activity in rd1 and rd10 mice. Journal of Neurophysiology 105, 3002–3009 [DOI] [PubMed] [Google Scholar]
- Stingl K., Bartz-Schmidt K.U., Besch D., Braun A., Bruckmann A., Gekeler F., Greppmaier U., Hipp S., Hörtdörfer G., Kernstock C., Koitschev A., Kusnyerik A., Sachs H., Schatz A., Stingl K.T., Peters T., Wilhelm B. & Zrenner E. (2013). Artificial vision with wirelessly powered subretinal electronic implant alpha-IMS. Proceedings of the Royal Society B: Biological Sciences 280, 20130077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone J.L., Barlow W.E., Humayan M.S., de Juan E. Jr., & Milam A.H. (1992). Morphometric analysis of macular photoreceptors and ganglion cells in retinas with retinitis pigmentosa. Archives of Ophthalmology 110, 1634–1639 [DOI] [PubMed] [Google Scholar]
- Sugano E., Isago H., Wang Z., Murayama N., Tamai M. & Tomita H. (2011). Immune responses to adeno-associated virus type 2 encoding channelrhodopsin-2 in a genetically blind rat model for gene therapy. Gene Therapy 18, 266–274 [DOI] [PubMed] [Google Scholar]
- Thyagarajan S., Van Wyk M., Lehmann K., Löwel S., Feng G. & Wässle H. (2010). Visual function in mice with photoreceptor degeneration and transgenic expression of channelrhodopsin 2 in ganglion cells. Journal of Neuroscience 30, 8745–8758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomic M., Kastelan S., Metez Soldo K. & Salopek-Rabatic J. (2013). Influence of BAK-preserved prostaglandin analog treatment on the ocular surface health in patients with newly diagnosed primary open-angle glaucoma. BioMed Research International 2013, 603782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita H., Sugano E., Fukazawa Y., Isago H., Sugiyama Y., Hiroi T., Ishizuka T., Mushiake H., Kato M., Hirabayashi M., Shigemoto R., Yawo H. & Tamai M. (2009). Visual properties of transgenic rats harboring the channelrhodopsin-2 gene regulated by the thy-1.2 promoter. PLoS One 4, e7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita H., Sugano E., Isago H., Hiroi T., Wang Z., Ohta E. & Tamai M. (2010). Channelrhodopsin-2 gene transduced into retinal ganglion cells restores functional vision in genetically blind rats. Experimental Eye Research 90, 429–436 [DOI] [PubMed] [Google Scholar]
- Tomita H., Sugano E., Yawo H., Ishizuka T., Isago H., Narikawa S., Kügler S. & Tamai M. (2007). Restoration of visual response in aged dystrophic RCS rats using AAV-mediated channelopsin-2 gene transfer. Investigative Ophthalmology and Visual Science 48, 3821–3826 [DOI] [PubMed] [Google Scholar]
- Toychiev A.H., Ivanova E., Yee C.W. & Sagdullaev B.T. (2013). Block of gap junctions eliminates aberrant activity and restores light responses during retinal degeneration. Journal of Neuroscience 33, 13972–13977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Lookeren Campagne M., LeCouter J., Yaspan B.L. & Ye W. (2014). Mechanisms of age-related macular degeneration and therapeutic opportunities. Journal of Pathology 232, 151–164 [DOI] [PubMed] [Google Scholar]
- Weiland J.D., Cho A.K. & Humayun M.S. (2011). Retinal prostheses: Current clinical results and future needs. Ophthalmology 118, 2227–2237 [DOI] [PubMed] [Google Scholar]
- Wheeler L.A. & Woldemussie E. (2001). Alpha-2 adrenergic receptor agonists are neuroprotective in experimental models of glaucoma. European Journal of Ophthalmology 2, S30–S35 [DOI] [PubMed] [Google Scholar]
- Zhang F., Vierock J., Yizhar O., Fenno L.E., Tsunoda S., Kianianmomeni A., Prigge M., Berndt A., Cushman J., Polle J., Magnuson J., Hegemann P. & Deisseroth K. (2011). The microbial opsin family of optogenetic tools. Cell 147, 1446–1457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ivanova E., Bi A. & Pan Z.H. (2009). Ectopic expression of multiple microbial rhodopsins restores ON and OFF light responses in retinas with photoreceptor degeneration. Journal of Neuroscience 29, 9186–9196 [DOI] [PMC free article] [PubMed] [Google Scholar]