Abstract
Objective:
Alcohol use and internalizing problems are often positively associated during adolescence and adulthood. However, the basis of this relationship remains poorly understood, and longitudinal data collected in population-based samples could improve the development of etiological models.
Method:
Using a prospective population-based U.K. cohort, the current study examined the relationship between frequency of drinking during adolescence (ages 13–15, N = 7,100) with problems with depression and anxiety at average age 17 years 10 months (n = 4,292). Analyses were conducted separately by sex and adjusted by the inclusion of potential individual- and familial-level confounders.
Results:
Among boys, drinking frequency was positively associated with later depression but not anxiety. This association was robust to adjustment for covariates/confounders. Among girls, drinking frequency was related to later depression and anxiety in univariable analyses. In multivariable analyses, only the association with depression remained after adjustment for covariates/confounders. Results were comparable across sexes, although the effect size of drinking frequency was higher among boys.
Conclusions:
Higher adolescent alcohol use, even at sub-clinical levels, is associated with an increased risk of later problems with depression but may not be associated with an aggregate measure of anxiety. Future research should consider the possibility of differential relationships between multiple measures of adolescent alcohol use and distinct internalizing outcomes later in development.
Internalizing problems, such as depression and anxiety, affect a substantial proportion of adolescents: 14% of U.S. 16-year-old participants in the National Comorbidity Survey (http://www.hcp.med.harvard.edu/ncs) have a lifetime history of major depression or dysthymia; 33% have a lifetime history of an anxiety disorder, although lower rates (∼15%–30%) have been reported in other Western populations (Beesdo et al., 2009). Such problems present health, economic, and social burdens (Lépine and Briley, 2011).
Likewise, alcohol use is common among adolescents: More than half (54%) of U.S. 10th graders (∼16 years old) have tried alcohol, and 16% report having five or more drinks in a row in the preceding 2 weeks (Johnston et al., 2013). In a 1999 report of U.K. adolescent drinking, more than 75% of 15- to 16-year-olds reported having been drunk, and 50% reported consuming five or more drinks on one occasion, in the past 30 days (Bauman and Phongsavan, 1999). This is despite U.K. public health advice recommending that young people under age 15 do not drink alcohol and those ages 15–17 years drink infrequently and always below the recommended daily limits for adults (https://www.education.gov.uk/consultations/downloadableDocs/CMO%20Guidance.pdf). As with mood and anxiety disorders, alcohol use can lead to substantial health, economic, and social costs (Bouchery et al., 2011).
Internalizing symptoms and alcohol use are often positively associated during adolescence and into adulthood (Boden and Fergusson, 2011; Saban and Flisher, 2010). This relationship has been observed in cross-sectional (Boschloo et al., 2011; Dawson et al., 2010; Grant et al., 2004; Schneier et al., 2010) and longitudinal (Mason et al., 2008; Needham, 2007) studies. Depression and anxiety are often correlated, and evidence suggests that they are etiologically related (Hettema, 2008; Kendler et al., 2007, 2011), but the relationship between alcohol-related phenotypes and anxiety is less consistent (e.g., Fröjd et al., 2011; Goodwin et al., 2004) than that between alcohol-related phenotypes and depression (Boden and Fergusson, 2011; Marmorstein, 2009; Pardini et al., 2007; Prescott et al., 2000). Many studies fail to consider both anxiety and depression in the same population, leaving open the possibility that inconsistencies are a function of the sample rather than the phenotype.
In addition, most studies have focused on the relationship between clinical levels of internalizing and alcohol problems (Boschloo et al., 2011; Dawson et al., 2010; Grant et al., 2004; Schneier et al., 2010); the relationship between nonclinical alcohol phenotypes and later clinical levels of internalizing problems has been less well characterized, although it has been the focus of some research (e.g., Mason et al., 2008; Needham, 2007; Rohde et al., 1996; Weitzman, 2004). Such information has important public health consequences: If normative drinking is predictive of later internalizing problems, education and prevention efforts should not be limited to the most severely affected adolescent drinkers (Rose, 2001).
The current study examined whether drinking frequency at ages 13–15 was related to clinically relevant depression and anxiety disorders at age 17 years 10 months in a longitudinally assessed, population-based sample in the United Kingdom. Given the breadth of phenotypic data collected on this large cohort, we were also able to conduct multiple secondary analyses incorporating relevant behavioral phenotypes (including mid-adolescent depressive symptoms and antisocial behavior). Based on the findings summarized above, which generally support a positive relationship between internalizing symptoms and alcohol use phenotypes during adolescence, and evidence that alcohol use phenotypes are highly correlated (Dick et al., 2011), we hypothesized that more frequent drinking would be positively associated with later internalizing problems.
Although some previous studies have not explored sex differences, many that have allowed for such differences have identified potentially important variation (e.g., Crum et al., 2008; Fleming et al., 2008; Marmorstein, 2009; McCarty et al., 2009). The relationship between internalizing symptoms and alcohol use is often more pronounced among girls (Fleming et al., 2008; Marmorstein, 2009; McCarty et al., 2009), although this is not always the case (Crum et al., 2008). Therefore, we conducted modeling separately by sex and hypothesized that any observed relationship between alcohol use and internalizing outcomes would be more pronounced among girls. We did not have a specific hypothesis regarding whether this relationship would differ between depression and anxiety.
