Abstract
Background
Although amphetamine-type stimulant (ATS) use is an important issue that has caused growing concerns in China as well as other countries, the knowledge of long-term patterns of ATS use in China is limited. This study explored long-term patterns of ATS use in Shanghai, China, and compared the differences by ATS use trajectory groups, seeking to identify risk factors that have implications for the development of targeted intervention programs.
Methods
A total of 377 ATS users were recruited from the Compulsory Isolation Center for Drug Rehabilitation in Shanghai. Group-based trajectory modeling was applied to identify distinctive trajectories of ATS use over 8 years at the time of interviews conducted in 2012. The mean number of days using ATS per month over a year from years 2005 to 2012 was analyzed with a censored normal model.
Results
Three distinctive groups were identified: high-use (19.1%), low-use (66.0%), and increasing-use (14.9%). Relative to the low-use group, the high-use and increasing-use groups were more likely to report having used opiate-type drugs and to have more craving experiences. Psychiatric symptoms following ATS use were frequently reported, with ATS users in the increasing-use and high-use groups more likely to report depression symptoms and suicide behaviors compared to the low-use group. The low-use and increasing-use groups reported more months in drug abuse treatment programs compared to the high-use group.
Conclusions
Addressing ATS use should take into consideration patients' use-related psychiatric symptoms as well as other risk factors, particularly among those with persistent high-level ATS use trajectories.
Keywords: Amphetamine-type stimulants, Trajectories, Dependence
1. INTRODUCTION
Amphetamine-type stimulant (ATS) drugs are a group of drugs whose principal members are amphetamine and methamphetamine (MA). The use of ATS drugs has become a part of the mainstream culture in many countries and has become a worldwide problem in recent years (UNODC, 2009). According to the UNODC, ATS drugs have become the world’s second most widely abused drug type after cannabis (UNODC, 2011). During the last decade, heroin and cocaine use attracted the most attention. However, since 2005 the number of ATS drug seizures increased considerably, causing growing concerns in affected countries (UNODC, 2013). Owing to their relative ease of manufacture, ATS drugs are attractive for millions of drug users. ATS drug use and related problems have been identified as a priority area for further research in Asian countries and populations (Hser et al., 2013).
China, one of the oldest countries in the world, also faces an ATS drug problem. In the late 1980s, with the implementation of the Reform and Open policy, drug abuse reappeared and increased sharply. The number of registered drug users rose from 70,000 in 1990 to 1.79 million in 2012 (Chu and Levy, 2005; MPS, 2012). To deal with the drug abuse problem and HIV/AIDS epidemic among this population, the Chinese government established a series of treatment sites and adopted harm reduction programs including methadone maintenance treatment (MMT) and a needle exchange program (NEP). Studies have documented that these strategies were successful in reducing drug abuse and drug-related risk behaviors (MPS, 2012; Wu et al., 2007). At present in China, traditional drugs of abuse (heroin and other opiate drugs) have been controlled effectively, but the abuse of ATS drugs, which appeared in China over the past decade, is growing. The proportion of this “new type” of drug use among all registered drug users was 6.7% in 2005, and data from the State Food and Drug Administration (SFDA) show that the proportion of drug users who use ATS drugs reached 34.4% in 2012 (MPS, 2012). It seems that ATS drugs will become even more widely abused in the future.
ATS drugs can induce psychotic states, and the heavier ATS users are at higher risk of psychosis. McKetin and colleagues (2006) reported that dependent ATS users were 3 times more likely to have experienced psychotic symptoms than non-dependent patients. Moreover, ATS use increases the risk of HIV infection due to the high-risk sexual behaviors, including multiple sexual partners with unprotected sexual practices, that have been reported in several different populations (Colfax et al., 2010; Degenhardt et al., 2010). ATS abuse has been considered as being intertwined with the epidemic of HIV (Molitor et al., 1998; Perry et al., 2001).
Many researchers raised an alert about ATS use/abuse around the world, and East Asia was regarded as a major region of concern because of its high MA production and trafficking (Glasner-Edward et al., 2010; Hser et al., 2008; He et al., 2013). The challenges of ATS abuse have been recognized in China, and a large body of research on ATS use has recently emerged (Bao et al., 2012; He et al., 2013; Zhang et al., 2013). Zhang et al. (2013) reported that males who used amphetamine combined with ketamine are more likely to develop psychotic disorders, while females are more likely to develop cognitive impairment. Bao et al. (2012) reported a high HCV prevalence among ATS users in 6 provinces in China. However, knowledge of the long-term patterns of ATS use is limited in China. Whether different trajectories of ATS use are associated with different risk characteristics has not been determined. In this article, we use timeline follow-back data collected in a drug rehabilitation center to explore the distinctive ATS trajectory patterns and associated characteristics in terms of drug use history and psychiatric symptoms. The present study explores the long-term patterns of ATS use and associated risk factors, which should have implications for developing more targeted treatment services and policies.
2. METHODS
2.1. Study design
This study utilized survey data from an intervention study focused on ATS abuse in Shanghai, China. The main aim of the original study was to test the effectiveness of a psychosocial intervention among ATS users. A total of 377 ATS users were recruited while they were in a Compulsory Isolation Center for Drug Rehabilitation. In Shanghai, according to the “Narcotic Control Law,” newly found drug users are sent to the drug abuse treatment hospital to assess the severity of their drug use, then back to the community to receive detoxification treatment under the supervision of social workers. If they relapse, drug users are sent to the Compulsory Isolation Center for Drug Rehabilitation, where they participate in a combination of detoxification treatment, physical exercise, and manual labor for 2 years. Although the center is under the judicial system, drug users at this facility are considered patients. The inclusion criteria for participants in our study were: (1) admission within 30 days of the study enrollment and ATS use prior to the admission (confirmed by a positive urine test for at least one ATS drug, including MA, Magu pills, the main component of which is MA, or MDMA); (2) the ability to understand the purpose of the study and complete study interviewing materials; and (3) being capable of giving consent. The exclusion criteria were: (1) prior history of psychotic disorders not caused by substance use; (2) risk of violence to clinical (research) staff; or (3) severe risk of self-harm. The study was approved by the Institutional Review Board (2011-37R) of the Shanghai Mental Health Center.
