Abstract
Background
Parental incarceration is associated with mental and physical health problems in children, yet little research directly tests mechanisms through which parental incarceration could imperil child health. We hypothesized that the incarceration of a woman or her romantic partner in the year before birth constituted an additional hardship for already-disadvantaged women, and that these additionally vulnerable women were less likely to engage in positive perinatal health behaviors important to infant and early childhood development.
Methods
We analyzed 2006-2010 data from the Pregnancy Risk Assessment and Monitoring System (PRAMS) to assess the association between incarceration in the year prior to the birth of a child and perinatal maternal hardships and behaviors.
Results
Women reporting incarceration of themselves or their partners in the year before birth of a child had 0.86 the odds (95% CI .78-.95) of beginning prenatal care in the first trimester compared to women not reporting incarceration. They were nearly twice as likely to report partner abuse and were significantly more likely to rely on WIC and/or Medicaid for assistance during pregnancy. These associations persist after controlling for socioeconomic measures and other stressors, including homelessness and job loss.
Conclusions
Incarceration of a woman or her partner in the year before birth is associated with higher odds of maternal hardship and poorer perinatal health behaviors. The unprecedented scale of incarceration in the U.S. simultaneously presents an underutilized public health opportunity and constitutes a social determinant of health that may contribute to disparities in early childhood development.
Keywords: Incarceration, maternal hardship, breastfeeding, prenatal care
INTRODUCTION
Concern is growing regarding the consequences of the unprecedentedly high levels of U.S. incarceration for family and population health. Prisoners largely come from disadvantaged backgrounds and communities, but the experience of incarceration may independently contribute to poor health outcomes and health behaviors rather than merely being a marker for disadvantage missed by more traditional population health measures. In order to consider the potential implications of incarceration for the health and wellbeing of infants, we analyzed the association between incarceration in the year prior to the birth of a child and perinatal hardships and behaviors using 2006-2010 data from the Pregnancy Risk Assessment and Monitoring System (PRAMS). We hypothesized that women exposed to incarceration (their own or partners’) in the year before birth were not only highly vulnerable but less likely to engage in perinatal health behaviors important to infant and early childhood development, even after accounting for coexisting adverse conditions.
BACKGROUND
The U.S. is experiencing what has been described as an epidemic of incarceration (1-3). Nearly 12 million people pass through jail annually and another 700,000 are released from prison each year (4, 5). Incarceration rates are partially a reflection of actual crime, but they also reflect inadequate availability of community-based mental health care (6-8) and drug treatment (9). Social scientists, advocates and practitioners have also argued that the criminal justice system has evolved as an instrument of racialized social control (1, 10-13). Incarceration rates are also inflated by the increased use since the 1980s of incarceration for minor and non-violent infractions such as missing a parole meeting or a payment on legal debt (14-16). Recidivism rates are high among people involved in the criminal justice system, with more than 40% of those released returning to state prison within three years (17). Thus for many, incarceration is not a one-time exposure but a cycle of “churning” between the community and correctional facilities.
People who pass through the criminal justice system have higher rates of unemployment, lower educational attainment, and worse health profiles than the general population (14, 18, 19). Although long-term health consequences are difficult to track – in part because so few population health datasets include incarceration history or incarcerated populations (20) – incarceration has been linked to increased risk of hypertension, asthma, and depression (21-24), along with social determinants of health like unemployment and homelessness (19, 25, 26). Evidence also suggests a strong association with the wellbeing of the prisoner’s family, including his/her children, partners, siblings, and even parents (27, 28). The incarceration of male relatives increases the risk of poor mental health for their mothers (27) and poor mental health, obesity, cardiovascular risk, self-reported health, and HIV risk for their wives or partners (29-32). The loss of family income is especially important (33, 34), as over half of incarcerated fathers provided primary financial support for their families (35); even where that is not the case, they may have been providing valuable services in kind, especially childcare (35, 36).
The removal of a parent may benefit children who are exposed to domestic violence, but the large number of people incarcerated for nonviolent offenses creates a net negative effect of parental incarceration (33, 34, 36-40). Because far more black than white children are at risk of parental incarceration, this experience may be one mechanism for ongoing racial disparities in childhood development and wellbeing, even if the individual-level effects of incarceration on blacks are no larger than the individual-level effects on whites (38, 41, 42). Parental incarceration is a marker of environmental risks like parental drug abuse (40), but is also a distinctive form of parental absence that has effects on child wellbeing separate from the behaviors that brought the parent to the attention of the criminal justice system. It may thus constitute a traumatic stressor beyond a distinct life event, beginning with the arrest itself if conducted in front of children (34, 35, 43).
The mechanisms at work appear to differ depending on whether a mother or father is incarcerated, however. Although the incarceration rate has grown more rapidly for women than for men in recent years, the vast majority of inmates are still male (4, 5), and 51-63% of men in state or federal prison have children (44). Studies identifying maternal or paternal incarceration, rather than parental incarceration in general, have found that while maternal incarceration is associated with children’s depressive symptoms (39), overall associations are inconclusive or null (45). By contrast, paternal incarceration is associated with a broader range of mental and physical health problems, including higher risk of abuse, homelessness, and drug use (39, 40, 46); increased aggressive, externalizing, and internalizing behaviors (37, 47); increased risk of obesity among daughters (48); and more deleterious health outcomes overall (40).
