Abstract
Mental health and health related quality of life is commonly affected in patients with chronic problems and their caregivers. In the present study, it was aimed to assess depression and anxiety in patients with beta thalassemia major (BTM) and in their caregivers; and to evaluate effects of these disorders on quality of life. The study was carried out in a district Hereditary Hemoglobinopathy Center and included 88 patients with BTM and 63 of their caregivers. All subjects were assessed using Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI) and Short Form-36 (SF-36) by a trained psychiatry resident via face-to-face interview. The BDI scores were 17 or above in 20.5% of the patients with BTM and 28.6% of their caregivers (P = 0.248). Of the patients with BTM, there were mild anxiety symptoms in 19.3%, while moderate and severe anxiety symptoms in 14.8% and 4.5%, respectively. Anxiety levels were similar between the patients with BTM and their caregivers (P = 0.878). It was found that BDI and BAI scores were negatively correlated to scores of physical health and mental health components of SF-36 in patients with BTM and their caregivers. In linear regression analysis, it was seen that depression affected physical and mental health of the patients with BTM and their caregivers regardless from anxiety. BTM leads an increase in the frequency of depression and anxiety in both patients and their caregivers, and affects negatively physical and mental components of quality of life.
Keywords: Beta-thalassemia, quality of life, anxiety, depression, caregivers
Introduction
Thalassemia is the most common form of inherited anemias [1]. Our country is among regions with high risk for thalassemia [2]. In the 2006 report of Ministry of Health and Turkish National Hemoglobinopathy Council, prevalence of beta thalassemia trait was reported as 4.3%. This rate was reported as 10% in Mediterranean region and 13.1% in Hatay province [3].
As in all chronic patients, patients with beta thalassemia major (BTM) are also vulnerable to emotional and behavioral problems [4]. Particularly, this vulnerability is enhanced in children with chronic diseases [5]. BTM affects emotional conditions, daily activities, family experiences and occupational capabilities of the patients and their caregivers because of lifelong complicated and burdensome therapeutic protocols.
Children with chronic hematological disorders can be predisposed to anxiety and depressive mood because of social problems such as separation from family, restricted social activities, physical and facial deformities, death anxiety, and limitations in school and play activities [6].On the other hand, there are studies reporting early psychological maturation in children with chronic disease as they are coping with psychological and medical consequences of the disease [7].
Factors influencing quality of life in patients with BTM include severity of anemia symptoms, frequency of transfusion, adverse effects of chelation therapy, comorbid diseases and psychological disorders such as depression and anxiety [8]. Although increased life expectancy and improved complication rates have been observed in patients with beta thalassemia in recent years, invasive medical interventions and their complications still affect quality of life in all patients and their caregivers [8].
In the literature, although there are published studies about psychiatric problems and quality of life in patients with BTM [8-12], there are limited number of studies investigating such problems in their caregivers [13-15]. In the present study, we aimed to assess levels of depression and anxiety in patients with beta thalassemia major (BTM) and their caregivers; and to evaluate effects of these disorders on quality of life.
Methods
The study was carried out with the approval of the Human Medical Ethics Committee of the Mustafa Kemal University Faculty of Medicine in Hatay.
Subjects
The study included 94 patients older than 12 years of age who presented to Hatay Public Health Directorship Center of Diagnosis, Control and Education of Thalassemia and Sickle Cell Anemia. According to the District Health Directorate Records, there were 393 BTM patients and 172 were over 12 years, and all of them were invited to participate. Among family members, the one who is responsible from care of the patient and/or one who spends more time with the patient were assigned as caregiver of the patient. Of these, 27 individuals who refused to participate or who are illiterate or who had chronic disease were excluded. Four patients with BTM were also excluded as they are illiterate.
Ninety patients with BTM and 67 caregivers completed a questionnaire addressing sociodemographic characteristics. Also, all subjects were assessed by Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI). To assess quality of life (QOL), Short Form-36 (SF-36) was applied by psychiatry residents via face-to-face interview. During assessments, 2 patient with BTM and 4 caregivers were excluded due to inadequate completion of questionnaire. Thus, data of 88 patients and 63 caregivers were included analysis.
