Abstract
Objective:
The clinical course of alcohol use disorder (AUD) has been widely researched over the past half-century and has been used to advance our understanding of the treatment of AUD. Nevertheless, new directions in AUD clinical course research could enhance its value in informing clinical decision-making in patient-centered treatment of AUD.
Method:
An overview, a critical analysis, and a discussion of AUD clinical course research are presented.
Results:
This article discusses three research directions that promote the advancement of the knowledge regarding the clinical course of AUD to better inform clinical decision-making in patient-centered treatment of AUD. Specifically, we hypothesized that (a) real-time data collection of the clinical course of AUD via ecological momentary assessment would help elucidate near real-time associations between risk factors and alcohol use, (b) future research designs should use person-centered and dynamic analyses of alcohol use over time, and (c) adaptive treatment designs would provide personalized and optimized AUD treatment. Consequently, the field will advance the development of clinical decision-making support systems to better inform clinicians and clients in making informed AUD treatment decisions. In addition, such research would advance clinical practice with more attention to theory and expansion of the study of the clinical course of AUD to include areas of life functioning besides alcohol use.
Conclusions:
These research directions have the potential to build a scientific knowledge base that could improve our understanding of AUD among individuals with alcohol problems, would allow providers to predict patient outcomes during and after treatment, and would offer practical strategies regarding steps that could ultimately improve the clinical course of AUD.
The clinical course of a psychiatric disorder may be defined as the progression of changes in symptoms of the disorder following initiation of formal treatment or self-initiated behavior change (Chung and Maisto, 2006; Frank et al., 1991). The empirical study of the clinical course of alcohol use disorder (AUD) spans more than five decades, beginning with Jellinek’s (Jellinek, 1960; also see Glatt, 1958) hypothesis of “progressivity” of (and recovery from) the disease of “alcoholism,” to the work of Edwards and colleagues (Edwards, 1984; Edwards and Gross, 1976; Orford et al., 1976; Taylor et al., 1986) on the chronic relapsing nature of AUD, to recent empirical studies on the dynamic process of changes in alcohol use following treatment (Witkiewitz et al., 2010b; Witkiewitz and Marlatt, 2007). The magnitude of public health concern about AUD (World Health Organization, 2011) places a high priority on research examining changes in alcohol use and related outcomes following treatment-induced or self-initiated change efforts. Accordingly, it is important to understand the clinical course of AUD.
What does the clinical course of AUD look like?
Clinicians and researchers have viewed the first 90 days following the initiation of abstinence or planned reductions in alcohol use as crucial to successful longer-term “remission” from AUD. This has been reflected in clinical practice in the Alcoholics Anonymous slogan of “90 meetings in 90 days” as a prescription for newly abstinent individuals. This prescription is somewhat based on Hunt and colleagues’ (1971) findings for alcohol dependence, heroin dependence, and cigarette smoking that abstinence was disrupted within the first 90 days following treatment completion for about 70% of each of the respective samples. Recent research suggests that 12 months after treatment may mark another crucial time in the clinical course of AUD, with sustained abstinence during the 12 months following the initiation or completion of AUD treatment associated with better longer-term functioning (Maisto et al., 1998, 2002).
Although prior research suggests that abstinence earlier in the clinical course is predictive of later alcohol use and related functioning, more recent research has shown that changes in alcohol use following treatment are discontinuous (Witkiewitz et al., 2010b). Witkiewitz and colleagues have studied alcohol treatment outcomes with an emphasis on using advanced data analytic techniques to gain a better understanding of drinking patterns during and following treatment. For example, Witkiewitz and Masyn (2008) combined discrete time survival analysis with latent growth mixture modeling to investigate variations in the time-to-lapse and the post-lapse drinking trajectories in the Relapse Replication and Extension Project data. The results supported a model with three drinking trajectories: (a) frequent heavy drinking, (b) frequent drinking following the first lapse and a return to less frequent drinking, and (c) infrequent moderate drinking. Similar drinking patterns were found using Project MATCH data (Matching Alcoholism Treatments to Client Heterogeneity; Witkiewitz et al., 2007) and the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study data (Witkiewitz et al., 2010b).
Despite the infrequency of achieving abstinence during and following treatment, many treatment programs (particularly those based on the Minnesota model) consider abstinence the only acceptable goal (Rosenberg and Davis, 1994). Yet some individuals prefer to have a choice in treatment goals (Sobell et al., 1992) and may prefer a non-abstinent, low-risk drinking goal (Heather et al., 2010). Recent research on “low-risk drinking” (defined as fewer than five drinks per occasion in a 30-day period; Kline-Simon et al., 2013) and “moderate drinking” (defined as fewer than 6 heavy drinking days in a 12-month period—with a heavy drinking day defined as five or more drinks for men and four or more drinks for women; Maisto et al., 2007) provides evidence that individuals who achieve these levels of controlled drinking have similar outcomes 12 months and 3 years later as compared with individuals who achieved abstinence during the same time frames. Based on the research evidence, the U.S. Food and Drug Administration (FDA) has moved toward low-risk drinking (defined as no heavy drinking days) as a primary endpoint for Phase III pharmaceutical trials (Falk et al., 2010). Thus, research on clinical course has directly informed policy at the FDA, which may ultimately affect the availability of FDA-approved pharmacotherapies for AUD.
