Abstract
Background
Several occupational stress studies of healthcare workers have predicted a high prevalence of anxiety symptoms, which can affect their quality of life and the care that they provide. However, few studies have been conducted among community healthcare workers in China. We attempted to explore whether burnout mediates the association between occupational stress and anxiety symptoms.
Methods
A cross-sectional survey was completed in Liaoning Province, China from November to December 2012. A total of 1,752 healthcare workers from 52 Community Health Centers participated in this study, and all participants were given self-administered questionnaires. These questionnaires addressed the following aspects: the Zung Self-Rating Anxiety Scale, the Chinese version of the effort-reward imbalance scale and the Maslach Burnout Inventory–General Survey. Finally, the study included 1,243 effective respondents (effective response rate, 70.95%). Hierarchical linear regression analysis, performed with SPSS 17.0, was used to estimate the effect of burnout.
Results
The prevalence of anxiety symptoms among the community healthcare workers was 38.0%. After adjusting for demographic characteristics, the effort–reward ratio and overcommitment positively predicted anxiety symptoms. Meanwhile, the effort–reward ratio and overcommitment were positively related to the emotional exhaustion and cynicism subscales of burnout. In addition, the emotional exhaustion and cynicism subscales were positively related to anxiety symptoms. Thus, there is a link between burnout, occupational stress and anxiety symptoms.
Conclusions
Burnout mediates the effect of occupational stress on anxiety symptoms. To effectively reduce the impact of occupational stress on anxiety symptoms, burnout management should be considered.
Introduction
With improved economic development, aging populations and lifestyle changes, an increasing number of chronic diseases seriously threaten population health in China. In such cases, more cost-effective, convenient primary care is particularly important. In the latest health care reform, China aimed to ensure equitable access to basic health care for its residents by building a strong, primary-care-based delivery system [1]. However, the Community Health Centers (CHCs) form the main pillar of primary-care providers in urban areas [2]. To maintain the desirability of primary healthcare, it is important to promote the physical and mental health of healthcare workers. However, few studies have investigated anxiety in CHC healthcare workers.
A previous study has shown that healthcare workers have a greater risk of developing anxiety (due to fear of making mistakes at work or impending weekends on duty), which is one of the most common psychiatric conditions encountered in primary care [3], [4]. Anxiety “is a psychologic and physiologic state characterized by cognitive, somatic, emotional and behavioral components” [5]. Anxiety is also described as a feeling of fear related to some uncertain or future event or mental distress that is caused by a threat to a person or his/her values [6]. A recent study reported that anxiety is associated with job burnout, sleeping problems and lifestyle factors [7]. Increasingly, data have indicated the adverse effects of anxiety. Anxiety can impair healthcare workers' quality of life, induce immune system changes [8], affect the safety of their patients and influence their job performance, which is reflected in both the greater risk of mistakes and the effects on their interactions with patients and colleagues [7], [9]. Healthcare worker anxiety undoubtedly has profound social effects. Many epidemiologic studies have suggested that psychiatric and non-psychiatric patients with chronic anxiety may be at risk for developing coronary heart disease [10]. To promote health in healthcare workers and to ensure that they provide high-quality care services, more attention should be directed toward reducing anxiety in healthcare workers.
Occupational stress has been identified as a risk factor for anxiety symptoms [7], [11]. Job demands, extrinsic effort, and over-commitment were associated with higher levels of anxiety [12]. Peplińska A et al. proposed that marital satisfaction mediated the relation between stress and anxiety [13]. According to the results of previous studies, occupational stress not only exerts a direct effect but also has an indirect effect on anxiety symptoms.
In particular, the effect of occupational stress on physical and mental illness has attracted attention [14]. Occupational or work-related stress is undoubtedly a major cause of mental health concerns worldwide [15]. However, healthcare workers, including physicians, nurses, medical technicians and administrative staff, experience high levels of occupational stress because of their heavy workloads, extended working hours and time-related pressure [16]. Additionally, Chinese healthcare workers are likely more vulnerable to increasing occupational stress because of the great demand for service quality, hospital-patient conflicts and health care reform. The mechanism by which occupational stress affects anxiety is worth exploring to provide efficient strategies for anxiety intervention.
