Abstract
Background
Dietary habits and depression are each associated with cardiovascular disease risk. Patient with depression often report poor eating habits and dietary factors may help explain commonly observed associations between depression and cardiovascular disease.
Method
From 1996–2000, 936 women were enrolled in the Women's Ischemia Syndrome Evaluation (WISE) at four US academic medical centers at the time of clinically indicated coronary angiography and then assessed (median follow-up, 5.9 years) for adverse outcomes (cardiovascular disease death, heart failure, myocardial infarction, stroke). Participants completed a protocol including coronary angiography (coronary artery disease severity), depression assessments (Beck Depression Inventory [BDI] scores, antidepressant use, & depression treatment history). A subset of 201 women (mean age= 58.5(SD=11.4) further completed the Food Frequency Questionnaire for Adults (FFQ; 1998 Block). We extracted daily fiber intake and daily servings of fruit and vegetables as measures of dietary habits.
Results
In separate Cox regression models adjusted for age, smoking, and coronary artery disease severity, Beck Depression Inventory scores (HR=1.05, 95% CI=1.01–1.10), antidepressant use (HR=2.4, 95% CI=1.01–5.9) and a history of treatment for depression (HR=2.4, 95%CI=1.1–5.3) were each adversely associated with time to cardiovascular disease outcomes. Fiber intake (HR=.87, 95% CI=.78–.97) and fruit and vegetable consumption (HR=.36, 95% CI=.19–.70) was associated with a decreased time to cardiovascular disease event risk. In models including dietary habits and depression, fiber intake and fruit and vegetable consumption remained associated with time to cardiovascular disease outcomes, whereas depression relationships were reduced by 10–20% and non-significant.
Conclusions
Among women with suspected myocardial ischemia, we observed consistent relationships between depression, dietary habits, and time to cardiovascular disease events. Dietary habits partly explained these relationships. These results suggest that dietary habits be included in future efforts to identify mechanisms linking depression to cardiovascular disease.
Keywords: cardiovascular disease, women, prospective, depression, diet
Intervention trial results suggest a key role for healthy dietary habits in the reduction of cardiovascular disease events and mortality1–2. Poor dietary habits are similarly a common correlate of depression3–5, with depression also a consistent but poorly understood predictor of cardiovascular disease events6–7. The potential role of dietary factors as a mechanism in the depression- cardiovascular disease relationship has not been widely studied. In a case-control study with a post-acute coronary syndrome sample, researchers reported that omega 3 fatty acid and docosahexaenoic acid (DHA) levels were significantly lower among patients with versus without depression8. Results from the Heart and Soul Study9 also reported lower omega 3 fatty acid levels among patients with versus without depression, but found no statistical evidence that omega 3 levels mediated prospective relationships between depression and cardiovascular disease events. Finally, a 2013 study reporting cross-sectional relationships of diet, depression, and cardiovascular disease risk observed evidence of a mediating effect of diet, such that adherence to a Mediterranean diet statistically mediated the relationship between depression and cardiovascular disease risk scores10. Because of the relatively narrow focus in prior research on specific dietary nutrients (e.g., fatty acids) and specific diets, more broadly evaluating the role of dietary factors in the study of depression and cardiovascular disease represents a promising opportunity for advancing knowledge in this field.
In the current study, we prospectively examined relationships between depression, dietary habits, and time to cardiovascular disease mortality and events among a sample of women with suspected myocardial ischemia. We hypothesized that dietary habits would explain the relationship between depression and cardiovascular disease outcomes consistent with a statistical mediation model. This model requires three parallel criteria: a) depression and dietary habits separately predicting time to cardiovascular disease outcomes; b) relationships between depression and dietary habits; c) dietary habits eliminating or reducing depression-time to cardiovascular disease outcome associations while remaining a significant independent predictor.
Methods
Participants
Women (18+ years old) undergoing a clinically indicated coronary angiogram for suspected myocardial ischemia were recruited for the Women’s Ischemia Syndrome Evaluation (WISE) study from four participating study sites (University of Alabama at Birmingham; University of Florida, Gainesville; University of Pittsburgh; & Allegheny General Hospital, Pittsburgh)11. The purpose of the WISE study was to improve the understanding and diagnosis of ischemic heart disease in women. Exclusion criteria included major comorbidity compromising follow-up, pregnancy, contraindication to provocative diagnostic testing, cardiomyopathy, New York Heart Association class IV heart failure, recent myocardial infarction or revascularization procedure, significant valvular or congenital heart disease, and language barrier. All participants provided written informed consent, and all participating sites obtained Institutional Review Board approval.
