Abstract
OBJECTIVES
This study determined whether insufficient help for ADL disability, a potentially modifiable condition, significantly increases activities of daily living (ADL) disabled older adults’ risk for future hospital admissions.
DESIGN
Prospective study.
SETTING
ADL disabled community living participants of the 1994, 1999, and/or 2004 National Long-term Care Survey (NLTCS).
PARTICIPANTS
5,884surveys were completed by Medicare recipients with one or more ADL disabilities.
MEASUREMENTS
Times to hospital admission in the year after the NLTCS community survey were obtained from linked Medicare claims. Insufficient ADL help for each ADL limitation was determined from a series of questions that were common to the three NLTCS community surveys.
RESULTS
Insufficient help for one or more ADL limitations was reported in 22% of surveys. Respondents to 3,629 surveys did not experience a hospital admission in the year after the survey. Among the remaining 2,255surveys, one admission occurred for 382 surveys, two admissions for 525 surveys, three admissions for 193 surveys, and four or more admissions for 155 surveys. Those reporting insufficient help were 14% (HR=1.14; 95% CI=1.01–1.28) more likely to experience one or more hospitalizations than those who do not report insufficient help after controlling for demographics, co-morbidities, prior hospitalizations and level of ADL disability.
CONCLUSION
Self-reports of insufficient help provide prognostic information beyond that which can be captured by typical health assessments. Greater recognition and referral for insufficient help for ADL disability may result in reduced rates of hospitalization in a population that is already at high risk for hospitalization.
Keywords: activities of daily living, disability, hospitalization, insufficient help
INTRODUCTION
More than 6.5 million older Medicare recipients have disability in one or more activities of daily living (ADL) such as toileting, bathing, dressing, transferring, and eating.1ADL disability is associated with higher rates of health care utilization including hospitalization; 14% of Medicare recipients with no ADL disabilities experience one or more hospitalizations per year compared to 34% of those with one or more ADL disabilities.1 Hospitalization among ADL disabled older adults is associated with worsening ADL disability,2 nursing home placement,3 and death.4 The success of interventions to reduce hospitalization and associated negative outcomes requires the recognition of factors that increase the risk of hospital admissions among ADL dependent older adults.
Nearly 20% of community-living disabled adults report a lack of sufficient assistance for their disabilities.5–7 Those with insufficient help report that they experienced falls, injuries, skin and muscle discomfort as a result of insufficient ADL help.8 These consequences suggest that some ADL disabled older adults experience suffering that is beyond that which can be attributed to disability alone. Another possible consequence of insufficient help is the need for additional health services, particularly hospitalization. ADL disabled older adults are already at high risk for hospitalization due to common risks for disability and hospitalization such as co-morbidity, low functioning, and poor social support9,10 Insufficient ADL help is a potentially modifiable condition. Determining whether it increases risk of future hospitalizations would inform the importance of investing in interventions to reduce insufficient ADL help.
The purpose of this study is to evaluate whether self-reports of insufficient ADL help are associated with increased risk of hospital admission after statistically controlling for commonly used and validated indicators of risk for hospital admission.11 Data for this study are from the National Long-term Care Survey (NLTCS), a study of randomly selected aged Medicare enrollees that began in 1982 to assess trends in the health and functioning and care giving resources of older adults. Linked Medicare data allows tracking of hospital admissions. This study will include data from the 1994, 1999, and 2004 surveys of community-living respondents. Findings will informclinicians whether self-reports of insufficient help provide prognostic information beyond that which can be captured by typical health assessments. Findings will also inform policy makers about potential costly consequences of programmatic cuts that result in older adults living with insufficient care for their ADL disabilities.12
METHODS
Data Source and Study Sample
Data are from the 1994, 1999, and 2004 community components of the National Long Term Care Survey (NLTCS) and linked Medicare and vital statistics data provided by the Centers for Medicare and Medicaid Services (CMS). The NLTCS samples were randomly selected from Medicare enrollees who were aged 65 years or older and living in the community in non-institutional housing. Approximately half of the respondents at each wave of the survey participated in an earlier wave. The NLTCS replenishes the sample by adding an “aged-in” sample of Medicare enrollees who turned 65 since the last survey and a “95+ supplement” sample who are 95 years or older and were not selected in any previous surveys. Therefore, each occasion includes new subjects. The NLTCS community survey data were collected by trained interviewers from the U.S. Census Bureau. Response rates to the community surveys were 95% or higher for the 1994 and 1999 waves and approximately 90% for the 2004 wave. Our study sample includes persons who had at least one ADL disability at the time of their community interview.
