Abstract
Frailty is a significant public health issue which is experienced by homeless and other vulnerable adults; to date, a frailty framework has not been proposed to guide researchers who study this hard-to-reach population. The Frailty Framework among Homeless and other Vulnerable Populations (FFHVP) has been developed from empirical research and consultation with frailty experts in an effort to characterize antecedents, i.e. situational, health-related, behavioral, resource, biological, and environmental factors which contribute to physical, psychological and social frailty domains and impact adverse outcomes. As vulnerable populations continue to age, a greater understanding of frailty will enable the development of nursing interventions.
Introduction
The domestic and international population is aging; by 2050, 25% of the population will be 65 and older while those over 85 will triple 1. The number of older homeless adults is expected to increase as well 2-4. Homeless service agencies report that nearly 33% of chronic homeless persons are over age 55 4; in Los Angeles County (LAC) alone, there were approximately 51,340 homeless adults in 2011 and nearly one quarter (23%) were 55 to 61 years of age 5.
Aging trends among vulnerable populations prompt several areas of research, one of which is identification of frailty; defined as a state which affects an individual who experiences an accumulation of deficits 6,7 in physical, psychological, and social domains, leading to adverse outcomes such as disability and mortality 8,9. There is a dearth of literature on frailty among homeless populations and based on the operational measure used, rates have differed. One study among a Canadian sample found that 7.2% of the population was frail at baseline, while another study among a Mexican-American sample found that found that 37.1% of the population was frail, 33.3% of the population was pre frail and 29.6% of the population was not frail 10 Among homeless populations, in one Boston-based homeless sample, aged 50-69, the prevalence of frailty was 16 percent 11. The purpose of this manuscript is to derive the Frailty Framework among Vulnerable Populations (FFVP), which is an adaptation of the Integrated Conceptual Model of Frailty 9, the Working Framework for Understanding Frailty 12, and vulnerable populations conceptual model 13.
Previous Frailty Models and Limitations
For over six decades, frailty has been debated in the literature and models have been devised to explain the physiological, biological and molecular pathways of the syndrome 12,14 without specific attention being paid to populations at significant risk (e.g. homeless). Previous biologic models of frailty have described the clinical pathways of frailty, such as underlying alterations, clinical features and adverse outcomes 14. Models likewise showcase age-related physiologic changes which include sarcopenia, neuroendocrine dysregulation, and immune dysfunction 14.
Bergman et al. (2004) developed a working framework for understanding frailty. Antecedents to frailty included biological, psychological, social, societal, and environmental factors; further, disease and a decline in physiologic reserve were conceptualized to lead to weight loss, under nutrition, weakness, decreased endurance and physical activity, slowness, cognitive decline, and depressive symptoms 15. Thus, frailty was described as leading to adverse outcomes, namely disability, morbidity, hospitalization, institutionalization and death 15. One of the major limitations of this model includes the fact that frailty is not divided into three respective components, namely physical, psychological or social. In addition, life span determinants are not specifically identified as they relate to vulnerable populations.
Gobbens et al. (2010) adapted the Bergman et al. (2004) Working Framework Model, labeling it the Integral Conceptual Frailty Model and apportioning frailty into physical, psychological and social domains. The Integral Conceptual Model of Frailty (ICMF) includes antecedents, such as sociodemographics (e.g. age, education, income, sex, and marital status), lifestyle, life events and biological factors 9. The limitations of the ICMF model, the Working Framework in Development Model 12 and biological models 14 are that they do not identify the difference between vulnerable populations in terms of significant behavioral factors, such as drug and alcohol use; biological factors, such as telomere shortening and heightened immune activation; environmental factors, which may include the built environment; type of lifestyle which may include gang membership, and certain life events such as incarceration and homelessness which may place them at greater risk for frailty. Further, these models do not take into account macro-level variables which may influence individual, situational, behavioral and health-related risk factors. In terms of the vulnerable populations conceptual model, the concept of frailty is not identified, which is similarly a limitation.
Vulnerability Defined
Vulnerable populations are defined as groups who have an increased relative risk, and decreased societal and environmental resources which lead to poor health status increasing the morbidity and mortality 13. These authors contend that resource availability can be socioeconomic and environmental; whereas, relative risk is exposure to risk factors which may include lifestyle, behaviors and choices. Data suggest that socially disenfranchised groups are at higher risk for negative health outcomes, including premature aging and mortality relative to the general population 16,17. Populations who may fall under the category of vulnerability include those on parole, probation, homeless and those who display high levels of relative risk. Vulnerability may place one at risk for frailty; however, vulnerable populations are not all frail. In an effort to begin to disentangle frailty and vulnerability, we need to identify specific antecedents which may place vulnerable populations at risk for frailty.
Risk Factors for Frailty across the Lifespan
Across the lifespan, homeless and otherwise vulnerable populations may have life events such as a fragmented childhood, adolescence, possible histories of incarceration and recidivism, foster placement, as well as behavioral factors, such as illicit drug use which may place them at greater risk for frailty. Early childhood events such as a disruptive and abusive home environment may curtail normalcy and encourage running away from home. Once on the street, a significant set of risk factors become avenues for physical, sexual abuse and victimization. A study among homeless men and women found that a higher rate of victimization was found among those who had a diagnosis of mania, drug dependence and of both alcohol and drug dependence 18.
Data reveal the drug and alcohol dependence may perpetuate incarceration and recidivism; in fact, one federal report found that 32% of State prisoners and 22% for Federal prisoners had used drugs at the time of the offense 19. For homeless female ex-offenders, challenges abound when reintegrating into society 20. In this qualitative, descriptive study among homeless female parolees (N=14), challenges which these women faced included challenges to accessing health care, moving forward, preventing relapse and program seeking 20.
