Abstract
Background:
Hospitalists have become dominant providers of inpatient care in many North American hospitals. Despite the global growth of hospital medicine, no objective method has been proposed for defining the hospitalist discipline and delineating among inpatient practices on the basis of physicians' clinical volumes. We propose a functional method of identifying hospital-based physicians using aggregated measures of inpatient volume and apply this method to a retrospective, population-based cohort to describe the growth of the hospitalist movement, as well as the prevalence and practice characteristics of hospital-based generalists in one Canadian province.
Methods:
We used human resource databases and financial insurance claims to identify all active fee-for-service physicians working in Ontario, Canada, between fiscal year 1996/1997 and fiscal year 2010/2011. We constructed 3 measures of inpatient volume from the insurance claims to reflect the time that physicians spent delivering inpatient care in each fiscal year. We then examined how inpatient volumes have changed for Ontario physicians over time and described the prevalence of full-time and part-time hospital-based generalists working in acute care hospitals in fiscal year 2010/2011.
Results:
Our analyses showed a significant increase since fiscal year 2000/2001 in the number of high-volume hospital-based family physicians practising in Ontario (p < 0.001) and associated decreases in the numbers of high-volume internists and specialists (p = 0.03), where high volume was defined as ≥ 2000 inpatient services/ year. We estimated that 620 full-time and 520 part-time hospital-based physicians were working in Ontario hospitals in 2010/2011, accounting for 4.5% of the active physician workforce (n = 25 434). Hospital-based generalists, consisting of 207 family physicians and 130 general internists, were prevalent in all geographic regions and hospital types and collectively delivered 10% of all inpatient evaluation and care coordination for Ontario residents who had been admitted to hospital.
Interpretation:
These analyses confirmed a substantial increase in the prevalence of general hospitalists in Ontario from 1996 to 2011. Systems-level analyses of clinical practice data represent a practical and valid method for defining and identifying hospital-based physicians.
Since the first hospitalist programs were established in the late 1990s, the hospitalist movement has grown rapidly in terms of the number of physicians specializing in hospital medicine, the proportion of inpatients cared for by hospital-based physicians, and the number of hospitals employing formal hospitalist groups.1–5 Although several studies have reported on the demographic characteristics, prevalence, and outcomes of care of US hospitalists,1,3,4,6,7 fundamental debate continues within the medical community as to what hospitalists are, how they should be defined, and what (if anything) distinguishes them from other hospital- based specialists.
The Society of Hospital Medicine has defined a hospitalist as "a physician who specializes in the practice of hospital medicine," which is in turn defined as "a medical specialty dedicated to the delivery of comprehensive medical care to hospitalized patients."8 While these definitions identify the hospitalist's professional focus, they offer little guidance on what characteristics differentiate the clinical hospitalist from other practitioners. As a consequence, the term "hospitalist" has become colloquialized and is now commonly used to refer to a general internist or family doctor who works in a hospital. However, there are exceptions to this general rule, and some hospitalists are now specializing, with new terms like "neurohospitalist," "surgical hospitalist," and "OB-GYN hospitalist" becoming increasingly commonplace.9
Two approaches have traditionally been applied when identifying hospitalists in comparative evaluations. The first uses voluntary surveys of institutional staff or professional society membership to estimate hospitalist prevalence. With this approach, the responding physician self-identifies as a hospitalist, but this method is impractical and imprecise for researchers and policymakers. Lacking a formal definition of the clinical hospitalist practice, any physician can choose to call himself or herself a hospitalist. Low response rates for such surveys have made it difficult to assess the population prevalence of hospital-based physicians, and the clinical workloads of practitioners are seldom explored. Furthermore, few countries offer certification or training in hospital medicine. Consequently, administrative databases rarely include physician-specialty codes that categorize physicians as hospitalists.
The second approach uses a functional definition, categorizing hospitalists by the amount of inpatient care provided. Most often a threshold is established whereby hospitalists are identified and classified on the basis of a certain proportion of each physician's practice being generated from the care of hospital inpatients (e.g., ≥ 90%). These definitions are more restrictive, limiting the category of hospitalists to direct providers of care. The associated methods are also problematic. Few authors have discussed the validity of proportional metrics, assessing whether the denominators used in their analyses have captured minimum volumes indicative of active practice (e.g., a physician with 90% inpatient practice may be classified as a hospitalist, even if he or she saw only 5 patients in the timeframe under investigation). Similarly, few, if any, authors have acknowledged the variability that exists between practice styles, adopting thresholds that can accommodate both full-time and part-time practitioners. As a result, high-volume parttime hospitalists who fall below the proportional thresholds are categorized in the comparison group alongside low-volume community providers, which mutes the effects of a hospitalist model of concentrated care.
Hospital medicine sits at a pivotal intersection for the way inpatient care is funded and delivered across the globe. With several North American, European, Asian, and Australasian governing bodies introducing activity-based funding models that reward hospitals for improved productivity and/or penalize those with lower than expected outcomes, hospital physicians and their institutions must become accountable for the quality of care and services they deliver. If the eventual goal in hospital medicine is to monitor and improve performance, a standardized, systems-level method is needed for defining the clinical hospitalist, independent of self-identification.
