Among patients with cancer, personal health record portal use is frequent and increasing; understanding the implications of this new technology will be central to the delivery of safe and effective care.
Abstract
Introduction:
Electronic portals are secure Web-based servers that provide patients with real-time access to their personal health record (PHR). These applications are now widely used at cancer centers nationwide, but their impact has not been well studied. This study set out to determine predictors and patterns of use of a Web-based portal for accessing PHRs and communicating with health providers among patients with cancer.
Methods:
Retrospective analysis of enrollment in and use of MyChart, a PHR portal for the Epic electronic medical record system, among patients seen at a National Cancer Institute–designated cancer center. Predictors of MyChart use were analyzed through univariable and multivariable regression models.
Results:
A total of 6,495 patients enrolled in MyChart from 2007 to 2012. The median number of log-ins over this period was 57 (interquartile range 17-137). The most common portal actions were viewing test results (37%), viewing and responding to clinic messages (29%), and sending medical advice requests (6.4%). Increased portal use was significantly associated with younger age, white race, and an upper aerodigestive malignancy diagnosis. Thirty-seven percent of all log-ins and 31% of all medical advice requests occurred outside clinic hours. Over the study period, the average number of patient log-ins per year more than doubled.
Conclusions:
Among patients with cancer, PHR portal use is frequent and increasing. Younger patients, white patients, and patients with upper aerodigestive malignancies exhibit the heaviest portal use. Understanding the implications of this new technology will be central to the delivery of safe and effective care.
Introduction
The electronic medical record (EMR) has emerged as a key priority for the US health care system. The EMR has been promoted by health professionals and government officials as a means to improve documentation and data availability, streamline order entry to decrease medical errors, and provide clinical reminders to increase rates of recommended screening. To accelerate the transition away from paper charts, in 2011 the Department of Health and Human Services began funding $27 billion in incentives for health care providers who implemented EMRs.
Electronic patient portals that provide access to patient health records (PHRs) have been designed to enhance the timeliness, efficiency, and patient centeredness of care. These applications provide a direct and secure means for patients to receive and convey information relevant to their medical care through the Internet, thereby increasing transparency in the medical system.1 As access to personal computers and mobile devices expands, it is likely that PHR availability and use rates will rise. Although PHR implementation and use have been evaluated in primary care and certain specialty populations,2–8 these parameters have not been well described among patients with cancer. Electronic PHR portals may introduce particular considerations in oncology populations. Longitudinal outpatient care is more intensive than that of most other specialties, potentially resulting in increased EMR and PHR data flow. Laboratory and radiology results may represent major clinical developments such as disease progression, which may result in heightened anxiety and confusion when viewed without concurrent clinician interpretation. Furthermore, due to the nature of the underlying disease, symptoms reported by patients with cancer may be more likely to represent medical emergencies, such as infections, blood clots, or neurologic complications. How such developments are communicated through PHR portals may pose concerns for patient safety and satisfaction. Given these considerations, we sought to study the prevalence and patterns of electronic PHR portal use in a large, contemporary oncology population.
Methods
MyChart Patient Portal
MyChart provides a secure, online portal for patients to access their PHR within the Epic EMR (Verona, WI) used throughout the University of Texas Southwestern Medical Center (UT Southwestern). MyChart became available through some clinical departments as early as 2005 and was first implemented in the Harold C. Simmons Cancer Center in 2007. Since then, at the time of registration, all patients at the Simmons Cancer Center have been offered MyChart access. Patients who express interest are sent an e-mail with a unique activation code.
Data Extraction
This study was approved by the Simmons Cancer Center Protocol Review and Monitoring Committee and the UT Southwestern Institutional Review Board (STU 062012-025). Working with two information resources analysts (S.G., J.C.), our team identified patients using MyChart by extracting data based on 19 cancer department-type appointments (35 possible fields) with an encounter or associated billing diagnosis of ICD9 140 to 239.99 (cancer diagnoses) between January 1, 2007 (when MyChart was first available throughout the cancer center) and December 31, 2012. Patient demographics and cancer type were extracted. We queried three different MyChart data tables for patient data, access patterns, and message actions: Patient_MYC (16 fields), MYC_Patient_USER_ACCSS (eight fields), MYC_MESG (36 fields). Epic demographic data were matched to MyChart data using unique patient medical record numbers.
