Abstract
Objective: We examined pregnant women’s likelihood of vaccinating their infants against seasonal influenza via a randomized message framing study. Using Prospect Theory, we tested gain- and loss-frame message effects and demographic and psychosocial correlates of influenza immunization intention. We also explored interactions among pregnant women who viewed “Contagion” to understand cultural influences on message perception.
Methods: Pregnant women ages 18–50 participated in a randomized message framing study from September 2011 through May 2012 that included exposure to intervention or control messages, coupled with questionnaire completion. Venue-based sampling was used to recruit racial and ethnic minority female participants at locations throughout Atlanta, Georgia. Bivariate and multivariate analyses were conducted to evaluate key outcomes.
Results: The study population (n = 261) included many lower income (≤ $20 000/yearly household earnings) pregnant participants (69.2%, n = 171) inclusive of Black/African Americans (88.5%, n = 230), Hispanic/Latinas (7.3%, n = 19), and Other/Multicultural women (4.2%, n = 11). Both gain [OR = 2.13, 90% CI: (1.120, 4.048)] and loss-frame messages [OR = 2.02, 90% CI: (1.083, 3.787)] were significantly associated with infant influenza vaccination intention compared with the control condition. Intention to immunize against influenza during pregnancy had a strong effect on intent to immunize infants [OR = 10.83, 90%CI: (4.923, 23.825)]. Those who had seen the feature film “Contagion” (n = 54, 20.69%) viewed gain- and loss-framed messages as appealing (x2 = 6.03, p = 0.05), novel (x2 = 6.24, p = 0.03), and easy to remember (x2 = 16.33, P = 0.0003).
Conclusions: In this population, both gain- and loss-framed messages were positively associated with increased maternal intent to immunize infants against influenza. Message resonance was enhanced among those who saw the film “Contagion.” Additionally, history of immunization was strongly associated with infant immunization intention.
Keywords: message framing, prospect theory, influenza vaccination, immunization coverage, pregnant women, racial/ethnic minorities, contagion
Introduction
Influenza causes significant morbidity and mortality, particularly among vulnerable populations such as pregnant women, who are at increased risk for influenza-related morbidity and mortality.1-4 The American College of Obstetricians and Gynecologists (ACOG) and the Advisory Committee on Immunization Practices (ACIP) recommend that pregnant and expecting women receive the trivalent inactivated influenza vaccine.3,5,6 Influenza immunization protects both mother and child, with infants up to six months showing decreased risk of contracting influenza.3 Maternal immunization is critical to reducing adverse fetal and neonatal outcomes such as premature birth and low gestational weight, which are seen in infants of mothers who do not receive the influenza vaccine.7,8
Despite the benefits of seasonal influenza immunization during pregnancy, vaccination coverage among pregnant women remains suboptimal. Common perceptions such as the vaccine giving influenza (14%), a lack of concern about influenza severity (12.6%), perceptions of vaccine ineffectiveness (11.7%), and a lack of health insurance and inability to handle immunization cost (6.8%) have been cited as significant barriers to immunization during pregnancy.9-12 Suboptimal coverage among pregnant women in the United States is also driven by sociodemographic disparities in immunization. Disparities in vaccination coverage for pregnant women are evident among those without higher education (39% coverage) compared with those with a college degree (53.9% coverage).
Studies indicate that racial and ethnic minorities may be less likely to receive12 and less aware of13 vaccines such as human papillomavirus virus vaccine (HPV) and the 2009 pandemic (H1N1) influenza vaccine. Black/African American and Hispanic pregnant women and younger infants have historically experienced higher morbidity, mortality, and hospitalizations due to influenza.14-20 Incidence data from 2010–2011 points to greater influenza-related mortality among Hispanic infants (68 cases/100 000 population) compared with non-Hispanics (39 cases/100 000).14,21-24
Low rates of vaccine acceptance and awareness in this population provide an epidemiologic argument for outreach to racial and ethnical minority women. To our knowledge, little immunization messaging and research has been done among racial and ethnic minority women, who have much lower vaccination rates compared with whites, and higher rates of influenza associated mortality and complications.17,25-27 As a result, we focused our study on identifying barriers to influenza immunization specific to pregnant minority women and a community based approach to raising vaccine coverage and awareness among this at-risk population.
Message framing
Developed by psychologist Daniel Kahneman,28,29 and backed by Prospect Theory,30,31 message framing has been proposed as a critical component of health behavioral change. Gain-framed messaging puts forth information by explaining the benefits of engaging in a health behavior, while loss-framed messages tell of the possible costs or risks of not engaging in the behavior.32 It has been found that gain-framed messages are most persuasive when they are advocating for behavior that prevents the onset of a health problem (e.g., immunization), while loss-framed messages are most persuasive when advocating for a behavior that detects a health problem (e.g., getting a Pap smear).32-36 Prospect Theory for risk communication is useful for understanding the confluent factors shaping vaccine decision-making for women and their babies.
To our knowledge message framing has not been systematically evaluated on maternal and infant immunization outcomes, particularly among minority women. Our study endeavored to test messages that would either articulate maternal-infant benefits associated with immunization (gain-frame) or illustrate negative consequences of foregoing immunization (loss-frame), and evaluate their effect on intent to immunize infants against seasonal influenza.37-39 Based on previous research, we hypothesized that gain-framed messages would be more effective in persuading women to vaccinate.32-36 We also sought to understand whether exposure to a popular film, “Contagion,” would influence the perceptions women had of the presented messages. The film depicts a pandemic situation caused by the introduction and rapid transmission of a novel virus and the efforts to find a vaccine. The recent 2009 H1N1 epidemics informed the plot for the film, which received praise for its scientific and public health accuracy.40,41 Understanding how messages shape intention to vaccinate, and how cultural influences shape perceptions toward messages, offers guidance on the development of community-level interventions to increase maternal and pediatric vaccination rates among highly vulnerable populations.
Materials and Methods
Formative research
Our team conducted 20–30 min semi-structured interviews with 21 pregnant Black/African American and Hispanic women ($20 compensation/subject) at clinics throughout Atlanta. Data was collected until saturation was achieved on emergent themes that informed the development of two intervention message types. The interviews generated ideas on language, images, and other message design aspects to guide graphic design concept development. We then presented the concepts to a subset of the women we initially interviewed to gather their rank order preference on the gain and loss frame messages for testing. For this study, we determined that all women, including those in the control condition, would see standard language from the Centers for Disease and Control (CDC) vaccine information fact sheet on the first page of their questionnaire:
“Information about the Flu Shot
Although pregnant women are about 1% of the U.S. population, they made up 5% of U.S. deaths from 2009 H1N1 (swine flu) reported to the Centers for Disease Control (CDC) from April 14–August 21, 2009. According to a study done during the first month of the outbreak, the rate of hospitalizations for 2009 H1N1 was four times higher in pregnant women than other groups.