Method
Sample
Data were drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC), an ongoing population-based study designed to investigate the effects of a wide range of influences on the health and development of children. Pregnant women residing in the southwest of England with an estimated date of delivery between April 1, 1991, and December 31, 1992, were invited to participate. The initial study cohort consisted of 14,062 pregnancies and 13,978 (52% boys and 48% girls) singletons/twins still alive at 12 months of age. Detailed information about ALSPAC is available online (http://www.bris.ac.uk/alspac). Ethical approval for the study was obtained from the ALSPAC Law and Ethics Committee and local research ethics committees. The study website contains details of all the data that are available through a fully searchable data dictionary (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary). As described in Boyd et al. (2013), children enrolled in ALSPAC were more educated at 16 compared with the national average, were more likely to be White, and were less likely to be eligible for free school meals.
Measures
Alcohol use.
The alcohol use variable included in the current study has been previously described (Heron et al., 2012). In brief, participants attended clinics at median ages 12 years 10 months, 13 years 10 months, and 15 years 5 months. During these clinic visits, participants answered questions related to their alcohol use via computerized questionnaires. For this study, we focused on participants’ reports of drinking frequency (FREQ), which was classified into three categories (none, occasional, or weekly use). This measure (assessed at three ages) was subjected to longitudinal latent class analysis to capture drinking frequency over time (ages 13–15), yielding three meaningful categories (low, medium, and high). This three-class variable was recoded into dummy variables for the current analyses. Data on FREQ class were available for 7,100 individuals (3,470 males).
Covariates/confounders.
Consistent with Heron et al. (2012), several pre-birth sociodemographic variables were included to reduce potential confounding effects. These were the following: (a) housing tenure (coded as owned/mortgaged, privately rented, subsidized housing rented from council/housing association), (b) crowding status (coded as the ratio of number of residents to number of rooms in house), and (c) maternal educational attainment (coded as no high school qualifications, high school, beyond high school); further details are available in Heron et al. (2012).
To control for liability to alcohol use and internalizing problems transmitted via maternal genomic contributions and maternally created environment, we included a measure of maternal harmful alcohol use (assessed at offspring age 12) and maternal history of depression. For the latter, we capitalized on the availability of multiple measures of maternal reports of depressive symptoms, which were assessed using the Edinburgh Postnatal Depression Scale (Cox et al., 1987). Using 10 maternal reports of depressive symptoms assessed between 18 weeks’ gestation of focal offspring to offspring’s age 11 years 2 months, we conducted a factor analysis and extracted individual-level factor scores to capture maternal liability to depression.
Last, we included a measure of conduct problems based on maternal reports of child behavior using the Strengths and Difficulties Questionnaire (Goodman et al., 2000) when the child was age 11. The measure consisted of three classes as described in Heron et al. (2012), where a score of 0 was coded as low, a score of 1–2 was coded as medium, and a score of 3 or more was coded as high.
To follow up on initial findings, we conducted a series of secondary analyses. First, we assessed whether our initial findings were robust to the inclusion of a measure of depressive symptoms experienced closer in time to the alcohol use assessments. For those analyses, we used sum scores from the Short Moods and Feelings Questionnaire (SMFQ; Angold et al., 1995), which were obtained by self-report at ages 13 years 6 months and 16 years 6 months. In another post hoc model, we tested the mediation effects of antisocial behavior at age 15 years 6 months, using a self-report measure based on the Edinburgh Study of Youth Transitions and Crime (Smith and Mc Vie, 2003). Last, we assessed whether initial associations remained significant after controlling for a later measure of alcohol use. For this model we used sum scores on the Alcohol Use Disorders Identification Test (AUDIT). The AUDIT items were included in a postal questionnaire completed by participants at age 16 years 6 months.
Depression- and anxiety-dependent variables.
The Clinical Interview Schedule–Revised (CIS-R; Lewis et al., 1992) was self-administered via computer at participants’ median age of 17 years 10 months. Using algorithms based on International Classification of Diseases, Tenth Revision (ICD-10; World Health Organization, 1992), criteria, it assessed last-month mild, moderate, and severe depressive episodes as well as anxiety disorders (generalized anxiety disorder, phobias, obsessive–compulsive disorder, and panic disorder). Individuals who met ICD criteria for a depressive episode or anxiety disorder were coded 1 for “DEP” or “ANX,” respectively; otherwise, they were coded 0. DEP and ANX data were available for 4,292 individuals (1,878 males).
Statistical analyses
All analyses were conducted in Mplus 5.21 (Muthén and Muthén, 1998–2007). Categorical variables with three or more classes were recoded into dummy variables. We used the maximum likelihood estimation with robust standard errors (MLR) estimator because of its handling of missing data. We first conducted univariable logistic regressions to assess the association between each sociodemographic variable, potential confounder, or alcohol phenotype and CIS-R–assessed depressive episode status (DEP) or anxiety problem status (ANX). Predictive variables that were nominally associated (p < .05) with the DEP/ANX outcome were then included in a multivariable model that allowed for correlations across predictive variables. All analyses were conducted separately by sex to evaluate whether the relationship between alcohol use and internalizing outcomes differed across the sexes in the context of covariates/confounders.
Attrition
Missing outcome data were more common among boys, participants whose mothers had lower levels of education, individuals living in rented or subsidized housing, individuals in crowded homes, those with higher levels of conduct problems, and those whose mothers exhibited harmful drinking at child age 12. Participants whose mothers had higher depression scores were more likely to be missing outcome data. Frequency of alcohol use was not associated with missing outcome data.
