Abstract
Objective
The purpose of this case report is to describe a patient with bilateral idiopathic osteonecrosis of the femoral head (ONFH), provide a discussion of differential diagnosis for anterior hip pain, imaging, and treatment recommendations for ONFH.
Clinical features
A 34-year-old man was initially treated by a chiropractic physician for low back pain. At the end of a three week trial of care, the patient’s low back pain resolved. However, he reported a new complaint of mild left anterior hip stiffness. After re-examination, a homecare exercise program was prescribed. The patient returned 1 month later with substantial left anterior hip pain and walked with a noticeable limp. Radiography of the left hip demonstrated advanced ONFH. Magnetic resonance imaging of both hips demonstrated the extent of involvement of the left hip while incidentally revealing ONFH on the right.
Intervention and Outcome
A total hip arthroplasty was performed on the left hip and the right hip is being monitored without intervention.
Conclusion
Osteonecrosis of the femoral head is a challenging clinical problem with non-specific and wide-ranging signs and symptoms requiring clinicians to engage a cautious and comprehensive differential diagnosis. Prompt recognition ensures that appropriate treatment can be initiated in a timely manner and optimal patient outcomes achieved.
Key indexing terms: Osteonecrosis; Avascular necrosis of femur head; Diagnosis, differential; Imaging, magnetic resonance; Chiropractic
Introduction
Anterior hip pain is a common musculoskeletal complaint with a broad differential diagnosis (Fig 1). Pain in the inguinal region (groin) is synonymous with anterior hip pain and is most commonly the result of intra-articular hip pathology such as osteoarthritis or labral tears.1 In the appropriate clinical setting, osteonecrosis of the femoral head (ONFH) should also be considered in the differential of anterior hip pain.1 ONFH has an annual incidence in the United States between 10 000 and 20 000.2 Previous trauma, long term corticosteroid use, and alcohol abuse are the most common risk factors for development of ONFH; however, idiopathic, or primary ONFH in which the patient has no known risk factors is not an infrequent finding.3 The underlying pathophysiological mechanism is reduction in blood flow to the subchondral bone of the femoral head. There is resulting bone death and collapse of the articular surface.4 The clinical presentation of ONFH is vague and can range from mild anterior hip pain to marked reduction of hip range of motion with severe pain.1 Radiography should be the first diagnostic imaging modality performed in suspected cases of ONFH or in cases of chronic hip pain that is non-responsive to therapy.5,6 Radiography is classically insensitive for the early detection of osseous pathology and magnetic resonance imaging (MRI) is ordered when radiographs are negative, but hip pathology is suspected.5,6 Staging the severity of ONFH is best done by combining clinical findings, including the presence of risk factors, with the radiographic and MRI findings.4 Accurate staging of ONFH is critical to select the best treatment option, and advanced disease almost always requires total hip arthroplasty.7 Considering that most patients with ONFH are diagnosed in their 40s, hip replacement at this relatively young age is problematic since multiple revisions are likely, given a life expectancy approaching 80.2
Fig 1.
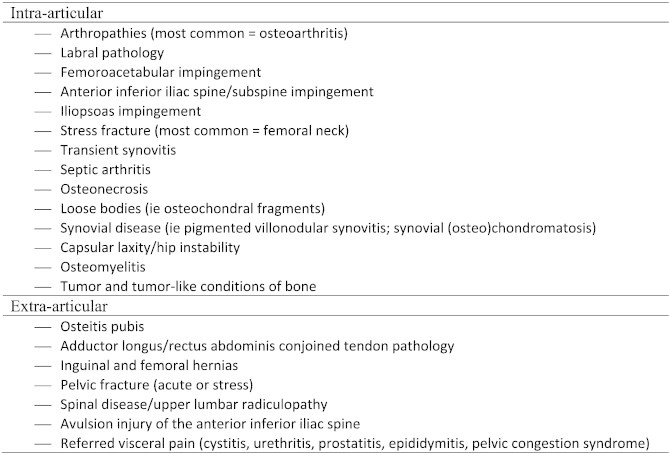
Sources of anterior hip pain.1,28,29
There are only four previous reports of diagnosis of ONFH published in the chiropractic literature.8–11 A better understanding of the diverse clinical manifestations and risk factors, appropriate imaging recommendations, current treatment strategies, and future research objectives of ONFH for clinicians who evaluate hip pain are needed. Therefore, the purpose of this case report is to describe a patient with bilateral idiopathic osteonecrosis of the femoral head (ONFH), provide a discussion of differential diagnosis for anterior hip pain, imaging, and treatment recommendations for ONFH.