Patient-initiated MyChart actions were categorized as follows: Appointments, Billing/Financial, Labs/Imaging (viewing test results), Medical Advice (communications to medical providers), Medical History, Messaging (viewing/responding to communications from medical providers or generated automatically), MyChart Account Maintenance, and Reference Library (viewing an on-line health reference). A detailed listing of specific MyChart actions included in each category is provided in Appendix Table A1 (online only). Opportunities for patients to generate free-text communication to providers include the Medical Advice Request, Medication Renewal Request, and Appointment Schedule Actions. When a medical provider generates a Message to a patient or responds to a patient Medical Advice Request, the provider may select whether or not the patient may reply to that communication. We recorded only patient MyChart actions. For example, generation of a Message from a provider or the MyChart system was recorded only if accessed by the patient.
Statistical Analysis
To test the association between MyChart use and patients characteristics, we categorized patients as frequent users (the number of MyChart use ≥ the median value of 57 log-ins) or nonfrequent users (the number of MyChart use < the median value of 57 log-ins) as the dependent variable. We also categorized MyChart use by tertile. Age, gender, race and primary cancer type were used as covariates. Univariable and multivariable logistic regression were implemented to test the association between the MyChart use and all these covariates. All statistical analysis and data summarization were performed using R 2.6 (Auckland, New Zealand).
Results
A total of 6,495 patients enrolled in MyChart were included in the analysis. Mean age was 60 years, and 67% were female. Additional baseline characteristics are listed in Table 1. The total number of MyChart log-ins was 707,746. Per-patient total log-ins are shown in Figure 1a. The median total number of log-ins per patient was 57 (interquartile range [IQR] 17-137), with a maximum number of 10,347. Per month, the median number of log-ins was 3.7 (mean 7.3). There were a total of 5,942,501 patient MyChart actions. The median total number of MyChart actions per patient was 516 (IQR 171-1,189). MyChart actions (excluding log-in/logout) are shown in Figure 1B. Three actions accounted for 85% of all MyChart use: viewing test results (37%), viewing and/or responding to messages (from providers, clinic staff, or administratively generated; 29%), and sending medical advice requests (6.4%). The median number of medical advice requests per patient was 14 (IQR 2-46), with a maximum number of 1,079. Accessing an online health reference library—which was designed to aid in patients' understanding of laboratory results, radiology results, and other data—accounted for 20,909 actions (0.4%).
Table 1.
Baseline Characteristics of Patients Enrolled in MyChart Electronic Patient Portal
| Characteristic | No. | % |
|---|---|---|
| Total patients | 6,495 | |
| Age, years | ||
| Mean | 60 | |
| SD | 13 | |
| Sex | ||
| Male | 2,091 | 32 |
| Female | 4,402 | 68 |
| Race | ||
| White | 3,256 | 47 |
| Black | 178 | 3 |
| Asian | 339 | 5 |
| Other | 41 | 1 |
| Unknown | 3,131 | 45 |
| Cancer type | ||
| Breast | 1,310 | 20 |
| GI/GU | 1,022 | 16 |
| Hematologic | 777 | 12 |
| Upper aerodigestive | 484 | 7 |
| Other | 2,139 | 33 |
| Unknown | 763 | 12 |
Abbreviations: GU, genitourinary; SD, standard deviation.
Figure 1.
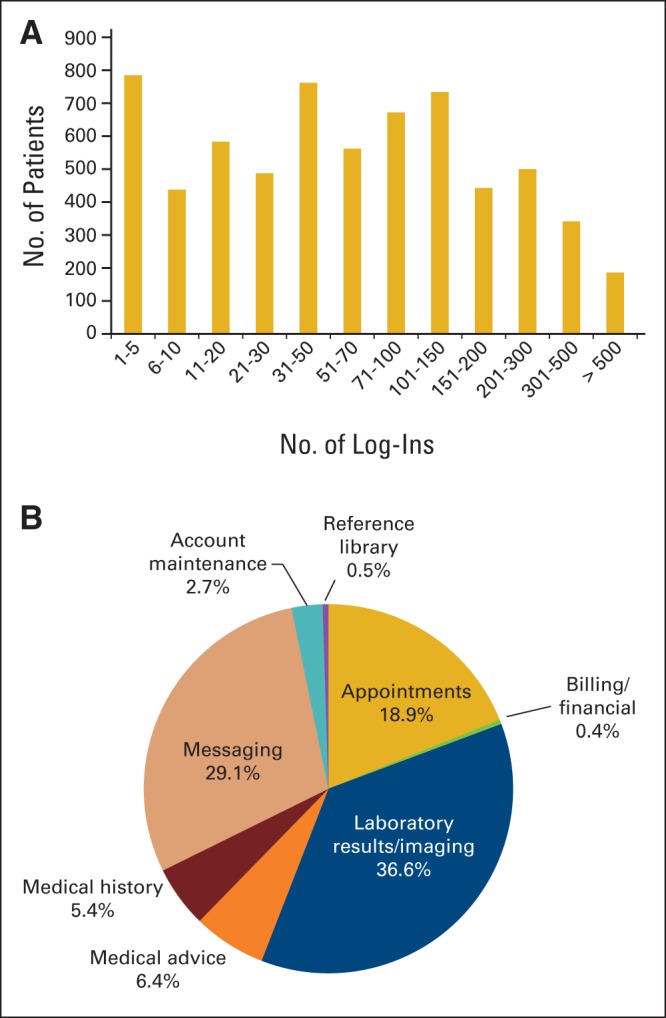
MyChart activity. (A) Number of log-ins per patient enrolled in MyChart, (B) Frequency of MyChart actions.