Because incarceration is especially prevalent among adults of childbearing age (14), it may also exert an important effect on both birth outcomes and early childhood development via reproductive and perinatal health behaviors (in addition to general maternal wellbeing during pregnancy). No research to date has linked parental incarceration to specific health behaviors directly affecting infant and early childhood development. Previous studies of PRAMS data addressing incarceration either clustered it with other life events in the year before delivery, or analyzed it without controlling for other important stressors (49-51), but they help to identify the pathways through which incarceration of the mother or her partner may influence pregnancy (e.g., through compromising available financial resources or increasing stress, both of which can adversely affect perinatal health) (51, 52). Examining specific perinatal health behaviors may provide further understanding of those pathways. We examined the association between exposure to incarceration in the year prior to delivery and both maternal disadvantage and perinatal health behaviors.
METHODS
The Centers for Disease Control and Prevention (CDC) coordinates with state Departments of Health to conduct an annual survey of women who have delivered infants. Currently 40 states and New York City participate, reflecting 78% of U.S. births (three states do not make their data available to the public) (53). Participating states conduct stratified, systematic sampling of women who are both residents of that state and delivered a live-born infant in that state, identified from birth certificates. Selected women are mailed a questionnaire two to six months following delivery, and nonresponders are contacted by telephone after three mailings. West Virginia and Washington excluded incarcerated women from their sample, but no other states reported doing so. PRAMS reports a 70% response rate threshold through 2006 and a 65% response rate threshold starting in 2007. We pooled all publicly-available data from 2006 to 2010 to create a larger sample size (200,226). The time period was chosen as not only the most recent years for which publicly-release data were available, but a period over which incarceration rates stabilized after several decades of rapid growth.
The explanatory variable was incarceration in the year before delivery, as measured by “My husband or partner or I went to jail.” We created two sets of outcome variables. Disadvantage was measured by (1) receipt of WIC during pregnancy; (2) payment for prenatal care or delivery by Medicaid; (3) whether the mother graduated from high school; (4) coexistence of other stressors; and (5) partner abuse before or during pregnancy. Perinatal health behaviors consisted of: (1) whether the respondent was trying to get pregnant at the time of conception; (2) whether the respondent was using any form of birth control at the time of conception if the pregnancy was unintended; (3) access of prenatal care in the first trimester; (4) whether the respondent had fewer than nine prenatal care visits over the course of the pregnancy; and (5) whether the infant had ever been breastfed.
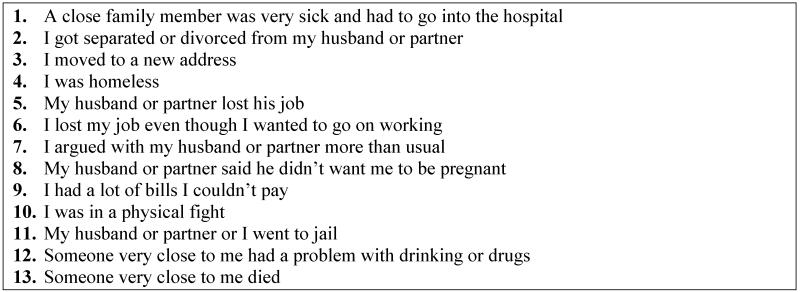
Control variables for most outcomes were race/ethnicity (non-Hispanic black, non-Hispanic white, Hispanic, all non-Hispanic others); age (17-19 years, 20-24, 25-29, 30-34, and 35 or older); educational level (8th grade or less completed; 9th-11th grade; high school degree; some college; BA or above); marital status (married vs. all other); and other stressors experienced in the year prior to delivery (see Figure 1). Other models have collapsed these variables into 4 categories of emotional, financial, partner-related, and traumatic stressors (49, 50) but we elected to include each stressor individually for greater precision. We tested and rejected models that added income and self-reported reception of WIC in the year before birth as measures of socioeconomic status, since results, including both covariates and measures of model fit, were virtually identical to models employing education but with a greater number of missing responses. Similarly we tested but rejected models that included dummy variables for state and year since they were virtually identical to the more parsimonious models and resulted in losing many additional degrees of freedom.
Figure 1.
Stressors during the 12 months before baby was born
Because Vermont did not release race/ethnicity variables, we dropped it from the dataset (n=5542). We then excluded 10,160 observations with invalid or missing data for the incarceration variable (n=2737) or any of the covariates, leaving a final sample of 184,424. The set of excluded observations were tested and found to be different from the final sample, but constituted only 4.7% of the population represented by the survey. Relative risk ratios were calculated for all outcomes using the binomial distribution with a log link in Stata 11 SE and using survey weights and strata information as provided by the CDC to account for complex sampling methodology. The study did not require IRB review as it utilized secondary data publicly available from the CDC.
RESULTS
Women who reported incarceration of themselves or their partners in the year prior to delivery were younger than other women (62.6% vs. 31.8% under 25 years old; Table 1). They also had lower educational attainment, lower income, and were less likely to be married (20.1% vs. 63.9%). They were more likely to experience other stressors during the same period and to have a greater number of stressors: Fully 25% of women reporting incarceration had six or more additional stressors, compared to only 2.8% of women reporting no incarceration.
