Abstract
The aim of this work was to present the LeFort I segmented osteotomy in consecutive patients using the piezoelectric system. A descriptive study was designed for patients operated on between November 2012 and January 2014. All the patients presented some type of skeletal anomaly and underwent orthognatic surgery via piezoelectric osteotomies. Each maxillary surgery was developed with that system and those patients who also received osteotomies with a reciprocating saw were excluded. Surgical time and complications were analyzed. 19 patients underwent surgery consecutively with an osteotomy average time of 45 minutes. The patients operated on at the beginning were longer surgeries, whereas the final cases were 40 minutes. No type of laceration of vascular elements or laceration of palatal tissue was observed. The protocol was fully implemented, incorporating all the advantages of piezoelectric systems. It is concluded that the LeFort I segmented osteotomy can be performed with low risk of injuring soft tissues and in a time probably less than 50 minutes for the maxillary osteotomy.
Keywords: Piezoelectric osteotomy, piezoelectric surgery, LeFort I osteotomy
Introduction
Nowadays, piezoelectric systems have modified aspects in osteotomies techniques [1,2]. These are systems characterized by the well defined and the clear osteotomy with low risk of injury to the surrounding soft tissue [3].
Labanca [3] conducted a broad review of the procedures performed in maxillofacial surgery with a piezoelectric system, showing mainly experiences of the best-known procedures. The results are favorable and describe advantages of using this system, including reduction in nerve injuries, sinus membrane and dura mater mainly due to the increased refrigeration and the selective cut that the system makes exclusively on mineralized tissue [4]. In addition, with the piezoelectric system there is a statistically more favorable bone repair both quantitatively and qualitatively than with traditional mechanical systems [5].
One relevant aspect in the development of the technique is that the learning curve is relatively low; for surgeons, well trained in the conventional surgical technique; the changeover to a piezoelectric system with low morbidity can be rapidly incorporated into the surgical technique [6].
The aim of this study was to describe the development of the segmented maxillary osteotomy with exclusive use of piezoelectric systems in consecutive cases.
Materials and methods
A descriptive cross-sectional study was designed and implemented in the Division of Oral and Maxillofacial Surgery at the Universidad de La Frontera, Temuco, Chile and in the private clinic of one of the authors (S.O.). The patients included in the study were informed of its scope and signed an informed consent.
Patients were included with no distinction of age or gender that underwent surgery between November 2012 and January 2014 by LeFort I segmented osteotomy (considering two to four segments). The patients had been diagnosed with class I, II or III facial deformity, facial asymmetry or anterior open bite deformity. Patients with not requirement of maxillary segmentation, patients with previous maxillofacial treatment such as osteogenic distraction, patients with a history of facial trauma or a diagnosis of maxillofacial congenital anomaly were excluded from the study.
Surgical technique
For the osteotomies, the Piezotome2® was used in D4 mode (Satelec Acteon). Under general anesthesia and standard conditions of hypotension, the procedure began with an incision with an electroscalpel over 8 mm from the mucogingival line, covering the distance from the first right premolar to the first left premolar. Once the maxilla had been exposed and the pyriform aperture released, the position of the osteotomies was determined.
This began with the BS1 tip (straight 10 mm deep and 2.5 mm wide), executing the LeFort I osteotomy from the right side between the pyriform aperture and the maxillary zygomatic buttress. Then the BSL tip (straight 1.5 mm deep, 3 mm wide and 1 mm thick) was used for the osteotomy behind the maxillary zygomatic buttress as far as the pterygoid fossa; the same procedure was used for the contralateral osteotomy. Then the curved Obwegeser osteotome was used in the pterygoid fossa, a vomer chisel in the nasal septum and with the BSL tip the osteotomy was performed on the medial wall of the maxillary sinus, following up to 20 mm posterior. Access was gained with Wagner osteotome to finalize the osteotomy of the medial wall of the maxillary sinus. At no stage was a reciprocating saw or drill used, nor a malleable retractor in the nasal fossa or external irrigation, using the irrigation integrated into the system exclusively.
