Abstract
Objective:
This study aimed to (a) characterize gender-specific risk of onset of alcohol, nicotine, and marijuana use developmentally; (b) investigate the effects of early-onset status and frequency of nicotine and marijuana use on alcohol outcomes, controlling for the effects of alcohol use; and (c) examine gender differences in the developmental trajectories of alcohol outcomes and the effects of nicotine and marijuana use on alcohol outcomes.
Method:
This study conducted secondary analysis on a longitudinal study that recruited at-risk youth through fathers’ drunk-driving records and door-to-door canvassing in the midwestern United States. The sample included 160 female–male sibling pairs who were assessed on substance use and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, diagnosis from early childhood to young adulthood.
Results:
Although males were at higher risk for being early-onset alcohol users, females tended to be at higher risk for initiating marijuana use at younger ages. When early onset and amount of alcohol use were controlled for, early onset of nicotine and marijuana use did not contribute to alcohol outcomes, but frequencies of nicotine and marijuana use did. We also found the associations of quantity/frequency of alcohol and marijuana use with drinking problems to be stronger among females than among males.
Conclusions:
Higher frequencies of nicotine and marijuana use may contribute to worse alcohol outcomes above and beyond the effect of alcohol use. Females tend to be at higher risk than males for initiating marijuana use and meeting an alcohol use disorder diagnosis at younger ages as well as being more vulnerable to a negative impact of alcohol and marijuana use.
A national survey found that alcohol use is highly comorbid with nicotine use and marijuana use among young people (Jackson et al., 2008). Yet, our knowledge is limited about the effects of nicotine and marijuana use on alcohol-related problems or alcohol use disorders (AUDs) above and beyond the well-known effects of early onset of alcohol use and the amount of alcohol consumption. Further, although the literature indicates that women tend to have a lower prevalence rate of AUDs (Hasin et al., 2007) and be more vulnerable to the negative effects of alcohol use (Nolen-Hoeksema, 2004) than men, gender differences are not clear regarding the risk of onset of alcohol, nicotine, and marijuana use across developmental periods as well as the effects of nicotine and marijuana use on alcohol outcomes. Understanding these gender differences might help us better design prevention and intervention programs tailored to the special timing and needs of each gender group.
Previous studies have shown that early onset of alcohol use is highly predictive of alcohol problems or AUDs (Behrendt et al., 2009; Buu et al., 2012; Dawson, 2000; DeWit et al., 2000). Early onset of nicotine use (Grant, 1998; Lewinsohn et al., 1999) or marijuana use (Grant et al., 2010; Kirisci et al., 2013) was also found to be associated with AUDs. A major limitation of this line of research is that the association between early onset of nicotine or marijuana use and alcohol outcomes has been mostly established without taking into account the effects of early onset of alcohol use and the amount of alcohol consumption. It is, therefore, unclear if the observed association is simply the result of early-onset drinkers or heavy drinkers also being early-onset users of nicotine or marijuana. Furthermore, a potential gender difference in such an association could have important implications for gender-specific intervention but has not yet been examined. Thus, it is a research question open to investigation.
National surveys of the U.S. adult population have shown that men tend to initiate alcohol use at earlier ages than women (Alvanzo et al., 2011; Keyes et al., 2010). A national survey of high school students in the United States also indicated that males are more likely than females to initiate smoking at younger ages (Everett et al., 1999). Nevertheless, another study on a treatment sample of adolescent smokers did not find any gender difference in the onset age of nicotine use (Thorner et al., 2007). Although we were not able to find national data on gender differences in the onset age of marijuana use, no gender difference was found among a community sample of middle-aged adults with lifetime alcohol dependence (Ehlers et al., 2010). A common limitation of these existing studies is that they are all cross-sectional; therefore, the accuracy of retrospective reports on onset ages of substance use remains a major concern, especially for individuals who had been using the substance for some years before data collection. Thus, a prospective longitudinal design that follows youth developmentally is highly desirable for a better understanding of gender differences in the risk of onset of these most commonly used substances. Further, statistical analysis characterizing the gender-specific risk for these substances across developmental ages can inform the optimal timing for prevention or intervention.
A national survey indicated that smokers had 4.5-fold higher odds of AUDs than never-smokers, after adjusting for drinking quantity (Grucza and Bierut, 2006). Another national survey found that the association between smoking and AUDs was greater among women than men (Husky et al., 2007). Such a gender effect was, however, tested without controlling for drinking quantity and thus could reflect women’s higher vulnerability to negative effects of alcohol consumption, because drinking and smoking are highly comorbid. Furthermore, although marijuana use has been legalized in a growing number of states and its prevalence has increased drastically in recent years (Miech and Koester, 2012), studies of its effect on alcohol-related problems or AUDs are sparse. A cross-sectional study in college students found that when drinking frequency was controlled for, marijuana use was associated with alcohol problems but nicotine use was not (Fenzel, 2005). In addition, the same study did not find a gender difference in the association between marijuana use and alcohol problems.
This study fills in the current knowledge gaps by conducting secondary analysis of data from a prospective longitudinal study in high-risk youth from early childhood to young adulthood. The first objective of this study was to characterize the gender-specific risk of onset of alcohol, nicotine, and marijuana use across developmental periods. The second objective was to investigate the longitudinal effects of early-onset status and frequency of nicotine and marijuana use on problem alcohol outcomes (including alcohol-related problems and AUD diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV; American Psychiatric Association, 1994]), controlling for early-onset status of alcohol use and the amount of alcohol consumption. The third objective was to examine if there are gender differences in the developmental trajectories of problem alcohol outcomes as well as in the effects of alcohol, nicotine, and marijuana use (including onset and quantity/frequency) on problem alcohol outcomes.
Method
Design and sample
The present study is part of the Michigan Longitudinal Study (MLS), an ongoing, multiwave, prospective study of families at high risk for substance use disorders spanning more than 20 years (Zucker et al., 1996, 2000). Participants were families ascertained through two interconnected population-based methods carried out in a four-county-wide area in the Midwest. Ascertainment of the highest risk portion of the sample was by way of the father’s drunk driving conviction with a sufficiently high blood alcohol concentration (.15% if a first conviction, .12% if multiple convictions) to virtually ensure that a later AUD diagnosis would be obtained. The remaining families were systematically recruited door to door in the same neighborhoods as the drunk-driver families, thus controlling for neighborhood ecological influences. Previous analyses from the MLS indicating significant neighborhood influences on long-term health outcomes in both parent and offspring suggest the importance of such a geographical control (Buu et al., 2007, 2009). The recruitment protocol also required the father to be living with a 3- to 5-year-old son (the male target child) and the boy’s biological mother. The study families were originally recruited as triads, but thereafter siblings within 8 years of the initial male target child were also recruited.
