Abstract
Objectives To examine development in illness perceptions of type 1 diabetes across adolescence and relationships with intelligence, diabetes responsibility, and diabetes outcomes. Methods Illness perceptions were measured via the Illness Perceptions Questionnaire at 3 times, every 6 months in 213 adolescents (M age = 13.00; SD = 1.54) with type 1 diabetes. Intelligence and adolescents’ perceived responsibility for diabetes were examined, and adolescents’ report of adherence and quality of life (QOL), and glycosylated hemoglobin (HbA1c) from medical records addressed diabetes-related outcomes. Results Linear growth models showed significant increases in perceptions of diabetes coherence, chronicity, consequences, personal and treatment control, and decreases in diabetes cyclicality and parental control across time. More favorable illness perceptions were generally associated with adolescent intelligence at baseline, more adolescent responsibility for management, better adherence and QOL, and lower HbA1c at each time point. Conclusions Results suggest that adolescents develop complex illness perceptions, which are associated with better diabetes management.
Keywords: adherence, adolescents, illness perceptions, metabolic control, quality of life, type 1 diabetes
Adolescence is a critical time in diabetes management, as adolescents take on more responsibilities for their diabetes (Helgeson, Reynolds, Siminerio, Escobar, & Becker, 2008; Wiebe et al., 2014), establish autonomy (Wysocki et al., 1996), and cope with biological changes (Inagaki & Hatano, 2006). As adolescents seek to make sense of their illness, they develop illness perceptions that guide illness management (Leventhal et al., 1997) and are associated with psychological and illness-related outcomes (Hagger & Orbell, 2003). Illness perceptions are defined as a set of beliefs about an illness (Leventhal et al., 1997) that develop through physical experiences, exposure to medical encounters, and interpretation of information from social and factual sources, and are believed to be proximal guides to illness management, even if they are medically incorrect (Hagger & Orbell, 2003; Leventhal et al., 1997). Dimensions of illness perceptions include chronicity (belief that the illness will last for a long time), cyclicality (beliefs about the variability of the illness), consequences (beliefs about the severity of the illness), personal control (one’s own perceived control over the illness), treatment control (beliefs in the efficacy of the treatment regimen), coherence (belief that the illness and its treatment make sense), and emotional representations (beliefs that the illness has negative emotional consequences). Very little work examines how illness perceptions develop during periods of rapid developmental change such as adolescence (Skinner, John, & Hampson, 2000). Cross-sectional research suggests that illness perceptions may differ with age such that older adolescents have a more advanced understanding of their chronic illness than do younger adolescents (Olsen, Berg, & Wiebe, 2008). The goal of this study was to examine trajectories in illness perceptions of type 1 diabetes through the course of adolescence and the association of these perceptions with developmental and diabetes-related outcomes.
Across adolescence, illness perceptions may change as adolescents develop in their cognitive and socioemotional understanding (Smetana, Campione-Barr, & Metzger, 2006; Steinberg, 2010) and take on greater responsibility for diabetes care (Wiebe et al., 2014). In early adolescence, changes in levels of intellectual functioning may allow for a greater understanding of symptoms, causes, and consequences of childhood illnesses (Myant & Williams, 2005; Siegelman, Maddock, Epstein, & Carpenter, 1993). For example, older adolescents understand the implications of high glycosylated hemoglobin (HbA1c) values better than younger adolescents (Patino-Fernandez, Eidson, Sanchez, & Delameter, 2010). Additionally, increased experience with illnesses such as type 1 diabetes in children and adolescents is associated with more sophisticated understanding of the illness (e.g., symptom control through diet and insulin administration; Rubovits & Siegel, 1994). During adolescence, this greater experience with the illness coincides with adolescents increasingly managing diabetes independently from their parents (Wiebe et al., 2014), which may affect perceptions of their own and their treatment’s control over the illness.
These broader developmental changes may relate to changes in illness perceptions. Cross-sectional findings reveal that older adolescents with type 1 diabetes view the illness as more chronic and severe (Olsen et al., 2008) and treatment having greater control over the illness than younger adolescents (Gaston et al., 2012). In the one study examining illness perceptions over time during adolescence (Skinner et al., 2000), adolescents perceived diabetes as more serious and their treatment as more effective across a 6-month time frame.
Understanding developmental trajectories in illness perceptions among adolescents with type 1 diabetes is important because these perceptions guide illness management decisions, and may relate to adherence and psychosocial adjustment. An extensive literature in adults with diabetes and other chronic conditions has linked illness perceptions to adherence and psychosocial adjustment (Hagger & Orbell, 2003). In a recent review involving studies with adolescents, Law, Tolgyesi, and Howard (2012) identified control beliefs as especially important for adolescents’ self-management of diabetes as well as other chronic illnesses. However, results for other perceptions were mixed. For instance, while chronicity beliefs were not associated with adherence in three studies of adolescents with diabetes (Griva, Myers, & Newman, 2000; Law, Kelly, Huey, & Summerbell, 2002; Skinner et al., 2003), Gaston et al. (2012) found chronicity was associated with lower blood glucose monitoring. Similarly, Gaston et al. found that greater perceived consequences were associated with better blood glucose monitoring, whereas Skinner et al. (2000) found perceived consequences predicted poorer dietary self-care in adolescents with type 1 diabetes. Olsen et al. (2008) found that lower coherence was associated with poorer adjustment in adolescents with type 1 diabetes, whereas Law et al. (2002) reported coherence was unrelated to adherence and well-being in adolescents with diabetes, as well as other chronic illness. Owing to inconsistencies in the literature, the nature of the relationships between illness perceptions and diabetes outcomes among adolescents remains unclear. The present study adds to this literature by examining how illness perceptions, developmental factors, and diabetes-related outcomes are longitudinally associated across three time points in a large sample of adolescents with type 1 diabetes.