Before that maxilla was in LeFort I down fracture, the osteotomies for the segmentation are marked with a CS3 tip (10 mm of cut) (Figures 1 and 2) and subsequent to the maxillary inferior repositioning, maxillary mobilization and hemostasis, the segmentations were made beginning with the CS3 tip (10 mm of cut) on the vestibular surface at dental level until reaching the upper limit of the osteotomy. The osteotomy continued on the palatal surface, starting from the posterior sector of the palatal bone and following through the maxilla until communicating with the anterior maxillary area, always reaching until the palatal periosteum could be felt. To finish, the osteotomy was extended with the BSL tip into the vestibular sector in order to communicate with the palatal cortex (premaxila area mainly). Alternatively, the CS1 tip was used to optimize the cutting surface but at no time were drills, saws or chisels used to perform the osteotomies and a T-shaped chisel was used when finalizing the procedure to render the segments mobile (Figure 3).
Figure 1.
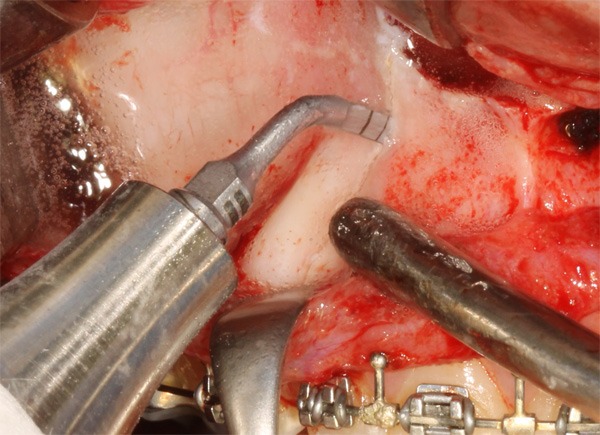
BS1 tip in position to perform the segmental osteotomy in the right side of the maxilla.
Figure 2.
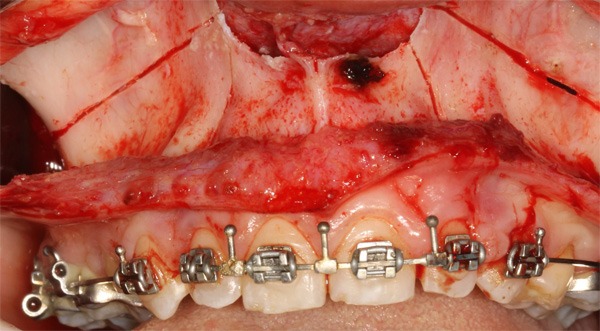
LeFort I osteotomy and partial segmented osteotomy performed before of down fracture.
Figure 3.
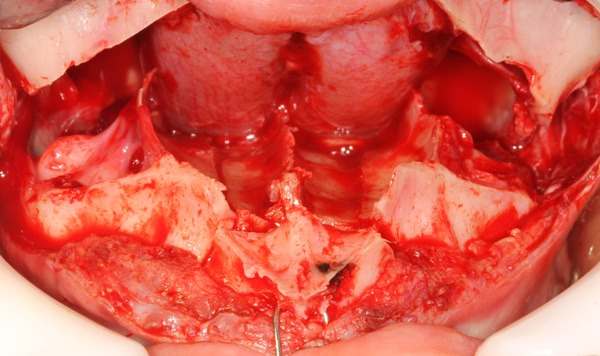
Classical “H” type segmented osteotomy on nasal floor with total sagittal extension; the cortical area of the palatal side is segmented and the buccal area is segmented.
The data were studied descriptively, analyzing the time spent on the maxillary surgery, the injuries generated in the palatal soft tissue, the associated complications and the subjective characteristics of the procedure.
Results
19 consecutive patients aged between 17 and 34 years underwent surgery with the technique described. In all the procedure was done without complications. The average time for the osteotomies was 48 minutes, considering that the first procedures took around 58 minutes and the last procedures around 40 minutes. No lesions were observed in the soft tissue or lacerations of the palatal mucosa, lacerations of the posterior soft tissue pedicle, or lacerations of the vascular elements. Injuries to the teeth, dental necrosis or necrosis of the osteotomized segments were not observed either (Figure 4).