Canadian hospitalists emerged alongside their US counterparts after cutbacks to physician reimbursement in the mid-1990s sparked an exodus of primary care practitioners from the hospital setting.2,10–12 Canada is unique within the hospitalist movement in that the majority of this country's hospitalists are trained as general practitioners or family physicians (GP/FPs) as opposed to specialists.2,3,13 The hospitalist career path is attractive to GP/FPs, as it provides an opportunity to practice higher-acuity medicine while earning a competitive compensation exceeding that of an officebased practice. However, hospital medicine is not recognized as a distinct area of focused practice. There are no certification or training guidelines for Canadian hospitalists, and no method (other than self-identification) exists of distinguishing hospital-based from office-based practitioners.12 As a result, the population prevalence of hospitalists is largely unknown and almost certainly under-reported, which makes hospital medicine an ideal setting to pilot the application of a functional volume framework.
In this article, we propose a novel method of defining hospital-based physicians that uses the volume of inpatient care combined with additional practice data to measure a physician's involvement in the provision of hospital care. We then apply this method at the systems level to describe the growth of the hospitalist movement, as well as the prevalence and characteristics of hospital-based physicians, in Ontario, Canada, over a 15-year timeframe.
Methods
Study population.
We constructed a retrospective population-based sample consisting of all clinically active physicians who practised in the province of Ontario, Canada, between 1 April 1996 and 31 March 2011 (fiscal 1996/1997 to fiscal 2010/2011) and who submitted claims for professional fees to the Ontario Health Insurance Plan (OHIP), a publicly funded plan that covers the cost of basic health care, including hospital care, to all permanent residents of the province. The cohort was identified using the Institute for Clinical Evaluative Sciences (ICES) Physician Database, a human resources database containing validated demographic, certification, and practice characteristics for all physicians licensed in the province since 1992. Active physicians were defined yearly according to guidelines developed by the Ontario Physician Human Resources Data Centre, which include maintaining an active licence with the College of Physicians and Surgeons of Ontario; being 25 to 85 years of age with a practice located within the province; having an OHIP billing number with active insurance claims; not being engaged in postgraduate studies; and not being identified as retired or inactive because of disability, leave, sabbatical, or other reason.14 Physicians were allowed to enter and leave the cohort throughout the 15-year observation window; however, once a physician was deemed active in a given fiscal year, it was assumed that he or she remained active throughout the fiscal period.
Outcome measures.
For each year, we extracted physicians' demographic, training, and practice characteristics from the ICES Physician Database. Each physician's medical specialty was determined by combining data on both certified and functional specialties, where certified specialty captured the most recent certification information on file and functional specialty reflected the services that the physician actually billed for in his or her practice, derived from aggregated OHIP billings and validated through periodic telephone follow-up with random physician samples. In cases of discrepancy, the physician was assigned to the medical specialty recorded most often in his or her OHIP claims for the particular year, on the assumption that a physician would not be allowed to bill under a specialty code unless licensed to do so. Pediatric surgeons and psychiatrists were combined with the corresponding adult practitioners, and diagnostic radiology, nuclear medicine, and all laboratory specialties were considered together (as "diagnostics").
Physicians' demographic characteristics were linked to OHIP billings through an encrypted identifier to determine the annual number of patient evaluation-andmanagement (E&M) claims billed in relation to the location of care delivery (inpatient setting, emergency department, office, long-term care facility, or the patient's home). An E&M claim was defined as any clinical visit, consultation, assessment, reassessment, death pronouncement, case conference, counselling session (patient, family, or group), or psychotherapy session billed to OHIP for an Ontario resident. Claims were used as a proxy indicator of the time that physicians spent in direct clinical care and case management. From the data, 3 measures of physicians' annual inpatient workloads were tabulated: (1) the total number of E&M claims billed for inpatient care, (2) the proportion of total claims generated from the care of hospital inpatients (inpatient claims/total claims), and (3) the total number of calendar days with OHIP billings for inpatient care. Because the primary role of the hospitalist is to provide direct clinical care and care coordination, procedure volumes were not explored.
The number of unique inpatients seen by each physician and the proportion of inpatients with whom physicians had a previous medical relationship (defined as patients for whom the physician had billed at least one E&M claim within 24 months before the date of admission) were determined for the most recent fiscal year (2010/2011). Characteristics of the hospitals where physicians billed the majority of inpatient care were extracted from the Ontario Hospital Reporting System, a database maintained by the Canadian Institute for Health Information that contains annual statistical information on all acute care hospitals operating in the province.
Definition of hospital-based physicians.
In Table 1 we propose a conceptual framework that uses annual
Table 1.