2.2. Instruments
2.2.1 Demographic, drug use, and risky sexual behavior
The interview protocol was developed by the study’s Shanghai research group. Demographic information, drug use/abuse history, and risky sexual behaviors were collected. Questions about drug-use history included the age of first ATS use, types of drugs ever used in addition to ATS drugs; whether use of ATS drugs was combined with other drugs; craving for ATS drugs during the past year if a participant could not get ATS drugs; and history of injecting ATS drugs. Craving for ATS drugs was assessed by the visual analog scale (VAS), which is a response scale that measures subjective attitudes that could not be observed directly. Participants were asked to indicate, on a scale from 0 (no craving for ATS drugs) to 10 (strong craving for ATS drugs), the extent of their craving for ATS drugs. Sexual behavior information included whether participants engaged in sexual behaviors after using ATS drugs, had multiple sexual partners or not after using ATS drugs in the past year, and used condoms or not.
2.2.2 Psychiatric symptoms after ATS use
Based on the Mini-International Neuropsychiatric Interview (MINI; Si et al., 2009), the research group selected psychiatric symptoms, depressive symptoms, and suicide items from the MINI to develop the questionnaire. Participants were asked if the following symptoms occurred following ATS use: persecutory delusions and delusions of reference (which were combined as delusion symptoms); thought reading, thought insertion, and strange or unusual beliefs (which were combined as thought disorders); and auditory hallucinations and visual hallucinations (which were combined as hallucination symptoms).
2.2.3 The Alcohol Use Disorders Identification Test (AUDIT)
This questionnaire was developed by the World Health Organization to identify hazardous and harmful alcohol use, as well as dependence, and is specifically designed for international use (Babor et al., 2001). The AUDIT consists of 10 items measuring the quantity and frequency of alcohol use, possible dependence symptoms, and recent and lifetime problems associated with alcohol use. The Cronbach’s alpha coefficient for the Chinese version of AUDIT was .87, and interclass correlation coefficients (ICCs) for total score and individual items were over .9. In the Chinese version, the cut-off score for harmful drinking was 7 (Li et al., 2003).
2.2.4 Timeline follow-back data of ATS use
The trajectory of ATS use frequencies (number of days per month) prior to this treatment were collected using timeline follow-back (TLFB; Sobell and Sobell, 1992). We used TLFB to collect data on retrospectively recalled events or behaviors in a chronological order starting from 2005, when the ATS use increased in China, until 2012, when the personal interviews were conducted.
2.3. Interview procedure
Fieldwork interviewers were trained research staff employed at the Shanghai Mental Health Center. All interviewers were psychiatrists and had more than 3 years of experience conducting research interviews in other studies of a similar nature. Potential participants were identified from a computerized database of ATS users by treatment staff in the compulsory isolation center. Individuals were approached by trained interviewers in a private room. Prior to commencement of the study, the trained interviewers explained the aim and content of this study and informed potential participants that they could decline to participate in the study without risk of compromising present or future medical care and without suffering a penalty or loss of benefits to which they were otherwise entitled. Also, participants were informed that they had the right to withdraw from the study at any time. After receiving a full explanation of the study and any potential risks and benefits of study participation, subjects provided written informed consent. The interviews took place in a private room of the compulsory isolation center. The average interview required 1 hour, and participants received a gift (about $6) for their time after the interview. In total, 389 individuals were approached, 12 of them were not enrolled because they did not understand the concept of consent, and 377 individuals completed the interview.
2.4. Statistical Analysis
A group-based trajectory model with SAS PROC TRAJ procedures (Jones, 2001) was applied to identify distinctive patterns of trajectories of ATS use from years 2005 to 2012. The repeated measures of days of using ATS drugs per month in each year from years 2005 to 2012 were analyzed with a censored normal model (i.e., minimum is 0 and maximum is 30). ATS use across years was established by a polynomial relationship as ATSijt=β0j+β1j*yearit+β2j*yearit2+εit, where i, j, t indicates subjects, trajectory group, and time, respectively, and εit is a disturbance normally distributed with a zero mean and a constant residual variance. The β0j, β1j, and β2j represent the intercept, linear, and quadratic parameters, which determined the shape of trajectory for group j. Variances of β0j , β1j, and β2j given each group j were constrained to zero. Subjects in each group have the same values on β0j , β1j, and β 2j . However, β0j , β1j, and β2j varied across groups. In addition, a probability of membership in each group was estimated for each subject. Probability of group membership was estimated in a multinomial distribution. Individuals were placed into their most likely group based upon the highest group probability of their trajectories. The modeling procedures were aimed to identify distinctive trajectory patterns among individuals and to examine individual differences among the identified trajectory groups (Jones and Nagin, 2007; Nagin, 1999; 2005). The number of distinctive trajectory groups was indicated by a latent class variable. The model was estimated by using a fixed number of groups. A series of models were fitted with an increasing number of trajectory groups. Goodness of model fit was evaluated with the Bayesian information Criterion (BIC; Schwartz, 1978). The best fitting model was chosen with a reasonably low absolute value of BIC and sufficient number of subjects in each group (e.g., 10% of total sample or more).