Seasonal flu shots have been given safely to millions of pregnant women over many years. As in previous years, vaccine companies are making plenty of preservative-free flu vaccine as an option for pregnant women and small children. The flu shot (not the nasal spray) is safe for pregnant women during any trimester. Nursing mothers can receive a flu shot or the nasal spray. One shot will last all flu season, even if you get it early in the season.”
Our formative research suggested that the resulting gain-framed message should include approximately four lines of factual information about influenza vaccination with a background visual depiction of a smiling pregnant woman. The loss-framed message included four lines of text emphasizing the risks of not protecting oneself and the unborn child(ren) from influenza, with a background visual of an ambulance and stretcher. (Figs. 1 and 2)

Figure 1. Gain-framed message presented to a subset of women upon enrollment.
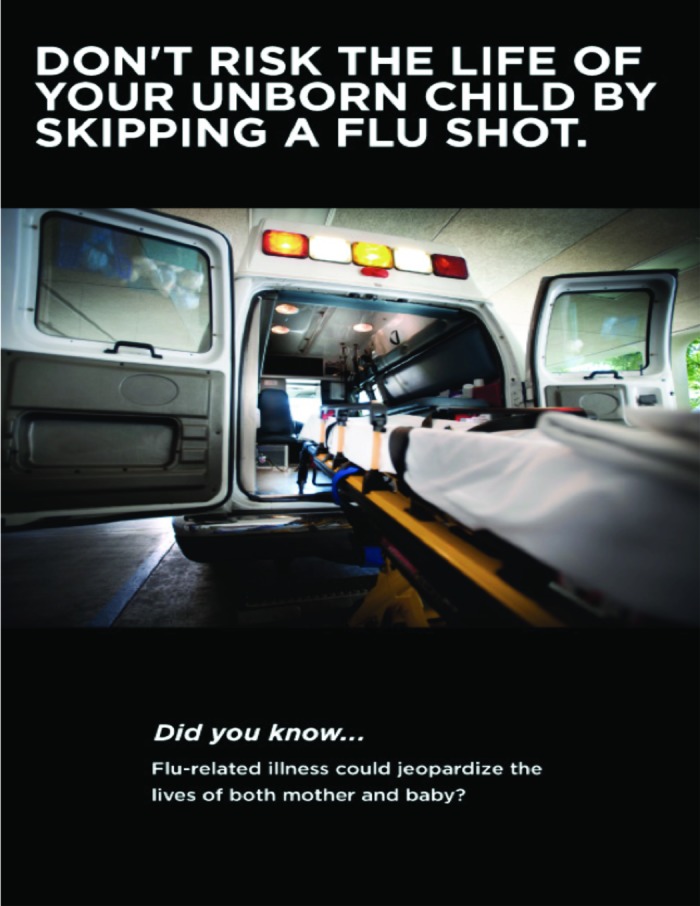
Figure 2. Loss-framed message presented to a subset of women upon enrollment.
Study design and sample
Cohort recruitment began at the inception of influenza season in September 2011 and concluded in May 2012. The study protocol was approved by the Emory University Institutional Review Board. The persons eligible for this study included women ages 18–50, who self-identified as Black/African American, Hispanic/Latina, or “Other/Multicultural” who could read and write English and/or Spanish, and who were able to provide written informed consent. In order to determine predictors of seasonal influenza immunization among pregnant women, only women who had not yet received the 2011–2012 seasonal influenza or Tdap vaccine were included in the study. Project staff conducted sampling in a variety of venues including clinics, parks, community meetings, churches, and other locations that gave permission for recruitment and study activities at various times and days of the week.
Women were asked if they were interested in participating in a survey about maternal influenza. Bilingual staff members completed a screening checklist with each participant that confirmed pregnancy status and expected due date. The staff member read through the informed consent, asked if the participant had any questions, and then had the participant sign and date the consent. Women were immediately assigned to one of three randomly selected conditions: gain, loss, or control. The surveys were conducted in semi-private or private locations offered by venue owners. Those who met the eligibility criteria and agreed to participate (n = 261) were interviewed that day and were compensated $20 for time and inconvenience. All participants were pregnant at the time of the interview.
Measurement
Study materials were developed in English and Spanish. Bilingual community members reviewed these documents to ensure their adequate readability and item comprehension prior to administration. The survey included 82 items, which were informed by the Integrated Behavioral model, formative interviews with community members, and prior behavioral research on influenza immunization among minority communities.11,12,59 Key behavioral assessments included history of seasonal influenza immunization, willingness to pay for vaccine, and intention to immunize infant. We determined that the Flesch-Kincaid reading score of 7.4 of the final survey in either language met the acceptable criteria of 6–8th grade reading level for our target population.60,61
Assessment of intent
Intent to immunize infants was assessed by a single item: “On a scale of 0 (definitely will not) to 10 (definitely will), please rank the likelihood you will vaccinate your new baby for the flu after he/she turns 6 months old.” Because our primary aim was to assess vaccination intention, we subsequently performed a median split procedure resulting in a dichotomized variable that allowed us to evaluate those “willing,” and “not willing” to vaccinate their baby after six months of age.
Assessment of demographic and behavioral correlates
Initial survey questions assessed sociodemographic measures (i.e., age, race/ethnicity, education, healthcare utilization, employment status). Furthermore, key behavioral assessments were completed. For example, using a 12-mo recall period, we asked about immunization history (other than seasonal or pandemic influenza) for illnesses such as tetanus, diphtheria, pertussis (Tdap) or others recommended by a healthcare provider (e.g., Hepatitis B). We also assessed healthcare seeking motivation and willingness-to-pay for influenza vaccination (i.e., $0/free to ≥ $30) using a 5-point scale.
In addition to the selected demographic and behavioral correlates, the questionnaire included items designed to measure psychosocial indicators of immunization intent (Table 1). A normative support scale inclusive of three items was developed based on previous quantitative and qualitative research findings, literature review, and vaccine clinical trial and community experience.62-65 We incorporated guidance from progenitors of the Integrated Behavioral Model to construct the items.66-68 A team of clinicians and behavioral researchers reviewed the instrument for adequacy of the measures. Each scale item was measured by a 5-point Likert scale (1-strongly disagree to 5-strongly agree), designed to assign meaningful values to an underlying continuum of ratings.69 Given the extent of evidence suggesting the importance of normative approval in vaccine decision-making,63,65,70 the items specifically assessed the perceived approval of doctors, work colleagues, family, and friends in deciding to vaccinate infants after six months of age (Cronbach’s α = 0.771).