The WISE Angiographic Core Laboratory (Rhode Island Hospital, Providence, RI) performed quantitative analysis of coronary angiograms, with investigators blinded to all other subject data12. Luminal diameter was measured at all stenoses and at nearby reference segments using an electronic cine projector-based “cross-hair” technique (Vanguard Instrument Corporation, Melville, New York). Each participant received a continuous coronary artery disease severity score based on angiogram results and a modified Gensini index12.
Clinical events
Women were contacted at six weeks post-baseline and annually thereafter for a median of 5.9 years (25th percentile=2.5 years; 75th percentile=6.9 years) to track their experiences of cardiovascular mortality and events, the latter including incident heart failure, stroke, or myocardial infarction. Follow-up consisted of a scripted telephone interview by an experienced research nurse. This data collection tool was validated previously against medical records13. A blinded study mortality committee reviewed death certificates to determine causes of death among deceased participants. In the current analyses, deaths coded as either probably or definitely resulting from cardiovascular disease causes were included as mortality events.
Dietary assessment
As part of the baseline assessment, a subset of participants completed the 1998 Block, Food Frequency Questionnaire for Adults. The WISE baseline assessment did not include the Food Frequency Questionnaire until months after initial recruitment, accounting for the subset of participants completing this measure. The block version of the Food Frequency Questionnaire is a 110-item measure designed to estimate usual and customary intake of a wide array of nutrients and food groups. Completion time for the Food Frequency Questionnaire is 30–40 minutes, with food items derived from the National Health and Nutrition Examination Survey (NHANES) III dietary recall data. From the Food Frequency Questionnaire website (http://www.nutritionquest.com/), the nutrient database was developed from the USDA Nutrient Database for Standard Reference. Individual portion size is assessed for each food, and pictures are provided to enhance accuracy of quantification.
Modifiable risk factors
Major cardiovascular disease risk factors ascertained in the WISE study included smoking status, blood pressure, dyslipidemia, diabetes, and obesity. We assessed smoking based on self-reported current, former, or never smoker status. We defined hypertension, dyslipidemia, and diabetes status for this report based upon participant’s report of a history of treatment for these conditi0ns (lifestyle or medication). We measured weight status in terms of body mass index. Self-reported education history served as a socioeconomic status indicator.
Depression
WISE participants completed three separate depression measures as part of the baseline assessment: 1) a validated measure (Beck Depression Inventory14]) of depressive symptom severity; 2) current use (i.e., use in the past week) of antidepressants; and 3) a self-reported history of treatment for depression. The Beck Depression Inventory is a 21-item measure, with each item response scored from 0–3, and validated in many prior cardiovascular disease studies. Higher Beck Depression Inventory scores indicate more severe symptoms.
Statistical Analyses
We completed descriptive and bivariate statistical comparisons using means, standard deviations, correlations, and t-tests. Non-normally distributed variables were log transformed for the regression models. We aggregated the separate fruit and vegetable variables to create a fruit + vegetable consumption composite variable. We used Cox regression methods to evaluate prospective relationships between depression measures, dietary habits, and cardiovascular disease events (combined cardiovascular disease mortality, heart failure, myocardial infarction, & stroke), with the results representing time to event relationships adjusted for coronary artery disease severity scores and other covariates. For non-dichotomous predictors, hazard ratio values represented time to cardiovascular disease event differences per serving increase in fiber intake, fruit and vegetable consumption, and per point increase in Beck Depression Inventory and coronary artery disease severity scores. We performed separate survival analyses for each of the three depression measures. Due to the moderate sample size, we limited covariates to those showing at least trends (p<.10) towards significant relationships with cardiovascular disease events in order to prevent over fitting of the hazard models. We computed additional models controlling for education history but this step produced no meaningful changes to the depression and diet relationships. All statistical analyses were completed using SPSS software, version 17.0 (SPSS Inc., Chicago, IL, USA), with statistical significance declared at p<.05.
Results
As shown in Table 1, the participating WISE sample consisted of women of predominantly middle age (mean=58.5[11.4]) and high school or greater educated (79.4% completing high school). Combined fruit and vegetable intake was less than 2.5 servings per day. Cardiovascular disease risk factors were common in the sample, ranging from nearly 20% reporting current smoking to nearly 75% with dyslipidemia. We include descriptions of the full WISE sample (N=936) and the subsamples with (n=201) and without (n=735) dietary information. There were no significant differences between women with versus without dietary information on any of the demographic, depression measures, or cardiovascular disease variables displayed in Table 1. We further compared participants with lower versus higher Beck Depression Inventory scores (using a median value of 9.0 on the scale) on the same study related variables, with results shown in Table 2.