Table 1.
Demographic characteristics of respondents (2006-2010), count and weighted percent
| No incarceration in 12 months before birth |
Self or partner incarcerated in 12 months before birth |
P value | |
|---|---|---|---|
| n= 175,394 (95.4%) | n=9130 (4.6%) | ||
| Age | p<.0001 | ||
| <=19 | 17,243 (9.2%) | 1918 (22.6%) | |
| 20-24 | 40,628 (22.6%) | 3611 (40%) | |
| 25-29 | 49,452 (29.1%) | 2101 (23%) | |
| 30-34 | 40,318 (24.4%) | 954 (9.5%) | |
| >=35 | 27,748 (14.7%) | 545 (4.9%) | |
| Race/ethnicity | p<.0001 | ||
| Black | 27,944 (13.9%) | 2665 (29%) | |
| Hispanic | 25,449 (16.7%) | 1030 (13.2%) | |
| White | 97,243 (62.2%) | 4185 (51.8%) | |
| Other | 24,758 (7.2%) | 1250 (6%) | |
| Education | p<.0001 | ||
| 8th grade or below | 6648 (4.4%) | 280 (3.5%) | |
| Grade 9-11 | 22,439 (12.4%) | 2477 (28.1%) | |
| HS degree | 49,770 (27.3%) | 3781 (41%) | |
| Some college | 43,725 (24.5%) | 2196 (22.9%) | |
| College degree | 52,812 (31.5%) | 396 (4.6%) | |
| Married | 110,603 (63.9%) | 2022 (20.1%) | p<.0001 |
| Previous births | 18,619 (10.2%) | 1383 (13.1%) | p<.0001 |
|
Other stresses in 12 months
before birth |
|||
| Divorce/separation | 13,276 (7%) | 3061 (31.9%) | p<.0001 |
| Moved | 60,239 (33%) | 5531 (59.8%) | p<.0001 |
| Homeless | 5265 (3%) | 1572 (15.3%) | p<.0001 |
| Partner lost job | 20,923 (12.1%) | 3003 (32.8%) | p<.0001 |
| Lost own job | 16,909 (9.4%) | 2331 (24.5%) | p<.0001 |
| Argued with partner more than usual |
42,734 (23.4%) | 5586 (59.7%) | p<.0001 |
| Partner didn’t want pregnancy | 13,491 (7.5%) | 1996 (21.1%) | p<.0001 |
| Couldn’t pay bills | 38,735 (21.1%) | 4687 (50.6%) | p<.0001 |
| Physical fight | 5519 (2.8%) | 2487 (25.7%) | p<.0001 |
| Someone close had substance problem |
20,117 (10.5%) | 4641 (49%) | p<.0001 |
| Someone close hospitalized | 40,750 (22.9%) | 3114 (34.3%) | p<.0001 |
| Someone close died | 30,707 (16.6%) | 2735 (28.2%) | p<.0001 |
| Total number of stresses aside from incarceration |
p<.0001 | ||
| 0 | 58,831 (35%) | 333 (4.1%) | |
| 1-2 | 76,610 (43.6%) | 2123 (24.9%) | |
| 3-5 | 34,518 (18.7%) | 4200 (46%) | |
| 6-11 | 5435 (2.8%) | 2474 (25%) |
A higher percentage of women reporting incarceration also reported an unintended pregnancy, receipt of WIC during pregnancy, and payment of prenatal care and/or delivery by Medicaid (Table 2). Women reporting incarceration also reported lower usage rates of birth control at both time of conception and time of response; lower rates of initiating prenatal care in the first trimester (65.6% compared to 81% of women not reporting incarceration); and lower rates of any breastfeeding (64.4% vs. 79.1%). They also experienced significantly higher rates of partner abuse both before (21.4% vs. 2.7%) and during (17% vs. 2.1%) pregnancy.
Table 2.
Count and weighted percent of outcomes by incarceration history, 2006-2010
| No incarceration in 12 months before birth |
Self or partner incarcerated in 12 months before birth |
p-value | |
|---|---|---|---|
| On WIC during pregnancy | 79,324 (43%) | 7094 (77.4%) | p<.0001 |
| Prenatal care paid by Medicaid | 71,123 (38.9%) | 7016 (77.2%) | p<.0001 |
| Delivery paid by Medicaid | 78,093 (42.7%) | 7411 (79.9%) | p<.0001 |
| Partner abuse before pregnancy | 5040 (2.7%) | 2122 (21.4%) | p<.0001 |
| Partner abuse during pregnancy | 3841 (2.1%) | 1660 (17%) | p<.0001 |
| Trying to get pregnant at time of conception |
85,217 (50%) | 2211 (24.1%) | p<.0001 |
| Using birth control when conceiveda |
40,154 (46.4%) | 2426 (36.9%) | p<.0001 |
| Prenatal care commenced first trimester |
138,615 (81%) | 5893 (65.6%) | p<.0001 |
| 9 or more prenatal care visits | 129,055 (81.1%) | 5695 (70.7%) | p<.0001 |
| Ever breastfed | 135,892 (79.1%) | 5718 (64.4%) | p<.0001 |
Asked of respondents who were not trying to get pregnant at time of conception
To isolate the association of incarceration relative to the other stressors, Table 3 presents two models. A comparison of Model 1 and Model 2 shows that only some of the association is due to other stressors; even after controlling for these stressors, all but one outcome remains significant in Model 2. Women reporting incarceration were not more likely to have unintended pregnancies than other respondents, but they were less likely to use birth control if the pregnancy was unintentional (Relative risk ratio [RRR] .70, 95% CI .68-.77), begin prenatal care in the first trimester (RRR .89, 95% CI .81-.98), or have breastfed since delivery. They were more likely to have had fewer than nine prenatal visits, experience partner abuse before and during pregnancy, and receive WIC and/or Medicaid during their pregnancy and delivery. They were also more likely to experience most of the other stressors (Table 4).