Burnout is a well-known psychological response in healthcare workers [17]. In addition, burnout is consistently associated with anxiety symptoms [18]–[20]. Attention should be focused on preventing exhaustion from work with the purpose of lessening anxiety symptoms [7]. The outcome of continued exposure to overwork, resulting in a progressive inability to perform job responsibilities, has been termed ‘burnout’ [8]. Burnout is characterized by emotional exhaustion (feeling emotionally overloaded with work), cynicism (active disengagement from one's job) and inefficacy (decreased personal accomplishment) [21]. Burnout is a prolonged response to chronic job-related stressors; therefore, it has a special significance in health care, in which staff experience both emotional and physical stresses [22]. High burnout scores are usually associated with the following variables: low salary, employment sector, age group, feeling of professional inadequacy and feelings of personal dissatisfaction [23]. Several studies have shown that occupational stress has significant power in predicting burnout [24]–[26], particularly in the emotional exhaustion and cynicism dimensions.
To the best of our knowledge, the effect of occupational stress on anxiety symptoms has been tested, but few studies have addressed the potential mechanism underlying the relationship between occupational stress and anxiety symptoms. Moreover, Gilbert et al. reported that burnout mediates the relationship between structural empowerment and organizational citizenship behaviors [27]. However, whether burnout mediates the relationship between occupational stress and anxiety symptoms in healthcare workers who mainly provide primary care in CHCs has not been investigated. To explore the mechanism between occupational stress and anxiety symptoms, it is important to understand the role of burnout in this relationship.
In this study, we investigated the prevalence of anxiety symptoms in community healthcare workers in China and hypothesized that burnout mediates the relationship between occupational stress and anxiety symptoms.
Methods
Ethics Statement
The study procedures were approved by the relevant ethical standards of the Committee on Human Experimentation of China Medical University. Written informed consent was obtained from each participant, all of whom voluntarily participated in the study. We protected the privacy and anonymity of individuals involved in our research.
Study Population and Procedure
A cross-sectional survey was conducted in Liaoning Province, China from November to December 2012. Participants in this study were selected using multi-stages cluster sampling. In the first stage, three cities at each financial level (GDP<100 billion, GDP = 100–200 billion and GDP>200 billion) were randomly selected based on the economic development of Liaoning Province. In the second stage, we randomly chose municipal districts from the 1/2 ratio from each selected city. In the third stage, three CHCs were randomly chosen from each selected municipal district. All healthcare workers in each CHC were invited to participate in our study. In total, 1752 healthcare workers were selected from fifty-two CHCs in nine cities. After all participants provided written informed consent, they received a self-administered questionnaire. We received effective responses from 1243 individuals (effective response rate, 70.95%), who formed the study sample. The individuals in this manuscript provided written informed consent (as outlined in the PLOS consent form) to publish these case details.
Measurement of Anxiety Symptoms
The Zung Self-Rating Anxiety Scale (SAS) was used to measure the anxiety related symptoms of the healthcare workers. This scale was prepared by Zung in 1971 [28] to evaluate the severity of anxiety symptoms in the investigated objects; it consists of 20 items. Each item is scored on a scale of 1–4 (never or occasionally, sometimes, frequently and most of the time), and the final score ranges from 20 to 80. In accordance with the Chinese norm, we defined the anxiety symptoms for a total raw score ≥40 [29]. Additionally, a higher score represented more serious anxiety symptoms.
The Chinese version of the questionnaire has previously been used in Chinese populations and is reliable [30], [31]. In the present study, Cronbach's alpha in SAS was 0.85. After revising several items, the confirmatory factory analysis confirmed the validity of the scale (RMSEA = 0.071, CFI = 0.902, GFI = 0.918).
Measurement of Occupational Stress
The effort-reward imbalance (ERI) model was first proposed by Siegrist in 1996 [32] to explain the psychological well-being in the workplace. This model emphasizes the mismatch between the high effort that individuals exert and the low reward they receive in occupational life, in which rewards are provided as money, esteem and career opportunities, including job security [33], [34].
The Chinese version of the ERI questionnaire, translated by Li and Yang, was used in this study [35]. The scale consisted of the following three dimensions: effort (6 items), reward (11 items) and overcommitment (6 items). The effort and reward dimensions represent extrinsic stress, and overcommitment represents intrinsic stress. For the effort and reward subscale, each item is scored from 1 to 5; 1 indicates the lack of a particularly stressful experience, and 5 indicates a high-stress experience. Participants answered the items in two steps. First, they indicated whether they agreed or disagreed with the item's description of their work situation; then, they were asked to evaluate how distressed they feel (from ‘not distressed’ to ‘very distressed’). The effort–reward ratio (ERR) is calculated with a predefined algorithm [36] and is calculated by dividing the effort score by the reward score, for which the latter score is multiplied by a correction factor of 6/11. For the overcommitment subscale, each item is scored from 1 (full disagreement) to 4 (full agreement).