Table 1.
Demographic, biomedical, and dietary variables among study participant groups (mean[standard deviation]).
| Variable |
Subsample with dietary data (n=201) |
Subsample without dietary data (n=735) |
Complete cohort (N=936) |
|---|---|---|---|
| Age | 58.5(11.4) | 58.2(11.7) | 58.3(11.6) |
| <High school education (%) | 20.6 | 19.5 | 19.7 |
| Beck Depression Inventory | 10.5(8.1) | 10.5(8.2) | 10.5(8.1) |
| Antidepressant use (%) | 14.4 | 18.3 | 17.6 |
| Depression treatment history (%) | 21.5 | 24.8 | 24.2 |
| CAD severity score* | 2.3(.76) | 2.4(.79) | 2.3(.79) |
| CVD events (%) | 16.4 | 18.8 | 18.3 |
| Daily fiber intake (grams) | 8.4(4.3) | NA | NA |
| Daily fruit servings | 1.2(.84) | NA | NA |
| Daily vegetable servings | 1.2(.78) | NA | NA |
| Regular multivitamin use (%) | 64.0 | NA | NA |
| Average calorie intake | 1269.1 | NA | NA |
| % calories from fat | 36.8 | NA | NA |
| % calories from protein | 16.3 | NA | NA |
| % calories from carbohydrate | 46.3 | NA | NA |
| # prior weight loss diets | 3.1(1.8) | NA | NA |
| Hypertensive (%) | 58.1 | 59.7 | 59.4 |
| Dyslipidemia (%) | 72.1 | 64.5 | 66.2 |
| Diabetic (%) | 24.0 | 25.4 | 25.1 |
| Body mass index≥30 (%) | 39.4 | 41.7 | 41.2 |
| Current smoker (%) | 19.7 | 20.3 | 20.2 |
Variable derived from quantitative angiogram result and logarithmically transformed to normalize distribution
CAD=Coronary Artery Disease CVD=Cardiovascular disease (CVD mortality, heart failure, myocardial infarction, & stroke)
Table 2.
Comparison of participants with lower (≤9) versus higher Beck Depression Inventory scores (mean[standard deviation]) on demographic, biomedical, and dietary variables.
| Variable |
Lower Beck Depression Inventory scores (n=105) |
Higher Beck Depression Inventory scores (n=96) |
|---|---|---|
| Age | 59.9(11.5) | 56.8(11.2) |
| <High school education (%) | 83.8 | 80.2 |
| Beck Depression Inventory | 4.9(2.7) | 16.9(7.4)** |
| Antidepressant use (%) | 11.4 | 19.8** |
| Depression treatment history (%) | 14.3 | 31.9** |
| CAD severity score* | 2.3(.8) | 2.3(.8) |
| CVD events (%) | 13.4 | 20.5**** |
| Daily fiber intake (grams) | 8.7(4.4) | 8.1(4.2) |
| Daily fruit servings | 1.3(.9) | 1.1(.9) |
| Daily vegetable servings | 1.3(.8) | 1.2(.8) |
| Regular multivitamin use (%) | 71.3 | 56.8** |
| Average calorie intake | 1314.7(736.1) | 1202.0(561.7) |
| % calories from fat | 36.6(9.9) | 36.7(11.5) |
| % calories from protein | 16.8(3.7) | 15.6(4.3) |
| % calories from carbohydrate | 46.0(10.1) | 47.0(12.4) |
| # prior weight loss diets | 2.9(1.6) | 3.3(1.9) |
| Hypertensive (%) | 54.3 | 61.1 |
| Dyslipidemia (%) | 52.4 | 59.3 |
| Diabetic (%) | 21.0 | 28.6 |
| Body mass index≥30 (%) | 40.0 | 37.4 |
| Current smoker (%) | 13.5 | 28.6** |
Variable derived from quantitative angiogram result and logarithmically transformed to normalize distribution
Group difference significant, p<.05 CAD=Coronary
Artery Disease CVD=Cardiovascular disease (CVD mortality, heart failure, myocardial infarction, & stroke)
Over a median 5.9 years of follow-up, 32 cardiovascular disease events occurred (five cardiovascular disease deaths, nine heart failure episodes, nine myocardial infarction events, & nine strokes). Among women completing the Food Frequency Questionnaire, fruit and vegetable consumption and fiber intake were below recommended nutrition guidelines of five or more daily servings of fruits and vegetables and 25 or more grams of fiber per day15.