Yet, many clinicians and policy-makers may still be wary of accepting low-risk drinking as a treatment goal (Sobell and Sobell, 2011). One concern of clinicians and policy-makers, as well as clients, is the accurate perception that low-risk drinking may be difficult to attain. Indeed, low-risk drinking has been shown in numerous studies to be the lowest probability outcome following treatment (Ilgen et al., 2008; Kline-Simon et al., 2013; Maisto et al., 2007). Using data from Project MATCH, Maisto and colleagues (2007) found that 19.5% of the outpatient sample could be classified as moderate drinkers during the first year following treatment initiation, and only 22.3% remained classified as moderate drinkers 3 years later. Kline-Simon and colleagues (2013) found that only 14% and 16% of their treatment sample could be classified as low-risk drinkers at 6 and 12 months, respectively. In summary, low-risk drinking seems to be sustained by a small proportion of individuals who have received alcohol treatment. Future AUD clinical course research should examine who is most likely to achieve low-risk drinking and how low-risk drinking patterns are maintained. Such research could directly inform treatment planning and help determine the need for varying levels of care.
Prediction of the clinical course of AUD
Both retrospective and prospective studies have illuminated individual characteristics and protective factors that help promote long-term recovery from AUD. In a general population study, Dawson and colleagues (2005) found that individuals who were married, female, older, and had no personality disorder had the highest likelihood of an abstinence recovery compared with ongoing alcohol dependence. Moos and Moos (2005, 2006, 2007) found protective resources that supported abstinence recoveries included self-efficacy, health status, financial status, Alcoholics Anonymous involvement, and support for abstinence from family, friends, and work. Similarly, Satre and colleagues (2012) found that treatment length, female gender, age (older adult), having friends who support abstinence, and positive life transitions predicted greater alcohol abstinence and remission from dependence 5 to 9 years following initial treatment. Other studies of treatment factors have found that longer treatment duration (Mertens et al., 2005, 2012) and receiving psychiatric (Ray et al., 2005) or medical services (Mertens et al., 2008) are associated with better long-term abstinence outcomes.
With regard to low-risk (i.e., moderate) drinking, lower dependence severity and less alcohol involvement are predictors of maintaining low-risk drinking following treatment (Dawson et al., 2005; Ilgen et al., 2008; Rosenberg, 1993). Other characteristics that have predicted low-risk drinking include being female, earning higher income, having more years of education, being married, and having greater social/psychological resources (Dawson et al., 2005; Ilgen et al., 2008; Kline-Simon et al., 2013; Kuerbis et al., 2012; Rosenberg, 1993).
In summary, AUD is a significant public health problem, and research on its clinical course is accordingly deemed significant for its potential to inform effective AUD treatment. As a result, there has been a high volume of research published on the clinical course of AUD in the last several decades. Such AUD clinical course research shows a heterogeneous pattern over time across individuals and has helped identify course predictors such as gender and age. Moreover, these findings from AUD clinical course research have influenced clinical practice.
AUD clinical course research and clinical practice
Research on AUD clinical course data has helped to advance AUD treatment in at least three ways. First, information on the factors related to how AUD changes over time following the initiation of behavior change can influence general conceptualizations of AUD and approaches to AUD treatment. McKay (2009) used the research base on the course of substance use disorders to conceptualize substance use disorders as “chronic diseases” and, therefore, to use a continuing care approach in their management. Results indicate that continuing care can result in greater alcohol abstinence rates up to 2 years following treatment (McKay et al., 2005b), and in clinical practice continuing care and aftercare groups are commonly used (e.g., http://www.hazelden. org/web/public/continuing_care_groups.page, last accessed on April 23, 2014).
Second, AUD clinical course data have contributed to the creation of AUD prevention and treatment interventions. For instance, classifying individuals according to the severity of the clinical course of AUD has informed ways to treat AUD by manipulating the factors that seem to lead to more favorable outcomes. Research on the clinical course of AUD made a substantial contribution in this regard with the development of relapse-prevention interventions (Maisto and Connors, 2006).
Third, AUD clinical course data have been used to evaluate the efficacy or effectiveness of interventions (Scott et al., 2008). AUD clinical course data can provide a reference for the expected course of AUD for a given population, which can be compared with the course following the use of an intervention applied to modify its course. Scott and colleagues (2008) adopted this approach to compare the clinical course among African Americans with that of Whites. The results indicated that the clinical course was largely the same between samples, except the frequency of problems was significantly greater in the White sample (Scott et al., 2008).
We believe AUD clinical course research has made major contributions to the content, intensity, and duration of AUD treatment. Yet, similar to the treatment of other psychiatric disorders, there remain important gaps between AUD clinical course research and its translation to effective clinical practice.
AUD clinical course research and clinical practice: Gaps
Kazdin (2008) noted, “The challenge of clinical decision-making can be conveyed by the effort to tailor treatment to meet the needs of individual patients. This statement is one we make and accept routinely in our clinical work, but researchers have yet to help us do that” (p. 149). In other words, the most useful research data are those allowing treatment to be person-centered and individualized. Unfortunately, AUD clinical course research has not provided the database needed to meet Kazdin’s challenge. This is not to deny the field’s concerted efforts to do so. A prominent example in this regard is the patient-treatment matching literature. As McKay (2009) noted, research on patient-treatment matching attempted to provide the field with an empirical foundation for individualizing alcohol (and other drug) treatment. However, almost 40 years of research on matching treatment intensity or type to patient characteristics has yielded mixed and weak effects.