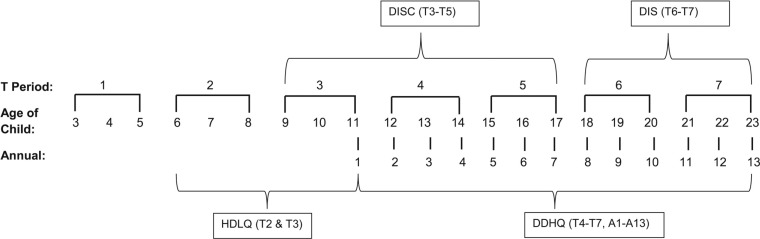
Participant families received extensive in-home assessments at baseline, and assessment waves thereafter took place at 3-year intervals (denoted as T). During the crucial period of alcohol use development in much of the U.S. population (ages 11–23; Wagner and Anthony, 2002), annual assessments (denoted as A) also were conducted. The various time points of assessments along with the specific measures administered are shown in Figure 1.
Figure 1.
The assessment schedule and substance use related measures of the Michigan Longitudinal Study. T = time; DISC = Diagnostic Interview Schedule for Children; DIS = Diagnostic Interview Schedule; HDLQ = Health and Daily Living Questionnaire; DDHQ = Drinking and Drug History Questionnaire.
The analysis of the present study used the longitudinal data from 160 participant families, each of which had a female–male sibling pair consisting of the male target child and his female sibling nearest in age. This design allowed us to examine gender differences developmentally while controlling for important confounds such as family density of alcoholism, demographic background, and unequal sample sizes of the gender groups. Sibling pairs have been used in observational studies to reduce heterogeneity (Altonji and Dunn, 1996; Dick et al., 2000). According to statistical theories, reducing heterogeneity reduces both sampling variability and sensitivity to unobserved bias, whereas increasing the sample size only reduces sampling variability but does little to reduce unobserved bias (Rosenbaum, 2005). Therefore, it is worth adopting this design despite the cost of reducing the sample size.
In this subsample, 72.5% of the families had at least one parent with lifetime DSM-IV AUD diagnosis. This number is slightly lower than that of the entire MLS sample of 298 families (76.51%). Their parents had on average 13.59 (SD = 1.94) years of education. The median family income was in the range of $30,000–$50,000. These demographic characteristics were comparable to the ones of the overall MLS sample (the average years of parental education = 13.47 [SD = 1.85]; the median family income = $30,000–$50,000). Further, among the 160 sibling pairs, the sister was on average 1.46 years older than the brother, with a wide range of -8 to 8 in age differences. About 38% of the MLS families had more than two children. For those families that had more than one daughter, the girl closest in age to the male target child was chosen to minimize the age difference between the two gender groups.
Measures
Onset ages of alcohol, nicotine, and marijuana use.
The Drinking and Drug History Questionnaire (DDHQ; Zucker et al., 1990) and the Health and Daily Living Questionnaire (HDLQ) were used to determine the onset ages of alcohol, nicotine, and marijuana use. The DDHQ incorporates items from national epidemiologic studies of drugs and alcohol (Cahalan et al., 1969; Johnston et al., 1979) as well as from a structured clinical symptom questionnaire (Schuckit, 1978). All of the items have been extensively used in a variety of survey and clinical settings. They provide data on quantity, frequency, and consequences of substance use. The instrument was administered at T4–T7 (ages 12–23) and A1–A13 (ages 11–23). The HDLQ is a younger children’s version of the DDHQ with items modified to be relevant for children under age 12 but covering the same substantive areas. The HDLQ was administered at T2–T3 (ages 6–11). To address reading difficulties at these younger ages, the HDLQ was administered in interview format in a room that separated the children from their parents to ensure privacy.
At each wave, the onset ages of alcohol, nicotine, and marijuana use were asked (the exact wording of the onset age of alcohol use was: “How old were you the first time you ever took a drink? Do not count the times when you were given a ‘sip’ by an adult.”). When there was discrepancy across waves, we took the age reported at the earliest wave as the best estimate because it was the least retrospective account (Parra et al., 2003). Those onset ages reported during childhood (T2–T3) were further validated using the onset ages consistently reported in later waves. Although the alcohol literature has a commonly adopted cutoff age of 14 for early-onset drinkers (Hingson et al., 2006), the definition of early onset for nicotine use and marijuana use varies across studies. In our study sample, the proportion of users who had the onset age of 14 or younger was 59% for alcohol, 48% for nicotine, and 42% for marijuana. Because moving the cutoff age by 1 year in either direction would drive the proportion further away from 50% for every substance, we defined the age for early-onset use of each of the substances as 14 or younger.
Amount of alcohol consumption, frequency of nicotine or marijuana use, and alcohol-related problems.
At each wave, the DDHQ (administered from ages 11 to 23) inquired about the average number of drinking days per month and the average number of drinks per drinking day in the past 6 months. We multiplied these two numbers together to estimate the amount of alcohol consumption at each wave. We also adopted the two items in the DDHQ that dealt with the frequency of nicotine use and the frequency of marijuana use in the past 12 months to quantify the use of these two substances. The item for nicotine use was a 0–4 scale (0 = never; 1 = once or twice; 2 = occasionally but not regularly; 3 = regularly for a while, but not now; 4 = regularly now). The item for marijuana use was a 0–7 scale (0 = none; 1 = 1–2 occasions; 2 = 3–5 occasions; 3 = 6–9 occasions; 4 = 10–19 occasions; 5 = 20–39 occasions; 6 = 40–99 occasions; 7 = ≥100 occasions). In addition to alcohol use patterns, the DDHQ consistently asked about 21 alcohol-related problems across waves, such as losing friends, getting a ticket for drunk driving, etc. We summed the number of problems at each wave as an indicator of alcohol outcomes.
DSM-IV alcohol use disorder diagnosis.