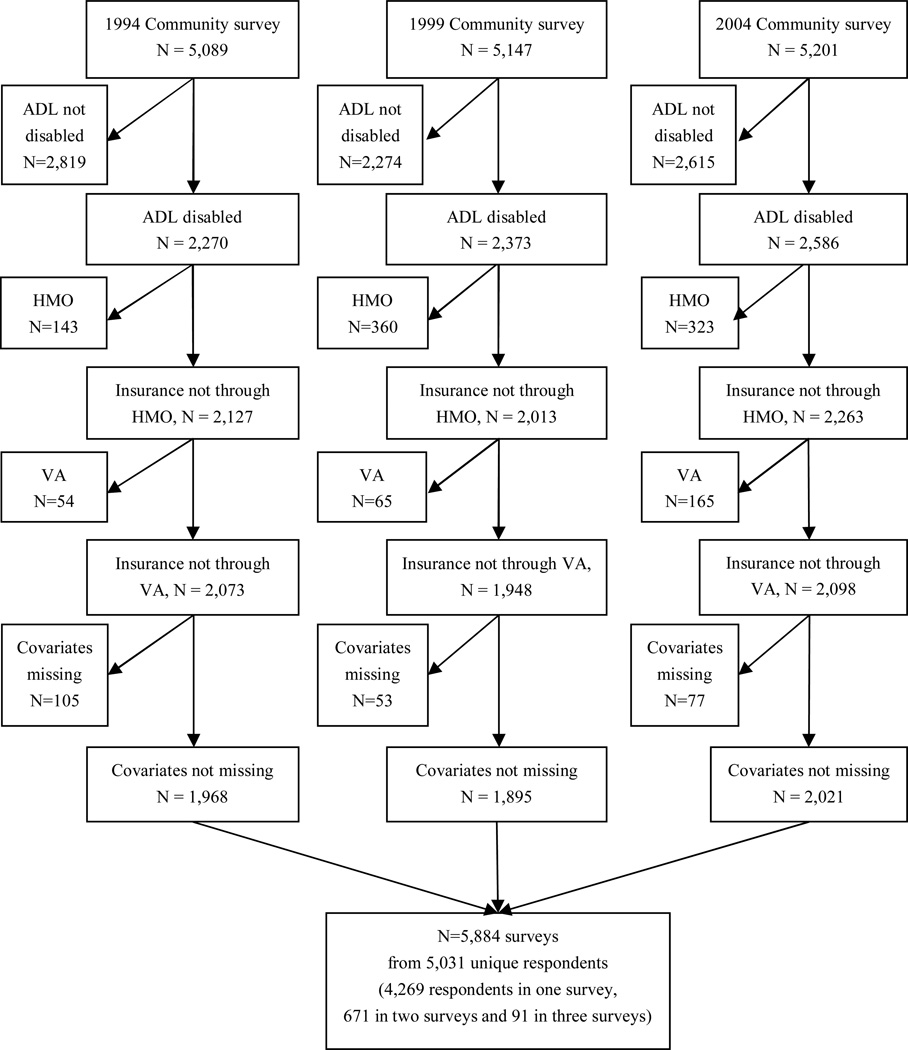
Among the 5,089 respondents in the 1994 community survey, 2,270 had at least one limitation in ADL functioning. Of these, 143 received insurance coverage through a Health Maintenance Organization (HMO) and 54 received medical coverage through insurance for dependents or survivors of military personnel and disabled veterans (VA) in the year following the interview. Respondents with HMO or VA medical insurance were not included in the analytic sample due to the potential that some hospital admissions not covered by Medicare would not be reported to Medicare. An additional 105 respondents were excluded due to missing values on at least one of the covariates. This resulted in 1,968 respondents from the 1994 survey in the final analytic sample. Similarly, we obtained 1,895 respondents from the 1999 survey and 2,021 respondents from the 2004 survey. Respondents excluded from the sample were more likely to have heart disease, cognitive impairment, and a proxy. The final analytic sample contained a total of 5,884 surveys from the 1994, 1999, and 2004 NLTCS. Some subjects who participated in more than one survey met inclusion criteria for the analytic sample in more than one survey. The 5,884 surveys included in the study were from 5,031 unique respondents. A total of 4,269 respondents were in one survey, 671 in two surveys, and 91 in three surveys. Details of the analytic sample derivation are shown in Figure 1.