As individuals age, they are more likely to be frail 21-23. Additionally, women with limited education, lower socioeconomic status and minority status are more likely to be frail 24-26. Data suggest that frail older adults who have been exposed to a lifetime of health inequities are vulnerable and are at increased risk for frailty. Based on the aforementioned empirical data, both frailty and homelessness make individuals more likely to be vulnerable to poor health care outcomes, premature morbidity and mortality.
Proposed Research Model
The FFVP is a modification of the Integral Conceptual Model of Frailty (ICMF) 8,9, the Working Frailty Framework model 12and the vulnerable populations model 13. The Frailty Framework among Vulnerable Populations (FFVP) has evolved from empirical research and consultation with frailty experts (R. Gobbens, personal communication, September 23, 2012; J. Morley, personal communication, December 7, 2011). The FFVP was developed to guide researchers who work with vulnerable populations, such as homeless adults, a hard-to-reach population. In order to build the model, we have explored empirical research in order to construct factors which we feel underlie micro-level relationships which affect the frailty triad and lead to the adverse events cascade. One vulnerable population which will serve as an exemplar will be homeless persons; we will delve into this literature throughout the manuscript providing the reader with an exemplar.
FFVP Assumptions
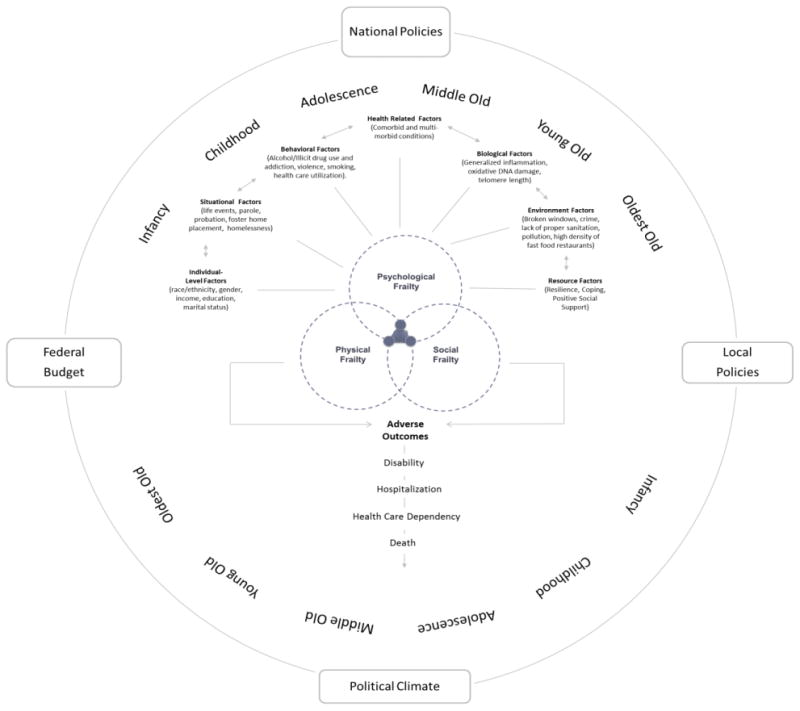
Figure 1 depicts the multidimensional FFVP framework designed to understand individual-level, situational, health-related, behavioral, resource, biological and environmental predictors which are conceptualized to affect frailty and adverse outcomes over the life course. It is important to note that some of these assumptions can be hypotheses and statistically tested:
Figure 1. Frailty Framework among Vulnerable Populations.
Frailty occurs across the life continuum, regardless of age.
Vulnerability and frailty are distinct concepts. Both can represent an accumulation of a different set of deficits. Frailty is an accumulation of deficits in physical, social and psychological spheres. Whereas, vulnerability is an accumulation of deficits in relative risk and poor resources.
Individual, situational, health-related, behavioral, resource, biological and environmental factors may influence frailty.
Frailty domains form a triad: (a) physical, (b) psychological, and (c) social and the presence of all three render an individual frail and at risk for adverse events.
Frailty leads to disability, increased health care utilization, hospitalization, health care dependency and death.
There is an opportunity for health promotion/prevention and clinical case management across this life continuum.
In the model, we have identified several variables which fall under relative risk and influence frailty. These include individual-level factors, situational, health-related, behavioral, resource, biological and environmental factors).
Macro-level variables
In the model, we have identified several macro – level variables which serve as external influences. For instance, both national and local policies may affect micro-level variables by leading to homelessness, increased health care utilization, and higher densities of fast food restaurants. In addition, the political climate of the nation may similarly affect these variables.
Risk Factors for Frailty
Factors which we feel place individuals at greater risk for frailty include individual-level, situational, health-related, behavioral, resource, biological, and environmental.
Individual-Level Factors
Individual-level factors include race/ethnicity, gender, income, education. Being a part of a specific race or ethnicity may result in similarities regarding geographic origin, ethnic origin, or sociocultural group. In addition, income or the amount of monetary currency exchanged for types of services rendered is an important situational variable. Some evidence suggests that African Americans, those with lower education and income are more likely to be frail compared to those who do not have these characteristics (p<.001) 27. In terms of gender, women are more likely to be frail when compared to men 29.
Life Events
Physical, sexual or verbal victimization can be defined as having experienced i.e. shootings, beatings, stabbings, battery, assault, and gang violence, sexual assault or verbal victimization during childhood or in adulthood. Certain life experiences, in particular, incarceration, a state of being confined, or being on probation or parole may lead to physical trauma. Both conditions represent being conditionally released as a prisoner without having served a complete sentence 30,31. One of the main undercurrents of incarceration is violence; behind bars data suggest that individuals are exposed to rape 32-34, beatings, stabbings which may affect health-related factors and contribute to frailty.