The Chinese version of the ERI questionnaire is a reliable, valid instrument for measuring psychosocial stress at work, particularly among Chinese healthcare workers [35]. Cronbach's alpha for the effort, reward and overcommitment are reported as 0.77, 0.81 and 0.66, respectively [37]. In our study, Cronbach's alpha for the effort, reward and overcommitment was 0.85, 0.89 and 0.71, respectively. After revising seven items, the confirmatory factory analysis confirmed that the Chinese version of the ERI had a satisfactory goodness-of-fit (RMSEA = 0.057, CFI = 0.923, GFI = 0.925).
Measurement of Burnout
Burnout was measured by the Maslach Burnout Inventory-General Survey (MBI-GS) [38], which includes the following three dimensions: emotional exhaustion (EE), cynicism (CY) and professional efficacy (PE). The total scale consists of 15 items, with five items measuring the EE subscale, four items measuring the CY subscale and six items measuring the PE subscale. Additionally, each item is rated from 0 (never) to 6 (every day) according to how often the statement is experienced [39]. A greater degree of burnout is predicted by higher scores for the emotion exhaustion and cynicism subscales and by lower scores for the professional efficacy subscale.
The Chinese version of the BMI-GS has high validity and reliability among Chinese medical professionals [40]. In our study, Cronbach's alpha was 0.84 for the BMI-GS and 0.94, 0.92 and 0.93 for the EE, CY and PE subscales, respectively. After revising ten items, the confirmatory factory analysis confirmed that the Chinese version of the BMI-GS had a satisfactory goodness-of-fit (RMSEA = 0.079, CFI = 0.963, GFI = 0.929).
Demographic Characteristics
The length of employment (years), weekly working hours and marital status were obtained in this study. Marital status was categorized as single, married/cohabitation and divorced/ separated/widow. The length of employment (working years) was categorized as ≤10 years, 11–20 years, 21–30 years and >30 years. The weekly working hours was categorized as ≤40 hours and >40 hours.
Statistical Analysis
The study variables were compared among the marital status groups, length of employment groups and weekly working days groups by an independent-samples T-test and one-way analysis of variance (ANOVA). Pearson's correlation coefficients were used to examine the correlations among the study variables. Multiple regression analysis using the hierarchical stepwise method was applied to examine whether burnout played a mediating role in the association between occupational stress and anxiety symptoms, according to the criteria proposed by Baron and Kenny [41]. In the regression equation, occupational stress was modeled as the independent variable, anxiety symptoms as the dependent variable, burnout as the mediator, and length of employment as the control variable. According to Baron and Kenny, for burnout to be a mediator between occupational stress and anxiety symptoms, the following four conditions should be met: (1) occupational stress significantly predicts anxiety symptoms; (2) occupational stress significantly predicts burnout; (3) burnout significantly predicts anxiety symptoms; and (4) the relationship between occupational stress and anxiety symptoms is reduced or insignificant upon the addition of burnout.
Before the regression analysis, we measured tolerance and variance to exclude multicollinearity. The independent variables were entered in the hierarchical linear regression equation in three steps. In the first step, the length of employment was added as the control variable; according to one-way ANOVA analysis, the only difference in the anxiety symptoms was for the length of employment. All significant occupational stress variables, including ERR and overcommitment, were included in the second step. All significant burnout variables, such as EE, CY and PE, were included in the third step. Additionally, we performed the Sobel test to determine the mediation role of burnout [42]. Except for the confirmatory factor analysis, all analyses were performed using SPSS 17.0 for Windows, and statistical significance was defined as p<0.05 (two-tailed). Confirmatory factor analysis was performed using Amos 17.0.
Results
Characteristics of the Study Population and the Prevalence of Anxiety Symptoms
The length of employment averaged 18.2 years (standard deviation [SD] 10.8), with 32.2% (400) of the participants working more than 40 hours per week; 79.3% (985) were married or cohabiting. The mean anxiety symptom score among the participants in the present study was 37.7 (SD 9.7), and the prevalence of anxiety symptoms was 38.0%.