Case Report
Informed consent was obtained by the patient to publish his health care information. A 34 year-old Hispanic male presented to an integrative chiropractic-allopathic medicine clinic with a chief complaint of mechanical low back pain that radiated into the left anterolateral thigh. This complaint had been present for 4 months. Tramadol/acetaminophen and naproxen were prescribed by a medical doctor for pain management following the onset of these symptoms. A lumbar spine MRI performed at an outside institution demonstrated intervertebral disc protrusions at the L4/5 and L5/S1 levels. Notably, at the time of initial presentation, the patient reported no complaints of either hip. Physical examination revealed decreased active ranges of motion of the thoracolumbar spine to approximately 60° flexion, 10° extension, and 15° of lateral flexion bilaterally. There was increased spinal pain at the end range of flexion. The lumbar paraspinal musculature was tender to touch at all levels, and there was decreased lumbar spine movement with motion palpation. The patient did not demonstrate any sensory or motor deficits. Kemp’s test and the prone instability test were positive for reproduction of lumbar spine pain and suggested spinal instability. The only positive hip examination finding was a positive modified Thomas test bilaterally, more pronounced on the left. This was attributed to minimal hip flexor hypertonicity. Following examination the patient was diagnosed with displacement of lumbar intervertebral discs without myelopathy, lumbar segmental dysfunction, and myofascial pain syndrome.
Intervention and Outcome
A trial of chiropractic care consisting of thoracolumbar spinal manipulative therapy, spinal biomechanics education, McKenzie repetitive extension exercises, and computerized traction/decompression therapy applied to the lumbar spine was initiated at twice per week for three weeks. McKenzie extension exercises were prescribed to be performed at home frequently throughout the day.
Approximately 3 weeks into care, the low back pain had resolved, however, the patient reported a mild to moderate amount of stiffness and pain in his left anterior hip region. A re-examination was performed revealing hypertonicity of the left hip flexors during a modified Thomas test. The remainder of the examination was unremarkable. The patient was prescribed a home exercise program consisting of spinal stabilization exercises and iliopsoas stretching to be done twice per day and was unable to return for follow-up owing to work commitments.
One month later, the patient presented in obvious distress and ambulated with a limp favoring his left side. He reported increasing pain of his left anterior hip that was temporarily relieved by his homecare stretching. Examination of the left hip revealed a positive C sign, in which the patient “cups” the anterior hip with their thumb and forefinger as to make the letter C, and significant anterior hip pain during FABERE (Patrick’s), hip impingement, McCarthy and modified Thomas tests. Radiography of the left hip was ordered to exclude femoroacetabular impingement. It revealed articular surface collapse with fragmentation of the femoral head and ill-defined sclerosis consistent with osteonecrosis (Fig 2). A subsequent bilateral hip MRI examination displayed the extent of involvement of the left femoral head while also incidentally demonstrating findings consistent with osteonecrosis on the right (Fig 3).
Fig 2.
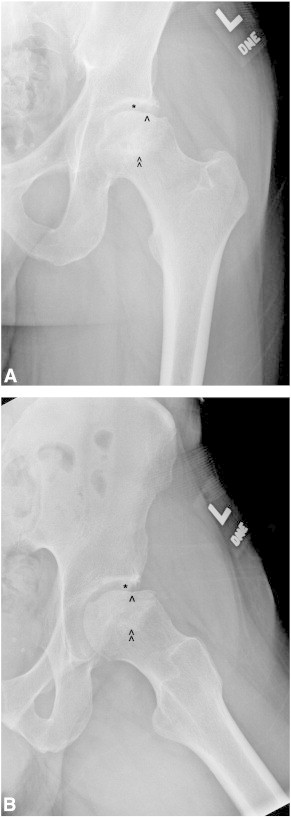
Anteroposterior (A) and lateral (B) radiographs of the left hip demonstrate collapse of the subarticular surface of the femoral head (single arrowhead) with subjacent sclerosis (double arrowheads) and preservation of joint space (asterisk) characteristic of osteonecrosis.