Questionnaire form
This form was developed by researchers to assess sociodemographic and clinical characteristics of the subjects. Form consisted of questions addressing sociodemographic characteristics including age, gender, educational status, monthly income and clinical characteristics including frequency of transfusion, type of iron chelation, presence of splenectomy, history of psychiatric disorder.
MOS 36-item short form health survey (SF-36)
It is a self-assessment tool used to measure quality of life in individuals with a physical disease, which was developed by Ware and Sherbourne in 1992 [16]. Turkish validity study was performed by Koçyiğit et al. 1999 [17]. It has 8 subscales including physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). The first five scales are summarized into the physical health dimension and the last three scales into the mental health dimension. Each subscale is rated between 0 and 100 points. Standards for Turkish population regarding scale ratings were identified by Demiral et al. in 2004 [18].
Beck Anxiety Inventory (BAI)
It is a self-assessment tool used to determine frequency of anxiety symptoms experienced by an individual, which was developed by Beck et al. in 1988. It includes 21 items, which are rated by a 3-points Likert type scale. Turkish reliability and validity studies were performed by Ulusoy et al. in 1998. In this tool, 8-15 points is considered as mild anxiety while 16-25 points and 26-63 points are considered as moderate and severe anxiety, respectively [19].
Beck Depression Inventory (BDI)
This tool measures physical, emotional, cognitive and motivational symptoms observed in depression. It includes 21 items, which are rated by a 3-points Likert type scale. Higher total scores indicate increased severity of depression [20]. Turkish adaptation, validation and reliability studies were performed by Hisli et al. who reported cut-off point as 17 [21].
Statistical analysis
The collected data were analyzed by using the SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Both descriptive and analytic statistics were used. Chi-square/Fischer’s test was used for comparisons between categorical variables. Normal distribution of continuous variables was tested with Kolmogorov-Smirnov test. Normally distributed parametric variables were compared between groups by using Student’s t test. The Mann–Whitney U test was used for the comparison of continuous variables which were not normally distributed. Pearson correlation coefficients were used to assess relationships among depression, anxiety, physical health dimension and mental health dimension scores of patients and their caregivers. The relationships between SF-36 main components (physical health component summary and mental health component summary) and depression or anxiety were assessed by linear logistic regression analysis. P < 0.05 was considered as statistically significant in all analysis.
Results
Of the 88 patients with BTM included to the study, 40.9% (n = 36) were men and 59.1% (n = 52) were female. Of the 63 caregivers, 50.8% (n = 32) were male and 49.2% (n = 31) were women. Of the 63 caregivers, 44.4% (n = 28) were mother and 46.1% (n = 29) were father, while 9.5% (n = 6) were siblings.
Mean age was 17.42 ± 4.65 years (min-max: 12-41) in patients with BTM, where as 36.25 ± 9.50 years (min-max: 16-77) in their caregivers. Sociodemographic characteristics and interactions in patients with thalassemia major and their relatives shown in Table 1. Disease and treatment related characteristics in patients with thalassemia major shown in Table 2.
Table 1.
Sociodemographic characteristics and interactions in patients with thalassemia major and their relatives
| Variables | Patient n (%) | Relatives n (%) |
|---|---|---|
| Education | ||
| Primary and secondary school | 67 (76.2%) | 56 (88.9%) |
| High School | 20 (22.7%) | 6 (9.5%) |
| University | 1 (1.1%) | 1 (1.6%) |
| Marital status | ||
| Single | 84 (95.5%) | 6 (9.5%) |
| Married | 4 (4.5%) | 57 (90.5%) |
| Economic class | ||
| Low income | 49 (55.7%) | 45 (71.4%) |
| Moderate | 28 (31.8%) | 10 (15.9%) |
| High | 11 (12.5%) | 8 (12.7%) |
| Residence | ||
| Rural | 44 (50.0%) | 37 (58.7%) |
| Suburban | 22 (25.0%) | 10 (15.9%) |
| Urban | 22 (25.0%) | 16 (25.4%) |
| History of psychiatric disorders | ||
| Positive | 83 (94.3%) | 59 (93.7%) |
| Negative | 5 (5.7%) | 4 (6.3%) |
| Suicidal ideation | ||
| Present | 85 (96.6%) | 62 (98.4%) |
| Absent | 3 (3.4%) | 1 (1.6%) |
| Smoking | ||
| No | 86 (97.7%) | 42 (66.7%) |
| Yes | 2 (2.3%) | 21 (33.3%) |
| Alcohol consumption | ||
| No | 84 (95.5%) | 60 (95.2%) |
| Yes | 4 (4.5%) | 3 (4.8%) |
Table 2.