Given the changes in diabetes management that occur across adolescence, as well as normal developmental changes, we anticipated progressions in how adolescents perceive their illness. The goals of this study were to examine: (1) How adolescents’ perceptions of diabetes develop across time; we anticipated increases in personal control, treatment control, consequences, coherence, and chronicity, and decreases in parental control. (2) Whether changes in illness perceptions are associated with cognitive ability and the adolescent’s responsibility for diabetes management; based on previous research, we anticipated that higher baseline cognitive ability and more responsibility for diabetes management would relate to higher personal and treatment control, higher coherence, and lower parental control. (3) Whether illness perceptions across development are associated with diabetes-related outcomes, including HbA1c, adherence, and quality of life (QOL); we expected that personal and treatment control would be associated with more positive diabetes outcomes.
Methods
Participants
Data were from a larger longitudinal study that followed 252 families in 6-month intervals for 2.5 years to examine how adolescents and their parents cope with type 1 diabetes during adolescence. Unless otherwise noted, data from Time 2 (6 months post-enrollment; n = 213, M age = 13.00, SD = 1.54), Time 3 (6 months later; n = 196), and Time 4 (6 months from Time 3; n = 183) were analyzed because this is when illness perceptions were measured. Eligibility criteria at enrollment included 10–14-year-olds diagnosed with type 1 diabetes for at least 1 year, living with mother, and able to read and write English or Spanish. Of the eligible patients approached, 66% agreed to participate; refusals primarily involved distance issues, time constraints, and lack of interest. Eligible patients who did versus did not participate were older (12.5 vs. 11.6 years, t(367) = 6.20, p < .01), but did not differ on gender, illness duration, pump status, or metabolic control (ps > .20). At enrollment, approximately half (50.8%) of participants were using an insulin pump, while all others were prescribed multiple daily injections (4.14 mean insulin injections per day, SD = 1.81, range: 0–10; 5.53 mean blood glucose checks per day, SD = 1.70, range: 1–11). Participants were primarily Caucasian (94%) and middle class, with 73% of families earning more than $50,000 a year; average Hollingshead Index (1975) was 42.04, indicating medium business, minor professional, technical status.
Procedures
The institutional review board approved this study. Parents gave written consent and adolescents provided written assent. Participants were recruited during routine visits to a university diabetes clinic (76%) or a community-based private practice (24%) that followed similar treatment regimens. At all time points, participants were mailed measures to be completed at home and returned at their laboratory appointment with the research team. Instructions reiterated the importance of individually completing measures, and that all questions be directed to the research team (see Wiebe et al., 2014, for full study details).
Measures
Illness Perceptions
Participants completed the Illness Perceptions Questionnaire Revised (IPQ-R; Moss-Morris et al., 2002), an assessment of beliefs and emotional reactions about a chronic illness. See Table I for descriptive information and correlations with other variables. We assessed the following perceptions via subscales: chronicity (e.g., “My diabetes is likely to be permanent rather than temporary”; α range across time points = .77–-.83), cyclicality (e.g., “I go through cycles in which my diabetes gets better and worse”; α = .69–.79), consequences (“My diabetes has major consequences on my life”; α = .68–.71), personal control (e.g., “There is a lot I can do to control my symptoms”; α = .66–.81), treatment control (e.g., “My treatment can control my diabetes”; α = .58–.61), coherence (e.g., “I have a clear picture or understanding of my diabetes”; α = .85–.87), and emotional representations (e.g., “I get depressed when I think about my diabetes”; α = .79–.89). We added questions related to parent control to assess adolescents’ perceptions of parents’ control over the illness (e.g., “There is a lot my mother/father can do to control my symptoms”; α = .66–.69). Participants answered all 44 IPQ-R items (five to six per subscale) using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). Higher scores on the subscales indicate strongly held perceptions about the illness (e.g., scoring high on chronicity suggests a firm belief that the illness will last for a long time).
Table I.