A doctoral-level clinical psychologist conducted year-by-year DSM-IV AUD diagnoses using information from the Diagnostic Interview Schedule (DIS; Robins et al., 1980, 1996) and the Diagnostic Interview Schedule for Children (DISC; Shaffer et al., 2000), supplemented by information from the DDHQ and HDLQ (described above). The DIS and DISC are well-validated and widely used diagnostic instruments that allow trained interviewers to gather extensive information about psychiatric, physical, alcohol-related, and other-drug-related symptoms. The DISC was administered at Waves T3–T5 (ages 9–17), and the DIS was administered at T6 and T7 (ages 18–23). The DIS/DISC data were used as the base to provide a best-estimate diagnosis, supplemented by the DDHQ/HDLQ data, under the principle that when a symptom was admitted, even from only one source, it probably was present. Interrater reliability was established by having another clinical psychologist blindly diagnose a subset of the protocols (κ = .81).
Analytic approach
The first objective of this study was to characterize the gender-specific developmental risk of onset of alcohol, nicotine, and marijuana use. We graphed the hazard function, which assesses the chance (risk) that a nonuser will start using the substance at the next instant, for males and females from birth to age 23 for each substance. These graphs allow us to identify developmental variations in pattern of emergence for substance use as well as the periods with the highest probability for its emergence. We estimated the hazard function using a kernel smoothing method implemented in the R package muhaz (cran.r-project.org/web/packages/muhaz). Technical details such as the global and local bandwidth selection algorithms and the boundary kernel formulations are described in Müller and Wang (1994). Moreover, the log-rank test and Wilcoxon test were adopted to examine gender differences in risk of onset of substance use (Klein and Moeschberger, 1997).
The second objective of this study was to investigate the longitudinal effects of nicotine and marijuana use on problem alcohol outcomes while controlling for the effect of alcohol use. The linear mixed model (Verbeke and Molenberghs, 2000) was used to predict alcohol-related problems; the generalized linear mixed model (Molenberghs and Verbeke, 2005) was fitted for AUD diagnoses. These models took account of the nonindependence of female–male sibling pairs and repeated measures within subjects by involving random effects. We first modeled the trajectories of alcohol outcomes by entering the intercept, the linear term of age, and the quadratic term of age in order. The higher order terms were only kept in the models if they were significant (p < .05) given the lower order terms. The second block of variables, the early-onset status of alcohol use and alcohol consumption, served as the control variables and remained in the models whether or not they were significant because we wanted to examine the effects of nicotine and marijuana use above and beyond the effect of alcohol use. Conditioning on the trajectories and the effect of alcohol use, we tested the effect of nicotine use (including early-onset status and frequency) before the effect of marijuana use (including early-onset status and frequency) because alcohol and nicotine have been suggested as “gateway drugs” for progression to marijuana use (Kandel et al., 1992).
We only kept the variables related to nicotine or marijuana use that had significant effects in the models. Our preliminary analysis using two dummy variables (the first variable contrasting early-onset users vs. the others; the second variable contrasting late-onset users vs. the others) showed that only the first variable was significant. Thus, we only included the first dummy variable in the analysis (i.e., nonusers and late-onset users together served as the reference group).
The third objective of this study was to examine if there are gender differences in the developmental trajectories of problem alcohol outcomes as well as in the effects of alcohol, nicotine, and marijuana use (including onset and quantity/frequency) on problem alcohol outcomes. To achieve this objective, we tested gender effects in the final stage of model building by entering the interactions between gender (male was coded as 1, female as 0) and each of the main effects remaining in the models from previous steps. Interactions were tested individually, and only the significant interaction terms were retained in the final models.
Results
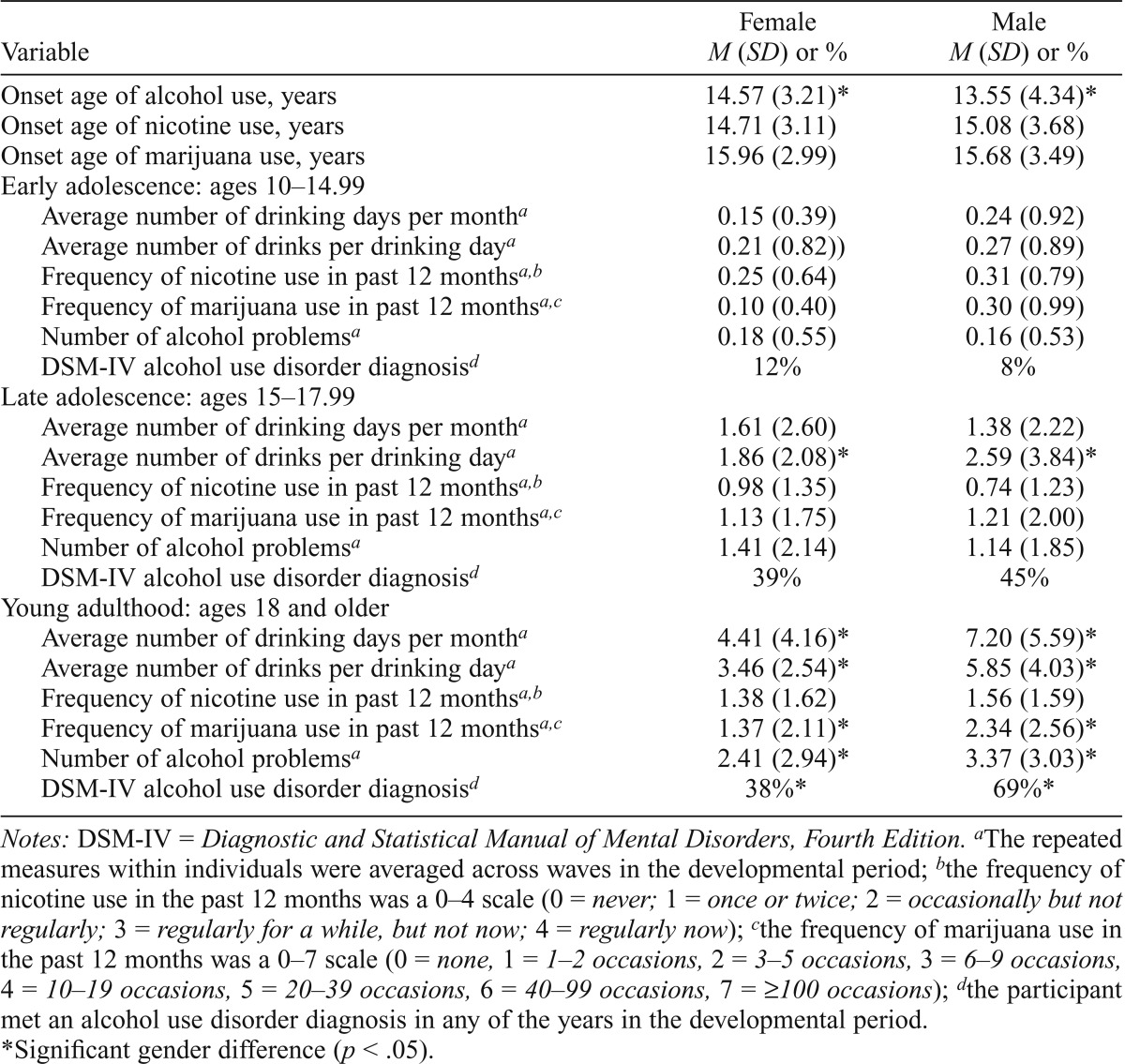
Table 1 shows the means and standard deviations of the onset ages, quantity/frequency of substance use, number of alcohol problems, and percentages of participants who met DSM-IV AUD diagnosis by gender. The paired t test was used to take account of the nonindependence of female and male samples. On average, males had an earlier onset age of alcohol use, whereas there was no gender difference in onset ages of nicotine and marijuana use. We took a developmental approach to examine gender differences in quantity/frequency of substance use and alcohol outcomes during three developmental periods: early adolescence (ages 10–14.99), late adolescence (ages 15–17.99), and young adulthood (ages 18 and older). In early adolescence, the levels of use and problems were low for both genders and there was no gender difference. In late adolescence, we observed some increases for both gender groups but only found one significant difference: Males consumed more drinks per drinking day. In young adulthood, there were significant gender differences in all substance use and alcohol outcomes except for nicotine use.