The three depression measures correlated moderately. Current antidepressant users (versus non-users) reported significantly higher Beck Depression Inventory scores (means=14.6[10.6] vs 9.7[7.4], respectively, p=.002). Women with a history of depression treatment (versus those without a treatment history) also endorsed higher depressive symptoms on the Beck Depression Inventory (means=14.8[10.4] vs 9.3[6.9], respectively, p<.001) and were more likely to report current antidepressant use (50.2% vs 17.5%, respectively, p<.001).
Depression, dietary habits, and cardiovascular diseaase risk factors
More severe depressive symptoms (Beck Depression Inventory scores) predicted a greater likelihood of current or former smoking (r=.23, p<.001) but were not associated with diabetes, dyslipidemia, hypertension, or obesity. Higher Beck Depression Inventory scores also correlated with lower fruit and vegetable consumption (r=−20, p=.006) and fiber intake (r=−.12, p=.09). Women reporting a history of treatment for depression showed higher rates of current smoking compared to women without a treatment history (31.1% vs 16.5%, respectively, p=.03) and lower levels of fruit and vegetable consumption (mean daily servings= 2.0[1.3] vs 2.5[1.3], respectively, p=.03). Participants reporting current antidepressant use (versus non-users) did not differ on cardiovascular disease risk factors or dietary habits.
Depression, dietary habits and cardiovascular disease events
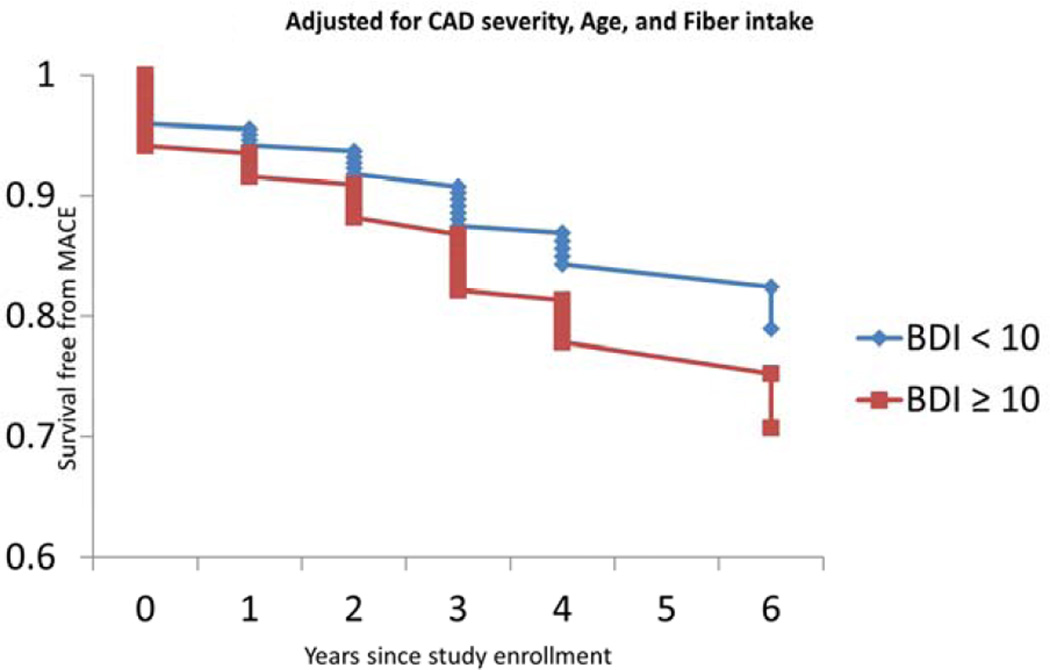
In Cox regression models adjusted for age and coronary artery disease severity scores, Beck Depression Inventory scores, (HR=1.06, 95% CI=1.01–1.11), antidepressant use (HR=4.7, 95% CI=1.9–12.0), depression treatment history (HR=3.6, 95% CI=1.5–8.6), smoking status (HR=1.5, 95% CI=.94–2.5), fiber intake (HR=.88, 95% CI=.78–.97), and fruit and vegetable consumption (HR=.63, 95% CI=.45–.88) each predicted time to cardiovascular disease events at p<.10.. Results from the separate hazard models containing 1) depression and fiber intake and 2) depression and fruit and vegetable intake appear in Table 3. Figures 1–3 illustrate the relationship between lower and higher Beck Depression Inventory scorers and time to events before and after adjustment for the nutritional factors. The same pattern of results manifested across the three depression measures: the magnitude of the hazard ratio between depression measure and time to cardiovascular disease events decreased by 10–20% with fiber intake or fruit and vegetable consumption concurrently in the model and the dietary habits remained significant predictors. In all six models, depression was no longer a statistically significant predictor of time to cardiovascular disease events after including the fiber intake or fruit and vegetable consumption variables.
