Abstract
Assessing the beliefs and attitudes of Health Care Workers (HCW) to influenza and influenza vaccination can be useful in overcoming low compliance rates. The purpose of our study is to evaluate the opinion of HCW and students regarding influenza, influenza vaccine and the factors associated with vaccination compliance. A survey was conducted between October 2010 and April 2011 in the Florence metropolitan area. A questionnaire was administered to HCW in three local healthcare units and at Careggi University Teaching Hospital. Students matriculating in health degree programs at Florence University were also surveyed.
The coverage with vaccination against seasonal and pandemic influenza is generally low, and it is lower in students than in HCW (12.5% vs 15% for the seasonal vaccination, 8.5% vs 18% for the pandemic vaccination). Individuals comply with vaccination offer mainly to protect themselves and their contacts. Individuals not receiving vaccination did not consider themselves at risk, had never been vaccinated before or believed that pandemic influenza was not a public health concern. Physicians had the highest compliance to vaccination and women were less frequently vaccinated than men. HCW do not appear to perceive their possible influenza infections as a risk for patients: HCW receive vaccination mainly as a form of personal protection.
Low compliance to vaccination is determined by various factors and therefore requires a multi-faceted strategy of response. This should include short-term actions to overcome organizational barriers, in addition to long-term interventions to raise HCW’s level of knowledge about influenza and influenza vaccination.
Keywords: attitudes towards vaccine, vaccine policy, health care workers, influenza, H1N1, pandemic
Introduction
Influenza is a major respiratory tract infection that can cause substantial morbidity and mortality.1-3 Moreover, influenza infections among hospitalized patients can have much more serious consequences than among the general population because an increasing proportion of hospital patients are elderly and/or immunocompromised.4
Vaccination is considered the best preventative measure against influenza. Because health care workers (HCW) are often in contact with patients, they are considered a potential source of transmission. Therefore, vaccinating HCW has been advocated to prevent transmission of the virus to patients.5
Influenza vaccination of HCW reduces the risk of infection for influenza-like-illnesses, prevents absenteeism, reduces presenteeism among staff,6-9 and it appears to prevent nosocomial infections among patients.10-12 Several studies have demonstrated the protective effects of influenza vaccination for patients in hospitals and long-term healthcare facilities.13-16
The World Health Organization, the United States Centers for Disease Control and Prevention, and the immunization guidelines of many countries recommend influenza vaccination of HCW to prevent transmission of influenza from HCW to patients.17-19 However, the same countries report a low uptake of influenza vaccine in HCW.21-26
Utilizing scientific and objective criteria to assess the beliefs and attitudes of HCW on influenza and influenza vaccination, identifying self-reported reasons for influenza vaccine acceptance or non-acceptance and determining predictive factors that are statistically associated with influenza vaccine acceptance can be useful in overcoming low compliance rates.
The purpose of our study was to evaluate the opinion of HCW and students regarding influenza and influenza vaccination and the predictive factors associated with influenza vaccine acceptance.
Results
Descriptive analysis
In total, 2598 subjects completed the questionnaire. Table 1 shows the results of the descriptive analysis. The percentage of missing responses was less than 5% for the following variables: gender, educational qualification, occupational category, local healthcare unit (LHU), vaccination against seasonal influenza in 2007 and 2008, and the declared willingness to get vaccinated in 2010. For all other variables, the percentage of missing responses was between 7% and 13%.
Table 1. Descriptive analysis.
| Variables | Total (n = 2598) | Coverage % Pandemic influenza vaccinated 2009 (n = 390; 15.0%)† |
Coverage % Seasonal influenza vaccinated 2009 (n = 467; 18.0%)‡ |
|
|---|---|---|---|---|
| N | %* | |||
| Gender | ||||
| Male | 661 | 25.4 | 22.6 | 26.1 |
| Female | 1820 | 70.1 | 12.3 | 15.2 |
| Educational qualification | ||||
|---|---|---|---|---|
| Elementary school | 7 | 0.3 | 14.3 | 28.6 |
| Middle school | 170 | 6.5 | 10.2 | 17.7 |
| High school | 1451 | 55.9 | 11.7 | 14.3 |
| Degree | 626 | 24.1 | 18.4 | 21.5 |