Table 1.
Gender differences in onset ages, quantity/frequency, and outcomes of substance use (N = 320)
| Female | Male | |
| Variable | M (SD) or % | M (SD) or % |
| Onset age of alcohol use, years | 14.57 (3.21)* | 13.55 (4.34)* |
| Onset age of nicotine use, years | 14.71 (3.11) | 15.08 (3.68) |
| Onset age of marijuana use, years | 15.96 (2.99) | 15.68 (3.49) |
| Early adolescence: ages 10–14.99 | ||
| Average number of drinking days per montha | 0.15 (0.39) | 0.24 (0.92) |
| Average number of drinks per drinking daya | 0.21 (0.82)) | 0.27 (0.89) |
| Frequency of nicotine use in past 12 monthsa,b | 0.25 (0.64) | 0.31 (0.79) |
| Frequency of marijuana use in past 12 monthsa,c | 0.10 (0.40) | 0.30 (0.99) |
| Number of alcohol problemsa | 0.18 (0.55) | 0.16 (0.53) |
| DSM-IV alcohol use disorder diagnosisd | 12% | 8% |
| Late adolescence: ages 15–17.99 | ||
| Average number of drinking days per montha | 1.61 (2.60) | 1.38 (2.22) |
| Average number of drinks per drinking daya | 1.86 (2.08)* | 2.59 (3.84)* |
| Frequency of nicotine use in past 12 monthsa,b | 0.98 (1.35) | 0.74 (1.23) |
| Frequency of marijuana use in past 12 monthsa,c | 1.13 (1.75) | 1.21 (2.00) |
| Number of alcohol problemsa | 1.41 (2.14) | 1.14 (1.85) |
| DSM-IV alcohol use disorder diagnosisd | 39% | 45% |
| Young adulthood: ages 18 and older | ||
| Average number of drinking days per montha | 4.41 (4.16)* | 7.20 (5.59)* |
| Average number of drinks per drinking daya | 3.46 (2.54)* | 5.85 (4.03)* |
| Frequency of nicotine use in past 12 monthsa,b | 1.38 (1.62) | 1.56 (1.59) |
| Frequency of marijuana use in past 12 monthsa,c | 1.37 (2.11)* | 2.34 (2.56)* |
| Number of alcohol problemsa | 2.41 (2.94)* | 3.37 (3.03)* |
| DSM-IV alcohol use disorder diagnosisd | 38%* | 69%* |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
The repeated measures within individuals were averaged across waves in the developmental period;
the frequency of nicotine use in the past 12 months was a 0–4 scale (0 = never; 1 = once or twice; 2 = occasionally but not regularly; 3 = regularly for a while, but not now; 4 = regularly now);
the frequency of marijuana use in the past 12 months was a 0–7 scale (0 = none, 1 = 1–2 occasions, 2 = 3–5 occasions, 3 = 6–9 occasions, 4 = 10–19 occasions, 5 = 20–39 occasions, 6 = 40–99 occasions, 7 = ≥100 occasions);
the participant met an alcohol use disorder diagnosis in any of the years in the developmental period.
Significant gender difference (p < .05).
Males reported more drinking days, greater quantities of alcohol consumed, higher frequencies of marijuana use, and more alcohol-related problems. In addition, about 69% of the male participants met a DSM-IV AUD diagnosis during any year(s) in young adulthood, whereas only 38% of the females had a positive diagnosis (p < .05). Moreover, about 64% of the multidrug users initiated alcohol use before starting to use the other two substances. For females, the predominant pattern was alcohol use onset before nicotine use onset before marijuana use onset (28%). In contrast, the predominant pattern among males was alcohol use onset before marijuana use onset before nicotine use onset (27%).