Univariable logistic regression modeling suggested MyChart use was more common among men and white patients. In addition, by cancer type, use was greatest for patients with upper aerodigestive malignancies (odds ratio [OR] = 1.23; 95% CI, 1.00 to 1.52; P = .05) and least for the “other” category (OR = 0.73; 95% CI, 0.69 to 0.91; P ≤ .001). Hematologic, gastrointestinal, breast, and, genitourinary malignancies conferred no statistically significant predictive value for MyChart use. In a multivariable model incorporating age, sex, race, and cancer type, there was a significant association between age, race, and cancer type. Logistic regression data for MyChart use is comprehensively depicted in Table 2.
Table 2.
Predictors of MyChart Use
| Characteristic | Univariable |
Overall P | Multivariable |
Overall P | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |||
| Age, years | .29 | .03 | ||||||
| ≤ 60 | Reference | Reference | ||||||
| > 60 | 1.05 | 0.96 to 1.16 | .29 | 0.87 | 0.76 to 0.99 | .03 | ||
| Sex | < .001 | .09 | ||||||
| Male | Reference | Reference | ||||||
| Female | 0.83 | 0.75 to 0.92 | < .001 | 0.88 | 0.75 to 1.12 | .09 | ||
| Race | < .001 | .002 | ||||||
| White | Reference | Reference | ||||||
| Black | 0.66 | 0.52 to 0.93 | < .001 | 0.67 | 0.53 to 0.84 | < .001 | ||
| Other | 1.09 | 0.83 to 1.44 | .53 | 1.03 | 0.78 to 1.3 | .85 | ||
| Unknown | 0.59 | 0.37 to 0.94 | .03 | 0.64 | 0.40 to 1.01 | .06 | ||
| Cancer type | < .001 | .008 | ||||||
| Breast | Reference | Reference | ||||||
| GI/GU | 1.10 | 0.94 to 1.20 | .24 | 0.97 | 0.78 to 1.20 | .75 | ||
| Hematologic | 1.07 | 0.99 to 1.28 | .45 | 1.05 | 0.84 to 1.32 | .66 | ||
| UAD | 1.23 | 1.00 to 1.52 | .05 | 1.18 | 0.92 to 1.5 | .20 | ||
| Other | 0.73 | 0.69 to 0.91 | < .001 | 0.81 | 0.68 to 0.97 | .03 | ||
Abbreviations: GU, genitourinary; OR, odds ratio; UAD, upper aerodigestive.
We also examined the association between patient characteristics and number of specific MyChart uses. These analyses are shown in Appendix Table A2 (online only). For medical advice requests, in multivariable analysis, there was a significant association with race; black patients (OR 0.67; P = .001) and “other” race patients (OR 0.74; P = .04) made fewer requests than other populations. For laboratory and imaging results, black and unknown race patients had lower use than white patients, and patients with hematologic malignancies had the highest use. For appointment requests, there was no association with demographic characteristics, although patients with upper aerodigestive malignancies had significantly increased use compared to other cancer types.
We also analyzed characteristics of those individuals with the highest rates of MyChart access, defined as the top quartile of use (data not shown). In general, these results did not differ substantially from the analysis categorized by median.
The day and time of MyChart use (log-ins and medical advice requests) are shown in Appendix Figure A1 (online only). The majority of MyChart use by patients occurred during clinic hours (Monday-Friday 8:00 am-5:00 pm). However, 25% occurred on weekdays before 8:00 am or after 5:00 pm, and 12% occurred during the weekend. Among all MyChart log-ins, 37% occurred outside clinic hours. Among medical advice requests, 31% occurred outside clinic hours.