Based on the distinctive trajectory groups identified from the group-based trajectory modeling, differences in personal characteristics, physical and mental health, and risk behaviors among the identified trajectory groups were examined. The Chi-square tests for categorical variables (e.g., severity of alcohol use) and ANOVA (e.g., SAS PROC ANOVA) or multivariate analyses (e.g., SAS PROC GLM) for continuous variables (e.g., HCV-related knowledge) were conducted for these comparisons.
In addition to comparisons of various covariates among the identified trajectory groups, a multinomial logistic regression model (SAS PROC LOGISTIC) was developed to further examine the multivariate relationship of risk/protected factors with trajectory groups of ATS use. The analysis included demographics, drug use history, risky sexual behaviors, ATS-related treatment, and psychiatric symptoms as potential covariates and the ATS trajectory groups as the main outcome measure. Odds ratios of ATS-use trajectories, given the potential covariates, were estimated simultaneously.
3. RESULTS
3.1. Trajectories of ATS use from years 2005 to 2012
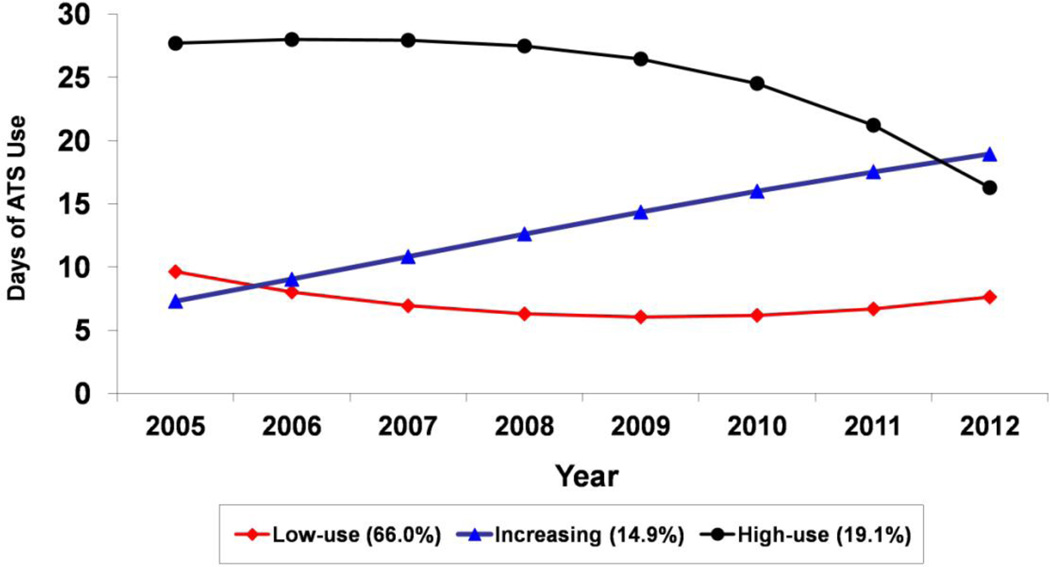
A series of group-based trajectory models, from a two- to six-trajectory pattern, were fitted to identify the optimal model. The BIC value increased from BIC=−6096.7 in the two-trajectory model to BIC=−6070.1 in the three-, BIC=−5991.9 in the four-, and BIC=−5980.8 in the five-trajectory model; the six-trajectory model did not converge after many attempts with various random starting values. The reasonably high BIC values in the five-, four-, and three-trajectory models indicate them as potential optimal models. However, the five- and four-trajectory models included a trajectory with a small subset of subjects (8.2%) and a non-interpretable curve. Consequently, the three-trajectory model was chosen as the best-fitting model. Figure 1 shows trajectories of estimated days of ATS use in a month of the three-trajectory model. About 19.1% of participants were classified in the persistent high-use group; these individuals remained at a high level of ATS use from year 2005 to 2012. Another 14.9% were classified in the increasing-use group, exhibiting an accelerating trajectory; these individuals reported a low level of ATS use in the initial year of 2005, but their level of ATS use increased significantly afterwards. The majority of individuals (66.0%) fell into the low-use group; these individuals remained at a low level of ATS use across the observed years.
Figure 1.
Trajectories of estimated days of ATS use in a month of the three-trajectory model.
3.2. Demographic and background characteristics of participants
In total, 377 participants completed baseline interviews. Overall, the sample was 81.1% male. The mean age of the sample was 35.5 years old (SD=7.8). About one-third (38.2%) of them were married or living as married, three-fourths of them had a middle school or lower level of education, and more than one-half (55.9%) were unemployed before admission. There were no significant differences in terms of general demographic characteristics by the ATS-use trajectory groups.
3.3. Drug-use histories and risky sexual behaviors by ATS use trajectory groups
The drug-use histories for all participants and by ATS use trajectory groups are presented in Table 2. The mean age of ATS drug initiation was 30.7 (7.9) years, and 82.1% of them had friends who used ATS drugs. More than half (58.7%) of them used drugs other than ATS drugs, including opiate-type drugs (54.0%), sleeping pills (1.3%), and other drugs (3.4%), but only 1.3% of them injected ATS drugs. Additionally, 15.5% of participants reported use of ATS drugs combined with other drugs. Approximately 65.5% of participants reported that they had craving experiences during the past year if they could not get ATS drugs, and the mean level of craving was 3.3 (SD=3.2). Based on the DSM-IV, 68.5% of them met the diagnosis of ATS dependence. More than four-fifths (84.6%) reportedly engaged in sexual behaviors after using ATS drugs, and 23.8% reported having had two or more sexual partners in the past year; 71.2% of those who had multiple sexual partners did not use condoms during sex.