Correlations Among Study Variablesa
| Variable | M (SD) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. IPQ chronicity | 3.99 (0.66) | −.14* | .08 | .29** | −.08 | .01 | .31** | −.04 | 0 | 0 | −.01 | −.15 | .01 |
| 2. IPQ cyclicality | 2.75 (0.83) | .44** | −.06 | .20** | −.06 | −.38** | .41** | −.37** | −.15* | .22** | .19** | −.33** | |
| 3. IPQ consequences | 3.28 (0.77) | .09 | .07 | −.07 | −.10 | .45** | −.35** | −.12 | .28** | .05 | −.30** | ||
| 4. IPQ personal control | 4.16 (0.60) | .08 | .47** | .35** | −.08 | .07 | .08 | .01 | .33** | .12 | |||
| 5. IPQ parent control | 3.05 (0.67) | .18* | −.12 | .11 | −.12 | .06 | .06 | −.28** | −.04 | ||||
| 6. IPQ treatment control | 3.72 (0.63) | .22** | −.20** | .14 | .12 | −.13 | −.16* | .16* | |||||
| 7. IPQ coherence | 4.09 (0.70) | −.39** | .34** | .02 | −.14* | −.38 | .10 | ||||||
| 8. IPQ emotional rep. | 2.42 (0.93) | −.52** | −.14* | .27** | .32** | −.15 | |||||||
| 9. Diabetes QOL | 70.54 (12.43) | .23** | −.39** | −.28** | −.17* | ||||||||
| 10. Adherence | 3.94 (0.58) | .27** | −.20** | 0 | .06 | ||||||||
| 11. HbA1c | 8.37 (1.58) | −.29** | −.31** | .08 | −.25** | ||||||||
| 12. DRS | 2.59 (0.62) | −.22** | −.01 | .02 | −.13 | ||||||||
| 13. KBIT-2 | 103.54 (13.36) | .29** | .12 | −.26** | −.17** |
Note. aAll variables in this table were measured at Time 2, with the exception of the KBIT-2, which was measured at Time 1.
**p < .01, *p < .05.
Diabetes Responsibility
Adolescents’ perceptions of who is responsible for completing 23 aspects of diabetes management (e.g., ‘‘Who determines the insulin dose?’’) were assessed with the Diabetes Responsibility and Conflict Scale (Rubin, Young-Hyman, & Peyrot, 1989), using a 5-point Likert-type scale (1 = I do it alone to 3 = I share equally with my parents to 5 = My parent does it alone) at each time point. Adolescents on diabetes pumps completed five additional items (e.g., “Who changes pump batteries?”), created through consultation with a diabetes educator and a person with diabetes, to be relevant to intensive management and pump regimens. Average scores across all items, including pump items when applicable, were analyzed, with a lower average score indicating greater personal responsibility for diabetes management. Internal consistency across items and each time point was excellent (α > .91).
Cognitive Functioning
As illness perceptions require cognitive understanding (Desrocher & Rovet, 2004), cognitive functioning (i.e., verbal intelligence measured with vocabulary and nonverbal intelligence measured with matrices) was measured at Time 1 only (i.e., 6 months before the first IPQ measure) using the Kaufman Brief Intelligence Test (KBIT-2; Kaufman & Kaufman, 2004). Split-half reliabilities were 0.92 for vocabulary and 0.87 for matrices/analogies; the composite score was used.
Diabetes Outcomes
Diabetes Quality of Life
Participants completed the Pediatric Quality of Life Inventory (PedsQL) Type 1 Diabetes Module (Varni et al., 2003), which assessed diabetes symptoms, treatment barriers, treatment adherence, worry, and communication over the preceding month. A large-scale factor analysis of the PedsQL supported the use of an overall QOL score (Nansel, Weisberg-Benchell, Wysocki, Laffel, & Anderson, 2008). At each time point, participants answered 28 items using a 5-point scale (0 = never a problem to 4 = almost always a problem). Internal consistency was good (α > .85 at all time points).
Adherence
Adherence to the diabetes regimen over the preceding month was assessed at each time point with a 16-item adapted version of the Self-Care Inventory (La Greca, Follansbee, & Skyler, 1990). The adaptations were made in consultation with a certified diabetes educator and a person with diabetes and involved adding two items (i.e., “How well have you followed recommendations for counting carbohydrates?” and “How well have you followed recommendations for calculating insulin doses based on carbohydrates in meals and snacks?”) and updating wording of items to capture current treatment standards. Adolescents rated adherence behaviors on a scale from 1 (never did it) to 5 (always did it as recommended without fail). Average scores across items were analyzed, with α ≥ .82 at all time points.
Metabolic Control
HbA1c levels were obtained by clinic staff using the Bayer DCA2000 at each time point, at the medical appointment before the research session. HbA1c is the average blood glucose level over the preceding 3 months, and is the current standard index to assess diabetes control, with a lower number indicating better metabolic control.
Analysis Plan
First, we performed a series of multilevel models (SAS PROC MIXED) examining longitudinal trajectories of each IPQ subscale across adolescence (ages 10–17). These unconditional growth models included no predictors or covariates except the indicator of growth, which was age, centered at 13 years. These models provided estimates of average intercepts and slopes, or fixed effects, as well as variability in intercepts and slopes. Second, we examined whether these intercepts or slopes were associated with intelligence at baseline and adolescent responsibility for managing diabetes at each time point. Finally, we examined in multilevel models whether illness perceptions were associated with diabetes-related outcomes across time, including HbA1c, adherence, and QOL (as time-varying covariates). In each of the models predicting diabetes outcomes, we controlled for gender, time since diagnosis, socioeconomic status (SES; Hollingshead Index), pump status, adolescent responsibility for diabetes management (at each time point), and intelligence. Due to associations among the IPQ subscales (rs up to .47), each subscale was examined in a separate multilevel model. Maximum likelihood estimation was used to account for missing data in all models.