Fig 3.
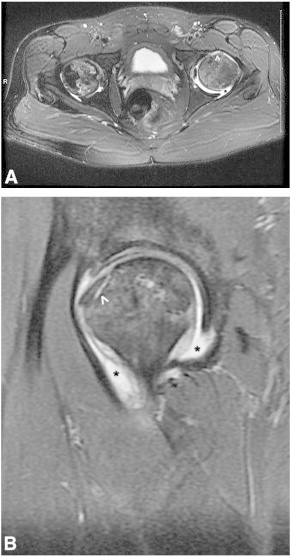
(A) Axial T2-weighted fat saturated MRI through both hip joints demonstrates heterogeneous high signal within the region of both femoral heads. Additionally, there is subchondral collapse of the left femoral head (white arrowhead) and a corresponding moderate left hip joint effusion (black asterisk). There is no acetabular involvement of either hip.
(B) Sagittal proton-density fat saturated MRI of the left hip demonstrates the region of subchondral collapse (white arrowhead). Heterogeneous high signal within the femoral head and a joint effusion (black asterisks) are again visualized.
The left hip was treated with a total hip arthroplasty. Currently, the patient is undergoing post-operative rehabilitation at another facility without incident. The asymptomatic right hip is being monitored without intervention.
Discussion
ONFH affects approximately 10 000 to 20 000 each year in the United States.2 The underlying pathophysiology is reduction in blood flow to the subarticular zone of the femoral head, either through intraluminal obstruction, vascular compression, or physical disruption of the blood vessel itself.4 There are many risk factors for the development of ONFH with the most common being previous trauma, followed by long term corticosteroid use and alcoholism.2,3 Idiopathic (primary or spontaneous) ONFH is a term utilized when no overt risk factors are present4 but most likely represents the fourth leading cause of ONFH.3 This form of ONFH is thought to occur from abnormal fat metabolism leading to both marrow infiltration producing vascular compression and fatty embolism causing intraluminal obstruction.12 Idiopathic ONFH demonstrates a male predilection with a peak age distribution in the 40s.3 As revealed in this case, idiopathic ONFH can be bilateral in up to 60% of cases at initial diagnosis.13 However, if an MRI of the contralateral hip is normal at initial diagnosis, the risk of subsequent development of ONFH is rare.14 Even if ONFH is present bilaterally, the patient will invariably present with unilateral symptoms.13 These symptoms range from mild anterior hip stiffness to marked pain with gait disturbances and limitations in range of motion.1
This case is unique due to the involvement of the contralateral hip and the rapid clinical progression of the disease. In this current case, the patient had restriction in hip flexion without symptoms that progressed to stiffness then severe pain with limitation in function over a period of approximately two months. At first, the modified Thomas was positive for a mild hip joint contracture which was thought to be due to hip flexor hypertonicity. Later in the disease process, the patient had increased anterior hip pain with the FABERE (Patrick’s), hip impingement, and McCarthy orthopedic tests. Although the Thomas test has high reported sensitivity (89%) and specificity (92%) in diagnosing intra-articular hip pathology,15 and the hip impingement test has a high positive predictive value (95.7%) for the diagnosis of labral tears,16 the overall diagnostic value of hip orthopedic testing is poor. Two recently published systematic reviews of the literature have concluded that limited high quality studies exist supporting the use of hip orthopedic testing to guide clinical decision making.17,18 Recognizing the limitations of orthopedic tests in the assessment of anterior hip pain is important as the differential diagnosis should be adjusted to reflect this poor diagnostic confidence (Fig 1).