Table 1. Questionnaire Items for maternal Intent to Immunize Infants.
| Survey item | Response choices |
|---|---|
| 1. On a scale of 0 (definitely will not) to 10 (definitely will), please rank the likelihood of you will vaccinate your new baby for the flu after he/she turns 6 mo old? | Continuous Scale: 0 = Definitely Will Not to 10 = Definitely Will |
| 2. In the past 12 mo, did you get sick with the flu? | 1 = Yes 2 = No 3 = Don’t Know |
| 3. In the past year, did anyone living with you acquire the flu? | 1 = Yes 2 = No 3 = Don’t Know 4 = Not applicable/I live alone |
| 4. In the past five years, how often have you receive a seasonal flu shot? | 1 = 5 times (e.g., every year: 2006, 2007, 2008, 2009, 2010) 2 = 2–4 times 3 = 1 time 4 = 0 times 5 = Don’t know |
| 5. Did you receive a flu shot this past flu season, last fall/winter (seasonal flu shot, H1N1, or both)? | 1 = Yes 2 = No |
| 6. What is the most you are willing to pay for your next flu shot? | 1 = $0/free/will not pay for shot 2 = Up to $5 3 = Up to $10 4 = Up to $20 5 = Up to $30 6 = $31 or more 7 = Don’t know |
| 7. Please indicate how protective you think the flu vaccine will be for a pregnant woman? | 0% = Not Protective 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% = Completely Protective |
| 8. I would worry that getting the flu shot would give me the flu. | 1 = Strongly Agree 2 = Agree 3 = Neutral/not sure 4 = Disagree 5 = Strongly disagree |
| 9.I would be less likely to get a flu vaccine if it had any minor side effects such as fatigue or fever. | 1 = Strongly Agree 2 = Agree 3 = Neutral/not sure 4 = Disagree 5 = Strongly disagree |
| 10. On a scale of 0 (definitely not) to 10 (definitely so), please rank your likelihood of getting a flu shot during your pregnancy: | Continuous scale: 0 = Definitely Not, to 10 = Definitely so |
| 11. On a scale of 0 (definitely not) to 10 (definitely so), please rank how likely it is that you could get the flu while pregnant? | Continuous scale: 0 = Definitely Not, to 10 = Definitely so |
| 12. How serious do you think it would be if you got flu while pregnant? | 1 = Not at all serious 2 = Not very serious 3 = Somewhat serious 4 = Serious 5 = Very serious 6 = Extremely serious 7 = Don’t know |
| 13. How serious do you think it would be if your unborn child got the flu? | 1 = Not at all serious 2 = Not very serious 3 = Somewhat serious 4 = Serious 5 = Very serious 6 = Extremely serious 7 = Don’t know |
| 14. What is your date of birth? | MM/DD/YYYY |
| 15. What is the highest level of school that you have completed? | 1 = K-8 grade 2 = 9–11 grade 3 = High school graduation/GED 4 = Technical/Vocational or Associates 5 = Bachelor degree 6 = Master’s degree 7 = Doctorate |
| 16. How would you describe your ethnic background? | 1 = African American/ Black 2 = Hispanic/ Latino/ Chicano 3 = Caucasian/ White 4 = Other. Please Specify. |
| 17. What is your relationship status? | 1 = Single/never married 2 = Married/ Domestic Partner 3 = Divorced/ Separated 4 = Widowed 5 = Other. Please Specify. |
| 18. Which of the following best describes your employment status? | 1 = Employed—full time 2 = Employed—Part-time 3 = Unemployed 4 = Other. Please Specify. |
| 19. What is your annual household income (i.e., combined income of all members of your family)? | 1 = Less than $20,000 2 = $20,001 -$40,000 3 = $40,001 -$60,000 4 = $60,001 -$80,000 5 = $80,001 -$100,000 6 = More than $100,001 |
| Message Resonance | |
| 20. Have you seen the movie “Contagion”? | 1 = Yes 2 = No |
| 21. “This ad is very appealing to me.” | 1 = Strongly Agree 2 = Agree 3 = Neutral/Not Sure 4 = Disagree 5 = Strongly Disagree |
| 22. “This ad is easy to remember.” | 1 = Strongly Agree 2 = Agree 3 = Neutral/Not Sure 4 = Disagree 5 = Strongly Disagree |
| 23. “This ad is new and fresh.” | 1 = Strongly Agree 2 = Agree 3 = Neutral/Not Sure 4 = Disagree 5 = Strongly Disagree |
Statistical analyses
We performed descriptive analyses and conducted t-tests and cross-tabulations to evaluate characteristic differences observed among enrolled arms. In addition to these univariate and bivariate analyses, we used a multiple logistic regression model to evaluate the association between predictor variables (gain-frame/loss-frame/control message) and the outcome variable (intent to immunize infants against influenza after six months of age), accounting for the influence of confounding. We also constructed three multiple logistic regression models in order to assess between-group comparison (i.e., gain frame vs. control, loss frame vs. control, and gain frame vs. loss frame). For each paired-group comparison, we ran a multivariate logistic regression that assessed the relationship between the study group and our primary outcome variable intention to immunize infant (adjusted for confounders). This allowed us to analyze potential variations between intervention arms in the association between predictor variables and intent to immunize.
Both statistical models accounted for potential confounding. Confounding variables were selected based on the relationship between outcome and exposure variables. If any of the related variables changed the influence of different messages on vaccine intention by at least 10%, we considered these to be confounders and included the items in the final model. We also assessed the potential for multicollinearity using a condition index of 20 and a VDP level of 0.5 when full model was determined.71,72 Our rigorous testing indicated that no collinearity was found in the model.73
Finally, we evaluated associations among those who reported that they saw the film “Contagion” and their message framing perceptions and outcome. We therefore developed questions to determine whether pregnant women who saw the film and were subsequently exposed to gain- or loss-frame messages found them to be appealing, memorable, and novel or found them to be disinteresting. Such effects are important primers of attention toward messages and are important indicators of whether high vs. low elaboration on messages is likely to result from cultural cues to action.74-76
Results
Approximately six hundred women were approached across metropolitan Atlanta, of which two-thirds were ineligible for enrollment based on preset criteria such as age, ability to read and write English and/or Spanish, and previous receipt of the seasonal influenza vaccine during the current pregnancy occurring between September 2011 and May 2012. Following screening and consent of the eligible women, 261 women were enrolled in the final study. Of these, 87 were assigned to the gain-frame condition and 90 to the loss-frame group. The control group comprised 84 women. The majority (88.5%, n = 230) of the study population included Black/African American women; 7.3% were Hispanic/Latina (n = 19) and 4.2% were Other/Multicultural women (n = 11) (Table 2). The mean age of the participants was 25.8 y. The majority of participants lived in lower-income households with total family earnings of ≤ $20 000 per year (69.2%, n = 171). Fifty-five percent (n = 144) of the women indicated that they were unemployed and 51.9% (n = 135) achieved high school or equivalent education. Seventy-two percent (n = 190) indicated that they were single or never married.