There were significant differences in all study variables for the length of employment (p<0.01). The EE (p<0.05) and CY (p<0.001) scores differed across weekly working hours. However, no significant difference was observed in the weekly working hours groups with respect to ERR, overcommitment, PE and anxiety symptoms. Within each marital status group, there was only a significant difference in the score for overcommitment. The participant characteristics and distributions of anxiety symptoms for the categorical variables are shown in Table 1.
Table 1. Participant characteristics and the distributions of anxiety symptoms by categorical variable.
| Category | Subcategory | Result (%) | Anxiety symptoms |
| Mean (SD) | |||
| Length of employment | ≤10 yr | 357 (28.7) | 39.1 (10.0) |
| 11–20 yr | 390 (31.4) | 37.3 (9.5) | |
| 21–30 yr | 328 (26.4) | 37.4 (9.3) | |
| >30 yr | 168 (13.5) | 35.9 (9.9) | |
| F | 4.834 | ||
| p | 0.002 | ||
| Weekly working hours | ≤40 hr | 843 (67.8) | 37.5 (9.5) |
| >40 hr | 400 (32.2) | 38.1 (10.2) | |
| t | −1.040 | ||
| p | 0.299 | ||
| Marital status | single | 188 (15.1) | 37.9 (9.8) |
| married/cohabitation | 985 (79.3) | 37.6 (9.7) | |
| divorced/separated/widow | 70 (5.6) | 38.0 (10.1) | |
| F | 0.093 | ||
| p | 0.911 |
The Relationship Between Occupational Stress, Burnout and Anxiety Symptoms
Correlations between the study variables are shown in Table 2. Length of employment was negatively related to ERR, EE, CY and anxiety symptoms. ERR, overcommitment, EE and CY were positively correlated with anxiety symptoms, whereas the length of employment and PE were negatively correlated with anxiety symptoms. ERR had a significant, positive relationship with EE and CY, and overcommitment had a significant, positive correlation with all three burnout dimensions.
Table 2. Means, standard deviations (SD) and correlations of all variables.
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | |
| 1. Length of employment | 18.2 (10.8) | ||||||
| Occupational stress | |||||||
| 2. Effort-reward ratio | 0.8 (0.3) | −0.08** | |||||
| 3. Over commitment | 15.5 (3.0) | 0.11** | 0.27** | ||||
| Burnout | |||||||
| 4. Emotional exhaustion | 10.1 (6.5) | −0.10** | 0.49** | 0.39** | |||
| 5. Cynicism | 5.7 (5.2) | −0.14** | 0.36** | 0.16** | 0.60** | ||
| 6. Professional efficacy | 24.1 (9.3) | 0.08** | −0.06* | 0.06** | 0.01 | −0.21** | |
| Anxiety | |||||||
| 7. Anxiety symptoms | 37.7 (9.7) | −0.10** | 0.34** | 0.18** | 0.46** | 0.49** | −0.26** |
*p<0.05, **p<0.01 (two-tailed).
Burnout as a Mediator of the Relationship between Occupational Stress and Anxiety Symptoms
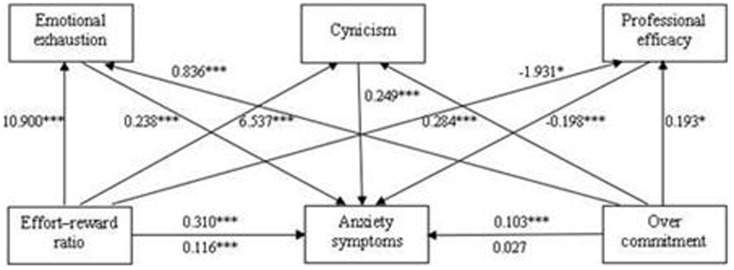
The results of the hierarchical linear regression analysis are shown in Table 3. The control variable (length of employment) significantly predicted anxiety symptoms in the first step (R2 = 0.009). ERR and overcommitment were significant predictors of anxiety symptoms in the second step and accounted for 12.3% of the variance. In the third step, EE and CY positively predicted anxiety symptoms, whereas PE negatively predicted anxiety symptoms, which explained an additional 19.3% of the variance. When EE, CY and PE were included, the relationship between ERR and anxiety symptoms was significantly reduced (from β = 0.310 to β = 0.116, p<0.001; Sobel test, z = 12.05, p<0.001), whereas overcommitment failed to reach the level of significance (from β = 0.103 to β = 0.027, p>0.05; Sobel test, z = 7.68, p<0.001). Therefore, burnout mediated the effect of occupational stress on anxiety symptoms (depicted in Figure 1).