It is also important to recognize that the gap in translating clinical course research into clinical practice may not be entirely attributable to the quality or type of data clinicians are provided. Rather, literature is rapidly accumulating showing that multilevel (e.g., patient, provider, program, system) barriers and facilitating factors together are determinants of whether and to what degree empirically supported interventions are implemented (Chaudoir et al., 2013; also see the special section in the June 2011 [Vol. 25] issue of Psychology of Addictive Behaviors).
In light of these considerations, we maintain that other factors contributing to the gap between AUD clinical course research and clinical practice stem from research design and methods of analyses used to model data. Research designs that typify AUD clinical course research and that generate aggregate outcomes do not represent individual alcohol consumption trajectories after treatment initiation or completion (e.g., Gueorguieva et al., 2012). Furthermore, the statistical models typically used to analyze AUD clinical course data are not able to capture the moment-to-moment or abrupt changes in alcohol use that characterize the clinical course of AUD (e.g., Witkiewitz and Marlatt, 2007), and the level of data obtained typically has not been adequate to capture nonlinear, abrupt changes with any precision.
Future research on the clinical course of AUD to advance clinical practice
Given the shortcomings of current AUD clinical course data to characterize the clinical course of AUD, research that is better able to inform clinicians’ efforts to tailor treatment goals, intensity, and content to individual patients in a particular context over time is needed. Consequently, clinical course research could make a larger contribution to the advancement of AUD treatment if it yielded a level of data that could capture abrupt changes in alcohol consumption, included person-centered dynamic modeling approaches, and could emphasize individualized treatment. Accordingly, three research directions could help improve treatment and inform clinical decision-making for AUD clinicians: (a) near real-time data collection, (b) person-centered and dynamic modeling approaches, and (c) adaptive treatment designs.
Real-time data collection
Prior studies examining predictors of the clinical course of AUD have often focused on static predictors measured at baseline, even though models of the alcohol clinical course process call for a complex examination of a multitude of interconnected and time-varying risk factors (e.g., Witkiewitz and Marlatt, 2004). To gain a better understanding of the clinical course of AUD, it is necessary to capture the momentary changes in variables influencing treatment outcomes. One such method, called ecological momentary assessment (EMA; Shiffman et al., 2008), has already proven useful in untangling the real-time associations between risk factors and the clinical course of smoking. In a prospective study of momentary negative affect and smoking, Shiffman and Waters (2004) found that slow-changing affect and stress did not predict smoking lapses on the subsequent day, but same-day increases in negative affect were related to same-day lapses. From a clinical perspective, this day-by-day level of predicting lapses could greatly inform relapse-prevention interventions. Specifically, these findings inform the clinician on which high-risk situations (e.g., negative affect) are most likely to predict a smoking lapse and when the client may be most vulnerable to lapsing (e.g., substantial increases in negative affect).
EMA achieves this level of specificity because it is used to assess individuals in their own environment in near real-time (Shiffman et al., 2008). Thus, EMA can assess the precipitants and antecedents of substance use behaviors in vivo as the behavior is happening or shortly after the behavior has occurred. EMA researchers can select from a wide variety of sampling strategies best suited for the behavior under observation. For example, smart phones can be programmed to sample behavior at specific times, randomly throughout the day, or as initiated by the user, every time a specific event occurs.
Our encouraging the use of EMA as part of AUD clinical course research is in full recognition that, as with most methods of measurement, there are difficulties that must be contended with in collecting such data. These may include participant compliance, possible assessment reactivity, and expense due to payment to participants required to achieve acceptable compliance rates (Beal and Weiss, 2003). However, investigators in multiple health-related fields, including AUD clinical research, have concluded that the advantages of EMA data outweigh the disadvantages of collecting such data (McKay et al., 2006). Importantly, we believe that researchers using EMA will benefit from continued attention to these issues. The research questions, EMA design (e.g., number of times per day, question format), and analysis of EMA data are all crucial steps in generating valuable data from EMA.
Person-centered and dynamic modeling approaches
In addition to the valuable information near real-time data collection techniques yield, statistical methodologies may be used to provide additional insights. The statistical approaches used by many prior studies to predict drinking outcomes have largely been based on aggregate changes and may be insensitive to predict individual changes in drinking outcomes. Person-centered approaches (i.e., analytic techniques that estimate individual-level change), however, may be more effective in predicting drinking outcomes over time (Muthén and Muthén, 2000) and may also detect associations previously undetected using models based on aggregate change (Witkiewitz et al., 2010a).
The need for new statistical methods is apparent when considering the discrepancy between what widely used methods assume and what research suggests is true of the clinical course of AUD. Specifically, statistical models most commonly applied in the AUD clinical course literature often assume that continuous change in a specific degree or amount in predictor variables results in a proportionate change in degree or amount in an outcome variable. In contrast, the clinical course of AUD has been described as discontinuous (Skinner, 1989), meaning that continuous change in predictor variables results in disproportionate and sudden changes in alcohol use and related problems.