Another significant issue is homelessness, defined as an individual who lacks a fixed, regular, and adequate nighttime residence, and who has a primary nighttime residence that is a supervised publicly or privately operated shelter designed to provide temporary living accommodations (United States Department of Housing and Urban Development [USDHUD], 1995). In 2011, Brown et al. studied older homeless adults (N=247) at risk for geriatric syndromes and found the prevalence of frailty was 16 percent 11.
Health-Related Factors
Health-related factors are defined as self-reported health conditions and nutritional deficiencies. In one study, nearly 85% of homeless adults over 50 years of age reported having at least one chronic health condition 35. Data suggest that correlates of frailty may include chronic kidney disease 36, diabetes mellitus 37, cognitive impairment 38-40, obesity 41 and human immunodeficiency virus (HIV) 42,43; these represent some, but not all of the significant health factors in this population.
Nutritional deficiencies are also a significant issue. While food is usually acquired in soup kitchens or other charitable programs; it is likely that food may also be acquired by other means, i.e. theft, sex trade work, selling items, or paid employment. In one cross sectional study in Germany, 29% of the homeless population sampled (N=75, 19-62) was malnourished and data suggest it was related to drug use and other chronic disease problems 44. Among older adults, malnutrition is similarly a significant issue; some authors have indicated that there is a malnutrition-sarcopenia syndrome which leads to lean body mass loss, strength and functionality 45.
Behavioral Factors
Certain behavioral factors which may be significant among this population, i.e. alcohol, drug use, smoking, violence and health care utilization, may affect health-related factors and may be influenced by biological factors and the environmental factors. Alcohol and illicit drugs include opioids, psychedelics, psycho-stimulants, general central nervous system depressants, and a combination of other drugs 46. Researchers have detailed that alcohol and illicit drug use are commonly used by homeless adults 47,48, and may influence homelessness 28.
Riley et al. (2007) found that among homeless adults (N=324), men were more likely to report crack cocaine in the last 30 days, heroin, methamphetamine and heavy alcohol use when compared to women. In particular, among women, 27% of the population reported crack cocaine use compared to 34% of men, while 7% of women reported heroin use when compared to 16% of men 28. In terms of heavy alcohol use, approximately 53% of women reported such use in the last 30 days compared to 58% of men 28. Data suggest that for both men and women, individuals who smoked heavily were more likely to have higher frailty scores 49. Among homeless adults, smoking is a considerable challenge 50; in fact, one study found that nearly 80% of chronically homeless adults (n=754) were current cigarette smokers 51.
Health care utilization is a significant issue among both frail adults 52 and homeless adults 53,54. Unmanaged chronic conditions increase hospital expenditures and care. Hahn et al. (2006) found that for homeless populations emergency department visits were prevalent.
Resource Factors
Resource factors such as resilience, coping and positive social networks may be protective over the life course; in fact, higher levels of resilience may encourage stress reduction. A study among homeless youth (N=47) found that increased time living on the street may affect resilience and increase psychological distress; however, perceived resilience may be related to lower suicidal ideation and lower psychological distress 55.While resilience may be a key resource,, this relationship has not been explicated among homeless adults and is not well understood in terms of its relationship with frailty.
Social support can be both formal and informal and have multiple dimensions which encompass type, source, perceptions of support 56, and cognitive/perceived, behavioral/received support 57. Social support can be further deconstructed to include emotional, financial and instrumental support 57. Poor social support has been associated with increased stress and poor coping among homeless populations 58. In a study of homeless youth, those who used problem-focused coping were more likely to decrease alcohol, when compared to those who used emotion-focused coping 59. In particular, instrumental social support was significantly correlated with problem-focused coping (p<.0005), emotional social support (p<.05), social isolation (p<.05) 59. Likewise, social isolation was significantly related to emotion-focused coping (p<.005), and stress (p<.05) 59.
Biological Factors
Biologic factors are modifiable risk factors which may be composed of generalized inflammation, oxidative DNA damage and telomere shortening. Generalized inflammation includes the presence of inflammatory cytokines, i.e. interleukin- 6, interleukin IB, and tumor necrosis factor (TNF). Biological factors caused by changes in gene expression and oxidative DNA damage may affect situational factors and health-related factors. In particular, decreased oxidative DNA damage leads to the decreased ability to build macromolecules, decreased protein synthesis, and decreased lean body mass, which may lead to a decrease in muscle function, strength and oxygen consumption 14. Telomeres, known as biomarkers of cellular senescence have been studied in relation to frailty. While one study found no correlation between telomere length, age and sex among community dwelling older adults 60 this has not been studied among homeless populations and may be a promising area for future exploration
Environmental Factors
The built environment is composed of the physical environment which may encompass broken windows and crime, lack of proper sanitation, pollution, and high density of fast food restaurants. In fact, broken windows of neighborhoods may be an indication of lack of safety and poor economic conditions. The built environment may have a positive or negative affect on health 61,62. Further, improper sanitation may have adverse effects on health; namely transmission of communicable diseases, i.e. Hepatitis A virus infection 63,64 which may affect biological systems, along with health-related factors. Additionally, excess fast food restaurants and lack of supermarkets make it challenging to obtain appropriate nutrition, ultimately affecting and leading to health related factors, such as comorbid and multi morbid conditions.
