Abstract
Introduction:
Monitoring the disease progression in amyotrophic lateral sclerosis (ALS) is a challenge due to different rates of progression between patients. Besides clinical methods to monitor disease progression, such as the ALS functional rating scale (ALSFRS) and the medical research council (MRC) sum score, quantitative methods like motor unit number estimation (MUNE) are of interest.
Objective:
The objective of the present study is to evaluate the rate of progression in ALS using multipoint incremental MUNE and to compare MUNE, ALSFRS and MRC sum score at baseline and at 6 months for progression of the disease.
Materials and Methods:
Multipoint incremental MUNE using median nerve, ALS-FRS and MRC sum score was carried out in 29 ALS patients at baseline and then at 6 months.
Results:
Of the 29 ALS patients studied, the mean MUNE at baseline was 21.80 (standard deviation [SD]: 19.46, range 4-73), 15.9 in the spinal onset group (SD: 14.60) and 30.16 (SD: 22.89) in the bulbar onset group. Spinal onset patients had 74.02% of baseline MUNE value while bulbar onset patients had only 24.74% baseline value MUNE at 6 months follow-up (Unpaired t-test, P = 0.001). ALSFRS and MRC sum score showed statistically significant decline (P < 0.001) at 6 months follow-up. MUNE had the highest sensitivity for progression of the disease when compared to the ALS FRS and MRC sum score.
Conclusion:
Multipoint incremental MUNE is a valuable tool for outcome measure in ALS and other diseases characterized by motor unit loss. The rate of decline of multipoint incremental MUNE is more sensitive than that of MRC sum score and ALSFRS-R, when expressed as the percentage change from baseline.
Keywords: Amyotrophic lateral sclerosis functional rating scale, amyotrophic lateral sclerosis, compound muscle action potential, medical research council sum score, motor unit estimation, single motor unit action potential amplitude
Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder of undetermined etiology that affects the upper and lower motor neurons.[1] Until now, there has been no effective treatment of ALS. Monitoring the disease progression is a challenge due to different rates of progression between patients. There is a growing interest in methods to monitor disease progression in ALS. Besides clinical methods to monitor disease progression, such as the ALS functional rating scale (ALSFRS) and the medical research council (MRC) scale, quantitative methods that are more directly related to the underlying disease process are of interest.[2,3] A motor unit consists of a single lower motor neuron and the muscle fibers that it innervates. The number of motor units in a muscle cannot be measured precisely, although various methods can be used to obtain a motor unit number estimate (MUNE). MUNE techniques,[4] are all based on surface electromyography (EMG) measurements. MUNE measures the actual number of axons that innervate a muscle, rapidly and reliably. The difference between many MUNE methods depends on the method of how the size of the single motor unit potentials (SMUP) is determined. In all the methods, the number of motor units in the muscle is calculated by dividing compound motor unit action potential (CMAP) by the size of the SMUP.[5,6,7,8] MUNE is the only method, which can concurrently show motor unit loss (decreased MUNE) and track collateral reinnervation (via increases in mean SMUP amplitude).
Multipoint incremental MUNE is a reliable and sensitive outcome measure in ALS and other diseases characterized by motor unit loss. It's repeatability and rates of decline that favorably compare with other previously described methods.[8] In this study, we examined the rate of progression in ALS using multipoint incremental MUNE and to compare MUNE, ALS FRS and MRC sum score at baseline and at 6 months for progression of disease and to know, which the better predictor of progression is.
Materials and Methods
The study was carried out at Sree Chitra Institute for Medical sciences and technology during the period of June 2010 to June 2012. The patients with ALS as defined by the modified El Escorial Criteria were included in the study. Modified ALS FRS[2] as well as the MRC sum score[3] was calculated at baseline and then at 6 months.
MUNE method
Median nerve of the right or left hand was studied. Recording electrodes were placed on the median nerve innervated abductor pollicis brevis muscle, using the standard belly-tendon method. Three stimulus locations were used for the median nerve; 2 cm proximal to the wrist crease, 4 cm proximal to the first stimulation site, and in the cubital fossa. Filter settings were 2 Hz-10 KHz. For each stimulation site, optimum stimulus location was determined using a submaximal stimulus and moving the stimulator to evoke the greatest response. Amplifier settings were then changed to 200 μV/division. Using standard 3-site motor conduction program traces were obtained and superimposed. Stimulus intensity was slowly increased until an all-or-nothing initial response was obtained and baseline to negative peak amplitude was measured. Three responses were obtained at each stimulation site with each response of 25 μV incremental amplitude. The negative peak amplitude of the third response was recorded. Stimulation at the second and third location was identical to the first and second. Once sample collection was complete, we reviewed all tracings for potential repeating motor units (so that they were not included more than once).