AUD clinical course concerns change over time (dynamic process), and empirical evidence from the AUD treatment outcome research literature favors the application of nonlinear dynamic models over the general linear model (e.g., Witkiewitz et al., 2007), as the clinical course of AUD is consistent with many of the characteristics of a nonlinear dynamic system (Gilmore, 1981). Importantly, the nonlinear nature of the clinical course of AUD has crucial implications for clinicians and researchers. A model accounting for the nonlinearity of AUD may identify different predictors of alcohol use and their timing than those inferred from linear models of change.
Adaptive treatment designs
Consistent with the need for more person-centered statistical modeling with AUD clinical course research is the shift toward more person-centered treatment options. With the existence of multiple efficacious treatments for substance use disorders (Miller and Wilbourne, 2002; Witkiewitz and Marlatt, 2011), the field is now moving toward a greater focus on personalized medicine (Hamburg and Collins, 2010). Recent efforts to personalize treatment approaches for AUD have ranged from individualizing treatment based on individual coping skills (Litt et al., 2009), pharmacogenetics (Johnson et al., 2011), and adaptive treatments (McKay et al., 2005a).
Adaptive treatment designs use algorithms to tailor treatment to an individual client. Such algorithms monitor changes in symptoms to adjust the treatment according to predetermined decision rules informed by research. In addition, baseline characteristics, such as genetics, can be used to further personalize treatment. Consequently, adaptive treatment designs allow a treatment provider to determine when and how to personalize and modify treatment to obtain optimal outcomes (Kranzler and McKay, 2012). However, research is only beginning to identify important variables for personalizing and modifying the treatment of AUD. Accordingly, adaptive treatment designs for AUD are still in the early phases of development. It is important to note that adaptive treatment designs differ from the patient-treatment matching literature cited earlier in that the latter typically considered static, pretreatment patient factors as the patient matching variables, compared with the more time-varying variables considered in adaptive designs.
To date, research on personalized and adaptive treatment has focused on identifying when and how to adapt and personalize treatment. O’Malley and colleagues (2003) used a nested sequence of randomized trials to examine when and how to adapt interventions for individuals with AUD. In this study, participants received naltrexone and were randomly assigned to receive either cognitive–behavioral therapy or primary care. Of those showing a good response to treatment after 10 weeks, participants were then randomized again to receive naltrexone or placebo. This study found that continued naltrexone was less beneficial for individuals who initially received cognitive–behavioral therapy. In another study, providing intensive, clinic-based continuing care to individuals who failed to reach the majority of treatment goals in intensive outpatient programs was found to be associated with better outcomes, whereas telephone continuing care resulted in better outcomes for responders to intensive outpatient program treatment (McKay et al., 2005a). Such results inform the emerging adaptive treatment design literature for when and how AUD treatments can be adapted to obtain optimal outcomes.
McKay and colleagues have highlighted variables important to treatment success, which may be used for developing decision rules for adaptive treatment designs. For example, gender and treatment history are important baseline variables to consider in personalizing AUD treatment (McKay and Hiller-Sturmhöfel, 2011). In contrast, motivation to change and social support for recovery are important to monitor throughout the course of treatment to obtain optimal outcomes (McKay et al., 2011). Despite promising initial findings, the factors associated with optimizing treatment outcomes are largely unknown. Without clearly identified variables that predict treatment success, creating adaptive treatment designs remains difficult. Consequently, identifying variables to personalize and optimize treatment is currently a practice of trial and error. However, current and future research can guide clinical decision-making in personalizing and adapting AUD treatment on the path toward adaptive treatment designs.
Using the resulting data to fill the gap
Combining new knowledge gained from research using EMA, person-centered and dynamic statistical modeling, and adaptive treatment design may ultimately provide clinicians with clinical decision support systems (CDSSs). A premise of this article is that our best effort in clinical decision-making can be achieved by applying the findings from clinical research. AUD clinical course data would be more easily applied to advance clinical practice by following the three directions for future research described in the previous sections. Of course, clinical decision-making would still be based on probabilities, but accuracy would be increased considerably by providing clinical course (and clinical trials) research findings that clinicians can more readily apply in treating their clients (Kazdin, 2008).
Early research has supported data-based decision-making as more useful and accurate than clinical judgment in predicting human behavior (Meehl, 1954). Recently, using treatment algorithms to inform patient-focused research has been advocated as an alternative approach to substance use disorders treatment research (Morgenstern and McKay, 2007). CDSSs have been developed for numerous medical conditions and have been shown to improve health care in diverse settings (Bright et al., 2012) and improve knowledge about treatment outcomes (Stacey et al., 2012). Although CDSSs have not been developed for AUDs, CDSSs for other chronic diseases (e.g., diabetes) have resulted in significant improvements in outcomes (Holbrook et al., 2009; Meigs et al., 2003).
As noted by Drake and colleagues (2010), the implementation of CDSSs may be particularly suited for mental health care, where patient–clinician interaction is often greater than in other medical settings. The CDSSs could provide valuable information for examining progress, which can ultimately promote patient-centeredness and personalized care. For example, in a cluster randomized clinical trial of 507 patients with schizophrenia and related disorders, Priebe and colleagues (2007) tested a computerized intervention that structured the patient–clinician dialogue to focus on patient quality of life and healthcare needs. Results showed that patients who received the computerized system had greater quality of life, fewer unmet treatment needs, and greater treatment satisfaction at a 12-month follow-up.