Results
Descriptive statistics and univariable analyses
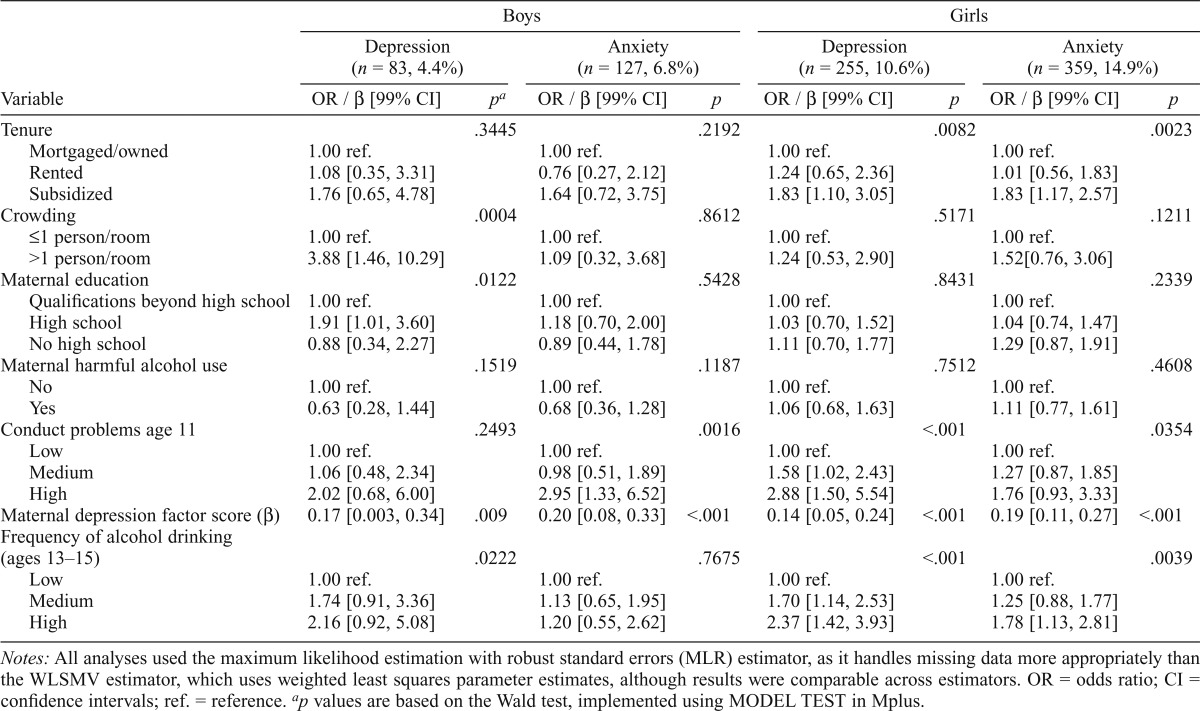
Frequency distributions for FREQ and internalizing outcomes are provided in Table 1. Girls were more likely than boys to meet criteria for DEP, χ2(1) = 58.20, p < .0001, and ANX, χ2(l) = 72.59, p < .0001; they also drank slightly more frequently, χ2(2) = 5.70, p = .06. Table 2 provides results from univariable analyses for both sexes. Among boys, crowding, maternal education, maternal depression, and FREQ were all associated with DEP based on Wald test p values, which represent the significance of the variable as a whole rather than individual levels of each variable. Only conduct problems and maternal depression were associated with ANX, although the relationship between FREQ and ANX was in the expected direction. We did not conduct further analyses on ANX in boys. Among girls, housing tenure, conduct problems, maternal depression, and FREQ were associated with both DEP and ANX. Thus, internalizing outcomes in both sexes were associated with demographic, family-level, and individual-level risk factors, although the specificities differed slightly (e.g., housing tenure was relevant among girls, whereas crowding was important among boys).
Table 1.
Distribution of drinking frequency classes (ages 13–15) and internalizing outcomes (age 17 years 10 months), by sex
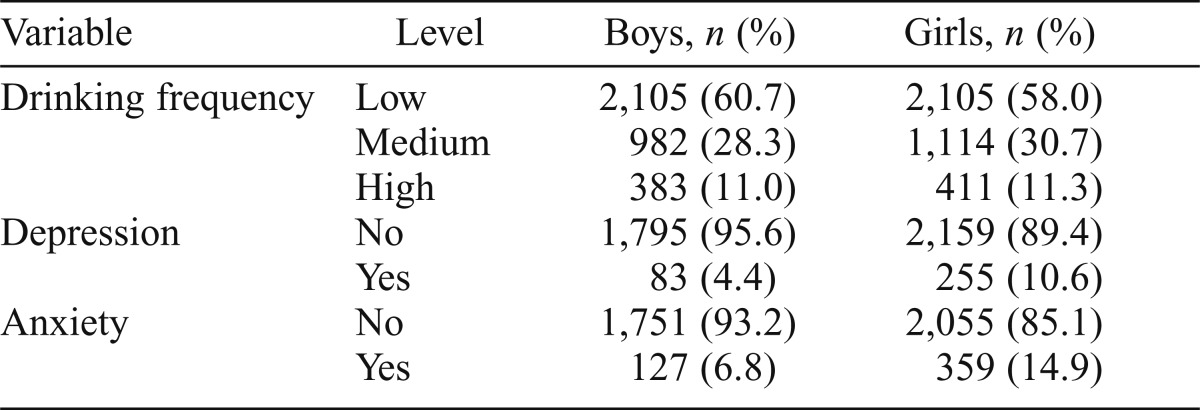
| Variable | Level | Boys, n (%) | Girls, n (%) |
| Drinking frequency | Low | 2,105 (60.7) | 2,105 (58.0) |
| Medium | 982 (28.3) | 1,114(30.7) | |
| High | 383 (11.0) | 411 (11.3) | |
| Depression | No | 1,795(95.6) | 2,159 (89.4) |
| Yes | 83 (4.4) | 255 (10.6) | |
| Anxiety | No | 1,751 (93.2) | 2,055(85.1) |
| Yes | 127 (6.8) | 359 (14.9) |
Table 2.
