Abstract
Introduction: Managing ventilation and oxygenation during laparoscopic procedures in severely obese patients undergoing weight loss surgery presents many challenges. Pressure-controlled ventilation, volume-guaranteed (PCV-VG) is a dual-control mode of ventilation and an alternative to pressure (PC) or volume (VC) controlled ventilation. PCV-VG features a user-selected tidal volume target, that is auto-regulated and pressure controlled. We hypothesized that PCV-VG ventilation would provide improved oxygenation and ventilation during laparoscopic bariatric surgery with a lower peak inflating pressure (PIP) than either PC or VC ventilation. Methods: This was a prospective cross-over cohort trial (n = 20). In random sequence each patient received the three modes of ventilation for 20 minutes during the laparoscopic portion of the procedure. For all modes of ventilation the goal tidal volume was 6-8 mL/kg, and the respiratory rate was adjusted to achieve normocarbia. The PIP, exhaled tidal volume, respiratory rate, and oxygen saturation were recorded every five minutes. At the end of 20 minutes, an arterial blood gas was obtained. Data were analyzed using a paired t-test. Results: PCV-VG and PC ventilation both resulted in significantly lower PIP (cmH2O) than VC ventilation (30.5 ± 3.0, 31.6 ± 4.9, and 36.3 ± 3.4 mmHg respectively; p < 0.01 for PCV-VG vs. VC and PC vs. VC). There was no difference in oxygenation (PaO2), ventilation (PaCO2) or hemodynamic variables between the three ventilation modes. Conclusions: In adolescents and young adults undergoing laparoscopic bariatric surgery, PCV-VG and PC were superior to VC ventilation in their ability to provide ventilation with the lowest PIP.
Keywords: Bariatric surgery, obesity, adolescent, ventilation, arterial blood gas analysis
Introduction
Up to 6% of children in the United States are severely obese, defined as an absolute body mass index (BMI) > 35 kg/m2 or > 20th percent of the 95th percentile [1]. In response to disappointing results associated with lifestyle interventions (i.e. diet, exercise and behavior modification), a mounting body of evidence has demonstrated the safe and efficacious application of surgical weight reduction procedures in the adolescent and young adult populations [1,2]. Managing ventilation and oxygenation to avoid hypoxemia, hypercarbia, and barotrauma is challenging in the severely obese population. Changes in functional residual capacity and closing volumes in the supine and anesthetized state lead to ventilation-perfusion inequalities and hypoxemia. Commonly suggested techniques to compensate for the physiologic changes of obesity include using positive end expiratory pressure (PEEP) during controlled ventilation, recruitment maneuvers, equal ratio ventilation, and reverse Trendelenburg positioning as possible [3-7]. In addition, many bariatric surgeries are completed using minimally invasive or laparoscopic techniques, which may further impact the physiologic derangements of respiratory function and further magnify ventilation-perfusion inequalities. In particular, intra-abdominal insufflation and the subsequent increase in intra-abdominal pressure reduce functional residual capacity as well alter resistance and compliance [8-10]. The resultant hypoxemia and hypercarbia may require further increases in minute ventilation and PIP to compensate for the increased resistance and decreased compliance.
Both pressure-controlled (PC) and volume-controlled (VC) ventilation strategies have been suggested to manage the severely obese adult undergoing laparoscopic procedures [11-15]. Pressure-controlled ventilation, volume-guaranteed (PCV-VG) is a dual-control mode of ventilation and an alternative to PC or VC ventilation that has recently been introduced into the operating room. PCV-VG features a user-selected tidal volume target, that is auto-regulated and pressure controlled. The ventilator adjusts the pressure limit of the next breath based on the previous breath’s measured exhaled tidal volume and has a pre-determined high pressure limit to avoid barotrauma. PCV-VG may thus achieve the desired tidal volume with the lowest peak inspiratory pressure (PIP). To date, there are no prospective trials in the pediatric population evaluating this mode of ventilation. We hypothesized that the PCV-VG mode of ventilation would provide improved oxygenation and ventilation during laparoscopic bariatric surgery with a lower PIP than either pressure or volume limited modes of ventilation.