Disease and treatment related characteristics in patients with thalassemia major
| Variables | Patient n (%) |
|---|---|
| Family history of hematological disease | |
| Sibling | 25 (28.4%) |
| Cousin | 8 (9.1%) |
| None | 55 (62.5%) |
| History of death due to hematological disease in the family | |
| No | 73 (82.4%) |
| Yes | 15 (17.6%) |
| Adherence to therapy | |
| Regular | 68 (77.3%) |
| Irregular | 20 (22.7%) |
| Transfusion frequency | |
| Once every 2 weeks | 5 (5.7%) |
| Once every 3 weeks | 60 (68.2%) |
| Once every 4 weeks | 23 (26.1%) |
| Adherence to iron therapy | |
| Regular | 74 (84.1%) |
| Irregular | 14 (15.9%) |
| Splenectomy | |
| No | 59 (67.0%) |
| Yes | 29 (33.0%) |
| Stem cell transplantation | |
| No | 86 (97.7%) |
| Yes | 2 (2.3%) |
Beck depression scores (BDS) were 8.89 ± 7.55 (min-max: 0-45) in patients with BTM and 10.63 ± 9.39 (min-max: 0-44) in their caregivers (P = 0.0211). BDS was below 17 points in 79.5% (n = 70) of the patients with BTM and 71.4% (n = 45) of their caregivers, while it was 17 points or above in 20.5% (n = 18) and 28.6% (n = 18) of the patients with BTM and their caregivers, respectively. The caregivers with depression symptoms included 11 mothers (61.1%), 5 fathers (27.8%) and 2 siblings (11.2%).
BDS were 8.45 ± 7.73 (min-max: 0-36) in patients with BTM and 7.85 ± 6.77 (min-max: 0-36) in their caregivers (P = 0.623). There was mild anxiety symptoms in 19.3% (n = 17), while moderate and severe anxiety symptoms in 14.8% (n = 13) and 4.5% (n = 4) of the patients with BTM, respectively. Of the caregivers, mild anxiety symptoms were detected in 23.8% (n = 15), while moderate and severe anxiety symptoms in 15.9% (n = 10) and 1.6% (n = 1), respectively. The caregivers with moderate and severe anxiety symptoms included 7 mothers (63.6%), 3 fathers (27.3%) and one sibling (9.1%).
Quality of life scores (SF-36) of patients with BTM and their caregivers were presented in Table 3. Physical functioning and general health scores were found to be significantly lower in patients with BTM when compared to their caregivers (P = 0.0001 and P = 0.007, respectively).
Table 3.
Health-related quality of life of the patients with beta-thalassemia major and their caregivers according to the Short Form-36 (SF-36) score
| Patients with Beta-Thalassemia Major | Caregivers | P | |
|---|---|---|---|
| Physical functioning | 66.53 ± 14.66 | 79.52 ± 16.50 | 0.0001* |
| Role-physical | 52.84 ± 33.56 | 53.57 ± 37.79 | 0.972** |
| Bodily pain | 78.73 ± 23.48 | 74.57 ± 28.28 | 0.595** |
| General health | 50.12 ± 18.10 | 58.23 ± 17.90 | 0.007* |
| Vitality | 55.45 ± 16.03 | 50.87 ± 15.46 | 0.081* |
| Social functioning | 84.65 ± 15.71 | 80.95 ± 17.22 | 0.160** |
| Role-emotional | 41.28 ± 41.36 | 45.50 ± 42.88 | 0.528** |
| Mental health | 59.77 ± 15.32 | 57.39 ± 12.71 | 0.316* |
| Physical health component summary | 60.73 ± 12.79 | 63.35 ± 14.09 | 0.237* |
| Mental health component summary | 61.90 ± 17.74 | 61.28 ± 16.24 | 0.826* |
All values are presented as mean ± standard deviation.