Frailty Domains
Frailty encompasses physical, psychological and social domains. Characterized by a decline in physical functioning, walking speed, and grip strength, physical frailty may be influenced by psychological and social frailty. Physical functioning is closely tied to mobility and research findings reveal that homeless populations are at risk for impairments in this domain 11. One study found that among homeless adults (N=247) impaired mobility affected 41% (102/247) of homeless adults over 50 11. Further, 37% (90/247) of older homeless adults reported difficulty with balance 11 and over half of the population reported that they had fallen in the previous year 11. Decreased grip strength may be closely related with disability, morbidity, mortality and frailty; in a cross-sectional study among men (n=411) and women (n=306) between 64-74 years of age, findings revealed that grip strength may be a more accurate predictor of frailty than chronological age 65.
Composed of depression and a decline in cognition, psychological frailty may affect physical, as well as, social frailty. Investigators have found that frail individuals who have cognitive impairment are less likely to rebound 66. A study among a community dwelling sample of older adults in Dublin, found that both pre-frail and frail elderly were more likely to have both anxiety and depression when compared to those who were robust 67. Among homeless populations, data suggest that depression is similarly a significant issue; in particular, Brown et al. (2011) found that 39% of the homeless population experienced depressed feelings for more than seven days.
A decline in social support may influence physical and psychological frailty; social frailty may predict increasing frailty, and for homeless adults, this may be a significant antecedent. One study investigated social determinants of frailty among a Chinese cohort of men (n=999) and women (n=1033) 68. Data reveal that women had a higher frailty index when compared to men 68. Number of relatives and neighbors, and frequency of participation in helping others all influence frailty scores; in fact, authors argue that individuals who have more social support similarly have lower frailty 68.
Adverse Outcomes
Adverse outcomes of frailty may include disability, hospitalization, health care dependency and death. Defined as having a physical and/or mental impairment, a disability limits daily activities which may include mobility, cognitive, hearing, and visual or speech impairments 69. While disability is not synonymous with frailty 70 both homelessness and frailty may place individuals at risk for disability. Homelessness may exacerbate physical disabilities or place individuals at high risk for acquiring a disability. In a study with homeless adults, both impairment with activities of daily living (ADL) and independent activities of daily living (IADL) were pronounced; in particular, approximately 30% (74/247) of the population reported an impairment with ADLs while 57% (140/247) reported difficulties with IADLs 11. Fried & Walston (2003) contend that disability can be an outcome of frailty or even a contributor to the condition. According to LAHSA (2011), approximately 22% of those surveyed suffer from physical disabilities.
Being hospitalized in a hospital for a physical, medical or emotional problem can be a significant issue for both frail adults 71,72 along with homeless adults who utilize larger percentages of health care resources 53. A nationally representative study among currently homeless populations (N=2974), found that nearly 63% had one or more ambulatory visits, 32% an emergency department visit and 23% had been hospitalized 73. Hahn et al. (2006) studied 14-year trends in homelessness and found that emergency department visits (p<.01), staying overnight in a hospital (p<.001) and mental health hospitalization (p<.001) increased from 1996 to 2003.
Defined as being dependent on an institution for nursing or long term care, health care dependency may be a significant issue. For frail adults who stay for extended periods in an institution servicing health care needs, i.e. hospital, nursing home or long term care facility, health care dependency may be a critical issue. Frail adults are at high risk for hospitalizations 52,71 and institutionalization 74. Frail adults are similarly at higher risk for death, which may be defined as the end of one's physical life on earth.
Synthesis
The FFVP is a framework which enables a greater understanding of unique antecedents which may be of significant issue to vulnerable populations. We believe that this framework extends to multiple populations; in this manuscript, we have drawn upon the homeless literature to apply the model itself. However, we similarly believe this is relevant among other vulnerable populations such as those incarcerated, rural populations, and those afflicted with HIV/AIDS.
Individual-level factors such as race/ethnicity, gender, income and education can influence situational factors (e.g. life events, parole/probation, foster home and homelessness). Further, life events (e.g. homelessness, incarceration, being on parole or probation) may similarly affect and be affected by behavioral factors which may include alcohol and illicit drug use-which have been empirically demonstrated to affect one another.
Behavioral factors may affect health-related factors and in consequence be affected by them. For vulnerable populations, chronic diseases and multi-morbid conditions affect health care utilization. Individuals who frequently live in shelters may not be able to manage chronic diseases. Equally important, increased stressors may similarly lead to generalized inflammation and oxidative stress. Immediate environmental factors may affect biological factors, health related factors, and situational factors. It is important to recognize that resource factors (e.g. coping, resilience and positive social support) aid in alleviating some of these factors. Frailty domains are interrelated; in particular, physical frailty and lack of mobility or strength may affect social frailty and lead to increased depressive states. Homeless populations can be socially isolated, which often predisposes them to serious health problems and while not studied and may exacerbate frailty. Hwang et al. (2009) studied multidimensional social support among homeless adults (N=544) and found that only seven percent of participants were able to be accompanied to a health care provider by a family or friend. Data reveal that this population may have high needs, however, a low amount of received social support57 all of which may have implications for healthcare.
Adverse events are predicted by frailty; in particular, behavioral factors, such as engaging in violence and having a history of incarceration may place one at greater risk for disability due to experience with fights, shootings, beatings, stabbings. These activities may lead to hospitalization and over the life span, lead to increased health care dependency and ultimately premature mortality. As a starting point, we believe that this model will be useful to help us to better understand frailty among vulnerable populations, identify unique frailty components, and unique antecedents in an effort to identify areas of intervention.
A Research-Driven Conceptual Framework and Application
As an exploratory model, the FFVP serves several purposes; first, it will help academicians move beyond overlapping concepts of frailty and vulnerability. In particular, not all homeless or vulnerable populations are frail; we believe that both are distinct concepts that place populations at greater risk for frailty and adverse outcomes. Second, the FFVP adapted framework will assist with identifying unique life span predictors which may place specific populations at greater risk for frailty which will encourage primary screening in an effort to identify worsening adverse events. For instance, if psychological and social frailty are both present; yet, physical frailty is not yet present; it may necessitate intervention in those areas to avoid adverse outcomes. In fact, for service agencies, it may be necessary to develop critical time point interventions which delay adverse events through screening. According to Bergman et al. (2004), development of interventions should be aimed at secondary prevention for chronic conditions. This can be equally true among vulnerable populations, but, it is important to move beyond screening, but rather chronic disease self-management.