Table 2. Participant sociodemographic characteristics (n = 261).
| Characteristic | Frequency | Participant Subgroup Assignments | |||
|---|---|---|---|---|---|
| Control (n = 84, 32.18%) |
Gain (n = 87, 33.33%) |
Loss (n = 90, 34.48%) |
P-value | ||
| Age (Mean = 25.83, Missing = 6) | 0.45 | ||||
| 18–25 | 140 (54.90%) | 43(52.44%) | 46 (53.49%) | 51(58.62%) | |
| 26–35 | 96 (37.65%) | 35(42.68%) | 34 (39.53%) | 27(31.03%) | |
| 36–45 | 19 (7.45%) | 4(4.88%) | 6 (6.98%) | 9(10.34%) | |
|
Educational Attainment
(Missing = 1) |
0.73 | ||||
| Less than High School | 47 (18.08%) | 15 (18.07%) | 19 (21.84%) | 13 (14.44%) | |
| High School of Less | 135 (51.92%) | 43 (51.81%) | 45 (51.72%) | 47 (52.22%) | |
| More than High School | 78 (30.00%) | 25 (30.12%) | 23 (26.44%) | 30 (33.33%) | |
| Racial/Ethnic Background | 0.40 | ||||
| African American/Black | 230 (88.46%) | 75(89.29%) | 79 (90.80%) | 76(84.44%) | |
| Hispanic / Latina | 19 (7.31%) | 5 (5.95%) | 6 (6.98%) | 8 (8.89%) | |
| Other/Multicultural | 11 (4.23%) | 4 (4.76%) | 1 (1.16%) | 6 (6.67%) | |
| Employment Status | 0.95 | ||||
| Employed | 101 (38.84%) | 30 (35.71) | 36 (41.38) | 35 (38.89%) | |
| Unemployed | 144 (55.38%) | 48(57.14%) | 46 (52.87%) | 50(55.56%) | |
| Other | 15 (5.77%) | 6 (7.14%) | 5 (5.75%) | 5(5.56%) | |
| Annual Household Income (Missing = 14) | 0.78 | ||||
| ≤ $20 000 | 171 (69.23%) | 57(72.15%) | 57 (71.25%) | 57(64.77%) | |
| $20 001–$40 000 | 41 (16.60%) | 11(13.92%) | 13 (16.25%) | 17(19.32%) | |
| $40 001–$80 000 | 27 (10.93%) | 10 (4.05) | 7 (8.75%) | 10 (11.36%) | |
| ≥ $80 000 | 8 (3.24%) | 1(1.27%) | 3 (3.75%) | 4 (4.55%) | |
| Relationship Status | 0.02 | ||||
| Single/Never Married | 190 (72.80%) | 62(73.81%) | 64 (73.56%) | 64(71.11%) | |
| Married/Domestic Partner | 51 (19.54%) | 18(21.43%) | 19 (21.84%) | 14(15.56%) | |
| Divorced/Separated | 8 (3.07%) | 0(0%) | 0 (0%) | 8(8.89%) | |
| Widowed | 1 (0.38.%) | 1(1.19%) | 0 (0%) | 0(0%) | |
| Other | 11 (4.21%) | 3(3.57%) | 4 (4.6%) | 4(4.44%) | |
There were no significant sociodemographic differences between the intervention groups, with the exception of relationship status. Fewer married participants or participants with domestic partners were in the loss-frame group.
Message framing outcomes
Nearly half of the respondents indicated that they intended to vaccinate their new infant after 6 mo of age (50.2%, n = 131). Compared with the controls both gain-framed messages [OR = 2.13, 90% CI: (1.120, 4.048)] and loss-framed messages [OR = 2.02, 90% CI: (1.083, 3.787)] were significantly associated with intention to vaccinate their infants. The goodness of fit indicate the model was a reasonable fit [p = 0.66]. The coefficients and corresponding confidence intervals for the full logistical model are included in Table 3.
Table 3. Factors associated with Infant Influenza Immunization (n = 261)a.
| Adjusted OR | 90%CI | |
|---|---|---|
| Exposure of Interest | ||
| Gain | 2.130 | (1.120, 4.048) |
| Loss | 2.025 | (1.083, 3.787) |
| Control | Referent | |
| Multivariate Factorsb | ||
| Maternal Vaccination Intention | ||
| Likely | 10.830 | (4.923, 23.825) |
| Not likely | Referent | |
| Race/Ethnicity | ||
| African American/ Black | 0.852 | (0.369, 1.966) |
| Hispanic/Other/Multicultural | Referent | |
| Perceived Influenza Susceptibility | ||
| Vulnerable | 2.702 | (1.566, 4.662) |
| Not vulnerable | Referent |
a Odds Ratio in BOLD indicates significance. bThe following covariates were also included in the final multivariate model—presence of health insurance, influenza illness within the past 12 mo, concern about potential vaccine side effects, perceived influenza severity for mother, perceived influenza severity for unborn child, and perceived vaccine efficacy. These variables were insignificant in the model, and therefore not included in the above table.
In the multivariate logistic regression models for paired comparisons between study groups (Model 1: gain- vs. loss-frame; Model 2: gain-frame vs. control; Model 3: loss-frame vs. control) intention to immunize infants was significantly higher among women exposed to gain-framed messages, compared with those exposed to control messages [OR = 2.20, 90% CI: (1.131, 4.302)] (Model 2). In contrast, exposure to loss-framed messages was not significantly associated with intention to vaccinate infants, when compared with women exposed to gain-framed messaged (Model 1) and when compared with women exposed to the control message (Model 3). Women who intended to obtain influenza vaccine during pregnancy were more likely to express intent to immunize infants; this effect was seen across all three paired group models [Model 1: OR = 5.55, 90% CI: (2.048, 15.058); Model 2: OR = 13.40, 90% CI: (4.699, 38.215)]; Model 3: [OR = 7.45, 90% CI: (2.676, 20.753)].
Perceived severity of influenza was also a strong predictor of intention to immunize infants. Women who perceived the illness as very serious were more likely to express the intent to immunize infants, as demonstrated in Model 1 [OR = 5.90, 90% CI: (1.171, 29.782)] and Model 2 [OR = 4.85, 90% CI: (1.345, 17.504)]. Mothers who perceived that they were susceptible to becoming ill with influenza during pregnancy also demonstrated greater intent to immunize infants against seasonal influenza as shown in model 1 [OR = 2.71, 90% CI: (1.315, 5.569)] and model 3 [OR = 2.90, 90% CI: (1.478, 5.705)]. The coefficients and corresponding confidence intervals for the multivariate logistic regression models for paired groups are listed in Table 4.