Table 3. Hierarchical linear regression analysis results.
| Anxiety symptoms | |||
| Step 1 | Step 2 | Step 3 | |
| Length of employment | −0.097** | −0.085** | −0.019 |
| Effort–reward ratio | 0.310*** | 0.116*** | |
| Over commitment | 0.103*** | 0.027 | |
| Emotional exhaustion | 0.238*** | ||
| Cynicism | 0.249*** | ||
| Professional efficacy | −0.198*** | ||
| R2 | 0.009 | 0.133 | 0.326 |
| ΔR2 | 0.009** | 0.123*** | 0.193*** |
*p<0.05, ** p<0.01, *** p<0.001 (two-tailed).
Figure 1. The mediating model: relationships between occupational stress and anxiety symptoms.
β–coefficient above the line: without the mediation; β–coefficient below the line: with the mediation. * p<0.05, *** p<0.001.
Discussion
The subjects in this study were selected from Liaoning Province using multistage cluster sampling. The subjects seemed to be representative of our study population, allowing for generalization of our conclusions. We examined the prevalence of anxiety symptoms and explored the relationship between occupational stress and anxiety symptoms in community healthcare workers in China. In total, 38.0% of the healthcare workers had anxiety symptoms. The prevalence was more than twice the prevalence in Chinese medical students (12.5%) [28] and the general population in Australia [43], as well as the prevalence for the elderly general population reported by Schwarz et al. [44].
The level of stress in healthcare workers has attracted increasing attention because of concern for the health of the individuals themselves and because of the possible impact on the quality of patient care [45]. Several studies have shown that healthcare workers, particularly nurses, have a greater risk than that of other professionals of developing emotional distress from job stress, such as burnout, anxiety and depression [46]. Rapid economic development, medical reform, aging populations, a shortage of qualified personnel and the growing burden of chronic diseases increase the job demands on community healthcare workers who are expected to meet their patients' basic health needs through effective, economic, comprehensive and continuous services [1], [47], [48]. Thus, in addition to their default challenges, healthcare providers have to balance the expectations of funding agencies, administrators and patients. This result is further complicated by the geographical inequity of health resources, fierce competition over work positions, problematic scheduling associated with shiftwork, emotional issues from handling illness or death, working relationships, demand for providing better medical services and increasingly complex doctor-patient relationship [11], [48]–[50], all of which increase a healthcare provider's workload. Of course, the challenges with which they are faced are not limited to those described above. The reward these workers receive is usually insufficient because of their low salaries. When intense effort is not met with adequate rewards, anxiety is more likely to develop.
The association between occupational stress and anxiety symptoms was consistent with a previously published study [51], in which both the positive effect of the extrinsic stress (ERR), and the effect of intrinsic stress (overcommitment) on anxiety symptoms was significant. Reasonable financial compensation and other effective strategies should be provided to balance the workload and reward. A possible explanation for the significance of overcommitment is that 32.2% of healthcare workers work more than 40 hours per week, and work is a significant part of their daily life. These healthcare workers do not have sufficient personal lives, which would otherwise relieve their stress.
In this study, we examined the relationship between the dimensions of burnout and anxiety symptoms. Emotional exhaustion and cynicism were positively related to anxiety symptoms, and professional efficacy was negatively related to anxiety symptoms. These results were correspondent with the results of a previous study [7]. Among Chinese healthcare workers, feeling emotionally overloaded with work or active disengagement from their work seems to make individuals prone to anxiety symptoms. They would fear making mistakes or impending weekends on duty.
Moreover, we found that length of employment was negatively related to ERR, emotional exhaustion, cynicism and anxiety symptoms. One possible reason for the negative relationship between length of employment and ERR is that the longer healthcare workers work, the more reward they achieve, such as a raise in salary. In this case, we can explain the relationship between length of employment and emotional exhaustion, cynicism and anxiety symptoms by the effect of occupational stress on burnout and anxiety symptoms.