Univariable model results
| Boys |
Girls |
|||||||
| Depression (n = 83, 4.4%) |
Anxiety (n = 127, 6.8%) |
Depression (n = 255, 10.6%) |
Anxiety (n = 359, 14.9%) |
|||||
| Variable | OR / β [99% CI] | pa | OR / β [99% CI] | p | OR / β [99% CI] | p | OR / β [99% CI] | p |
| Tenure | .3445 | .2192 | .0082 | .0023 | ||||
| Mortgaged/owned | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| Rented | 1.08 [0.35, 3.31] | 0.76 [0.27, 2.12] | 1.24 [0.65, 2.36] | 1.01 [0.56, 1.83] | ||||
| Subsidized | 1.76 [0.65, 4.78] | 1.64 [0.72, 3.75] | 1.83 [1.10, 3.05] | 1.83 [1.17, 2.57] | ||||
| Crowding | .0004 | .8612 | .5171 | .1211 | ||||
| ≤1 person/room | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| >1 person/room | 3.88 [1.46, 10.29] | 1.09 [0.32, 3.68] | 1.24 [0.53, 2.90] | 1.52[0.76, 3.06] | ||||
| Maternal education | .0122 | .5428 | .8431 | .2339 | ||||
| Qualifications beyond high school | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| High school | 1.91 [1.01, 3.60] | 1.18 [0.70, 2.00] | 1.03 [0.70, 1.52] | 1.04 [0.74, 1.47] | ||||
| No high school | 0.88 [0.34, 2.27] | 0.89 [0.44, 1.78] | 1.11 [0.70, 1.77] | 1.29 [0.87, 1.91] | ||||
| Maternal harmful alcohol use | .1519 | .1187 | .7512 | .4608 | ||||
| No | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| Yes | 0.63 [0.28, 1.44] | 0.68 [0.36, 1.28] | 1.06 [0.68, 1.63] | 1.11 [0.77, 1.61] | ||||
| Conduct problems age 11 | .2493 | .0016 | <.001 | .0354 | ||||
| Low | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| Medium | 1.06 [0.48, 2.34] | 0.98 [0.51, 1.89] | 1.58 [1.02, 2.43] | 1.27 [0.87, 1.85] | ||||
| High | 2.02 [0.68, 6.00] | 2.95 [1.33, 6.52] | 2.88 [1.50, 5.54] | 1.76 [0.93, 3.33] | ||||
| Maternal depression factor score (β) | 0.17 [0.003, 0.34] | .009 | 0.20 [0.08, 0.33] | <.001 | 0.14 [0.05, 0.24] | <.001 | 0.19 [0.11, 0.27] | <.001 |
| Frequency of alcohol drinking (ages 13–15) | .0222 | .7675 | <.001 | .0039 | ||||
| Low | 1.00 ref. | 1.00 ref. | 1.00 ref. | 1.00 ref. | ||||
| Medium | 1.74 [0.91, 3.36] | 1.13 [0.65, 1.95] | 1.70 [1.14, 2.53] | 1.25 [0.88, 1.77] | ||||
| High | 2.16 [0.92, 5.08] | 1.20 [0.55, 2.62] | 2.37 [1.42, 3.93] | 1.78 [1.13, 2.81] | ||||
Notes: All analyses used the maximum likelihood estimation with robust standard errors (MLR) estimator, as it handles missing data more appropriately than the WLSMV estimator, which uses weighted least squares parameter estimates, although results were comparable across estimators. OR = odds ratio; CI = confidence intervals; ref. = reference.
p values are based on the Wald test, implemented using MODEL TEST in Mplus.
