Abstract
Background/Aims:
The aim of the following study is to compare the behavioral and psychological symptoms of dementia (BPSD) in patients of Alzheimer disease (AD) and vascular dementia (VaD).
Materials and Methods:
We used National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association criteria for diagnosing AD and National Institute of Neurological Disorders and Stroke-Association International pour la Recherche et l’Enseignement en Neurosciences Criteria for diagnosing VaD. VaD cohort was further subcategorized into small vessel and large vessel disease. The severity of cognitive impairment and the BPSD were studied by means of the Clinical Dementia Rating Scale (CDR) and the Neuropsychiatric Inventory respectively.
Results:
We studied 50 AD and 50 VaD patients of whom 38 were small vessels and 12 were large vessels VaD. The severity of dementia was comparable in both groups. The agitation/aggression, depression/dysphoria, anxiety, apathy/indifference, irritability, aberrant motor behavior, appetite and eating behavior and night-time behaviors occurred significantly more frequently in patients with VaD than AD. We found a weak positive correlation between the CDR score and the number of neuropsychiatric symptoms per patient in both cohorts. Elation/euphoria, agitation/aggression was significantly more frequent in patients with large vessel in comparison to small vessel VaD.
Conclusions:
BPSD are common in both types of dementia and they are more severe in VaD than AD when the groups have similar levels of cognitive impairment.
Keywords: Alzheimer disease, behavioral and psychological symptoms of dementia, neuropsychiatric inventory, small vessel disease, vascular dementia
Introduction
Along with cognitive decline, most patients of dementia develop changes in mood, perception, thought and personality. These neuropsychiatric symptoms are increasingly recognized as important clinical features of the dementia syndromes and have been designated as “behavioral and psychological symptoms of dementia” (BPSD) by the International Psychogeriatric Association.[1] These symptoms impact the quality-of-life of patients with dementia and have been associated with increased caregiver burden, more rapid progression of cognitive and functional decline and earlier institutionalization and mortality.
Several studies have found that neuropsychiatric symptoms are common both in patients with Alzheimer disease (AD) and those with vascular dementia (VaD). Though VaD is the second most common type of dementia world-wide, in contrast to AD only a couple of small studies on neuropsychiatric symptoms have been conducted in VaD.
VaD can be broadly classified as small-vessel disease (lacunes, white matter hyperintensities or bilateral thalamic lesions, multiple lacunar lesions in basal ganglia) or large vessel disease (large territorial or strategic infarcts) or combination of both diseases. A broad variety of psychological and behavioral symptoms have been demonstrated in both small and large vessel VaD and in contrast to AD, apathy, depressive symptoms and agitation/aggression have been found more common and severe in VaD.[2,3,4,5,6,7,8,9] The studies examining VaD and AD have been hampered by methodological shortcomings. First, VaD was mostly not the main diagnosis under study as studies investigated a large sample of AD patients with a small additional group of VaD patients. Furthermore, diagnostic criteria and methods to assess presence of symptoms, are difficult to compare due to differences in populations, diagnostic criteria and methods to assess presence of symptoms.
Many studies from India reported a high prevalence of BPSD in patients with dementia.[10,11,12,13,14] These studies however, reported higher frequencies of symptoms in patients with AD as compared to patients with VaD.[10,12] Although some of them were clinic-based studies[10,11,12,14] others were community-based studies.[13] In most of these studies criteria for AD and VaD was not well-defined. Some of them have noted a strong correlation between the severities of dementia with that of BPSD[10,11,14] while others found less number of symptoms in advanced stage of dementia.[12]
In a recent study, Gupta et al., used Neuropsychiatric Inventory (NPI) as tool to assess BPSD and showed that all patients of VaD and 89% of patients with vascular cognitive impairment without dementia (VCI-ND) reported some neuropsychiatric symptoms.[14]
The BPSD lead to lower levels of cognitive functioning. Early recognition and characterization of BPSD is important as their management is feasible. The treatment of BPSD leads to the overall functional improvement and quality-of-life of patient with dementia.[15] Thus, knowledge about the frequencies and severity of BPSD of common types of dementia is important for their management.