Table 3.
Adjusted relative risk ratios of women reporting self/partner incarceration in the year before birth compared to women who did not, 2006-2010
| Model 1a | Model 2b | |
|---|---|---|
| On WIC during pregnancy | 1.61 (1.44-1.80) | 1.20 (1.07-1.35) |
| Prenatal care paid by Medicaid | 1.90 (1.70-2.12) | 1.33 (1.18-1.49) |
| Delivery paid by Medicaid | 1.85 (1.65-2.08) | 1.29 (1.15-1.46) |
| Partner abuse before pregnancy | 5.78 (5.16-6.46) | 1.87 (1.63-2.15) |
| Partner abuse during pregnancy | 5.71 (5.04-6.47) | 1.75 (1.50-2.04) |
| Trying to get pregnant at conception | .76 (.68-.84) | 1.01 (.91-1.13) |
| Using birth control when conceived (of those not trying to get pregnant) |
.69 (.63-.76) | .70 (.63-.77) |
| Prenatal care commenced first trimester |
.79 (.72-.86) | .89 (.81-.98) |
| Nine or more prenatal care visits | .78 (.72-.86) | .85 (.77-.94) |
| Ever breastfed | .87 (.80-.95) | .86 (.78-.94) |
Controlled for age, race/ethnicity, education, marital status, and previous children. Boldface denotes statistical significance.
Controlled for Model 1 measures and other stressors (see Figure 1)
Table 4.
Adjusted odds ratios of other stressors for women reporting self/partner incarceration in 12 months before delivery
| Other stressor | |
| Separated/divorced | 1.72 (1.54-1.93) |
| Moved | 1.26 (1.15-1.38) |
| Homeless | 1.88 (1.62-2.17) |
| Partner lost job | 1.44 (1.30-1.59) |
| I lost job | 1.08 (.97-1.21) |
| Argued with partner more than usual | 1.35 (1.22-1.50) |
| Partner didn’t want pregnancy | .86 (.76-.97) |
| Couldn’t pay bills | 1.31 (1.18-1.46) |
| Got in physical fight | 2.94 (2.60-3.32) |
| Someone close had a substance problem |
3.17 (2.88-3.49) |
| Close family hospitalized | 1.04 (.94-1.15) |
| Someone close died | 1.02 (.91-1.14) |
Controlled for age, race/ethnicity, education, marital status, and other stressors. Boldface denotes statistical significance.
DISCUSSION
Incarceration of a mother or her partner in the 12 months prior to delivery is associated with increased risk of maternal hardship and behaviors in turn associated with problems in early childhood development. Without claiming to provide evidence of a causal relationship, this finding suggests that incarceration is an important framework for public health interventions. At the same time, our findings add weight to growing evidence that the unprecedented scale of incarceration in the U.S. constitutes a social determinant of health in and of itself that may be contributing to disparities in early childhood development. These findings indicate that incarceration operates as a stratifying institution not only generally (54, 55) but at the perinatal stage more specifically.
Studies of the relatively small number of births during incarceration have yielded contradictory conclusions about whether incarceration during pregnancy improves birth outcomes (56-58). Women who are incarcerated have high rates of substance dependence, STIs, and other health problems that can complicate neonatal health (59-62). For this population, incarceration may constitute a period of relative stability and improved access to prenatal care that can improve birth outcomes (56, 63, 64), although one study found improvement only among white women (64). Although the dataset does not allow identification of whether the mother herself or her partner was incarcerated, it is safe to assume that in the vast majority of cases women are reporting on their husband/partner’s incarceration rather than their own. The number of incarcerated women in the U.S. increased steadily from 2000 to 2010 (65) but men still constitute about 90% of all inmates. Our results supplement previous findings that men’s incarceration has adverse consequences for not only their children’s wellbeing as described above, but the wellbeing and health behaviors of their female partners as well (28, 29, 32, 66). Thus, even male incarceration may present a public health opportunity to target interventions aimed at maternal disadvantage and perinatal behaviors that influence infant and early childhood development. At the same time, the possibility of a causal relationship between incarceration and maternal disadvantage means that it will be critical for policymakers to support alternatives to incarceration (e.g. for offenses like nonpayment of fines) to reduce these disparities in perinatal disadvantage and associated risk of poor health behaviors. We point to three of our findings in particular as bases for more specific recommendations.