Appendix Figure A1 displays the number of patients actively using MyChart (defined as one or more log-ins) and total MyChart use (defined according to number of log-ins) by year. From 2007 to 2012, the number of patients actively using MyChart (defined as having at least one log-in) increased almost five-fold. Total log-ins increased by over 10-fold during the same time period.
Discussion
Oncology practices have widely adopted the EMR, with use exceeding that of many other specialties.9 It follows that PHR portals would be desired and used by oncology patients. For instance, in a cohort of patients with hematologic malignancies, 89% expressed interest in accessing electronic health records.10 Additionally, disease burden and complexity in medical oncology may lead to greater health care need, which in turn has been associated with increased portal use.11
To our knowledge, this is the first study to examine PHR portal use in a large, contemporary oncology cohort. Even considering differences in portal technology and study methodology, it appears that portal use by patients with cancer clearly exceeds that reported in other populations. In our study, the average number of log-ins was 109, with a maximum of 13,347. In contrast, a urology practice patient population connected to an Internet medical Web page an average of 8 total times (range, 1 to 22).5 Among families of children under multidisciplinary care for congenital heart disease, the average number of log-ins to a Web-based portal was 25 (range 1 to 440).12 Furthermore, over the 6-year period of our analysis (2007-2012), the number of enrolled patients increased five-fold, and the total number of log-ins increased more than 10-fold. This suggests that not only are patient portals being used by a greater proportion of patients, but they are also being used more intensively. A similar trend was observed in a large primary care cohort, with a four-fold increase in portal enrollment (from 2.7% to 14.1% of eligible patients) between 1999 and 2002.13
In our cohort, more frequent MyChart use was observed among younger patients, men, and white patients. Numerous other studies have reported similar trends, with minority and older populations consistently less likely to use patient portals.2,7,11,14 It is important to note that other studies have used enrollment rather than intensity of use as end points for these analyses. Nevertheless, similar factors may underlie these observations, such as frequency of access to and familiarity with this technology. Alternatively, lower rates of portal use by certain populations, such as older patients, could represent more general differences in health care information and participation preferences, which have been described previously.15 We also observed use-specific trends. For instance, laboratory and radiology test result viewing was greatest among patients with hematologic malignancies, which may reflect the more frequent outpatient laboratory monitoring of these patients.
Test result viewing was the most common use of the patient portal, accounting for 37% of all actions. The interpretation of such data by individuals without formal medical training outside the context of a health care encounter raises a number of questions. In instances where tests convey major clinical developments, such as disease progression, viewing results without concurrent clinician interpretation and support might cause psychosocial distress. Anxiety might also result from abnormal radiographic findings or laboratory values of no clinical significance, which is a common event among patients undergoing highly sensitive imaging studies or laboratory test panels with numerous individual components. To help patients understand such information, the MyChart portal has an electronic health reference library; however, it was used rarely by patients in our study, accounting for only 0.5% of MyChart actions. Earlier studies addressing such questions have yielded mixed findings. A survey of patients with breast cancer with access to electronic health records reported a reduction in stress attributed to decreased wait time for results.16 Conversely, other series have described anxiety experienced by patients when viewing results electronically.17
Another critical issue going forward is the use of patient health portals as a means to contact the health care team. The “medical advice request” function in MyChart allows patients to send messages directly to providers and clinic staff. Perhaps most importantly, if time-sensitive messages are not seen promptly by the medical team, urgently needed medical attention may be delayed. More than 30% of medical advice requests were sent during nonclinic hours; for messages sent Friday afternoon, it is over 60 hours before clinic staff return to work. In contrast, patients who call our cancer center clinic after hours are connected via an operator to an on-call physician; there is no option to leave a voice message. Although the MyChart medical advice request function contains a warning to patients not to use the feature for medically urgent issues, this warning requires patients to be able to triage their own symptoms. There is also a growing societal expectation that text messaging provides a means of real-time communication.