| Postgraduate | 208 | 8 | 33.8 | 38.9 |
| Occupational category (profession) | ||||
|---|---|---|---|---|
| Physicians | 258 | 9.9 | 41.4 | 45.1 |
| Nurses | 1017 | 39.1 | 13.5 | 15.0 |
| Other healthcare workers | 496 | 19.1 | 12.8 | 17.7 |
| Non-healthcare workers | 99 | 3.8 | 19.4 | 27.8 |
| Students | 602 | 23.2 | 8.5 | 12.5 |
| Department (if healthcare workers, n = 1996) | ||||
|---|---|---|---|---|
| Primary care | 184 | 9.2 | 23.8 | 27.3 |
| Surgical | 278 | 13.9 | 16.2 | 19.6 |
| Medical | 393 | 19.7 | 15.3 | 16.8 |
| Intensive care unit | 175 | 8.8 | 12.0 | 13.4 |
| Emergency/first aid | 206 | 10.3 | 15.7 | 18.3 |
| Gynaecology, obstetrics and infant management | 111 | 5.6 | 15.3 | 14.4 |
| Healthcare management | 77 | 3.9 | 36.8 | 41.3 |
| Laboratory and pharmaceutical | 92 | 4.6 | 22.0 | 26.7 |
| Radiology and diagnostic imaging | 79 | 4.0 | 15.2 | 20.5 |
| Community services | 10 | 0.5 | 11.1 | 30.0 |
| Maintenance services | 2 | 0.1 | 100.0 | 100.0 |
| Other | 134 | 6.7 | 22.6 | 27.9 |
| Company affiliation | ||||
|---|---|---|---|---|
| AOU Careggi | 240 | 12.0 | 18.8 | 22.8 |
| LHU Empoli | 467 | 23.4 | 28.9 | 29.8 |
| LHU Pistoia | 1229 | 61.6 | 12.1 | 16.4 |
| University (students) | 662 | 23.2 | 8.5 | 12.5 |
| Vaccination against seasonal influenza in 2008 | ||||
|---|---|---|---|---|
| Yes | 458 | 17.6 | 55.5 | 79.6 |
| No | 2031 | 78.2 | 5.6 | 4.2 |
| Vaccination against seasonal influenza in 2007 | ||||
|---|---|---|---|---|
| Yes | 471 | 18.1 | 49.3 | 73.9 |
| No | 2038 | 78.4 | 6.4 | 5.2 |
| (Willingness) Plans to vaccinate in 2010 | ||||
|---|---|---|---|---|
| Yes | 413 | 15.9 | 58.2 | 80.2 |
| No | 2141 | 82.4 | 6.8 | 6.2 |
| Preferred type of vaccine | ||||
|---|---|---|---|---|
| Adjuvanted | 490 | 18.9 | 26.0 | 30.2 |
| Non-adjuvanted | 419 | 16.1 | 16.5 | 22.3 |
| Do not know/not care | 1381 | 53.2 | 12.8 | 15.1 |
| Type of administration | ||||
|---|---|---|---|---|
| Intramuscular injection/subcutaneous | 987 | 38.0 | 18.5 | 22.0 |
| Intradermic | 380 | 14.6 | 17.6 | 24.3 |
| Do not know/not care | 999 | 38.5 | 13.0 | 15.4 |
| Self-perceived health status in two categories | ||||
|---|---|---|---|---|
| Not good (1–5) | 137 | 5.3 | 25.4 | 28.6 |
| Good (6–10) | 2274 | 87.5 | 14.5 | 17.7 |
| Age | Total (n = 2598) | Pandemic influenza vaccinated 2009 (n = 390; 15.0%)† | Seasonal influenza vaccinated 2009 (n = 467; 18.0%)‡ | |
|---|---|---|---|---|
| N (%) | 2376 (91.5) | 2366 (91.1) | 2333 (89.8) | |
| Media (DS) | 38.3 (11.6) | 42.8 (11.5)§ | 42.0 (11.8)‖ | |
| Range | 18 – 66 | 18–65 | 18–66 | |
*Difference between 100% and the sum of the percentages of each variable corresponds to missing values; †For all categorical variables, distribution compared with pandemic influenza vaccination (vaccinated vs. not vaccinated): P < 0.05 (Chi2 test); ‡For all categorical variables, distribution compared with seasonal influenza vaccination (vaccinated vs. not vaccinated): P < 0.05 (Chi2 test); §Comparison between averages for pandemic influenza vaccinated vs. not vaccinated: P < 0.05 (t Student test); ‖Comparison between averages for seasonal influenza vaccinated vs. not vaccinated: P < 0.05 (t Student test).
The percentage of subjects who accepted vaccination offer was 15% and 18% for pandemic and seasonal influenza, respectively. In 2009, 305 subjects were vaccinated against both pandemic and seasonal influenza, 162 solely against seasonal influenza, and 85 solely against pandemic influenza. In contrast, 2046 subjects had received neither vaccination.
The uptake of vaccination, both for seasonal and pandemic influenza, was significantly associated with all the variables under consideration, with higher prevalence in the following groups: males, individuals with post-graduate degrees, physicians, healthcare managers, maintenance workers and non-medical technicians, employees in Empoli LHU, individuals previously vaccinated, and individuals willing to be vaccinated against seasonal influenza in 2010. Moreover, coverage is higher among those who prefer the adjuvanted vaccine, intramuscular injection for vaccination against pandemic influenza and intradermic injection against seasonal influenza, and among those who believed their own health is “not good”. Furthermore, the vaccinated subjects have significantly higher mean age than the non-vaccinated.
Reasons to be vaccinated or not
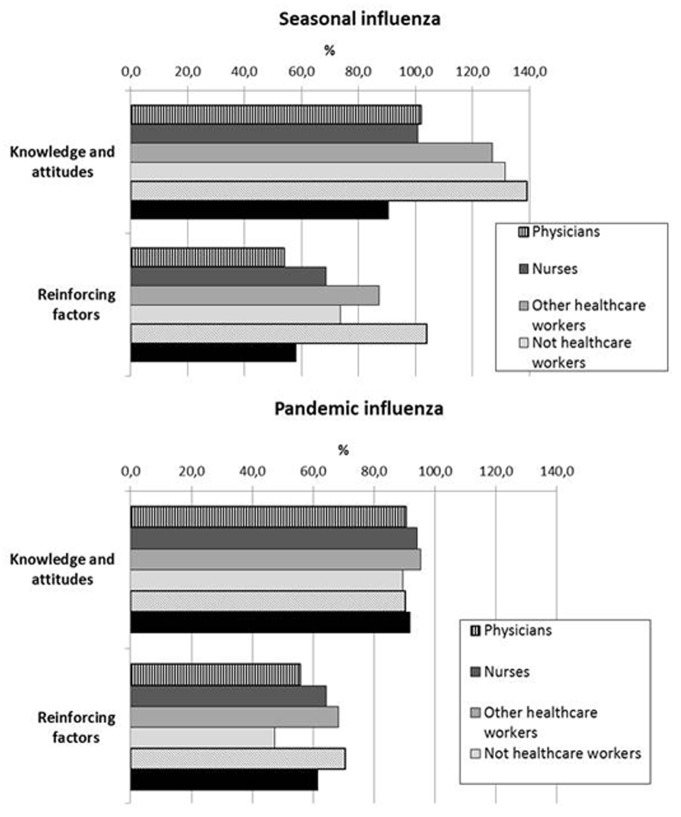
For the 390 respondents who were vaccinated against pandemic influenza and the 467 who were vaccinated against seasonal influenza in 2009, the main determinants of willingness to be vaccinated were primarily personal knowledge and attitudes about influenza and the influenza vaccine (Fig. 1).