Aim of the study
In this study, we planned to determine the frequency of different types of neuropsychiatric and behavioral manifestations in patients of AD and VaD and to compare the profile of neuropsychiatric symptoms between these two groups. We also aimed to compare the neuropsychiatric and behavioral manifestations in patients of small-vessel VaD and large vessel VaD.
Materials and Methods
Participants, materials and procedure
We selected patients from Neurology out-patient department and the Cognitive Disorders Clinic of the Institute between January 2011 and December 2012. Consecutive patients of AD and VaD were included for the study. We excluded patients of mixed dementia and those of mild cognitive impairment (MCI), VCI-ND and patients having combination of small and large vessel VaD. Each patient was clinically evaluated with detailed history supplemented with general physical and neurological examination and assessment of cognitive functions as per protocol. We used the mini-mental status exam (MMSE) for initial screening. Further, we used the Kolkata Cognitive Test Battery[16] and we also separately tested the language, praxis performance, executive functioning, as well as visuospatial and visuoperceptual functioning using standard methods. Each patient was then subjected to investigations including hematological, biochemical and radiological test as well as tests for venereal disease research laboratory and human immunodeficiency virus. A cranial magnetic resonance imaging or computed tomography scan was also performed. Some special investigations (e.g., electroencephalography, cerebrospinal fluid analysis) were undertaken wherever investigators thought they were necessary. The diagnosis of dementia was made according to the Diagnostic and Statistical Manual of mental disorders, 4th edition criteria.[4] Severity of dementia was assessed by clinical dementia rating scale (CDR).[17]
We used National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association criteria for diagnosing AD and National Institute of Neurological Disorders and Stroke-Association International pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN) criteria for diagnosing VaD. The VaD cohort was further subcategorized into small-vessel and large vessel disease according to the operational definitions for NINDS-AIREN criteria (radiological) of VaD.[18] Based on these criteria patients were classified as having large vessel VaD (strategic large-vessel infarct of the dominant hemisphere or bilateral hemispheric strokes) or small vessel VaD (white matter hyperintensities involving atleast a quarter of the white matter, multiple lacunes or bilateral thalamic lesions). We excluded those patients who were having both small and large vessel disease in imaging.
Behavioral and psychological symptoms were evaluated on the basis of the NPI[19] in the presence of a reliable caregiver. The original NPI was translated in to Bengali by two neurologists and a psychologist independently. These translations were pooled together and a final version was prepared. The Bengali version was then translated back in to English. The translation-retranslation reliability was found to be satisfactory. The Bengali version was then used for the study. The individual domain scores for each of the 12 neuropsychiatric symptoms was obtained by calculating the product of the frequency and severity scores of each symptom. The sum of these domain scores yielded the total NPI score for each patient.
Statistical analysis
The mean age and educational status and the mean number of neuropsychiatric symptoms per patient, between AD and VaD groups were compared using the unpaired t test, whereas the gender distribution and frequency of occurrence of individual neuropsychiatric symptoms were compared by the Chi-square test. Correlations between the CDR score and the number of neuropsychiatric symptoms or the NPI score (individual domain scores and total NPI scores) were obtained by calculating Spearman correlation coefficients. P ≤ 0.05 was considered to be statistically significant.
Results and Analysis
In the present study, a total of 100 patients were studied. These patients included 50 patients with AD and 50 patients with VaD.
Demographic profile
The mean age of the entire patient group was 65.76 (standard deviation [SD] 11.68, range: 48-81) years. Although the mean age of the AD patients was 71.94 (SD 6.05, range: 60-81) years, that of VaD patients was 59.58 (SD 6.56, range: 48-79) years. Thus, our AD cohort were older than our VaD cohort (P < 0.05). The entire group was comprised of 69% men and 31% women [Table 1]. The AD patients included 31 men (62%) and 19 women (38%), whereas the VaD group included 38 men (76%) and 12 women (24%) respectively. In both the AD and VaD groups, male patients outnumbered female patients, but the two groups did not significantly differ in gender.
Table 1.