Diagnostic imaging is crucial in the diagnosis of ONFH. Currently, four imaging-based classification systems are used to stage ONFH19: Ficat and Arlet (most commonly used); The University of Pennsylvania (Steinberg); Association Research Circulation Osseous (ARCO); and the classification of the Japanese Orthopedic Association. In general, these classifications consider early ONFH an MRI finding only with normal radiography, and advanced (final stage) ONFH characterized radiographically as femoral head collapse, sclerosis, fragmentation and marked degenerative changes of the femoroacetabular joint.19 The more refined classifications also consider lesion location and percent of femoral head involvement on MRI, with mild being less than 15% and severe greater than 30% involvement.19
In this case, the patient’s left femoral head demonstrated subchondral collapse and poorly defined sclerosis with preservation of femoroacetabular joint space at radiography consistent with a Ficat and Arlet stage III lesion. The asymptomatic right hip joint was not radiographed, so classification staging was not identified. However, the MRI demonstrated heterogeneous high signal with T2-weighting consistent with osteonecrosis. Furthermore, there was no subchondral collapse. Therefore, the right femoral head would have been classified either a Ficat and Arlet stage I or IIa or a University of Pennsylvania (Steinberg) stage I or II. Interestingly, neither hip demonstrated the classic “double line sign” in which an inner high signal line representing granulation tissue is surrounded by an outer rim of low signal sclerotic bone with T2-weighting.4 It is imperative that the healthcare provider remember that while radiographic signs of patchy sclerosis, subchondral collapse, and fragmentation of the femoral head are virtually pathognomonic of ONFH, these findings are observed late in the disease process and MRI, not radiography, is the most sensitive imaging test for ONFH detection.20
Advances in MRI technology seem promising in the evaluation of ONFH. While diffusion-weighted imaging currently adds little clinical value in discriminating amongst Ficat and Arlet stages of ONFH, there are significant differences in diffusion values in the necrotic bone compared with healthy controls.21 Conversely, dynamic contrast enhanced (perfusion) MRI may be more sensitive in the detection of early ONFH than MRI using standard pulse sequences.22 These results are preliminary however and require validation.
Treatment for ONFH is determined by the stage of the disease. In a recent review, Banerjee et al. outlined currently available non-operative and operative treatments for ONFH. Non-operative treatments consist of non-weight bearing, administration of bisphosphonates, anticoagulants, and hypolipidemics, extracorporeal shock wave therapy, pulsed electromagnetic therapy, hyperbaric oxygen, and vasodilators. With the exception of pulsed electromagnetic therapy, there is preliminary scientific support for the use of these non-operative therapies.7 Recent data using an animal model also supports the use of exogenous erythropoietin in the treatment of corticosteroid induced ONFH.23 Operative treatment of ONFH consists of core decompression, nonvascularized bone grafting, vascularized bone grafting, and administration of bone morphogenetic proteins, stem cell therapy, proximal femoral osteotomies, and hip arthroplasty.7 The patient in this case report had advanced ONFH on the left (Ficat and Arlet stage III) and was treated with a total hip arthroplasty. The most commonly performed procedure in early stage ONFH is core decompression. Marker and colleagues reported that 79% of Ficat and Arlet stage I patients treated with a core decompression procedure had no radiographic progression of the disease at a minimum follow-up of 36 months.24 This core decompression procedure has been modified by some to a less invasive, multiple percutaneous small-hole drilling procedure.24 In Ficat and Arlet stage III or IV patients, hip arthroplasty is recommended.25 Despite concerns of performing a joint replacement in a relatively young patient, advances in orthopedic surgery seem to have improved the overall outcome of this procedure.25 Recent data indicate that more hip arthroplasties are being performed to treat ONFH.26
When the contralateral femoral head shows signs of necrosis on MRI but is asymptomatic, as in this case, it should be monitored closely. In one recent study, 32% of asymptomatic hips with ONFH collapsed within 4 years.13 In this study by Min et al, collapse was preceded by symptoms for 8 months on average. Lesion size and lesion location appear to be most predictive for progression to symptoms and collapse, with large, lateral lesions being the most worrisome.13,27 Currently, there is no accepted treatment protocol for asymptomatic ONFH; therefore, an aim for future research could be to examine the effectiveness of non-operative and operative interventions on these asymptomatic hips.