First, women reporting incarceration in the year before delivering are at increased risk for multiple measures of disadvantage. They are at higher risk of most other stressors in the PRAMS data and are also more likely to be unmarried, without a high school degree, and subject to partner abuse before and during pregnancy. Women reporting incarceration are also 20-33% more likely to need public assistance in the form of WIC and Medicaid than other women. Adding this need to the already-massive price tag of incarceration might be influential with policymakers who are already increasingly concerned with the prominence of correctional expenses in state/local budgets and prompt them to invest in alternatives to incarceration such as drug courts.
Second, while many perinatal health behaviors were associated with incarceration, reproductive intentionality was a noteworthy exception. Likewise, the only stressor for which women reporting incarceration had lower odds was whether the partner did not want the pregnancy (Table 4). However, this finding may reflect a greater lack of engagement on the part of women’s partners rather than greater enthusiasm for the pregnancy, and among women who were not trying to get pregnant, women experiencing incarceration were less likely to be using birth control. Although we cannot know the relative timing of incarceration and conception for these respondents, family planning interventions targeting not only female but also male inmates may be effective preparation for post-release sex and reproductive intentionality. Correctional facilities present an especially important opportunity given high rates of recidivism, meaning that incarceration is not a one-time exposure for many couples. Clarke et al. found that 45% of women who conceived between incarceration episodes did so within 90 days of release, indicating the need for interventions prior to release (67).
Finally, our findings point to specific populations in need of targeted interventions regarding timely and adequate prenatal care and breastfeeding, both of which are critical to infant and early childhood development. Women reporting incarceration were not less likely to say that healthcare workers spoke to them about these and other perinatal health behaviors (data not shown), but our data suggest that incarceration history marks a high-risk population that may benefit from intensified attention by healthcare workers to improve their rates of prenatal care and breastfeeding. Outreach to incarcerated husbands/partners is unlikely to be efficacious in this case, but public health departments could work with correctional facilities to target visiting hours as a means of disseminating information about prenatal care and other perinatal health behaviors. Despite the stigma associated with incarceration (34, 68) health care providers might also use it as an indicator of patients at additional risk for disadvantage and need.
The study is subject to several limitations. Most importantly, we were unable to isolate the extent to which the association between incarceration, maternal hardship, and perinatal health behaviors was due to the mother’s own incarceration versus her partner’s. Given the high rate of co-occurrence between drug use, incarceration, and the outcomes of interest, a serious limitation is that we are unable to control for maternal drug use, which PRAMS does not ask about. In a similar vein, since our analysis relies on cross-sectional data, we are unable to make strong claims about whether incarceration causes the poor outcomes of these women and, presumably, their children, or is merely associated with it. We were also unable to determine whether the length of the incarceration episode or how long ago it occurred is significant. It is also possible that some respondents took the wording of the question (whether either parent “went to jail”) literally, and did not include incarceration in prison, thereby underestimating the true burden of incarceration.
CONCLUSION
The mechanisms linking parental incarceration to child wellbeing have become somewhat more transparent, but research to date has not linked parental incarceration to specific parental health behaviors known to directly affect child health. We show that incarceration of a woman or her partner in the year before birth is associated with higher odds of maternal hardship and perinatal health behaviors associated with poorer infant and early childhood development. This association persists after controlling for socioeconomic measures and other stressors, including homelessness and job loss. Although interest is growing in the U.S. to find alternatives to incarceration for nonviolent and minor offenses, for the foreseeable future correctional facilities provide a repeated opportunity to interrupt cycles of disadvantage and adverse health behaviors affecting infant and childhood wellbeing. Involvement of either the woman or her partner in the criminal justice system can be utilized by public health practitioners as a focus for targeting interventions to high-risk populations.
ACKNOWLEDGMENTS
Jennifer G. Clarke is supported by NICHHD R01 HD054890 and Pamela A. Valera is supported by NCI K01CA154861. The authors wish to acknowledge Rachel Cain of the Rhode Island Department of Health Center for Health Data and Analysis and the CDC PRAMS Working Group: Izza Afgan, MPH (AL), Kathy Perham-Hester, MS, MPH (AK), Mary McGehee, PhD (AR), Alyson Shupe, PhD (CO), Jennifer Morin,MPH (CT), George Yocher, MS (DE), Avalon Adams-Thames, MPH, CHES (FL), Chinelo Ogbuanu, MD, MPH, PhD (GA), Emily Roberson, MPH (HI), Theresa Sandidge, MA (IL), Sarah Mauch, MPH (IA), Amy Zapata, MPH (LA), Tom Patenaude, MPH (ME), Diana Cheng, MD (MD), Emily Lu, MPH (MA), Cristin Larder, MS (MI), Judy Punyko, PhD, MPH (MN), Brenda Hughes, MPPA (MS), Venkata Garikapaty, MSc, MS, PhD, MPH (MO), JoAnn Dotson (MT), Brenda Coufal (NE), David J. Laflamme, PhD, MPH (NH), Lakota Kruse, MD (NJ), Eirian Coronado, MPH (NM), Anne Radigan-Garcia (NY), Candace Mulready-Ward, MPH (New York City), Kathleen Jones-Vessey, MS (NC), Sandra Anseth (ND), Connie Geidenberger PhD (OH), Alicia Lincoln, MSW, MSPH (OK), Kenneth Rosenberg, MD, MPH (OR), Tony Norwood (PA), Sam Viner-Brown, PhD (RI), Mike Smith, MSPH (SC), Rochelle Kingsley, MPH (TX), David Law, PhD (TN), Lynsey Gammon, MPH (UT), Peggy Brozicevic (VT), Marilyn Wenner (VA), Linda Lohdefinck (WA), Melissa Baker, MA (WV), Katherine Kvale, PhD (WI), Amy Spieker, MPH (WY), CDC PRAMS Team, Applied Sciences Branch, Division of Reproductive Health.