Table 2.
Substance use history and sexual risk behaviors by ATS Use Trajectory Group
| Total (n=377) |
Low-use (n=249) |
Increasing-use (n=56) |
High-use (n=72) |
|
|---|---|---|---|---|
| Have friends use ATS, n (%) | 301(82.1) | 203(83.8) | 43(78.2) | 55(78.6) |
| Age of first ATS use, mean (SD) | 30.7(7.9) | 31.2(8.6) | 29.1(7.8) | 30.4(8.0) |
| Use other drugs besides ATS, n (%) |
222(58.7) | 136(54.6) | 36(64.3) | 50(69.4) |
| Opiate* | 204(54.0) | 122(48.9)a | 36(64.3)b | 46(63.9)b |
| Sleep pill | 5(1.3) | 4(1.6) | 0(0.0) | 1(1.4) |
| Others | 13(3.4) | 10(4.0) | 0(0.0) | 3(4.2) |
| Use ATS combined with other drugs, n(%) |
58(15.5) | 32(13.0) | 13(23.2) | 13(18.3) |
| Injected ATS, n(%) | 5(1.3) | 2(0.8) | 0(0.0) | 3(4.2) |
| AUDIT>=7, n(%) | 116(30.8) | 76(30.5) | 19(33.9) | 21(29.2) |
| Engage sexual behaviors after using ATS, n(%) |
318(84.6) | 210(84.7) | 46(82.1) | 62(86.1) |
| Multiple sexual partners during last year, n(%) |
74(23.8) | 44(21.4) | 12(26.1) | 18(30.5) |
| No Condom use during after using ATS among those with multiple sexual partners, n(%) |
47(71.2) | 25(64.1) | 9(81.8) | 13(81.3) |
| Craving for ATS during last year, n(%)** |
245(65.2) | 149(59.8)a | 42(75.0)b | 54(76.1)b |
| Level of craving for ATS, mean (SD) ** |
3.30(3.2) | 2.65(2.8)a | 4.29(3.1)b | 4.79(3.8)b |
| ATS dependence, n(%)** | 255(68.5) | 146(59.6)a | 47(83.9)b | 62(87.3)b |
| Months in treatment during 2005–2012, mean (SD)* | 14.1(14.7) | 14.6(15.9)a | 15.1(17.4)a | 8.9(9.8)b |
Chi-square test or ANOVA:
p<0.05 ;
p<0.01.
Pair-wise comparisons are indicated by superscripts a, b, and c. Values with different superscripts are significantly different, p<0.05.
The average number of months in drug-abuse treatment programs was 14.1 (14.7). History of opiate use, craving experiences for ATS drugs, months in drug-abuse treatment programs, and prevalence of ATS dependence were all significantly different by ATS use trajectory group. Relative to the low-use group, the increasing-use and high-use groups were more likely to report lifetime use of opiates and to have more craving experiences. The low-use and increasing-use groups stayed more months in drug-abuse treatment programs compared to the high-use group.
3.4. ATS-induced psychiatric symptoms by ATS use trajectory groups
The participants reported diverse psychiatric symptoms related to ATS use, including delusions (55.4%), hallucinations (59.2%), and thought disorders (46.4%). More than one-half (64.2%) of the participants reported having depressive symptoms, 17.0% reported suicidal ideation, and 11.4% reported suicide behaviors. While the prevalence of psychiatric symptoms among these participants was high, only 9.8% of them had sought treatment for psychiatric symptoms. Relative to the low-use group, more patients in the increasing-group and high-use group reported depressive symptoms and suicide behaviors.
3.5. Multinomial regression model of risk and protected factors by ATS use trajectory groups
Table 4 presents estimates of odds ratios of ATS use trajectory groups with the potential risk and protected factors considered simultaneously. Older participants, compared to younger participants, were more likely to belong to the increasing trajectory (OR=1.09). Participants who started ATS use at a younger age, relative to those who initiated ATS use at an older age, were more likely to exhibit an increasing ATS use trajectory (OR=3.47). In addition, level of craving for ATS drugs and ATS dependence were significant risk factors associated with higher levels of ATS use over time. Participants with ATS dependence, in contrast to those without ATS dependence, were more likely to belong to the increasing (OR=3.30) or the high (OR=3.57) ATS use trajectory. On the other hand, length of treatment is a significant protective factor to ATS use; participants with a longer period of treatment were less likely to be in the high ATS use trajectory group (OR=0.95). Additionally, participants who ever had suicide behavior were associated with a higher likelihood of being in the high ATS use trajectory group (OR=3.30).
Table 4.