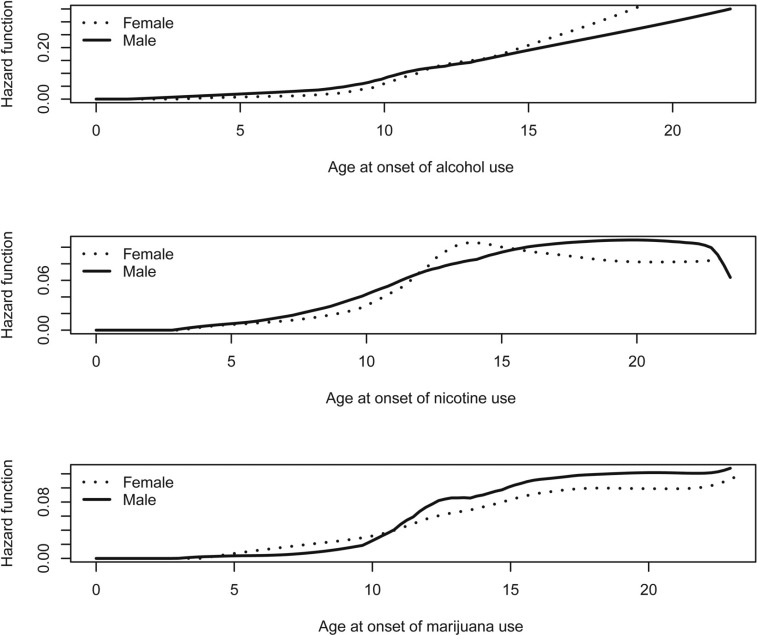
Figure 2 characterizes the gender-specific risk of onset of substance use from early childhood to young adulthood. In general, the risk of onset of using each of the three substances increased over time. The top panel shows that males tended to be at higher risk before age 14, whereas females were at higher risk later in adolescence. The Wilcoxon test that places more weight on the hazard function at younger ages indicated a significant gender difference, χ2(1) = 4.71, p < .05, but the log-rank test with more weight at older ages did not, χ2(1) = 1.29, p > .05. The middle panel shows that males were at higher risk for initiating nicotine use across time except for a short period between ages 12 and 16, but the gender difference was not statistically significant at either younger ages, Wilcoxon test result: χ2(1) = 0.15, p > .05, or at older ages, log-rank test result: χ2(1) = 0.27, p > .05. The bottom panel of Figure 2 demonstrates that females were at higher risk for onset of marijuana use before age 11, but males were at higher risk afterward. The results of the Wilcoxon test, χ2(1) = 4.11, p < .05, and the log-rank test, χ2(1) = 3.79, p < .05, suggest significant gender differences at both the younger ages and the older ages.
Figure 2.
Gender-specific developmental risk of onset of alcohol, nicotine, and marijuana use
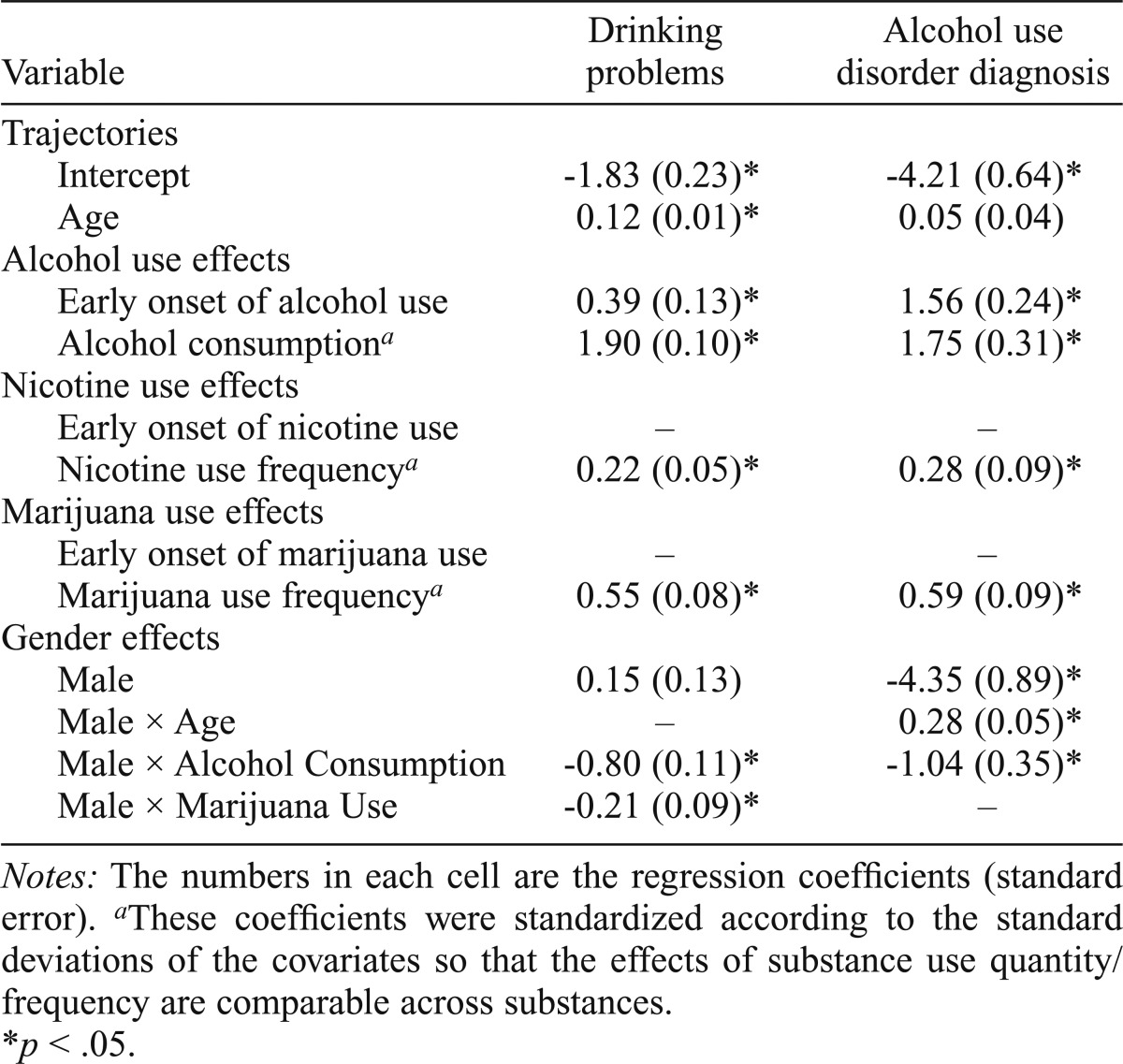
Table 2 displays the fitted longitudinal models of the effects of nicotine and marijuana use on drinking problems and AUD diagnosis, controlling for alcohol use effects. The left data column lists the estimated regression coefficients and standard errors of the linear mixed model of drinking problems. The drinking problems increased almost linearly with age. Both the early onset of alcohol use and larger amount of alcohol consumption contributed to more drinking problems. Conditioning on the alcohol use effects, the early-onset statuses of nicotine use and marijuana use did not have significant effects on drinking problems, whereas higher frequencies of nicotine use and marijuana use were both associated with more drinking problems. Because the regression coefficients corresponding to the quantity/frequency of substance use were standardized, the magnitude of the associations can be ranked across substances: Alcohol had the highest association with drinking problems, marijuana was second, and nicotine had the lowest association. Further, the associations of alcohol consumption and marijuana use with drinking problems were lower for males. This implies that females tended to be more vulnerable to the effects of these two substances.