Results
Trajectories of Illness Perceptions Across Time
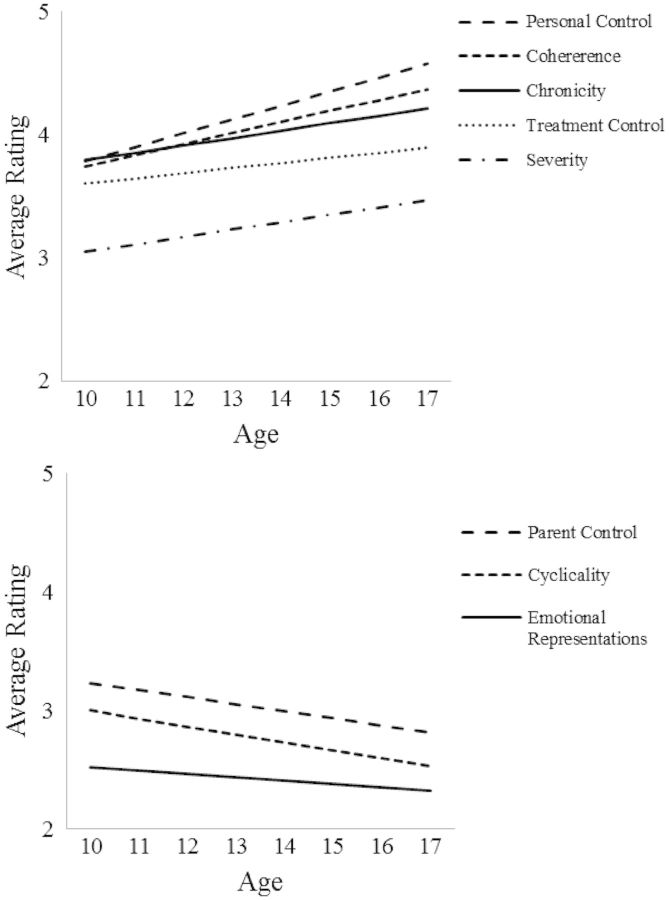
Table II presents results of unconditional growth models, which estimated fixed, or average, values of intercepts and slopes, and provided information about variability in intercepts and slopes (see Figure 1 for average trajectories). Significant linear slopes were found for all IPQ dimensions, with the exception of negative emotional perceptions, indicating that most illness perceptions changed over time. Significant positive slopes were found for chronicity, consequences, personal and treatment control, and coherence. Adolescents viewed their illness as increasing in chronicity and negative consequences, felt increasing personal and treatment control over the illness, and had a more coherent understanding of the illness as they became older. Significant negative slopes were found for cyclicality and parent control, suggesting that over time adolescents viewed their illness as less cyclical and their parents as having less control.
Table II.
Longitudinal Trajectories of Illness Representations: Results of Unconditional Growth Modelsa
| Variable | Fixed effects |
Variance components |
||||
|---|---|---|---|---|---|---|
| b | SE(b) | p | σ2 | SE | p | |
| Chronicity | ||||||
| Intercept | 3.97 | 0.04 | <.01 | 0.30 | 0.04 | <.01 |
| Slope (age)b | 0.06 | 0.02 | .01 | not estimated | ||
| Cyclicality | ||||||
| Intercept | 2.79 | 0.05 | <.01 | 0.36 | 0.07 | <.01 |
| Slope (age) | −0.07 | 0.03 | .02 | 0.02 | 0.02 | .40 |
| Consequences | ||||||
| Intercept | 3.23 | 0.05 | <.01 | 0.28 | 0.05 | <.01 |
| Slope (age) | 0.06 | 0.03 | .02 | 0.02 | 0.01 | .14 |
| Personal control | ||||||
| Intercept | 4.12 | 0.03 | <.01 | 0.18 | 0.02 | <.01 |
| Slope (age)b | 0.11 | 0.02 | <.01 | not estimated | ||
| Parent control | ||||||
| Intercept | 3.05 | 0.04 | <.01 | 0.21 | 0.04 | <.01 |
| Slope (age) | −0.06 | 0.02 | .00 | 0.00 | 0.01 | .83 |
| Treatment control | ||||||
| Intercept | 3.73 | 0.04 | <.01 | 0.13 | 0.03 | <.01 |
| Slope (age) | 0.04 | 0.02 | .05 | 0.02 | 0.01 | .04 |
| Coherence | ||||||
| Intercept | 4.02 | 0.05 | <.01 | 0.29 | 0.05 | <.01 |
| Slope (age) | 0.09 | 0.03 | <.01 | 0.02 | 0.02 | .25 |
| Emotional representations | ||||||
| Intercept | 2.43 | 0.06 | <.01 | 0.52 | 0.08 | <.01 |
| Slope (age) | −0.03 | 0.03 | .37 | 0.03 | 0.02 | .22 |
Note. aAge, centered at 13 years, was the marker of time (slope).
bThe initial model estimated negative variance in the slope, indicating variability in slopes was close to 0. The final model did not include a variance component for slope.