Conceptual framework for defining community and hospital-based physicians using information from administrative databases
| Aspect of framework | Comprehensive community practitioner | Mixed-practice physician | Part-time hospital-based physician | Full-time hospital-based physician |
|---|---|---|---|---|
| Description of practice | Physicians practise primarily within the community but provide occasional inpatient care. Physicians also provide long-term care, emergency, and/or home care services as appropriate. | Full-time practice is split between outpatient and inpatient care. | Majority of practice is inpatient evaluation and management, but physician works at a part-time equivalency. Inpatient practice may be general or specialty-based. | Majority of practice is inpatient evaluation and management on a full-time basis. Inpatient practice may be general or specialty-based. |
| Scope of inpatient practice | Hospital inpatients are enrolled in the physician's primary practice either individually or within a team; inpatients are generally lowrisk medical and ALC patients. | Hospital inpatients often come from outside the physician's primary practice through rotating call; inpatients may be general, complex medical, and ALC patients. | Physicians typically have no previous relationship with hospital inpatients; inpatients are general, complex medical, and ALC patients; physicians are often involved in comanagement of specialty patients. | |
| Compensation mechanism | Fee-for-service billing to insurance plans; physicians have no direct financial relationship with hospitals. | Fee-for-service billing to insurance plans. Hospitals may "top up" physicians' feefor- service billings. | Fee-for-service billings plus negotiated salary stipend or alternative funding plans; hospitals may pay a portion or all of the physicians' income from their operating budgets. Physicians often work as independent contractors to individual hospitals. | |
| Annual inpatient volume* | < 30% of clinical volume is hospital-based, and total annual volume indicates an active community practice (> 50% of total volume is generated from office, nursing home, or home care; total volume ≥ 100 services; inpatient volume ≥ 10 services). | 30%–79% of total volume is hospital-based, and inpatient volumes reflect an active and substantial inpatient practice (≥ 500 inpatient services annually). | ≥ 80% of total volume is hospital-based, but volumes reflect a part-time case load (500–1999 inpatient services annually). | ≥ 80% of total volume is hospital-based and volumes reflect a full-time case load (≥ 2000 inpatient services annually). |
ALC = alternate level of care (patients waiting in hospital to be transferred to a complex continuing care or long-term care setting).
Inpatient volume can be left as a continuous measure of a physician's hospital experience in regression models, eliminating the need for categorization.
inpatient volumes and additional practice data to define and delineate hospital-based physicians. We began with a functional definition validated by Kuo et al.,1 identifying all active physicians in each fiscal year who had a minimum total volume of 100 E&M claims and for whom at least 80% of total claims were generated from the care of hospital inpatients. We then plotted the frequency distribution of active physicians by year and medical specialty according to the following 4 variables: (1) total number of inpatient claims billed, (2) proportion of total claims generated from the care of hospital inpatients, (3) the relationship between total claims volume and the proportion of claims billed for inpatient care, and (4) the relationship between inpatient claims volume and the proportion of claims billed for inpatient care. In examining variables 3 and 4, two concerns became apparent with the functional definition proposed by Kuo et al.1: first, total claims volume was not a specific metric, which meant that too many low-volume physicians were categorized as hospitalists (false positives); and second, the definition did not discriminate
between full-time and part-time practitioners. Parttime practitioners with moderately high inpatient volumes practising exclusively in the hospital would be correctly classified as hospitalists, whereas physicians with equivalent inpatient volumes but whose practices were split between hospital and community (e.g., 70% inpatient, 30% long-term care) would incorrectly fall in the comparison group. We therefore updated the definition of Kuo et al.,1 replacing total claims volume with inpatient claims volume and distinguishing full-time from part-time but strictly hospital-based physicians on the basis of their volume of inpatient care provision. We then proposed 2 novel classifications: mixed-practice physicians (physicians with average-to-high inpatient volumes whose clinical practice is split between inpatient and outpatient care) and comprehensive community practitioners (community-based physicians who provide a full range of medical services including hospital care) (see online Appendix A for an evaluation of concordance between the 2 frameworks). The proposed thresholds were established by examining the distributions of the 4 variables listed above, looking for points at which consistent changes in physician density formed over time, indicated by an increasing frequency of high-volume practitioners and a consistent density of mid-volume practitioners (see online Appendix B and online Appendix C for selected distributions).
Statistical analysis.
After describing the characteristics of physicians who provided inpatient care in Ontario hospitals by year, we plotted the distribution of active physicians according to the annual number of inpatient claims billed by year and medical specialty. To confirm whether upward or downward trends in inpatient volumes were significant over time, the proportions of physicians achieving each billing level (i.e., ≥ 2000 inpatient claims) in fiscal year t were entered into separate autoregressive models by specialty, with a lag set to 1. This model can be presented as logit(ρt ) = α + β1 ρt–1 + et , where ρt is the proportion of physicians in a given specialty achieving each billing threshold in fiscal year t, β1 confirms the significance of volume changes over time, ρt–1 is the proportion of physicians achieving the billing threshold in the previous year, and et is the error term. Autoregressive models were needed to adjust for the autocorrelation of residuals because the physicians' inpatient volume in a given year was found to be dependent on inpatient volume in the previous year. We then used the inpatient volumes billed in 2010/2011 to describe the current population of hospital-based physicians according to the functional categories proposed in Table 1, excluding practitioners with low total billings (< 100 total claims) and low inpatient billings (< 10 inpatient claims). SAS software, version 9.2 (SAS Institute Inc., Cary, N.C.), was used for analyses. Ethics approval was obtained from Sunnybrook Health Sciences Centre and from the Health Sciences Research Ethics Board at the University of Toronto.
Results
Descriptive characteristics of physicians providing inpatient care in Ontario hospitals are shown in Table 2 for selected fiscal years. In 1996/1997, three-quarters of active physicians working in the province provided inpatient evaluation-and-management services (n = 15 275 of 19 922; 76.7%), and almost half of all inpatient physicians were trained in family medicine (n = 7418; 48.6%). Beginning in 1998, the proportion of active physicians providing inpatient services began to decline, and this trend has continued each fiscal year since. Although many specialties experienced an exodus of practitioners from provision of hospital care, the largest declines have occurred among GP/FPs (Table 2, Figure 1). In 1996/1997, nearly three-quarters of active GP/FPs provided some level of inpatient care to hospital inpatients, but by 2010, fewer than half continued to do so (71.0% v. 47.2%).
Table 2.
