Abstract
Background: The relationship between ABO blood group and clinical characteristics had been studied in several cancers. However, its role in esophageal cancer (EC) is unclear. The aim of this study was to determine whether ABO blood group is associated with overall survival in patients with esophageal squamous cell carcinoma (ESCC). Methods: From 2005 to 2008, a retrospective analysis of 496 consecutive patients with ESCC was conducted. The relationship between ABO blood group and clinicopathologic features of ESCC was analyzed. Prognostic factors for overall survival of ESCC were also analyzed. Results: The 5-year overall survival of ESCC patients with blood group A, B, AB and O were 47.8%, 44.1%, 43.2%, and 38.4%, respectively (P = 0.165). However, patients with blood group non-O have a better 5-year overall survival than patients with blood group O (45.7% vs. 38.4%; P = 0.043). Multivariate analyses showed ABO blood group (O vs. non-O; P = 0.034) is an independent prognostic factors. Conclusions: ABO blood group is associated with overall survival in patients with ESCC. We concluded that patients with blood group O have a significantly worse overall survival than non-O blood groups.
Keywords: Esophageal cancer, squamous cell carcinoma, ABO blood group, esophagectomy, prognostic factor, overall survival
Introduction
Esophageal cancer (EC) is the eighth most common cancer and the sixth leading death worldwide [1]. The estimated overall incidence rate (standardized for world population) was 5.7/100,000 in 2008 [1]. In China, however, the incidence was 20.9/100,000 in 2008 [2]. Thus, China still suffers a great disease burden from EC.
Over the past few decades, various prognostic factors for EC have been identified, including lymph node metastasis, depth of tumor invasion, and other miscellaneous factors [3,4]. Since the association between blood group A and gastric cancer was reported by Aird et al. [5] in 1953, the relationship between ABO blood group and clinicopathologic characteristics had been studied in many cancers [6-8]. However, its role in EC is unclear. Esophageal squamous cell carcinoma (ESCC) accounts for the most common pathological type of EC in China, in contrast to the predominance of adenocarcinoma in the Western world. The aim of this study was to determine whether ABO blood group is associated with overall survival in ESCC.
Patients and methods
A retrospective analysis was conducted of 496 patients with ESCC who underwent radical esophagectomy in our hospital from January 2005 to December 2008. All of the patients were confirmed by histopathology. All of the patients were treated with radical esophagectomy. The standard surgical approach included the Ivor Lewis and McKeown procedure. The lymph node dissection included two-field and three-field lymphadenectomy. The most frequent postoperative chemotherapy included 5-fluorouracil and cisplatin. Postoperative radiation was initially performed through the anteroposterior field to 36 Gy, then through the parallel opposing oblique fields to 14 Gy, in order to avoid the spinal cord. Ethical approval was obtained from The Ethical Committees of Zhejiang Cancer Hospital.
Based on the medical records, the clinical characteristics were collected for each patient, such as age, gender, tumor location, tumor length, differentiation, ABO blood group, T grade, N staging and other miscellaneous characteristics. In our institute, the surviving patients were followed up in our outpatient department every 3 to 6 months for the first 2 years, then annually. X-ray and computed tomography of the chest were performed during the follow-up. The last follow-up time was Nov. 2011.
Statistical analysis
Statistical evaluation was conducted with SPSS 17.0 (SPSS Inc., Chicago, IL, USA). The relationship between ABO blood group and clinicopathological variables was assessed using chi-squared test. The overall survival was calculated by the Kaplan-Meier method, and the difference was assessed by the log-rank test. Univariate and multivariate analyses of Cox regression proportional hazard model were performed to evaluate the prognostic parameters for survival. A P value less than 0.05 was considered to be statistically significant.
Results
In our study, there were 185 (37.3%) patients with blood group O, 138 (27.8%) with A, 136 (27.4%) with B and 37 (7.5%) with AB. However, no relationship was found between ABO blood groups and clinicopathologic characteristics (Table 1).
Table 1.