The Potential for Clinical Application
This FFVP framework provides context and a foundation for service agencies and providers to identify areas of intervention and screen for frailty. In fact, it may delay the onset of adverse outcomes if clinicians and service providers can intervene. The following case study provides an exemplar:
Ms. Johnson is a 64-year-old woman who recently was released from county jail and has been in and out of homelessness for the last several years; she completed the eighth grade and has not had a job in the last decade. Currently, she is frequenting shelters in order to meet basic necessities which include food, water and clothing. She recently found out she has type II diabetes; however, the shelter which she sleeps in does not have the ability to dispense medications. She is the only remaining member of her family and does not indicate she has any close friends or relatives. Recently, she has been spending time in the emergency department because of her inability to move around.
Ms. Johnson has several risk factors which place her at greater risk for frailty and subsequent adverse events. Due to her parole conditions, cyclical homelessness and limited education and job skills, the inability to meet basic challenges encouraged both recidivism and problems reintegrating into society. Ms. Johnson's current diagnosis of type II diabetes presents further challenges with the need for her to learn to manage diet and exercise in a shelter which leaves little control over diet. For the clinician's plan of care, it is imperative that they work with the participant and understand the environmental challenges of managing care. Further, linking clients into social support networks, temporary and permanent housing is essential to allay adverse outcomes. Equally important, it is important to understand the reasons for cyclical patterns of incarceration and homelessness and assess causes with a greater understanding that this leads to adverse outcomes.
Proposed Opportunities for Testing Nursing Interventions
Although the FFVP is an exploratory model, some areas of intervention can be identified. For the academician, this model can serve as a roadmap to better understanding areas for interventions, identifying relevant interventions and testing interventions in order to identify ways in which to reduce frailty and subsequent adverse outcomes.
For clinicians and service providers, several opportunities for intervention may include identifying if someone is on parole or probation, at risk of homelessness or homeless, linking clients into housing and healthcare services. If behavioral factors are identified, it's important to encourage anger management classes, smoking reduction and cessation, and identify frequent users of health care services, reasons and causes of such utilization. In terms of comorbid and multi-morbid conditions, it is equally important to institute chronic disease self-management programs and understand the environmental challenges which create challenges for managing disease conditions. Further, for those with poor resources, it is important to understand the importance of teaching coping skills and encouraging positive social support networks. It is presumed that effective interventions would encompass health promotion, prevention, case management and wraparound health services.
The FFVP framework is designed to provide a greater understanding of how these intervening variables impact the health outcomes of vulnerable populations in order to develop effective interventions. The FFVP provide a context in order to implement frailty diagnostic criteria in clinics and community settings while designing cost effective nurse-led interventions which will reduce the progression of the syndrome.
Implications for Theory Testing and Advancement of Nursing Practice
For the discipline of nursing, understanding frailty among vulnerable populations is necessary in order to create and sustain targeted clinical interventions. As the vulnerable populations continue to age, it will become increasingly necessary to focus on identification of frailty. Research related to predictors, mediators and adverse outcomes of frailty among homeless adults are not well understood. Developing targeted interventions to prevent exacerbations of frailty necessitates a clear understanding of these antecedents and outcomes. Also, it is imperative not to assume that frailty is part of vulnerability and vice versa; not all vulnerable populations are frail.
Nurses are the vanguard of caring for vulnerable populations and this necessitates a need for awareness, particularly based on the unique needs of this graying population. As trusted healthcare clinicians, nurses will continue to care for chronic and episodically homeless older adults and otherwise vulnerable populations and experience the complexity of the population shift commensurate with a greater burden of disease. There is a need for further exploration and strategies to institute frailty prevention programs, efforts and greater services.
Acknowledgments
This work was supported by the National Institute of Health (NIH)/Nursing Research (NINR) T32 NR007077, University of California Los Angeles (UCLA) Dissertation Year Fellowship Award, and the University of California, Los Angeles Community Academic Partnership for Research in Aging (L.A. CAPRA) Center NIH Grant 1RC4AG038182-01. We acknowledge the support of Dr. Robert Gobbens in providing guidance with the review of the Frailty Framework among Homeless and Vulnerable Populations-A Life Course Perspective. We similarly thank the Los Angeles-based skid row homeless participants who inspired this framework based on their willingness to share of their time and experiences.
Contributor Information
Benissa E. Salem, Email: bsalem@sonnet.ucla.edu, University of California, Los Angeles School of Nursing.
Adeline Nyamathi, Email: anyamath@sonnet.ucla.edu, Associate Dean for International Research and Scholarly Activities, University of California, Los Angeles School of Nursing.
Linda R. Phillips, Email: lrphillips@sonnet.ucla.edu, University of California, Los Angeles School of Nursing.
Janet Mentes, Email: jmentes@sonnet.ucla.edu, University of California, Los Angeles School of Nursing.
Catherine Sarkisian, Email: csarkisian@mednet.ucla.edu, UCLA Division of Geriatrics, VA Greater Los Angeles Healthcare System, Geriatric Research Education Clinical Center (GRECC).
Lynn Brecht, Email: lbrecht@mednet.ucla.edu, UCLA School of Nursing.
References
- 1.United States Census. [Accessed June 23, 2012];National Population Projections Released 2008. 2008 http://www.census.gov/population/www/projections/summarytables.html.