Single motor unit action potential amplitude (SMUAP) and MUNE calculation
The SMUAP amplitude was calculated by summing amplitude of the third response at each site and then divided by nine. The MUNE was calculated by dividing SMUP by the maximum compound motor unit action potential (CMAP) amplitude. MUNE was calculated at baseline and at 6 month for evaluation of rate of decline.
At the first visit, the upper limbs were evaluated clinically, if both upper limbs had clinically detectable weakness, the stronger of the two hands was chosen. In case of weakness only in one limb, that limb was studied. The presence of median neuropathy at the wrist was ruled out in the selected hand for study by performing standard motor and sensory nerve conduction study using standard technique. If the CMAP amplitude was <5 mV, the other hand was studied in similar fashion, to choose a nerve/muscle not affected by focal neuropathy and with CMAP amplitude in the low normal range. MUNE in all patients was done by Preetha Govind and test retest reliability was 0.8.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences version 17. Paired t-tests were used to compare MUNE, ALSFRS and MRC sum score at baseline and at 6 months. Survival functions of patients with MUNE value below and above five were explored using the Kaplan–Meier survival curves and the log-rank test. Receiver operator curve (ROC) curve analysis was done for prediction of death during follow-up using the MUNE, ALSFRS and MRC sum scores at baseline.
Results
There were 29 patients, 19 were males and 10 were females. Age of onset was 24.5-78.9 year (mean: 51.5). The duration of symptom was 1-60 months (mean: 13 month). There were 17 patients with spinal onset and 12 with the bulbar onset. Mean duration of symptom in spinal onset was 18 months (range: 3-24 month), while in bulbar onset it was 6 months (range: 1-18). Age of onset in spinal onset group was 24.5-61.6 year (mean: 45.0). Age of onset in bulbar onset group was 45-78.9 year (mean: 58.6). Five patients had definite, 15 had Probable and nine had laboratory supported probable ALS as per modified El Escorial criteria. The mean MUNE in patients at entry in the study was 21.80 (standard deviation [SD] 19.46, range: 4-73). At the entry in the study, the mean MUNE in male was 18.4 (SD: 15.52) and 28.96 (SD: 24.70) in females, which did not show any statistical significance.
In spinal onset group, the MUNE was 15.9 (SD: 14.60) and 30.16 (SD: 22.89) in the bulbar onset group, revealed no statistical significance. At 6 months, MUNE was 8.46 (SD: 14.03) and 24 (SD: 15.37) in spinal and bulbar onset group, respectively. Limb onset patients had 74.02% of baseline value, while bulbar onset patients had only 24.74% MUNE at 6 months follow-up when compared to the baseline value, unpaired t-test, P = 0.001 [Figure 1].
Figure 1.

Graph showing decline of motor unit number estimation between bulbar and spinal-onset group at baseline and 6 months
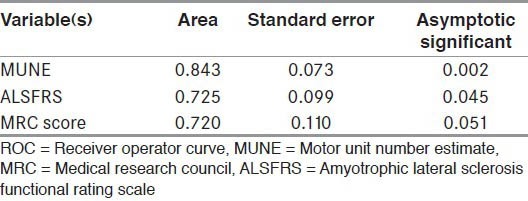
Mean ALS FR score was 37.12 (SD: 6.4) at study entry and 32 (SD: 7.9) at 6 months follow-up which showed statistically significant decline (P < 0.001). Mean MRC sum score was 50.86 (SD: 11.72) at study entry and 44.73 (SD: 14.64) at 6 months follow-up which showed statistically significant decline (P < 0.001). Of the MUNE, ALS-FR score and MRC sum score, MUNE had the highest sensitivity for progression of the disease when compared to the ALS FR and MRC sum score [Table 1, Figure 2]. Eleven patients expired during follow-up within 3 months to 12 months of first visit [Table 2]. The mean MUNE in these patients was 9.3 (range: 4-26) with a CMAP amplitude of 6.0 (range: 5-8). Kaplan–Meier survival analysis revealed a significantly lower mean survival (Log rank test, P = 0.002) with MUNE value of below five as compared to MUNE value above five, the mean survival times being 7.5 months and 10.5 months respectively, [Table 2, Figure 3]. ROC analysis revealed MUNE value as the more accurate predictor of death during follow-up with a higher area under curve for MUNE as compared to ALS-FRS. Area under the ROC curve for MRC sum score was not statistically significant [Table 3].