Figure 1.
Changes in illness representations across adolescence, centered at age 13.
Note: The downward trend for emotional representations was not significant.
Significant variability in the intercepts was found for each illness perception subscale, indicating that individuals differed in their average illness perception scores at age 13 (i.e., age was centered at 13 years). However, significant variation in slopes was only found for treatment control, indicating that with the exception of treatment control, individuals did not significantly vary in how rapidly illness representations changed over time.
Factors Associated With Illness Perceptions
We next conducted multilevel models predicting illness perceptions across time from intelligence, measured at baseline (Time 1), and adolescent diabetes responsibility (lower scores reflecting greater responsibility), measured at each time point. Adolescents with higher intelligence perceived that their diabetes was less cyclical (b = −0.017, SE = 0.004, p < .01), and that they (b = 0.008, SE = 0.002, p < .01) and their treatment (b = 0.008, SE = 0.002, p < .01) could control their diabetes. Higher intelligence was also associated with greater coherence (b = 0.007, SE = 0.003, p = .03), lower perceived consequences (b = −0.009, SE = 0.003, p < .01), and lower negative emotional response when thinking about diabetes (b = −0.009, SE = 0.004, p = .03). Adolescents with more diabetes responsibility perceived less parental control of diabetes (b = 0.287, SE = 0.057, p < .01), that treatment could help control their diabetes (b = −0.124, SE = 0.056, p = .03), and a more coherent diabetes understanding (b = −0.285, SE = 0.070, p < .01) across time. Adolescents with more diabetes responsibility also reported less negative emotional response when thinking about diabetes (b = 0.409, SE = 0.075, p < .01) and were less likely to believe their diabetes was cyclical (b = 0.151, SE = 0.073, p < .05).
Associations of Illness Perceptions With Diabetes Management Outcomes
To examine the associations between illness perceptions and diabetes-related outcomes across time, multilevel models were conducted to predict QOL, adherence, and HbA1c across time from the dimensions of the IPQ, controlling for baseline adolescent intelligence, SES, gender, and time since diagnosis, as well as pump status and diabetes responsibility, which were measured at each time point. Separate models were examined for each of these diabetes-related outcomes (Table III). Analyses predicting adherence indicated that across adolescence (ages 10–17), greater personal control, parental control, treatment control, coherence, and lower negative emotional representations were associated with better adherence (ps < .05). For analyses predicting metabolic control (HbA1c), perceiving the illness to have less severe consequences, to be less under parents’ control, to be more coherent, and to have fewer negative emotional consequences was associated with better Hba1c across adolescence (ps < .05). Finally, for analyses predicting QOL, lower cyclicality, lower consequences, higher treatment control, higher coherence, and lower negative emotional representations were associated with better QOL (ps < .05).
Table III.
Results of Multilevel Models Predicting Diabetes Outcomes From IPQ Subscalesa
| IPQ subscale | Adherence |
HbA1cb |
Quality of lifeb |
|||
|---|---|---|---|---|---|---|
| b | SE(b) | b | SE(b) | b | SE(b) | |
| Chronicity | 0.02 | 0.04 | 0.15 | 0.10 | −1.02 | 0.77 |
| Cyclicality | −0.04 | 0.03 | 0.15 | 0.08† | −1.94 | 0.61** |
| Consequences | −0.01 | 0.03 | 0.29 | 0.10** | −3.23 | 0.69** |
| Personal control | 0.19 | 0.04** | −0.11 | 0.12 | 1.23 | 0.85 |
| Parent control | 0.08 | 0.04* | 0.32 | 0.11** | 0.13 | 0.79 |
| Treatment control | 0.12 | 0.04** | −0.06 | 0.10 | 1.72 | 0.77* |
| Coherence | 0.11 | 0.03** | −0.23 | 0.10* | 2.59 | 0.70** |
| Emotional representations | −0.12 | 0.03** | 0.29 | 0.08** | −5.33 | 0.56** |
Note. †p < .08; *p < .05; **p < .01.
aEach IPQ subscale was entered in a separate model. Each model controlled for gender, time since diagnosis, baseline SES (Hollingshead Index), insulin pump status (time-varying), parent diabetes responsibility (time-varying), and baseline teen intelligence.
bIn all of the initial HbA1c models, and two of the initial quality of life models (i.e., models with IPQ consequences and emotional representations), results indicated a negative variance in the slope (i.e., Heywood Case). These models were subsequently re-estimated with the variance in the slope set to zero.
Discussion
This study demonstrates that adolescents’ perceptions of diabetes change across time and are associated with intelligence, diabetes responsibility, and diabetes outcomes. Adolescents viewed their diabetes as becoming more chronic, coherent, and controllable by both self and treatment, and involving more severe consequences. They also viewed their diabetes as becoming less cyclical and less controlled by parents, while emotional representations remained stable overall. Developments in illness perceptions are likely to be highly important, given our findings that illness perceptions also covaried with important indicators of diabetes management over time.
Illness perceptions occur in the context of other factors across adolescence, including one’s general intellectual ability and changing responsibility for diabetes management across time. The results suggest that a coherent understanding of diabetes that includes its severity and one’s personal and treatment control occurs in the context of greater intellectual ability and increasing responsibility for diabetes management. Greater intellectual ability and changes in adolescent responsibility may provide a context for the development of illness perceptions that reflect the serious nature of diabetes together with developing notions of personal and treatment control.