Figure 1. Reasons reported for the uptake of seasonal or pandemic influenza vaccine in 2009 (the sum of the percentage is over 100% since it was possible to give more than one answer).
The results show a clear preponderance of responses such as “I do not want to get sick” (81.0% for pandemic vaccination, 82.4% for seasonal vaccination) and “I want to protect the patients and my family” (77.7% and 74.5%, respectively). Moreover, all the categories seem to minimize the importance of getting vaccinated to protect patients.
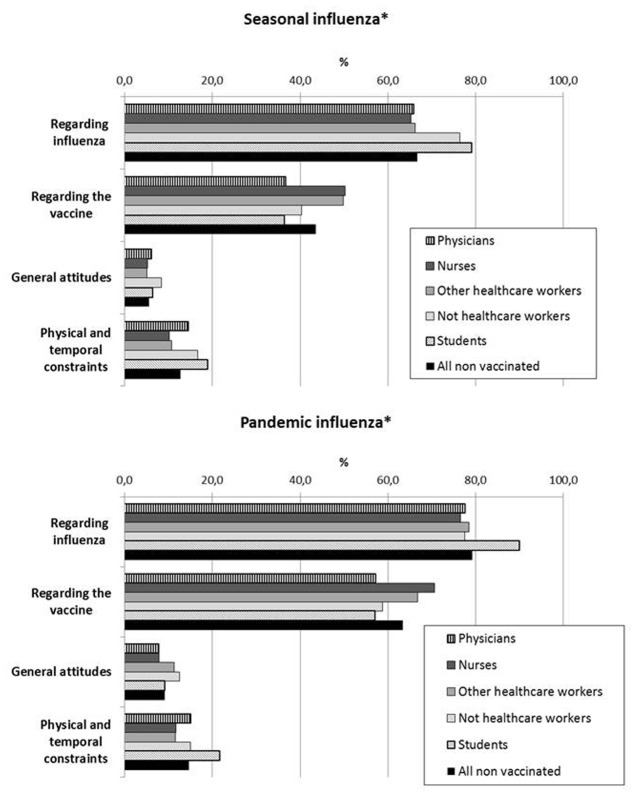
The reasons for non-vaccination primarily focus on the disease (79.3% for the pandemic, 66.6% for the seasonal vaccination) and the vaccine (63.5%, 43.5%, respectively) (Fig. 2). Specifically, the motivations most frequently reported were “I do not belong to a high risk group” (40.6% for the pandemic, 39.9% for the seasonal vaccination), “I have never been vaccinated before” (34.5% for the seasonal vaccination), and “Pandemic flu is not a serious disease” (41.6% for the pandemic vaccination).
Figure 2. Reasons reported for non-acceptance of seasonal or pandemic influenza vaccine in 2009 (*Chi2 test p < 0.05).
Several subjects were not vaccinated for a more general reason, i.e., fear of needles (5.6%).
Students reported higher numbers of non-vaccination linked to reasons concerning the illness and the scarce availability of the vaccine, while nurses and other HCW refused more often based on the characteristics of the vaccine. Moreover, physicians and students were less likely to attribute non-vaccination to issues related to the type and composition of the vaccine.
Logistic regression analysis
Table 2 shows the results of the multivariate logistic regression. This table does not include variables related to previous vaccinations or to a willingness to be vaccinated during the course of 2010 season.
Table 2. Multivariate logistic regression analysis without variables related to previous influenza vaccinations and the intention to get vaccinated in 2010 (adjusted by sampling method).
