Abstract
Background
Children unreached by vaccination are at higher risk of poor health outcomes and India accounts for nearly a quarter of unvaccinated children worldwide. The objective of this study was to investigate compositional and contextual determinants of non-receipt of childhood vaccines in India using multilevel modelling.
Methods and Findings
We studied characteristics of unvaccinated children using the District Level Health and Facility Survey 3, a nationally representative probability sample containing 65 617 children aged 12–23 months from 34 Indian states and territories. We developed four-level Bayesian binomial regression models to examine the determinants of non-vaccination. The analysis considered two outcomes: completely unvaccinated (CUV) children who had not received any of the eight vaccine doses recommended by India’s Universal Immunization Programme, and children who had not received any dose from routine immunisation services (no RI). The no RI category includes CUV children and those who received only polio doses administered via mass campaigns. Overall, 4.83% (95% CI: 4.62–5.06) of children were CUV while 12.01% (11.68–12.35) had received no RI. Individual compositional factors strongly associated with CUV were: non-receipt of tetanus immunisation for mothers during pregnancy (OR = 3.65 [95% CrI: 3.30–4.02]), poorest household wealth index (OR = 2.44 [1.81–3.22] no maternal schooling (OR = 2.43 [1.41–4.05]) and no paternal schooling (OR = 1.83 [1.30–2.48]). In rural settings, the influence of maternal illiteracy disappeared whereas the role of household wealth index was reinforced. Factors associated with no RI were similar to those for CUV, but effect sizes for individual compositional factors were generally larger. Low maternal education was the strongest risk factor associated with no RI in all models. All multilevel models found significant variability at community, district, and state levels net of compositional factors.
Conclusion
Non-vaccination in India is strongly related to compositional characteristics and is geographically distinct. Tailored strategies are required to overcome current barriers to immunisation.
Introduction
Vaccination is a key strategy for reducing child mortality [1], [2]. In 1974, the World Health Organization (WHO) established the Expanded Programme on Immunization (EPI) to ensure that all children had access to six basic vaccines: Bacille Calmette-Guérin vaccine (BCG), diphtheria-tetanus-pertussis vaccine (DTP), oral poliovirus vaccine (OPV), and measles-containing vaccine (MCV) [3]. A recent report suggests that vaccination against four diseases targeted by the EPI - diphtheria, tetanus, pertussis and measles - averts an estimated 2 to 3 million deaths every year [4], [5]. Despite this success, 22.6 million infants remained unvaccinated (defined as non-receipt of DTP1)-or under-vaccinated (defined as non-receipt of DTP3) worldwide in 2012 [6]. According to the Child Health Epidemiology Reference Group (CHERG), of the estimated 8.8 million deaths of children under 5 years of age worldwide in 2008, 1.5 million (17%) were due to vaccine preventable diseases (VPDs) [7], [8].
Of 12.6 million children who had not received a DTP1 dose in 2012 (commonly considered as proxy for access to vaccination services), approximately 3 million were Indians [6]. Numerous studies have addressed the question of suboptimal childhood vaccination in India. For example, one recent systematic review [9] identified several risk factors related to child (gender, birth order), family (area of residence, wealth, parental education), demography (religion, caste), and community (access to care, community literacy) characteristics. Though the cumulative evidence is impressive, it offers a limited perspective. First, while the characteristics of unvaccinated children are likely to be different from those of undervaccinated children, primary studies have generally considered partially vaccinated and unvaccinated children together, and relatively few have focussed on unvaccinated children [10]. Second, previous studies limited their analysis mainly to individual- and household level-factors using fixed effects models [11], [12]. Third, the few previous researches that examined broader contextual-level factors did not take into account the simultaneous net effects resulting from a wider set of compositional and contextual or community factors [13], [14]. Consequently, an approach restricted to a sole level, either the individual level or the macro-scale of contexts, generates conceptual and practical limiting problems [15], [16].
Considering these limitations, investigation of factors related to non-vaccination is yet to be explored accurately in the context of India. This issue is even more important in regard to the call for universal health care by 2020 in India [17]. Indeed, to scale up coverage successfully contingent to well-known scaling up concern, the problem is not just to reach more children, but to reach those facing specific barriers. It is therefore essential to conduct population-based assessments of patterns, distribution and determinants of non-vaccination in order to identify barriers within subpopulations in every context [18]. Given the complexity of the different relationships between influential variables at individual and contextual levels, it is important to assess their relative contribution in a multilevel model that can properly account for individual and contextual factors and their potential interactions.
Our objective was to investigate the role of potential compositional and contextual determinants of non-receipt of basic vaccines among 12–23-month-old children in India. Specifically, we aimed to: (i) ascertain whether individual or household level (compositional) factors are significantly associated with childhood non-vaccination, net of community-level factors in India; (ii) determine whether there was a significant contextual variation of childhood non-vaccination; (iii) assess whether contextual variation was explained by individual- and contextual-level factors.
Methods
We used data from the District Level Household and Facility Survey 3 (DLHS-3), a nationwide household survey at district level, conducted in 2007–2008 in 34 Indian states and territories [19]. The DLHS-3 was designed as a cross-sectional study that used a stratified, systematic, multistage cluster sampling design [19].
Outcome measure
The basic Indian vaccination schedule is proposed by Universal Immunization Programme (UIP). The UIP is the largest immunization program in the world and targets 27 million infants annually. The UIP protects children against 7 vaccine-preventable diseases: tuberculosis, diphtheria, tetanus, pertussis, polio, measles (added in 1985) and hepatitis (added in 1990). Vaccines are provided free of cost and delivered through strategies such as routine immunization, village health and nutrition days, and outreach campaigns [20]. In keeping with the definition in standard use in India, full immunisation is defined as a child 12–23 months of age receiving all of the following vaccines: a dose of BCG vaccine at birth (or as soon as possible); three doses of DPT vaccine at 6, 10 and 14 weeks of age; at least three doses of OPV at 6, 10 and 14 weeks of age; and one dose MCV at 9 months of age. Vaccination information of 12–23 month-old children in DLHS-3 was obtained either from health cards or from mother’s or caregiver verbal reports.
We created two binary outcomes to study non-vaccination in this sample. First, children 12–23 months of age who had not received any of the following eight vaccine doses (1 dose of BCG vaccine, 3 doses each of DTP vaccine and OPV, and 1 dose of MCV were considered completely unvaccinated (CUV), and were compared to children who had received at least one dose of vaccine. Second, children were considered to have received no routine immunisation (no RI) if they had not received any of the five recommended doses administered only through routine services (1 dose of BCG vaccine, 3 doses of DTP vaccine, and 1 dose of MCV), and were compared to children who had received at least one routine immunisation dose. Full immunization coverage can be attained only through improving routine immunisation systems. For several decades, as part of the global eradication initiative, India has had a very strong polio programme operating largely in campaign mode in parallel to routine immunization services [21], [22]. We therefore also studied those children 12–23 months of age who had not received a single dose of vaccine from routine immunization services.
Explanatory variables
Individual and household (compositional) characteristics
We included the following compositional variables: child sex (male or female), birth order (1, 2, 3, 4 and more), mother’s age (15–24, 25–34, or 35 years or older), mother’s and father’s educational attainment (0 year, 1–5 years, 6–8 years, 9–10 years, 11–12 years, or 13 or more years), caste (scheduled tribe, scheduled caste, other backward caste -OBC- and general), religion (Hindu, Muslim and others i.e. Sikh, Christian, Buddhist and others), antenatal care –ANC- (prenatal visits, tetanus injection during pregnancy), postnatal care (No PNC within 2 weeks), and household wealth. Household wealth index was computed by combining household assets and material possessions by IIPS and divided into quintiles (poorest to the richest groups accounting for the lowest to the highest quintiles).
Contextual characteristics
Contextual characteristics are defined at community, district and state levels. State-level characteristics considered included area of residence (urban and rural) and region of residence categorised into two groups as follows:
The first group included Empowered Action Group States (EAG) and Assam (EAGA). The EAG states, which account for about 45% of India’s population and have particularly high fertility and mortality indicators, were designated as “High Focus States” by the Indian Government in 2001. Due to lagging social and demographic indicators, Assam is often considered with this group. EAGA states were: Assam, Bihar, Chhattisgarh, Jammu and Kashmir, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttar Pradesh, Uttarakhand).
The second group (other states) included: Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Sikkim, Tripura, Andaman and Nicobar Islands, Andhra Pradesh, Chandigarh, Dadra and Nagar Haveli, Daman and Diu, Delhi, Goa, Gujarat, Haryana, Himachal, Pradesh, Karnataka, Kerala, Lakshadweep, Maharashtra, Pondicherry, Punjab, Tamil Nadu, West Bengal).