As previously mentioned, more attention should be given to reducing occupational stress and alleviating anxiety symptoms in healthcare workers. We attempted to explore the mechanism by which occupational stress affects anxiety symptoms. We hope our results can help to develop effective interventions for anxiety.
This study is the first to verify that burnout mediates the association between occupational stress and anxiety symptoms in community healthcare workers in China. Apart from the direct effect of occupational stress on anxiety symptoms, the results of this study indicated that through the mediation of burnout, occupational stress could also affect anxiety symptoms. High occupational stress may enhance burnout, thereby causing anxiety. Health managers should be aware of the prevalence of emotional exhaustion and cynicism in the workplace to ensure that they develop strategies to advance professional efficacy and to improve the health status of healthcare works. Gómez-Gascón et al. researched interventions for preventing and treating burnout in primary health care professionals [52]; the authors reported that organizational measures are important for preventing burnout syndrome. Additionally, healthcare professionals should be provided with coping strategies. Another study in Canada showed that psychological empowerment in healthcare workers can reduce the effects of stressors on burnout [47].
This study has some limitations. First, we conducted a cross-sectional investigation; therefore, we cannot define causal relationship between occupational stress, burnout and anxiety symptoms. These findings should be confirmed with longitudinal studies. Second, all data were based on self-reported questionnaires; therefore, bias introduced by the common method variance cannot be avoided. Moreover, healthcare workers belong to a special group, and we cannot extended the results to other populations without clear evidence.
Conclusions
There was a high prevalence of anxiety symptoms in community healthcare workers in China. After adjusting for demographic characteristics, the extrinsic stress (ERR), intrinsic stress (overcommitment), emotional exhaustion and cynicism subscales were positively associated with anxiety symptoms. However, professional efficacy was negatively associated with anxiety symptoms. Additionally, burnout mediated the relationship between occupational stress and anxiety symptoms. The combination of decreasing occupational stress with reducing burnout may be more useful in preventing anxiety symptoms in Chinese Community Health Center healthcare workers.
Acknowledgments
The authors thank all administrators in the studied CHCs who helped us to acquire written informed consent from the participants and to distribute the questionnaires to our subjects. We also thank all healthcare workers who participated in our study.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. Data may be obtained from Figshare using the DOI http://dx.doi.org/10.6084/m9.figshare.1136113.
Funding Statement
The authors have no support or funding to report.
References
- 1. Chen Z (2009) Launch of the health-care reform plan in China. Lancet 373: 1322–1324. [DOI] [PubMed] [Google Scholar]
- 2. Jiang HL, Chen W, Bi KN, Ying XH (2009) Are services delivered by community health centers more cost-effectve? Evidence from urban China. Health Econ 18: 107–117. [DOI] [PubMed] [Google Scholar]
- 3. Fiabane E, Giorgi I, Sguazzin C, Argentero P (2013) Work engagement and occupational stress in nurses and other healthcare workers: the role of organizational and personal factors. J Clin Nurs 22: 2614–2624. [DOI] [PubMed] [Google Scholar]
- 4. Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, et al. (2011) Lay health worker led intervention for depressive and anxiety disorders in India: impact on clinical and disability outcomes over 12 months. BJP 199: 459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahmed I, Banu H, AL-Fageer R, AL-Suwaidi R (2009) Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care 24: 1–7. [DOI] [PubMed] [Google Scholar]
- 6. Begat I, Ellefsen B, Severinsson E (2005) Nurses' satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses' experience of well-being – a Norwegian study. J Nurs Manag 13: 221–230. [DOI] [PubMed] [Google Scholar]