Increases in chronicity and severity of consequences and decreases in cyclicality over time may reflect a growing view of diabetes as an incurable illness. The increase in chronicity is consistent with cross-sectional findings of adolescents’ view of their diabetes (Gaston, Cottrell, & Fullen, 2012; Olsen et al., 2008), and the increase in consequences is consistent with results from cross-sectional (Olsen et al., 2008) and short-term longitudinal (Skinner et al., 2000) research. Although outcomes in the literature are mixed regarding illness consequences (Law et al., 2012), this increase may reflect a development of greater awareness of potential negative diabetes outcomes. Additionally, increases in treatment control over time suggest that adolescents are gaining better comprehension of their treatment regimen’s ability to control the symptoms of diabetes. These increases in treatment control occur while adolescents are perceiving their illness as more severe, suggesting that perceived severity motivates them toward greater adherence to aspects of their diabetes regimen as they approach adulthood. Support for this idea comes from the study by Gaston and colleagues (2012), where greater perceived threat of diabetes and greater perceived treatment control were associated with better blood glucose monitoring.
Greater personal control and illness coherence and lower parental control across time are consistent with developmental changes in adolescents gaining independence in managing their illness (Wiebe et al., 2014) and likely developing confidence in managing diabetes-related problems. Increases in illness coherence occurred at the same time that diabetes was perceived as becoming more chronic and severe. Developmental changes in cognitive and socioemotional maturation across this period (Smetana et al., 2006) may allow for greater understanding and acceptance of diabetes as a chronic disease with serious consequences. It should be noted that the increases across time in personal control and coherence and decreases in parental control were not found in the only other longitudinal study of illness perceptions (Skinner et al., 2000). The differences may be explained by increased sensitivity of using a longer time frame and larger sample size in this study.
It is interesting that adolescents are developing a more coherent understanding of diabetes and its treatment and view diabetes as increasingly controllable across a period during which adherence and metabolic control typically worsen (Helgeson et al., 2008; King, Berg, Butner, Butler, & Wiebe, 2014). Although these findings may appear contradictory, it is likely that increased independence in diabetes management may allow adolescents to develop perceptions of their illness that may not sufficiently counter other factors that contribute to poorer adherence and metabolic control across time such as pubertal changes, peer influences, and declining parental responsibility. For instance, Wiebe et al. (2014) found that across adolescence, declines in parental responsibility occur at the same time that increases in self-efficacy and declines in adolescent adherence occur. Additional longitudinal research across adolescence and emerging adulthood may elucidate how changes in illness perceptions prepare individuals for managing diabetes more independently from parents in the context of friends and romantic partners.
Illness Perceptions and Diabetes-Related Outcomes
These developments in illness perceptions are significant because illness perceptions were associated with adhering to the complex diabetes regimen, achieving good metabolic control, and maintaining QOL. Our findings revealed somewhat different patterns of associations across these outcomes. Across time, fluctuations in personal and treatment control covaried with fluctuations in adherence; when adolescents perceived greater control, they also reported better adherence. These results are in line with Law et al.’s (2012) conclusions that perceptions of personal and treatment control are most consistently related to illness management during adolescence. The fact that control perceptions were unrelated to QOL and metabolic control suggests that they may primarily be important for facilitating the behavioral management of diabetes. Coherence, which has not been systematically studied among adolescence, also related to better adherence. This belief could relate to a better overall understanding of healthy versus unhealthy metabolic control, leading to an easier time maintaining regimen adherence. Finally, parental control was associated with better adherence over time, which is consistent with previous research suggesting that early withdrawal of parental involvement is associated with declines in adherence (Wiebe et al., 2014).
Although illness representations were associated with diabetes outcomes across time, it is important to note that our analyses do not allow us to disentangle the direction of effects. Leventhal’s self-regulation model (Leventhal et al., 1997) conceives illness perceptions as part of a dynamic model in which perceptions are continuously updated by illness-relevant experiences, but also guide subsequent illness management behaviors. These bidirectional processes may explain the associations of illness perceptions with QOL and metabolic control, where fluctuations in perceived negative consequences of diabetes and cyclical beliefs were associated with fluctuations in poorer outcomes across time. It is possible that perceiving serious consequences contributes to poorer metabolic control and QOL (e.g., by creating pessimistic views of one’s current and future life). Alternatively, when adolescents experience poorer metabolic control or believe that their illness undermines QOL, they may perceive diabetes as having more negative consequences (Hagger & Orbell, 2003). Poor metabolic control may therefore contribute to both lower QOL and greater variability in symptoms (Wagner, Muller-Godeffroy, Von Sengbusch, Hager, & Thyen, 2005). Bidirectional associations may also have contributed to the associations between parental control and diabetes outcomes. We suspect that the association between parental control and HbA1c reflects that HbA1c is a salient predictor to parents of how well their adolescent is doing at managing diabetes, and that poor metabolic control cues parents to step in and more actively facilitate their adolescent’s diabetes management (Berg et al., 2013). Future research aimed at disentangling potential bidirectional effects will be important for understanding the complex association between beliefs regarding parent control and diabetes outcomes.