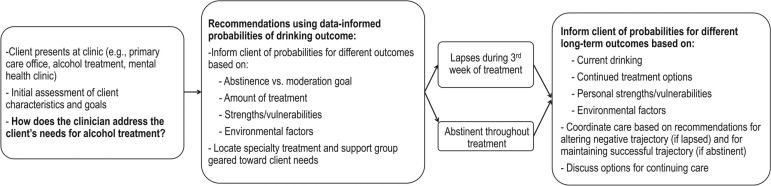
Figure 1 presents an example of how such a CDSS could be used in the context of AUD treatment. The CDSS could inform an individualized, likelihood-based approach to providing treatment recommendations. Figure 1 also helps to clarify how the kind of clinical course research recommended earlier directly contributes to a person-centered, individualized treatment-planning approach. Near real-time data obtained from EMA can add the assessment of time-varying factors (e.g., coping skills, self-efficacy) found to predict the clinical course of AUD along with more static variables typically measured in traditional AUD clinical course studies (e.g., AUD severity) (Witkiewitz and Marlatt, 2004).
Figure 1.
Hypothesized best practice guidelines using a clinical decision-making support system in alcohol use disorder treatment
The CDSS provided in Figure 1 could address multiple aspects of personalizing treatment to meet individual client needs. First, the initial treatment setting is an important determinant of the treatment trajectory. An individual who is initially screened at a primary care office may be more interested in a medical approach. Recent research has found extended-release naltrexone to be an effective intervention for reducing heavy drinking and increasing rates of abstinence in primary care (Lee et al., 2012), and future research could continue to examine what client characteristics best predict treatment response in primary care settings. The focus on strengths, vulnerabilities, and environmental factors is likely a crucial component of the CDSS, and much of the research on clinical course, described earlier, has identified factors that may predict probabilities of various drinking outcomes, such as gender, marital status, social support for abstinence, psychiatric comorbidity, financial support, and self-efficacy (Dawson et al., 2005; Ilgen et al., 2008; Moos and Moos, 2005, 2006, 2007; Satre et al., 2012). Despite these substantial contributions, however, AUD clinical course research should give more attention to conceptual development and to multiple indices of treatment outcome as crucial next steps in AUD clinical course research.
Further enhancing AUD clinical course research: Attention to conceptual development and multiple measures of functioning
The large majority of AUD clinical course research either has not demarcated milestones following treatment initiation or completion or has focused on AUD lapse/relapse. Any theoretical underpinning of clinical course research has been predominantly in the relapse area. Yet, the clinical course of AUD may include several clinically important “change points in [alcohol] use and [AUD] symptom status over time” (Chung and Maisto, 2006, p. 157) that could significantly advance the field if defined and operationalized. Such an innovation would enhance the value of clinical course research to clinicians and researchers alike by more precisely defining the clinical course of AUD and therefore targeting research findings to more targeted clinical contexts.
Moreover, a focus on AUD change points would be consistent with research done in other areas, such as the clinical course of depression (e.g., Frank et al., 1991), and has already developed preliminary findings. For example, Chung and Maisto (2006) defined and operationalized crucial change points in the clinical course of adolescent AUD to include the following: response is the beginning of the offset of all or some symptoms to a subdiagnostic threshold during treatment or a self-change attempt; remission occurs when the initial response is maintained and may be called full or partial; relapse may occur during a period of remission and is a signal of possible symptom reemergence; recovery is the continued absence of symptoms after the maximum time specified for full remission; and recurrence is the reappearance of symptoms of a disorder that occurs following a period of recovery. Each of these change points potentially corresponds to a critically different treatment approach (i.e., indicating if the individual requires a higher or lower level of care).
We acknowledge the complexity involved in identifying crucial change points because of differences among treatment populations and contexts. We also argue that operationalizing clinically important demarcations has direct implications for deriving algorithms to be used in adaptive treatment designs and thus would further their development. EMA data and person-centered data analytic techniques could provide data to derive demarcation points for future clinical algorithms, which may ultimately improve the content and timing of the “adaptive” component of adaptive treatment designs.
Multiple indices of treatment outcome
Throughout this article and the AUD clinical course literature, the focus has been on alcohol consumption as the AUD “symptom” (although in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, consumption per se is not a symptom of AUD [American Psychiatric Association, 2013]) to be monitored in AUD treatment and clinical course. This is sensible from the perspective of AUD treatment consumers, as alcohol use typically is the major concern among individuals who present for treatment as well as for their social network members, because the typical perception is that many life problems are directly attributable to excessive alcohol use. Furthermore, alcohol use is ostensibly straightforward to measure, and any changes in such use have a clear interpretation. Nevertheless, AUD is a biopsychosocial disorder that is associated with multiple areas of life functioning that also typically are part of the clinical presentation and must be addressed in treatment. Consideration of multiple areas of life functioning as part of AUD clinical research and practice is not a new idea (Sobell et al., 1987) but also is not an idea that has been pursued systematically. For example, there is no consensus on what would constitute a “core set” of outcome variables for any treatment population or setting (cf., Tiffany et al., 2012), although there have been attempts to derive composite measures of outcome that include alcohol consumption and other areas of life functioning (Zweben and Cisler, 2003). AUD clinical course research that incorporates the conceptualization of AUD as a biopsychosocial problem that has multiple determinants and consequences would be of greater relevance to clinicians and the complexity of cases they treat.