Contributor Information
Dora M. Dumont, Rhode Island Department of Health, At the time work was completed: The Miriam Hospital, Providence, RI.
Christopher Wildeman, Yale University, New Haven, CT, christopher.wildeman@yale.edu.
Hedwig Lee, University of Washington, Seattle, WA, hedylee@u.washington.edu.
Annie Gjelsvik, Brown University, Providence, RI; 2. Hasbro Children’s Hospital, Providence, RI, annie_gjelsvik@brown.edu.
Pamela A. Valera, Columbia University Mailman School of Public Health, New York, NY, pv2155@columbia.edu.
Jennifer G. Clarke, Memorial Hospital of Rhode Island, Pawtucket, RI; 2. Brown University, Providence, RI, jennifer_clarke@brown.edu.
REFERENCES
- 1.Drucker E. A plague of prisons: the epidemiology of mass incarceration in America. The New Press; New York: 2011. [Google Scholar]
- 2.Rich JD, Wakeman SE, Dickman SL. Medicine and the epidemic of incarceration in the United States. New England Journal of Medicine. 2011;364(22):2081–3. doi: 10.1056/NEJMp1102385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine and National Research Council . Health and Incarceration: A Workshop Summary. National Academies Press; Washington, D.C.: 2013. [PubMed] [Google Scholar]
- 4.Carson A, Sabol W. Prisoners in 2011. U.S. Department of Justice, Bureau of Justice Statistics; Washington, D.C.: 2012. [Google Scholar]
- 5.Minton T. Jail inmates at midyear 2011 - statistical tables. Bureau of Justice Statistics; Washington, D.C.: 2012. [Google Scholar]
- 6.Baillargeon J, Hoge SK, Penn JV. Addressing the challenge of community reentry among released inmates with serious mental illness. Am J Community Psychol. 2010;46(3-4):361–75. doi: 10.1007/s10464-010-9345-6. [DOI] [PubMed] [Google Scholar]
- 7.Lamb HR, Weinberger LE. The shift of psychiatric inpatient care from hospitals to jails and prisons. J Am Acad Psychiatry Law. 2005;33(4):529–34. [PubMed] [Google Scholar]
- 8.Yoon J. Effect of increased private share of inpatient psychiatric resources on jail population growth: evidence from the United States. Soc Sci Med. 2011;72(4):447–55. doi: 10.1016/j.socscimed.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009;301(2):183–90. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander M. The new Jim Crow: mass incarceration in the age of colorblindness. The New Press; New York: 2010. [Google Scholar]
- 11.Dumont DM, Allen SA, Brockmann BW, Alexander NE, Rich JD. Incarceration, community health, and racial disparities. J Health Care Poor Underserved. 2013;24(1):78–88. doi: 10.1353/hpu.2013.0000. [DOI] [PubMed] [Google Scholar]
- 12.Wacquant L. Deadly symbiosis: When ghetto and prison meet and mesh. Punishment Soc. 2001;3(1):95–133. [Google Scholar]
- 13.Wacquant L. Class, race & hyperincarceration in revanchist America. Daedalus. 2010;139(3):74–90. [Google Scholar]
- 14.Collateral costs: incarceration’s effect on economic mobility. Pew Charitable Trusts; Washington, D.C.: 2010. [Google Scholar]
- 15.Gottschalk M. The past, present, and future of mass incarceration in the United States. Criminology and Public Policy. 2011;10(3):483–503. [Google Scholar]
- 16.Harris A, Evans H, Beckett K. Drawing blood from stones: legal debt and social inequality in the contemporary United States. Am J Soc. 2010;115(6):1753–1798. [Google Scholar]
- 17.State of Recidivism: The Revolving Door of America’s Prisons. The Pew Charitable Trusts; Washington, D.C.: 2011. States PCot. [Google Scholar]
- 18.Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. Journal of Epidemiology and Community Health. 2009;63(11):912–9. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- 19.Pager D, Western B, Bonikowski B. Discrimination in a low-wage labor market: a field experiment. American Sociology Review. 2009;74(5):777–799. doi: 10.1177/000312240907400505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahalt C, Binswanger IA, Steinman M, Tulsky J, Williams BA. Confined to ignorance: the absence of prisoner information from nationally representative health data sets. Journal of General Internal Medicine. 2012;27(2):160–6. doi: 10.1007/s11606-011-1858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turney K, Lee H, Comfort M. Discrimination and Psychological Distress Among Recently Released Male Prisoners. Am J Mens Health. 2013 doi: 10.1177/1557988313484056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang EA, Green J. Incarceration as a key variable in racial disparities of asthma prevalence. BMC Public Health. 2010;10:290. doi: 10.1186/1471-2458-10-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang EA, Pletcher M, Lin F, Vittinghoff E, Kertesz SG, Kiefe CI, et al. Incarceration, incident hypertension, and access to health care: findings from the coronary artery risk development in young adults (CARDIA) study. Arch Intern Med. 2009;169(7):687–93. doi: 10.1001/archinternmed.2009.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schnittker J, Massoglia M, Uggen C. Out and down: incarceration and psychiatric disorders. J Health Soc Behav. 2012;53(4):448–64. doi: 10.1177/0022146512453928. [DOI] [PubMed] [Google Scholar]