We used the term community to describe clustering within the same geographical living environment. Communities were based on sharing a common primary sample unit (PSU) within the DLHS-3 data as it is the most consistent measure of community in the DHS surveys [23]. Since poverty and education characteristics of communities were not directly available, they were constructed by aggregating individual-level characteristics at the PSU level. Specifically, these weighted measures were derived by summing the values obtained on individual women in each community and dividing then by the total number of women respondents living in each one. The community’s poverty status was defined as the proportion of households below 20% of wealth index. The proportion of women with no formal education was generated from native individuals in the database and aimed to represent female illiteracy in the community. In our study, these group-measures were based on an average of 3 women per community (from 1 to 31), which provides a sufficient number 1) to generate reliable estimates [24] and 2) to use Monte Carlo Markov Chains for achieving our computations [25].
Statistical analysis
The entire national sample (n = 65,617) of children aged 12–23 months was analyzed. Data typically have a hierarchical structure in which children were nested within mothers, mothers were clustered within households, households were nested within communities which were clustered within districts, and finally districts were nested within states. To account for unequal selection probabilities and ensure representativeness of the sample, we applied the appropriate sampling weights.
Determinants of non-vaccination were assessed by using Bayesian binomial regression models. We specified a 4-level model for each binary outcome y, i.e., non-vaccination, for child i living in community j in district k and state l. Probability was related to a set of categorical predictors X and a random effect for each level by a logit-link function as logit (πijkl) = β0+βX+u0jkl+v0kl+f0l. A child level was defined by collapsing child-, mother- and household-level data. The linear predictor of the equation consisted of a fixed part (β0+βX) estimating the conditional coefficients for the covariates. The 3 random intercepts were respectively attributable to communities (u0jkl), districts (v0kl) and states (f0l), each assumed to have an independent and identical distribution and variance estimated at a corresponding level. All models were estimated by using Bayesian methods implemented via Markov Chain Monte Carlo (MCMC) simulation and the Metropolis-Hastings algorithm [26]. We used diffuse default prior distribution for all parameters [26]. Starting values of the distribution were derived from two previous estimations using Iterated Generalized Least Squares (IGLS) and second order penalised quasi-likelihood linearization (PQL2). MCMC estimation was adopted in the analysis to reduce bias in the estimates of random effect parameters. Indeed, such bias can arise when multilevel models with discrete outcomes are estimated using maximum-likelihood procedures [27]–[29].
All estimations were performed by MLwiN within STATA 12 MP (Stata, Corp.) and MLWiN 2.26 through runmlwin procedure [30]. Our computations were based on chains of length 50 000 iterations after a burn-in of 5000. Bayesian deviance information criterion (BIC) was used to estimate the goodness of fit of consecutive models [31] The BIC values for each model were compared, and the model with the lowest value was considered the better one for hierarchical models [31].
We examined separately the association between non-vaccination and compositional (individual-household) and contextual variables. The first model is a null model (Model 1), which provides information on the extent to which communities, districts and states vary and further justify assessing random effects at these levels. Model 2 included only individual characteristics while model 3 contained community characteristics. Model 4 expanded model 3 by adding individual level variables. We further fitted a fifth model to analyse a cross-level interaction between household wealth and area of residence (rural and urban). Since we found a significant (p = 0.035) interaction term (area of residence * wealth index), we present separate models including all individual and contextual variables stratified for rural and urban areas of residence.
The fixed effects, i.e., the association between non-vaccination and selected variables, were shown as odds ratio (OR) with its 95% credible interval (CrI). Meanwhile, random effects (measures of variation) were estimated by median odds ratio (MOR) rather than using intra-cluster correlation (ICC) which is better fitted for linear models [32], [33]. The MOR quantifies the unexplained contextual heterogeneity, otherwise it quantifies contextual-level variance on the odds ratio scale and is always greater than or equal to 1 [32].
Ethical considerations
This study is based on an analysis of existing survey data with all identifier information removed. The survey was approved by the Ministry of Health & Family Welfare, Government of India and the International Institute of Population Sciences (IIPS) institutional review board. All study participants gave informed consent before participation and all information was collected confidentially. Data of DLHS-3 were obtained from the IIPS as they are made available in the public domain for analysis by researchers. Therefore, no additional ethics review is required for this work by the Montréal University committee of ethics.
Results
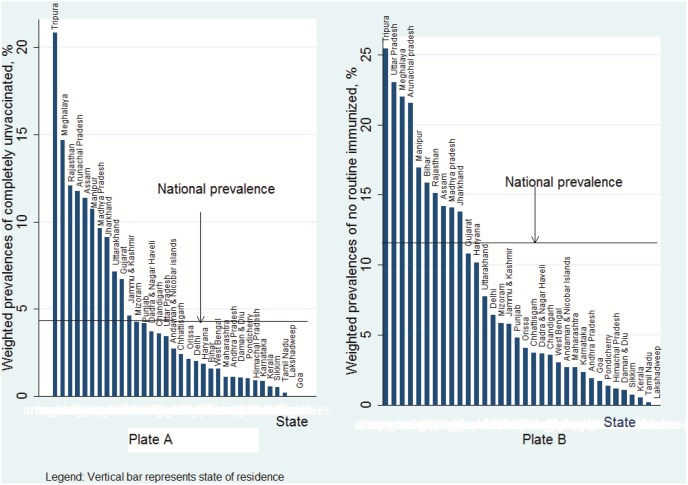
Of 65 617 children aged from 12 to 23 months, 3173 (4.83%, [95% Confidence Intervals (CI): 4.62–5.06]) were completely unvaccinated (CUV) and failed to receive any of the eight recommended vaccine doses while 7883 (12.01%, [95% CI: 11.68–12.35]) did not receive any vaccine dose through routine services (No-RI). The distribution of CUV and No-RI children showed substantial variation between states. The weighted prevalence of CUV extended from 0% (Goa and Lakshadweep) to 20.9% (Tripura) (Figure 1 Plate A) while that of No-RI ranged from 0% (Lakshadweep) to 25.4% (Tripura) (Figure 1 Plate B). Proportions of non-receipt of basic vaccines varied according to characteristics of children, parents and households (Tables 1 & 2).
Figure 1. Weighted prevalences of completely unvaccinated and no routine immunized by state, India DLHS-3, 2007–2008.
Table 1. Weighted proportions of non-vaccination by individual characteristics among 65617 children aged 12–23 months, India, DLHS-3, 2007–2008.
| Characteristics | Completely Unvaccinated(CUV) | No Routine Immunisation(No RI) |
| Individual-related characteristics | Number (weighted %) | Number (weighted %) |
| Child (n = 65617) | ||
| Sex | 3189 (5.0) | 7921 (12.0) |
| Male | 1620 (4.8) | 3945 (11.0) |
| Female | 1569 (5.0) | 3975 (13.0) |
| Birth order (n = 64637) | 3155 (5.0) | 7796 (12.0) |
| 1 | 901 (4.0) | 1771 (8.0) |
| 2 | 972 (4.0) | 1540 (9.0) |
| 3 | 509 (5.0) | 1274 (13.0) |
| ≥4 | 1073 (7.0) | 3211 (22.0) |
| Parents (n = 65617) | ||
| Mother’s schooling, years | 3189 (5.0) | 7921 (12.0) |
| 0 | 2225 (8.0) | 5976 (20.0) |
| 1–5 | 451 (5.0) | 991 (10.0) |
| 6–8 | 309 (3.0) | 577 (6.0) |
| 9–12 | 183 (1.0) | 352 (3.0) |
| ≥13 | 21 (1.0) | 25 (1.0) |
| Mother’s marital status (n = 65617) | 3189 (5.0) | 7921 (12.0) |
| Currently married | 3138 (5.0) | 7816 (12.0) |
| Currently alone (single, divorced, widowed, deserted) | 51 (7.0) | 105 (15.0) |
| Mother’s age group, years (n = 65617) | 3189 (5.0) | 7921 (12.0) |
| 15–19 | 303 (5.0) | 587 (13.0) |
| 20–24 | 1075 (4.0) | 2570 (10.0) |
| 25–34 | 1567 (5.0) | 3801 (12.0) |
| 35–49 | 344 (7.0) | 963 (20.0) |
| Mother received four ANC during pregnancy (n = 64701) | 3158 (5.0) | 7803 (12.0) |
| Yes | 88 (1.0) | 166 (2.0) |
| No | 3070(5.7) | 7637 (14.0) |
| Tetanus toxin injection during pregnancy (n = 64701) | 3159 (5.0) | 7803 (12.0) |
| Yes | 873 (2.0) | 2541 (5.0) |
| No | 2286 (12.0) | 5262 (29.0) |
| Postnatal care within 2 weeks (n = 61613) | 3121 (5.0) | 7715 (12.0) |
| Yes (reference) | 525 (2.0) | 1555 (6.0) |
| No | 2595 (8.0) | 6160 (18.0) |
| Husband’s education, years | ||
| 0 | 3189 (5.0) | 7921 (12.0) |
| 1–5 | 1368 (9.0) | 3557 (22.0) |
| 6–8 | 595 (6.0) | 1506 (14.0) |
| 9–12 | 554 (5.0) | 1237 (11.0) |
| ≥13 | 578 (3.0) | 1414 (7.0) |
Table 2. Weighted proportions of non-vaccination by household and contextual characteristics among 65617 children aged 12–23 months, India, DLHS-3, 2007–2008.