Comparison of demographic profile between AD versus VaD and between small vessel VaD versus large vessel VaD
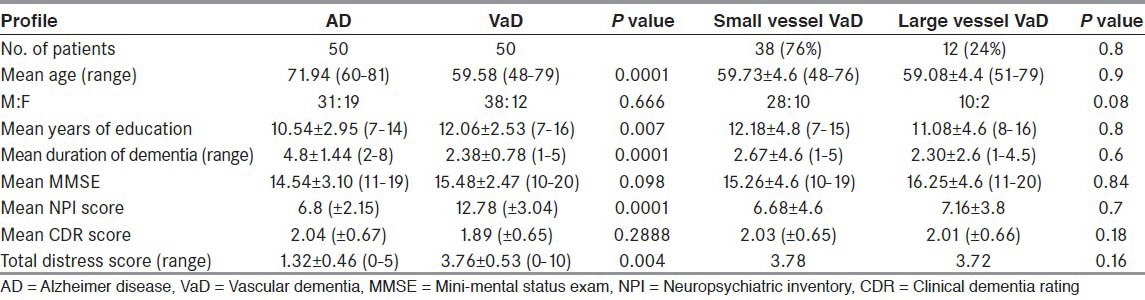
The mean years of education was 10.54 years (SD 2.95, range: 7-14) for the AD group and 12.06 years (SD 2.53, range: 7-16) for the VaD group indicating that the mean years of education was higher in the VaD group in comparison to the AD group (P = 0.007).
Duration of dementia
The mean duration of dementia was 4.8 years (SD 1.44, range: 2-8) for the AD group and 2.38 years (SD 0.78, range: 1-5) for the VaD group. The mean duration of dementia at the time of attendance to our clinic was greater in the AD group than in the VaD group (P = 0.0001).
MMSE score in AD and VaD
The mean MMSE score was 14.54 (SD 3.10, range: 11-19) for AD group and 15.48 (SD 2.47, range 10-20) for VaD group. The mean MMSE scores of both groups were not different (P = 0.098).
In the AD group of patients the mean CDR score was 2.04 (SD: 0.67, range: 1-3) and in the VaD group of patients the mean CDR score was 2.02 (SD: 0.65, range: 1-3). The mean CDR score of both groups were not significantly different (P = 0.288).
NPI score
Overall, 96% patients displayed at least one neuropsychiatric symptom on the NPI. The number of patients with a NPI score ≥1 was 46 (92%) in the AD group and 48 (96%) in the VaD group. Thus, neuropsychiatric manifestation is almost universal in patients with AD and patients with VaD. The mean number of symptoms per patient on the NPI was 6.8 (±2.15) in the AD group and 12.78 (±3.04) in the VaD group. Thus, our VaD cohort demonstrated more neuropsychiatric symptoms when compared to our AD cohort (P = 0.0001).
Total distress score
Patients were analyzed regarding their total distress score. The mean total distress scores were 1.32 (SD 0.46, range: 0-5) for the AD group and 3.76 (SD 0.53, range: 1-10) for the VaD group. The total distress score was significantly greater in VaD patients than AD patients (P = 0.004).
Neuropsychiatric profile
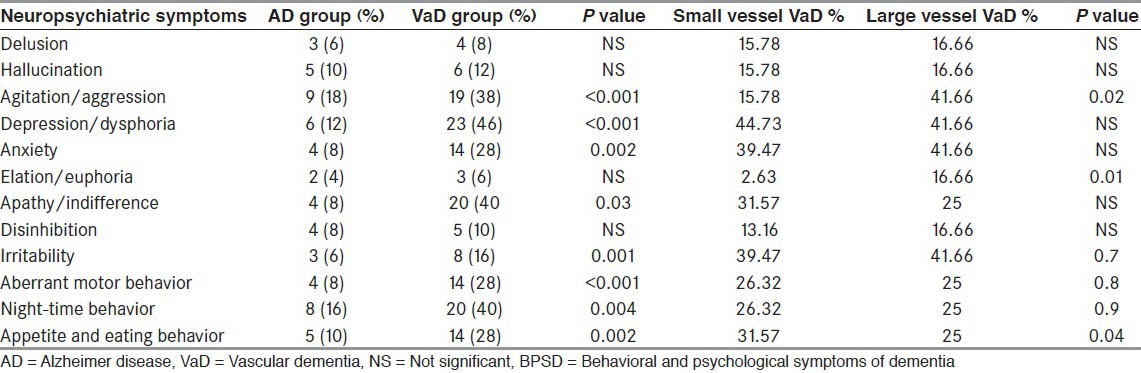
The neuropsychiatric profile was assessed using NPI scale. Agitation/aggression (38% in VaD vs. 18% in AD, P < 0.02), depression/dysphoria (46 % vs. 12%, P < 0.001), anxiety (28% vs. 8%, P = 0.003), apathy/indifference (40% vs. 8%, P < 0.001), irritability (16% vs. 6%, P = 0.001), aberrant motor behavior (28% vs. 8%, P < 0.001), appetite and eating behavior (28% vs. 10%, P = 0.002) and night-time behaviors (40% vs. 16%, P = 0.004) occurred more frequently in VaD patients than in AD patients. The frequency of delusions, hallucinations, disinhibition, elation/euphoria was although observed slightly higher in VaD patients than in AD patients, the difference was not significant (P > 0.05). As an overall view, almost all the neuropsychiatric symptoms were more frequent in the VaD patients in comparison to the AD patients when the groups demonstrated similar levels of cognitive impairment [Table 2].