Multinomial Logistic Regression Analysis of the Three ATS Trajectory Groups
| Odds Ration of Increasing vs. Low (95% Confidence Interval) |
Odds Ration of High vs. Low (95% Confidence Interval) |
|
|---|---|---|
| Demographics | ||
| Males (vs. Females) | 1.84 (0.75 – 4.52) | 2.02 (0.86 – 4.72) |
| Age at interview | 1.09 (1.02 – 1.16) * | 1.04 (0.97 – 1.10) |
| Married (vs. Not-Married) | 0.62 (0.31 – 1.23) | 0.58 (0.31 – 1.11) |
| High School or Higher (vs. Others) | 0.99 (0.49 – 2.01) | 0.72 (0.36 – 1.45) |
| ATS Use History | ||
| Friends use ATS (yes vs. no) | 0.64 (0.28 – 1,42) | 0.56 (0.26 – 1.21) |
| Age of first ATS use (before age 30 vs. after age 30) | 3.47 (1.31 – 9.20) * | 1.69 (0.67 – 4.25) |
| Level of Craving for ATS (0–10) | 1.10 (0.99 – 1.23) | 1.20 (1.08 – 1.32) ** |
| ATS Dependence (yes vs. no) | 3.30 (1.41 – 7.73) ** | 3.57 (1.59 – 8.04) ** |
| Months in treatment during 2005–2012 (0–78) | 0.99 (0.97 – 1.01) | 0.95 (0.93 – 0.98) ** |
| Risk Behaviors | ||
| Use other opiates (yes vs. no) | 1.33 (0.66 – 2.69) | 1.92 (0.97 – 3.83) |
| Severe alcohol use (AUDIT>=7) | 1.05 (0.53 – 2.10) | 0.68 (0.34 – 1.34) |
| Engaged sex after ATS use (yes vs. no) | 0.66 (0.26 – 1.67) | 0.94 (0.37 – 2.40) |
| Multiple sexual partners (yes vs. no) | 1.19 (0.52 – 2.71) | 1.42 (0.67 – 3.01) |
| ATS Psychiatry Symptoms | ||
| Depression (yes vs. no) | 1.14 (0.53 – 2.50) | 0.94 (0.44 – 1,98) |
| Suicide behavior (yes vs. no) | 2.12 (0.79 – 5.70) | 3.30 (1.35 – 8.06) ** |
| Treatment for the symptoms (yes vs. no) | 2.05 (0.76 – 5.51) | 0.69 (0.23 – 2.08) |
p<0.05;
p<0.01
4. DISCUSSION
Based on the group-based trajectory modeling results, the present study identified three groups with distinctive use trajectories of ATS drugs over 8 years among the sample while they were in the compulsory isolation detoxification center. A majority of participants (66%) used ATS drugs at a low level, but some participants used ATS drugs at a high level persistently (19.1%) or increased their use level to a high level over the years (14.9%). These last two groups are of particular concern because many of them demonstrated ATS dependence and associated psychiatric symptoms (depression, suicide ideation). Furthermore, all three groups, mostly in their mid 30s, were engaged in high-risk sexual behaviors following ATS use, which could put them at risk for infectious diseases such as HIV.
Opiate use was common among this sample. More than half of participants reported lifetime opiate use, and this rate was significantly higher among participants in the high-use and increasing-use groups than the low-use group. Effects of ATS drugs and opiates are different on the central nervous system, and it has been reported that ATS drugs and opiates are often co-abused to reduce negative effects (Williamson et al., 1997). Studies have also suggested that opiate users had a greater lifetime prevalence of drug-use disorders, including amphetamine use disorder, than drug users who did not use opiates (Inglez et al., 2008; Fairbairn et al., 2007; McKetin et al., 2008; Wu et al., 2011). Given the long history of opiate use in China and the Chinese government’s recent strict policy toward opiate use, it could be that more heroin users have switched to ATS drugs, which can partially explain the study finding. The current study, nevertheless, did not collect data that allow the determination of the timing and sequence of opiate use. Based on the literature, it is reasonable to expect that concomitant use of opiates and ATS drugs may increase the health risk more than using ATS drugs or opiates alone. Furthermore, there have been some recent reports indicating that MA users are beginning to inject drugs, increasing their HIV/HCV risks (Werd et al., 2013). While few participants in the present study reported ATS injection, given that many ATS users in China also have a history of opiate use (which is often administered by injection), the possibility of ATS drugs being injected in the future could be a problem that calls for close monitoring for timely prevention and intervention.
Other characteristics related to the distinctive trajectory patterns include sexual behaviors and ATS-related psychiatric symptoms. Individuals in the high-use and increasing-use groups were more likely to report sexual risk behaviors and psychiatric symptoms compared to the low-use group, although the sexual behavior differences were not significant. Consistent with previous studies (McKetin et al., 2006), psychiatric symptoms were common in this sample. The prevalence of depression, delusions, hallucinations, and thought disorders were 64.2%, 55.4%, 59.2%, and 46.4%, respectively, and suicidal thinking and suicide behaviors (17.0%, and 11.4%) were much higher than that reported in the general population in China (Micheal et al., 2009). This finding confirms previous research (Gold et al., 2009; McKetin et al., 2006) that found psychiatric symptoms are frequently associated with ATS use, and that increased ATS use may contribute to the exacerbation of depression or anxiety. In contrast, lower ATS use was associated with fewer depression symptoms. These findings highlight the importance of the association between psychiatric symptoms and ATS use trajectories.
In this study, few of the participants reported using ATS drugs by injection, and there were no reports of shared injection equipment. This result is similar to other studies reported in China, where the main route of ATS use is by smoking (Bao et al., 2012; Wang et al., 2008). However, sexual risk behavior was serious among this population, with almost one-quarter of them having multiple sexual partners after ATS use, and 72.5% of them reportedly not using condoms. Similar to a study by Colfax and colleagues (2005), the high-use and increasing-use groups had more risky sexual behaviors compared with the low-use group, but the differences were not significant. The findings of the study confirm that ATS use leads to unprotected sexual behaviors that pose a risk of transmitting HIV or other sexual transmitted diseases, especially among high- and increasing-level ATS users. ATS use can increase individuals' sexual desire and pleasure responses, weaken their self-control, and result in failure to use condoms. Self-efficacy and gender empowerment have been reported to be important factors that determine condom use among drug users (Gullette et al., 2009; Tony et al., 2010). The findings of this study provide clinical evidence that prevention and treatment need to target these behaviors and problems.