| Variable | Pandemic influenza vaccination* | Seasonal influenza vaccination† | ||||
|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | |
| Gender (ref. = Male) | ||||||
| Female | 0.56 | <0.001 | 0.43–0.72 | 0.61 | <0.001 | 0.48–0.78 |
| Living with carriers of chronic diseases (ref. Yes) | ||||||
|---|---|---|---|---|---|---|
| No | 0.53 | <0.001 | 0.38–0.73 | 0.56 | <0.001 | 0.41–0.76 |
| Occupational category (profession) (ref. = Physician) | ||||||
|---|---|---|---|---|---|---|
| Nurse | 0.33 | <0.001 | 0.23–0.46 | 0.26 | <0.001 | 0.19–0.38 |
| Other healthcare workers | 0.23 | <0.001 | 0.16–0.36 | 0.26 | <0.001 | 0.18–0.39 |
| Not healthcare workers | 0.23 | <0.001 | 0.12–0.45 | 0.28 | <0.001 | 0.15–0.51 |
| Students | 0.29 | <0.001 | 0.16–0.51 | 0.32 | <0.001 | 0.19–0.55 |
| Department (ref. = medical) | ||||||
|---|---|---|---|---|---|---|
| Surgical | 1.23 | 0.350 | 0.79–1.92 | 1.33 | 0.196 | 0.86–2.05 |
| Gynaecology, obstetrics and infant management | 1.48 | 0.210 | 0.80–2.71 | 1.12 | 0.727 | 0.60–2.07 |
| Intensive care unit | 0.65 | 0.130 | 0.37–1.13 | 0.68 | 0.165 | 0.39–1.17 |
| Emergency/first aid | 0.91 | 0.697 | 0.55–1.48 | 1.01 | 0.970 | 0.63–1.62 |
| Healthcare management | 3.35 | <0.001 | 1.78–6.29 | 2.72 | 0.002 | 1.45–5.08 |
| Laboratory and pharmaceutical | 2.17 | 0.015 | 1.16–4.04 | 2.04 | 0.019 | 1.12–3.70 |
| Radiology and diagnostic imaging | 1.25 | 0.547 | 0.60–2.58 | 1.37 | 0.350 | 0.70–2.67 |
| Community services | 0.58 | 0.617 | 0.07–5.01 | 1.98 | 0.360 | 0.46–8.55 |
| Primary care | 1.43 | 0.145 | 0.88–2.32 | 1.47 | 0.108 | 0.92–2.36 |
| Maintenance services | 1.02 | 0.990 | 0.09–11.38 | 1.08 | 0.948 | 0.09–12.21 |
| Others | 1.34 | 0.290 | 0.78–2.30 | 1.66 | 0.054 | 0.99–2.79 |
| Self-perceived health status (ref. = Not good) | ||||||
|---|---|---|---|---|---|---|
| Good | 0.54 | 0.005 | 0.35–0.83 | - | - | - |
| Chronic pulmonary disease (ref. = Yes) | ||||||
|---|---|---|---|---|---|---|
| No | - | - | - | 0.46 | 0.002 | 0.28–0.75 |
| Diabetes (ref. = Yes) | ||||||
|---|---|---|---|---|---|---|
| No | - | - | - | 0.26 | 0.002 | 0.11–0.60 |
*Number of observations = 2579; LR Chi2 (40 d.f.) = 230.33; Prob > Chi2 < 0.001; Pseudo R2 = 0.1051; †Number of observations = 2537; LR Chi2 (25 d.f.) = 265.10; Prob > Chi2 < 0.001; Pseudo R2 = 0.1094.
For pandemic influenza, women have a significantly lower likelihood of vaccination than men. Other groups with a lower likelihood include those who do not live with carriers of chronic diseases, nurses, other health care providers, non-medical staff and students (especially compared with physicians), and those who tend to report a “good” health status. In addition, health department staff, laboratory workers, and pharmaceutical staff have a significantly higher likelihood of vaccination than those who work in medical wards.
For vaccination against seasonal influenza, the results are similar. Women have a significantly lower likelihood of vaccination, as well as those who do not live with carriers of chronic diseases, nurses, other health care providers, non-medical staff and students (compared with physicians), and those without chronic respiratory diseases or diabetes. Again, health department staff, laboratory workers, and pharmaceutical staff have significantly higher odds than those who work in medical wards.
When the variables related to previous influenza vaccinations or the willingness to get vaccinated in 2010 were entered into the model, the results differed markedly (Table 3).
Table 3. Multivariate logistic regression analysis with variables related to previous influenza vaccinations and the intention to get vaccinated in 2010 (adjusted by sampling method).
| Variable | Pandemic influenza vaccination* | Seasonal influenza vaccination† | ||||
|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | |
| Gender (ref. = Male) | ||||||
| Female | 0.71 | 0.033 | 0.53–0.97 | - | - | - |
| Occupational category (profession) (ref. = Physician) | ||||||
|---|---|---|---|---|---|---|
| Nurse | 0.62 | 0.030 | 0.33–0.74 | |||
| Other healthcare workers | 0.42 | 0.001 | 0.26–0.69 | |||
| Not healthcare workers | 0.48 | 0.046 | 0.23–0.99 | |||
| Student | 0.41 | 0.001 | 0.24–0.69 | |||
| Seasonal influenza vaccination 2008 (ref. = Yes) | ||||||
|---|---|---|---|---|---|---|
| No | 0.14 | <0.001 | 0.10–0.20 | 0.08 | <0.001 | 0.05–0.13 |
| Seasonal influenza vaccination 2007 (ref. = Yes) | ||||||
|---|---|---|---|---|---|---|
| No | - | - | - | 0.32 | <0.001 | 0.19–0.53 |
| (Willingness) Plans to vaccinate in 2010 (ref. = Yes) | ||||||
|---|---|---|---|---|---|---|
| No | 0.20 | <0.001 | 0.14–0.28 | 0.07 | <0.001 | 0.05–0.11 |
*Number of observations = 2579; LR Chi2 (12 d.f.) = 727.84; Prob > Chi2 < 0.001; Pseudo R2 = 0.3387; †Number of observations = 2537; LR Chi2 (7 d.f.) = 1402.83; Prob > Chi2 < 0.001; Pseudo R2 = 0.5790.
The variables which maintain a statistically significant association with the outcomes of interest (i.e., having been vaccinated against pandemic influenza in 2009 and against seasonal influenza in 2009) are as follows: gender, age, profession, having been vaccinated for seasonal influenza in 2008, and the willingness to be vaccinated in 2010 against the seasonal vaccination for pandemic influenza; previous vaccination for seasonal influenza in 2007 or 2008, and willingness to be vaccinated in 2010 for seasonal influenza.
In particular, the model yields lower odds of having been vaccinated against the pandemic influenza for women, all occupational groups other than physicians, those who were not vaccinated against seasonal influenza in 2008, and those who are unwilling to receive vaccination in 2010.
For vaccination against seasonal influenza, are significantly less likely to be vaccinated those who were not vaccinated against seasonal influenza in 2007 or 2008, and those who are unwilling to receive vaccination in 2010.
Missing values have been included in the models as a specific category of each variables. For any category, missing values have not shown a statistically significant association with the outcome variables, so they are not included either in Table 2 or in Table 3.