Table 4. Factors associated with infant influenza immunization by exposure (n = 261)a .
| MODEL1: GAIN v. LOSS n = 177 |
MODEL 2: GAIN v. CONTROL n = 171 |
MODEL 3: LOSS v. CONTROL n = 174 |
||||
|---|---|---|---|---|---|---|
| aOR | 90% CI | aOR | 90% CI | aOR | 90% CI | |
| Exposure of Interest | ||||||
| Gain | 1.316 | (0.697, 2.483) | 2.206 | (1.131, 4.302) | N/A | N/A |
| Loss | Referent | N/A | N/A | 1.780 | (0.925, 3.427) | |
| Control | N/A | N/A | Referent | Referent | ||
| Multivariate Factorsb | ||||||
| Maternal Vaccination Intention | ||||||
| Likely | 5.554 | (2.048, 15.058) | 13.401 | (4.699, 38.215) | 7.452 | (2.676, 20.753) |
| Not likely | Referent | Referent | Referent | |||
| Race/Ethnicity | ||||||
| African American/Black | 0.754 | (0.280, 2.208) | 1.198 | (0.335, 4.288) | 0.638 | (0.241, 1.689) |
| Hispanic/Other/Multicultural | Referent | Referent | Referent | |||
| Perceived Influenza Susceptibility | ||||||
| Vulnerable | 2.706 | (1.315, 5.569) | 2.019 | (0.945, 4.313) | 2.904 | (1.478, 5.705) |
| Not vulnerable | Referent | Referent | Referent | |||
| Perceived Influenza Severity | ||||||
| Serious | 5.904 | (1.171, 29.782) | 4.852 | (1.345, 17.504) | 1.139 | (0.312, 4.160) |
| Not serious | 1.520 | (0.148, 15.639) | 1.018 | (0.153, 6.763) | 0.631 | (0.093, 4.273) |
| Unsure/Don't know | Referent | Referent | Referent | |||
| Normative Support | 1.823 | (0.887, 3.747) | 1.123 | (0.582, 2.387) | 1.841 | (0.956, 3.546) |
a Odds Ratio in BOLD indicate significance. bThe following covariates were also included for each logistic regression model in the paired group analysis—presence of health insurance, influenza illness within the past 12 mo, concern about potential vaccine side effects, perceived influenza severity for mother, perceived influenza severity for unborn child, and perceived vaccine efficacy. These variables were insignificant in the models, and therefore not included in the above table.
Healthcare experience and psychosocial indicators of maternal immunization
Women who expressed the intent to immunize themselves against seasonal influenza during pregnancy were 10 times more likely express intent to vaccinate infants against seasonal influenza, compared with those who did not intend to immunize against seasonal influenza during pregnancy [OR = 10.83, 90%CI: (4.923, 23.825)]. Additionally, respondents expressed that they were more likely to vaccinate their infants if they perceived higher susceptibility of getting the flu during pregnancy [OR = 2.70, 90% CI: (1.566, 4.662)].
Race was not a significant contributing factor in maternal intent to immunize infants, which was the primary outcome for our final multivariate model. In addition to controlling for race and ethnicity, we also conducted bivariate analyses to assess the relationship between intention to immunize an infant and potential psychosocial indicators of interest. These indicators included perceived severity of influenza during pregnancy, perceived or anticipated side effects associated with influenza, myths and misperceptions (i.e., getting influenza from the vaccine), cost concerns, healthcare seeking behavior, and perceived potential for household transmission. Data for these variables is not shown as the results were insignificant in the analyses and therefore not included in the final multivariate logistic regression model.
Message framing and “contagion” effects
“Contagion” opened in US cinemas at the inception of our study (September 2011). Fifty-four (20.7%) of the total study participants viewed the movie (x2 = 5.87, p = 0.06). Women who saw the movie were more likely to have health insurance (x2 = 7.30, p = 0.03), compared with those who had not viewed the movie. A direct relationship was not observed between having seen the film and the outcome (x2 = 5.75, p = 0.363). However this effect is likely mediated through attitudes that form the basis of perceptions and subsequent intentions.42,43 Evidence for such a pathway is seen in the higher proportion of those who considered the gain- and loss-frame messages more appealing (x2 = 6.03, p = 0.05), easy to remember (x2 = 16.33, p = 0.0003), and novel (new and fresh) (x2 = 6.24, p = 0.03) compared with a lower proportion among those who did not see the film and yet were exposed to the same messages. Moreover, we found that among audience members assigned to gain- and loss-arms, there were fewer who were tired of the type of messages presented by either gain- or loss-frame strategy (x2 = 9.31, p = 0.01) or agreed that the message “left them cold” (x2 = 6.23, p = 0.04) compared with those who did not see the film but were exposed to the very same messages.
Discussion
This study adds to the literature on the importance of message framing to maternal intent to immunize infants.33,44,45 In our study, both gain- and loss-frame messages were positively associated with greater intention to vaccinate, compared with control messages. These findings are among the first to demonstrate that for pregnant minority women, well-designed communication messages are more likely than the standard of care to improve intention to immunize infants. As previous research with minority women has demonstrated, inherent in vaccine decision-making is distrust of information sources, particularly if immunization messages are disseminated by the government.12 Our results indicate that for minority women, a community-developed approach to vaccine messaging based on formative research with the target population, is a promising approach to the promotion of vaccine acceptance and cultivating maternal intent to immunize infants. By utilizing “culture-centered” forms of communication with messages created by community members, source distrust may be effectively overcome.46,47 For example, recent research suggests that interventions promoting vaccine communication among minority women’s social networks will alter perceptions of HPV immunization effectiveness.48
The results of this study demonstrate some inconsistencies with Prospect Theory and previous message framing studies.33,44,45,49 We hypothesized that gain-frame messages would have a larger influence than loss-frame messages on intention to engage in prevention behavior (immunization of infants). However, results of our primary model showed that, when compared with the control message, gain- and loss-frame messages have similar effects on maternal intent to immunize. This effect is in line with previous studies with minority women that have demonstrated the critical importance of tailored communication to enhance message relevance and cognitive processing over standardized communication.50
Furthermore, results of our paired-groups comparison model indicated no significant difference in intention to vaccinate when comparing gain- to loss-frame messages. In one study of framing effects on measles, mumps and rubella (MMR) vaccine, loss-framed vaccine messages were more effective than gain-framed messages in promoting MMR immunization51 Other studies indicate that use of gain-framed messages among low-income minority women are effective in promoting preventive behaviors such as testing or screening for cervical cancer,52,53 which may be qualitatively different from immunization behavior and intent. Similarly, a meta-analysis of health message framing effects indicates that message framing may have the weakest direct effect on immunization, compared with all other preventive behaviors.33 Factors such as perceived disease susceptibility, vaccine safety concerns, and media coverage should be considered in tandem with Prospect Theory when considering gain- vs. loss-framed message effects.
Promoting immunization among women during pregnancy and childbearing years sets forth a positive trajectory for subsequent immunization of children, who quickly become vulnerable once maternal antibodies decline in the six months following birth. Our study offers evidence that the delivery of well-crafted messages during pregnancy is likely to achieve important behavioral effects.54,55 Our data indicate that the intention of a pregnant woman to vaccinate herself against influenza during pregnancy corresponds with a 10-fold increase of intention to immunize her infant. This suggests that vaccine acceptance among pregnant minority women is positively correlated with maternal intent to vaccinate infants following pregnancy. Promoting vaccine acceptance during pregnancy, using well-crafted communication messages, is likely to promote infant immunization after pregnancy. Based on these results, we argue that vaccination messages need to be incorporated in provider visits as a standard of care.