| Completely Unvaccinated (CUV) | No Routine Immunisation (No-RI) | |
| Characteristics | Number (weighted %) | Number (weighted %) |
| Caste group (n = 64424) | 3084 (5.0) | 7780 (12.0) |
| Scheduled caste | 575 (5.0) | 1553 (12.0) |
| Scheduled tribe | 1059 (10.0) | 1609 (15.0) |
| Other backward caste (OBC) | 1003 (4.0) | 3513 (13.0) |
| General | 447 (3.0) | 1104 (8.0) |
| Religion (n = 65614) | 3189 (5.0) | 7920 (12.0) |
| Hindu | 2131 (4.0) | 5366 (11.0) |
| Muslims | 602 (6.0) | 1868 (19.0) |
| Others/no religion | 451 (7.0) | 686 (11.0) |
| Household-related characteristics | ||
| Wealth index (n = 65603) | 3189 (5.0) | 7921 (12.0) |
| Poorest | 1145. (9.0) | 2853 (21.0) |
| Poorer | 919 (7.0) | 2265 (16.0) |
| Middle | 630 (5.0) | 1483 (11.0) |
| Richer | 362 (3.0) | 950 (7.0) |
| Richest | 133 (1.0) | 370 (3.0) |
| Contextual-related characteristics | ||
| Place of residence (n = 65617) | 3189 (5.0) | 7921 (12.0) |
| Rural | 2820 (5.0) | 6931 (13.0) |
| Urban | 369 (3.0) | 990 (8.0) |
| Region (n = 65617) | 3189 (5.0) | 7921 (12.0) |
| EAG-Assam | 2276 (6.0) | 6322 (16.0) |
| Other | 913 (3.0) | 1599 (6.0) |
CUV: received none of the eight basic vaccine doses; No-RI: received none of the five recommended vaccine doses delivered exclusively through the routine immunisation system; EAG: Empowered- Action Group; wealth index based on household amenities and possessions calculated by International Institute for Population Science.
Tables 3&4 present four-level univariate logistic regression results. Increasing maternal and paternal educational attainment was protective against child non-receipt of vaccines through a graded trend (P trend <0.0001) (table 3). Children at birth ranks ≥3 were more likely to be unvaccinated. Lack of utilisation of health services during and after pregnancy by the mother was positively associated to being CUV. In comparison to the reference group, children born from women with less than 4 ANC visits or no tetanus injection during pregnancy had nearly 8 time the risk of being CUV (OR = 7.56 [95% Credible Interval (CrI): 6.09–9.37] and OR = 7.25 [6.69–7.85], respectively). Furthermore, not receiving PNC within 2 weeks after birth was also associated with CUV status (OR = 4.16 [3.78–4.57]). Finally, when contrasting both outcomes, the strength of association of variables related to individual characteristics appeared generally more pronounced for No-RI while magnitudes were larger among CUV for variables related to health services utilization by mother and household wealth index.
Table 3. Four-level univariate logistic regression modeling of individual factors associated with non-vaccination among children aged 12–23 months, India, 2007–2008.
| Characteristics | Completely Unvaccinated (CUV) | No Routine Immunisation (No-RI) | ||
| Weighted Prevalence, % [95% CI] | 4.83 (4.62–5.06) | 12.01 (11.68–12.35) | ||
| Odds Ratio (95% CrI) | P-value | Odds Ratio (95% CrI) | P-value | |
| Individual-related characteristics | ||||
| Child | ||||
| Sex Male (Reference) | 1 | 0.145 | 1 | 0.003 |
| Female | 1.05 (0.98–1.13) | 1.13 (1.08–1.20) | ||
| Birth order 1 (Reference) | 1 | <0.001 | 1 | <0.0001 |
| 2 | 0.97 (0.87–1.07) | 1.16 (1.08–1.25) | ||
| 3 | 1.25 (1.11–1.40) | 1.44 (1.32–1.57) | ||
| ≥4 | 1.91 (1.75–2.10) | 2.16 (2.00–2.33) | ||
| Parents | ||||
| Mother’s schooling years | <0.0001 | <0.0001 | ||
| 0 | 12.50 (8.12–19.24) | 19.56 (12.87–29.75) | ||
| 1–5 | 7.86 (5.07–12.20) | 10.30 (6.74–15.74) | ||
| 6–8 | 4.95 (3.18–7.72) | 6.10 (3.97–9.33) | ||
| 9–12 | 2.13 (1.35–3.35) | 2.95 (1.91–4.55) | ||
| ≥13 (Reference) | 1 | 1 | ||
| Currently alone versus currently married | 1.66 (1.25–2.19) | <0.0001 | 1.42 (1.11–1.82) | <0.0001 |
| Mother’s age group, years | <0.0001 | <0.0001 | ||
| 15–19 (Reference) | 1 | 1 | ||
| 20–24 | 0.92 (0.79–1.08) | 0.81 (0.72–0.90) | ||
| 25–34 | 1.17 (1.00–1.37) | 0.99 (0.89–1.10) | ||
| 35–49 | 1.68 (1.40–2.01) | 1.39 (1.22–1.58) | ||
| Less than 4 ANC visits | 7.56 (6.09–9.37) | <0.0001 | 4.11 (3.82–4.43) | <0.0001 |
| No Tetanus toxin injection during pregnancy | 7.25 (6.69–7.85) | <0.0001 | 5.60 (5.23–6.00) | <0.0001 |
| No PNC visit within 2 weeks | 4.16 (3.78–4.57) | 2.71 (2.52–2.92) | <0.0001 | |
ANC Antenatal consultation; PNC Postnatal consultation; 95% CI: 95% Confidence interval.
Table 4. Four-level univariate logistic regression modeling of household and contextual factors associated with non-vaccination among children aged 12–23 months, India, 2007–2008.
| Characteristics | Completely Unvaccinated (CUV) | No Routine Immunisation (No-RI) | ||
| Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value | |
| Husband’s Educational attainment, y | <0.0001 | <0.0001 | ||
| 0 | 6.58 (5.29–8.20) | 6.87 (5.84–8.07) | ||
| 1–5 | 4.46 (3.55–5.60) | 4.67 (3.95–5.51) | ||
| 6–8 years | 3.60 (2.86–4.53) | 3.43 (2.90–4.05) | ||
| 9–12 years | 2.01 (1.60–2.53) | 2.10 (1.79–2.47) | ||
| ≥13 years (reference) | 1 | 1 | ||
| Caste group General (reference) | 1 | <0.0001 | 1 | <0.0001 |
| Other backward caste (OBC) | 1.19 (1.06–1.33) | 1.41 (1.30–1.54) | ||
| Scheduled caste | 1.43 (1.26–1.63) | 1.60 (1.46–1.76) | ||
| Scheduled tribe | 3.29 (2.94–3.69) | 2.45 (2.17–2.77) | ||
| Religion Hindu (reference) | 1 | <0.0001 | 1 | <0.0001 |
| Muslims | 1.49 (1.36–1.64) | 1.96 (1.80–2.13) | ||
| Others/no religion | 1.87 (1.68–2.07) | 1.23 (1.03–1.46) | ||
| Household’s Wealth index | <0.0001 | <0.0001 | ||
| Poorest | 8.29 (6.88–9.99) | 7.82 (6.78–9.03) | ||
| Poorer | 6.21 (5.14–7.50) | 5.40 (4.69–5.22) | ||
| Middle | 4.48 (3.69–5.44) | 3.69 (3.19–4.23) | ||
| Richer | 2.48 (2.02–3.04) | 2.37 (2.05–2.74) | ||
| Richest (reference) | 1 | 1 | ||
| Contextual-level characteristics | ||||
| Rural versus urban residence | 1.82 (1.63–2.04) | <0.0001 | 1.69 (1.51–1.87) | <0.0001 |
| EAG-Assam states versus other states | 1.08 (0.46–2.07) | 0.117 | 1.95 (0.87–4.34) | 0.132 |
| Community Illiterate women | 1.12 (0.89–1.40) | 0.886 | 0.91 (0.80–1.02) | 0.511 |
| Community poverty | 0.89 (0.58–1.31) | 0.220 | 1.05 (0.90–1.22) | 0.107 |
EAG: Empowered- Action Group; 95% CI: 95% Confidence interval.