Characteristics of active physicians providing inpatient care in Ontario hospitals for selected fiscal years
| Characteristic | Fiscal year; no. (%)* | ||||
|---|---|---|---|---|---|
| 1996/1997 | 2000/2001 | 2004/2005 | 2008/2009 | 2010/2011 | |
| Total no. of active physicians | 19 922 | 20 368 | 21 814 | 23 872 | 25 434 |
| No. providing inpatient care (% of active physicians) | 15 275 (76.7) | 14 914 (73.2) | 15 020 (68.9) | 15 949 (66.8) | 16 820 (66.1) |
| Age, yr, mean (SD) | 46.5 (11.2) | 47.4 (10.9) | 47.9 (10.8) | 48.5 (11.0) | 48.6 (11.2) |
| Time in practice, yr, mean (SD) | 20.6 (11.4) | 21.4 (11.2) | 21.8 (11.2) | 22.2 (11.5) | 22.3 (11.8) |
| Sex | |||||
| Male | 11 660 (76.3) | 11 056 (74.1) | 10 742 (71.5) | 10 981 (68.9) | 11 357 (67.5) |
| Female | 3 615 (23.7) | 3 858 (25.9) | 4 278 (28.5) | 4 968 (31.1) | 5 463 (32.5) |
| Canadian medical graduate | |||||
| Yes | 9 791 (64.1) | 10 542 (70.7) | 11 205 (74.6) | 12 192 (76.4) | 12 763 (75.9) |
| No | 5 430 (35.5) | 4 324 (29.0) | 3 771 (25.1) | 3 719 (23.3) | 4 007 (23.8) |
| Unknown | 54 (0.4) | 48 (0.3) | 44 (0.3) | 38 (0.2) | 50 (0.3) |
| Census metropolitan area of practice, by population | |||||
| ≥ 1 250 000 | 6 426 (42.1) | 6 166 (41.3) | 6 360 (42.3) | 6 671 (41.8) | 7 030 (41.8) |
| 500 000 to 1 249 999 | 2 594 (17.0) | 2 535 (17.0) | 2 565 (17.1) | 2 757 (17.3) | 2 939 (17.5) |
| 100 000 to 499 999 | 3 782 (24.8) | 3 688 (24.7) | 3 497 (23.3) | 4 011 (25.1) | 4 232 (25.2) |
| 9000 to 99 999 | 1 465 (9.6) | 1 480 (9.9) | 1 494 (9.9) | 1 468 (9.2) | 1 558 (9.3) |
| < 9000 | 1 002 (6.6) | 1 034 (6.9) | 1 104 (7.4) | 1 042 (6.5) | 1 050 (6.2) |
| Unknown | 6 (< 0.1) | 11 (< 0.1) | 0 (0.0) | 0 (0.0) | 11 (< 0.1) |
| Medical specialty | |||||
| Anesthesiology | 722 (4.7) | 761 (5.1) | 871 (5.8) | 1 048 (6.6) | 1 130 (6.7) |
| Diagnostics† | 502 (3.3) | 508 (3.4) | 579 (3.9) | 628 (3.9) | 728 (4.3) |
| General internal medicine | 897 (5.9) | 829 (5.6) | 885 (5.9) | 771 (4.8) | 795 (4.7) |
| General practice/family medicine | 7 418 (48.6) | 6 751 (45.3) | 6 174 (41.1) | 5 894 (37.0) | 5 970 (35.5) |
| Internal medicine specialties‡ | 1 791 (11.7) | 1 950 (13.1) | 2 171 (14.5) | 2 715 (17.0) | 2 975 (17.7) |
| Obstetrics and gynecology | 558 (3.7) | 563 (3.8) | 581 (3.9) | 641 (4.0) | 668 (4.0) |
| Pediatrics§ | 626 (4.1) | 673 (4.5) | 728 (4.8) | 850 (5.3) | 936 (5.6) |
| Psychiatry | 1 212 (7.9) | 1 315 (8.8) | 1 417 (9.4) | 1 540 (9.7) | 1 644 (9.8) |
| Surgery¶ | 1 549 (10.1) | 1 564 (10.5) | 1 614 (10.7) | 1 862 (11.7) | 1 974 (11.7) |
Except where indicated otherwise.
Includes diagnostic radiology, nuclear medicine, and all laboratory specialties.
Includes cardiology, clinical immunology, community and geriatric medicine, dermatology, endocrinology, gastroenterology, hematology, infectious diseases, medical genetics, medical oncology, nephrology, neurology, physical medicine and rehabilitation, radiation oncology, respirology, and rheumatology.
Includes general pediatrics and all pediatric internal medicine specialties.
Includes all adult and pediatric surgeons licensed to practice by the Royal College of Physicians and Surgeons of Canada.
Figure 1.
Distribution of active Ontario physicians, according to annual number of inpatient evaluation-andmanagement claims billed to the Ontario Health Insurance Plan (OHIP), fiscal year 1996/1997 to fiscal year 2010/2011.
(A) General practitioners and family physicians, (B) general internists, and (C) internal medicine specialists. Significant increases (*) and significant decreases (†) in the proportion of physicians achieving each billing level over time, based on autoregressive models with a lag set to 1 (p < 0.05), are marked.