Figure 4.
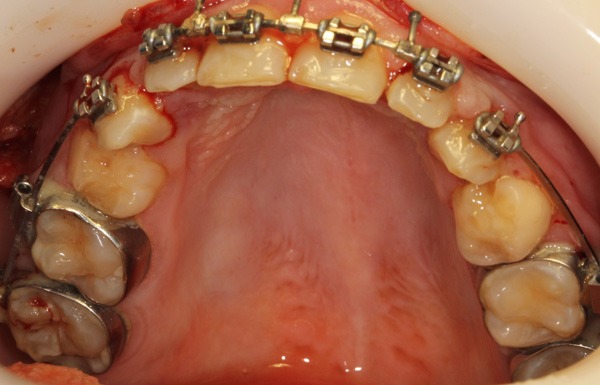
Palatal soft tissue after segmented LeFort I Osteotomy, showing absence of laceration, edema or other complication related to the osteotomy.
The osteotomy was most time-consuming in the maxillary zygomatic buttress due to the greater amount of cortical bone. Throughout the procedure a clear and stable view was achieved, with a low level of bleeding and adequate irrigation of the cutting area. Separation of the nasal mucosa was not needed during the LeFort I osteotomy and protection retractors were not used in the segmented osteotomy either.
Discussion
Piezoelectric systems have evolved favorably in recent years. Their use has made possible the optimization of some surgical techniques1 and attained favorable results, reducing the risks of the surgery.
This technique has been reported as successful in other procedures [3] and it has been described that its use presents great advantages, such as 1) clarity and control in the osteotomy, 2) decrease in the severity of tissue separation and detachment, 3) irrigation in the system itself, reducing the need for irrigation by the assistant, 5) lower risk of injuring soft tissues and vascular structures.
The first reports of the maxillary segmented osteotomy with piezoelectric systems came from Robiony [7], who presented the technique together with the analysis of some cases; nevertheless, it was a low-power piezosurgery system. Recently, other cortical segmentation techniques have been published that permit accelerated dental movements with a low risk of periodontal damage [8].
Landes [2] published a critical review of orthognatic surgery performed with a piezoelectric system, reporting that during the LeFort I osteotomy, in the stages of separating the maxilla with the pterygoid process and separating the nasal septum, chisels were needed in 100% of the cases, as in conventional technique. Our results also relate the same indication for work with chisels, which are related to the anatomical variations and to the difficulty the approach with this tips those places. Nevertheless, a recent study by Guilles [9] showed a new tip design in the piezoelectric system that might eliminate the need for chisels during surgery.
It has been indicated that the main disadvantages of orthognatic surgery with a piezoelectric system are the increased surgery time and control of the pressure that the tip places on the bone since the increase in this phase can increase the temperature and damage tissue [10], although Schütz [11] have already shown that this temperature may not be not relevant. Spinelli [12] also reported an increase in surgery time of the bimaxillary osteotomy. Nevertheless, the new piezoelectric osteotomy systems, like those used in this study, can exceed the limitations of surgery time, reporting efficient results in times similar to those with a reciprocating saw [13]. Shirota [14] also reported that surgery time did not present any differences compared to the osteotomy with reciprocating saw and osteotomy with a piezoelectric system. Considering the learning curve, in this group of consecutive patients, lower surgery times were observed in the last patients compared to the first operated on with this technique, demonstrating that achieving adequate times for performing the LeFort I segmented osteotomy is viable.
One of the important results of this study is the total absence of soft tissue injuries, both in the posterior pedicle and in the vascular elements and palatal tissues; this gives the surgery a great deal of security during the procedure. Spinelli [12] indicated that the piezoelectric system represents a low risk for the LeFort I osteotomy, also reporting less post-operative edema and less blood loss than in osteotomies with saws.
Finally, taking the limitations of this study into consideration, it can be concluded that segmented maxillary osteotomies with piezoelectric systems can be performed with a low risk of injuring soft tissues and in a time probably less than 50 minutes for the maxillary osteotomy.
Disclosure of conflict of interest
None.