Methods
Approval for this study was granted by The Institutional Review Board of Nationwide Children’s Hospital (Columbus, Ohio). The study was registered at clinicaltrials.gov (NCT01890564). Severely obese (BMI ≥ 40 kg/m2) adolescents and young adults presenting for laparoscopic-assisted bariatric surgery were eligible. The need for written, informed consent was waived. This prospective, cross-over cohort trial evaluated the effects of three modes of ventilation (PC, VC and PCV-VG) on PIP, ventilation and oxygenation, as well as hemodynamic variables during laparoscopic vertical sleeve gastrectomy in twenty consecutive patients.
Anesthetic monitoring included American Society of Anesthesiologists’ specific monitors. As part of our standard practice for these procedures, an arterial cannula was placed after anesthetic induction. Premedication with 2 mg of intravenous midazolam preceded an intravenous induction with propofol (2-3 mg/kg) and fentanyl (2-3 µg/kg). Endotracheal intubation was facilitated by the administration of either rocuronium or succinylcholine. Maintenance of anesthesia included dexmedetomidine up to 0.3 µg/kg/hour, desflurane titrated to maintain the bispectral index (BIS, Philips Healthcare, Andover MA, USA) at 40 to 60, and remifentanil titrated from 0.05-0.3 µg/kg/min to maintain hemodynamic stability. Postoperative analgesia was provided by intravenous hydromorphone and acetaminophen. Prophylaxis for postoperative nausea and vomiting included the preoperative placement of a scopolamine patch and the intraoperative administration of ondansetron (4 mg) and dexamethasone (4 mg).
In a random order, each patient received the 3 modes of ventilation (VC, PC and PCV-VG) using a Datex-Ohmeda Avance Anesthesia Machine (GE Healthcare, Madison WI USA) for 20 minutes during the laparoscopic portion of the procedure. Standard patient positioning during the procedure and data collection included 15-30° reverse Trendelenburg position. For all modes of ventilation, the inspired oxygen concentration was held at 0.5 with a positive end expiratory pressure (PEEP) of 5 cmH2O. The respiratory rate was adjusted to achieve normocarbia and the inspiratory time was set at 1.5 seconds. The goal exhaled tidal volume in all three modes of ventilation was 6-8 mL/kg. VC and PCV-VG ventilation were provided with a set tidal volume of 6-8 mL/kg. PC ventilation was provided with the PIP adjusted to deliver a tidal volume of 6-8 mL/kg. If the desired tidal volume could not be achieved with a set inspiratory time of 1.5 seconds and a PIP ≤ 40 cmH2O, the inspiratory time was lengthened. If this was not successful in lowering the PIP with an I: E ratio of 1: 1, that mode of ventilation was terminated and the next mode was initiated. During the 20 minute study period for each mode of ventilation, the PIP, exhaled tidal volume, respiratory rate, and oxygen saturation were recorded every five minutes. At the end of 20 minutes, an arterial blood gas was obtained. In addition to respiratory rate, the end-tidal desflurane concentration, BIS value, remifentanil infusion rate, heart rate, and blood pressure (systolic, diastolic, and mean) were recorded every five minutes. Data were analyzed using paired t-tests.
Results
The study cohort included twenty severely obese adolescents (17 females) with a mean age of 17.2 ± 2.3 years and BMI of 49.3 kg/m2. The demographic data are listed in Table 1. Table 2 summarizes the parameters of airway pressure, exhaled tidal volume, respiratory rate, ventilation and oxygenation by ventilation mode. Both the PCV-VG and PC modes of ventilation resulted in a significantly lower PIP (cmH2O) than VC ventilation (30.6 ± 3.4, 31.6 ± 5.5, and 36.5 ± 5.0 cmH2O respectively; p < 0.001 for PCV-VG vs. VC and p < 0.01 for PC vs. VC, Figure 1). No significant difference was found between the PIP for PCV-VG and PC ventilation. In one patient, the VC mode was abandoned since despite adjustments of the inspiratory time, the PIP was greater than 40 cmH2O. In four other patients during VC ventilation, adjustments in the inspiratory time were needed to deliver the tidal volume with a PIP ≤ 40 cmH2O. No patient failed ventilation with PC or PCV-VG ventilation modes. During all other modes of ventilation and in all other patients, the inspiratory time was maintained at approximately 1.5 seconds. There was no significant difference between the three ventilation modes when comparing the PaCO2, PaO2, and pH (Table 2). Likewise, there was no significant difference in the hemodynamic parameters (HR and blood pressure), bispectral index, remifentanil infusion rate, or end-tidal desflurane concentration between the three groups (Tables 3 and 4).
Table 1.