Figure 1 shows the distribution of GP/FPs, general internists, and internal medicine specialists according to the annual volume of inpatient claims billed over time. Since 1997/1998, the proportion of GP/FPs providing low-to-no hospital care (< 250 inpatient claims/ year) increased from 70.7% to 83.5% (p < 0.001; Figure 1A). In turn, high-volume GP/FPs (≥ 2000 inpatient claims/year) filled the resulting gap in inpatient care provision, increasing in prevalence from 0.9% of active GP/FPs in 1996/1997 to 2.5% in 2010/2011, with growth beginning in 2000 (p < 0.001). Conversely, the percentages of high-volume general internists and specialists have decreased over time (p = 0 .03; Figures 1 B, 1 C), which may be indicative of lighter inpatient workloads or more balanced distributions between inpatient and outpatient practices.
Despite large declines in the number of GP/FPs providing hospital care over time, the total volume of inpatient services delivered by these practitioners across the province has dropped only minimally, accounting for 32.1% of total provincial inpatient E&M claims in 1996/1997, just under 30% in the period from 2000/2001 to 2004/2005, and 28.4% in 2008/2009 (see online Appendix D). To maintain this consistent level of care, fewer GP/FPs have provided higher volumes of inpatient care in each fiscal year (see online Appendix E). Although the average volume of services has increased for those GP/FPs who have maintained hospital privileges, median volumes have decreased, which suggests that rising inpatient caseloads pertain only to practitioners to the right of the median (i.e., the high-volume GP/FP hospitalists).
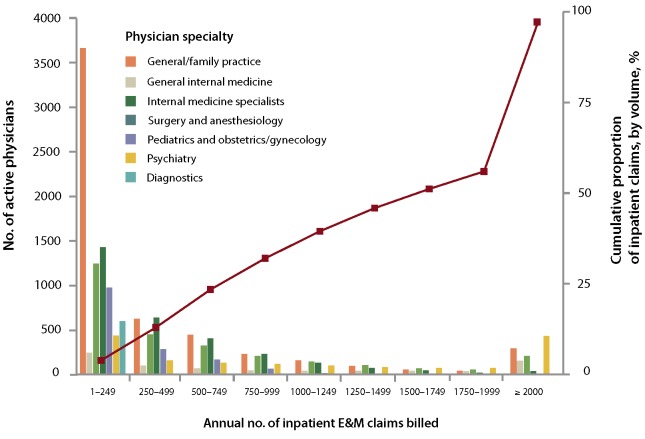
Figure 2 shows the current distribution of inpatient care physicians by medical specialty and annual volume. Overlaid is the cumulative distribution of total inpatient E&M claims billed in Ontario to depict the relationship between workforce density and service volume. In 2010/2011, a total of 1143 high-volume physicians (≥ 2000 claims; 6.8% of inpatient physician workforce) delivered 42% of all inpatient E&M services in the province of Ontario. Conversely, 8600 lowvolume physicians (< 250 claims; 51.1% of inpatient physician workforce) billed just 6% of provincial claims.
Figure 2.
Relationship between workforce density and service volume, represented as current distribution of inpatient physician workforce by medical specialty and annual inpatient volume, overlaid with the cumulative distribution of total inpatient evaluation-and-management (E&M) claims billed in Ontario, for fiscal year 2010/2011.
Applying the clinical volume algorithms from Table 1, we estimated that 620 full-time and 520 part-time hospital-based physicians were working in Ontario in fiscal year 2010/2011, of whom 548 (48.1%) were psychiatrists, 207 (18.2%) were GP/FPs, and 130 (11.4%) were general internists. The remaining physicians were internal medicine specialists (n = 105; 9.2%), anesthesiologists ( n = 8 3; 7 .3%), pediatricians ( n = 43; 3.8%), and surgeons (n = 24; 2.1%). The majority of the 2164 mixed-practice physicians were internal medicine specialists (n = 645; 29.8%), psychiatrists (n = 426; 19.7%), and surgeons (n = 303; 14.0%), while comprehensive community practitioners were primarily GP/FPs (n = 2320 of 4479; 51.8%). Table 3 presents the demographic and practice characteristics of the hospital-based GP/FPs and general internists, herein referred to as "general hospitalists," with data for mixedpractice and comprehensive community practitioners provided for comparison (data for additional specialties are available by request to the authors). Full-time general hospitalists delivered 10% of total inpatient E&M services in 2010/2011, billing an average of 3649 inpatient claims and accounting for 614 unique hospital inpatients and 220 days worked in hospital. Using mean volumes, these metrics equate to an average clinical workload of 16.6 patient interactions and 2.8 new patients evaluated per workday, excluding nonbillable reassessments and any additional outpatient services. Part-time general hospitalists evaluated an average of 11.0 inpatients and 2.6 new patients per hospital day worked, while mixed-practice physicians evaluated 11.6 inpatients and 2.3 new patients per day. All full-time general hospitalists worked a minimum of 100 calendar days in hospital, and all part-time practitioners (part-time hospitalists and mixed-practice physicians) exceeded 50 days. As expected, general hospitalists had limited previous medical relationships with their hospital inpatients, seeing an average of 10.8% of these patients within the 2 years before admission. On average, the comprehensive community generalists had seen more than half of their patients before admission to hospital (51.5%).
Table 3.