- 2.Cohen CI, Sokolovsky J, Crane M. Aging, homelessness, and the law. International journal of law and psychiatry. 2001 Mar-Jun;24(2-3):167–181. doi: 10.1016/s0160-2527(01)00067-x. [DOI] [PubMed] [Google Scholar]
- 3.National Coalition for the Homeless. Homelessness among elderly persons. 2007 http://www.nationalhomeless.org/publications/facts/Elderly.pdf.
- 4.Los Angeles Services Housing Authority. 2011 Greater Los Angeles Homeless Count Report. 2011 [Google Scholar]
- 5.LAHSA LAHaSA. Greater Los Angeles Homeless Count: A Summary Report. Los Angeles: 2011. [Google Scholar]
- 6.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. The journals of gerontology. Series A, Biological sciences and medical sciences. 2007 Jul;62(7):722–727. doi: 10.1093/gerona/62.7.722. [DOI] [PubMed] [Google Scholar]
- 7.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clinics in geriatric medicine. 2011 Feb;27(1):17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nursing outlook. 2010 Mar-Apr;58(2):76–86. doi: 10.1016/j.outlook.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Towards an integral conceptual model of frailty. The journal of nutrition, health & aging. 2010 Mar;14(3):175–181. doi: 10.1007/s12603-010-0045-6. [DOI] [PubMed] [Google Scholar]
- 10.Aranda MP, Ray LA, Snih SA, Ottenbacher KJ, Markides KS. The protective effect of neighborhood composition on increasing frailty among older mexican americans: a barrio advantage? Journal of aging and health. 2011 Oct;23(7):1189–1217. doi: 10.1177/0898264311421961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric Syndromes in Older Homeless Adults. Journal of general internal medicine. 2011 Aug 31; doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergman H, Karunananthan S, Hummel S, Hogan D, Wolfson C. Developing a Working Framework for Understanding Frailty. Gérontologie et société. 2004;(109):15–29. [Google Scholar]
- 13.Flaskerud JH, Winslow BJ. Conceptualizing vulnerable populations health-related research. Nursing research. 1998 Mar-Apr;47(2):69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Fried, Walston . Frailty and Failure to Thrive. In: Hazzard WR, Blass JP, Halter JB, Ouslander JG, Tinetti ME, editors. Principles of Geriatric Medicine & Gerontology. 5. Vol. 5. New York: McGraw Hill; 2003. [Google Scholar]
- 15.Bergman H, Beland F, Karunananthan S, Hummel S, Hogan D, Wolfson C. Developing a Working Framework for Understanding Frailty. Gerontologie et societe. 2004;109:15–29. [Google Scholar]
- 16.Nyamathi A, Koniak-Griffin D, Greengold BA. Development of nursing theory and science in vulnerable populations research. Annu Rev Nurs Res. 2007;25:3–25. [PubMed] [Google Scholar]
- 17.Villareal DT, Banks M, Siener C, Sinacore DR, Klein S. Physical frailty and body composition in obese elderly men and women. Obes Res. 2004 Jun;12(6):913–920. doi: 10.1038/oby.2004.111. [DOI] [PubMed] [Google Scholar]
- 18.Wenzel SL, Koegel P, Gelberg L. Antecedents of physical and sexual victimization among homeless women: a comparison to homeless men. American journal of community psychology. 2000 Jun;28(3):367–390. doi: 10.1023/A:1005157405618. [DOI] [PubMed] [Google Scholar]
- 19.Mumola CJ, Karberg JC. Drug Use and Dependence, State and Federal Prisoners, 2004. United States: 2006. [Google Scholar]
- 20.Salem BE, Nyamathi A, Idemundia F, Slaughter R, Ames M. At a Crossroads: Reentry Challenges and Healthcare Needs Among Homeless Female Ex-Offenders. Journal of Forensic Nursing Journal of Forensic Nursing. 2013;9(1):14–22. doi: 10.1097/jfn.0b013e31827a1e9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed N, Mandel R, Fain MJ. Frailty: an emerging geriatric syndrome. The American journal of medicine. 2007 Sep;120(9):748–753. doi: 10.1016/j.amjmed.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 22.Lang IA, Hubbard RE, Andrew MK, Llewellyn DJ, Melzer D, Rockwood K. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. Journal of the American Geriatrics Society. 2009 Oct;57(10):1776–1780. doi: 10.1111/j.1532-5415.2009.02480.x. [DOI] [PubMed] [Google Scholar]
- 23.Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women's Health Initiative Observational Study. J Am Geriatr Soc. 2005 Aug;53(8):1321–1330. doi: 10.1111/j.1532-5415.2005.53405.x. [DOI] [PubMed] [Google Scholar]
- 24.Cawthon PM, Marshall LM, Michael Y, et al. Frailty in Older Men: Prevalence, Progression, and Relationship with Mortality. Journal of the American Geriatrics Society. 2007;55(8):1216–1223. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- 25.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001 Mar;56(3):M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 26.Shi L, Stevens GD. Vulnerable populations in the United States. 2005 http://www.netlibrary.com/urlapi.asp?action=summary&v=1&bookid=124337.
- 27.Fried L, Tangen C, Walston J, et al. Frailty in older adults: evidence for a phenotype. The journals of gerontology Series A, Biological sciences and medical sciences. 2001 Mar;56(3):M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 28.Riley ED, Weiser SD, Sorensen JL, Dilworth S, Cohen J, Neilands TB. Housing patterns and correlates of homelessness differ by gender among individuals using San Francisco free food programs. Journal of urban health : bulletin of the New York Academy of Medicine. 2007 May;84(3):415–422. doi: 10.1007/s11524-006-9153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alvarado BE, Zunzunegui MV, Beland F, Bamvita JM. Life course social and health conditions linked to frailty in Latin American older men and women. The journals of gerontology Series A, Biological sciences and medical sciences. 2008 Dec;63(12):1399–1406. doi: 10.1093/gerona/63.12.1399. [DOI] [PubMed] [Google Scholar]
- 30.California Department of Corrections and Rehabilitation. Parolee Conditions. 2012 http://www.cdcr.ca.gov/Parole/Parolee_Conditions/index.html.