Discussion
The results of the survey show that uptake of vaccination against seasonal (18%) and pandemic (15%) influenza is low, and even lower in students than in HCW. These results are in line with data observed in other studies.27-29 In our study, and as described by other researchers,30 vaccination is performed mainly for self-protection from disease and for the protection of partners and contacts. Individuals who do not get vaccinated tend to avoid this preventive measure because they do not consider themselves at risk, have never been vaccinated before, and/or believe that pandemic influenza is not a public health concern.
These conclusions are confirmed by logistic regression analysis, which shows a positive association between subjects vaccinated in 2009 and a previous tendency to receive vaccinations. Additional factors include living with carriers of chronic diseases, the presence of a medical history of specific chronic diseases (e.g., diabetes, chronic respiratory disease) or the perception of a lack of good health.
The analysis suggests that there is a lack of information on the importance of getting vaccinated to protect patients. Thus, there is a tendency for these individuals to receive vaccination mainly as a personal protection—a trend maintained by the vaccinated subjects over the years (as previous vaccinations are the strongest predictor of the tendency to receive future vaccinations).
Among the reasons for non-vaccination, respondents most often reported concerns about the vaccine, especially for the seasonal influenza, while other causes were less frequently reported. This seems to confirm the fact that the organization of vaccination campaigns in Tuscan LHUs is quite good; on the other hand, students reported few opportunities to be vaccinated at a high rate, seeming to suggest some organizational constraints in accessing vaccination.
Professional categories are most strongly associated with non-vaccination, and, for pandemic influenza, this variable has an independent effect even when variables relating to the tendency toward vaccination are excluded. Any professional category other than physicians has a significantly lower likelihood of being vaccinated for seasonal influenza, with the exception of hospital personnel not operating in medical wards.
Other studies report that the uptake of vaccination is lower among nurses than doctors,29,30 but there is insufficient data about the attitude toward influenza vaccination of other health professionals or non-HCW who work in health care sector.
The limitations of this study are mainly related to the design. It was necessary to adapt strategies for the distribution of the questionnaires to the specific needs of the HCW. This allowed us to obtain information on as many students and professionals from different healthcare areas and level of education as possible. However, this strategy also had the potential to limit the generalizability of the collected data, introducing a confounder.
The ability to administer the questionnaire in classrooms, both for students and professionals involved in training courses, led to high response rates to the survey (97.5%), including the participation of some “less motivated” personnel. On the other hand, the use of locked boxes in the departments to collect questionnaires (i.e., the mode of data collection adopted for the university hospital of Careggi and the LHU of Empoli) resulted in lower levels of compliance (36.1%). As a result, we cannot exclude the possibility that the different rates of vaccination occurring in those different contexts could result from a selection bias. As a matter of fact, considering the descriptive analysis, a statistically significant association between company affiliation and uptake of vaccination occurred as well as, in the univariate logistic regression analysis, between “sampling method” (i.e., mode of data collection) and the outcome variables. For this reasons, we included the sampling method in the multivariate regression analysis as adjusting factor. Therefore, the role of the predictors was assessed controlling for the procedures we have used in the different settings. Moreover, it should be noted that in the multivariate logistic regression models, the company affiliation is not significantly associated with the outcome variables.
On the other hand, the study design is also a strength of the survey: the overall number of subjects, the diversity of the structures involved (LHUs with hospitals and other services, a University Teaching Hospital, the Faculty of Medicine including many graduation courses), the large number of aspects investigated and the level of statistical analysis provide many causes for reflection.
In conclusion, the results highlight the importance of improving vaccination among HCW in Italy and which professional categories are most important to target when promoting higher vaccine uptake. The study also highlights the importance of improving knowledge about nosocomial influenza transmission and consequences of this among HCW. Moreover, the results indicate the need to strengthen the knowledge about the risk related to influenza among the students, who will be the future health care professionals. As a matter of facts, the study highlights two levels of predictors of getting vaccinated: those that emerges mainly from Table 2 (diseases, occupational category, department) and those that emerges mainly from Table 3 (previous vaccination). Target population should be identified both considering occupational category and department, as well as who have not received the vaccine previously.
The complexity of the factors that could determine low compliance to vaccination requires a multi-pronged approach. This would involve both short-term actions aimed at eliminating organisational barriers and long-term interventions tailored to the HCW’s “profession-sensitive” level of knowledge regarding characteristics of influenza and influenza vaccine31,32 that could promote a higher vaccination uptake.
Having received vaccination in the past is the strongest predictor of vaccination. This result in itself is partially expected as it is assumed that the motivations of vaccination/non-vaccination remain more or less unchanged over the years. The confirmation of this statement is important, however, in the view of promoting vaccination: the results suggest that interventions (and resources) used to promote vaccination, if effective, will have to endure over time because it can introduce a positive behavior that tends to maintain itself over the years. In this regard, interventions of proven effectiveness were found to be, in addition to active offer and free availability of the vaccine, the development of training courses for HCW, the use of mobile vaccination carts in the wards in addition to normal programs of vaccination, giving a feedback on the coverage to each single department, immunization acceptance from some leading figures among HCW and the implementation of an efficient registry of vaccinated professionals.33,34 Furthermore, during university education training, the knowledge about nosocomial influenza transmission and the protection offered by vaccination should be strengthened.
Materials and Methods
Setting
The survey was conducted between October 2010 and April 2011 in the Florence metropolitan area and the data were collected between October and November 2010. In Italy, seasonal influenza vaccination is offered free of charge every year to all HCW. During the influenza pandemic, influenza vaccination was offered free of charge to both HCW and students.