Multivariable analyses
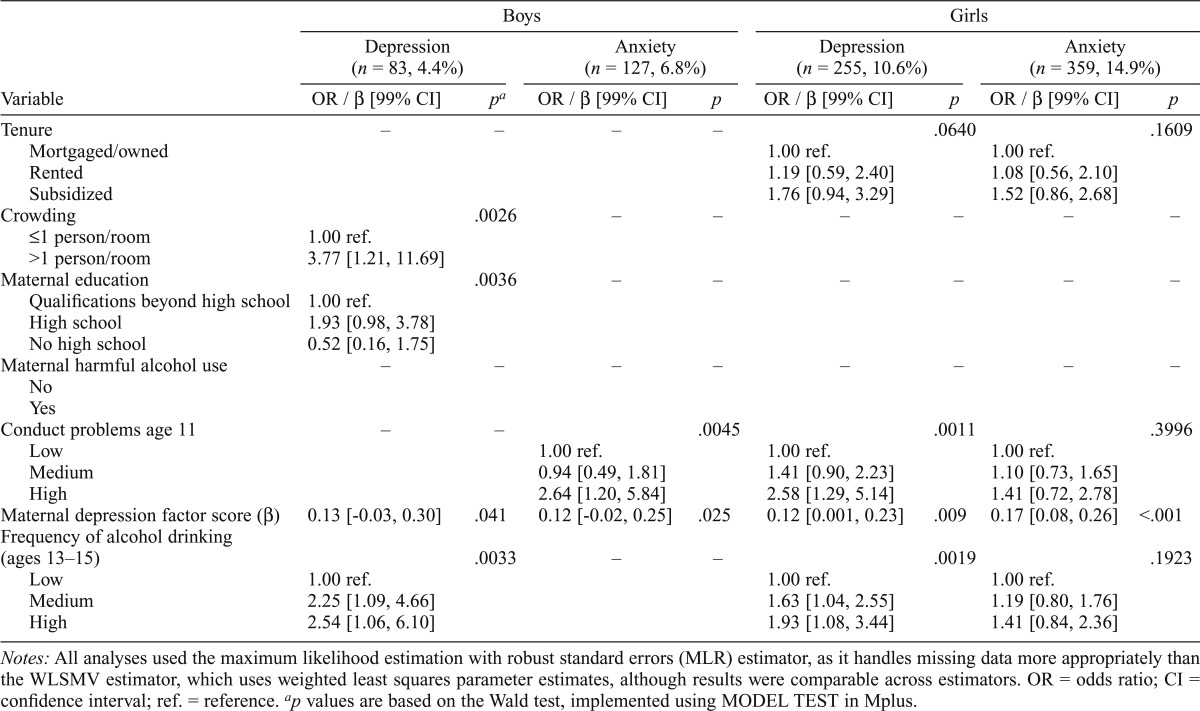
As shown in Table 3, boys who drank more frequently during adolescence were more likely to meet criteria for a later depressive episode even after controlling for relevant covariates/confounders. The results suggest a dose-response pattern, although confidence intervals for the medium and high classes overlap. Family-level risk factors (crowding and maternal education) also remain significant predictors. Among girls, conduct problems, maternal depression, and FREQ were associated with later DEP in multivariable models (Table 3). However, only maternal depression remained associated with ANX in multivariable analyses, although FREQ’s effect was in the expected direction.
Table 3.
Multivariable model results
| Boys |
Girls |
|||||||
| Depression (n = 83, 4.4%) |
Anxiety (n = 127, 6.8%) |
Depression (n = 255, 10.6%) |
Anxiety (n = 359, 14.9%) |
|||||
| Variable | OR / β [99% CI] | pa | OR / β [99% CI] | p | OR / β [99% CI] | p | OR / β [99% CI] | p |
| Tenure | – | – | – | – | .0640 | .1609 | ||
| Mortgaged/owned | 1.00 ref. | 1.00 ref. | ||||||
| Rented | 1.19 [0.59, 2.40] | 1.08 [0.56, 2.10] | ||||||
| Subsidized | 1.76 [0.94, 3.29] | 1.52 [0.86, 2.68] | ||||||
| Crowding | .0026 | – | – | – | – | – | – | |
| ≤1 person/room | 1.00 ref. | |||||||
| >1 person/room | 3.77 [1.21, 11.69] | |||||||
| Maternal education | .0036 | – | – | – | – | – | – | |
| Qualifications beyond high school | 1.00 ref. | |||||||
| High school | 1.93 [0.98, 3.78] | |||||||
| No high school | 0.52 [0.16, 1.75] | |||||||
| Maternal harmful alcohol use | – | – | – | – | – | – | – | – |
| No | ||||||||
| Yes | ||||||||
| Conduct problems age 11 | – | – | .0045 | .0011 | .3996 | |||
| Low | 1.00 ref. | 1.00 ref. | 1.00 ref. | |||||
| Medium | 0.94 [0.49, 1.81] | 1.41 [0.90, 2.23] | 1.10 [0.73, 1.65] | |||||
| High | 2.64 [1.20, 5.84] | 2.58 [1.29, 5.14] | 1.41 [0.72, 2.78] | |||||
| Maternal depression factor score (β) | 0.13 [-0.03, 0.30] | .041 | 0.12 [-0.02, 0.25] | .025 | 0.12 [0.001, 0.23] | .009 | 0.17 [0.08, 0.26] | <.001 |
| Frequency of alcohol drinking (ages 13–15) | .0033 | – | – | .0019 | .1923 | |||
| Low | 1.00 ref. | 1.00 ref. | 1.00 ref. | |||||
| Medium | 2.25 [1.09, 4.66] | 1.63 [1.04, 2.55] | 1.19 [0.80, 1.76] | |||||
| High | 2.54 [1.06, 6.10] | 1.93 [1.08, 3.44] | 1.41 [0.84, 2.36] | |||||
Notes: All analyses used the maximum likelihood estimation with robust standard errors (MLR) estimator, as it handles missing data more appropriately than the WLSMV estimator, which uses weighted least squares parameter estimates, although results were comparable across estimators. OR = odds ratio; CI = confidence interval; ref. = reference.
p values are based on the Wald test, implemented using MODEL TEST in Mplus.
The effect size of maternal depression on child depression was similar across the sexes, but its effect on child anxiety was stronger among girls (although confidence intervals overlapped across the sexes). As was observed among boys, the association between FREQ and DEP is suggestive of a dose response, but confidence intervals overlap. Of note, FREQ and DEP remained associated in models that included all covariates (i.e., not just those demonstrated to be associated with DEP in univariable analyses; data not shown) among both boys and girls.