Student T-test;
Mann Whitney U Test.
It was found that there was a negative correlation between BDS and scores of physical health component summary and mental health component summary in patients with BTM and their caregivers. Also, it was found that there was a negative correlation between Beck anxiety scores and scores of physical health component summary and mental health component summary in patients with BTM and their caregivers (Table 4).
Table 4.
Correlation of physical and mental health dimensions of SF-36 with BDI and BAI in patients and their caregivers
| SF-36 Main Components | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Physical health component summary | Mental health component summary | |||||||||
|
|
|
|||||||||
| Patients | Caregivers | Patients | Caregivers | |||||||
| Depression Symptoms | Present | 51.70 ± 9.71 (n:18) | p = 0.0001 R = -0.468 | 54.77 ± 15.66 (n:18) | p = 0.0001 R = -0.533 | 55.26 ± 19.96 (n:18) | p = 0.0001 R = -0.368 | 50.95 ± 8.10 (n:18) | p = 0.0001 R = -0.433 | |
| Absent | 63.06 ± 12.4 (n:70) | 66.8 ± 11.95 (n:45) | 63.61 ± 16.86 (n:70) | 65.41 ± 16.89 (n:45) | ||||||
| Anxiety Symptoms | Moderate or severe | 55.23 ± 15.71 (n:17) | p = 0.0001 R = -0.366 | 53.32 ± 17.43 (n:11) | p = 0.0001 R = -0.478 | 56.59 ± 20.32 (n:17) | p = 0.006 R = -0.291 | 55.65 ± 17.97 (n:11) | p = 0.048 R = -0.250 | |
| None or mild | 62.05 ± 11.73 (n:71) | 65.47 ± 12.47 (n:52) | 63.17 ± 16.98 (n:71) | 62.47 ± 15.78 (n:52) | ||||||
Linear regression analysis was performed to determine contribution of depression and anxiety scores to physical health component summary scores in patients with BTM and their caregivers. It was found that physical health component summary score was influenced by depression scores while anxiety scores had no effect on physical health component scores in patients with BTM and their caregivers (Figure 1).
Figure 1.
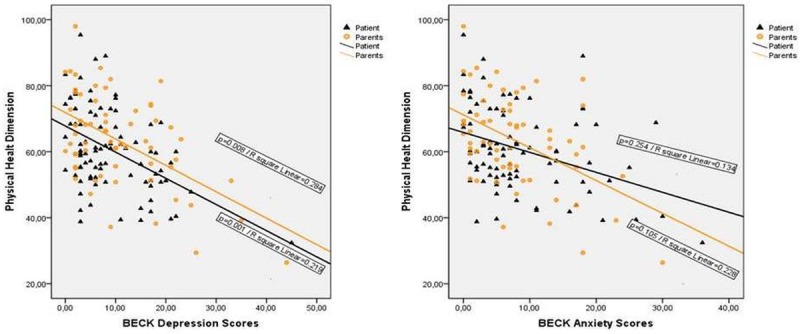
Linear regression analysis on determinants of the physical health component summary scores among patients with BTM and their caregivers.
In the linear regression analysis performed to determine contribution of depression and anxiety scores to mental health component summary scores, it was found that mental health component summary score was influenced by depression scores while anxiety scores had no effect on mental health component scores in patients with BTM and their caregivers (Figure 2).
Figure 2.