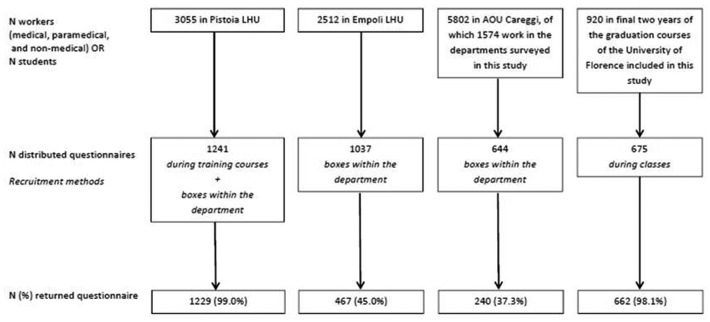
We recruited the study sample among HCW in the LHUs of Empoli (Empoli Hospitals, the Department of Prevention, and local general practitioners) and Pistoia (Pistoia Hospitals, the Department of Prevention, and local health districts), at Careggi University Teaching Hospital (AOU Careggi), and among students attending medical and paramedical degree courses at Florence University in the Faculty of Medicine and Surgery (Students attending the degree programs in Medicine, Nursing, Health Care Assistance, and Techniques of Prevention in the Environment and in the Workplace). At Careggi Teaching Hospital, we restricted the study to the departments of obstetrics and gynecology, cardiology, emergency, and general surgery due to the high influenza risk for patients and HCW in those departments. We also included the department of Occupational Medicine, that has the assigned responsibility to vaccinate all HCW. Among students attending the graduation courses in Medicine, Nursing and other fields, we restricted the survey to students in the final two years of study. This is the period during which students are involved in practical training and, therefore, in direct contact with patients and the general population within the hospital.
The LHUs of Empoli and Pistoia consist of a total of 2512 and 3055 workers, respectively, including both hospital and community services. The Careggi University Teaching Hospital has 5802 workers, of which 1574 work in the departments surveyed in this study. These data refer to the total number of employees, including medical, paramedical, and non-medical workers.
The final two years of the graduation courses in Medicine, Nursing, Health Care Assistance, and Techniques of Prevention in the Environment and in the Workplace consist of approximately 920 students.
The study was conducted according to the Helsinki Declaration of 1975.
Questionnaire and sampling mode
The tool used for the survey was an anonymous self-administered questionnaire with closed-ended questions. The questionnaire was validated in a survey of 95 HCW. It was composed of three sections. In the first section, study participants recorded their agreement or disagreement with factual statements regarding influenza and influenza vaccine. In the second section, participants indicated their previous influenza vaccination status (against pandemic influenza in 2009 and against seasonal influenza between 2007 and 2009) and their reasons for having been vaccinated or not vaccinated. Participants were also asked about their role in administering influenza vaccine, their preferred type of influenza vaccine and which categories of patients they would recommend to be vaccinated. The third section included questions on participants’ socio-demographic characteristics; their degree, qualifications, and home department; whether they lived with people at risk of influenza; and the participant’s medical history regarding cardiovascular chronic disease, chronic respiratory disease, chronic renal failure, diabetes, autoimmune disease, and respiratory infections within the last year. Those last questions indicated a history of conditions leading to complications with influenza, or conditions associated with a higher or lower perception of influenza risk. Finally, the questionnaire required an assessment of self-perceived health status (from 1—bad to 10—excellent), subsequently grouped into two categories (“not good” from 1 to 5; “good” from 6 to 10).
The study was conducted on a convenience sample, and the recruitment of the participants occurred through different methods. In the Empoli LHU and at the Careggi University Teaching Hospital, the study team reached the HCW directly in their departments. The study team asked HCW to complete the questionnaire and to return it to a locked box located within the department. In the Pistoia LHU, the study team participated in mandatory training events to which all of the HCW were invited, while the students of the graduation courses were recruited during classes. At the beginning of each meeting or class, the reasons for the study were explained and participants were asked to complete the questionnaire. Participants returned the completed questionnaire to the study team at the end of the session or class. In the case of HCW in Pistoia hospital who did not participate in the training courses, the study team placed locked boxes in various departments to collect completed questionnaires.
There were 675 students attending the sessions (73% of all registered).
The total number of distributed questionnaires was 3597 (1241 Pistoia LHU, 1037 Empoli LHU, 644 AOU Careggi, 675 University lessons), of which 2627 were returned (1229 Pistoia LHU, 467 Empoli LHU, 240 AOU Careggi, 662 University lessons). The response rate to the survey was very high in training events and sessions, but lower when the questionnaire was self-administered and returned in boxes, although attempts to increase the response rate through repeated contacts with the HCW. Figure 3 shows the flowchart of the sampling procedure.
Figure 3. Flowchart of the sampling procedure.
Twenty-nine questionnaires were excluded from analysis because they did not report vaccination status against pandemic and seasonal influenza in 2009.
Statistical analysis
The collected data were entered in a database created ad hoc. The statistical analysis was performed using STATA 8.0. In this article, we present the results of the data analysis for the second and third sections of the questionnaire. A thorough analysis of the data collected among students has been described in a previous publication.35
A descriptive analysis and a logistic regression analysis were performed, including an evaluation of associations using the Chi2 test and of the differences between means using the Student's t-test for independent data.
To perform the descriptive analysis, the reasons for having received or not having received (in 2009) seasonal or pandemic influenza vaccination were grouped according to the categories proposed by Hollmeyer.30 These included “knowledge and attitudes” and “reinforcing factors” for those having received vaccination and “reasons regarding influenza”, “reasons regarding the vaccine”, “general attitudes”, and “physical and temporal constraints” for those not having received vaccination (Table 4).