Controlling for prior depression
To test whether the association between FREQ and DEP was robust to controlling for an earlier measure of depression, we re-ran the multivariable analyses and added self-reported depression scores derived from the SMFQ, from age 13 years 6 months or age 16 years 6 months, as a predictor. For boys, the relationship between FREQ and DEP persisted (p < .05) regardless of which SMFQ score was included. For girls, when we controlled for depressive symptoms at age 13 years 6 months, the association between FREQ and DEP diminished in statistical significance (p = .0788) but the magnitude of the effect increased slightly (i.e., odds ratios were higher). Controlling for age 16 years 6 months depression did not diminish the relationship between FREQ and DEP (p < .05). Thus, overall the relationship between FREQ in early adolescence and later DEP existed above and beyond symptoms of depression experienced concurrently with or shortly after alcohol use.
Mediation through externalizing behavior
We further tested whether the association between FREQ and DEP was mediated through externalizing behavior. These analyses were limited to girls because conduct problems were not associated with DEP in the boys’ univariable analysis. For the mediation model to be temporally logical, we used a measure of externalizing behavior (adapted from the Edinburgh Study of Youth Transitions and Crime; Smith and Mc Vie, 2003) at age 15 years 6 months, such that it occurred between the assessments of FREQ and DEP. There was insufficient evidence for a mediation pathway, Wald χ2(2) = 0.357, p = .8367.
Mediation through later alcohol use
Last, we tested a mediation model that included both direct pathways from FREQ to DEP and mediation through a later measure of alcohol use (AUDIT score at age 16 years 6 months). Among girls, the mediation pathway could be dropped from the model, Wald χ2(2) = 1.463, p = .4813. Likewise, there was insufficient evidence of a mediation pathway between FREQ and DEP among boys, Wald χ2(2) = 2.618, p = .2702.
Discussion
The goal of the current study was to examine whether adolescent drinking behavior was related to problems with later episodes of depression and anxiety, using a population-based sample of U.K. participants. Results indicated that individuals who were drinking more frequently at ages 13–15 were more likely to experience episodes of depression as late adolescents (age ∼18). The strength of the association was similar for boys and girls. There was insufficient evidence of an association with anxiety.
Relationship between adolescent alcohol use and internalizing outcomes across the sexes
We predicted that the relationship between alcohol use and internalizing outcomes would be more pronounced among girls; this hypothesis was not fully supported. In univariable analyses, drinking frequency was associated with both depression and anxiety in girls but only with depression in boys. However, the association with anxiety among girls was not evident in multivariable analyses. In adjusted analyses, the effect sizes of medium and high drinking frequency classes on depression overlapped but were also slightly higher among boys than among girls, as the adjustments moved the effect upward for boys and downward for girls. Although most individuals in the medium and high frequency classes did not go on to meet criteria for depression in either sex, individuals in those classes were disproportionately likely to experience later problems with depression. These results suggest that membership in these classes should be considered a modest risk factor for both boys and girls.
Specificity of effects
We found insufficient evidence of a moderate or strong association between frequency of alcohol use and anxiety, which is consistent with some previous research (Fröjd et al., 2011; Goodwin et al., 2004) and suggests that the association between alcohol use and internalizing problems may be specific to mood disorders. However, other studies have reported positive associations between alcohol phenotypes and anxiety (Brook et al., 1998; Kaplow et al., 2001). These inconsistencies could be attributable to variation across ages or in the nature of the phenotypes used. The use of current versus lifetime/last-year problems also could affect results. We note that the confidence intervals of odds ratios for FREQ’s relationship with ANX overlapped the point estimates for DEP. This is suggestive of a positive association between FREQ and ANX; this relationship should be examined further in similar samples, particularly those in which assessment of anxiety symptoms/disorders is more extensive.
Role of conduct problems
Some studies have found that the relationship between alcohol use and internalizing phenotypes is related to both phenotypes’ correlation with externalizing behavior (Hussong et al., 2011) or is diminished once externalizing behavior is accounted for (Hopwood and Grilo, 2010; Maggs et al., 2008), although this is not always the case (Marmorstein, 2010). This potential relationship was relevant to the current multivariable model predicting depression in girls: In that model, both frequency of alcohol use and age 11 conduct problems were associated with the outcome. Therefore, we tested whether later antisocial behavior mediated the relationship between alcohol use and depression in girls. Results indicated that there was no significant mediation by antisocial behavior. This finding suggests that the relation between alcohol use and internalizing problems is not a function of positive correlations between internalizing and externalizing phenotypes.
Role of later alcohol use
We considered the possibility that alcohol use during any period of adolescence was associated with later depression: Perhaps drinking frequency at ages 13–15 is not uniquely predictive of later internalizing problems. We therefore tested a model wherein a measure of alcohol use at age 16 years 6 months mediated the relationship between earlier drinking frequency and depression. The mediation pathways could be dropped from the model in both boys and girls, but the direct pathways could not, suggesting that alcohol use during early to mid-adolescence represents a specific risk factor (or indicator) whose effect cannot be accounted for, or substituted by, alcohol misuse later in adolescence. These findings warrant replication in other samples and with other measures of alcohol use. Although the AUDIT sum scores are reasonably distributed in this sample, the underlying items are based on problematic alcohol use. A different pattern of effects might be observed using a qualitatively different measure of alcohol use at this age.
Conclusions
These results demonstrate that, in a population-based U.K. sample, adolescent drinking was positively associated with CIS-R–assessed depression, but not anxiety, at age 17 years 10 months. The association was consistent across the sexes and robust to adjustment for potential confounders, including externalizing behavior and liability to depression and alcohol misuse transmitted via participants’ mothers. These findings suggest that more frequent adolescent drinking could be an indicator of, or risk factor for, later problems with depression. The specificity of the observed effect to depression was not entirely consistent with previous reports (Brook et al., 1998; Kaplow et al., 2001). However, other studies have found that anxiety and alcohol use phenotypes are not associated after controlling for crucial covariates (Dawson et al., 2005; Goodwin et al., 2004; Linden et al., 2013; MacDonald et al., 2010).