Characteristics of comprehensive community, mixed-practice and hospital-based generalists, fiscal year 2010/2011
| Physician group; no. (%) of physicians* | ||||
|---|---|---|---|---|
| Characteristic | Comprehensive community practitioners | Mixed-practice physicians | Part-time hospitalists | Full-time hospitalists |
| Total no. of physicians | 2478 | 512 | 126 | 211 |
| Age, yr, mean (SD) | 50.6 (11.2) | 46.0 (11.1) | 41.7 (9.2) | 45.7 (10.2) |
| Time in practice, yr, mean (SD) | 23.9 (11.8) | 19.4 (11.8) | 15.0 (9.7) | 18.5 (10.8) |
| Sex | ||||
| Male | 1670 (67.4) | 325 (63.5) | 76 (60.3) | 117 (55.5) |
| Female | 808 (32.6) | 187 (36.5) | 50 (39.7) | 94 (44.5) |
| Canadian medical graduate | ||||
| Yes | 2049 (82.7) | 363 (70.9) | 107 (84.9) | 147 (69.7) |
| No | 429 (17.3) | 149 (29.1) | 19 (15.1) | 64 (30.3) |
| Medical specialty | ||||
| General practice/family medicine | 2320 (93.6) | 280 (54.7) | 62 (49.2) | 145 (68.7) |
| General internal medicine | 158 (6.4) | 232 (45.3) | 64 (50.8) | 66 (31.3) |
| Census metropolitan area of practice, by population | ||||
| ≥ 1 250 000 | 639 (25.8) | 208 (40.6) | 42 (33.3) | 87 (41.2) |
| 500 000 to 1 249 999 | 240 (9.7) | 80 (15.6) | 33 (26.2) | 26 (12.3) |
| 100 000 to 499 999 | 529 (21.3) | 147 (28.7) | 39 (31.0) | 80 (37.9) |
| 9 000 to 99 999 | 471 (19.0) | 60 (11.7) | 11 (8.7) | 18 (8.5) |
| < 9 000 | 599 (24.2) | 17 (3.3) | < 5 (0.8)† | 0 (0.0) |
| Hospital size, no. of acute care beds | ||||
| ≥ 300 | 223 (9.0) | 121 (23.6) | 54 (42.9) | 58 (27.5) |
| 200–299 | 384 (15.5) | 123 (24.0) | 29 (23.0) | 63 (29.9) |
| 100–199 | 582 (23.5) | 170 (33.2) | 32 (25.4) | 61 (28.9) |
| 1–99 | 1287 (51.9) | 93 (18.2) | 11 (8.7) | 29 (13.7) |
| Unknown | < 5 (<0.1)† | 5 (1.0) | 0 (0.0) | 0 (0.0) |
| Hospital location, residents/km2 | ||||
| Urban (> 400) | 711 (28.7) | 223 (43.6) | 49 (38.9) | 91 (43.1) |
| Mixed-urban (100–400) | 474 (19.1) | 127 (24.8) | 42 (33.3) | 59 (28.0) |
| Mixed-rural (20–99) | 820 (33.1) | 117 (22.9) | 28 (22.2) | 45 (21.3) |
| Rural (< 20) | 471 (19.0) | 43 (8.4) | 7 (5.6) | 16 (7.6) |
| Unknown | < 5 (0.1)† | < 5 (0.4)† | 0 (0.0) | 0 (0.0) |
| Hospital type | ||||
| Academic teaching hospital | 406 (16.4) | 172 (33.6) | 72 (57.1) | 79 (37.4) |
| Community hospital | 2072 (83.6) | 340 (66.4) | 54 (42.9) | 132 (62.6) |
| Clinical workload | ||||
| Inpatient E&M claims billed, mean (SD) | 409 (451) | 2090 (1589) | 1261 (444) | 3649 (1962) |
| Unique hospital inpatients seen, mean (SD) | 109 (101) | 408 (309) | 304 (161) | 614 (291) |
| Calendar days billed for hospital care, mean (SD) | 120 (92) | 180 (80) | 115 (49) | 220 (49) |
| % inpatients with previous medical relationship with physician, mean (SD) | 51.5 (30.7) | 20.0 (18.1) | 11.3 (7.0) | 10.8 (7.3) |
| Distribution of practice, %, mean (SD) | ||||
| Inpatient care | 9.1 (7.9) | 54.2 (15.5) | 91.4 (5.9) | 91.5 (5.9) |
| Office-based care | 78.9 (17.4) | 36.5 (19.4) | 6.6 (5.5) | 5.8 (4.8) |
| Emergency care | 6.3 (11.2) | 5.8 (11.7) | 1.9 (3.5) | 1.3 (2.9) |
| Long-term institutional care | 4.7 (12.3) | 3.3 (9.8) | 0.2 (1.0) | 1.4 (3.3) |
| Home-based care | 0.9 (3.2) | 0.3 (2.0) | 0.0 (0.0) | 0.0 (0.1) |
E&M = evaluation and management.
Except where indicated otherwise.
Counts < 5 have been suppressed.
To test our definitional algorithm, we validated the list of institutions where full-time and part-time general hospitalists (classified according to Table 1 and described in Table 3) billed the majority of inpatient services in 2010/2011 against 62 hospitals with and 101 hospitals without publicly disclosed hospitalist programs. The algorithm correctly identified 90% of hospitals known to employ hospitalists (specificity 98%, positive predictive value 97%). All of the false negatives (n = 6) were small community hospitals that had introduced hospitalist programs partway through the 2010/2011 fiscal year; the 2 false positives were large academic hospitals with general medicine teaching wards.