Table 4. Categories of reasons reported for receipt or non-receipt of seasonal or pandemic influenza vaccine.
| Seasonal Influenza | Pandemic Influenza |
|---|---|
| Vaccinated | |
| Knowledge and attitudes | |
| I do not want to get sick I want to protect the patients and my family I am vaccinated every year I was sick with influenza in the past I felt compelled to be vaccinated |
I do not want to get sick I want to protect the patients and my family I am vaccinated every year I was sick with influenza in the past I felt compelled to be vaccinated |
| Reinforcing factors | |
|---|---|
| The vaccine administration was convenient I have recommended vaccination |
The vaccine administration was convenient I have recommended vaccination |
| Unvaccinated | |
|---|---|
| Regarding influenza | |
| I am not in the target group I am healthy and I don’t become sick with influenza I forgot to be vaccinated I have never been vaccinated before |
I am not in the target group I am healthy and I don’t become sick with influenza I forgot to be vaccinated I have never been vaccinated before I was vaccinated for seasonal influenza Pandemic influenza is not a serious disease |
| Fear of side effects The vaccine does not work I am concerned about getting influenza from the vaccine |
Fear of side effects The vaccine does not work I am concerned about getting influenza from the vaccine The vaccine is not safe |
| Fear of needle | Fear of needle |
| The vaccine administration was not convenient I did not have time to be vaccinated No one informed me about the vaccination campaign |
The vaccine administration was not convenient I did not have time to be vaccinated No one informed me about the vaccination campaign |
The univariate and multivariate logistic regression analysis was performed to assess the degree of association, as measured by odds ratio (OR), between all the variables and the two outcome variables of having been vaccinated against pandemic influenza in 2009 and having been vaccinated against seasonal influenza in 2009.
In the univariate analysis, the variables statistically associated with having been vaccinated against pandemic influenza were as follows: gender, age, having received the seasonal influenza vaccine in 2008, having received the seasonal influenza vaccine in 2007, willingness to be vaccinated against seasonal influenza in 2010, profession, field of work, local health unit or degree program, suffering from chronic cardiovascular diseases, chronic respiratory failure, chronic renal failure, diabetes, autoimmune diseases, having suffered from one or more respiratory infections in 2008, and living with people 65 y or older and/or with people suffering from chronic diseases, sampling method (classrooms or boxes). The same variables also have a statistically significant association with having been vaccinated against seasonal influenza in 2009.
These variables were entered into multivariate logistic regression models conducted using the backward stepwise method: first, all the variables have been included, then, using a stepwise procedure, the variables with not statistically significant association have been removed. The final models include only the variables with a statistically significant association with the outcome variables in the multivariate analysis. The final four models are presented in this article as follows: for each outcome variable (respectively, having received the seasonal and having received the pandemic vaccination) two different models have been performed, one that includes previous influenza vaccinations and willingness to receive the influenza vaccination; one that does not include previous influenza vaccinations and does not include willingness to receive the vaccination. This approach stems from the need to investigate both the predictive factors for vaccination and the tendency toward receiving vaccinations. Since the sampling method (classrooms or boxes) have shown a statistically significant association in the univariate analysis, either for pandemic or seasonal influenza vaccination, this variable has been included in each model as a confounder.
For all the analyses the α level was 0.05.
Acknowledgments
The authors want to thank Giuditta Niccolai, Barbara Porchia, Gianrocco Martino and Lorenza Giannarelli.
Glossary
Abbreviations:
- HCW
health care workers
- LHU
local healthcare unit
- OR
odds ratio
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Opstelten W, van Essen GA, Heijnen ML, Ballieux MJ, Goudswaard AN. High vaccination rates for seasonal and pandemic (A/H1N1) influenza among healthcare workers in Dutch general practice. Vaccine. 2010;28:6164–8. doi: 10.1016/j.vaccine.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 2.Cox NJ, Subbarao K. Influenza. Lancet. 1999;354:1277–82. doi: 10.1016/S0140-6736(99)01241-6. [DOI] [PubMed] [Google Scholar]
- 3.Donaldson LJ, Rutter PD, Ellis BM, Greaves FE, Mytton OT, Pebody RG, Yardley IE. Mortality from pandemic A/H1N1 2009 influenza in England: public health surveillance study. BMJ. 2009;339:b5213. doi: 10.1136/bmj.b5213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals--a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 5.Smith NM, Bresee JS, Shay DK, Uyeki TM, Cox NJ, Strikas RA, Advisory Committee on Immunization Practices Prevention and control of influenza: recommendations of the advisory committee on immunization practices (ACIP) MMWR Recomm Rep. 2006;55(RR-10):1–42. [PubMed] [Google Scholar]
- 6.Wilde JA, McMillan JA, Serwint J, Butta J, O’Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999;281:908–13. doi: 10.1001/jama.281.10.908. [DOI] [PubMed] [Google Scholar]
- 7.Saxén H, Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18:779–83. doi: 10.1097/00006454-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–8. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 9.Lester RT, McGeer A, Tomlinson G, Detsky AS. Use of, effectiveness of, and attitudes regarding influenza vaccine among house staff. Infect Control Hosp Epidemiol. 2003;24:839–44. doi: 10.1086/502146. [DOI] [PubMed] [Google Scholar]
- 10.Oshitani H, Saito R, Seki N, Tanabe N, Yamazaki O, Hayashi S, Suzuki H. Influenza vaccination levels and influenza-like illness in long-term-care facilities for elderly people in Niigata, Japan, during an influenza A (H3N2) epidemic. Infect Control Hosp Epidemiol. 2000;21:728–30. doi: 10.1086/501725. [DOI] [PubMed] [Google Scholar]
- 11.Carman WF, Elder AG, Wallace LA, McAulay K, Walker A, Murray GD, Stott DJ. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–7. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 12.Potter J, Stott DJ, Roberts MA, Elder AG, O’Donnell B, Knight PV, Carman WF. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burls A, Jordan R, Barton P, Olowokure B, Wake B, Albon E, Hawker J. Vaccinating healthcare workers against influenza to protect the vulnerable--is it a good use of healthcare resources? A systematic review of the evidence and an economic evaluation. Vaccine. 2006;24:4212–21. doi: 10.1016/j.vaccine.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 14.Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, Murad S, Watson JM. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas RE, Jefferson T, Lasserson TJ. Influenza vaccination for healthcare workers who work with the elderly: systematic review. Vaccine. 2010;29:344–56. doi: 10.1016/j.vaccine.2010.09.085. [DOI] [PubMed] [Google Scholar]
- 16.van den Dool C, Bonten MJ, Hak E, Heijne JC, Wallinga J. The effects of influenza vaccination of health care workers in nursing homes: insights from a mathematical model. PLoS Med. 2008;5:e200. doi: 10.1371/journal.pmed.0050200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization Influenza vaccines. Wkly Epidemiol Rec. 2002;77:230–9. [PubMed] [Google Scholar]
- 18.Harper SA, Fukuda K, Uyeki TM, Cox NJ, Bridges CB, Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2004;53(RR-6):1–40. [PubMed] [Google Scholar]
- 19.National Advisory Committee on Immunization. Canadian Immunization Guide. Available at: www.phac-aspc.gc.ca/publicat/cig-gci/index.html Accessed on May 15, 2013.