Multivariate four-level regression results adjusted for potentially confounders showed results of association between CUV and individual (Table 5) and contextual-level (Table 6) variables. Model 2 shows associations for individual-level factors. Firstly, children born from mothers with no schooling relative to those born from mothers having at least 13 years of schooling were almost two and a half times more likely to be CUV. A similar but less marked trend was observed with respect to father’s educational attainment. Secondly, variables related to health services utilization by the mother remained significant, particularly maternal tetanus immunization during pregnancy which was the strongest individual-level factor related to CUV status. Thirdly, the association between CUV and wealth index showed a significant, dose-response relationship indicating that the risk of being CUV increased with lower household wealth. The effects of the inclusion of contextual factors are shown in Table 6 (Model 3). Rural residence and living in an EAG-Assam state increased the likelihood of a child being CUV with respective ORs of 1.57 [1.33–1.81] and 3.15 [1.14–6.86]. In Model 4 (Table 6), the inclusion of the community-level variables had minimal effect on the contribution of compositional variables on the likelihood of being CUV. Inversely, the effect of living in rural settings reversed and became protective against being CUV (OR = 0.71 [0.59–0.86]) while the effect of living in an EAG-Assam state disappeared.
Table 5. Four-level multivariate logistic regression modeling of fixed and random-effect of individual factors associated to non-vaccination (completely unvaccinated, CUV) among 12–23 months children in India, 2007–2008.
| Model 1 (Empty) OR(95% CrI) | Model 2 (Individual) OR(95% CrI) | Model 3 (Contextual) OR(95% CrI) | Model 4 (Individual & Contextual)OR (95% CrI) | |
| Individual-level factors | ||||
| Sex Female vs. male | 1.09 (1.00–1.20) | 1.09 (1.00–1.19) | ||
| Birth order 1 (reference) | 1 | 1 | ||
| 2 | 0.93 (0.82–1.08) | 0.93 (0.81–1.06) | ||
| 3 | 0.97 (0.82–1.13) | 0.97 (0.82–1.13) | ||
| ≥4 | 1.10 (0.94–1.28) | 1.10 (0.94–1.27) | ||
| Mother’s schooling, years | ||||
| 0 | 2.41 (1.31–3.96) | 2.43 (1.41–4.05) | ||
| 1–5 | 1.80 (1.01–2.95) | 1.82 (1.04–3.03) | ||
| 6–8 | 1.68 (0.95–2.79) | 1.69 (0.97–2.11) | ||
| 9–12 | 1.01 (0.57–1.67) | 1.02 (0.59–1.69) | ||
| ≥13 (reference) | 1 | 1 | ||
| Mother’s age group, years | ||||
| 15–19 (reference) | 1 | 1 | ||
| 20–24 | 0.98 (0.78–1.20) | 0.98 (0.80–1.19) | ||
| 25–34 | 1.04 (0.82–1.29) | 1.04 (0.83–1.28) | ||
| 35–49 | 0.92 (0.70–1.19) | 0.92 (0.71–1.19) | ||
| Less than 4 ANC visits | 1.52 (1.12–1.96) | 1.53 (1.25–1.88) | ||
| No TTI during pregnancy | 4.25 (3.78–4.78) | 3.65 (3.30–4.02) | ||
| No PNC within 2 weeks | 1.89 (1.61–2.12) | 1.81 (1.59–2.04) | ||
| Father’s schooling, years | ||||
| 0 | 1.81 (1.32–2.40) | 1.83 (1.30–2.48) | ||
| 1–5 | 1.43 (1.03–1.91) | 1.44 (1.03–1.97) | ||
| 6–8 | 1.41 (1.03–1.88) | 1.43 (1.04–1.94) | ||
| 9–12 | 1.14 (0.85–1.51) | 1.17 (0.85–1.57) | ||
| ≥13 (reference) | 1 | 1 |
ANC Antenatal consultation; PNC Postnatal consultation; TTI: Tetanus Toxin Injection; 95% CI: 95% Confidence interval.
Table 6. Four-level multivariate logistic regression modeling of fixed and random-effect of individual and contextual factors associated to non-vaccination (completely unvaccinated, CUV) among 12–23 months children in India, 2007–2008.
| Model 1 (Empty) OR (95% CrI) | Model 2 (Individual) OR (95% CrI) | Model 3 (Contextual) OR (95% CrI) | Model 4 (Individual & Contextual) OR(95% CrI) | |
| Caste group General (reference) | 1 | 1 | ||
| Other backward caste (OBC) | 1.04 (0.88–1.21) | 1.03 (0.87–1.20) | ||
| Scheduled caste | 1.19 (1.00–1.42) | 1.17 (1.00–1.40) | ||
| Scheduled tribe | 1.46 (1.18–1.78) | 1.46 (1.19–1.78) | ||
| Religion Hindu (reference) | 1 | 1 | ||
| Muslims | 1.89 (1.57–2.24) | 1.82 (1.52–2.16) | ||
| Others/no religion | 1.04 (0.80–1.32) | 1.05 (0.81–1.33) | ||
| Household Wealth index | ||||
| Poorest | 2.10 (1.58–2.76) | 2.44 (1.81–3.22) | ||
| Poorer | 1.78 (1.36–2.31) | 2.05 (1.57–2.49) | ||
| Middle | 1.59 (1.22–2.05) | 1.80 (1.36–2.32) | ||
| Richer | 1.36 (1.05–1.75) | 1.48 (1.30–1.91) | ||
| Richest (reference) | 1 | 1 | ||
| Contextual-level factors | ||||
| Rural vs. Urban | 1.57 (1.33–1.81) | 0.71 (0.59–0.86) | ||
| EAG-Assam versus other | 3.15 (1.14–6.86) | 1.09 (0.49–2.47) | ||
| Community Illiterate women | 1.05 (0.84–1.32) | 1.09 (0.86–1.37) | ||
| Community poverty | 0.93 (0.62–1.34) | 0.90 (0.58–1.32) | ||
| Variance (SE) | ||||
| Community | 2.04 (0.13) | 1.66 (0.12) | 2.02 (0.12) | 1.69 (0.13) |
| District | 1.15 (0.12) | 0.84 (0.10) | 1.14 (0.12) | 0.83 (0.10) |
| State | 1.93 (0.60) | 1.06 (0.35) | 1.72 (0.54) | 1.10 (0.37) |
| MOR | ||||
| Community | 3.90 (3.58–4.25) | 3.42 (3.12–3.73) | 3.88 (3.59–4.20) | 3.44 (3.14–3.79) |
| District | 2.78 (2.51–3.09) | 2.40 (2.18–2.65) | 2.77 (2.50–3.08) | 2.39 (2.17–2.64) |
| State | 3.76 (2.66–5.77) | 2.67 (2.03–3.75) | 3.79 (2.51–5.27) | 2.72 (2.04–3.44) |
EAG: Empowered- Action Group; MOR: Median odds ratio; 95% CrI: Credible interval.
Tables 7&8 presents multivariate logistic regression results related to non-receipt of routine immunisation. As compared to CUV, being No-RI (Model 4, Tables 7&8) was more strongly associated to mother’s educational attainment, being Muslim, female gender, and living in urban areas. Notably, maternal education was the strongest factor. Other findings were similar to those in Tables 5&6.