Interpretation
To our knowledge, this is the first study to propose a functional framework for defining and delineating physicians' inpatient practices on the basis of clinical volume of inpatient care. Our definition of hospitalist practice aligns with the functional approach of Kuo et al.1,15–22 but improves the administrative methodology by adding a continuous measure of inpatient volume, which allowed us to differentiate providers by their daily clinical workloads. In presenting this framework, our intent is not to suggest that these thresholds are exact or concrete, but rather to provide a descriptive structure that can accommodate the variety of practice styles and medical specialties that exist in hospital medicine. In doing so, we aim to move the methodology toward more objective and dynamic definitions of hospitalist practice, whereby clinical inpatient volumes can be analyzed as the primary predictor of physician practice and performance, accounting for additional provider characteristics, such as medical specialty, as desired. By examining the quality of general inpatient care as a function of a physician's annual case volume, we can extend the application of the hospitalist literature to additional acute care delivery models around the world that have instituted parallel focused-inpatient practices without necessarily establishing formalized hospitalist programs. The volume metrics and descriptive variables used in this study are simple to derive and are often captured at the population level through insurance billings and/or service utilization databases.
This is also the first study to describe the prevalence and characteristics of Ontario general hospitalists using systems-level data and to describe the emergence of hospital medicine and its impact on the provision of hospital care by other inpatient physicians. By examining changes in physician billing volumes over time, clinical practice data confirmed the introduction of GP/FP hospitalists to Ontario in the early 21st century and significant growth in the number of full-time general hospitalists practising each fiscal year since. Our estimates for the current number of hospitalists in practice vastly exceed those reported by the Canadian Society of Hospital Medicine based on its voluntary membership survey ( n = 1 10),13 which confirms our premise that self-reporting as a hospitalist underestimates the functional prevalence of hospital-based practitioners. Our demographic data for general hospitalists are consistent with those reported elsewhere.2,3,13
For ethical reasons we were unable to link de-identified administrative billings to a known cohort of hospitalist physicians to validate the inpatient volume thresholds proposed in our functional framework. This remains an important step in creating and refining a clinical definition of hospitalist practice. Despite this limitation, we were able to define and characterize a distinct cohort of general physicians who functionally devoted the majority of their practice to the care and management of hospital inpatients. We were able to validate our definitions at the institutional level with high precision and good sensitivity. Our definitions also had face validity triangulated across the 3 clinical volume metrics. In addition, we were able to describe trends in inpatient volume only among fee-for-service physicians, who account for about 90% of physicians working in Ontario. It is unlikely that this limitation affected our calculation of inpatient volumes or hospitalist estimates, as the majority of hospital services for general practitioners are still remunerated through feefor- service billings. Alternative payment plans are used primarily to reimburse community-based physicians and were reported to be uncommon among hospitalists responding to the Canadian Society of Hospital Medicine survey.13 Finally, this analysis focused exclusively on direct clinical care and case management; procedure volumes were not explored. This distinction resulted in some hospital-based specialties (surgery, anesthesiology, obstetrics and gynecology) having lower inpatient volumes than might have been expected. In many instances, these subspecialty inpatients are managed or comanaged by general hospitalists, which would reduce specialists' inpatient E&M claims to those immediately preceding or following a procedure.
When we replicated the functional definition of Kuo et al.1 with 2010/2011 OHIP claims data using a minimum volume of 100 E&M claims and an 80% inpatient practice ratio, prevalence estimates of general hospitalist practitioners were overinflated by 17%, capturing 67 physicians with low inpatient volumes reflecting minimally active practices. More importantly, the Kuo definition ignored a large segment of mixed-practice generalists (n = 512) whose clinical volumes and workload appeared to parallel if not exceed those of parttime hospitalists (Table 3). In a comparative evaluation, these physicians would be classified into the reference category, muting any associations that might ultimately be driven by clinical volume or experience, a wellestablished determinant of outcomes in health care delivery.23 To our knowledge, the relationship between clinical inpatient volume and outcomes of care has not been assessed.
Inpatient physicians are unified by the common goal of caring for hospital inpatients, and it is that professional focus which defines all practitioners, irrespective of medical specialty. As general and specialty hospitalists continue to grow in number across the globe, continuous metrics of clinical volume reflecting the dynamic continuum of inpatient practice may be advantageous for defining, identifying, and monitoring hospital-based physicians and their performance. By using the definitional framework proposed in this study, researchers can begin to test structural differences between inpatient delivery models, exploring which aspects of physician care—clinical experience, medical training, or a combination of both—correlate with changes in the processes of care delivery that in turn help to drive improvements in operating efficiency and clinical outcomes.
Footnotes
None declared.
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Heather White is supported by a Canada Graduate Scholarship provided through the Canadian Institutes of Health Research (CIHR FRN 96303) and by a doctoral fellowship provided through the Health System Performance Research Network (HSPRN), a multi-institution collaborative network also supported by the MOHLTC. Richard Glazier is supported as a Clinician Scientist in the Department of Family and Community Medicine at the University of Toronto and at St. Michael's Hospital. The opinions, results, and conclusions expressed in this manuscript are those of the authors and are independent from the funding sources. No endorsement by ICES, CIHR, HSPRN, or the Ontario MOHLTC is intended or should be inferred.
Contributor Information
Heather L. White, Heather L. White, MSc, is a PhD candidate at the Institute of Health Policy, Management and Evaluation, University of Toronto, and a student at the Institute for Clinical Evaluative Sciences, Toronto, Ontario.
Thérèse A. Stukel, Thérèse A. Stukel, PhD, is a Senior Scientist at the Institute for Clinical Evaluative Sciences, Toronto, Ontario; an Adjunct Professor at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Hanover, New Hampshire; and a Professor at the Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, Ontario.