The role of motion pictures in shaping attitudes and promoting message resonance and recall is also highlighted in this study. Previous studies have demonstrated the impact of film on attitudes toward health issues.56 Women in our study who had seen the movie “Contagion” found our messages easier to remember and more appealing. This suggests affective engagement with the film’s content, particularly as it highlighted the impact of viral transmission on families and communities and likely resonated with this audience segment. Influenza vaccination campaigns have targeted audiences in cinemas as an opportunity for social learning for adults with children 6 mo to 2 y of age in the US.57 Exposure to messages in this format has greater potential to promote immunization through affective engagement with tailored messages and relevant storylines.58 A previous study conducted in San Diego identified improved recall of influenza vaccination messages when presented on cinema screens (24%).57 The involvement of mass media, including entertainment, movie advertising, and public service announcements (PSAs) could potentially enhance recall of well-designed messages among pregnant women.57
Limitations
There are some limitations to this study. Venue-based sampling of minority women from one southeastern city was used, which may not be representative of other cities in the United States. Additionally, we acknowledge the potential for selection bias as women who were agreeable to participating in the study were included and therefore may not be representative of the actual population of pregnant Black/African American, Hispanic/Latina, and women from multicultural backgrounds. Women who choose to participate in our study may be more likely to accept vaccines or have a history of immunization. Finally, our study utilized a cross-sectional sample. Multiple exposures to the same messages are associated with differentiation of behavioral effects over time. It is therefore possible that a stronger differentiation of effect would be temporally observed with multiple message exposures.
Conclusions
Effective maternal immunization messages can contribute to successful, practical, and cost-effective interventions to increase pediatric immunization acceptance among highly vulnerable populations. Our findings present compelling evidence that women exposed to health message framing are more likely to express intention to immunize their infants, compared with those who receive the standard vaccine information sheets. We observed that maternal history of seasonal influenza immunization is positively associated with increased intention to vaccinate infants, providing evidence that improving immunization among women during childbearing years may subsequently improve pediatric influenza vaccine coverage in minority communities. Finally, both gain- and loss-frame message resonance was intensified among those who saw the film “Contagion.” Our findings present compelling evidence for improving maternal influenza immunization and delivering community-based, well-crafted vaccine messages during pregnancy to improve pediatric influenza vaccine coverage in minority communities.
Author Disclosure Statement
No competing financial interests exist.
Sources of Support
This study was partially supported by a Kaiser Permanente Georgia community benefits grant and a grant from the Centers for Disease Control and Prevention (CDC), grant 5P01TP000300 to the Emory Preparedness and Emergency Response Research Center, Emory University (Atlanta, Georgia).
Acknowledgments
This study was partially supported by a Kaiser Permanente Georgia community benefits grant and a grant from the Centers for Disease Control and Prevention (CDC), grant 5P01TP000300 to the Emory Preparedness and Emergency Response Research Center, Emory University (Atlanta, Georgia). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC. The authors would like to offer our gratitude to Drs. Ruth Berkelman, Vicki Freimuth, and Robert Davis, and to Ms. Ellen Whitney for their support and guidance throughout this study. Special thanks to Mr Rick Kern, MixIt Marketing, for development of message concepts tested in this study.
References
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, Fukuda K. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 3.Ahluwalia IB, Jamieson DJ, Rasmussen SA, D’Angelo D, Goodman D, Kim H. Correlates of seasonal influenza vaccine coverage among pregnant women in Georgia and Rhode Island. Obstet Gynecol. 2010;116:949–55. doi: 10.1097/AOG.0b013e3181f1039f. [DOI] [PubMed] [Google Scholar]
- 4.Creanga AA, Kamimoto L, Newsome K, D’Mello T, Jamieson DJ, Zotti ME, Arnold KE, Baumbach J, Bennett NM, Farley MM, et al. Seasonal and 2009 pandemic influenza A (H1N1) virus infection during pregnancy: a population-based study of hospitalized cases. Am J Obstet Gynecol. 2011;204(Suppl 1):S38–45. doi: 10.1016/j.ajog.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 5.Beigi RH, Wiringa AE, Bailey RR, Assi TM, Lee BY. Economic value of seasonal and pandemic influenza vaccination during pregnancy. Clin Infect Dis. 2009;49:1784–92. doi: 10.1086/649013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moro PL, Tepper NK, Grohskopf LA, Vellozzi C, Broder K. Safety of seasonal influenza and influenza A (H1N1) 2009 monovalent vaccines in pregnancy. Expert Rev Vaccines. 2012;11:911–21. doi: 10.1586/erv.12.72. [DOI] [PubMed] [Google Scholar]
- 7.Bednarczyk RA, Adjaye-Gbewonyo D, Omer SB. Safety of influenza immunization during pregnancy for the fetus and the neonate. Am J Obstet Gynecol. 2012;207(Suppl):S38–46. doi: 10.1016/j.ajog.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, Ramakrishnan U. Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: a retrospective cohort study. PLoS Med. 2011;8:e1000441. doi: 10.1371/journal.pmed.1000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Pregnant Women and Flu Shots. 2011.
- 10.Setse RW, Euler GL, Gonzalez-Feliciano AG, Bryan LN, Furlow C, Weinbaum CM, Singleton JA, Centers for Disease Control and Prevention (CDC) Influenza vaccination coverage - United States, 2000-2010. MMWR Surveill Summ. 2011;60(Suppl):38–41. [PubMed] [Google Scholar]
- 11.Frew PM, Painter JE, Hixson B, Kulb C, Moore K, del Rio C, Esteves-Jaramillo A, Omer SB. Factors mediating seasonal and influenza A (H1N1) vaccine acceptance among ethnically diverse populations in the urban south. Vaccine. 2012;30:4200–8. doi: 10.1016/j.vaccine.2012.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frew PM, Hixson B, del Rio C, Esteves-Jaramillo A, Omer SB. Acceptance of pandemic 2009 influenza A (H1N1) vaccine in a minority population: determinants and potential points of intervention. Pediatrics. 2011;127(Suppl 1):S113–9. doi: 10.1542/peds.2010-1722Q. [DOI] [PubMed] [Google Scholar]
- 13.Wong KY, Do YK. Are there socioeconomic disparities in women having discussions on human papillomavirus vaccine with health care providers? BMC Womens Health. 2012;12:33. doi: 10.1186/1472-6874-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Maternal and infant outcomes among severely ill pregnant and postpartum women with 2009 pandemic influenza A (H1N1)--United States, April 2009-August 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1193–6. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. 2009 H1N1 and Seasonal Influenza and Hispanic Communities: Questions and Answers. 2010; February 16, 2010:http://www.cdc.gov/h1n1flu/qa_hispanic.htm
- 16.Georgia Department of Health. Annual Vaccine Preventable Diseases Surveillance Report - Georgia, 2010. 2010; http://health.state.ga.us/pdfs/epi/vpd/2010%20VPD%20Report.pdf
- 17.Louie JK, Acosta M, Jamieson DJ, Honein MA, California Pandemic (H1N1) Working Group Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362:27–35. doi: 10.1056/NEJMoa0910444. [DOI] [PubMed] [Google Scholar]
- 18.Ahluwalia IB, Singleton JA, Jamieson DJ, Rasmussen SA, Harrison L. Seasonal influenza vaccine coverage among pregnant women: pregnancy risk assessment monitoring system. J Womens Health (Larchmt) 2011;20:649–51. doi: 10.1089/jwh.2011.2794. [DOI] [PubMed] [Google Scholar]
- 19.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Neuzil KM, Reed GW, Mitchel EF, Simonsen L, Griffin MR. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol. 1998;148:1094–102. doi: 10.1093/oxfordjournals.aje.a009587. [DOI] [PubMed] [Google Scholar]
- 21.Tucker Edmonds BM, Coleman J, Armstrong K, Shea JA. Risk perceptions, worry, or distrust: what drives pregnant women’s decisions to accept the H1N1 vaccine? Matern Child Health J. 2011;15:1203–9. doi: 10.1007/s10995-010-0693-5. [DOI] [PubMed] [Google Scholar]
- 22.Groseclose SL, Brathwaite WS, Hall PA, Connor FJ, Sharp P, Anderson WJ, Fagan RF, Aponte JJ, Jones GF, Nitschke DA, et al. Centers for Disease Control and Prevention (CDC) Summary of notifiable diseases--United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;51:1–84. [PubMed] [Google Scholar]
- 23.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. 2003;52:1–113. [PubMed] [Google Scholar]
- 24.Prevention CfDCa. Influenza Vaccination Coverage Among Pregnant Women—United States, 2010-11 Influenza Season. 2010.