The characteristics of patients with different ABO blood groups
| O (n=185) | A (n=138) | B (n=136) | AB (n=37) | P-value | |
|---|---|---|---|---|---|
| Age (years) | 0.991 | ||||
| ≤ 60 | 105 | 76 | 77 | 21 | |
| > 60 | 80 | 62 | 59 | 16 | |
| Gender | 0.700 | ||||
| Female | 24 | 19 | 23 | 4 | |
| Male | 161 | 119 | 113 | 33 | |
| Tumor length (cm) | 0.936 | ||||
| ≤ 3 | 54 | 40 | 37 | 12 | |
| > 3 | 131 | 98 | 99 | 25 | |
| Tumor location | 0.946 | ||||
| Upper | 7 | 6 | 8 | 2 | |
| Middle | 93 | 69 | 66 | 21 | |
| Lower | 85 | 63 | 62 | 14 | |
| Differentiation | 0.575 | ||||
| Well | 29 | 23 | 18 | 3 | |
| Moderate | 127 | 88 | 95 | 24 | |
| Poor | 29 | 27 | 23 | 10 | |
| Vessel involvement | 0.713 | ||||
| Negative | 152 | 117 | 108 | 30 | |
| Positive | 33 | 21 | 28 | 7 | |
| T grade | 0.629 | ||||
| T1 | 37 | 28 | 21 | 5 | |
| T2 | 28 | 25 | 21 | 6 | |
| T3 | 98 | 78 | 78 | 22 | |
| T4a | 22 | 7 | 16 | 4 | |
| N staging | 0.525 | ||||
| N0 | 104 | 86 | 70 | 23 | |
| N1 | 47 | 28 | 43 | 8 | |
| N2 | 23 | 16 | 11 | 4 | |
| N3 | 11 | 8 | 12 | 2 | |
| Adjuvant therapy | 0.887 | ||||
| No | 134 | 100 | 98 | 29 | |
| Yes | 51 | 38 | 38 | 8 |
Univariate analyses showed that tumor length (P < 0.001), vessel involvement (P = 0.004), differentiation (P = 0.021), ABO blood group (P = 0.043), T grade (P < 0.001) and N staging (P < 0.001) were predictive of survival (Table 2). Then multivariate analyses were performed with the Cox proportional hazards model. In that model, we demonstrated that ABO blood group (O vs. non-O; P = 0.034) is an independent prognostic factors (Table 3).
Table 2.
Univariate analyses in patients with ESCC
| Cases (n, %) | OS (%) | HR (95% CI) | P-value | |
|---|---|---|---|---|
| Age (years) | 0.453 | |||
| ≤ 60 | 279 (56.3) | 44.4 | 1.000 | |
| > 60 | 217 (43.7) | 41.0 | 1.093 (0.865-1.381) | |
| Gender | 0.079 | |||
| Female | 70 (14.1) | 51.4 | 1.000 | |
| Male | 426 (85.9) | 41.5 | 1.373 (0.959-1.965) | |
| Tumor length (cm) | < 0.001 | |||
| ≤ 3 | 143 (28.8) | 61.5 | 1.000 | |
| > 3 | 353 (71.2) | 35.4 | 2.056 (1.531-2.761) | |
| Tumor location | 0.249 | |||
| Upper/Middle | 272 (54.8) | 46.3 | 1.000 | |
| Lower | 224 (45.2) | 38.8 | 1.146 (0.907-1.447) | |
| Vessel involvement | 0.004 | |||
| Negative | 407 (82.2) | 45.7 | 1.000 | |
| Positive | 89 (17.8) | 30.3 | 1.415 (1.067-1.876) | |
| Differentiation | 0.021 | |||
| Well/Moderate | 407 (82.2) | 44.5 | 1.000 | |
| Poor | 89 (17.8) | 36.0 | 1.403 (1.049-1.878) | |
| ABO blood group | 0.043 | |||
| Non-O group | 311 (62.7) | 45.7 | 1.000 | |
| O group | 185 (37.3) | 38.4 | 1.275 (1.005-1.617) | |
| T grade | < 0.001 | |||
| T1-2 | 173 (34.9) | 61.3 | 1.000 | |
| T3-4a | 323 (65.1) | 33.1 | 2.135 (1.623-2.810) | |
| N staging | < 0.001 | |||
| N0 | 283 (57.6) | 61.1 | 1.000 | |
| N1-3 | 213 (42.4) | 18.8 | 2.965 (2.331-3.772) | |
| Adjuvant therapy | 0.097 | |||
| No | 361 (72.8) | 45.7 | 1.000 | |
| Yes | 135 (27.2) | 35.6 | 1.236 (0.960-1.591) |
ESCC, esophageal squamous cell carcinoma; OS, overall survival; HR, hazard ratio; CI, confidence interval.
Table 3.