Reports of ONFH in the chiropractic literature are limited. Fried and Gerow described a case of ONFH in a 62-year-old woman with a history of alcohol abuse. In their case, the patient initially had sciatica-like pain that later progressed to anterior hip pain.8 Thorkeldsen and Cantillon9 and Pajaczkowski10 described cases of idiopathic ONFH that initially presented as constant, dull anterior hip pain in males 77 years and 27 years old, respectively. In the former case, there were extensive degenerative changes of the contralateral hip that may also have progressed to osteonecrosis. The typical pattern of ONFH is for joint space to be preserved until late in the disease process, however. Lastly, Karim and Goel presented a patient with known risk factors of prior trauma and corticosteroid use who developed ONFH.11 This current case is unique in that early involvement of the contralateral hip is described. Furthermore, there was rapid clinical progression of the disease from anterior hip tightness to severe pain with gait disturbance in less than two months. The duration of complaints in the above cases was between 6 months (post-trauma) and 6 years.
Limitations
This is a case report, thus only reporting the findings for one study. The findings of this case report cannot necessarily be generalized to other patients or the general public.
Conclusion
This case highlights two important features of ONFH: (1) involvement of the asymptomatic contralateral side must be excluded with the use of MRI; and (2) ONFH can progress rapidly, therefore non-specific anterior hip discomfort or pain in a middle-aged patient that is non-responsive to care should raise the suspicion for ONFH even in the absence of identifiable risk factors. Thorough differential diagnoses for anterior hip pain, diagnostic imaging, and treatment recommendations to aid in rapid diagnosis and treatment are recommended.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Wilson J.J., Furukawa M. Evaluation of the patient with hip pain. Am Fam Physician. 2014;89(1):27–34. [PubMed] [Google Scholar]
- 2.Lavernia C.J., Sierra R.J., Grieco F.R. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7(4):250–261. doi: 10.5435/00124635-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Fukushima W., Fujioka M., Kubo T., Tamakoshi A., Nagai M., Hirota Y. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010;468(10):2715–2724. doi: 10.1007/s11999-010-1292-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Resnick D.S.D., Madewell J.E. Diagnosis of bone and joint disorders. W.B, Saunders; Philadelphia, Pennsylvania: 2002. Osteonecrosis: Pathogenesis, Diagnostic techniques, specific situations, and complications; pp. 3599–3685. [Google Scholar]
- 5.Seeger LL D.R., Weissman B.N., Arnold E. ACR Appropriateness Criteria avascular necrosis (osteonecrosis) of the hip cited 2014 March 31. http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/ChronicHipPain.pdf Available from.
- 6.Taljanovic MS D.R., Weissman B.N., Appel M. ACR Appropriateness Criteria chronic hip pain cited 2014 March 31. http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/ChronicHipPain.pdf Available from.
- 7.Banerjee S., Issa K., Pivec R., Kapadia B.H., Khanuja H.S., Mont M.A. Osteonecrosis of the hip: treatment options and outcomes. Orthop Clin North Am. 2013;44(4):463–476. doi: 10.1016/j.ocl.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Fried N.R., Gerow G. Avascular necrosis of the femur head. J Manipulative Physiol Ther. 1989;12(3):228–230. [PubMed] [Google Scholar]
- 9.Thorkeldsen A., Cantillon V. Idiopathic osteonecrosis of the hip. J Manipulative Physiol Ther. 1993;16(1):37–42. [PubMed] [Google Scholar]
- 10.Pajaczkowski J.A. The stubborn hip: idiopathic avascular necrosis of the hip. J Manipulative Physiol Ther. 2003;26(2):107–110. doi: 10.1067/mmt.2003.13. [DOI] [PubMed] [Google Scholar]
- 11.Karim R., Goel K.D. Avascular necrosis of the hip in a 41-year-old male: a case study. J Can Chiropr Assoc. 2004;48(2):137–141. [PMC free article] [PubMed] [Google Scholar]