Table 3.
Cox regression models describing covariate-adjusted relationships between depression, dietary habit variables, and CVD and mortality events.
| Model 1: Beck Depression Inventory scores and fiber intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.00 | .97–1.04 | |
| Coronary artery disease severity score* | 2.33 | 1.54–3.53 | |
| Smoking status | 1.24 | .71–1.91 | |
| Beck Depression Inventory | 1.04 | .99–1.09 | |
| Fiber intake | .89 | .79–.99 | |
| Model 2: BDI scores and fruit and vegetable intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.00 | .97–1.04 | |
| Coronary artery disease severity score* | 2.41 | 1.62–3.72 | |
| Smoking status | 1.10 | .66–1.91 | |
| Beck Depression Inventory | 1.04 | .99–1.09 | |
| Fruit & vegetable consumption | .68 | .47–.98 | |
| Model 3: Antidepressant use and fiber intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.02 | .98–1.06 | |
| Coronary artery disease severity score* | 2.30 | 1.62–3.53 | |
| Smoking status | 1.20 | .73–2.02 | |
| Antidepressant use | 2.21 | .90–5.41 | |
| Fiber intake | .89 | .80–.99 | |
| Model 4: Antidepressant use and fruit and vegetable intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.02 | .99–1.06 | |
| Coronary artery disease severity score* | 2.42 | 1.63–3.72 | |
| Smoking status | 1.20 | .70–2.02 | |
| Antidepressant use | 2.12 | .88–5.31 | |
| Fruit & vegetable consumption | .68 | .48–.97 | |
| Model 5: Depression treatment history and fiber intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.02 | .99–1.06 | |
| Coronary artery disease severity score* | 2.44 | 1.61–3.72 | |
| Smoking status | 1.24 | .73–2.01 | |
| Depression treatment history | 2.20 | .95–5.04 | |
| Fiber intake | .89 | .80–.99 | |
| Model 6: Depression treatment history and fruit and vegetable intake | |||
| Final model | Variable | Hazard ratio | 95% CI |
| Age | 1.02 | .99–1.06 | |
| Coronary artery disease severity score* | 2.50 | 1.63–3.81 | |
| Smoking status | 1.22 | .70–2.01 | |
| Depression treatment history | 2.03 | .90–4.73 | |
| Fruit & vegetable consumption | .69 | .48–.98 | |
Derived from angiogram result and logarithmically transformed to normalize distribution
Significant results are highlighted in bold text
Figure 1.
The relationship Beck Depression Inventory scores and cardiovascular disease event rates over follow-up (MACE=Major Adverse Coronary Events).
Figure 3.
The relationship Beck Depression Inventory scores and cardiovascular disease event rates after adjusting for fruit and fiber intake (MACE=Major Adverse Coronary Events).
Discussion
This report describes preliminary evidence supporting specific dietary habits – including fiber intake and fruit and vegetable consumption – as factors that help explain relationships between depression and time to cardiovascular disease mortality and events. Using three distinct measures of depression (symptom severity, current antidepressant use, and history of depression treatment), hazard models predicting combined time to cardiovascular disease mortality and events (heart failure, myocardial infarction, and stroke) showed that depression, fiber intake, and fruit and vegetable consumption independently predicted time to events after adjusting for age, smoking status, and coronary artery disease severity over a 5.9 year median follow-up. Jointly including dietary habits and depression in the survival analyses, however, revealed a consistent pattern across each depression measure. Dietary habits remained significant event predictors while reducing depression relationships to nonsignificance. This pattern is consistent with the hypothesis that dietary factors partly account for the relationship between depression and time to cardiovascular disease events.
Relative to prior research on the topic of depression, diet, and cardiovascular disease, this study offers several novel contributions. These include the validation of the relationship patterns achieved by replicating across three separate depression measures, the focus on a clinical sample of women completing coronary angiograms to quantify coronary artery disease severity, and the inclusion of fiber, fruit, and the use of vegetable intake variables in a longitudinal study of depression and cardiovascular disease events. Despite considerable evidence of poorer dietary practices among those experiencing depression16–17 and growing support for the role of diet in cardiovascular disease risk18–19, few prospective studies have examined dietary variables in the context of depression and cardiovascular disease relationships9. Existing studies primarily focused on fatty acids8–9 showing that depression was associated with lower levels of omega 3 fatty acids. The current study, therefore, expands the range of dietary variables linked to depression in cardiovascular disease.