Table 7. Four-level multivariate logistic regression modeling of fixed and random-effect of individual actors associated with non-receipt of routine immunisation (No-RI) among 12–23 months children in India, 2007–2008.
| Model 1 (Empty) OR (95% CrI) | Model 2 (Individual) OR (95% CrI) | Model 3 (Contextual) OR (95% CrI) | Model 4 (Individual & Contextual) OR (95% CrI) | |
| Individual-level factors | ||||
| Sex Female vs. male | 1.18 (1.11–1.25) | 1.18 (1.11–1.25) | ||
| Birth order 1 (reference) | 1 | 1 | ||
| 2 | 1.09 (0.98–1.19) | 1.08 (0.99–1.19) | ||
| 3 | 1.21 (1.09–1.35) | 1.20 (1.08–1.35) | ||
| ≥4 | 1.44 (1.29–1.60) | 1.42 (1.28–1.59) | ||
| Mother’s schooling, years | ||||
| 0 | 4.35 (3.82–6.18) | 4.92 (3.18–6.94) | ||
| 1–5 | 3.13 (2.03–4.50) | 3.55 (2.29–4.99) | ||
| 6–8 | 2.42 (1.58–3.47) | 2.73 (1.75–3.82) | ||
| 9–12 | 1.77 (1.16–2.54) | 1.99 (1.29–2.78) | ||
| ≥13 (reference) | 1 | 1 | ||
| Mother’s age group, years | ||||
| 15–19 (reference) | 1 | 1 | ||
| 20–24 | 0.80 (0.70–0.91) | 0.80 (0.70–0.91) | ||
| 25–34 | 0.74 (0.64–0.85) | 0.74 (0.64–0.84) | ||
| 35–49 | 0.71 (0.60–0.84) | 0.70 (0.59–0.84) | ||
| Less than 4 ANC visits | 1.73 (1.45–2.07) | 1.75 (1.42–2.06) | ||
| No TTI during pregnancy | 4.00 (3.73–4.30) | 4.02 (3.73–4.33) | ||
| No PNC within 2 weeks | 1.55 (1.43–1.67) | 1.56 (1.43–1.69) | ||
| Father’s schooling, years | ||||
| 0 | 2.02 (1.65–2.45) | 1.93 (1.63–2.35) | ||
| 1–5 | 1.58 (1.35–2.05) | 1.60 (1.35–1.96) | ||
| 6–8 | 1.53 (1.25–1.86) | 1.47 (1.22–1.79) | ||
| 9–12 | 1.30 (1.07–1.57) | 1.27 (1.07–1.53) | ||
| ≥13 (reference) | 1 | 1 | ||
| Caste group General (reference) | 1 | 1 | ||
| Other backward caste (OBC) | 1.04 (0.88–1.21) | 1.10 (0.99–1.22) | ||
| Scheduled caste | 1.17 (1.04–1.31) | 1.15 (1.01–1.30) | ||
| Scheduled tribe | 1.40 (1.21–1.77) | 1.41 (1.21–1.63) |
ANC; Antenatal care; PNC; Postnatal care; TTI: tetanus Toxin injection; 95% CrI: Credible interval.
Table 8. Four-level multivariate logistic regression modeling of fixed and random-effect of individual and contextual actors associated with non-receipt of routine immunisation (No-RI) among 12–23 months children in India, 2007–2008.
| Model 1 (Empty) | Model 2 (Individual) | Model 3 (Contextual) | Model 4 (Individual & Contextual) | |
| Religion Hindu (reference) | 1 | 1 | ||
| Muslims | 2.10 (1.89–2.33) | 2.00 (1.81–2.22) | ||
| Others/no religion | 1.09 (0.89–1.34) | 1.13 (0.92–1.33) | ||
| Household Wealth index | ||||
| Poorest | 1.84 (1.53–2.19) | 2.27 (1.73–2.73) | ||
| Poorer | 1.55 (1.29–1.83) | 1.89 (1.59–2.27) | ||
| Middle | 1.33 (1.12–1.57) | 1.58 (1.32–1.88) | ||
| Richer | 1.24 (1.05–1.45) | 1.39 (1.17–1.64) | ||
| Richest (reference) | 1 | 1 | ||
| Contextual-level factors | ||||
| Rural vs. Urban | 1.27 (1.14–1.41) | 0.61 (0.54–0.68) | ||
| EAG-Assam states versus other states | 5.96 (2.12–15.04) | 1.91 (0.77–6.73) | ||
| Community Illiterate women | 0.88 (0.73–1.07) | 1.00 (0.99–1.00) | ||
| Community Poverty | 1.02 (0.50–1.86) | 0.84 (0.62–1.11) | ||
| Variance (SE) | ||||
| Community | 1.36 (0.07) | 1.03 (0.07) | 1.36 (0.07) | 1.01 (0.06) |
| District | 0.69 (0.06) | 0.37 (0.04) | 0.68 (0.06) | 0.37 (0.04) |
| State | 2.10 (0.63) | 0.97 (0.32) | 1.76 (0.54) | 0.99 (0.36) |
| MOR | ||||
| Community | 3.04 (2.89–3.21) | 2.63 (2.46–2.80) | 3.05 (2.89–3.22) | 2.61 (2.47–2.77) |
| District | 2.21 (2.06–2.39) | 1.79 (1.68–1.90) | 2.20 (2.05–3.37) | 1.79 (1.69–1.91) |
| State | 3.98 (2.83–6.11) | 2.56 (1.99–3.53) | 3.54 (2.56–5.32) | 2.58 (1.77–3.72) |
EAG: Empowered- Action Group; MOR: Median odds ratio; 95% CrI: Credible interval.
Tables 9&10 presents results stratified by area of residence (rural versus urban) for CUV and no-RI. Maternal education attainment continued to influence the risk of being CUV uniquely among urban children. Conversely, father’s schooling remained significant in urban and rural areas although its magnitude was larger in urban areas. Interestingly, the household wealth index had almost no effect on risk of being CUV in urban areas but remained a strong determinant of CUV in rural settings. Maternal education remained the strongest determinant of No-RI in both settings whilst the influence of higher birth rank appeared more marked as well as being a girl in urban area.
Table 9. Four-level multivariate logistic regression modeling of individual factors associated with non-vaccination among 12–23 months children by area of residence in India, 2007–2008 (model 5).
| Rural CUV | Rural No-RI | Urban CUV | Urban No-RI | |
| Sex Female vs. male | 1.05 (0.95–1.15) | 1.16 (1.09–1.23) | 1.26 (1.01–1.61) | 1.34 (1.13–1.59) |
| Birth order 1 (reference) | 1 | 1 | 1 | 1 |
| 2 | 0.93 (0.80–1.07) | 1.07 (0.96–1.18) | 0.93 (0.64–1.27) | 1.22 (0.94–1.57) |
| 3 | 0.94 (0.79–1.10) | 1.14 (1.01–1.27) | 1.08 (0.71–1.53) | 1.88 (1.40–2.51) |
| ≥4 | 1.13 (0.95–1.32) | 1.40 (1.26–1.55) | 0.88 (0.56–1.27) | 1.83 (1.34–2.47) |
| Mother’s schooling, years | ||||
| 0 | 1.09 (0.92–1.83) | 4.55 (2.55–6.33) | 3.39 (1.43–7.88) | 7.39 (4.10–13.84) |
| 1–5 | 0.88 (0.57–1.42) | 3.45 (1.89–4.82) | 1.60 (0.65–3.79) | 3.73 (1.95–7.34) |
| 6–8 | 0.77 (0.49–1.24) | 2.47 (1.36–3.47) | 2.29 (0.98–5.16) | 4.06 (2.22–7.53) |
| 9–12 | 0.48 (0.30–1.78) | 1.96 (1.06–2.81) | 1.25 (0.53–2.79) | 2.30 (1.25–4.18) |
| ≥13 (reference) | 1 | 1 | 1 | 1 |
| Mother’s age group, years | ||||
| 15–19 (reference) | 1 | 1 | 1 | 1 |
| 20–24 | 0.93 (0.75–1.13) | 0.81 (0.69–0.91) | 1.87 (1.01–3.35) | 0.75 (0.52–1.03) |
| 25–34 | 0.98 (0.77–1.18) | 0.75 (0.63–0.86) | 2.03 (1.04–3.66) | 0.67 (0.44–0.92) |
| 35–49 | 0.88 (0.67–1.15) | 0.72 (0.59–0.85) | 1.81 (0.80–3.55) | 0.63 (0.38–0.97) |
| Less than 4 ANC visits | 1.65 (1.08–2.77) | 1.66 (1.32–2.01) | 1.31 (0.78–2.07) | 1.85 (1.42–2.35) |
| No TTI during pregnancy | 4.33 (3.78–4.91) | 4.05 (3.76–4.36) | 3.95 (3.06–5.03) | 3.83 (3.14–4.64) |
| No PNC within 2 weeks | 1.75 (1.49–2.00) | 1.59 (1.46–1.73) | 1.91 (1.40–2.59) | 1.58 (1.26–1.87) |
| Father’s schooling, years | ||||
| 0 | 1.85 (1.36–2.52) | 1.83 (1.49–2.48) | 2.20 (1.15–3.91) | 2.56 (1.54–4.48) |
| 1–5 | 1.47 (1.09–1.98) | 1.54 (1.25–1.94) | 1.79 (1.01–3.16) | 1.93 (1.12–3.35) |
| 6–8 | 1.44 (1.06–1.96) | 1.41 (1.15–1.77) | 1.90 (1.01–3.21) | 1.75 (1.05–3.03) |
| 9–12 | 1.20 (0.87–1.61) | 1.23 (1.01–1.53) | 1.40 (0.78–2.31) | 1.35 (0.83–2.24) |
| ≥13 (reference) | 1 | 1 | 1 | 1 |
CUV: received none of the eight basic vaccine doses; No-RI: received none of the five recommended vaccine doses delivered exclusively through the routine immunisation system; ANC: Antenatal care; PNC: Postnatal care; TTI: tetanus Toxin injection; 95% CrI: Credible interval.