Multivariate analyses in patients with ESCC
| HR (95% CI) | P-value | |
|---|---|---|
| Tumor length (> 3 cm vs. ≤ 3 cm) | 1.372 (0.991-1.900) | 0.057 |
| Vessel involvement (Positive vs. Negative) | 1.056 (0.790-1.412) | 0.713 |
| Differentiation (Poor vs. Well/Moderate) | 1.430 (1.065-1.919) | 0.017 |
| ABO blood group (O vs. Non-O) | 1.293 (1.019-1.640) | 0.034 |
| T grade (T3-4a vs. T1-2) | 1.421 (1.041-1.940) | 0.027 |
| N staging (N1-3 vs. N0) | 2.453 (1.890-3.184) | < 0.001 |
ESCC, esophageal squamous cell carcinoma; HR, hazard ratio; CI, confidence interval.
The 5-year overall survival was 42.9% in our study. The 5-year overall survival of patients with blood group A, B, AB and O were 47.8%, 44.1%, 43.2%, and 38.4%, respectively (P = 0.165; Figure 1). However, patients with blood group non-O have a better 5-year overall survival than patients with blood group O (45.7% vs. 38.4%; P = 0.043) (Figure 2).
Figure 1.
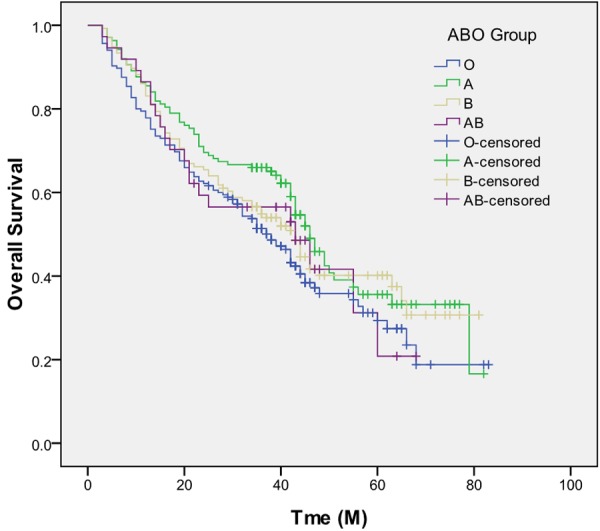
Kaplan-Meier curves of overall survival in patients with different ABO blood groups (P = 0.165).
Figure 2.
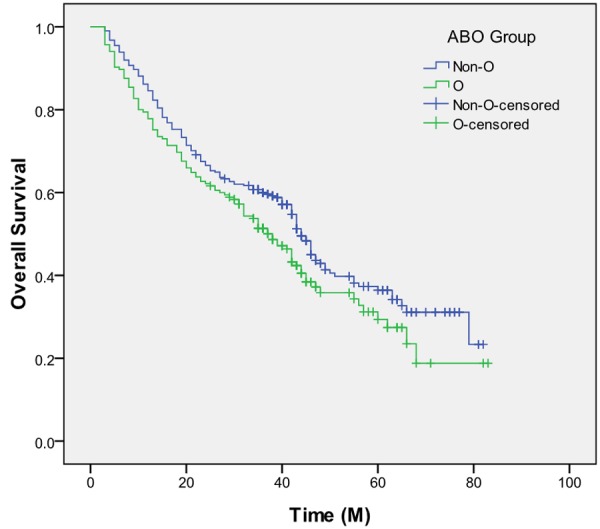
Kaplan-Meier curves of overall survival between patients with blood group O and blood group non-O (P = 0.043).
Discussion
To our knowledge, this may be the first study to determine the prognostic value of ABO blood group in ESCC. Our results showed that ABO blood group is a predictive factor for long-term overall survival in ESCC. Specifically, in our study, we identified blood group O as a potential predictor of mortality in ESCC patients. Patients with blood group O had a 29.3% increased mortality risk compared with those with blood group non-O (P = 0.034).
Possible associations between ABO blood group and the risk of some epithelial malignancies, including pancreatic cancer, colorectal cancer and gastric cancer have been reported [5,6,8]. However, there is little information available regarding the relationship between ABO blood group and clinicopathologic characteristics of EC. In our study, type O was the most common (37.3%) blood group. This observation is in line with data from Su et al. [9], but is contrary to the result of Nozoe et al. [10], who demonstrated that type A was the most common (46.1%) blood group. Nozoe et al. [10] also showed that the proportion of poorly differentiated ESCC among patients with blood group O was significantly lower than in those patients with other blood types (P = 0.001). However, no relationship was found between ABO blood groups and clinicopathologic characteristics in our study (Table 2).