Demographic data of the study cohort
| Age (Years) | 17.2 ± 2.3 |
| Weight (kg) | 128.8 ± 26 |
| Body Mass Index (BMI) (kg/m2) | 49.3 ± 9.3 |
| Gender (male-female) | 3-17 |
The data are listed as the mean ± SD.
Table 2.
Arterial blood gas and ventilation parameters by mode of ventilation
| Mode of Ventilation | VC | PC | PCV-VG |
|---|---|---|---|
| PIP (cmH2O) | 36.5 ± 5.0 | 31.6 ± 5.5+ | 30.6 ± 3.4* |
| PaO2 (mmHg) | 161 ± 45 | 169 ± 47 | 166 ± 52 |
| pH | 7.32 ± 0.04 | 7.33 ± 0.05 | 7.34 ± 0.03 |
| PaCO2 (mmHg) | 40.9 ± 3.3 | 40.2 ± 3.7 | 38.8 ± 4.1 |
| Respiratory rate (breaths/minute) | 9.2 ± 2.1 | 9.4 ± 2.2 | 9.2 ± 2.1 |
| Exhaled tidal volume (mL) | 760 ± 124 | 737 ± 135 | 750 ± 121 |
VC = volume-controlled; PC = pressure-controlled; PCV-VG = pressure-controlled ventilation, volume guaranteed. The data are listed as the mean ± SD.
p < 0.001 for PCV-VG vs. VC;
p < 0.01 for PC vs. VC.
Figure 1.
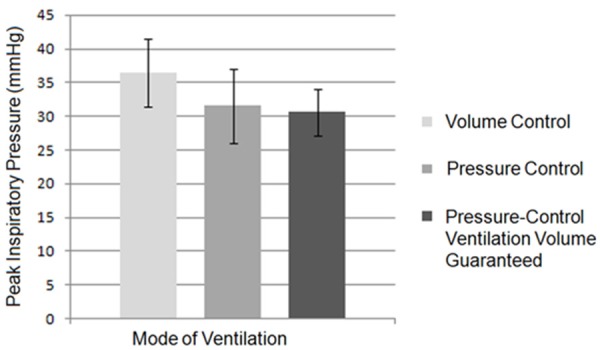
Mean peak inspiratory pressures by ventilation mode. Peak inspiratory pressure (mmHg) dependent on the type of ventilation. The peak inspiratory pressure was significantly less during pressure control and pressure-control ventilation, volume guaranteed when compared to volume control ventilation.
Table 3.
Hemodynamic parameters by mode of ventilation
| Hemodynamic variable | VC | PC | PCV-VG |
|---|---|---|---|
| Heart rate (beats/minute) | 77 ± 10 | 73 ± 11 | 71 ± 11 |
| Systolic blood pressure (mmHg) | 99 ± 10 | 98 ± 11 | 96 ± 16 |
| Diastolic blood pressure (mmHg) | 62 ± 8 | 60 ± 11 | 59 ± 11 |
| Mean arterial pressure (mmHg) | 74 ± 8 | 72 ± 10 | 70 ± 11 |
VC = volume-controlled; PC = pressure-controlled; PCV-VG = pressure-controlled ventilation, volume guaranteed. The data are listed as the mean ± SD. For the hemodynamic variables, the value at each 5 minute interval was averaged to provide a single data point for each patient. P = NS for all variables and each mode of ventilation.
Table 4.
Anesthetic variables by mode of ventilation
| Anesthetic variable | VC | PC | PCV-VG |
|---|---|---|---|
| BIS Value (0-100) | 48 ± 8 | 47 ± 7 | 46 ± 6 |
| Remifentanil infusion rate (mcg/kg/minute) | 0.13 ± 0.06 | 0.14 ± 0.06 | 0.12 ± 0.05 |
| End-tidal desflurane concentration (%) | 4.1 ± 1.0 | 4.2 ± 0.8 | 4.2 ± 0.9 |
VC = volume-controlled; PC = pressure-controlled; PCV-VG = pressure-controlled ventilation, volume guaranteed. The data are listed as the mean ± SD. For the anesthetic variables, the value at each 5 minute interval was averaged to provide a single data point for each patient. P = NS for all variables and each mode of ventilation.