Table 10. Four-level multivariate logistic regression modeling of individual and contextual factors associated with non-vaccination among 12–23 months children by area of residence in India, 2007–2008 (model 5).
| Rural CUV | Rural No-RI | Urban CUV | Urban No-RI | |
| Caste group General (reference) | 1 | 1 | 1 | 1 |
| Other backward caste (OBC) | 1.10 (0.89–1.31) | 1.10 (1.00–1.22) | 0.79 (0.55–1.12) | 1.09 (0.85–1.37) |
| Scheduled caste | 1.20 (0.96–1.46) | 1.13 (1.01–1.28) | 1.12 (0.75–1.64) | 1.25 (0.93–1.69) |
| Scheduled tribe | 1.50 (1.17–1.86) | 1.39 (1.20–1.61) | 1.38 (0.77–2.38) | 1.28 (0.79–2.00) |
| Religion Hindu (reference) | 1 | 1 | 1 | 1 |
| Muslims | 1.88 (1.52–2.31) | 2.01 (1.78–2.26) | 1.74 (1.26–2.36) | 1.96 (1.52–2.46) |
| Others/no religion | 1.09 (0.81–1.44) | 1.18 (0.95–1.45) | 1.37 (0.75–2.26) | 1.20 (0.66–1.95) |
| Household Wealth index | ||||
| Poorest | 2.95 (1.90–3.43) | 2.39 (2.00–2.92) | 1.21 (0.61–2.18) | 1.40 (0.88–2.06) |
| Poorer | 2.47 (1.59–3.72) | 1.95 (1.63–2.39) | 1.42 (0.84–2.26) | 1.77 (1.23–2.44) |
| Middle | 2.10 (1.37–3.16) | 1.67 (1.39–2.06) | 1.60 (1.04–2.38) | 1.20 (0.87–1.60) |
| Richer | 1.67 (1.08–2.47) | 1.46 (1.20–1.81) | 1.39 (1.01–1.95) | 1.19 (0.93–1.49) |
| Richest (reference) | 1 | 1 | 1 | 1 |
| Contextual-level factors | ||||
| EAG-Assam versus other states | 1.33 (0.70–2.26) | 1.33 (0.79–1.77) | 1.53 (0.51–3.97) | 1.54 (0.61–2.85) |
| Community Illiterate women | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | 0.99 (0.99–1.00) | 0.99 (0.99–1.00) |
| Community poverty | 0.88 (0.57–1.31) | 0.87 (0.63–1.15) | 1.05 (0.36–2.45) | 0.54 (0.22–1.31) |
| Variance (SE) | ||||
| Community | 1.62 (0.14) | 1.02 (0.07) | 0.0007 (0.0002) | 0.79 (0.14) |
| District | 0.84 (0.09) | 0.40 (0.04) | 0.69 (0.17) | 0.32 (0.09) |
| State | 1.4 90.39) | 0.96 (0.32) | 0.82 (0.41) | 0.62 (0.29) |
| MOR | ||||
| Community | 3.37 (3.07–3.81) | 2.62 (2.46–2.79) | 1.02 (NA) | 2.12 (1.58–3.03) |
| District | 2.40 (1.19–2.64) | 1.82 (1.71–1.95) | 2.21 (1.82–2.68) | 1.72 (1.50–1.99) |
| State | 2.77 (2.06–3.98) | 2.54 (1.96–3.50) | 2.38 (1.68–3.62) | 2.33 (2.01–2.66) |
MOR: Median odds ratio; CUV: received none of the eight basic vaccine doses; No-RI: received none of the five recommended vaccine doses delivered exclusively through the routine immunisation system; 95% CrI: Credible interval.
Random effects measures are also presented for all adjusted analyses (Tables 6, 8 and 10). In Table 6, results showed a significant variation of CUV across the communities (u-CUV = 2.04, p<0.0001), districts (v-CUV = 1.15, p<0.0001) and states (f-CUV = 1.93, p = .001). These findings point to significant heterogeneity at each level as confirmed by corresponding MORs. To assess further the influence of compositional and contextual variables on random effects, we compared the null model (Model 1) with the three other models. By controlling for all compositional factors, the proportion of total variation attributed to community, district and state declined. Nonetheless, variation at these three levels remained highly significant (p<0.001), indicating that compositional characteristics may explain only a part of geographic variation. Consistently, MORs confirmed such heterogeneity.
After controlling for defined contextual variables in Model 3, community and district levels variances barely changed in comparison to Model 1 (Tables 6 & 8). Controlling for all compositional variables and contextual variables in Model 4 induced a substantial variances decrease in comparison to Model 1. Strikingly, the procedure showed little effect on proportional change of variance relative to Model 3. Correspondingly, clustering of on receipt of recommended vaccines remained significant at the community-, district- and state-levels, as indicated by respective MOR for CUV [3.44, (95% CrI: 3.14–3.79), 2.39 (95% CrI: 2.17–2.64) and 2.72 (95% CrI: 2.04–3.44)]. In stratified analyses by area of residence (Tables 9 & 10) controlling for all individual and contextual variables, significant variation of the outcome still persisted at community, district and states levels. This feature suggests that models did not fully explain contextual variation of non-vaccination. Furthermore, the level of community was more important in the determination of CUV status in rural settings while the state level was the most prominent in urban areas.
Discussion
This is the first study to analyse unvaccinated children in India in order to appreciate potentially different contextual and compositional determinants associated with different vaccine delivery modes. Using multilevel modelling and the most recent representative probability sample of 65 617 children aged 12 to 23 months recruited from 34 states or territories of India, we found that 4.8% (95% CrI: 4.6–5.1) of Indian children were left out of India’s Universal Immunization Programme and had not received even a single vaccine dose (CUV). Results also showed wide inter-state variation ranging from 0% (Goa and Lakshadweep) to 20.9% (Tripura). In 2014, the World Health Organization certified India polio-free. India’s high-performing polio program will hence downscale efforts in future, and routine immunization services will shoulder the task of reaching every child. By documenting the magnitude of the coverage gap associated with failure to receive routine immunization and associated risk factors, our analysis provides key information to inform service delivery improvements in India. A much higher proportion of children had received no vaccinations from routine services, an indication of weak health systems. The prevalence of No-RI is 12.01% (95% CI: 11.68–12.35%) nationally, ranging from 0% (Lakshadweep) to 25.4% (Tripura). The prevalence of No-RI was above 20% in Tripura, Uttar Pradesh, Meghalaya and Arunachal Pradesh. CUV and no-RI children are concentrated in particular states, increasing the risk of transmitting VPDs to other unvaccinated and undervaccinated children.
Equity in coverage of maternal and child lifesaving interventions such as vaccinations in resource-limited countries remains a major focus of global health agenda [34], [35]. Subsequently, reaching unreached children is recognised as central to this vision [18]. Actually, those left out from vaccinations are thought to be at highest risk of VPDs and are also unlikely to access other essential child health services [36], [37]. Our multilevel analysis identifies key findings that are relevant to understanding the role of certain contextual and compositional factors in influencing non-receipt of any basic vaccine-dose in India, a country concentrating 25% of unvaccinated children globally [6].