Table 2.
Comparison of frequency of various BPSD between AD and VaD and between small vessel VaD versus large vessel VaD
We found a weak positive correlation between the CDR score and the number of symptoms per patient (r = 0.217) in both cohorts, suggesting increased numbers of neuropsychiatric symptoms with increased severity of dementia.
Neuropsychiatric profile in small vessel and large vessel VaD
After subcategorization of the VaD patients into small-vessel (small-vessel VaD) and large vessel groups (large vessel VaD). We analyzed and compared the demographic profile as well as the frequency of neuropsychiatric symptoms in the two subgroups. In our study, small-vessel disease was found to be more frequent (76% vs. 24%) than large vessel VaD. We did not find any significant difference in demographic parameters between small-vessel and large vessel VaD. In our study, neuropsychiatric profiles were found to be different in two subgroups of VaD. Elation/euphoria (16.66% inlarge-vessel VaD vs. 2.63% in small-vessel VaD, P = 0.01) and agitation/aggression (41.66% vs. 15.78%, P = 0.02), were observed more frequently in patients with large vessel VaD in comparison to small-vessel VaD. Though there were minor differences in frequency of other neuropsychiatric parameters between small-vessel and large vessel VaD, these differences were not significant (P > 0.05).
Discussion
The current study was performed to determine the frequency of neuropsychiatric manifestations among patients of AD and VaD and to compare the profile of neuropsychiatric manifestations among them. We also planned to look into the neuropsychiatric profiles of two common subcategories of VaD, (large vessels vs. small vessels disease).
While comparing the demographic profiles of two cohorts, we found that AD patients were older; less educated and reported longer duration of dementia than VaD patients. However, the mean MMSE and CDR score were not different across the two groups. Of the neuropsychiatric symptoms, agitation/aggression, depression/dysphoria, anxiety, apathy/indifference, irritability, aberrant motor behavior, appetite and eating behavior and night-time behavior were observed significantly more frequently in VaD patients than AD patients. The frequency of delusions, hallucinations, disinhibition, elation/euphoria was although slightly more common in VaD patients than in AD patients, but this difference was not significant (P > 0.05). These findings demonstrate that VaD patients display more severe behavioral retardation, depression and anxiety than AD patients, when the groups demonstrate similar levels of cognitive impairment which probably reflects the contrasting brain regions generally involved in the two disorders. This high prevalence of depression, blunted affect, apathy, behavioral retardation in patients with VaD reflect the involvement of subcortical-frontal pathway that occurs with cerebrovascular disease. Patients with AD experience involvement of more posterior cortical regions than patients with VaD, which suggests that these regions may not play an important role in the expression of these particular psychiatric symptoms.