Summary and conclusions
In this article, we have provided an overview of AUD clinical course research and how it has contributed to the advancement of AUD treatment. We also have argued that, despite its significant contributions to improving AUD treatment, AUD clinical course research has not provided clinicians with the information they need to aid their decision-making about the treatment of individual patients. Accordingly, we have suggested three major research directions AUD clinical course research could take to further the development of an evidence-based clinical decision-making support system. Such a system, unprecedented in the alcohol treatment field, could be widely disseminated to clinicians, program evaluators, and policy makers to help improve alcohol treatment decision-making and ultimately to improve AUD treatment outcomes.
Footnotes
This research was supported by Senior Career Scientist Research and Mentoring Award 2K05 AA16928 (to Stephen A. Maisto, principal investigator), by a training fellowship to Megan Kirouac (1T32 AA0018108-01A1; Barbara S. McCrady, principal investigator), and by National Institute on Alcohol Abuse and Alcoholism Grant 1R01 AA022328 (to Katie Witkiewitz, principal investigator).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: Author; 2013. [Google Scholar]
- Beal DJ, Weiss HM. Methods of ecological momentary assessment in organizational research. Organizational Research Methods. 2003;6:440–464. [Google Scholar]
- Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, Lobach D. Effect of clinical decision-support systems: A systematic review. Annals of Internal Medicine. 2012;157:29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, Dugan AG, Barr CHI. Measuring factors affecting implementation of health innovations: A systematic review of structural, organizational, provider, patient, and innovation level measures. Implementation Science. 2013;8(22) doi: 10.1186/1748-5908-8-22. Retrieved from http://www.implementationscience.com/content/8/1/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: Review and reconsideration of relapse as a change point in clinical course. Clinical Psychology Review. 2006;26:149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Drake RE, Deegan PE, Woltmann E, Haslett W, Drake T, Rapp CA. Comprehensive electronic decision support systems. Psychiatric Services. 2010;61:714–717. doi: 10.1176/ps.2010.61.7.714. [DOI] [PubMed] [Google Scholar]
- Edwards G. Drinking in longitudinal perspective: Career and natural history. British Journal of Addiction. 1984;79:175–183. doi: 10.1111/j.1360-0443.1984.tb00260.x. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: Provisional description of a clinical syndrome. British Medical Journal. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, Litten RZ. Percentage of subjects with no heavy drinking days: Evaluation as an efficacy endpoint for alcohol clinical trials. Alcoholism: Clinical and Experimental Research. 2010;34:2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Weissman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: Remission, recovery, relapse, and recurrence. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Gilmore R. Catastrophe theory for scientists and engineers. New York, NY: Wiley; 1981. [Google Scholar]
- Glatt MM. Group therapy in alcoholism. British Journal of Addiction to Alcohol & Other Drugs. 1958;54:133–148. [Google Scholar]
- Gueorguieva R, Wu R, Donovan D, Rounsaville BJ, Couper D, Krystal JH, O’Malley SS. Baseline trajectories of heavy drinking and their effects on postrandomization drinking in the COMBINE Study: Empirically derived predictors of drinking outcomes during treatment. Alcohol. 2012;46:121–131. doi: 10.1016/j.alcohol.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamburg MA, Collins FS. The path to personalized medicine. The New England Journal of Medicine. 2010;363:301–304. doi: 10.1056/NEJMp1006304. [DOI] [PubMed] [Google Scholar]
- Heather N, Adamson SJ, Raistrick D, Slegg GP the UKATT Research Team. Initial preference for drinking goal in the treatment of alcohol problems: I. Baseline differences between abstinence and non-abstinence groups. Alcohol and Alcoholism. 2010;45:128–135. doi: 10.1093/alcalc/agp096. [DOI] [PubMed] [Google Scholar]
- Holbrook A, Thabane L, Keshavjee K, Dolovich L, Bernstein B, Chan D, Gerstein H the COMPETE II Investigators. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. Canadian Medical Association Journal. 2009;181:37–44. doi: 10.1503/cmaj.081272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt WA, Barnett LW, Branch LG. Relapse rates in addiction programs. Journal of Clinical Psychology. 1971;27:455–456. doi: 10.1002/1097-4679(197110)27:4<455::aid-jclp2270270412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Wilbourne PL, Moos BS, Moos RH. Problem-free drinking over 16 years among individuals with alcohol use disorders. Drug and Alcohol Dependence. 2008;92:116–122. doi: 10.1016/j.drugalcdep.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jellinek EM. The disease concept of alcoholism. New Haven, CT: Hillhouse Press; 1960. [Google Scholar]