Figure 1.
Sample source
Measures
Hospital Admissions
The outcome of interest was time to hospital admission in the year since the community survey. Admission records were obtained from Medicare claims data. Observations were right-censored at the time of death or at the end of 2005.
Insufficient ADL help
Insufficient ADL help was determined from a series of questions that were common to the 1994, 1999, and 2004 community surveys. For each ADL task respondents were asked whether they received help from another person or used equipment. If the response was yes, respondents were then asked whether they needed more human help or had to wait to do the task because the respondent did not have enough human help. If the respondent said yes, then the respondent was designated as having insufficient ADL help. If the respondent did not receive human help, but had a person who stayed nearby in case the respondent needed help, they were asked whether they could have used more help or had to wait to do the task because they did not have enough help. If the response was yes, then the person was classified as having insufficient ADL care. For each ADL task for which respondents said they did not have any direct or stand by help, they were asked if they could have used human help for that task. Those who responded positively were also designated as having insufficient ADL help for that task. This definition is similar to prior studies of unmet need for ADL disabilities.6–8, 13, 14
Covariates
Demographic variables included gender, age (65–74, or 75 or more), race (white or other), marital status (married or other), and living arrangements (alone or not alone). The presence of co-morbid conditions was determined from respondents’ reports of whether or not they currently had any of the following medical conditions: arthritis, diabetes, or cancer. They were also asked if they experienced any of the following in the twelve months prior to the interview: heart disease, a heart attack or other heart problems, a stroke, or emphysema. Whether or not the respondent experienced a hospitalization admission in the prior 12 months was determined through the survey data, as well as the linked Medicare inpatient claims data. Cognitive impairment was determined from respondents’ answers to mental status screens. In 1994 and 2004 the Short Portable Mental Status Questionnaire (SPMSQ) was administered to subjects, but in 1999 the Mini-Mental State Exam (MMSE) was used. Those who had dementia, a SPMSQ score of 3 or above, an MMSE score of 23 or below, or were mentally incapable of completing the mental status screen were considered to have cognitive impairment.15, 16 Subjects without data for any of the variables used to determine cognitive impairment were coded as missing. The presence of ADL disability was determined through a series of questions that were common to the 1994, 1999, and 2004 surveys. For each ADL task (bathing, dressing eating, toileting, and transferring from a bed or around a room), a respondent was considered to have ADL disability if they received help to complete the task, received stand by help, did not receive help for the task, but stated they needed help to complete the task, or required the use of equipment to complete the task. Those who required the use of equipment to complete ADL tasks were designated as having ADL disability because equipment use for ADL tasks reduces need for human assistance17 and reports of insufficient ADL help, the primary independent variable in this study.18
Statistical Analyses
Rates of hospitalization were computed as the total number of hospital admissions divided by total person-years. For the multivariate analysis, we used the survival analysis model proposed by Andersen and Gill (AG)19 to examine the effect of insufficient ADL help on risk of hospital admissions. This model is an extension of the Cox proportional hazards model for recurrent event data. The traditional Cox proportional hazards model is not used because multiple hospital admissions clustered within a subject are correlated. The AG model is a marginal model in which the dependence between multiple event times within a subject is accounted for by adjusting the standard error estimates using the robust sand wich variance estimators. In analysis of non-survey data, simulation studies have shown that the AG model with sand wich variance estimators provides more efficient inference and gives more reliable parameter estimates compared to other marginal approaches.20 For analysis of complex survey data, weighted sandwich variance estimators are used to provide valid standard errors.21 The AG model also accommodates discontinuous risk intervals. The risk intervals in our analysis are discontinuous because when subjects are hospitalized they are not at risk of another hospitalization until they have been discharged. Therefore the duration of the hospitalization must be excluded from the risk set.22
All results were weighted using the NLTCS survey weights that reflectrespondents’ probability of inclusion in the sample. Standard errors for rates of hospitalizations were adjusted for the complex survey sampling design using the Taylor series linearization approach (found in the SAS survey procedure SURVEYMEANS). For the AG model the standard errors based on the Taylor series linearization approach and the weighted sandwich variance estimation approach proposed by Binder (1992) are approximately equal when the sampling fraction from the population is small and the sample size is large relative to the number of parameters. To obtain design consistent parameter estimates we used the SAS procedure PROC PHREG with weights and applied the weighted sandwich variance estimation to obtain standard errors. All statistical analyses were performed with SAS 9.