Non-vaccination is highly associated with the mother’s and her partner’s educational attainments. Mothers that not reached at least 6 years of schooling had a higher risk to have unvaccinated children. Importantly, the effect of maternal schooling attainment appears less apparent for completely unvaccinated children in rural areas while paternal education appears systematically manifest for both outcomes in all settings. The finding relative to maternal education is consistent with a body of evidence from India and other resources limited settings. Thus, they provide further evidence that mother education remains a strong determinant of child vaccination in certain circumstances [13], [38]–[40]. The finding that husband’ education is associated with childhood vaccination is in line with previous reports [41]. Indeed, the protective role of husband’s education has been recognized [42], [43] as reinforcing factor for mothers propensity to seek for child’s vaccination. Finally, the positive association between parental education and non-vaccination lends credence to the importance of reinforcing demand-related factors.
Of note, three other individual-level effects are notably important. In unadjusted and multivariate models, the risk of being unvaccinated is strongly associated with all the compositional antenatal and postnatal covariates related to health services utilization by mothers. Thus, we found that children born from a mother who had not received tetanus toxin injection during pregnancy had a 4-fold risk of being unvaccinated. Furthermore, unvaccinated children were more likely to have mother who neither attended recommended full ANC visits nor PNC visit within the two weeks following birth. These associations remain significant even after controlling for all individual and contextual variables. These findings highlight the fact that the continuum of care throughout pregnancy and postpartum period is critically important for children vaccination in India. Indeed, the association between child vaccination and prenatal and postnatal care utilisation suggests that this pattern may be indicative of health services attendance during early childhood, as previously reported by Kogan [44]. Moreover, these findings are consistent with those of many others in resources limited settings [45], [46], though Choi & Lee found only such link for the subgroup of rural boys [47].
Socioeconomic factors are consistently linked to non-vaccination [48]–[50]. Accordingly, we showed that household wealth index was inversely associated with non-vaccination through a dose-response pattern while controlling for compositional and contextual variables. Importantly, this association appears mostly marked in rural settings.
Interestingly, our investigation found that the determinants of non-vaccination were similar between CUV and No-RI, but the magnitude of associations for individual factors such as maternal education, tetanus immunization during the pregnancy, ANC visits and child gender were usually stronger among No-RI. In order words, No-RI outcome usually accentuated the force of these associations. This pattern suggests that the polio programme operating largely in campaign mode in parallel to routine vaccination services seems to better reach undeserved groups such as very illiterate parents. Lessons from the polio programme’s approach to reaching underserved population groups may be useful for improving routine immunization services.
Turning to contextual variables, only place of residence was found to be significantly associated to non-vaccination. Meanwhile, residing in a rural area was associated with non-vaccination in unadjusted and multivariate models when considering only contextual factors. Conversely, this variable was found protective when taking into account both compositional and contextual factors. This inverse association between place of residence and non-vaccination contradicts the impressive body of evidence reported from both Asia and Africa [49]–[51]. Nonetheless, other African studies showed that children living in urban places are more likely to be non-vaccinated compared to their rural counterparts [42], [52]. This apparent discrepancy raises the question of whether the so called “urban advantage” remains pertinent in regard to growing urban population and for whom access to health services may be precarious [11], [53], [54].
Overall, even after controlling for observed characteristics, unexplained heterogeneity in non-receipt of any vaccine remains significant at contextual levels net of what could be attributed to compositional factors. In terms of the relative importance of the three contextual levels, the community-level was observed to be relatively more important in rural settings while the state-level appeared more influential in urban areas in the determination of non-receipt of any vaccine. Finally, none of the considered contextual variables seemed to have a greater impact on non-vaccination relative to compositional characteristics. Therefore, the relationship between the non-vaccination and the context may be more complex than captured in this study. The evidence of a state-level clustering effect, as well as the clustering of district and community levels, suggests that unexplained factors should be sought in future analysis. In particular, we could not assess the potential contribution of the availability of health facilities (only available for rural areas in the DHLS-3), state or district level governance.
Our study has several strengths. Firstly, it is original as we used more stringent measures of non-vaccination compared to traditional measure of non-vaccination based only on coverage of DPT1 [6]; second, we modelled the non-receipt of vaccines throughout two different delivery systems; third, we used highly computational but robust statistical techniques within a multilevel framework. Finally, we minimized potential selection bias and achieved nationwide representative estimates (generalization) by using India’s most recent publicly available nationally representative survey data, the DLHS-3.
There are some limitations to this study. The cross-sectional nature of the data limits the ability to draw causal inferences. We also recognized that our study may be potentially limited by the fact that the determination of vaccination status was based mainly on mother or care giver report, which may be less precise than information provided by health card. Nevertheless, this practice is commonly used by the Demographic and Health Surveys (DHS) which form the basis for the DLHS since its first series [55]. Moreover, other studies have shown that mothers’ reports of their children’s vaccination status are fairly accurate [56]–[58]. Finally, additional information on unmeasured individual and community level variables by data source such as health services characteristics that were only available for rural areas, and cultural norms and beliefs, difficult to collect in such large-scale survey, would have also benefited this study.
Our results have potentially important implications for public health policies and programs aimed at reducing non-vaccination in India. At the individual level, the results suggest that health programs need to be adapted geographically and to focus on attracting poor children particularly in rural settings and less educated women and encouraging them to use health services including vaccination. Our findings further reiterate the urgent need for a comprehensive maternal health package that addresses the spectrum of maternal and extended newborn care –envisaged as critical components in achieving targets 4, 5a and 5b of the UN Millennium Development Goals [59]. The persistence of significant community-, district- and state-level variation in non-vaccination illustrates that current large population surveys such as DLHS are insufficient in measuring the range of cultural influences on health-seeking behavior, and more focused-research is needed to understand the dynamics of contextual influences on individuals.
Acknowledgments
We greatly acknowledge the support of the International Institute for Population Sciences, Mumbai for providing data from DLHS-3. We express our gratitude to Georges Karna Koné for his support in preparing vaccination variables.
Funding Statement
DS holds a Canadian Institutes of Health Research Fellowship Award for Health Professionals. DS was also funded by French Rotary District 1690 (Bursary Henri Sabourin) and the Strategic Training Program in Global Health Research, a partnership of the Canadian Institutes of Health Research and the Québec Population Health Research Network. HT holds a salary award (chercheur boursier) from the Fonds de la recherche en santé du Québec. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bryce J, Terreri N, Victora CG, Mason E, Daelmans B, et al. (2006) Countdown to 2015: tracking intervention coverage for child survival. Lancet 368: 1067–1076. [DOI] [PubMed] [Google Scholar]
- 2.Bloom DE (2011) The value of vaccination. Hot Topics in Infection and Immunity in Children VII: Springer. 1–8.
- 3. Keja K, Chan C, Hayden G, Henderson RH (1988) Expanded programme on immunization. World Health Stat Q 41: 59–63. [PubMed] [Google Scholar]
- 4. Andre FE, Booy R, Bock HL, Clemens J, Datta SK, et al. (2008) Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ 86: 140–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duclos P, Okwo-Bele JM, Gacic-Dobo M, Cherian T (2009) Global immunization: status, progress, challenges and future. BMC Int Health Hum Rights 9 Suppl 1S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control Prevention (2013) Global routine vaccination coverage - 2012. MMWR Morb Mortal Wkly Rep 62: 858–861. [PMC free article] [PubMed] [Google Scholar]
- 7. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, et al. (2010) Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375: 1969–1987. [DOI] [PubMed] [Google Scholar]
- 8.Anonymous (2013) Global Immunization Data. In: World Health Organization, editor. Geneva (Switzerland): World Health Organization.
- 9. Mathew JL (2012) Inequity in childhood immunization in India: a systematic review. Indian Pediatr 49: 203–223. [DOI] [PubMed] [Google Scholar]
- 10. Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, et al. (2011) Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999–2009. Vaccine 29: 8215–8221. [DOI] [PubMed] [Google Scholar]
- 11. Agarwal S, Bhanot A, Goindi G (2005) Understanding and addressing childhood immunization coverage in urban slums. Indian Pediatr 42: 653–663. [PubMed] [Google Scholar]
- 12. Corsi DJ, Bassani DG, Kumar R, Awasthi S, Jotkar R, et al. (2009) Gender inequity and age-appropriate immunization coverage in India from 1992 to 2006. BMC Int Health Hum Rights 9 Suppl 1S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parashar S (2005) Moving beyond the mother-child dyad: women's education, child immunization, and the importance of context in rural India. Soc Sci Med 61: 989–1000. [DOI] [PubMed] [Google Scholar]
- 14. Kiros G-E, White MJ (2004) Migration, community context, and child immunization in Ethiopia. Social Science & Medicine 59: 2603–2616. [DOI] [PubMed] [Google Scholar]
- 15. Merlo J, Chaix B, Yang M, Lynch J, Rostam L (2005) A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. Journal of epidemiology and community health 59: 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duncan C, Jones K, Moon G (1998) Context, composition and heterogeneity: using multilevel models in health research. Social Science & Medicine 46: 97–117. [DOI] [PubMed] [Google Scholar]
- 17. Reddy KS, Patel V, Jha P, Paul VK, Kumar AK, et al. (2011) Towards achievement of universal health care in India by 2020: a call to action. Lancet 377: 760–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brearley L, Eggers R, Steinglass R, Vandelaer J (2013) Applying an equity lens in the Decade of Vaccines. Vaccine 31 Suppl 2B103–107. [DOI] [PubMed] [Google Scholar]
- 19.International Institute for Population Sciences (2010) District level household and facility survey (DLHS 3) 2007–08. Mumbai (India): International Institute for Population Sciences. 306p.