Our observation with respect to the neuropsychiatric profiles of AD and VaD patients is similar to the observations by Sultzer et al.,[20] Cooper et al.,[21] Swearer et al.,[22] Sultzer et al., observed in their studies that patients with VaD showed greater subjectively experienced symptoms of behavioral disorder, anxiety, depression than patients with AD, in addition to more severe neuro-vegetative signs when the groups demonstrated similar levels of cognitive impairment.[20] A study by Swearer et al., also found increased frequency of depression, delusion, hallucination and other behavioral disturbances in patients with advanced VaD.[22] Cooper et al., also had similar findings.[21] However, Bucht et al., reported that patients with VaD reported lower level of depression or fewer psychopathological symptoms than patients with AD.[23] In another study, Kim et al., found that BPSD were more severe in VaD patients as compared to AD patients.[24] Fuh et al., found that neuropsychiatric symptoms were more common in VaD patients when compared to AD patients and sleep disturbance was the most common symptom.[25]
We found a weak positive correlation between the severity of dementia and severity of neuropsychiatric symptom in both the AD and VaD group of patients. Studies of Román et al.,[7] and Suzuki et al.,[9] showed no significant correlations between severity of cognitive impairment and extent of most personality changes in patients with VaD. Some other studies however, have demonstrated a strong correlation between the severity of BPSD and the degree of cognitive impairment in VaD.[26] On the other hand, Kim et al., observed a strong correlation of BPSD with cognitive and activities of daily living impairment in AD patients but not in VaD patients.[24] In another study Zhang et al., compared the prevalence of neuropsychiatric symptoms across the declining memory continuum in AD patients (i.e., normal controls, subjective cognitive impairment, MCI and mild AD) and found the prevalence of BPSD to be higher at the higher end of the spectrum, i.e., mild AD. The total NPI scores also were found to increase progressively along the continuum. Agitation, apathy and aberrant motor behavior were significantly more common in mild AD group than in the other groups.[27] In their study Gupta et al., reported a significant positive correlation between the CDR score and the number of symptoms per patient in patients of VaD.[14]
After sub-categorization of VaD patients into large vessel (n = 38, 76%) and small vessel VaD (n = 12, 24%) we compared the demographic profile and neuropsychiatric profile among the two sub-groups of VaD. In our cohort, small-vessel group of VaD were larger (76% vs. 24%) than large vessel group of VaD. We did not find any significant differences in the demographic parameters between small-vessel and large vessel group of VaD. The neuropsychiatric profiles were found to be different in the two subgroups of VaD. Elation/euphoria and agitation/aggression were observed significantly more frequently in patients with large vessel VaD in comparison to small-vessel VaD in the current experiment. Though there was minor difference in frequency of other neuropsychiatric parameters between large and small vessel VaD these differences are not statistically significant (P > 0.05). This observation is concordant with the study of Staekenborg et al.,[28] who found that the profile of neuropsychiatric symptoms differed between small-vessel and large vessel VaD. They also observed that agitation/aggression and euphoria were more severe in patients with large-vessel VaD; whereas apathy, aberrant motor behavior and hallucinations were more severe and more frequent in patients with small-vessel VaD. In their study, Fuh et al., found that neuropsychiatric symptoms were more common in cortical VaD patients as compared to subcortical VaD and AD patients.[25] Sleep disturbance was the most common symptom.
Erkinjuntti et al., showed that depression and apathy were common in patients with VaD affecting subcortical structures.[2] Ishii et al., found that mood changes, lack of initiative and akinetic mutism were common in patients with lacunar stroke and hypothesized that this increased frequency was due to lacunae in the frontal white matter and basal ganglia.[29] In the current study, however, no significant difference in frequency of apathy, aberrant motor behavior and hallucinations were found between small-vessel and large vessel VaD. This may be because of smaller sample size in current series.
The strength of this study is that it was a clinic based study and thus each patient was evaluated in detail using a standardized assessment tool and brain imaging. The data was collected by a single investigator. Moreover, subgroups have similar demographic characteristics. However, the current study was limited in atleast two ways. First, participants in the study were selected from the Cognitive clinic of a tertiary referral center, which means that caution should be taken in generalizing the results of the study until they can be replicated in further studies. Second, the rate of diagnostic misclassification was uncertain because of the lack of neuropathological confirmation in the study. The future studies must look into the neuropsychiatric symptoms of a larger number of patients involving all subgroups and autopsy confirmation of the diagnosis. That would give a more detailed insight about the subject.