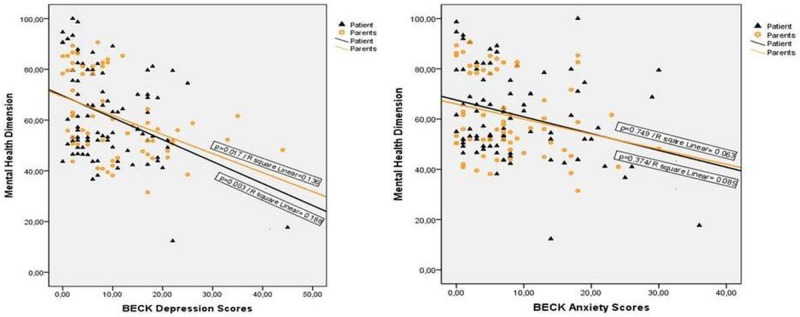
Linear regression analysis on determinants of the mental health component summary score among patients with BTM and their caregivers.
Discussion
Changes in mental health and health related quality of life in chronically ill patients were well established previously. To best of our knowledge, this is the first study in Turkey investigating mental health and quality of life both in patients with BTM and their caregivers. Also results of the present study is striking and has potential implications for future research.
Cakaloz et al. reported that psychopathology was common in patients with BTM [22]. Authors reported that, among these, incidences of social withdrawal, somatic complaints, social externalizing, attention disorders and anxiety-depression were higher; in particular, major depression and anxiety were most frequently seen psychological disorders. Similarly, Ghanizadeh et al. reported that most commonly observed psychopathologies were major depression and anxiety in patients with BTM [10]. Authors reported that there was depressive mood in 49%, anger and irritability in 62.7% and repetitive death anxiety in 43% of the patients. In addition, no significant difference was found regarding suicidality in that study [10]. Cakaloz et al. detected depressive disorder in 15% and anxiety disorder in 30% of the children with TM [22]. In a study by Aydınok et al., frequency of depressive disorder was reported as 23% in patients with TM [9]. In our study, depression symptoms were detected in 20.5%, while anxiety symptoms at varying severity were detected in 38.6% of patients with BTM. No significant difference was found between patients with BTM and their caregivers regarding suicidality.
In a study, in which frequency of depression was evaluated in mothers of the patients with thalassemia or hematological malignancies, Shargi et al. reported the frequency of depression as 51% [15]. In a study from Pakistan, Aziz K et al. reported this rate as 71% [13]. In our study, depression symptoms were detected in 28.6% of the caregivers of BTM patients. Of the caregivers with depression symptoms, 61.1% were mothers, while 27.8% and 11.1% were fathers and siblings. Depression was most commonly observed in mothers. In our study, it was found that depression was present in 39.3% of all mothers, whereas in 17.2% of all fathers. Anxiety symptoms at varying severity were detected in 41.3% of the caregivers of BTM patients. It was seen that although majority of the caregivers (63.6%) with moderate or severe anxiety symptoms were mother, rate of anxiety was 25% among all mothers and 10.3% among all fathers. Although proportions of mothers and fathers were similar among caregivers, rates of depression and anxiety were found to be higher among mothers. This can be explained by the fact that mothers are emotionally more vulnerable and that they undertake the caregiver role in Turkish families.
Psychological disorders in patients with BTM are important factors influencing quality of life. In the literature, it has been reported that psychiatric or psychological counseling to patients is beneficial for improvement in both adherence to treatment and mental quality of life [23]. Similarly, it has been reported that, in addition to medical therapies, psychopathological evaluation and treatment, if indicated, can positively affect quality of life in patients with BTM [24].
In a study on patients with thalassemia major or intermedia, Azarkeivan A et al. reported that depression negatively affected quality of life in both physical and mental manner. Authors demonstrated that anxiety had negative effects on quality of life in mental manner [25]. Hajibeii B et al. evaluated effects of anxiety and depression on sleep quality and quality of life in patients with BTM and found that these psychopathologies negatively affected sleep quality and quality of life independent from somatic complaints. In our study, we detected that there was a decrease in physical and mental quality of life in BTM patients with depressive symptoms. Moreover, both physical and mental quality of life decreased in BTM patients with anxiety symptoms. In regression analysis, it was seen that physical and mental quality of life was influenced from presence of depression but not anxiety in BTM patients.