- 25.Read JS, Riley L. Progress in overcoming barriers to influenza immunization of pregnant women. Am J Obstet Gynecol. 2012;207(Suppl):S1–2. doi: 10.1016/j.ajog.2012.06.067. [DOI] [PubMed] [Google Scholar]
- 26.Flowers L, Sinclair S, AARP Public Policy Institute Racial and ethnic disparities in influenza and pneumococcal immunization rates among Medicare beneficiaries. Project Report. 2007 [PubMed] [Google Scholar]
- 27.Logan JL. Disparities in influenza immunization among US adults. J Natl Med Assoc. 2009;101:161–6. doi: 10.1016/s0027-9684(15)30830-0. [DOI] [PubMed] [Google Scholar]
- 28.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–8. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 29.Kahneman D, Tversky A. Prospect Theory - Analysis of Decision under Risk. Econometrica. 1979;47:263–91. doi: 10.2307/1914185. [DOI] [Google Scholar]
- 30.Tversky A, Kahneman D, Kahneman D. Advances in Prospect Theory: Cumulative Representation of Uncertainty. J Risk Uncertain. 1992;5:297–323. doi: 10.1007/BF00122574. [DOI] [Google Scholar]
- 31.Satia JA, Barlow J, Armstrong-Brown J, Watters JL. Qualitative study to explore Prospect Theory and message framing and diet and cancer prevention-related issues among African American adolescents. Cancer Nurs. 2010;33:102–9. doi: 10.1097/NCC.0b013e3181be5e8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartels RD, Kelly KM, Rothman AJ. Moving beyond the function of the health behaviour: the effect of message frame on behavioural decision-making. Psychol Health. 2010;25:821–38. doi: 10.1080/08870440902893708. [DOI] [PubMed] [Google Scholar]
- 33.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med. 2012;43:101–16. doi: 10.1007/s12160-011-9308-7. [DOI] [PubMed] [Google Scholar]
- 34.Jung ME, Martin Ginis KA, Phillips SM, Lordon CD. Increasing calcium intake in young women through gain-framed, targeted messages: a randomised controlled trial. Psychol Health. 2011;26:531–47. doi: 10.1080/08870441003611544. [DOI] [PubMed] [Google Scholar]
- 35.Gallagher KM, Updegraff JA, Rothman AJ, Sims L. Perceived susceptibility to breast cancer moderates the effect of gain- and loss-framed messages on use of screening mammography. Health Psychol. 2011;30:145–52. doi: 10.1037/a0022264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hull SJ. Perceived risk as a moderator of the effectiveness of framed HIV-test promotion messages among women: a randomized controlled trial. Health Psychol. 2012;31:114–21. doi: 10.1037/a0024702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Snyder LB. Health communication campaigns and their impact on behavior. J Nutr Educ Behav. 2007;39(Suppl):S32–40. doi: 10.1016/j.jneb.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Snyder LB, Hamilton MA, Mitchell EW, Kiwanuka-Tondo J, Fleming-Milici F, Proctor D. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. J Health Commun. 2004;9(Suppl 1):71–96. doi: 10.1080/10810730490271548. [DOI] [PubMed] [Google Scholar]
- 39.National Cancer Institute. Making Health Communication Programs Work. 1989.
- 40.Jabr F. Contagion doesn't skimp on science. New Scientist 2011; http://www.newscientist.com/blogs/culturelab/2011/09/contagion-doesnt-skimp-on-science.html Accessed September 15, 2011.
- 41.Offitt P. Contagion, the Movie: An Expert Medical Review. 2011; http://www.medscape.com/viewarticle/749482 Accessed September 13, 2011.