Table 1.
Comparison between MUNE, ALSFRS and MRC sum score at baseline and 6 months
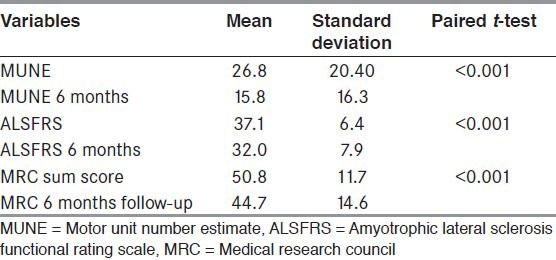
Figure 2.
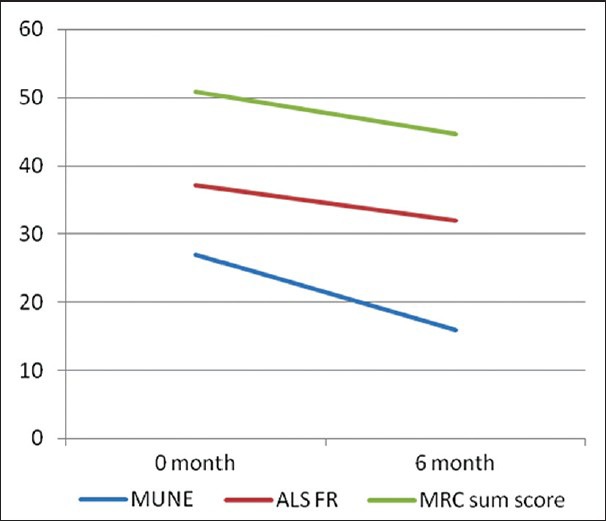
Graph showing comparison between motor unit number estimation, amyotrophic lateral sclerosis functional rating scale and medical research council sum score at baseline and 6 month
Table 2.
Number of patients who expired with MUNE value below and above 5
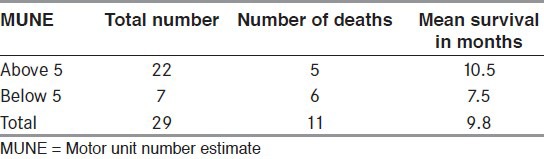
Figure 3.
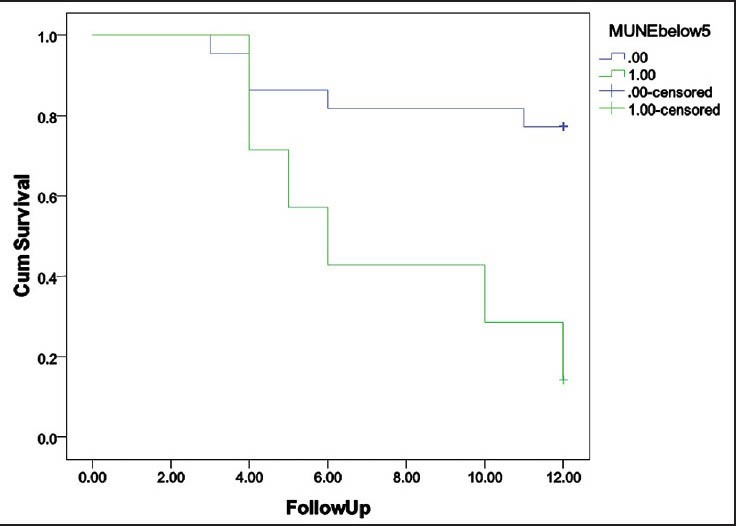
Kaplan–Meier survival curve with motor unit number estimation (MUNE) value of below and above 5; 1-survival curve of patients who expired with MUNE value below and above 5
Table 3.