- 20. Taneja GS, KS; Mishra (2013) S (2013) Routine Immunization in India: A perspective. Indian J of Community Health 25: 5. [Google Scholar]
- 21. Aylward B, Tangermann R (2011) The global polio eradication initiative: lessons learned and prospects for success. Vaccine 29 Suppl 4D80–85. [DOI] [PubMed] [Google Scholar]
- 22. Grassly NC (2013) The final stages of the global eradication of poliomyelitis. Philos Trans R Soc Lond B Biol Sci 368: 20120140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Griffiths P, Madise N, Whitworth A, Matthews Z (2004) A tale of two continents: a multilevel comparison of the determinants of child nutritional status from selected African and Indian regions. Health Place 10: 183–199. [DOI] [PubMed] [Google Scholar]
- 24. Theall KP, Scribner R, Broyles S, Yu Q, Chotalia J, et al. (2011) Impact of small group size on neighbourhood influences in multilevel models. J Epidemiol Community Health 65: 688–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo G, Zhao H (2000) Multilevel modeling for binary data. Annual review of sociology: 441–462.
- 26.Browne WJ (2009) MCMC estimation in MLwiN. Brsitol (UK): Centre for Multilevel Modelling, University of Bristol.
- 27. Browne WJ, Draper D (2006) A comparison of Bayesian and likelihood-based methods for fitting multilevel models. Bayesian Analysis 1: 473–514. [Google Scholar]
- 28.Rodriguez G, Goldman N (1995) An assessment of estimation procedures for multilevel models with binary responses. Journal of the Royal Statistical Society Series A (Statistics in Society): 73–89.
- 29. Rodriguez G, Goldman N (2001) Improved estimation procedures for multilevel models with binary response: a case-study. Journal of the Royal Statistical Society: Series A (Statistics in Society) 164: 339–355. [Google Scholar]
- 30.Leckie G, Charlton C (2011) runmlwin: Stata module for fitting multilevel models in the MLwiN software package.
- 31. Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A (2002) Bayesian measures of model complexity and fit. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 64: 583–639. [Google Scholar]
- 32. Merlo J, Ohlsson H, Lynch KF, Chaix B, Subramanian S (2009) Individual and collective bodies: using measures of variance and association in contextual epidemiology. Journal of epidemiology and community health 63: 1043–1048. [DOI] [PubMed] [Google Scholar]
- 33. Larsen K, Merlo J (2005) Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol 161: 81–88. [DOI] [PubMed] [Google Scholar]
- 34. Barros AJ, Ronsmans C, Axelson H, Loaiza E, Bertoldi AD, et al. (2012) Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet 379: 1225–1233. [DOI] [PubMed] [Google Scholar]
- 35. Victora CG, Barros AJ, Axelson H, Bhutta ZA, Chopra M, et al. (2012) How changes in coverage affect equity in maternal and child health interventions in 35 Countdown to 2015 countries: an analysis of national surveys. Lancet 380: 1149–1156. [DOI] [PubMed] [Google Scholar]
- 36. Anand A, Luman ET, O'Connor PM (2012) Building on success–potential to improve coverage of multiple health interventions through integrated delivery with routine childhood vaccination. J Infect Dis 205 Suppl 1S28–39. [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization W (2006) Challenges in global immunization and the Global Immunization Vision and Strategy 2006–2015. Wkly Epidemiol Rec 81: 190–195. [PubMed] [Google Scholar]
- 38. Vikram K, Vanneman R, Desai S (2012) Linkages between maternal education and childhood immunization in India. Soc Sci Med 75: 331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gage AJ, Sommerfelt AE, Piani AL (1997) Household Structure and Childhood Immunization in Niger and Nigeria. Demography 34: 295–309. [PubMed] [Google Scholar]
- 40. Abuya BA, Onsomu EO, Kimani JK, Moore D (2011) Influence of maternal education on child immunization and stunting in Kenya. Matern Child Health J 15: 1389–1399. [DOI] [PubMed] [Google Scholar]
- 41. Desai S, Alva S (1998) Maternal education and child health: Is there a strong causal relationship? Demography 35: 71–81. [PubMed] [Google Scholar]
- 42. Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD (2012) Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: a multilevel analysis. PLoS One 7: e37905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steele F, Diamond I, Amin S (1996) Immunization uptake in rural Bangladesh: a multilevel analysis. Journal of the Royal Statistical Society Series A (Statistics in Society): 289–299.
- 44. Kogan MD, Alexander GR, Jack BW, Allen MC (1998) The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United States. Pediatrics 102: 25–30. [DOI] [PubMed] [Google Scholar]
- 45. Sullivan MC, Tegegn A, Tessema F, Galea S, Hadley C (2010) Minding the immunization gap: family characteristics associated with completion rates in rural Ethiopia. J Community Health 35: 53–59. [DOI] [PubMed] [Google Scholar]
- 46.Antai D (2011) Rural-urban inequities in childhood immunisation in Nigeria: The role of community contexts. African Journal of Primary Health Care & Family Medicine 3: 8 pages.
- 47. Choi JY, Lee SH (2006) Does prenatal care increase access to child immunization? Gender bias among children in India. Soc Sci Med 63: 107–117. [DOI] [PubMed] [Google Scholar]
- 48. Smith PJ, Chu SY, Barker LE (2004) Children who have received no vaccines: who are they and where do they live? Pediatrics 114: 187–195. [DOI] [PubMed] [Google Scholar]
- 49. Gaudin S, Yazbeck AS (2006) Immunization in India 1993–1999: wealth, gender, and regional inequalities revisited. Soc Sci Med 62: 694–706. [DOI] [PubMed] [Google Scholar]
- 50. Lauridsen J, Pradhan J (2011) Socio-economic inequality of immunization coverage in India. Health Econ Rev 1: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Uddin MJ, Koehlmoos TP, Saha NC, Khan IA (2010) Child immunization coverage in rural hard-to-reach areas of Bangladesh. Vaccine 28: 1221–1225. [DOI] [PubMed] [Google Scholar]
- 52. Cassell JA, Leach M, Fairhead JR, Small M, Mercer CH (2006) The social shaping of childhood vaccination practice in rural and urban Gambia. Health Policy Plan 21: 373–391. [DOI] [PubMed] [Google Scholar]
- 53. Matthews Z, Channon A, Neal S, Osrin D, Madise N, et al. (2010) Examining the “urban advantage” in maternal health care in developing countries. PLoS Med 7: e1000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ghei K, Agarwal S, Subramanyam MA, Subramanian SV (2010) Association between child immunization and availability of health infrastructure in slums in India. Arch Pediatr Adolesc Med 164: 243–249. [DOI] [PubMed] [Google Scholar]
- 55.Boerma JT, Bicego GT (1993) The quality of data on child immunization in the DHS-I surveys. An assessment of the quality of health data in DHS-I surveys Calverton (MD): Macro International: 81–93.
- 56. Langsten R, Hill K (1998) The accuracy of mothers' reports of child vaccination: evidence from rural Egypt. Soc Sci Med 46: 1205–1212. [DOI] [PubMed] [Google Scholar]
- 57. George K, Victor S, Abel R (1990) Reliability of mother as an informant with regard to immunisation. Indian journal of pediatrics 57: 588–590. [DOI] [PubMed] [Google Scholar]
- 58. Gareaballah E, Loevinsohn B (1989) The accuracy of mother's reports about their children's vaccination status. Bulletin of the World Health Organization 67: 669. [PMC free article] [PubMed] [Google Scholar]
- 59. Travis P, Bennett S, Haines A, Pang T, Bhutta Z, et al. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet 364: 900–906. [DOI] [PubMed] [Google Scholar]