Discussion
The current study demonstrates a beneficial role for pressure-mediated ventilation (PC or PCV-VG) strategies in morbidly obese adolescents and young adults undergoing laparascopic-assisted weight loss surgery. Most importantly, we found that VC ventilation could not be accomplished in one patient within the pre-set PIP limit of the study protocol (PIP ≤ 40 cmH2O). Despite these findings, we noted no change in oxygenation or ventilation between the groups. Additionally, a similar hemodynamic and anesthetic profile was noted in the groups. In a patient population where high airway pressures and barotrauma are of particular concern, pressure-mediated ventilation appears to mitigate the degree of raised PIP and may minimize potential barotrauma while providing effective ventilation and oxygenation.
Similar studies comparing ventilation modes in obese adults undergoing laparoscopic procedures have found varying results. Neither pressure nor volume controlled ventilation resulted in lower PIP in several studies [12,13,15]. However, others have noted that similar to our findings, pressure-controlled ventilation was able to significantly reduce PIP in obese adults undergoing during intra-abdominal procedures [11]. Pressure mediated ventilation (PC and PCV-VG ventilation) modes provide a decelerating inspiratory flow and constant inspiratory pressure to the alveoli in the lungs thereby improving ventilation to alveoli with varying time constants related to altered resistance and compliance. The alveolar units in the lungs of morbidly obese adolescents undergoing laparoscopy may be heterogeneous, in varied stages of inflation with variable time constants. These physiologic changes may be further magnified by supine position, reverse Trendelenburg position, and the administration of intravenous and inhalational general anesthetic agents. Under these circumstances, pressure mediated ventilation may inflate the atelectatic alveoli without causing barotrauma to those prone to over-inflation more effectively than volume controlled ventilation.
A recent review by Aldenkortt and colleagues assessed 13 studies that included more than 500 patients comparing volume and pressure controlled ventilation in obese adults [15]. This group found no difference in airway pressures or measures of oxygenation or ventilation between pressure or volume controlled ventilation [15]. This meta-analysis suggests that there is no advantage in obese adults of VC or PC modes of ventilation to minimize PIP or improve oxygenation or ventilation. However, given the findings of our study, we would postulate that the beneficial effects of pressure mediated ventilation could potentially be more pronounced in obese adolescents and young adults when compared to older adults. Without the usual changes associated with aging including loss of elastic tissue within the lungs, the adolescent lungs may be generally healthier than those of adults. Furthermore, none of our patients were tobacco users, another significant co-morbid condition noted in the adult population. Without intrinsic restrictive or obstructive disease, the physiological benefits of pressure mediated ventilation, used with PEEP (as in our study), may become apparent. In diseased lungs, additional factors may complicate alveolar physiology and the ability of pressure ventilation to overcome the isolated effects of obesity may be lost.
Although our study found no difference between the PCV-VG and PC ventilation modes, our clinical experience has demonstrated that PCV-VG is an easier mode of ventilation to manage during conditions of changing respiratory compliance and resistance such as may occur during laparoscopic procedures where abrupt changes in intra-abdominal pressure may occur. Changes in depth of anesthesia and muscle relaxation as well as surgical manipulations have the potential to substantially alter both compliance and resistance. With the PC ventilation, when tidal volume is dependent on the resistance and compliance, this may result in wide fluctuations of the tidal volume. This may require frequent alterations in the PIP to ensure appropriate ventilation. PCV-VG will accommodate to changes in compliance and resistance automatically, resulting in a constant tidal volume.
Neither pressure nor volume limited modes of ventilation resulted in any superiority for improving ventilation or oxygenation in obese adolescents in this study. Varying results have been reported in obese adults during intraoperative mechanical ventilation. Volume controlled ventilation has been found to provide superior ventilation with lower PaCO2 values than pressure controlled ventilation [12]. Pressure controlled ventilation has been found to improve oxygenation (PaO2) when compared to volume controlled ventilation [13]. Similar to our results, the meta analysis by Aldenkortt and colleagues found no difference in either oxygenation or ventilation with ventilation mode in obese adults undergoing abdominal procedures [15]. One parameter that could potentially affect oxygenation is the inspiratory time and inspiratory: expiratory (I: E) ratio. In our study we attempted to hold the inspiratory time constant at 1.5 seconds, and quite successfully achieved this aim. However, in four of the patients during VC ventilation (all ventilation modes), it was necessary to adjust the inspiratory time as the PIP was greater than 40 cmH2O. It is possible that oxygenation could be improved during PC ventilation modes by lengthening the inspiratory time given its impact on mean airway pressure and therefore oxygenation. Important to note is that VC ventilation was not capable of adequately ventilating one patient and had to be abandoned for a pressure mediated ventilation mode.