Previous publications from WISE showed that depression is a robust predictor of time to mortality and events in this clinical sample of women. Separate findings from prior reports demonstrated that depression was a reliable predictor of time to events after adjusting for cardiovascular disease risk factors25, that depression was associated with increased healthcare costs in addition to increased event risk26, and that depression may overlap with related mental health conditions such as anxiety in predicting time to event risk27. The results of this and previous WISE reports suggest that depression is a common comorbid condition among women presenting to cardiology settings. The high prevalence of depression in the WISE cohort (about 1/5th using antidepressants, ¼ reporting a history of depression treatment, and over ½ reporting elevated depressive symptoms on the Beck Depression Inventory compared to an overall depression prevalence in U.S. women of 6.7% based on NHANES data28) reinforces attention to depression among women in this context.
This study collected dietary data using the 1998 version of the Food Frequency Questionnaire. For the purpose of this study, we chose to focus on a subset of American Heart Association29 and empirically supported dietary factors including fiber, fruit, and vegetable consumption to offer a theoretically driven approach to the study of depression-diet- time to cardiovascular disease relationships. Fruit and vegetable consumption overlaps with fiber intake, but is not equivalent (e.g., whole grains are another important fiber source). WISE women reported low fiber (8.4 grams/day), fruit, and vegetable intake (<3 servings/day), values comparable to pre- and post-menopausal women groups described in previous NHANES III publications30. Our findings are consistent with previous studies linking these dietary habits to cardiovascular disease risk18–19 while offering possible insight into novel mechanisms linking depression to cardiovascular disease.
Study limitations
Although this study offers potentially important new information for understanding depression- cardiovascular disease relationships, our findings provide only an incomplete picture of the multidirectional relationship between depression and diet. Depression may undermine healthy eating habits in several ways, for example, by affecting appetite, disturbing sleep, and producing food cravings20–21. Alternatively, poorer dietary habits may promote depressive symptoms through mechanisms such as inflammation (e.g., lower omega 3 fatty acid consumption), poor blood sugar control, and nutritional deficiencies, and by affecting gut flora linked to psychiatric disorders and cardiovascular disease22–24. Factors such as lower socioeconomic status and physical activity could influence both depression and dietary habits. Achieving a broader understanding of the depression-diet relationship will require a combination of laboratory, interventional, and prospective methodologies.
There are several important limitations to consider in the interpretation of this work. Neither dietary habits nor psychosocial factors were the primary target of the WISE study and we administered these measures to only a subgroup of the WISE sample. Dietary factors in WISE were assessed as part of an observational study design. The results should not be construed to imply a causal relationship between diet and depression. Although we observed no evidence to indicate systematic differences between participants with versus without dietary data, we cannot confirm that the subsample described in this paper accurately generalizes to the complete WISE cohort. We collected dietary and depression data at only one time point, an approach that overlooks the dynamic nature of these variables. Lastly, we assessed dietary (Food Frequency Questionnaire) and depression (Beck Depression Inventory, treatment status) variables using self-report measures, a methodology that is known to produce results differing somewhat from more objective measures of dietary intake31 and structured interview measures of depression32.
Conclusions
This study reported relationships between depression (measured via Beck Depression Inventory scores, current antidepressant use, and a history of treatment for depression), dietary habits, and time to cardiovascular disease mortality and events. These relationships are consistent with prior studies but expanded upon in the current paper by the use of multiple depression measures and dietary habits previously unexplored in this context. Our results further suggested that fiber intake and fruit and vegetable consumption each partially mediated associations between depression and time to cardiovascular disease events, showing that these dietary habits remained independent predictors of time to cardiovascular disease events while eliminating statistically significant relationships between depression and time to cardiovascular disease events. The findings support future investigations of diet as a potentially important mechanism in the depression-cardiovascular disease relationship.
Figure 2.
The relationship Beck Depression Inventory scores and cardiovascular disease event rates after adjustment for fiber intake (MACE=Major Adverse Coronary Events).
Clinical Significance.
Dietary habits such as fruit and vegetable consumption may help explain depression-cardiovascular disease relationships.
Depression is a highly prevalent condition among female patients seen in routine cardiology settings.
Depression information collected in brief, even single-item assessments may aid in cardiovascular disease event prediction.