- 7. Sun W, Fu JL, Chang Y, Wang L (2012) Epidemiological study on risk factors for anxiety disorder among Chinese doctors. J Occup Health 54: 1–8. [DOI] [PubMed] [Google Scholar]
- 8. Bargellini A, Barbieri A, Rovesti S, Vivoli R, Roncaglia R, et al. (2000) Relation between immune variables and burnout in a sample of physicians. Occup Environ Med 57: 453–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ruitenburg MM, Frings-Dresen MH, Sluiter JK (2012) The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res 12: 292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dudek D, Jaeschke R, Styczeń K, Pilecki M (2013) Depression and anxiety in the practice of cardiology. Kardiol Pol 71: 781–786. [DOI] [PubMed] [Google Scholar]
- 11. DiGiacomo M, Adamson B (2001) Coping with stress in the workplace: implications for new health professionals. J Allied Health 30: 106–111. [PubMed] [Google Scholar]
- 12. Mark G, Smith AP (2012) Occupational stress, job characteristics, coping, and the mental health of nurses. Br J Health Psychol 17: 505–521. [DOI] [PubMed] [Google Scholar]
- 13. Peplińska A, Jeżewska M, Leszczyńska I, Połomski P (2013) Stress and the level of perceived anxiety among mariners: the mediating role of marital satisfaction. Int Marit Health 64: 221–225. [DOI] [PubMed] [Google Scholar]
- 14. Shirazi A, Rasekhnia M, Ajdary H (2011) An empirical examination of the relationship between occupational stress and mental health. IJCRB 3: 101–109. [Google Scholar]
- 15. Nakao M (2010) Work-related stress and psychosomatic medicine. Biopsyosoc Med 4: 4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tsai YC, Liu CH (2012) Factors and symptoms associated with work stress and health- promoting lifestyles among hospital staff: a pilot study in Taiwan. BMC Health Serv Res 12: 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nordang K, Hall-Lord ML, Farup PG (2010) Burnout in health-care professionals during reorganizations and downsizing. A cohort study in nurses. BMC Nurs 9: 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peterson U, Demerouti E, Bergström G, Samuelsson M, Asberg M, et al. (2008) Burnout and physical and mental health among Swedish healthcare workers. J Adv Nurs 62: 84–95. [DOI] [PubMed] [Google Scholar]
- 19. Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52: 397–422. [DOI] [PubMed] [Google Scholar]
- 20. Turnipseed DL (1998) Anxiety and burnout in the health care work environment. Psychol Rep 82: 627–642. [DOI] [PubMed] [Google Scholar]
- 21. Maslach C, Leiter MP (2008) Early predictors of job burnout and engagement. J Appl Psychol 93: 498–512. [DOI] [PubMed] [Google Scholar]
- 22. Piko BF (2006) Burnout, role conflict, job satisfaction and psychosocial health among Hungarian health care staff: a questionnaire survey. Int J Nurs Stud 43: 311–318. [DOI] [PubMed] [Google Scholar]
- 23. Pavlakis A, Raftopoulos V, Theodorou M (2010) Burnout syndrome in Cypriot physiotherapists: a national survey. BMC Health Serv Res 10: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dai JM, Collins S, Yu HZ, Fu H (2008) Combining job stress models in predicting burnout by hierarchical multiple regressions: a cross-sectional investigation in Shanghai. J Occu Environ Med 50: 785–790. [DOI] [PubMed] [Google Scholar]
- 25. Lin QH, Jiang CQ, Lam TH (2013) The relationship between occupational stress, burnout, and turnover intention among managerial staff from a Sino-Japanese joint venture in Guangzhou, Chian. J Occup Health 55: 458–467. [DOI] [PubMed] [Google Scholar]
- 26. Xie Z, Wang A, Chen B (2011) Nurse burnout and its association with occupational stress in a cross-sectional study in Shanghai. J Adv Nurs 67: 1537–1546. [DOI] [PubMed] [Google Scholar]
- 27. Gilbert S, Laschinger HK, Lerter M (2010) The mediating effect of burnout on the relationship between structural empowerment and organizational citizenship behaviours. J Nurs Manag 18: 339–348. [DOI] [PubMed] [Google Scholar]
- 28. Zung WW (1971) A rating instrument for anxiety disorders. Psychosomatics 12: 371–379. [DOI] [PubMed] [Google Scholar]
- 29.Wang ZY (1984) Chinese version of Zung's self-rating anxiety scale. J Shanghai Psychiatry 2: 73–74. [Article in Chinese].