References
- 1.Olate S, Unibazo A, Almeida A, de Moraes M. Mandibular condylectomy revisited: technical notes concerning the use of an ultrasonic system. J Oral Maxillofac Surg. 2014;72:481–484. doi: 10.1016/j.joms.2013.09.040. [DOI] [PubMed] [Google Scholar]
- 2.Landes C, Stübinger S, Rieger J, Willinger B, Ha TK, Sader R. Critical evaluation of piezoelectric osteotomy in orthognathic surgery: operative technique, blood loss, time requirement, nerve and vessel integrity. J Oral Maxillofac Surg. 2008;66:657–674. doi: 10.1016/j.joms.2007.06.633. [DOI] [PubMed] [Google Scholar]
- 3.Labanca M, Azzola F, Vinci R, Rodella L. Piezoelectric surgery: twenty years of use. Br J Oral Maxillofac Surg. 2008;46:265–269. doi: 10.1016/j.bjoms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Eggers G, Klein J, Blank J, Hassfeld S. Piezosurgery: an ultrasound device for cutting bone and its use and limitations in maxillofacial surgery. Br J Oral Maxillofac Surg. 2004;42:451–453. doi: 10.1016/j.bjoms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Gülnahar Y, Hüseyin Kösger H, Tutar Y. A comparison of piezosurgery and conventional surgery by heat shock protein 70 expression. Int J Oral Maxillofac Surg. 2013;42:508–510. doi: 10.1016/j.ijom.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 6.Pavlíková G, Foltán R, Burian M, Horká E, Adámek S, Hejel A, Hanzelka T, Sedú J. Piezosurgey prevents brain tissue damage: an experimental study on a new rat model. Int J Oral Maxillofac Surg. 2011;40:840–844. doi: 10.1016/j.ijom.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Robiony M, Polini F, Costa F, Vercellotti T, Politi M. Piezoelectronic bone cutting in multipiece maxillary osteotomies. J Oral Maxillofac Surg. 2004;62:759–61. doi: 10.1016/j.joms.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Bertossi D, Vercellotti T, Podesta A, Nocini PF. Orthodontic microsurgery for rapid dental repositioning in dental malpositions. J Oral Maxillofac Surg. 2011;69:747–753. doi: 10.1016/j.joms.2009.07.112. [DOI] [PubMed] [Google Scholar]
- 9.Gilles R, Couvreur T, Dammous S. Ultrasonic orthognathic surgery: enhacements to established osteotomies. Int J Oral Maxillofac Surg. 2013;42:981–987. doi: 10.1016/j.ijom.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Budd JC, Gekelman D, White JM. Temperature rise of the post and on the root surface during ultrasonic post removal. Int Endod J. 2005;38:705–11. doi: 10.1111/j.1365-2591.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- 11.Schütz S, Egger J, Kühl S, Filippi A, Lambrecht JT. Intraosseous temperatura changes during the use of piezosurgical inserts in vitro. Int J Oral Maxillofac Surg. 2012;41:1338–1343. doi: 10.1016/j.ijom.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Spinelli G, Lazzeri D, Conti M, Agostini T, Mannelli G. Comparison of Piezosurgery and Traditional Saw in Bimaxillary Orthognathic Surgery. J Craniomaxillofac Surg. 2014 doi: 10.1016/j.jcms.2014.02.011. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Monnazzi MS, Real Gabrielli MF, Passeri LA, Cabrini Gabrielli MA, Spin-Neto R, Pereira-Filho VA. Inferior alveolar nerve function after sagital split ramus osteotomy by reciprocating saw or piezosurgery instrument: prospective double-blinded study. J Oral Maxillofac Surg. 2014;72:1168–72. doi: 10.1016/j.joms.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Shirota T, Kamatani T, Yamaguchi T, Ogura H, Maki K, Shintani S. Effectiveness of piezoelectric surgery in reducing surgical complications after bilateral sagittal Split osteotomy. Br J Oral Maxillofac Surg. 2014;52:219–222. doi: 10.1016/j.bjoms.2013.11.015. [DOI] [PubMed] [Google Scholar]