Conclusions
The present study demonstrated that behavioral and psychiatric disturbances are very common in patients with AD as well as patients with VaD. The current study also demonstrates that patients with VaD report more severe behavioral and psychiatric symptoms than patients with AD when the group's report similar levels of cognitive impairment. This finding probably reflects the contrasting brain regions typically involved in the two disorders. The agitation/aggression, depression/dysphoria, anxiety, apathy/indifference, irritability, aberrant motor behavior, appetite and eating behavior and night-time behavior occurred more frequently in patients with VaD than in patients with AD. The frequency of delusions, hallucinations, disinhibition, elation/euphoria was common in patients with VaD as well as in patients with AD. We found a weak positive correlation between the CDR score and the number of neuropsychiatric symptoms per patient in both cohorts suggesting an increase in the number of neuropsychiatric symptoms with increasing severity of dementia. The neuropsychiatric profiles were found to be different in two subgroups of VaD. Elation/euphoria, agitation/aggression was more frequent in patients with large vessel VaD in comparison to small vessel VaD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Finkel SI, Costa de Silva J, Cohen G, Miller S, Sartorius N. Behavioral and psychological signs and symptoms of dementia: A consensus statement on current knowledge and implications for research and treatment. Int Psychogeriatr. 1996;8:497–500. doi: 10.1017/s1041610297003943. [DOI] [PubMed] [Google Scholar]
- 2.Erkinjuntti T, Hachinski VC. Rethinking vascular dementia. Cerebrovasc Dis. 1993;3:3–23. [Google Scholar]
- 3.World Health Organisation. Geneva: World Health Organisation; 1995. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; pp. 50–1. [Google Scholar]
- 4.American Psychiatric Association. Washington DC: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM IV) pp. 143–7. [Google Scholar]
- 5.Bowler JV, Hachinski V. Vascular dementia. In: Feinberg TE, Farah MJ, editors. Behavioural Neurology and Neurophysiology. McGraw-Hill: New York; 1997. pp. 589–603. [Google Scholar]
- 6.Chui HC, Victoroff JI, Margolin D, Jagust W, Shankle R, Katzman R. Criteria for the diagnosis of ischemic vascular dementia proposed by the State of California Alzheimer's Disease Diagnostic and Treatment Centers. Neurology. 1992;42:473–80. doi: 10.1212/wnl.42.3.473. [DOI] [PubMed] [Google Scholar]
- 7.Román GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, et al. Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250–60. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 8.Almkvist O. Neuropsychological deficits in vascular dementia in relation to Alzheimer's disease: Reviewing evidence for functional similarity or divergence. Dementia. 1994;5:203–9. doi: 10.1159/000106724. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki K, Kutsuzawa T, Nakazima K, Hatano S. Epidemiology of vascular dementia and stroke in Akita, Japan. In: Hartmann A, Kuschinsky W, Hoyer S, editors. Cerebral Ischemia and Dementia. Berlin: Springer-Verlag; 1991. pp. 16–24. [Google Scholar]
- 10.Pinto C, Seethalakshmi R. Behavioral and psychological symptoms of dementia in an Indian population: Comparison between Alzheimer's disease and vascular dementia. Int Psychogeriatr. 2006;18:87–93. doi: 10.1017/S104161020500311X. [DOI] [PubMed] [Google Scholar]
- 11.Pinto C, Seetalakshmi R. Longitudinal progression of behavioral and psychological symptoms of dementia: A pilot study from India. Psychogeriatrics. 2006;6:154–8. [Google Scholar]