In China, drug users (both heroin and ATS users) mainly receive two kinds of drug treatment. One is compulsory rehabilitation treatment controlled by the judicial system, and the other is voluntary drug abuse treatment controlled by the health system. Compulsory rehabilitation treatment centers offered vocational training, various sports activities, and psychotherapy to change drug use behaviors. Voluntary drug abuse treatment provides antipsychotic and psychotherapy to those with severe psychotic symptoms. Given that ATS drugs are relatively new drugs of abuse in China, effective intervention programs targeting ATS abuse were limited. Nevertheless, our multinomial regression analyses provide support that treatment is a significant protective factor, with longer periods of treatment being associated with less likelihood of having a high ATS use trajectory. Obviously, greater treatment participation should be encouraged for those in need. Furthermore, our trajectory analysis not only identified the need for those at high-risk to be targeted for intervention, but also identified risk factors associated with distinctive trajectory patterns. Future development of improved intervention programs should take these risk factors into consideration.
We acknowledge a number of study limitations. First, trajectory data were based on retrospective self-report, which is subject to reporting bias. Second, the timing of opiate use and ATS use were not known, which limits the understanding of use patterns of these two drugs. Third, data on the presence of psychiatric symptoms following ATS use were collected but not the severity, duration, frequency, or diagnosis of such. The study also has limited data on risk factors; other biological and social factors related to the high risk of ATS use need to be examined in future studies. Finally, the sample is limited to those in the compulsory center, and therefore the study findings may not be generalizable to ATS users in the community. The ages of initiation of ATS use in the study sample were mostly the early 30s, which is in contrast to other studies that suggest ATS initiation typically occurs at a younger age (MPS, 2012). Nevertheless, other background characteristics such as marital status, education level, and employment status closely resemble those found in the general hospital and community populations in China. Future studies should replicate this study in other settings to increase the confidence of the present study findings.
Despite study limitations, to our best knowledge, this is the first study that has explored the characteristics of ATS users in accordance with long-term ATS use trajectories. It is an important addition to the literature on ATS use and related risk factors among Chinese ATS users. While the majority of these ATS users were using ATS drugs at a persistently low level, their ATS use has brought them to the attention of officials and their treatment in the Compulsory Isolation Center for Drug Rehabilitation. There were also groups with a persistently high level of ATS use or increasing level of ATS use who had increased likelihood of ATS dependence and associated psychiatric symptoms. These ATS users were in their mid-30s and many were engaged in risky sexual behaviors following ATS use. The high prevalence of lifetime opiate use also suggests an area requiring further research, as well as the need for potential interventions in the event of emergent drug injection behaviors.
Table 1.
Demographic Characteristics of Participants by ATS Use Trajectory Group
| Total (n=377) |
Low-use (n=249) |
Increasing-use (n=56) |
High-use (n=72) |
|
|---|---|---|---|---|
| Gender,n(%) | ||||
| Males | 305(81.1) | 198 (79.5) | 47 (83.9) | 61 (84.7) |
| Females | 71(18.9) | 51 (20.5) | 9 (16.1) | 11 (15.3) |
| Age, mean (SD) | 35.5 (7.8) | 35.3(8.3) | 36.1(6.8) | 35.9(6.9) |
| Age,n(%) | ||||
| 16–25 | 46(12.3) | 34(13.7) | 4(7.1) | 8(11.3) |
| 26–35 | 149(39.7) | 99(39.9) | 24(42.9) | 26(36.6) |
| 36–45 | 146(38.9) | 89(35.9) | 25(44.6) | 32(45.1) |
| 46–60 | 34 (9.1) | 26(10.5) | 3(5.4) | 5(7.0) |
| Marital status, n(%) | ||||
| Never married/Single | 127(33.8) | 78 (31.6) | 19 (33.9) | 30 (41.7) |
| Married /Living together | 143(38.1) | 101(40.9) | 18(32.1) | 24(33.3) |
| Divorced/ Separated | 105(28.0) | 68(27.5) | 19(33.9) | 18(25.0) |
| Education, n(%) | ||||
| Elementary school | 50(13.2) | 37(14.9) | 4(7.1) | 9(12.5) |
| Middle school | 222(58.9) | 141(56.7) | 36(64.3) | 45(62.5) |
| High school or above | 105(27.9) | 71(28.5) | 16(28.6) | 18(25.0) |
| Employment, n(%) | ||||
| Employed | 110(29.3) | 76(30.7) | 19(33.9) | 15(20.8) |
| Unemployed | 210(55.9) | 135(54.4) | 27(48.2) | 48(66.7) |
| Other/retired | 56(14.8) | 37(14.9) | 10(17.9) | 9(12.5) |
Table 3.