These findings should be interpreted in the context of some limitations. First, our sample is relatively ethnically homogeneous, consistent with the state’s population from which the sample was drawn. The development of illness perceptions could vary in different cultural contexts (Bauman, 2003). For example, fatalistic perceptions that little can be done to avoid the complications of chronic illness have been expressed among those of Latino and Hispanic cultural backgrounds (Quatromoni et al., 1994), which may relate to a different developmental course of perceived personal and treatment control. Second, given the restrictions of data analysis with variables having high multicollinearity, we were unable to examine statistically which dimension of the IPQ was most strongly associated with diabetes outcomes (i.e., could not examine the variables simultaneously). This limitation also created additional analyses that may have inflated our type 1 error rate. Third, it should be noted that adherence, diabetes responsibility, and illness perceptions are teen-reported, and thus may reflect a shared underlying construct related to adolescent perceptions. Fourth, although intelligence as measured by the K-BIT is considered stable, it would have been helpful to have this measured each time point, as performance could potentially be impacted by variation in blood glucose levels. Finally, having only three time points may have prevented us from finding individual variation in rate of change of illness representations across time. Examining illness representations across a longer period would allow for more complex models of change that would address specific directions of effects between illness representations and diabetes-related outcomes, including reciprocal relationships.
Implications and Future Directions
These results suggest that diverse aspects of illness perceptions are involved in an adolescent’s evolving understanding of type 1 diabetes. Understanding such illness perceptions and their development may be useful for healthcare providers, as they assist adolescents in better diabetes management. Understanding whether these perceptions are adaptive in promoting good illness management is an important area for future research. If so, measuring illness perceptions in clinical settings and using that information to guide diabetes education efforts, or developing clinical interventions to increase cognitive or behavioral factors underlying perceptions such as diabetes control and coherence, could improve diabetes outcomes. Such illness perceptions may intersect with numerous other developments during adolescence, including greater competencies in diabetes numeracy (e.g., counting carbohydrates and dosing insulin; Mulvaney, Lilley, Cavanaugh, Pittel, & Rothman, 2013), cognitive changes, and socioemotional abilities. As teens increasingly managing their diabetes independently from their parents, adolescence may be a key time for developing illness perceptions.
Acknowledgments
The authors thank the families that participated, the physicians (Mary Murray, David Donaldson, Rob Lindsay, Carol Foster, Michael Johnson, and Marie Simard) and staff of the Utah Diabetes Center, Mike T. Swinyard, and all members of the ADAPT team. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Funding
National Institute of Diabetes and Digestive Kidney Diseases Grant R01 DK063044-01A1, awarded to D. J. W. (principal investigator) and C. A. B. (coprincipal investigator).
Conflicts of interest: None declared.
References
- Bauman L C. Culture and illness representations. In: Cameron L D, Leventhal H, editors. The self-regulation of health and illness behavior. London, UK: Taylor & Francis; 2003. pp. 242–254. [Google Scholar]
- Berg C A, Butner J E, Butler J M, King P S, Hughes A E, Wiebe D J. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychology. 2013;32:719–728. doi: 10.1037/a0029427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desrocher M, Rovet J. Neurocognitive correlates of type 1 diabetes mellitus in childhood. Child Neuropsychology. 2004;10:36–52. doi: 10.1076/chin.10.1.36.26241. [DOI] [PubMed] [Google Scholar]
- Gaston A M, Cottrell D J, Fullen T. An examination of how adolescent-caregiver dyad illness representations relate to adolescents’ reported diabetes self-management. Child: Care, Health and Development. 2012;38:513–519. doi: 10.1111/j.1365-2214.2011.01269.x. [DOI] [PubMed] [Google Scholar]
- Griva K, Myers L B, Newman S. Illness perceptions and self-efficacy beliefs in adolescents and young adults with insulin dependent diabetes mellitus. Psychology and Health. 2000;15:733–750. [Google Scholar]
- Hagger M S, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychology and Health. 2003;18:141–184. [Google Scholar]
- Helgeson V S, Reynolds K A, Siminerio L, Escobar O, Becker D. Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology. 2008;33:497–508. doi: 10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead A B. Four factor index of social status. 1975 Unpublished manuscript, Yale University, New Haven, CT. [Google Scholar]
- Inagaki K, Hatano G. Young children’s conception of the biological world. Current Directions in Psychological Science. 2006;15:177–181. [Google Scholar]
- Kaufman A S, Kaufman N L. Kaufman brief intelligence test. 2nd ed. Circle Pines, MN: AGS Publishing; 2004. [Google Scholar]