- 42.O'Keeffe DJ. Persuasion: Theory & Research. second ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 43.Petty RE, Cacioppo JT. Attitudes and persuasion: Classic and contemporary approaches. Boulder, CO: Westview Press; 1996. [Google Scholar]
- 44.Ferguson E, Gallagher L. Message framing with respect to decisions about vaccination: the roles of frame valence, frame method and perceived risk. Br J Psychol. 2007;98:667–80. doi: 10.1348/000712607X190692. [DOI] [PubMed] [Google Scholar]
- 45.Gallagher KM, Updegraff JA. Erratum to: Health Message Framing Effects on Attitudes, Intentions, and Behaviors: A Meta-analytic Review. Ann Behav Med. 2013;46:12. doi: 10.1007/s12160-012-9446-6. [DOI] [PubMed] [Google Scholar]
- 46.Dutta-Bergman MJ. Theory and practice in health communication campaigns: a critical interrogation. Health Commun. 2005;18:103–22. doi: 10.1207/s15327027hc1802_1. [DOI] [PubMed] [Google Scholar]
- 47.Dutta-Bergman MJ. Primary sources of health information: comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004;16:273–88. doi: 10.1207/S15327027HC1603_1. [DOI] [PubMed] [Google Scholar]
- 48.Casillas A, Singhal R, Tsui J, Glenn BA, Bastani R, Mangione CM. The impact of social communication on perceived HPV vaccine effectiveness in a low-income, minority population. Ethn Dis. 2011;21:495–501. [PubMed] [Google Scholar]
- 49.Gerend MA, Shepherd MA. Message Framing, It Does a Body Good: Effects of Message Framing and Motivational Orientation on Young Women's Calcium Consumption. J Health Psychol. 2013;18:1296–306. doi: 10.1177/1359105312463587. [DOI] [PubMed] [Google Scholar]
- 50.Kreuter MW, Skinner CS, Steger-May K, Holt CL, Bucholtz DC, Clark EM, Haire-Joshu D. Responses to behaviorally vs culturally tailored cancer communication among African American women. Am J Health Behav. 2004;28:195–207. doi: 10.5993/AJHB.28.3.1. [DOI] [PubMed] [Google Scholar]
- 51.Abhyankar P, O’Connor DB, Lawton R. The role of message framing in promoting MMR vaccination: evidence of a loss-frame advantage. Psychol Health Med. 2008;13:1–16. doi: 10.1080/13548500701235732. [DOI] [PubMed] [Google Scholar]
- 52.Apanovitch AM, McCarthy D, Salovey P. Using message framing to motivate HIV testing among low-income, ethnic minority women. Health Psychol. 2003;22:60–7. doi: 10.1037/0278-6133.22.1.60. [DOI] [PubMed] [Google Scholar]
- 53.Rivers SE, Salovey P, Pizarro DA, Pizarro J, Schneider TR. Message framing and pap test utilization among women attending a community health clinic. J Health Psychol. 2005;10:65–77. doi: 10.1177/1359105305048556. [DOI] [PubMed] [Google Scholar]
- 54.Vannice KS, Salmon DA, Shui I, Omer SB, Kissner J, Edwards KM, Sparks R, Dekker CL, Klein NP, Gust DA. Attitudes and beliefs of parents concerned about vaccines: impact of timing of immunization information. Pediatrics. 2011;127(Suppl 1):S120–6. doi: 10.1542/peds.2010-1722R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Link-Gelles R, Chamberlain AT, Schulkin J, Ault K, Whitney E, Seib K, Omer SB. Missed opportunities: a national survey of obstetricians about attitudes on maternal and infant immunization. Matern Child Health J. 2012;16:1743–7. doi: 10.1007/s10995-011-0936-0. [DOI] [PubMed] [Google Scholar]
- 56.Wahl OF, Lefkowits JY. Impact of a television film on attitudes toward mental illness. Am J Community Psychol. 1989;17:521–8. doi: 10.1007/BF00931176. [DOI] [PubMed] [Google Scholar]
- 57.Peddecord KM, Jacobson IG, Engelberg M, Kwizera L, Macias V, Gustafson KW. Can movie theater advertisements promote health behaviors? Evaluation of a flu vaccination pilot campaign. J Health Commun. 2008;13:596–613. doi: 10.1080/10810730802285149. [DOI] [PubMed] [Google Scholar]
- 58.Flynn BS, Worden JK, Bunn JY, Connolly SW, Dorwaldt AL. Evaluation of smoking prevention television messages based on the elaboration likelihood model. Health Educ Res. 2011;26:976–87. doi: 10.1093/her/cyr082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frew PMAM, Archibald M, Hixson B, del Rio C. Socioecological influences on community involvement in HIV vaccine research. Vaccine. 2011;29:6136–43. doi: 10.1016/j.vaccine.2011.06.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Davis TC, Mayeaux EJ, Fredrickson D, Bocchini JA, Jr., Jackson RH, Murphy PW. Reading ability of parents compared with reading level of pediatric patient education materials. Pediatrics. 1994;93:460–8. [PubMed] [Google Scholar]
- 61.Miller B, Bodie M. Determination of reading comprehension level for effective patient health-education materials. Nurs Res. 1994;43:118–9. doi: 10.1097/00006199-199403000-00013. [DOI] [PubMed] [Google Scholar]
- 62.Hutchins SS, Fiscella K, Levine RS, Ompad DC, McDonald M. Protection of racial/ethnic minority populations during an influenza pandemic. Am J Public Health. 2009;99(Suppl 2):S261–70. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salmon DA, Moulton LH, Omer SB, Chace LM, Klassen A, Talebian P, Halsey NA. Knowledge, attitudes, and beliefs of school nurses and personnel and associations with nonmedical immunization exemptions. Pediatrics. 2004;113:e552–9. doi: 10.1542/peds.113.6.e552. [DOI] [PubMed] [Google Scholar]
- 64.Allred NJ, Shaw KM, Santibanez TA, Rickert DL, Santoli JM. Parental vaccine safety concerns: results from the National Immunization Survey, 2001-2002. Am J Prev Med. 2005;28:221–4. doi: 10.1016/j.amepre.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 65.Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118:e1287–92. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- 66.Ajzen I, Fishbein M. Understanding attitudes and predicting behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 67.Fishbein M, Ajzen I. Belief, attitude, intention, and behavior. Menlo Park, CA: Addison-Wesley; 1975. [Google Scholar]
- 68.Montano DE, Kasprzyk D. Theory of Reasoned Action, Theory of Planned Behavior, and The Integrated Behavioral Model. In: Glanz K, Rimer B, Viswanath K, eds. Health Behavior and Health Education: Theory, Research, and Practice San Francisco, CA: Jossey-Bass; 2008:67-96. [Google Scholar]
- 69.Meyers LS, Gamst G, Guarino AJ. Applied Multivariate Research: Design and Interpretation. Thousand Oaks: Sage Publications; 2006. [Google Scholar]
- 70.Shui I, Kennedy A, Wooten K, Schwartz B, Gust D. Factors influencing African-American mothers’ concerns about immunization safety: a summary of focus group findings. J Natl Med Assoc. 2005;97:657–66. [PMC free article] [PubMed] [Google Scholar]
- 71.Markovitz BP. The principle of multicollinearity. Pediatr Crit Care Med. 2005;6:94–5, author reply 94-5. doi: 10.1097/01.PCC.0000149232.77830.E0. [DOI] [PubMed] [Google Scholar]
- 72.Feher K, Whelan J, Müller S. Exploring multicollinearity using a random matrix theory approach. Stat Appl Genet Mol Biol. 2012;11:15. doi: 10.1515/1544-6115.1668. [DOI] [PubMed] [Google Scholar]
- 73.York R. Residualization is not the answer: Rethinking how to address multicollinearity. Soc Sci Res. 2012;41:1379–86. doi: 10.1016/j.ssresearch.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 74.Frew PM, Macias W, Chan K, Harding AC. In “Step” with HIV Vaccines? A Content Analysis of Local Recruitment Campaigns for an International HIV Vaccine Study. Journal of health & mass communication. 2009;1(1):11-39. [PMC free article] [PubMed] [Google Scholar]
- 75.Nakamura M, Saito K, Wakabayashi M. [Effects of attitude formation, persuasive message, and source expertise on attitude change: an examination based on the Elaboration Likelihood Model and the Attitude Formation Theory] Shinrigaku Kenkyu. 1990;61:15–22. doi: 10.4992/jjpsy.61.15. [DOI] [PubMed] [Google Scholar]
- 76.White PH, Harkins SG. Race of source effects in the elaboration likelihood model. J Pers Soc Psychol. 1994;67:790–807. doi: 10.1037/0022-3514.67.5.790. [DOI] [PubMed] [Google Scholar]