- 12.Shaji KS, George RK, Prince MJ, Jacob KS. Behavioral symptoms and caregiver burden in dementia. Indian J Psychiatry. 2009;51:45–9. doi: 10.4103/0019-5545.44905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shaji S, Bose S, Kuriakose S. Behavioral and psychological symptoms of dementia: A study of symptomatology. Indian J Psychiatry. 2009;51:38–41. doi: 10.4103/0019-5545.44903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta M, Dasgupta A, Khwaja GA, Chowdhury D, Patidar Y, Batra A. The profile of behavioral and psychological symptoms in vascular cognitive impairment with and without dementia. Ann Indian Acad Neurol. 2013;16:599–602. doi: 10.4103/0972-2327.120488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brody JA. An epidemiologist views senile dementia — Facts and fragments. Am J Epidemiol. 1982;115:155–62. doi: 10.1093/oxfordjournals.aje.a113286. [DOI] [PubMed] [Google Scholar]
- 16.Das SK, Banerjee TK, Mukherjee CS, Bose P, Biswas A, Hazra A, et al. An urban community-based study of cognitive function. Neurol Asia. 2006;11:37–48. [Google Scholar]
- 17.Morris JC. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993;43:2412–4. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 18.van Straaten EC, Scheltens P, Knol DL, van Buchem MA, van Dijk EJ, Hofman PA, et al. Operational definitions for the NINDS-AIREN criteria for vascular dementia: An interobserver study. Stroke. 2003;34:1907–12. doi: 10.1161/01.STR.0000083050.44441.10. [DOI] [PubMed] [Google Scholar]
- 19.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–14. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 20.Sultzer DL, Levin HS, Mahler ME, High WM, Cummings JL. A comparison of psychiatric symptoms in vascular dementia and Alzheimer's disease. Am J Psychiatry. 1993;150:1806–12. doi: 10.1176/ajp.150.12.1806. [DOI] [PubMed] [Google Scholar]
- 21.Cooper JK, Mungas D, Weiler PG. Relation of cognitive status and abnormal behaviors in Alzheimer's disease. J Am Geriatr Soc. 1990;38:867–70. doi: 10.1111/j.1532-5415.1990.tb05701.x. [DOI] [PubMed] [Google Scholar]
- 22.Swearer JM, Drachman DA, O’Donnell BF, Mitchell AL. Troublesome and disruptive behaviors in dementia. Relationships to diagnosis and disease severity. J Am Geriatr Soc. 1988;36:784–90. doi: 10.1111/j.1532-5415.1988.tb04260.x. [DOI] [PubMed] [Google Scholar]
- 23.Bucht G, Adolfsson R, Winblad B. Dementia of the Alzheimer type and multi-infarct dementia: A clinical description and diagnostic problems. J Am Geriatr Soc. 1984;32:491–8. doi: 10.1111/j.1532-5415.1984.tb02233.x. [DOI] [PubMed] [Google Scholar]
- 24.Kim JM, Lyons D, Shin IS, Yoon JS. Differences in the behavioral and psychological symptoms between Alzheimer's disease and vascular dementia: Are the different pharmacologic treatment strategies justifiable? Hum Psychopharmacol. 2003;18:215–20. doi: 10.1002/hup.466. [DOI] [PubMed] [Google Scholar]
- 25.Fuh JL, Wang SJ, Cummings JL. Neuropsychiatric profiles in patients with Alzheimer's disease and vascular dementia. J Neurol Neurosurg Psychiatry. 2005;76:1337–41. doi: 10.1136/jnnp.2004.056408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson C, Brodaty H, Trollor J, Sachdev P. Behavioral and psychological symptoms associated with dementia subtype and severity. Int Psychogeriatr. 2010;22:300–5. doi: 10.1017/S1041610209991220. [DOI] [PubMed] [Google Scholar]
- 27.Zhang M, Wang H, Li T, Yu X. Prevalence of Neuropsychiatric Symptoms across the Declining Memory Continuum: An Observational Study in a Memory Clinic Setting. Dement Geriatr Cogn Dis Extra. 2012;2:200–8. doi: 10.1159/000338410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Staekenborg SS, Su T, van Straaten EC, Lane R, Scheltens P, Barkhof F, et al. Behavioural and psychological symptoms in vascular dementia; differences between small- and large-vessel disease. J Neurol Neurosurg Psychiatry. 2010;81:547–51. doi: 10.1136/jnnp.2009.187500. [DOI] [PubMed] [Google Scholar]
- 29.Ishii H, Meguro K, Yamaguchi S, Ishikawa H, Yamadori A. Prevalence and cognitive performances of vascular cognitive impairment no dementia in Japan: The Osaki-Tajiri Project. Eur J Neurol. 2007;14:609–16. doi: 10.1111/j.1468-1331.2007.01781.x. [DOI] [PubMed] [Google Scholar]