- 25.London A, Myers N. Race, incarceration, and health: a life-course approach. Research on Aging. 2006;28(3):409–422. [Google Scholar]
- 26.Pager D, Western B, Sugie N. Sequencing disadvantage: barriers to employment facing young black and white men with criminal records. Ann Am Polit Sci Soc. 2009;623:195–210. doi: 10.1177/0002716208330793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green KM, Ensminger ME, Robertson J, Juon HS. Impact of adult sons’ incarceration on African American mothers’ psychological distress. J Marriage Fam. 2006;68:430–441. doi: 10.1111/j.1741-3737.2006.00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H, Wildeman C. Things fall apart: health consequences of mass imprisonment for African American women. Review of Black Political Economy. 2011:1–14. [Google Scholar]
- 29.Lee H, Wildeman C. A heavy burden? the cardiovascular health consequences of having a family member incarcerated. Am J Public Health. 2013 doi: 10.2105/AJPH.2013.301504. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grinstead OA, Faigeles B, Comfort M, Seal D, Nealey-Moore J, Belcher L, et al. HIV, STD, and hepatitis risk to primary female partners of men being released from prison. Women Health. 2005;41(2):63–80. doi: 10.1300/J013v41n02_05. [DOI] [PubMed] [Google Scholar]
- 31.Grinstead Reznick O, Comfort M, McCartney K, Neilands TB. Effectiveness of an HIV prevention program for women visiting their incarcerated partners: the HOME Project. AIDS Behav. 2011;15(2):365–75. doi: 10.1007/s10461-010-9770-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wildeman C, Schnittker J, Turney K. Despair by association? The mental health of mothers with children by recently incarcerated fathers. Am Soc Rev. 2012;77(2):216–243. [Google Scholar]
- 33.Geller A, Garfinkel I, Cooper CE, Mincy RB. Parental incarceration and child wellbeing: implications for urban families. Social Science Quarterly. 2009;90(5):1186–1202. doi: 10.1111/j.1540-6237.2009.00653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray J, Farrington DP, Sekol I. Children’s antisocial behavior, mental health, drug use, and educational performance after parental incarceration: a systematic review and meta-analysis. Psychological Bulletin. 2012;138(2):175–210. doi: 10.1037/a0026407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sugie N. Punishment and welfare: paternal incarceration and families’ receipt of public assistance. Soc Forces. 2012;90(4):1403–1427. doi: 10.1093/sf/sos055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartz-Soicher O, Geller A, Garfinkel I. The effect of paternal incarceration on material hardship. Soc Service Rev. 2011;85(3):447–473. doi: 10.1086/661925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wakefield S, Wildeman C. Mass imprisonment and racial disparities in childhood behavioral problems. Criminology Public Policy. 2011;10(3):793–817. [Google Scholar]
- 38.Pager D, Western B, Bonikowski B. Discrimination in a low-wage labor market: a field experiment. Am Sociol Rev. 2009;74(5):777–799. doi: 10.1177/000312240907400505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Foster HW. Maternal and paternal imprisonment in the stress process. Soc Sci Res. 2013;42:650–669. doi: 10.1016/j.ssresearch.2013.01.008. J. H. [DOI] [PubMed] [Google Scholar]
- 40.Lee RD, Fang X, Luo F. The impact of parental incarceration on the physical and mental health of young adults. Pediatrics. 2013;131(4):e1188–95. doi: 10.1542/peds.2012-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wakefield S, Wildeman C. Mass imprisonment and racial disparities in childhood behavioral problems. American Society of Criminology. 2011;10(3):793–817. [Google Scholar]
- 42.Wildeman C. Parental incarceration, the prison boom, and the concentration of childhood disadvantage. Demography. 2009;46(2):265–280. doi: 10.1353/dem.0.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Comfort M. Punishment beyond the legal offender. Annual Rev Law Soc Sci. 2007;3:271–296. [Google Scholar]
- 44.Glaze LE, Maruschak LM. Parents in prison and their minor children. U.S. Dept. of Justice, Office of Justice Programs, Bureau of Justice Statistics; Washington, DC: 2008. [Google Scholar]
- 45.Wildeman C, Turney K. Positive, negative, or null? the effects of maternal incarceration on children’s behavioral problems. Woodrow Wilson School of Public and International Affairs, Yale University; Princeton, NJ: 2012. [Google Scholar]