- King PS, Berg C, Butner J, Butler J M, Wiebe D J. Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychology. 2014;33:424–432. doi: 10.1037/a0032804. doi:10.1037/a0032804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A M, Follansbee D, Skyler J S. Developmental and behavioral aspects of diabetes management in youngsters. Children’s Health Care. 1990;19:132–139. [Google Scholar]
- Law G U, Kelly T P, Huey D, Summerbell C. Self-management and well-being in adolescents with diabetes mellitus: Do illness representations play a regulatory role? Journal of Adolescent Health. 2002;31:381–385. doi: 10.1016/s1054-139x(02)00397-x. [DOI] [PubMed] [Google Scholar]
- Law G U, Tolgyesi C S, Howard R A. Illness beliefs and self-management in children and young people with chronic illness: a systematic review. Health Psychology Review. 2012;8:362–380. doi: 10.1080/17437199.2012.747123. doi:10.1080/17437199.2012.747123. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Benjamin Y, Brownlee S, Diefenbach M, Leventhal E A, Patrick-Miller L, Robitaille C. Illness representations: Theoretical foundations. In: Petrie K J, Weinman J, editors. Perceptions of health and illness. London, UK: Harwood Academic Publishers; 1997. pp. 19–45. [Google Scholar]
- Moss-Morris R, Weinman J, Petric K J, Horne R, Cameron L D, Buick D. The revised illness perception questionnaire (IPQ-R) Psychology and Health. 2002;17:1–16. [Google Scholar]
- Mulvaney S A, Lilley J S, Cavanaugh K L, Pittel E J, Rothman R L. Validation of the diabetes numeracy test with adolescents with type 1 diabetes. Journal of Health Communication: International Perspectives. 2013;18:795–804. doi: 10.1080/10810730.2012.757394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myant K A, Williams J M. Children’s concepts of health and illness: Understanding of contagious illnesses, non-contagious illnesses and injuries. Journal of Health Psychology. 2005;10:805–819. doi: 10.1177/1359105305057315. [DOI] [PubMed] [Google Scholar]
- Nansel T R, Weisberg-Benchell J, Wysocki T, Laffel L, Anderson B. Quality of life in children with type 1 diabetes; A comparison of general and diabetes-specific measures, and support for a unitary diabetes quality of life construct. Diabetes Medicine. 2008;25:1316–1323. doi: 10.1111/j.1464-5491.2008.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen B, Berg CA, Wiebe DJ. Dissimilarity in mother and illness representations of type 1 diabetes and negative emotional adjustment. Psychology and Health. 2008;23:113–129. doi: 10.1080/08870440701437343. [DOI] [PubMed] [Google Scholar]
- Patino-Fernandez A M, Eidson M, Sanchez J, Delameter A M. What do youth with type 1 diabetes know about the HbA1c test? Children’s Health Care. 2010;38:157–167. doi: 10.1080/02739610902813328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quatromoni P A, Milbauer M, Posner B M, Carballeira N P, Brunt M, Chipkin S T. Use of focus groups to explore nutrition practices and health beliefs of urban Caribbean Latinos with diabetes. Diabetes Care. 1994;17: 869–873. doi: 10.2337/diacare.17.8.869. [DOI] [PubMed] [Google Scholar]
- Rubin R R, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes Care. 1989;38:28A. [Google Scholar]
- Rubovits D S, Siegel A W. Developing conceptions of chronic disease: A comparison of disease experience. Children Health Care. 1994;23:267–285. doi: 10.1207/s15326888chc2304_3. [DOI] [PubMed] [Google Scholar]
- Siegelman C, Maddock A, Epstein J, Carpenter W. Age differences in understandings of disease causality: AIDS, colds and cancer. Child Development. 1993;64:272–284. [PubMed] [Google Scholar]
- Skinner T C, Howells L, Greene S, Edgart K, McEvilly K, Johansson A. Development, reliability and validity of the Diabetes Illness Representations Questionnaire: Four studies with adolescents. Diabetic Medicine. 2003;20:283–289. doi: 10.1046/j.1464-5491.2003.00923.x. [DOI] [PubMed] [Google Scholar]
- Skinner T C, John M, Hampson S E. Social support and personal models of diabetes as predicators of self-care and well-being: A longitudinal study of adolescents with diabetes. Journal of Pediatric Psychology. 2000;25:257–267. doi: 10.1093/jpepsy/25.4.257. [DOI] [PubMed] [Google Scholar]
- Smetana J G, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annual Review of Psychology. 2006;57:255–284. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Varni J W, Burwinkle T M, Jacobs J R, Gottschalk M, Kaufman F, Jones K L. The PedsQLTM in type 1 and type 2 diabetes: Reliability and validity of the pediatric quality of life inventory generic core scales and type 1 diabetes module. Diabetes Care. 2003;26:631–637. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- Wagner V M, Muller-Godeffroy E, von Sengbusch S, Hager S, Thyen U. Age, metabolic control and type of insulin regime influences health-related quality of life in children and adolescents with type 1 diabetes mellitus. European Journal of Pediatrics. 2005;164:491–496. doi: 10.1007/s00431-005-1681-4. [DOI] [PubMed] [Google Scholar]
- Wiebe D J, Chow C M, Palmer D L, Butner J, Butler J M, Osborn P, Berg C A. Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. Journal of Pediatric Psychology. 2014;39:532–541. doi: 10.1093/jpepsy/jsu006. doi:10.1093/jpepsy/jsu006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Linschied T R, Taylor A, Yeates K O, Hough B S, Naglieri J A. Deviation from developmentally appropriate self-care autonomy. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]