Walter P. Wodchis, Walter P. Wodchis, PhD, is an Associate Professor at the Institute of Health Policy, Management and Evaluation, University of Toronto; an Adjunct Scientist at the Institute for Clinical Evaluative Sciences; and a Scientist at the Toronto Rehabilitation Institute, Toronto, Ontario.
Richard H. Glazier, Richard H. Glazier, MD, MPH, FCFP, is a Senior Scientist at the Institute for Clinical Evaluative Sciences; a Professor at the Institute of Health Policy, Management and Evaluation and the Department of Family and Community Medicine, University of Toronto; a Scientist at the Centre for Research on Inner City Health in the Keenan Research Centre of the Li Ka Shing Knowledge Institute, St. Michael's Hospital; and a Clinician Scientist and Family Physician in the Department of Family and Community Medicine, St. Michael's Hospital, Toronto, Ontario.
References
- 1.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yousefi V, Wilton D. Re-designing hospital care: learning from the experience of hospital medicine in Canada. J Glob Health Care Syst. 2011;1(3):1–10. Available from: http://jghcs.info/index.php/j/article/view/47/57. [Google Scholar]
- 3.Soong C, Fan E, Howell EE, Maloney RJ, Pronovost PJ, Wilton D, et al. Characteristics of hospitalists and hospitalist programs in the United States and Canada. J Clin Outcomes Manag. 2009;16(2):69–74. [Google Scholar]
- 4.Wachter RM. The state of hospital medicine in 2008. Med Clin North Am. 2008;92(2):265–273. doi: 10.1016/j.mcna.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Wachter RM, Bell D. Renaissance of hospital generalists. BMJ. 2012;344:e652–e652. doi: 10.1136/bmj.e652. [DOI] [PubMed] [Google Scholar]
- 6.Kralovec PD, Miller JA, Wellikson L, Huddleston JM. The status of hospital medicine groups in the United States. J Hosp Med 2006. 1;2:75–80. doi: 10.1002/jhm.82. [DOI] [PubMed] [Google Scholar]
- 7.White H, Glazier R. Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58–58. doi: 10.1186/1741-7015-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Definition of a hospitalist and hospital medicine. Philadelphia (PA): Society of Hospital Medicine; 2009. Available from: www.hospitalmedicine.org/AM/Template.cfm?Section=Hospitalist_Definition&Template=/CM/HTMLDisplay.cfm&ContentID=24835 (accessed 2010 Jan 31). [Google Scholar]
- 9.Nelson JR, Wellikson L, Wachter RM. Specialty hospitalists: analyzing an emerging phenomenon. JAMA. 2012;307(16):1699–1700. doi: 10.1001/jama.2012.526. [DOI] [PubMed] [Google Scholar]
- 10.Dawes R, Newman E, Lofsky S, McNestry G, Willet J, Devilla E, et al. Why Ontario physicians are leaving hospital work: results of a 2002 OMA study. Ont Med Rev. 2004;3:9–9. [Google Scholar]
- 11.Sullivan P. Enter the hospitalist: new type of patient creating a new type of specialist. CMAJ. 2000;162(9):1345–1346. [PMC free article] [PubMed] [Google Scholar]
- 12.Smith SD, Sivjee K. Defining training needs, core competencies and future certification for Canadian hospitalists. CMAJ. 2012;184(14):1557–1558. doi: 10.1503/cmaj.110925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilton D, Maloney R. The Canadian national hospitalists survey 2007. Refining the hospitalist model. Toronto (ON): Canadian Society of Hospital Medicine; 2008. [Google Scholar]
- 14. Ontario Physician Human Resources Data Centre , author. Physicians in Ontario 2010: reports from the active physician registry. Hamilton (ON): McMaster University; 2010. Available from: www.ophrdc.org/Public/Report.aspx (accessed 2013 Feb 2). [Google Scholar]
- 15.Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999;130(4 Pt 2):338–342. doi: 10.7326/0003-4819-130-4-199902161-00002. [DOI] [PubMed] [Google Scholar]
- 16.Wachter RM, Goldman L. The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335(7):514–517. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- 17.Sharma G, Freeman J, Zhang D, Goodwin JS. Continuity of care and intensive care unit use at the end of life. Arch Intern Med. 2009;169(1):81–86. doi: 10.1001/archinternmed.2008.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Craig DE, Hartka L, Likosky WH, Caplan WM, Litsky P, Smithey J. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med. 1999;130(4 Pt 2):355–359. doi: 10.7326/0003-4819-130-4-199902161-00005. [DOI] [PubMed] [Google Scholar]
- 19.Yousefi V, Evan M. Hospital medicine maturity framework: proposing a novel framework for defining stages of hospital medicine in Canada. Healthc Q. 2011;14(4):67–73. doi: 10.12927/hcq.2011.22653. [DOI] [PubMed] [Google Scholar]
- 20.Kuo YF, Goodwin JS. Effect of hospitalists on length of stay in the medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58(9):1649–1657. doi: 10.1111/j.1532-5415.2010.03007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fletcher KE, Sharma G, Zhang D, Kuo YF, Goodwin JS. Trends in inpatient continuity of care for a cohort of Medicare patients 1996� 2006. J Hosp Med. 2011;6(8):438–444. doi: 10.1002/jhm.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152–159. doi: 10.1059/0003-4819-155-3-201108020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]