Psychiatry symptoms by ATS Use Trajectory Group
| Total (n=377) |
Low-use-d (n=249) |
Increasing-use (n=56) |
High-use (n=72) |
|
|---|---|---|---|---|
| Depressive , n(%)* | 240(64.2) | 147(59.5)a | 41(73.2)a,b | 52(73.2)b |
| delusion symptoms, n(%) | 209(55.4) | 133(53.4) | 33(58.9) | 43(59.7) |
| Hallucination symptoms, n(%) |
223(59.2) | 145(58.2) | 34(60.7) | 44(61.1) |
| Thought disorder, n(%) | 175(46.4) | 113(45.4) | 25(44.6) | 37(51.4) |
| Suicide ideation, n(%) | 64(17.0) | 36(14.5) | 11(19.6) | 17(23.6) |
| Suicide behavior, n(%)** | 43(11.4) | 17(6.8)a | 10(17.9)b | 16(22.2) b |
| Treatment for these symptoms, n(%) |
32 (9.8) | 17(8.1) | 9(18.4) | 6(9.4) |
| Outpatient treatment,n(%) | 18(5.6) | 9(4.3) | 5(10.2) | 4(6.3) |
| Inpatient treatment,n(%) | 14(4.2) | 8(3.8) | 4(8.2) | 2(3.1) |
Chi-square test or ANOVA:
p<0.05 ;
p<0.01.
Pair-wise comparisons are indicated by superscripts a, b, and c. Values with different superscripts are significantly different, p<0.05.
Highlights.
We explored long-term patterns of ATS use over 8 years prior to the admission to the Compulsory Isolation Center for Drug Rehabilitation in Shanghai, China.
We applied group-based trajectory modeling and identified three groups with distinctive ATS use trajectory patterns: high-use (19.1%), low-use (66.0%), and increasing-use (14.9%).
Compared to the low-use group, the high-use and increasing-use groups were more likely to have used opiate-type drugs, to have ATS craving experiences, and to report psychiatry symptoms following ATS use.
Acknowledgments
Role of funding source
Funding was provided by Natural Science Foundation of China (grant number: 81271468) and National Science & Technology Pillar Program during the Twelfth Five-year Plan Period (grant number: 2012BAI01B07) for the conduct of this research and preparation of the manuscript. Dr. Hser is also supported by a NIDA grant (P30DA016383). The funding agencies had no final role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All decisions taken by the investigators were unrestricted. Dr. Jiang Du was supported by National Institute on Drug Abuse DISCA award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Yih-Ing Hser &Min Zhao conceived of the design of the current study. David Huang performed the data analysis and interpretation. Jiang Du drafted the manuscript and Yih-Ing Hser revised it. Other authors collected data and reviewed the manuscript. All authors approved the final version of the paper for submission.
Conflicts of interest
Authors of the paper referenced above, have no financial and personal relationships with other people or organizations that could inappropriately influence (bias) this study.
REFERENCES
- Albertson TE, Derlet RW, Van Hoozen BE. Methamphetamine and the expanding complications of amphetamines. West. J. Med. 1999;170:214–219. [PMC free article] [PubMed] [Google Scholar]
- Babor TF, John C, Saunders JB, Maristela G. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. 2nd ed. Geneva: World Health Organization; 2001. [Google Scholar]
- Bao YP, Liu ZM, Lian Z, Li JH, Zhang RM, Zhang CB, Hao W, Wang XY, Zhao M, Jiang HF, Yan SY, Wang QL, Qu Z, Zhang HR, Wu P, Shi J, Lu L. Prevalence and correlates of HIV and HCV infection among amphetamine-type stimulant users in 6 provinces in China. J. AIDS. 2012;60:4384–4346. doi: 10.1097/QAI.0b013e31825694f2. [DOI] [PubMed] [Google Scholar]
- Chu TX, Levy JA. Injection drug use and HIV/AIDS transmission in China. Cell Res. 2005;15:865–869. doi: 10.1038/sj.cr.7290360. [DOI] [PubMed] [Google Scholar]
- Colfax G, Santos GM, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376:458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- Colfax G, Coates TJ, Husnik MJ, Huang YJ, Buchbinder S, Koblin B, Chesney M, Vittinghoff E. Longitudinal patterns of methamphetamine, popper(amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J. Urban Health. 2005;82 doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Mathers B, Guarinieri M, Panda S, Phillips B, Strathdee SA, Tyndall M, Wiessing L, Wodak A, Howard J. Meth/amphetamine use and associated HIV: implications for global policy and public health. Int. J. Drug Policy. 2010;21:347–358. doi: 10.1016/j.drugpo.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Fairbairn N, Kerr T, Buxton JA, Li K, Montaner JS, Wood E. Increasing use and associated harms of crystal methamphetamine injection in a Canadian setting. Drug Alcohol Depend. 2007;88:313–316. doi: 10.1016/j.drugalcdep.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, Rawson RA. Psychopathology in methamphetamine-dependent adults 3 years after treatment. Drug Alcohol Rev. 2010;29:12–20. doi: 10.1111/j.1465-3362.2009.00081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MS, Kobeissy FH, Wang KK, Merlo LJ, Bruijnzeel AW, Krasonov IN, Cadet JL. Methamphetamine- and trauma-induced brain injuries: comparative cellular and molecular neurobiological substrates. Biol. Psychiatry. 2009;66:118–127. doi: 10.1016/j.biopsych.2009.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gullette DL, Wright PB, Booth BM, Feldman Z, Stewart KE. Stages of change, decisional balance, and self-efficacy in condom use among rural African-American stimulant users. J. Assoc. Nurses AIDS Care. 2009;20:428–441. doi: 10.1016/j.jana.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: crystal methamphetamine drug use in relation to HIV transmission. J. Homosex. 2001;41:17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- Hser Y, Huang D, Brecht ML, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. J. Addict. Dis. 2008;27:13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Xie Y, Tao J, Su H, Wu W, Zou S, Zhang J, Zhang J, Zhang H, Yang X, Guo J, Tang W, Zhang F, Liu J, Liu L, Chen Y, Wen N, Kosten TR, Zhang XY. Gender differences in socio-demographic and clinical characteristics of methamphetamine inpatients in a Chinese population. Drug Alcohol Depend. 2013;130:94–100. doi: 10.1016/j.drugalcdep.2012.10.014. [DOI] [PubMed] [Google Scholar]