- 46.Foster HW, Hagan J. Incarceration and intergenerational social exclusion. Soc Problems. 2007;54(4):399–433. [Google Scholar]
- 47.Wildeman C, Western B. Incarceration in fragile families. Future of Children. 2010;20(2):157–77. doi: 10.1353/foc.2010.0006. [DOI] [PubMed] [Google Scholar]
- 48.Roettger ME. Paternal incarceration and trajectories of marijuana and other illegal drug use from adolescence into young adulthood: evidence from longitudinal panels of males and females in the United States. Addiction (Abingdon, England) 2011;106(1):121. doi: 10.1111/j.1360-0443.2010.03110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.LaCoursiere DY, Hirst KP, Barrett-Connor E. Depression and pregnancy stressors affect the association between abuse and postpartum depression. Maternal and Child Health Journal. 2012;16(4):929–35. doi: 10.1007/s10995-011-0816-7. [DOI] [PubMed] [Google Scholar]
- 50.Lu MC, Chen B. Racial and ethnic disparities in preterm birth: the role of stressful life events. American Journal of Obstetrics & Gynecology. 2004;191(3):691–9. doi: 10.1016/j.ajog.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 51.Wildeman C. Imprisonment and infant mortality. Social Problems. 2012;59(2):228–257. [Google Scholar]
- 52.Braveman P, Marchi K, Egerter S, Kim S, Metzler M, Stancil T, et al. Poverty, near-poverty, and hardship around the time of pregnancy. Maternal and Child Health Journal. 2010;14(1):20–35. doi: 10.1007/s10995-008-0427-0. [DOI] [PubMed] [Google Scholar]
- 53.CDC . Participating PRAMS states. Centers for Disease Control and Prevention; Atlanta, GA: 2012. [Google Scholar]
- 54.Massoglia M, Warner C. The consequences of incarceration: challenges for scientifically informed and policy-relevant research. Criminology Public Policy. 2011;10(3):851–863. [Google Scholar]
- 55.Wakefield S, Uggen C. Incarceration and stratification. Annual Review of Sociology Ann Rev Sociol. 2010;36:387–406. [Google Scholar]
- 56.Bell JF, Zimmerman FJ, Cawthon ML, Huebner CE, Ward DH, Schroeder CA. Jail incarceration and birth outcomes. Journal of Urban Health. 2004;81(4):630–44. doi: 10.1093/jurban/jth146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Howard DL, Strobino D, Sherman SG, Crum RM. Timing of incarceration during pregnancy and birth outcomes: exploring racial differences. Matern Child Health J. 2009;13(4):457–66. doi: 10.1007/s10995-008-0376-7. [DOI] [PubMed] [Google Scholar]
- 58.Knight M, Plugge E. The outcomes of pregnancy among imprisoned women: a systematic review. BJOG. 2005;112(11):1467–74. doi: 10.1111/j.1471-0528.2005.00749.x. [DOI] [PubMed] [Google Scholar]
- 59.Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. Am J Public Health. 2010;100(3):476–82. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hammett TM, Drachman-Jones A. HIV/AIDS, sexually transmitted diseases, and incarceration among women: national and southern perspectives. Sexually Transmitted Diseases. 2006;33(7 Suppl):S17–22. doi: 10.1097/01.olq.0000218852.83584.7f. [DOI] [PubMed] [Google Scholar]
- 61.Lewis C. Treating incarcerated women: gender matters. Psychiatric Clinics of North America. 2006;29(3):773–89. doi: 10.1016/j.psc.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 62.Nijhawan AE, Salloway R, Nunn AS, Poshkus M, Clarke JG. Preventive healthcare for underserved women: results of a prison survey. Journal of Women’s Health. 2010;19(1):17–22. doi: 10.1089/jwh.2009.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Clarke JG, Adashi EY. Perinatal care for incarcerated patients: a 25-year-old woman pregnant in jail. JAMA. 2011;305(9):923–9. doi: 10.1001/jama.2011.125. [DOI] [PubMed] [Google Scholar]
- 64.Howard DL, Strobino D, Sherman SG, Crum RM. Timing of incarceration during pregnancy and birth outcomes: exploring racial differences. Maternal and Child Health Journal. 2009;13(4):457–66. doi: 10.1007/s10995-008-0376-7. [DOI] [PubMed] [Google Scholar]
- 65.Guerino P, Harrison P, Sabol W. Prisoners in 2010 (revised) U.S. Department of Justice, Bureau of Justice Statistics; Washington, D.C.: 2011. Report No.: NCJ 236096. [Google Scholar]
- 66.Wildeman C, Lee H, Comfort M. A new vulnerable population? The health of female partners of men recently released from prison. Womens Health Issues. 2013;23(6):e335–40. doi: 10.1016/j.whi.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Clarke JG, Phipps M, Tong I, Rose J, Gold M. Timing of conception for pregnant women returning to jail. Journal of Correctional Health Care. 2010;16(2):133–8. doi: 10.1177/1078345809356533. [DOI] [PubMed] [Google Scholar]
- 68.Schnittker J, John A. Enduring stigma: the long-term effects of incarceration on health. Journal of Health and Social Behavior. 2007;48(2):115–30. doi: 10.1177/002214650704800202. [DOI] [PubMed] [Google Scholar]