- 31.Garner BA, Black HC. Black's law dictionary. St. Paul, MN: Thomson Reuters; 2011. [Google Scholar]
- 32.Butler T, Kariminia A. Prison violence: perspectives and epidemiology. New South Wales public health bulletin. 2006 Jan-Feb;17(1-2):17–20. doi: 10.1071/nb06005. [DOI] [PubMed] [Google Scholar]
- 33.Lahm KF. Inmate-On-Inmate Assault: A Multilevel Examination of Prison Violence. Criminal justice and behavior. 2008 Jan 1;35(1):120–137. 2008. [Google Scholar]
- 34.Richters J, Butler T, Schneider K, et al. Consensual sex between men and sexual violence in Australian prisons. Archives of sexual behavior. 2012 Apr;41(2):517–524. doi: 10.1007/s10508-010-9667-3. [DOI] [PubMed] [Google Scholar]
- 35.Garibaldi B, Conde-Martel A, O'Toole TP. Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. Journal of general internal medicine. 2005 Aug;20(8):726–730. doi: 10.1111/j.1525-1497.2005.0142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilhelm-Leen ER, Hall YN, M KT, Chertow GM. Frailty and chronic kidney disease: the Third National Health and Nutrition Evaluation Survey. The American journal of medicine. 2009 Jul;122(7):664–671. 662. doi: 10.1016/j.amjmed.2009.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cacciatore F, Testa G, Galizia G, et al. Clinical frailty and long-term mortality in elderly subjects with diabetes. Acta diabetologica. 2012 Jun 26; doi: 10.1007/s00592-012-0413-2. [DOI] [PubMed] [Google Scholar]
- 38.Boyle PA, Buchman AS, Wilson RS, Leurgans SE, Bennett DA. Physical frailty is associated with incident mild cognitive impairment in community-based older persons. Journal of the American Geriatrics Society. 2010 Feb;58(2):248–255. doi: 10.1111/j.1532-5415.2009.02671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boyle PA, Wilson RS, Buchman AS, et al. Lower extremity motor function and disability in mild cognitive impairment. Experimental aging research. 2007 Jul-Sep;33(3):355–371. doi: 10.1080/03610730701319210. [DOI] [PubMed] [Google Scholar]
- 40.Ni Mhaolain AM, Gallagher D, Crosby L, et al. Correlates of frailty in Alzheimer's disease and mild cognitive impairment. Age and ageing. 2011 Sep;40(5):630–633. doi: 10.1093/ageing/afr066. [DOI] [PubMed] [Google Scholar]
- 41.Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. The journals of gerontology Series A, Biological sciences and medical sciences. 2010 Apr;65(4):377–381. doi: 10.1093/gerona/glp186. [DOI] [PubMed] [Google Scholar]
- 42.Shah K, Hilton TN, Myers L, Pinto JF, Luque AE, Hall WJ. A new frailty syndrome: central obesity and frailty in older adults with the human immunodeficiency virus. Journal of the American Geriatrics Society. 2012 Mar;60(3):545–549. doi: 10.1111/j.1532-5415.2011.03819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piggott DA, Muzaale AD, Mehta SH, et al. Frailty, HIV infection, and mortality in an aging cohort of injection drug users. PloS one. 2013;8(1):e54910. doi: 10.1371/journal.pone.0054910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Langnase K, Muller MJ. Nutrition and health in an adult urban homeless population in Germany. Public health nutrition Jun. 2001 Jun;4(3):805–811. doi: 10.1079/phn2000119. [DOI] [PubMed] [Google Scholar]
- 45.Vandewoude MF, Alish CJ, Sauer AC, Hegazi RA. Malnutrition-sarcopenia syndrome: is this the future of nutrition screening and assessment for older adults? Journal of aging research. 2012;2012:651570. doi: 10.1155/2012/651570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lehne RA. Pharmacology for nursing care. St Louis, Mo: Saunders Elsevier; 2007. [Google Scholar]
- 47.Gomez R, Thompson SJ, Barczyk AN. Factors associated with substance use among homeless young adults. Substance abuse : official publication of the Association for Medical Education and Research in Substance Abuse. 2010 Jan;31(1):24–34. doi: 10.1080/08897070903442566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nyamathi AM, Leake B, Gelberg L. Sheltered versus nonsheltered homeless women differences in health, behavior, victimization, and utilization of care. Journal of general internal medicine. 2000 Aug;15(8):565–572. doi: 10.1046/j.1525-1497.2000.07007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hubbard RE, Searle SD, Mitnitski A, Rockwood K. Effect of smoking on the accumulation of deficits, frailty and survival in older adults: a secondary analysis from the Canadian Study of Health and Aging. The journal of nutrition, health & aging. 2009 May;13(5):468–472. doi: 10.1007/s12603-009-0085-y. [DOI] [PubMed] [Google Scholar]
- 50.Goldade K, Whembolua GL, Thomas J, et al. Designing a smoking cessation intervention for the unique needs of homeless persons: a community-based randomized clinical trial. Clinical trials. 2011 Dec;8(6):744–754. doi: 10.1177/1740774511423947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsai J, Rosenheck RA. Smoking among chronically homeless adults: prevalence and correlates. Psychiatric services. 2012 Jun;63(6):569–576. doi: 10.1176/appi.ps.201100398. [DOI] [PubMed] [Google Scholar]
- 52.Hoeck S, Francois G, Geerts J, Van der Heyden J, Vandewoude M, Van Hal G. Health-care and home-care utilization among frail elderly persons in Belgium. European journal of public health. 2012 Oct;22(5):671–677. doi: 10.1093/eurpub/ckr133. [DOI] [PubMed] [Google Scholar]