Acknowledgments
Funding
This work was supported by contracts from the National Heart, Lung and Blood Institutes, [N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164], grants [U0164829, U01 HL649141, U01 HL649241], a General Clinical Research Center grant [MO1-RR00425] from the National Center for Research Resources, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Denville, New Jersey, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, California, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, Pennsylvania, and The Edythe Broad Endowment for Women's Heart Research, Los Angeles, California.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: All authors declared no study-related conflicts of interest in the development of this manuscript.
Author declaration: All listed authors had full access to the data for this manuscript and contributed directly to the development of the manuscript through writing, editorial review, and statistical analyses
References
- 1.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 3.Payne ME, Steck SE, George RR, Steffens DC. Fruit, vegetable, and antioxidant intakes are lower in older adults with depression. J Acad Nutr Diet. 2012;112:2022–2027. doi: 10.1016/j.jand.2012.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McMartin SE, Jacka FN, Colman I. The association between fruit and vegetable consumption and mental health disorders: evidence from five waves of a national survey of Canadians. Prev Med. 2013;56:225–230. doi: 10.1016/j.ypmed.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Kronish IM, Carson AP, Davidson KW, Muntner P, Safford MM. Depressive symptoms and cardiovascular health by the American Heart Association's definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS One. 2012;7:e52771. doi: 10.1371/journal.pone.0052771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004 Nov-Dec;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 7.Leung YW, Flora DB, Gravely S, Irvine J, Carney RM, Grace SL. The impact of premorbid and postmorbid depression onset on mortality and cardiac morbidity among patients with coronary heart disease: meta-analysis. Psychosom Med. 2012;74:786–801. doi: 10.1097/PSY.0b013e31826ddbed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frasure-Smith N, Lespérance F, Julien P. Major depression is associated with lower omega-3 fatty acid levels in patients with recent acute coronary syndromes. Biol Psychiatry. 55:891–896. doi: 10.1016/j.biopsych.2004.01.021. 20041. [DOI] [PubMed] [Google Scholar]
- 9.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antonogeorgos G, Panagiotakos DB, Pitsavos C, Papageorgiou C, Chrysohoou C, Papadimitriou GN, Stefanadis C. Understanding the role of depression and anxiety on cardiovascular disease risk, using structural equation modeling; the mediating effect of the Mediterranean diet and physical activity: the ATTICA study. Ann Epidemiol. 2012;22:630–637. doi: 10.1016/j.annepidem.2012.06.103. [DOI] [PubMed] [Google Scholar]
- 11.Bairey Merz CN, Kelsey SF, Pepine CJ, Reichek N, Reis SE, Rogers WJ, Sharaf BL, Sopko G. The Women’s Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology, and feasibility report. J Am Coll Cardiol. 1999;33:1453–1461. doi: 10.1016/s0735-1097(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 12.Sharaf BL, Pepine CJ, Kerensky RA, Reis SE, Reichek N, Rogers WJ, Sopko G, Kelsey SF, Holubkov R, Olson M, Miele NJ, Williams DO, Bairey Merz CN. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] study angiographic core laboratory) Am J Cardiol. 2001;87:937–941. doi: 10.1016/s0002-9149(01)01424-2. [DOI] [PubMed] [Google Scholar]
- 13.Mahoney EM, Jurkovitz CT, Chu H, Becker ER, Culler S, Kosinski AS, Robertson DH, Alexander C, Nag S, Cook JR, Demopoulos LA, DiBattiste PM, Cannon CP, Weintraub WS. Cost and cost effectiveness of an early invasive vs. conservative strategy for the treatment of unstable angina and non-ST-segment elevation myocardial infarction. JAMA. 2002;288:1851–1858. doi: 10.1001/jama.288.15.1851. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT. Depression inventory. Philadelphia: Center for Cognitive Therapy; 1978. [Google Scholar]