Numerous studies have reported a positive association—frequently longitudinal in nature—between clinical/diagnostic levels of alcohol problems and depression (Boschloo et al., 2012a, 2012b; Marmorstein, 2009; Marmorstein et al., 2010; Rao et al., 2000). The current findings extend that work and contribute to previous evidence (e.g., Dixit and Crum, 2000; Fleming et al., 2008) that a nonclinical measure of alcohol use is related to clinical depression.
This observation suggests that the public health costs of alcohol use are not limited to a selected (e.g., clinically affected) group. We note that much previous research has examined the link between early depression and later alcohol use (Brook et al., 1998; Crum and Pratt, 2001; Crum et al., 2008; Marmorstein, 2009; McCarty et al., 2009). Of note, the social associations of alcohol use are quite dynamic from early adolescence through late adolescence, shifting from deviant behavior to more normative experimentation. During the same developmental period, manifestations of internalizing symptoms are changing along with the prevalence of those symptoms (e.g., separation anxiety declines while depressive symptoms become more common).
These fluctuations could contribute to inconsistencies in the presence, strength, and direction of associations between alcohol use and internalizing symptoms from early adolescence into emerging adulthood. For all its strengths, the current data set does not include consistent and frequent measures of alcohol use or internalizing symptoms across this broad developmental time frame, precluding more thorough longitudinal modeling of dynamic pathways between these phenotypes. However, these results provide some insight into how alcohol use and internalizing problems are related across this tumultuous period.
Limitations
The current findings should be considered in light of several limitations. The CIS-R only focuses on the last month, a relatively short reporting period; a small number of individuals likely experienced a depressive episode shortly after being assessed or shortly before the past-month time frame. Thus, our measure does not capture everyone who experienced a depressive episode in a period that could be relevant to our analyses.
The low prevalence of symptoms necessitated collapsing all anxiety disorders into a single anxiety variable, which could have obscured differences in the relation between alcohol use and different manifestations of anxiety, such as social phobia versus generalized anxiety disorder (e.g., Fröjd et al., 2011; Kaplow et al., 2001). In addition, the alcohol use variables used were categorical rather than quantitative and were derived in the current sample, making comparisons to other studies less straightforward. Both alcohol use and internalizing symptoms were based on self-reports, and previous work has suggested that the observed relationship between these phenotypes might vary across reporters (McCarty et al., 2012). ALSPAC participants are largely of European descent, and these results might not be generalizable to other ethnicities. As is typical of long-term longitudinal studies, attrition has been nontrivial; however, individuals with missing outcome data did not differ from those with complete data on key related variables.
Last, these analyses did not explicitly examine potential genetic correlations between alcohol use and internalizing problems, which could account for co-occurrence. However, maternal harmful drinking and depression were included as covariates in an effort to control for genetic liability to both phenotypes. Despite these potential limitations, these analyses provide support from a large, representative, and densely assessed sample for a positive association between subclinical alcohol use during adolescence and later problems with depression.
Acknowledgments
The authors are grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses.
Footnotes
The U.K. Medical Research Council and the Wellcome Trust (Grants 092731 and 074268/Z/07/Z) and the University of Bristol provide core support for the Avon Longitudinal Study of Parents and Children. This research was specifically funded by National Institutes of Health Grants K01AA021399 to Alexis C. Edwards, K02AA018755 to Danielle M. Dick, and R01AA018333 to Danielle M. Dick and Kenneth S. Kendler. This publication is the work of the authors, and the corresponding author will serve as guarantor for the contents of this article.
References
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. [Google Scholar]
- Bauman A, Phongsavan P. Epidemiology of substance use in adolescence: Prevalence, trends and policy implications. Drug and Alcohol Dependence. 1999;55:187–207. doi: 10.1016/s0376-8716(99)00016-2. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106:906–914. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- Boschloo L, van den Brink W, Penninx BW, Wall MM, Hasin DS. Alcohol-use disorder severity predicts first-incidence of depressive disorders. Psychological Medicine. 2012a;42:695–703. doi: 10.1017/S0033291711001681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, Smit JH, van den Brink W, Veltman DJ, Beekman AT, Penninx BW. Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders: Findings from the Netherlands Study of Depression and Anxiety (NESDA) Journal of Affective Disorders. 2011;131:233–242. doi: 10.1016/j.jad.2010.12.014. [DOI] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Veltman DJ, Beekman AT, Penninx BW. Alcohol use disorders and the course of depressive and anxiety disorders. British Journal of Psychiatry. 2012b;200:476–484. doi: 10.1192/bjp.bp.111.097550. [DOI] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. American Journal of Preventive Medicine. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Smith GD. Cohort profile: The ‘children of the 90s’—the index offspring of the Avon Longitudinal Study of Parents and Children. International Journal of Epidemiology. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Cohen P, Brook DW. Longitudinal study of co-occurring psychiatric disorders and substance use. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:322–330. doi: 10.1097/00004583-199803000-00018. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Crum RM, Pratt LA. Risk of heavy drinking and alcohol use disorders in social phobia: A prospective analysis. American Journal of Psychiatry. 2001;158:1693–1700. doi: 10.1176/appi.ajp.158.10.1693. [DOI] [PubMed] [Google Scholar]