- 30. Liu XC, Oda S, Peng X, Asai K (1997) Life events and anxiety in Chinese medical students. Soc Psychiatry Psychiatr Epidemiol 32: 63–67. [DOI] [PubMed] [Google Scholar]
- 31. Wang XQ, Lambert CE, Lambert AV (2007) Anxiety, depression and coping strategies in post-hysterectomy Chinese women prior to discharge. Tnt Nurs Rev 54: 271–279. [DOI] [PubMed] [Google Scholar]
- 32. Siegrist J (1996) Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol 1: 27–41. [DOI] [PubMed] [Google Scholar]
- 33. Maina G, Bovenzi M, Palmas A, Larese Filon F (2009) Associations between two job stress models and measures of salivary cortisol. Int Arch Occup Environ Health 82: 1141–1150. [DOI] [PubMed] [Google Scholar]
- 34. Tsutsumi A, Kawanami S, Horie S (2012) Effort-reward imbalance and depression among private practice physicians. Int Arch Occup Environ Health 85: 153–161. [DOI] [PubMed] [Google Scholar]
- 35. Li J, Yang W, Cheng Y, Siegrist J, Cho SI (2005) Effort-reward inbalance at work and jof dissatisfaction in Chinese healthcare workers: a validation study. Int Arch Occup Enviren Health 78: 198–204. [DOI] [PubMed] [Google Scholar]
- 36. Siegrist J, Starke D, Chandola T, Godin I, Marmot M, et al. (2004) The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med 58: 1483–1499. [DOI] [PubMed] [Google Scholar]
- 37. Chor D, Werneck GL, Faerstein E, Alves MG, Rotenberg L (2008) The Brazilian version of the effort-reward imbalance questionnaire to assess job stress. Cad Saude Publica 24: 219–224. [DOI] [PubMed] [Google Scholar]
- 38. Maslach C, Jackson SE (1981) The measurement of experiences burnout. J Occup Behav 2: 99–103. [Google Scholar]
- 39. Wang Y, Liu L, Wang J, Wang L (2012) Work-family conflict and burnout among Chinese doctors: the mediating role of psychological capital. J Occup Health 54: 232–240. [DOI] [PubMed] [Google Scholar]
- 40. Wu S, Li H, Zhu W, Lin S, Chai W, et al. (2012) Effect of work stressors, personal strain, and coping resources on burnout in Chinese medical professionals: a structural equation model. Ind Health 50: 279–287. [DOI] [PubMed] [Google Scholar]
- 41. Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51: 1173–1182. [DOI] [PubMed] [Google Scholar]
- 42. MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V (2002) A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 7: 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McEvoy PM, Grove R, Slade T (2011) Epidemiology of anxiety disorders in the Auatralian general population: fingdings of the 2007 Australian national survey of mental health and wellbeing. Aust N Z J Psychiatry 45: 957–967. [DOI] [PubMed] [Google Scholar]
- 44. Schwarz R, Gunzelmann T, Hinz A (2001) Anxiety and depression in the normal population aged above 60 years. Deut Med Wochenschr 126: 611–615. [DOI] [PubMed] [Google Scholar]
- 45. Haynes C (2000) Stress in health professionals. Psychologist 13: 128–129. [Google Scholar]
- 46. Fiabane E, Giorgi I, Sguazzin C, Argentero P (2013) Work engagement and occupational stress in nurses and other healthcare workers: the role of organizational and peisonal factors. J Clin Nurs 22: 2614–2624. [DOI] [PubMed] [Google Scholar]
- 47. Boudrias JS, Morin AJ, Brodeur MM (2012) Role of psychological empowerment in the reduction of burnout in Canadian healthcare workers. Nurs Health Sci 14: 8–17. [DOI] [PubMed] [Google Scholar]
- 48. Wu SY, Li HY, Tian J, Zhu W, Li J, et al. (2011) Health-related quality of life and its main related factors among nurses in China. Ind Health 49: 158–165. [DOI] [PubMed] [Google Scholar]
- 49. Dib HH, Sun P, Minmin Z, Wei S, Li L (2010) Evaluating community health centers in the city of Dalian, China: how satisfied are patents with the medical services provided and their health professionals? Health Place 16: 477–488. [DOI] [PubMed] [Google Scholar]
- 50. Zhang X, Smith DR, Zheng Y, Wang RS (2011) Occupational stress and psychosomatic complaints among health professionals in Beijing, China. Work 40: 239–245. [DOI] [PubMed] [Google Scholar]
- 51. Gao YQ, Pan BC, Sun W, Wu H, Wang L, et al. (2012) Anxiety symptoms among Chinese nurses and the associated factors: a cross sectional study. BMC Psychiatry 12: 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gómez-Gascón T, Martín-Fernández J, Gálvez-Herrer M, Tapias-Merino E, Beamud-Lagos M, et al. (2013) Effectiveness of an intervention for prevention and treatment of burnout in primary health care professionals. BMC Fam Pract 14: 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. Data may be obtained from Figshare using the DOI http://dx.doi.org/10.6084/m9.figshare.1136113.