Table 2.
Linear mixed model and generalized linear mixed model of the longitudinal effects of nicotine and marijuana use on alcohol outcomes, controlling for alcohol use effects (N = 320)
| Variable | Drinking problems | Alcohol use disorder diagnosis |
| Trajectories | ||
| Intercept | -1.83 (0.23)* | -4.21 (0.64)* |
| Age | 0.12 (0.01)* | 0.05 (0.04) |
| Alcohol use effects | ||
| Early onset of alcohol use | 0.39 (0.13)* | 1.56 (0.24)* |
| Alcohol consumptiona | 1.90 (0.10)* | 1.75 (0.31)* |
| Nicotine use effects | ||
| Early onset of nicotine use | – | – |
| Nicotine use frequencya | 0.22 (0.05)* | 0.28 (0.09)* |
| Marijuana use effects | ||
| Early onset of marijuana use | – | – |
| Marijuana use frequencya | 0.55 (0.08)* | 0.59 (0.09)* |
| Gender effects | ||
| Male | 0.15 (0.13) | -4.35 (0.89)* |
| Male × Age | – | 0.28 (0.05)* |
| Male × Alcohol Consumption | -0.80 (0.11)* | -1.04 (0.35)* |
| Male × Marijuana Use | -0.21 (0.09)* | – |
Notes: The numbers in each cell are the regression coefficients (standard error).
These coefficients were standardized according to the standard deviations of the covariates so that the effects of substance use quantity/frequency are comparable across substances.
p < .05.
The right data column of Table 2 shows the regression coefficients with standard errors of the generalized linear mixed model for AUD diagnosis. Both the early onset of alcohol use and larger amount of alcohol consumption contributed to higher risk of AUD. Conditioning on the early-onset status of alcohol use and the amount of alcohol consumption, the early-onset statuses of nicotine use and marijuana use did not contribute to the development of AUD. On the other hand, higher frequencies of nicotine use and marijuana use both were related to greater odds of meeting an AUD diagnosis (the association of marijuana use was higher than the one of nicotine use), but their associations with an AUD diagnosis were both lower than the one of alcohol consumption. Moreover, the association between alcohol consumption and the odds of meeting an AUD diagnosis was weaker among males.
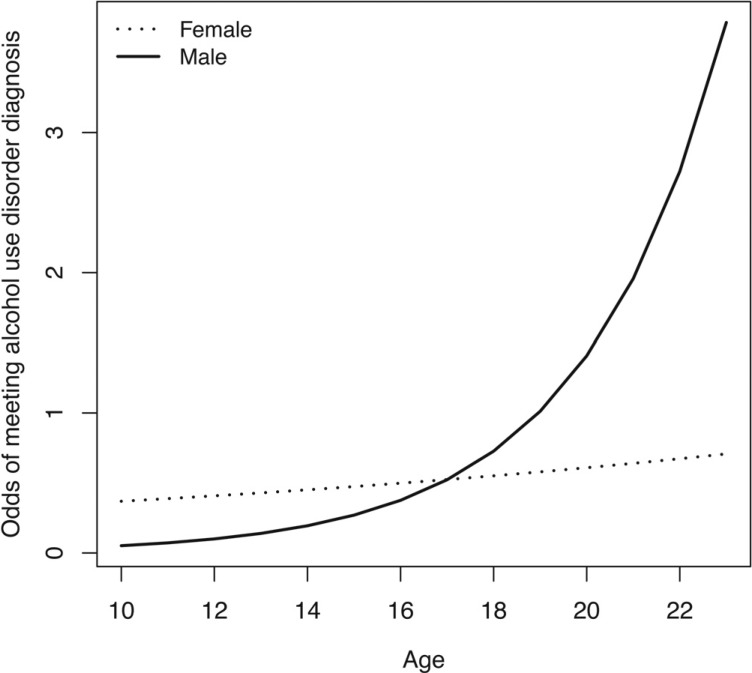
To characterize the gender-specific developmental trajectories of risk of AUD, we used the fitted generalized linear mixed model in Table 2 to calculate the estimated odds of meeting an AUD diagnosis from ages 10 to 23 for each gender group, holding the quantity/frequency of substance use at the sample means. The results are presented in Figure 3. Although females had greater odds of meeting an AUD diagnosis in early adolescence, males exhibited greater increases across time and elevated levels of odds in late adolescence and young adulthood.
Figure 3.
Gender-specific developmental trajectories of risk of alcohol use disorder
Discussion
This study found some important gender differences that could inform future prevention and intervention. First, although males are at higher risk for being early-onset alcohol users, females tend to be at higher risk for initiating marijuana use at younger ages. Recent national data (Chen and Jacobson, 2012) also found that females tend to be involved in higher levels of marijuana use than males in early adolescence. Thus, we may need to put more efforts into early intervention for marijuana use among girls.
Second, the effects of alcohol consumption on both drinking problems and AUD diagnosis are stronger among females, whereas the effect of marijuana use is only stronger on drinking problems among females. This result implies that female drinkers who also use marijuana may be at particularly high risk for developing drinking problems.
Third, our longitudinal analysis found gender differences in the developmental trajectories of AUD diagnosis but no gender differences in the ones for drinking problems. In particular, the odds of meeting an AUD diagnosis among males are initially lower at younger ages but increase rapidly with age, whereas the odds do not increase with age among females. This implies that the crucial period for AUD prevention/intervention should probably be extended beyond adolescence, especially for males.
The hazard functions as graphed in Figure 2 are consistent with the findings of the national surveys showing that males tend to start alcohol and nicotine use at younger ages (Alvanzo et al., 2011; Everett et al., 1999; Keyes et al., 2010). However, our finding of females’ tendency to be at higher risk for initiating marijuana use at younger ages is contrary to the result of an existing study that found no gender difference in retrospectively reported ages of marijuana use onset among a community sample of middle-aged adults with lifetime alcohol dependence (Ehlers et al., 2010). Because this area of research has previously relied on cross-sectional data, our study makes a unique contribution by providing prospective longitudinal data on onset ages that minimize potential bias due to recall errors or motivational revision of past behavior. Such gains in accuracy are crucial when characterizing developmental risk in people with an early onset of substance use (Parra et al., 2003). Furthermore, our analysis and graph characterize the developmental changes in gender-specific risk of onset of substance use beyond a simple comparison of mean onset ages and thus provide a new piece of information about the crucial period for intervention.