RESULTS
The average follow-up period of the 5,884 surveys was 333.2 days with a standard deviation of 76.5 days. Hospitalization did not occur in the follow-up period of 3,629 surveys. In the follow-up period of the remaining 2,255 surveys, there were a total of 3,742 hospital admissions. Exactly one admission occurred for 382 surveys, two admissions for 525 surveys, three admissions for 193 surveys, and four or more admissions for 155 surveys.
Table 1 shows the unweighted and weighted sample characteristics. Most of the sample was aged 75 or older, female, and white. Nearly forty percent lived alone and 29% had a proxy respondent. Self-reports of medical conditions revealed that 74% had arthritis, 24% had diabetes, 8% had cancer, 39% had heart disease, 11% had experienced a stroke, and 8% had emphysema. Forty-one percent had experienced a hospital admission in the prior year and 27% had cognitive impairment. Nearly a third had one ADL dependency, half had 2–4 ADL dependencies, and 14% had 5 ADL dependencies. Twenty-two percent reported insufficient help for one or more ADL disabilities.
Table 1.
Sample characteristics at the time of the community interview among NLTCS community respondents with ADL disability
| N | Percent | ||
|---|---|---|---|
| Unweighted | Weighted | ||
| Age | |||
| Less than 75 years | 1166 | 19.8 | 28.8 |
| 75+ years | 4718 | 80.2 | 71.2 |
| Gender | |||
| Female | 4329 | 73.6 | 71.9 |
| Male | 1555 | 26.4 | 28.1 |
| Race | |||
| White | 5104 | 86.7 | 84.9 |
| Other | 780 | 13.3 | 15.1 |
| Living arrangement | |||
| Alone | 2429 | 41.3 | 38.9 |
| Not alone | 3455 | 58.7 | 61.1 |
| Marital status | |||
| Married | 1887 | 32.1 | 35.1 |
| Other | 3997 | 67.9 | 64.9 |
| Proxy | |||
| No | 4068 | 69.1 | 70.7 |
| Yes | 1816 | 30.9 | 29.3 |
| Arthritis | |||
| No | 1538 | 26.1 | 25.8 |
| Yes | 4346 | 73.9 | 74.2 |
| Diabetes | |||
| No | 4623 | 78.6 | 76.0 |
| Yes | 1261 | 21.4 | 24.0 |
| Cancer | |||
| No | 5396 | 91.7 | 91.6 |
| Yes | 488 | 8.3 | 8.4 |
| Heart disease | |||
| No | 3595 | 61.1 | 61.2 |
| Yes | 2289 | 38.9 | 38.8 |
| Stroke | |||
| No | 5259 | 89.4 | 88.8 |
| Yes | 625 | 10.6 | 11.2 |
| Emphysema | |||
| No | 5444 | 92.5 | 91.8 |
| Yes | 440 | 7.5 | 8.2 |
| Hospital admission in prior 12 months | |||
| No | 3495 | 59.4 | 58.7 |
| Yes | 2389 | 40.6 | 41.3 |
| Cognitive Status | |||
| Normal | 3023 | 51.4 | 52.4 |
| Impaired | 1633 | 27.7 | 26.6 |
| Missing | 1228 | 20.9 | 21.0 |
| Number of ADL s with limitations | |||
| 1 | 1846 | 31.4 | 32.2 |
| 2–4 | 3189 | 54.2 | 53.6 |
| 5 | 849 | 14.4 | 14.2 |
| Lack of sufficient ADL help | |||
| No | 4651 | 79.0 | 78.3 |
| Yes | 1233 | 21.0 | 21.7 |
Table 2 shows the bivariate associations between the risk factors and hospital admissions during the 12 months after the community interview. Those at higher risk for hospital admissions were males, those who had a proxy respondent, and those with diabetes, cancer, heart disease, a stroke, or emphysema. Respondents who were hospitalized in the 12 months prior to the interview were twice as likely to be hospitalized in the 12 months following the interview. Those with cognitive impairment or who had missing cognitive data were more likely to be hospitalized. Greater numbers of ADL dependencies were associated with higher risks of hospitalization. The rate of hospitalization for those who reported insufficient help was significantly higher (0.85) than for those who did not report insufficient help (0.66; HR=1.30; 95% CI=1.16–1.46).
Table 2.