- Johnson BA, Ait-Daoud N, Seneviratne C, Roache JD, Javors MA, Wang X-Q, Li MD. Pharmacogenetic approach at the serotonin transporter gene as a method of reducing the severity of alcohol drinking. American Journal of Psychiatry. 2011;168:265–275. doi: 10.1176/appi.ajp.2010.10050755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist. 2008;63:146–159. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Kline-Simon AH, Falk DE, Litten RZ, Mertens JR, Fertig J, Ryan M, Weisner CM. Posttreatment low-risk drinking as a predictor of future drinking and problem outcomes among individuals with alcohol use disorders. Alcoholism: Clinical and Experimental Research, 37, Supplement. 2013;1:E373–E380. doi: 10.1111/j.1530-0277.2012.01908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranzler HR, McKay JR. Personalized treatment of alcohol dependence. Current Psychiatry Reports. 2012;14:486–493. doi: 10.1007/s11920-012-0296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Morgenstern J, Hail L. Predictors of moderated drinking in a primarily alcohol-dependent sample of men who have sex with men. Psychology of Addictive Behaviors. 2012;26:484–495. doi: 10.1037/a0026713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JD, Grossman E, Huben L, Manseau M, McNeely J, Rotrosen J, Gourevitch MN. Extended-release naltrexone plus medical management alcohol treatment in primary care: Findings at 15 months. Journal of Substance Abuse Treatment. 2012;43:458–462. doi: 10.1016/j.jsat.2012.08.012. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E. Individualized assessment and treatment program for alcohol dependence: Results of an initial study to train coping skills. Addiction. 2009;104:1837–1838. doi: 10.1111/j.1360-0443.2009.02693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Longabaugh R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. Journal of Studies on Alcohol. 2002;63:397–403. doi: 10.15288/jsa.2002.63.397. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ. Relapse in the addictive behaviors: Integration and future directions. Clinical Psychology Review. 2006;26:229–231. doi: 10.1016/j.cpr.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of three-year outcomes. Journal of Studies on Alcohol and Drugs. 2007;68:419–427. doi: 10.15288/jsad.2007.68.419. [DOI] [PubMed] [Google Scholar]
- Maisto SA, McKay JR, O’Farrell TJ. Twelve-month abstinence from alcohol and long-term drinking and marital outcomes in men with severe alcohol problems. Journal of Studies on Alcohol. 1998;59:591–598. doi: 10.15288/jsa.1998.59.591. [DOI] [PubMed] [Google Scholar]
- McKay JR. Treating substance use disorders with adaptive continuing care. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- McKay JR, Franklin TR, Patapis N, Lynch KG. Conceptual, methodological, and analytical issues in the study of relapse. Clinical Psychology Review. 2006;26:109–127. doi: 10.1016/j.cpr.2005.11.002. [DOI] [PubMed] [Google Scholar]
- McKay JR, Hiller-Sturmhöfel S. Treating alcoholism as a chronic disease: Approaches to long-term continuing care. Alcohol Research & Health. 2011;33:356–370. [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Morgenstern J, Forman RF, Pettinati HM. Do patient characteristics and initial progress in treatment moderate the effectiveness of telephone-based continuing care for substance use disorders? Addiction. 2005a;100:216–226. doi: 10.1111/j.1360-0443.2005.00972.x. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Archives of General Psychiatry. 2005b;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Oslin DW, Ivey M, Drapkin ML, Coviello DM, Lynch KG. Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction. 2011;106:1760–1769. doi: 10.1111/j.1360-0443.2011.03483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehl PE. Clinical versus statistical prediction: A theoretical analysis and a review of the evidence. Minneapolis, MN: University of Minnesota Press; 1954. [Google Scholar]
- Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, Nathan DM. A controlled trial of web-based diabetes disease management: The MGH Diabetes Primary Care Improvement Project. Diabetes Care. 2003;26:750–757. doi: 10.2337/diacare.26.3.750. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Flisher AJ, Satre DD, Weisner CM. The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug and Alcohol Dependence. 2008;98:45–53. doi: 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Kline-Simon AH, Delucchi KL, Moore C, Weisner CM. Ten-year stability of remission in private alcohol and drug outpatient treatment: Non-problem users versus abstainers. Drug and Alcohol Dependence. 2012;125:67–74. doi: 10.1016/j.drugalcdep.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner CM, Ray GT. Readmission among chemical dependency patients in private, outpatient treatment: Patterns, correlates and role in long-term outcome. Journal of Studies on Alcohol. 2005;66:842–847. doi: 10.15288/jsa.2005.66.842. [DOI] [PubMed] [Google Scholar]
- Miller WR, Wilbourne PL. Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Sixteen-year changes and stable remission among treated and untreated individuals with alcohol use disorders. Drug and Alcohol Dependence. 2005;80:337–347. doi: 10.1016/j.drugalcdep.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Treated and untreated alcohol-use disorders: Course and predictors of remission and relapse. Evaluation Review. 2007;31:564–584. doi: 10.1177/0193841X07306749. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, McKay JR. Rethinking the paradigms that inform behavioral treatment research for substance use disorders. Addiction. 2007;102:1377–1389. doi: 10.1111/j.1360-0443.2007.01882.x. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- O’Malley SS, Rounsaville BJ, Farren C, Namkoong K, Wu R, Robinson J, O’Connor PG. Initial and maintenance naltrexone treatment for alcohol dependence using primary care vs specialty care: A nested sequence of 3 randomized trials. Archives of Internal Medicine. 2003;163:1695–1704. doi: 10.1001/archinte.163.14.1695. [DOI] [PubMed] [Google Scholar]