Conclusions
In the adolescent and young adult bariatric population undergoing laparoscopy, PCV-VG and PC ventilation were superior to VC ventilation in the ability to mechanically ventilate with the lowest PIP. PCV-VG ventilation may require fewer adjustments than PC ventilation with variations in lung compliance and resistance. No other differences were noted between the modes of ventilation when considering oxygenation, ventilation, hemodynamic variables, and intraoperative anesthetic requirements.
Acknowledgements
Approval for this study was granted by The Institutional Review Board of Nationwide Children’s Hospital (Columbus, Ohio). For this type of study formal consent is not required, thus The Institutional Review Board waived the need for written, informed consent.
Disclosure of conflict of interest
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, Urbina EM, Ewing LJ, Daniels SR Hypertension, Metabolism; American Heart Association Atherosclerosis, Hypertension and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, Council on Clinical Cardiology. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–1712. doi: 10.1161/CIR.0b013e3182a5cfb3. [DOI] [PubMed] [Google Scholar]
- 2.Barnett SJ. Surgical management of adolescent obesity. Adv Pediatr. 2013;60:311–25. doi: 10.1016/j.yapd.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Schumann R. Anaesthesia for bariatric surgery. Best Pract Res Clin Anaesthesiol. 2011;25:83–93. doi: 10.1016/j.bpa.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Talab HF, Zabani IA, Abdelrahman HS, Bukhari WL, Mamoun I, Ashour MA, Sadeq BB, El Sayed HI. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg. 2009;109:1511–6. doi: 10.1213/ANE.0b013e3181ba7945. [DOI] [PubMed] [Google Scholar]
- 5.Mousa WF. Equal ratio ventilation (1:1) improves arterial oxygenation during laparoscopic bariatric surgery: A crossover study. Saudi J Anaesth. 2013;7:9–13. doi: 10.4103/1658-354X.109559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brenn BR. Anesthesia for pediatric obesity. Anesthesiol Clin North America. 2005;23:745–764. doi: 10.1016/j.atc.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Samuels PJ. Anesthesia for adolescent bariatric surgery. Int Anesthesiol Clin. 2006;44:17–31. doi: 10.1097/01.aia.0000196250.61280.65. [DOI] [PubMed] [Google Scholar]
- 8.Tobias JD, Holcomb GW III, Brock JW III, Deshpande JK, Lowe S, Morgan WM III. Cardio respiratory changes during laparoscopy in children. J Pediatr Surg. 1995;30:33–6. doi: 10.1016/0022-3468(95)90603-7. [DOI] [PubMed] [Google Scholar]
- 9.Tobias JD. Anesthetic considerations for laparoscopy in children. Semin Laparosc Surg. 1998;5:60–6. doi: 10.1177/155335069800500111. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ, Wolfe BM. Effects of pneumoperitoneum on intraoperative pulmonary mechanics and gas exchange during laparoscopic gastric bypass. Surg Endosc. 2004;18:64–71. doi: 10.1007/s00464-002-8786-x. [DOI] [PubMed] [Google Scholar]
- 11.Hans GA, Pregaldien AA, Kaba A, Sottiaux TM, DeRoover A, Lamy ML, Joris JL. Pressure-controlled ventilation does not improve gas exchange in morbidly obese patients undergoing abdominal surgery. Obes Surg. 2008;18:71–6. doi: 10.1007/s11695-007-9300-2. [DOI] [PubMed] [Google Scholar]
- 12.De Baerdemaeker LE, Van der Herten C, Gillardin JM, Pattyn P, Mortier EP, Szegedi LL. Comparison of volume-controlled and pressure-controlled ventilation during laparoscopic gastric banding in morbidly obese patients. Obes Surg. 2008;18:680–5. doi: 10.1007/s11695-007-9376-8. [DOI] [PubMed] [Google Scholar]
- 13.Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D. Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth. 2008;100:709–16. doi: 10.1093/bja/aen067. [DOI] [PubMed] [Google Scholar]
- 14.Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilator strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth. 2009;102:862–8. doi: 10.1093/bja/aep084. [DOI] [PubMed] [Google Scholar]
- 15.Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramer MR. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109:493–502. doi: 10.1093/bja/aes338. [DOI] [PubMed] [Google Scholar]