- Crum RM, Storr CL, Ialongo N, Anthony JC. Is depressed mood in childhood associated with an increased risk for initiation of alcohol use during early adolescence? Addictive Behaviors. 2008;33:24–40. doi: 10.1016/j.addbeh.2007.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: Likelihood, expression and course. Drug and Alcohol Dependence. 2010;112:9–17. doi: 10.1016/j.drugalcdep.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug and Alcohol Dependence. 2005;77:139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Dick DM, Meyers JL, Rose RJ, Kaprio J, Kendler KS. Measures of current alcohol consumption and problems: Two independent twin studies suggest a complex genetic architecture. Alcoholism: Clinical and Experimental Research. 2011;35:2152–2161. doi: 10.1111/j.1530-0277.2011.01564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. American Journal of Psychiatry. 2000;157:751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Fröjd S, Ranta K, Kaltiala-Heino R, Marttunen M. Associations of social phobia and general anxiety with alcohol and drug use in a community sample of adolescents. Alcohol and Alcoholism. 2011;46:192–199. doi: 10.1093/alcalc/agq096. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. British Journal of Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Association between anxiety disorders and substance use disorders among young persons: Results of a 21-year longitudinal study. Journal of Psychiatric Research. 2004;38:295–304. doi: 10.1016/j.jpsychires.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Heron J, Macleod J, Munafò MR, Melotti R, Lewis G, Tilling K, Hickman M. Patterns of alcohol use in early adolescence predict problem use at age 16. Alcohol and Alcoholism. 2012;47:169–177. doi: 10.1093/alcalc/agr156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema JM. What is the genetic relationship between anxiety and depression? American Journal of Medical Genetics. Part C, Seminars in Medical Genetics. 2008;148C:140–146. doi: 10.1002/ajmg.c.30171. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Grilo CM. Internalizing and externalizing personality dimensions and clinical problems in adolescents. Child Psychiatry and Human Development. 2010;41:398–408. doi: 10.1007/s10578-010-0175-4. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2012: Vol. 1. Secondary school students. Bethesda, MD: National Institute on Drug Abuse; 2013. [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. Journal of Clinical Child Psychology. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. American Journal of Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychological Medicine. 2007;37:453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- Lépine JP, Briley M. The increasing burden of depression. Journal of Neuropsychiatric Disease and Treatment, 7, Supplement. 2011;1:3–7. doi: 10.2147/NDT.S19617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: A standardized assessment for use by lay interviewers. Psychological Medicine. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- Linden AN, Lau-Barraco C, Milletich RJ. The role of protective behavioral strategies and anxiety in problematic drinking among college students. Journal of Studies on Alcohol and Drugs. 2013;74:413–422. doi: 10.15288/jsad.2013.74.413. [DOI] [PubMed] [Google Scholar]
- MacDonald R, Crum RM, Storr CL, Schuster A, Bienvenu OJ. Sub-clinical anxiety and the onset of alcohol use disorders: Longitudinal associations from the Baltimore ECA follow-up, 1981-2004. Journal of Addictive Diseases. 2010;30:45–53. doi: 10.1080/10550887.2010.531667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggs JL, Patrick ME, Feinstein L. Childhood and adolescent predictors of alcohol use and problems in adolescence and adulthood in the National Child Development Study. Addiction, 103, Supplement. 2008;1:7–22. doi: 10.1111/j.1360-0443.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009;33:49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between depressive symptoms and alcohol problems: The influence of comorbid delinquent behavior. Addictive Behaviors. 2010;35:564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, Malone SM. Longitudinal associations between depression and substance dependence from adolescence through early adulthood. Drug and Alcohol Dependence. 2010;107:154–160. doi: 10.1016/j.drugalcdep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, Shin C. Dimensions of adolescent alcohol involvement as predictors of young-adult major depression. Journal of Studies on Alcohol and Drugs. 2008;69:275–285. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Kosterman R, Mason WA, McCauley E, Hawkins JD, Herrenkohl TI, Lengua LJ. Longitudinal associations among depression, obesity and alcohol use disorders in young adulthood. General Hospital Psychiatry. 2009;31:442–450. doi: 10.1016/j.genhosppsych.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73:444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Los Angeles, CA: Authors; 1998-2007. [Google Scholar]
- Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science & Medicine. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and Alcohol Dependence, 88, Supplement. 2007;1:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott CA, Aggen SH, Kendler KS. Sex-specific genetic influences on the comorbidity of alcoholism and major depression in a population-based sample of US twins. Archives of General Psychiatry. 2000;57:803–811. doi: 10.1001/archpsyc.57.8.803. [DOI] [PubMed] [Google Scholar]
- Rao U, Daley SE, Hammen C. Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:215–222. doi: 10.1097/00004583-200002000-00022. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology. 2001;30:427–432. doi: 10.1093/ije/30.3.427. discussion 433–434. [DOI] [PubMed] [Google Scholar]
- Saban A, Flisher AJ. The association between psychopathology and substance use in young people: A review of the literature. Journal of Psychoactive Drugs. 2010;42:37–47. doi: 10.1080/02791072.2010.10399784. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Foose TE, Hasin DS, Heimberg RG, Liu SM, Grant BF, Blanco C. Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2010;40:977–988. doi: 10.1017/S0033291709991231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DJ, McVie S. Theory and method in the Edinburgh Study of Youth Transitions and Crime. British Journal of Criminology. 2003;43:169–195. [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, Tenth Edition. Geneva, Switzerland: Author; 1992. [Google Scholar]