Our study found that after we controlled for the effect of early-onset status of alcohol use, the early-onset statuses of nicotine and marijuana use do not contribute to alcohol problems or an alcohol abuse/dependence diagnosis. In our sample, the participants who were early-onset drinkers also tended to be early-onset smokers and marijuana users. The odds of being early-onset smokers for those early-onset drinkers were 8.20 times the odds for those late-onset drinkers or nondrinkers; the odds of being early-onset marijuana users for those early-onset drinkers were 25.47 times the odds for those late-onset drinkers or nondrinkers. This is consistent with previous studies showing that early-onset smokers tended to start drinking at younger ages (Grant et al., 1998) and early-onset drinking and smoking were associated with an early-onset age of marijuana use (Behrendt et al., 2012). Our finding implies that the association between early onset of nicotine or marijuana use and AUDs observed in previous studies (Kirisci et al., 2013; Lewinsohn et al., 1999) may have been confounded by the effect of early onset of alcohol use, which tends to be a strong and consistent predictor of drinking-related problems and AUD diagnosis longitudinally.
The major limitation of this study involves generalizability of the findings to the larger population. Yet, the MLS design was never intended for this purpose. Rather, it was intended to sample from the subpopulation of families that were at elevated risk for major substance use problems and disorders and also would be of greatest likelihood to need substance use intervention in adolescence and thereafter. From that perspective, the study is potentially more informative for early programming relating to the arrest of high-risk patterns of use before their emergence in full-blown disorders. Nevertheless, it is limited in generalizability to minority populations because it consisted of only White youth.
In addition, because of the study design, results were generalizable only to families that are intact in early childhood, although as these children grew older, a great many of their parents separated or divorced. Also by design, the study was more heavily seeded with alcoholic families than is true of the general population. These inclusionary criteria reduce generalizability to populations of lower risk, involving youth from racial minorities, or those raised in a less coupled relationship during their very early development.
Moreover, because this is an observational study, the statistical models fitted on the data cannot be used to make causal inference. In other words, the statistical effects we observed in the models may also be potentially interpreted as the effects of outcomes on covariates. Another limitation of the study is that the data on nicotine use frequency were relatively weak in comparison to the data on the other two substances because this measure was more qualitative whereas the other two measures were more quantitative.
This study also has some important strengths. First, the recruitment protocol allowed us to observe the longitudinal development of high-risk children in the family context from early childhood to adulthood so that we could characterize the developmental risk of substance use using prospective data. Second, our family-informative sample mapping onto the population of children of alcoholic parent(s) who lived in largely lower middle to lower class communities allowed us to contribute to the literature of children of alcoholics. In fact, previous findings from our study have been shown to be consistent with the results of at least two other longitudinal studies on community samples of children of alcoholics (Hussong et al., 2007, 2008a, 2008b, 2008c, 2010). Third, our analysis involving female–male sibling pairs made it possible to examine gender differences developmentally while controlling for important confounds such as family density of alcoholism, demographic background, and unequal sample sizes of the gender groups.
Footnotes
This work was supported by National Institute on Alcohol Abuse and Alcoholism Grants K01 AA016591 (to Anne Buu) and R37 AA007065 (to Robert A. Zucker).
References
- Altonji JG, Dunn TA. Using siblings to estimate the effect of school quality on wages. The Review of Economics and Statistics. 1996;78:665–671. [Google Scholar]
- Alvanzo AH, Storr CL, La Flair L, Green KM, Wagner FA, Crum RM. Race/ethnicity and sex differences in progression from drinking initiation to the development of alcohol dependence. Drug and Alcohol Dependence. 2011;118:375–382. doi: 10.1016/j.drugalcdep.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Behrendt S, Beesdo-Daum K, Höfler M, Perkonigg A, Bühringer G, Lieb R, Wittchen HU. The relevance of age at first alcohol and nicotine use for initiation of cannabis use and progression to cannabis use disorders. Drug and Alcohol Dependence. 2012;123:48–56. doi: 10.1016/j.drugalcdep.2011.10.013. [DOI] [PubMed] [Google Scholar]
- Behrendt SS, Wittchen HU, Höfler MM, Lieb RR, Beesdo KK. Transitions from first substance use to substance use disorders in adolescence: Is early onset associated with a rapid escalation? Drug and Alcohol Dependence. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- Buu A, Wang W, Schroder SA, Kalaida NL, Puttler LI, Zucker RA. Developmental emergence of alcohol use disorder symptoms and their potential as early indicators for progression to alcohol dependence in a high risk sample: A longitudinal study from childhood to early adulthood. Journal of Abnormal Psychology. 2012;121:897–908. doi: 10.1037/a0024926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, DiPiazza C, Wang J, Puttler LI, Fitzgerald HE, Zucker RA. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. Journal of Studies on Alcohol and Drugs. 2009;70:489–498. doi: 10.15288/jsad.2009.70.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcoholism: Clinical and Experimental Research. 2007;31:1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahalan D, Cisin I, Crossly H. American drinking practice: A national study of drinking behavior and attitudes. New Brunswick, NJ: Publications Division, Rutgers Center of Alcohol Studies; 1969. [Google Scholar]
- Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health. 2012;50:154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. The link between family history and early onset alcoholism: Earlier initiation of drinking or more rapid development of dependence? Journal of Studies on Alcohol. 2000;61:637–646. doi: 10.15288/jsa.2000.61.637. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: A risk factor for the development of alcohol disorders. American Journal of Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Dick DM, Johnson JK, Viken RJ, Rose RJ. Testing between-family associations in within-family comparisons. Psychological Science. 2000;11:409–413. doi: 10.1111/1467-9280.00279. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Vieten C, Gilder DA, Stouffer GM, Lau P, Wilhelmsen KC. Cannabis dependence in the San Francisco family study: Age of onset of use, DSM-IV symptoms, withdrawal, and heritability. Addictive Behaviors. 2010;35:102–110. doi: 10.1016/j.addbeh.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett SA, Warren CW, Sharp D, Kann L, Husten CG, Crossett LS. Initiation of cigarette smoking and subsequent smoking behavior among U.S. high school students. Preventive Medicine. 1999;29:327–333. doi: 10.1006/pmed.1999.0560. [DOI] [PubMed] [Google Scholar]