In our study, the 5-year overall survival of patients with blood group A, B, AB and O were 47.8%, 44.1%, 43.2%, and 38.4%, respectively (P = 0.165). However, patients with blood group non-O have a better 5-year overall survival than patients with blood group O (45.7% vs. 38.4%). Then multivariate analyses demonstrated that ABO blood group is independently associated with overall survival in patients undergoing esophagectomy for ESCC (P = 0.034). However, Nozoe et al. [10] showed that there was not any significant difference between ABO blood group and survival.
However, environmental, geographic and racial concerns can never be neglected in discussing correlations of ABO blood group with cancer [11]. The proportion of patients with each blood group was roughly concomitant with the ABO blood group distribution in our study, however, a correlation of ABO blood group with a predisposition to tumorigenesis and prognosis of ESCC can’t be inferred. Our study showed patients with blood group non-O have a better 5-year overall survival than patients with blood group O (45.7% vs. 38.4%).
In conclusion, ABO blood group is independently associated with overall survival in patients undergoing esophagectomy for ESCC. We concluded that patients with blood group O have significantly worse overall survival than non-O blood groups.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2897. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Cancer Registration Annual Report 2011. Beijing: Military Medical Sciences; 2012. National Cancer Center. [Google Scholar]
- 3.Peyre CG, Hagen JA, DeMeester SR, Altorki NK, Ancona E, Griffin SM, Hölscher A, Lerut T, Law S, Rice TW, Ruol A, van Lanschot JJ, Wong J, DeMeester TR. The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. Ann Surg. 2008;248:549–556. doi: 10.1097/SLA.0b013e318188c474. [DOI] [PubMed] [Google Scholar]
- 4.Wijnhoven BP, Tran KT, Esterman A, Watson DI, Tilanus HW. An evaluation of prognostic factors and tumor staging of resected carcinoma of the esophagus. Ann Surg. 2007;245:717–725. doi: 10.1097/01.sla.0000251703.35919.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aird I, Bentall HH, Roberts JA. A relationship between cancer of the stomach and the ABO blood groups. Br Med J. 1953;1:799–801. doi: 10.1136/bmj.1.4814.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolpin BM, Chan AT, Hartge P, Chanock SJ, Kraft P, Hunter DJ, Giovannucci EL, Fuchs CS. ABO blood group and the risk of pancreatic cancer. J Natl Cancer Inst. 2009;101:424–431. doi: 10.1093/jnci/djp020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engin H, Bilir C, Üstün H, Gökmen A. ABO blood group and risk of pancreatic cancer in a Turkish population in Western Blacksea region. Asian Pac J Cancer Prev. 2012;13:131–133. [PubMed] [Google Scholar]
- 8.Urun Y, Ozdemir NY, Utkan G, Akbulut H, Savas B, Oksuzoglu B, Oztuna DG, Dogan I, Yalcin B, Senler FC, Onur H, Demirkazik A, Zengin N, Icli F. ABO and Rh Blood Groups and Risk of Colorectal Adenocarcinoma. Asian Pac J Cancer Prev. 2012;13:6097–6100. doi: 10.7314/apjcp.2012.13.12.6097. [DOI] [PubMed] [Google Scholar]
- 9.Su M, Lu SM, Tian DP, Zhao H, Li XY, Li DR, Zheng ZC. Relationship between ABO blood groups and carcinoma of esophagus and cardia in Chaoshan inhabitants of China. World J Gastroenterol. 2001;7:657–661. doi: 10.3748/wjg.v7.i5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nozoe T, Ezaki T, Baba H, Kakeji Y, Maehara Y. Correlation of ABO blood group with clinicopathologic characteristics of patients with esophageal squamous cell carcinoma. Dis Esophagus. 2004;17:146–149. doi: 10.1111/j.1442-2050.2004.00392.x. [DOI] [PubMed] [Google Scholar]
- 11.Iodice S, Maisonneuve P, Botteri E, Sandri MT, Lowenfels AB. ABO blood group and cancer. Eur J Cancer. 2010;46:3345–3350. doi: 10.1016/j.ejca.2010.08.009. [DOI] [PubMed] [Google Scholar]