We have found, similarly, a significant impairment in caregivers of β-thalassaemic children in terms of physical health (concerning energy and fatigue, pain and discomfort, sleep and rest subscales), psychological health (bodily image and appearance, feelings, self-esteem, thinking, learning, memory and concentration subscales) and domains assessing overall QoL. Poor QoL of caregivers could be explained by a sense of guilt for having generated a child with a genetically determined disease.
An additional goal of the present study was to evaluate QoL of caregivers and effects of depression and anxiety on QoL. In caregivers of children the quality of life was found low on all subscales. Physical and mental components of QoL was both decreased in the caregivers with depression symptoms and anxiety symptoms. However, it was found that physical and psychological QoL was influenced from depression independent from anxiety. Clinical manifestations usually develop early in the life and continuous desferoxamine infusions, local reactions, health care costs leads maladaptive coping strategies and high levels of anxiety with psychosocial dysfunction in caregivers [26,27].
In conclusion, BTM leads an increase in the frequency of depression and anxiety in both patients and their caregivers. This increase results in negative effects on physical and mental quality of life in patients and their caregivers. In particular, depression plays role in these negative effects independently from anxiety.
Patients with BTM expose to intensive and serious medical therapies and their complications lifelong. Thus, psychological status of these patients has important effects on their quality of life.
Disclosure of conflict of interest
None.
References
- 1.Aydinok Y. Thalassemia. Hematology. 2012;17(Suppl 1):S28–31. doi: 10.1179/102453312X13336169155295. [DOI] [PubMed] [Google Scholar]
- 2.Savas N, Turhan E, Inandi T, Kaya H. Hemoglobinopathy awareness among high school students in Antakya (Antioch), Turkey. Int J Hematol. 2010;91:413–418. doi: 10.1007/s12185-010-0539-3. [DOI] [PubMed] [Google Scholar]
- 3.Canatan D, Kose MR, Ustundag M, Haznedaroglu D, Ozbas S. Hemoglobinopathy control program in Turkey. Community Genet. 2006;9:124–126. doi: 10.1159/000091493. [DOI] [PubMed] [Google Scholar]
- 4.Keskek SO, Kirim S, Turhan A, Turhan FG. Depression in subjects with beta-thalassemia minor. Ann Hematol. 2013;92:1611–1615. doi: 10.1007/s00277-013-1851-9. [DOI] [PubMed] [Google Scholar]
- 5.Messina G, Colombo E, Cassinerio E, Ferri F, Curti R, Altamura C, Cappellini MD. Psychosocial aspects and psychiatric disorders in young adult with thalassemia major. Intern Emerg Med. 2008;3:339–343. doi: 10.1007/s11739-008-0166-7. [DOI] [PubMed] [Google Scholar]
- 6.Pradhan PV, Shah H, Rao P, Ashturkar D, Ghaisas P. Psychopathology and self-esteem in chronic illness. Indian J Pediatr. 2003;70:135–138. doi: 10.1007/BF02723739. [DOI] [PubMed] [Google Scholar]
- 7.Yellowlees PM, Kalucy RS. Psychobiological aspects of asthma and the consequent research implications. Chest. 1990;97:628–634. doi: 10.1378/chest.97.3.628. [DOI] [PubMed] [Google Scholar]
- 8.Telfer P, Constantinidou G, Andreou P, Christou S, Modell B, Angastiniotis M. Quality of life in thalassemia. Ann N Y Acad Sci. 2005;1054:273–282. doi: 10.1196/annals.1345.035. [DOI] [PubMed] [Google Scholar]
- 9.Aydinok Y, Erermis S, Bukusoglu N, Yilmaz D, Solak U. Psychosocial implications of Thalassemia Major. Pediatr Int. 2005;47:84–89. doi: 10.1111/j.1442-200x.2004.02009.x. [DOI] [PubMed] [Google Scholar]