- 15.U.S. Department of Agriculture and U.S. Department of Health and Human Services. 7th Edition. Washington, DC: U.S. Government Printing Office; 2010. [December 2010]. Dietary Guidelines for Americans. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skarupski KA, Tangney CC, Li H, Evans DA, Morris MC. Mediterranean Diet and Depressive Symptoms among Older Adults over Time. J Nutr Health Aging. 2013;17:441–445. doi: 10.1007/s12603-012-0437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lucas M, Mirzaei F, O'Reilly EJ, Pan A, Willett WC, Kawachi I, Koenen K, Ascherio A. Dietary intake of n-3 and n-6 fatty acids and the risk of clinical depression in women: a 10-y prospective follow-up study. Am J Clin Nutr. 2011;93:1337–1343. doi: 10.3945/ajcn.111.011817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leenders M, Sluijs I, Ros MM, Boshuizen HC, Siersema PD, Ferrari P, Weikert C, Tjønneland A, Olsen A, Boutron-Ruault MC, Clavel-Chapelon F, Nailler L, Teucher B, Li K, Boeing H, Bergmann MM, Trichopoulou A, Lagiou P, Trichopoulos D, Palli D, Pala V, Panico S, Tumino R, Sacerdote C, Peeters PH, van Gils CH, Lund E, Engeset D, Redondo ML, Agudo A, Sánchez MJ, Navarro C, Ardanaz E, Sonestedt E, Ericson U, Nilsson LM, Khaw KT, Wareham NJ, Key TJ, Crowe FL, Romieu I, Gunter MJ, Gallo V, Overvad K, Riboli E, Bueno-de-Mesquita HB. Fruit and Vegetable Consumption and Mortality: European Prospective Investigation Into Cancer and Nutrition. Am J Epidemiol. 2013 Apr 18; doi: 10.1093/aje/kwt006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Pereira MA, O'Reilly E, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med. 2004;164:370–376. doi: 10.1001/archinte.164.4.370. [DOI] [PubMed] [Google Scholar]
- 20.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Gibson EL. The psychobiology of comfort eating: implications for neuropharmacological interventions. Behav Pharmacol. 2012;23:442–460. doi: 10.1097/FBP.0b013e328357bd4e. [DOI] [PubMed] [Google Scholar]
- 22.Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fetissov SO, Déchelotte P. The new link between gut-brain axis and neuropsychiatric disorders. Curr Opin Clin Nutr Metab Care. 2011;14:477–482. doi: 10.1097/MCO.0b013e32834936e7. [DOI] [PubMed] [Google Scholar]
- 24.Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012;10:735–742. doi: 10.1038/nrmicro2876. [DOI] [PubMed] [Google Scholar]
- 25.Vaccarino V, McClure C, Johnson BD, Sheps DS, Bittner V, Rutledge T, Shaw LJ, Sopko G, Olson MB, Krantz DS, Parashar S, Marroquin OC, Merz CN. Depression, the metabolic syndrome and cardiovascular risk. Psychosom Med. 2008;70:40–48. doi: 10.1097/PSY.0b013e31815c1b85. [DOI] [PubMed] [Google Scholar]
- 26.Rutledge T, Vaccarino V, Johnson BD, Bittner V, Olson MB, Linke SE, Cornell CE, Eteiba W, Sheps DS, Francis J, Krantz DS, Bairey Merz CN, Parashar S, Handberg E, Vido DA, Shaw LJ. Depression and cardiovascular health care costs among women with suspected myocardial ischemia: prospective results from the WISE (Women's Ischemia Syndrome Evaluation) Study. J Am Coll Cardiol. 2009;53:176–183. doi: 10.1016/j.jacc.2008.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whittaker KS, Krantz DS, Rutledge T, Johnson BD, Wawrzyniak AJ, Bittner V, Eastwood JA, Eteiba W, Cornell CE, Pepine CJ, Vido DA, Handberg E, Merz CN. Combining psychosocial data to improve prediction of cardiovascular disease risk factors and events: The National Heart, Lung, and Blood Institute--sponsored Women's Ischemia Syndrome Evaluation study. Psychosom Med. 2012;74:263–270. doi: 10.1097/PSY.0b013e31824a58ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pratt LA, Brody DJ. NCHS data brief, no 7. Hyattsville, MD: National Center for Health Statistics; 2008. Depression in the United States Household Population, 2005–2006. [PubMed] [Google Scholar]
- 29.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010 Feb 2;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 30.Carter SJ, Roberts MB, Salter J, Eaton CB. Relationship between Mediterranean Diet Score and atherothrombotic risk: findings from the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Atherosclerosis. 2010;210:630–636. doi: 10.1016/j.atherosclerosis.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 31.Schoeller DA. Limitations in the assessment of dietary energy intake by self-report. Metabolism. 1995;44:18–22. doi: 10.1016/0026-0495(95)90204-x. [DOI] [PubMed] [Google Scholar]
- 32.Fisher L, Skaff MM, Mullan JT, Arean P, Mohr D, Masharani U, Glasgow R, Laurencin G. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care. 2007;30:542–548. doi: 10.2337/dc06-1614. [DOI] [PubMed] [Google Scholar]