- Hser YI, Chang L, Wang GJ, Li M, Rawson R, Shoptaw S, Normand J, Tai B. Capacity building and collaborative research on cross-national studies in the Asian region. J. Food Drug Anal. 2013;21:117–122. doi: 10.1016/j.jfda.2013.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglez-Dias A, Hahn JA, Lum PJ, Evans J, Davidson P, Page-Shafer K. Trends in methamphetamine use in young injection drug users in San Francisco from 1998 to 2004: the UFO Study. Drug Alcohol Rev. 2008;27:286–291. doi: 10.1080/09595230801914784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociolog. Methods Res. 2001;29:374–394. [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol. Methods Res. 2007;35:542–571. [Google Scholar]
- Lee TS, Chen YP, Chang CW. Gender differences in the perceived self-efficacy of safer HIV practices among polydrug abusers in Taiwan. Compr. Psychiatry. 2010;52:763–768. doi: 10.1016/j.comppsych.2010.10.015. [DOI] [PubMed] [Google Scholar]
- Li B, Yu CS, Boquan Z, Xiao HZ, Xiao GZ. The test of audit in China. Chin. Ment. Health J. 2003;17:22–24. [Google Scholar]
- Li J, Zhang RM, Liu HJ. A preliminary study of methamphetamine use in Yunnan, China. AIDS Patient Care STDS. 2008;22:543–544. doi: 10.1089/apc.2007.0205. [DOI] [PubMed] [Google Scholar]
- McKetin R, Kelly E, McLaren J. Characteristics of treatment provided for amphetamine use in New South Wales, Australia. Drug Alcohol Rev. 2005;24:433–436. doi: 10.1080/09595230500290858. [DOI] [PubMed] [Google Scholar]
- McKetin R, Kelly E, McLaren J, Proudfoot H. Impaired physical health among methamphetamine users in comparison with the general population: the role of methamphetamine dependence and opioid use. Drug Alcohol Rev. 2008;27:482–489. doi: 10.1080/09595230801914776. [DOI] [PubMed] [Google Scholar]
- McKetin R, Mcalaaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006;101:1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- Mendelson J, Jones RT, Upton R, Jacob P. Methamphetamine and ethanol interactions in humans. Clin. Pharmacol. Ther. 1995;57:559–568. doi: 10.1016/0009-9236(95)90041-1. [DOI] [PubMed] [Google Scholar]
- Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West. J. Med. 1998;168:93–97. [PMC free article] [PubMed] [Google Scholar]
- MPS--The Ministry of Public Security of China. Annual Drug Abuse Report. Beijing: 2012. [Google Scholar]
- National Narcotics Control Commission. Annual report on drug control in China. Beijing: The Ministry of Public Security of People’s Republic of China; 2012. [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: a semiparametric group-based approach. Psychol. Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-Based Modeling Of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Phillips MR, Zhang JX, Shi QC, Song ZQ, Ding ZJ, Pang ST, Li XY. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001—05: an epidemiological survey. Lancet. 2009;373:2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- Sullivan GR, Wu Z. Rapid Scale up of harm reduction in China. Int. J. Drug Policy. 2007;18:118–128. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimension of a model. Ann. Stat. 1978;6:461–464. [Google Scholar]
- Si TM, Shu L, Dang WM. Evaluation of the reliability and validity of Chinese version of the Mini- International Neuropsychiatric Interview. Chin. Ment Health J. 2009;23:457–462. [Google Scholar]
- Sobell LC, Sobell MB. Measuring Alcohol Consumption. Totwa, NJ: Humana Press; 1992. Timeline Follow-Back: A Technique For Assessing Self-Reported Alcohol Consumption; pp. 41–72. [Google Scholar]
- UNODC--United Nations Office on Drug Use and Crime (UNODC) World Drug Report. Vienna: United Nations; 2009. [Google Scholar]
- UNODC--United Nations Office on Drug Use and Crime (UNODC) World Drug Report. Vienna: United Nations; 2011. [Google Scholar]
- UNODC--United Nations Office on Drug Use and Crime (UNODC) World Drug Report. Vienna: United Nations; 2013. [Google Scholar]
- Wang YF, Zhang YZ, Lian Z. EpidemIological characteristics of three new drugs of abuse in BeijIng. Chin. J. Drug Depend. 2008;17:445–454. [Google Scholar]
- Werb D, Kerr T, Buxton J, Shoveller J, Richardson C, Montaner J, Wood E. Crystal methamphetamine and initiation of injection drug use among street involved youth in a Canadian setting. CMAJ. 2013;185:1569–1575. doi: 10.1503/cmaj.130295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson S, Gossop M, Powis B, Griffiths P, Fountain J, Strang J. Adverse effects of stimulant drugs in a community sample of drug users. Drug Alcohol Depend. 1997;44:87–94. doi: 10.1016/s0376-8716(96)01324-5. [DOI] [PubMed] [Google Scholar]
- Wu Z, Sullivan GS, Wang Y, Rotheram-Borus JM, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369:679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Blazer DG. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Addict. Med. 2011;5:28–35. doi: 10.1097/ADM.0b013e3181e0364e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Lu C, Zhang J, Hu L, Song H, Li J, Kang L. Gender differences in abusers of amphetamine-type stimulants and ketamine in southwestern China. Addict. Behav. 2013;38:1424–1430. doi: 10.1016/j.addbeh.2012.06.024. [DOI] [PubMed] [Google Scholar]