- 20.Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, Murad S, Watson JM. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray SB, Skull SA. Poor health care worker vaccination coverage and knowledge of vaccination recommendations in a tertiary Australia hospital. Aust N Z J Public Health. 2002;26:65–8. doi: 10.1111/j.1467-842X.2002.tb00273.x. [DOI] [PubMed] [Google Scholar]
- 22.Habib S, Rishpon S, Rubin L. Influenza vaccination among healthcare workers. Isr Med Assoc J. 2000;2:899–901. [PubMed] [Google Scholar]
- 23.Smedley J, Palmer C, Baird J, Barker M. A survey of the delivery and uptake of influenza vaccine among health care workers. Occup Med (Lond) 2002;52:271–6. doi: 10.1093/occmed/52.5.271. [DOI] [PubMed] [Google Scholar]
- 24.Weingarten S, Riedinger M, Bolton LB, Miles P, Ault M. Barriers to influenza vaccine acceptance. A survey of physicians and nurses. Am J Infect Control. 1989;17:202–7. doi: 10.1016/0196-6553(89)90129-6. [DOI] [PubMed] [Google Scholar]
- 25.Russell ML, Henderson EA. The measurement of influenza vaccine coverage among health care workers. Am J Infect Control. 2003;31:457–61. doi: 10.1016/S0196-6553(03)00085-3. [DOI] [PubMed] [Google Scholar]
- 26.Russell DW, Cameron DJ, Lockey RF, Behnke RH, Sinnott JT, Ganguly R. Influenza vaccination acceptance among health care professionals. Vaccine. 1991;9:691–2. doi: 10.1016/0264-410X(91)90206-L. [DOI] [PubMed] [Google Scholar]
- 27.Rachiotis G, Mouchtouri VA, Kremastinou J, Gourgoulianis K, Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among healthcare workers in Greece. Euro Surveill. 2010;15:19486. [PubMed] [Google Scholar]
- 28.Mereckiene J, Cotter S, Nicoll A, Lévy-Bruhl D, Ferro A, Tridente G, Zanoni G, Berra P, Salmaso S, O’Flanagan D, et al. VENICE Project Gatekeepers Group National seasonal influenza vaccination survey in Europe, 2008. Euro Surveill. 2008;13:19017. doi: 10.2807/ese.13.43.19017-en. [DOI] [PubMed] [Google Scholar]
- 29.Kaboli F, Astrakianakis G, Li G, Guzman J, Donovan T, Naus M. Influenza vaccination and intention to receive the pandemic H1N1 influenza vaccine among healthcare workers of British Columbia, Canada: a cross-sectional study. Infect Control Hosp Epidemiol. 2010;31:1017–24. doi: 10.1086/655465. [DOI] [PubMed] [Google Scholar]
- 30.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals--a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 31.Cadena J, Prigmore T, Bowling J, Ayala BA, Kirkman L, Parekh A, Scepanski T, Patterson JE. Improving influenza vaccination of healthcare workers by means of quality improvement tools. Infect Control Hosp Epidemiol. 2011;32:616–8. doi: 10.1086/660198. [DOI] [PubMed] [Google Scholar]
- 32.Esolen LM, Kilheeney KL, Merkle RE, Bothe A. An alternate approach to improving healthcare worker influenza vaccination rates. Infect Control Hosp Epidemiol. 2011;32:703–5. doi: 10.1086/660762. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Interim results: influenza A (H1N1) 2009 monovalent and seasonal influenza vaccination coverage among health-care personnel - United States, August 2009-January 2010. MMWR Morb Mortal Wkly Rep. 2010;59:357–62. [PubMed] [Google Scholar]
- 34.Sartor C, Tissot-Dupont H, Zandotti C, Martin F, Roques P, Drancourt M. Use of a mobile cart influenza program for vaccination of hospital employees. Infect Control Hosp Epidemiol. 2004;25:918–22. doi: 10.1086/502320. [DOI] [PubMed] [Google Scholar]
- 35.Bonaccorsi G, Lorini C, Porchia BR, Niccolai G, Martino G, Giannarelli L, Santomauro F. Vaccinazione antinfluenzale: copertura e percezione del rischio tra gli stusenti dell’ area sanitaria dell’ Univesità di Firenze. Ann Ig. 2013;25:181–9. doi: 10.7416/ai.2013.1920. [DOI] [PubMed] [Google Scholar]