- 12.Kawai K., Maruno H., Watanabe Y., Hirohata K. Fat necrosis of osteocytes as a causative factor in idiopathic osteonecrosis in heritable hyperlipemic rabbits. Clin Orthop Relat Res. 1980;153:273–282. [PubMed] [Google Scholar]
- 13.Min B.W., Song K.S., Cho C.H., Lee S.M., Lee K.J. Untreated asymptomatic hips in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res. 2008;466(5):1087–1092. doi: 10.1007/s11999-008-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sugano N., Nishii T., Shibuya T., Nakata K., Masuhara K., Takaoka K. Contralateral hip in patients with unilateral nontraumatic osteonecrosis of the femoral head. Clin Orthop Relat Res. 1997;334:85–90. [PubMed] [Google Scholar]
- 15.McCarthy J.C., Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics. 1995;18(8):753–756. doi: 10.3928/0147-7447-19950801-12. [DOI] [PubMed] [Google Scholar]
- 16.Hananouchi T., Yasui Y., Yamamoto K., Toritsuka Y., Ohzono K. Anterior impingement test for labral lesions has high positive predictive value. Clin Orthop Relat Res. 2012;470(12):3524–3529. doi: 10.1007/s11999-012-2450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reiman M.P., Goode A.P., Hegedus E.J., Cook C.E., Wright A.A. Diagnostic accuracy of clinical tests of the hip: a systematic review with meta-analysis. Br J Sports Med. 2013;47(14):893–902. doi: 10.1136/bjsports-2012-091035. [DOI] [PubMed] [Google Scholar]
- 18.Rahman L.A., Adie S., Naylor J.M., Mittal R., So S., Harris I.A. A systematic review of the diagnostic performance of orthopedic physical examination tests of the hip. BMC Musculoskelet Disord. 2013;14:257–264. doi: 10.1186/1471-2474-14-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee G.C., Khoury V., Steinberg D., Kim W., Dalinka M., Steinberg M. How do radiologists evaluate osteonecrosis? Skeletal Radiol. 2014;43(5):607–614. doi: 10.1007/s00256-013-1803-4. [DOI] [PubMed] [Google Scholar]
- 20.Scheiber C., Meyer M.E., Dumitresco B. The pitfalls of planar three-phase bone scintigraphy in nontraumatic hip avascular osteonecrosis. Clin Nucl Med. 1999;24(7):488–494. doi: 10.1097/00003072-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Oner A.Y., Aggunlu L., Akpek S. Staging of hip avascular necrosis: is there a need for DWI? Acta Radiol. 2011;52(1):111–114. doi: 10.1258/ar.2010.100231. [DOI] [PubMed] [Google Scholar]
- 22.Chan W.P., Liu Y.J., Huang G.S. Relationship of idiopathic osteonecrosis of the femoral head to perfusion changes in the proximal femur by dynamic contrast-enhanced MRI. AJR Am J Roentgenol. 2011;196(3):637–643. doi: 10.2214/AJR.10.4322. [DOI] [PubMed] [Google Scholar]
- 23.Chen S., Li J., Peng H., Zhou J., Fang H. Administration oferythropoietin exerts protective effects against glucocorticoid-induced osteonecrosis of the femoral head in rats. Int J Mol Med. 2014;33(4):840–848. doi: 10.3892/ijmm.2014.1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marker D.R., Seyler T.M., Ulrich S.D., Srivastava S., Mont M.A. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;466(5):1093–1103. doi: 10.1007/s11999-008-0184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Issa K., Pivec R., Kapadia B.H., Banerjee S., Mont M.A. Osteonecrosis of the femoral head: the total hip replacement solution. Bone Joint J. 2013;95-B(11 Suppl. A):46–50. doi: 10.1302/0301-620X.95B11.32644. [DOI] [PubMed] [Google Scholar]
- 26.Johnson A.J., Mont M.A., Tsao A.K., Jones L.C. Treatment of femoral head osteonecrosis in the United States: 16-year analysis of the Nationwide Inpatient Sample. Clin Orthop Relat Res. 2014;472(2):617–623. doi: 10.1007/s11999-013-3220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang J.S., Moon K.H., Kwon D.G., Shin B.K., Woo M.S. The natural history of asymptomatic osteonecrosis of the femoral head. Int Orthop. 2013;37(3):379–384. doi: 10.1007/s00264-013-1775-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tibor L.M., Sekiya J.K. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12):1407–1421. doi: 10.1016/j.arthro.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 29.Blankenbaker D.G., Tuite M.J. Non-femoroacetabular impingement. Semin Musculoskelet Radiol. 2013;17(3):279–285. doi: 10.1055/s-0033-1348094. [DOI] [PubMed] [Google Scholar]