- Fenzel LM. Multivariate analyses of predictors of heavy episodic drinking and drinking-related problems among college students. Journal of College Student Development. 2005;46:126–140. [Google Scholar]
- Grant BF. Age at smoking onset and its association with alcohol consumption and DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10:59–73. doi: 10.1016/s0899-3289(99)80141-2. [DOI] [PubMed] [Google Scholar]
- Grant JD, Lynskey MT, Scherrer JF, Agrawal A, Heath AC, Bucholz KK. A cotwin-control analysis of drug use and abuse/dependence risk associated with early-onset cannabis use. Addictive Behaviors. 2010;35:35–41. doi: 10.1016/j.addbeh.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Bierut LJ. Cigarette smoking and the risk for alcohol use disorders among adolescent drinkers. Alcoholism: Clinical and Experimental Research. 2006;30:2046–2054. doi: 10.1111/j.1530-0277.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatrics & Adolescent Medicine. 2006;160:739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- Husky MM, Paliwal P, Mazure CM, McKee SA. Gender differences in association with substance use diagnoses and smoking. Journal of Addiction Medicine. 2007;1:161–164. doi: 10.1097/ADM.0b013e318142d06c. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Bauer DJ, Huang W, Chassin L, Sher KJ, Zucker RA. Characterizing the life stressors of children of alcoholic parents. Journal of Family Psychology. 2008a;22:819–832. doi: 10.1037/a0013704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Cai L, Curran PJ, Flora DB, Chassin LA, Zucker RA. Disaggregating the distal, proximal, and time-varying effects of parent alcoholism on children’s internalizing symptoms. Journal of Abnormal Child Psychology. 2008b;36:335–346. doi: 10.1007/s10802-007-9181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Flora DB, Curran PJ, Chassin LA, Zucker RA. Defining risk heterogeneity for internalizing symptoms among children of alcoholic parents. Development and Psychopathology. 2008c;20:165–193. doi: 10.1017/S0954579408000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Huang W, Curran PJ, Chassin L, Zucker RA. Parent alcoholism impacts the severity and timing of children’s externalizing symptoms. Journal of Abnormal Child Psychology. 2010;38:367–380. doi: 10.1007/s10802-009-9374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: Entry points for an antisocial pathway to alcoholism. Journal of Abnormal Psychology. 2007;116:529–542. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult substance use. Alcoholism: Clinical and Experimental Research. 2008;32:723–737. doi: 10.1111/j.1530-0277.2008.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Bachman JG, O’Malley PM. Drugs and the class of ’78: Behaviors, attitudes, and recent national trends. Washington, DC: National Institute on Drug Abuse, Division of Research, U.S. Department of Health, Education, and Welfare; 1979. [Google Scholar]
- Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. Journal of Studies on Alcohol. 1992;53:447–457. doi: 10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, Hasin DS. Telescoping and gender differences in alcohol dependence: New evidence from two national surveys. American Journal of Psychiatry. 2010;167:969–976. doi: 10.1176/appi.ajp.2009.09081161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirisci L, Tarter R, Ridenour T, Zhai ZW, Fishbein D, Reynolds M, Vanyukov M. Age of alcohol and cannabis use onset mediates the association of transmissible risk in childhood and development of alcohol and cannabis disorders: Evidence for common liability. Experimental and Clinical Psychopharmacology. 2013;21:38–45. doi: 10.1037/a0030742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein JP, Moeschberger ML. Survival analysis: Techniques for censored and truncated data. New York, NY: Springer; 1997. [Google Scholar]
- Lewinsohn PM, Rohde P, Brown RA. Level of current and past adolescent cigarette smoking as predictors of future substance use disorders in young adulthood. Addiction. 1999;94:913–921. doi: 10.1046/j.1360-0443.1999.94691313.x. [DOI] [PubMed] [Google Scholar]
- Miech R, Koester S. Trends in U.S., past-year marijuana from 1985 to 2009: An age-period-cohort analysis. Drug and Alcohol Dependence. 2012;124:259–267. doi: 10.1016/j.drugalcdep.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molenberghs G, Verbeke G. Models for discrete longitudinal data. New York, NY: Springer; 2005. [Google Scholar]
- Müller HG, Wang JL. Hazard rate estimation under random censoring with varying kernels and bandwidths. Biometrics. 1994;50:61–76. [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Parra GR, O’Neill SE, Sher KJ. Reliability of self-reported age of substance involvement onset. Psychology of Addictive Behaviors. 2003;17:211–218. doi: 10.1037/0893-164X.17.3.211. [DOI] [PubMed] [Google Scholar]
- Robins L, Helzer J, Croughan J, Ratcliff KS. The NIMH Diagnostic Interview Schedule: Its history, characteristics and validity. St. Louis, MO: Washington University School of Medicine; 1980. [Google Scholar]
- Robins L, Marcus L, Reich W, Cunningham R, Gallagher T. Diagnostic Interview Schedule Version IV (DIS-IV) St. Louis, MO: Washington University School of Medicine; 1996. [Google Scholar]
- Rosenbaum PR. Heterogeneity and causality: Unit heterogeneity and design sensitivity in observational studies. The American Statistician. 2005;59:147–152. [Google Scholar]
- Schuckit MA. Research questionnaire. San Diego, CA: Alcoholism Treatment Program, V A. Medical Center, University of California; 1978. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Thorner ED, Jaszyna-Gasior M, Epstein DH, Moolchan ET. Progression to daily smoking: Is there a gender difference among cessation treatment seekers? Substance Use & Misuse. 2007;42:829–835. doi: 10.1080/10826080701202486. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York, NY: Springer-Verlag; 2000. [Google Scholar]
- Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26:479–488. doi: 10.1016/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Ellis DA, Fitzgerald HE, Bingham CR, Sanford K. Other evidence for at least two alcoholisms: II. Life Course variation in antisociality and heterogeneity of alcoholic outcome. Development and Psychopathology. 1996;8:831–848. [Google Scholar]
- Zucker RA, Fitzgerald HE, Noll RB. Drinking and drug history version 4. East Lansing, MI: Michigan State University; 1990. [Google Scholar]
- Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implications for a differentiated social policy. In: Fitzgerald HE, Lester BM, Zuckerman BS, editors. Children of addiction. New York, NY: Garland Press; 2000. pp. 109–142. [Google Scholar]