Our study has a number of limitations. Race data are missing for almost half of patients. MyChart portal use by patients in the cohort was not necessarily restricted to their oncology care, as the MyChart application is currently used across various UT Southwestern clinical departments. We were not able to differentiate between viewing of laboratory and radiology results, with the latter possibly more likely to convey significant disease-related changes. Changes in MyChart functionality over the period of our study (eg, bill viewing and paying functions were not available until 2012, the last year of our study) skew our analysis of type of MyChart use. However, because billing options were the only function change during this period, the resulting impact on our findings is limited. Finally, generalizability of our findings is limited by the study cohort, as patients seeking care at National Cancer Institute–designated centers differ from the broader population by race, geographic location, and socioeconomic statusrace.18,19
The impact of electronic patient health portals on clinical care remains unclear. Recent systematic reviews have found no clear difference in health outcomes, but have noted possible increases in treatment compliance and patient perception of control with portal use.20,21 Somewhat unexpectedly, online access to medical records and clinicians has recently been associated with increased use of other medical services.3 As in other medical fields, implementation of this technology in oncology practice raises questions of cost, security, assignment of rights and responsibilities, and liability.22 From a clinical perspective, disease complexity and severity in cancer populations raise additional considerations for patients and providers, including the viewing of test results and sending of medical updates. Significant increases in portal use will place dramatic demands on clinical staff time and effort. Yet there is no standard means by which practices can be reimbursed for these tasks. Addressing these and other questions to ensure safety of patients and satisfaction of both patients and providers will be essential to realizing the benefits of this new technology.
Acknowledgment
Supported by a National Cancer Institute Cancer Clinical Investigator Team Leadership Award (1P30 CA142543-01 supplement, D.E.G.), National Institutes of Health 5R01CA152301, and Cancer Prevention and Research Institute of Texas RP101251 (Y.X.). Biostatistical support was provided by the Biostatistics and Bioinformatics Shared Resource at the Harold C. Simmons Cancer Center, University of Texas Southwestern Medical Center, Dallas, TX, which is supported in part by National Cancer Institute Cancer Center Support Grant 1P30 CA142543-03. S.J.C.L. is supported in part by a grant from the Agency for Healthcare Research and Quality (R24 HS022418) and the UT Southwestern Center for Patient-Centered Outcomes Research.
Presented in part at the ASCO Quality Care Symposium, San Diego, CA, November 1-2, 2013.
Appendix
Figure A1.
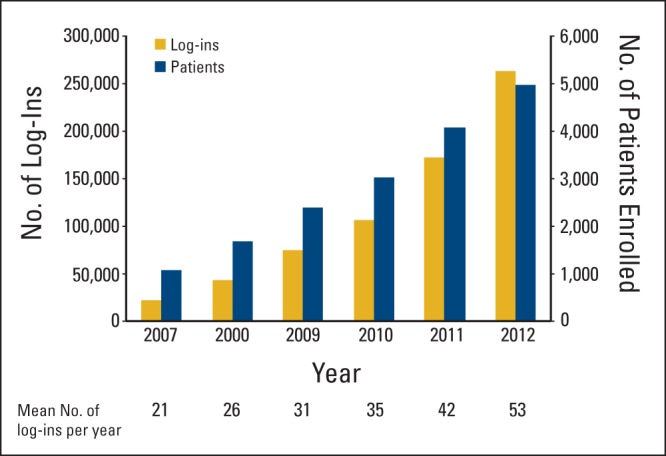
Number of active patients and total MyChart log-ins by year, timing of MyChart activity.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: David E. Gerber, Jingsheng Yan, Yang Xie, Simon J. Craddock Lee
Financial support: David E. Gerber
Administrative support: David E. Gerber, Simon J. Craddock Lee
Collection and assembly of data: David E. Gerber, Andrew L. Laccetti, Jingsheng Yan, Jennifer Cai, Samantha I. Gates, Yang Xie, Simon J. Craddock Lee
Data analysis and interpretation: David E. Gerber, Andrew L. Laccetti, Beibei Chen, Jingsheng Yan, Yang Xie, Simon J. Craddock Lee
Manuscript writing: All authors
Final approval of manuscript: All authors
References
- 1.Feeley TW, Shine KI. Access to the medical record for patients and involved providers: Transparency through electronic tools. Ann Intern Med. 2011;155:853–854. doi: 10.7326/0003-4819-155-12-201112200-00010. [DOI] [PubMed] [Google Scholar]
- 2.Goel MS, Brown TL, Williams A, et al. Patient reported barriers to enrolling in a patient portal. J Am Med Inform Assoc. 2011;18(suppl 1):i8–i12. doi: 10.1136/amiajnl-2011-000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palen TE, Ross C, Powers JD, et al. Association of online patient access to clinicians and medical records with use of clinical services. JAMA. 2012;308:2012–2019. doi: 10.1001/jama.2012.14126. [DOI] [PubMed] [Google Scholar]