ROC curve analysis was done for prediction of death during follow-up
Discussion
This study shows that multipoint incremental MUNE value declines faster than other commonly employed outcome measures like ALS FRS-R, MRC sum score used in ALS trials. Using the multipoint method, % change of MUNE was found to be greater than change in MRC sum score or the revised ALS FRS over a 6 month period, approaching 60% on average. A similar decline in multipoint MUNE in natural history study of patients with ALS was found in the study by Mitsumoto et al.[7] A study by Shefner also showed average 60% decline in MUNE at 1 year.[10] A study employing an entirely different technique, the incremental method, by Dantes and McComas identified virtually the same rate of decline.[11] The protocol performing this method of motor unit estimation is simple and can be performed on any EMG machine and in a uniform fashion. The ALSFRS-R is commonly used as the primary outcome in recent ALS trials. The rates of decline of multipoint incremental MUNE compares favorably to both MRC sum score and ALSFRS-R, when expressed as % change from baseline.[12]
The advantages of multipoint incremental MUNE are (1) relatively easy to perform, amplitude criteria used rather than duration avoiding variation in calculation (2) can be performed on any EMG machine, (3) good test retest reliability and (4) is well-tolerated by patients.[8] The limitation of this method are (1) there may be error in estimation using amplitude as the measure of interest when summation of units is not linear, (2) same unit may be sampled at different locations, resulting in the further reduction of the sample on which MUNE is estimated. Despite this, multipoint incremental MUNE can be considered as a valuable tool for outcome measurement in patients with ALS.
Conclusion
Multipoint incremental MUNE is a valuable tool for outcome measure in ALS and other diseases characterized by motor unit loss. The rate of decline of multipoint incremental MUNE is more sensitive than that of MRC sum score and ALSFRS-R, when expressed as percentage change from baseline.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Dengler R. Amyotrophic lateral sclerosis: Who has the lead, the upper or the lower motor neuron? Clin Neurophysiol. 2011;122:433–4. doi: 10.1016/j.clinph.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al. The ALSFRS-R: A revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III) J Neurol Sci. 1999;169:13–21. doi: 10.1016/s0022-510x(99)00210-5. [DOI] [PubMed] [Google Scholar]
- 3.Kleyweg RP, van der Meché FG, Schmitz PI. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle Nerve. 1991;14:1103–9. doi: 10.1002/mus.880141111. [DOI] [PubMed] [Google Scholar]
- 4.Shefner JM, Cudkowicz ME, Schoenfeld D, Conrad T, Taft J, Chilton M, et al. A clinical trial of creatine in ALS. Neurology. 2004;63:1656–61. doi: 10.1212/01.wnl.0000142992.81995.f0. [DOI] [PubMed] [Google Scholar]
- 5.McComas AJ, Fawcett PR, Campbell MJ, Sica RE. Electrophysiological estimation of the number of motor units within a human muscle. J Neurol Neurosurg Psychiatry. 1971;34:121–31. doi: 10.1136/jnnp.34.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang FC, Delwaide PJ. Number and relative size of thenar motor units estimated by an adapted multiple point stimulation method. Muscle Nerve. 1995;18:969–79. doi: 10.1002/mus.880180908. [DOI] [PubMed] [Google Scholar]
- 7.Mitsumoto H, Ulug AM, Pullman SL, Gooch CL, Chan S, Tang MX, et al. Quantitative objective markers for upper and lower motor neuron dysfunction in ALS. Neurology. 2007;68:1402–10. doi: 10.1212/01.wnl.0000260065.57832.87. [DOI] [PubMed] [Google Scholar]
- 8.Shefner JM, Watson ML, Simionescu L, Caress JB, Burns TM, Maragakis NJ, et al. Multipoint incremental motor unit number estimation as an outcome measure in ALS. Neurology. 2011;77:235–41. doi: 10.1212/WNL.0b013e318225aabf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armon C, Brandstater ME. Motor unit number estimate-based rates of progression of ALS predict patient survival. Muscle Nerve. 1999;22:1571–5. doi: 10.1002/(sici)1097-4598(199911)22:11<1571::aid-mus13>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 10.Shefner JM. Motor unit number estimation in human neurological diseases and animal models. Clin Neurophysiol. 2001;112:955–64. doi: 10.1016/s1388-2457(01)00520-x. [DOI] [PubMed] [Google Scholar]
- 11.Dantes M, McComas A. The extent and time course of motoneuron involvement in amyotrophic lateral sclerosis. Muscle Nerve. 1991;14:416–21. doi: 10.1002/mus.880140506. [DOI] [PubMed] [Google Scholar]
- 12.Yuen EC, Olney RK. Longitudinal study of fiber density and motor unit number estimate in patients with amyotrophic lateral sclerosis. Neurology. 1997;49:573–8. doi: 10.1212/wnl.49.2.573. [DOI] [PubMed] [Google Scholar]