- 53.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. Journal of general internal medicine. 2006 Jul;21(7):775–778. doi: 10.1111/j.1525-1497.2006.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Andersen Behavioral Model for Vulnerable Populations. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2012 Jan;31(1):20–30. doi: 10.1037/a0023643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cleverley K, Kidd SA. Resilience and suicidality among homeless youth. Journal of adolescence. 2011 Oct;34(5):1049–1054. doi: 10.1016/j.adolescence.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 56.Lam JA, Rosenheck R. Social support and service use among homeless persons with serious mental illness. The International journal of social psychiatry Spring. 1999;45(1):13–28. doi: 10.1177/002076409904500103. [DOI] [PubMed] [Google Scholar]
- 57.Hwang SW, Kirst MJ, Chiu S, et al. Multidimensional social support and the health of homeless individuals. Journal of urban health : bulletin of the New York Academy of Medicine. 2009 Sep;86(5):791–803. doi: 10.1007/s11524-009-9388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nyamathi A, Stein JA, Brecht ML. Psychosocial predictors of AIDS risk behavior and drug use behavior in homeless and drug addicted women of color. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1995 May;14(3):265–273. doi: 10.1037//0278-6133.14.3.265. [DOI] [PubMed] [Google Scholar]
- 59.Unger JB, Kipke MD, Simon TR, Johnson CJ, Montgomery SB, Iverson E. Stress, Coping, and Social Support among Homeless Youth. Journal of Adolescent Research Journal of Adolescent Research. 1998;13(2):134–157. [Google Scholar]
- 60.Woo J, Tang NL, Suen E, Leung JC, Leung PC. Telomeres and frailty. Mechanisms of ageing and development. 2008 Nov;129(11):642–648. doi: 10.1016/j.mad.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 61.DeGuzman PB, Kulbok PA. Changing Health Outcomes of Vulnerable Populations Through Nursing's Influence on Neighborhood Built Environment: A Framework for Nursing Research. Journal of Nursing Scholarship. 2012;44(4):341–348. doi: 10.1111/j.1547-5069.2012.01470.x. [DOI] [PubMed] [Google Scholar]
- 62.Heath GW, Troped PJ. The role of the built environment in shaping the health behaviors of physical activity and healthy eating for cardiovascular health. Future Cardiol Future Cardiology. 2012;8(5):677–679. doi: 10.2217/fca.12.52. [DOI] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention. [Accessed November 1, 2011];Hepatitis A Information for Health Professionals. 2012 http://www.cdc.gov/hepatitis/HAV/index.htm.
- 64.United States Health and Human Services National Digestive Diseases Information Clearinghouse. [Accessed October 1, 2010];What I need to know about Hepatitis A 2012. 2012 Oct 1; http://digestive.niddk.nih.gov/ddiseases/pubs/hepa_ez/
- 65.Syddall H, Cooper C, Martin F, Briggs R, Aihie Sayer A. Is grip strength a useful single marker of frailty? Age and ageing. 2003 Nov;32(6):650–656. doi: 10.1093/ageing/afg111. [DOI] [PubMed] [Google Scholar]
- 66.Cano C, Samper-Ternent R, Al Snih S, Markides K, Ottenbacher KJ. Frailty and cognitive impairment as predictors of mortality in older Mexican Americans. The journal of nutrition, health & aging. 2012 Feb;16(2):142–147. doi: 10.1007/s12603-011-0104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.AM NM, Gallagher D, Crosby L, et al. Correlates of frailty in Alzheimer's disease and mild cognitive impairment. Age and ageing. 2011;40(5):630–633. doi: 10.1093/ageing/afr066. [DOI] [PubMed] [Google Scholar]
- 68.Woo J, Goggins W, Sham A, Ho SC. Social determinants of frailty. Gerontology. 2005 Nov-Dec;51(6):402–408. doi: 10.1159/000088705. [DOI] [PubMed] [Google Scholar]
- 69.Act AwD, editor. Americans with Disabilities Act. Public Law 101-336: Americans with Disabilities Act of 1990 (as amended) Washington D.C: 1990. pp. 101–336. [Google Scholar]
- 70.Fried, Ferrucci, Darer, Williamson, Anderson Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. The journals of gerontology Series A, Biological sciences and medical sciences. 2004 Mar;59(3):255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 71.Fried TR, Mor V. Frailty and hospitalization of long-term stay nursing home residents. Journal of the American Geriatrics Society. 1997 Mar;45(3):265–269. doi: 10.1111/j.1532-5415.1997.tb00938.x. [DOI] [PubMed] [Google Scholar]
- 72.Puts MT, Lips P, Deeg DJ. Sex differences in the risk of frailty for mortality independent of disability and chronic diseases. Journal of the American Geriatrics Society. 2005 Jan;53(1):40–47. doi: 10.1111/j.1532-5415.2005.53008.x. [DOI] [PubMed] [Google Scholar]
- 73.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA : the journal of the American Medical Association. 2001 Jan 10;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 74.Puts ME, Lips P, Ribbe M, Deeg DH. The effect of frailty on residential/nursing home admission in the Netherlands independent of chronic diseases and functional limitations. Eur J Ageing. 2005 Dec 01;2(4):264–274. doi: 10.1007/s10433-005-0011-z. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]