- 4.Honeyman A, Cox B, Fisher B. Potential impacts of patient access to their electronic care records. Inform Prim Care. 2005;13:55–60. doi: 10.14236/jhi.v13i1.579. [DOI] [PubMed] [Google Scholar]
- 5.Cathala N, Brillat F, Mombet A, et al. Patient followup after radical prostatectomy by Internet medical file. J Urol. 2003;170:2284–7. doi: 10.1097/01.ju.0000095876.39932.4a. [DOI] [PubMed] [Google Scholar]
- 6.Byczkowski TL, Munafo JK, Britto MT. Variation in use of Internet-based patient portals by parents of children with chronic disease. Arch Pediatr Adolesc Med. 2011;165:405–411. doi: 10.1001/archpediatrics.2011.55. [DOI] [PubMed] [Google Scholar]
- 7.Fisher B, Bhavnani V, Winfield M. How patients use access to their full health records: A qualitative study of patients in general practice. J R Soc Med. 2009;102:539–544. doi: 10.1258/jrsm.2009.090328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weingart SN, Rind D, Tofias Z, et al. Who uses the patient internet portal? The PatientSite experience. J Am Med Inform Assoc. 2006;13:91–95. doi: 10.1197/jamia.M1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu PP. The evolution of oncology electronic health records. Cancer J. 2011;17:197–202. doi: 10.1097/PPO.0b013e3182269629. [DOI] [PubMed] [Google Scholar]
- 10.Wiljer D, Bogomilsky S, Catton P, et al. Getting results for hematology patients through access to the electronic health record. Can Oncol Nurs J. 2006;16:154–164. doi: 10.5737/1181912x163154158. [DOI] [PubMed] [Google Scholar]
- 11.Ralston JD, Rutter CM, Carrell D, et al. Patient use of secure electronic messaging within a shared medical record: A cross-sectional study. J Gen Intern Med. 2009;24:349–355. doi: 10.1007/s11606-008-0899-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burke RP, Rossi AF, Wilner BR, et al. Transforming patient and family access to medical information: Utilisation patterns of a patient-accessible electronic health record. Cardiol Young. 2010;20:477–4784. doi: 10.1017/S1047951110000363. [DOI] [PubMed] [Google Scholar]
- 13.Hsu J, Huang J, Kinsman J, et al. Use of e-Health services between 1999 and 2002: A growing digital divide. J Am Med Inform Assoc. 2005;12:164–171. doi: 10.1197/jamia.M1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Leon SF, Silfen SL, Wang JJ, et al. Patient experiences at primary care practices using electronic health records. J Med Pract Manage. 2012;28:169–176. [PubMed] [Google Scholar]
- 15.Cassileth BR, Zupkis RV, Sutton-Smith K, et al. Information and participation preferences among cancer patients. Ann Intern Med. 1980;92:832–836. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- 16.Wiljer D, Leonard KJ, Urowitz S, et al. The anxious wait: Assessing the impact of patient accessible EHRs for breast cancer patients. BMC Med Inform Decis Mak. 2010;10:46. doi: 10.1186/1472-6947-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ward ME. A cautionary tale of technology: Not a substitute for careful collaboration and effective communication. JONAS Healthc Law Ethics Regul. 2012;14:77–80. doi: 10.1097/NHL.0b013e318263eb0e. [DOI] [PubMed] [Google Scholar]
- 18.Onega T, Duell EJ, Shi X, et al. Determinants of NCI Cancer Center attendance in Medicare patients with lung, breast, colorectal, or prostate cancer. J Gen Intern Med. 2009;24:205–10. doi: 10.1007/s11606-008-0863-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onega T, Duell EJ, Shi X, et al. Influence of NCI cancer center attendance on mortality in lung, breast, colorectal, and prostate cancer patients. Med Care Res Rev. 2009;66:542–560. doi: 10.1177/1077558709335536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis Giardina T, Menon S, Parrish DE, et al. Patient access to medical records and healthcare outcomes: A systematic review. J Am Med Inform Assoc. doi: 10.1136/amiajnl-2013-002239. [epub ahead of print on October 23, 2013] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: A systematic review of controlled trials. J Med Internet Res. 2012;14:e162. doi: 10.2196/jmir.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beard L, Schein R, Morra D, et al. The challenges in making electronic health records accessible to patients. J Am Med Inform Assoc. 2012;19:116–20. doi: 10.1136/amiajnl-2011-000261. [DOI] [PMC free article] [PubMed] [Google Scholar]