- 10.Ghanizadeh A, Khajavian S, Ashkani H. Prevalence of psychiatric disorders, depression, and suicidal behavior in child and adolescent with thalassemia major. J Pediatr Hematol Oncol. 2006;28:781–784. doi: 10.1097/01.mph.0000243665.79303.9e. [DOI] [PubMed] [Google Scholar]
- 11.Aydin B, Yaprak I, Akarsu D, Okten N, Ulgen M. Psychosocial aspects and psychiatric disorders in children with thalassemia major. Acta Paediatr Jpn. 1997;39:354–357. doi: 10.1111/j.1442-200x.1997.tb03752.x. [DOI] [PubMed] [Google Scholar]
- 12.Mikelli A, Tsiantis J. Brief report: Depressive symptoms and quality of life in adolescents with b-thalassaemia. J Adolesc. 2004;27:213–216. doi: 10.1016/j.adolescence.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Aziz K, Sadaf B, Kanwal S. Psychosocial problems of Pakistani parents of Thalassemic children: a cross sectional study done in Bahawalpur, Pakistan. Biopsychosoc Med. 2012;6:15. doi: 10.1186/1751-0759-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsiantis J, Dragonas T, Richardson C, Anastasopoulos D, Masera G, Spinetta J. Psychosocial problems and adjustment of children with beta-thalassemia and their families. Eur Child Adolesc Psychiatry. 1996;5:193–203. doi: 10.1007/BF00538846. [DOI] [PubMed] [Google Scholar]
- 15.Sharghi A, Karbakhsh M, Nabaei B, Meysamie A, Farrokhi A. Depression in mothers of children with thalassemia or blood malignancies: a study from Iran. Clin Pract Epidemiol Ment Health. 2006;2:27. doi: 10.1186/1745-0179-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 17.Koçyiğit H, Aydemir Ö, Ölmez N, Memiş A. Kısa form 36’nın (KF-36) Türkçe versiyonunun güvenilirliği ve geçerliliği. İlaç ve Tedavi Dergisi. 1999;12:102–106. [Google Scholar]
- 18.Demiral Y, Ergör G, Ünal B, et al. Sağlıkta yaşam kalitesi sempozyumu özet kitabı. İzmir: Emek matbaası; 2004. SF-36 yaşam kalitesi ölçeğinin genel toplum örneğinde güvenilirliği. [Google Scholar]
- 19.Ulusoy M, Şahin NH, Erkmen H. Turkish version of the Beck Anxiety Inventory: Psychometric properties. Journal of Cognitive Psychotheraphy. 1998;12:163–172. [Google Scholar]
- 20.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 21.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 22.Cakaloz B, Cakaloz I, Polat A, Inan M, Oguzhanoglu NK. Psychopathology in thalassemia major. Pediatr Int. 2009;51:825–828. doi: 10.1111/j.1442-200X.2009.02865.x. [DOI] [PubMed] [Google Scholar]
- 23.Gollo G, Savioli G, Balocco M, Venturino C, Boeri E, Costantini M, Forni GL. Changes in the quality of life of people with thalassemia major between 2001 and 2009. Patient Prefer Adherence. 2013;7:231–236. doi: 10.2147/PPA.S42133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hajibeigi B, Azarkeyvan A, Alavian SM, Lankarani MM, Assari S. Anxiety and depression affects life and sleep quality in adults with beta-thalassemia. Indian J Hematol Blood Transfus. 2009;25:59–65. doi: 10.1007/s12288-009-0015-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azarkeivan A, Hajibeigi B, Alavian SM, Lankarani MM, Assari S. Associates of poor physical and mental health-related quality of life in beta thalassemia-major/intermedia. J Res Med Sci. 2009;14:349–355. [PMC free article] [PubMed] [Google Scholar]
- 26.Canatan D, Ratip S, Kaptan S, Cosan R. Psychosocial burden of beta-thalassaemia major in Antalya, south Turkey. Soc Sci Med. 2003;56:815–819. doi: 10.1016/s0277-9536(02)00080-1. [DOI] [PubMed] [Google Scholar]
- 27.Kuo HT, Tsai MY, Peng CT, Wu KH. Pilot study on the “quality of life” as reflected by psychosocial adjustment of children with thalassemia major undergoing iron-chelating treatment in western Taiwan. Hemoglobin. 2006;30:291–299. doi: 10.1080/03630260600642641. [DOI] [PubMed] [Google Scholar]