- Orford J, Oppenheimer E, Edwards G. Abstinence or control: The outcome for excessive drinkers two years after consultation. Behaviour Research and Therapy. 1976;14:409–418. doi: 10.1016/0005-7967(76)90087-5. [DOI] [PubMed] [Google Scholar]
- Priebe S, McCabe R, Bullenkamp J, Hansson L, Lauber C, Martinez-Leal R, Wright DJ. Structured patient–clinician communication and 1-year outcome in community mental healthcare: Cluster randomised controlled trial. British Journal of Psychiatry. 2007;191:420–426. doi: 10.1192/bjp.bp.107.036939. [DOI] [PubMed] [Google Scholar]
- Ray GT, Weisner CM, Mertens XR. Relationship between use of psychiatric services and five-year alcohol and drug treatment outcomes. Psychiatric Services. 2005;56:164–171. doi: 10.1176/appi.ps.56.2.164. [DOI] [PubMed] [Google Scholar]
- Rosenberg H. Prediction of controlled drinking by alcoholics and problem drinkers. Psychological Bulletin. 1993;113:129–139. doi: 10.1037/0033-2909.113.1.129. [DOI] [PubMed] [Google Scholar]
- Rosenberg H, Davis L-A. Acceptance of moderate drinking by alcohol treatment services in the United States. Journal of Studies on Alcohol. 1994;55:167–172. doi: 10.15288/jsa.1994.55.167. [DOI] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Mertens XR, Weisner CM. Effects of age and life transitions on alcohol and drug treatment outcome over nine years. Journal of Studies on Alcohol and Drugs. 2012;73:459–468. doi: 10.15288/jsad.2012.73.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott DM, Williams CD, Cain GE, Kwagyan J, Kalu N, Ehlers CL, Taylor RE. Clinical course of alcohol dependence in African Americans. Journal of Addictive Diseases. 2008;27:43–50. doi: 10.1080/10550880802324754. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ. Negative affect and smoking lapses: A prospective analysis. Journal of Consulting and Clinical Psychology. 2004;72:192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- Skinner HA. Butterfly wings flapping: Do we need more ‘chaos’ in understanding addictions. British Journal of Addiction. 1989;84:353–356. doi: 10.1111/j.1360-0443.1989.tb00577.x. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Brochu S, Sobell LC, Roy J, Stevens JA. Alcohol treatment outcome evaluation methodology: State of the art 1980-1984. Addictive Behaviors. 1987;12:113–128. doi: 10.1016/0306-4603(87)90018-9. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC. It is time for low-risk drinking goals to come out of the closet. Addiction. 2011;106:1715–1717. doi: 10.1111/j.1360-0443.2011.03509.x. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Bogardis J, Leo GI, Skinner W. Problem drinkers’ perceptions of whether treatment goals should be self-selected or therapist-selected. Behavior Therapy. 1992;23:43–52. [Google Scholar]
- Stacey D, Kryworuchko J, Bennett C, Murray MA, Mullan S, Légaré F. Decision coaching to prepare patients for making health decisions: A systematic review of decision coaching in trials of patient decision AIDS. Medical Decision Making. 2012;32:E22–E33. doi: 10.1177/0272989X12443311. [DOI] [PubMed] [Google Scholar]
- Taylor C, Brown D, Duckitt A, Edwards G, Oppenheimer E, Sheehan M. Alcoholism and the patterning of outcome: A multivariate analysis. British Journal of Addiction. 1986;81:815–823. doi: 10.1111/j.1360-0443.1986.tb00409.x. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Friedman L, Greenfield SF, Hasin DS, Jackson R. Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction. 2012;107:709–718. doi: 10.1111/j.1360-0443.2011.03581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Hartzler B, Donovan D. Matching motivation enhancement treatment to client motivation: Re-examining the Project MATCH motivation matching hypothesis. Addiction. 2010a;105:1403–1413. doi: 10.1111/j.1360-0443.2010.02954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Maisto SA, Donovan DM. A comparison of methods for estimating change in drinking following alcohol treatment. Alcoholism: Clinical and Experimental Research. 2010b;34:2116–2125. doi: 10.1111/j.1530-0277.2010.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Modeling the complexity of post-treatment drinking: It’s a rocky road to relapse. Clinical Psychology Review. 2007;27:724–738. doi: 10.1016/j.cpr.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt A. Behavioral therapy across the spectrum. Alcohol Research & Health. 2011;33:313–319. [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychology of Addictive Behaviors. 2008;22:157–167. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, van der Maas HLJ, Hufford MR, Marlatt GA. Nonnormality and divergence in posttreatment alcohol use: Re-examining the Project MATCH data “another way.”. Journal of Abnormal Psychology. 2007;116:378–394. doi: 10.1037/0021-843X.116.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global Status Report on Alcohol and Health. Geneva, Switzerland: Author; 2011. [Google Scholar]
- Zweben A, Cisler RA. Clinical and methodological utility of a composite outcome measure for alcohol treatment research. Alcoholism: Clinical and Experimental Research. 2003;27:1680–1685. doi: 10.1097/01.ALC.0000091237.34225.D7. [DOI] [PubMed] [Google Scholar]