Bivariate association between risk factors and hospital admissions during 12 months after the community interview among NLTCS community respondents with ADL disability
| Rate* (per person year) |
Hazard Ratio (95% Confidence Interval) |
|
|---|---|---|
| Overall sample | 0.699 | |
| Age | ||
| Less than 75 years | 0.664 | 1.00 |
| 75+ years | 0.713 | 1.08 (0.95 – 1.22) |
| Gender | ||
| Female | 0.661 | 1.00 |
| Male | 0.803 | 1.22 (1.10 – 1.36) |
| Race | ||
| White | 0.689 | 0.91 (0.78 – 1.05) |
| Other | 0.757 | 1.00 |
| Living arrangement | ||
| Alone | 0.700 | 1.00 (0.91 – 1.11) |
| Not alone | 0.698 | 1.00 |
| Marital status | ||
| Married | 0.671 | 0.94 (0.85 – 1.04) |
| Other | 0.714 | 1.00 |
| Proxy | ||
| No | 0.656 | 1.00 |
| Yes | 0.810 | 1.24 (1.12 – 1.38) |
| Arthritis | ||
| No | 0.705 | 1.00 |
| Yes | 0.697 | 0.99 (0.88 – 1.11) |
| Diabetes | ||
| No | 0.621 | 1.00 |
| Yes | 0.949 | 1.54 (1.38 – 1.72) |
| Cancer | ||
| No | 0.677 | 1.00 |
| Yes | 0.968 | 1.44 (1.22 – 1.69) |
| Heart disease | ||
| No | 0.594 | 1.00 |
| Yes | 0.871 | 1.47 (1.33 – 1.63) |
| Stroke | ||
| No | 0.682 | 1.00 |
| Yes | 0.838 | 1.24 (1.07 – 1.43) |
| Emphysema | ||
| No | 0.667 | 1.00 |
| Yes | 1.080 | 1.63 (1.39 – 1.92) |
| Hospital admission in prior 12 months | ||
| No | 0.497 | 1.00 |
| Yes | 1.001 | 2.04 (1.85 – 2.25) |
| Cognitive Status | ||
| Normal | 0.619 | 1.00 |
| Impaired | 0.760 | 1.23 (1.10 – 1.39) |
| Missing | 0.831 | 1.35 (1.19 – 1.53) |
| Number of ADL s with limitations | ||
| 1 | 0.574 | 1.00 |
| 2–4 | 0.745 | 1.31 (1.17 – 1.47) |
| 5 | 0.825 | 1.45 (1.24 – 1.69) |
| Lack of sufficient ADL help | ||
| No | 0.659 | 1.00 |
| Yes | 0.850 | 1.30 (1.16 – 1.46) |
Hospitalization rates were calculated by dividing the total number of hospital admissions in the follow-up period by the total years of follow-up
Table 3 shows that self-reports of insufficient ADL help are prognostic of subsequent hospital admissions after statistically controlling for known risks for development of ADL disability and hospital admission. The results reveal that those reporting insufficient help are 14% (HR=1.14; 95% CI=1.01–1.28) more likely to be hospitalized than those who do not report insufficient help.
Table 3.
Results of the multivariate analysis of risk of hospitalization admission
| Hazard Ratio (95% Confidence Interval) |
P-value | |
|---|---|---|
| Age: 75+ years | 1.15 (1.01 – 1.30) | 0.034 |
| Gender: Male | 1.20 (1.07 – 1.34) | 0.003 |
| Race: White | 0.97 (0.84 – 1.11) | 0.625 |
| Living alone | 1.05 (0.94 – 1.18) | 0.396 |
| Married | 0.87 (0.77 – 0.99) | 0.033 |
| Proxy | 1.06 (0.93 – 1.21) | 0.376 |
| Arthritis | 0.99 (0.89 – 1.11) | 0.923 |
| Diabetes | 1.44 (1.29 – 1.61) | <0.001 |
| Cancer | 1.23 (1.05 – 1.44) | 0.012 |
| Heart disease | 1.23 (1.11 – 1.36) | <0.001 |
| Stroke | 0.95 (0.82 – 1.10) | 0.460 |
| Emphysema | 1.46 (1.24 – 1.72) | <0.001 |
| Hospital admission in prior 12 months | 1.81 (1.63 – 2.00) | <0.001 |
| Cognitive status: impaired | 1.15 (1.03 – 1.29) | 0.025 |
| Cognitive status: missing | 1.26 (1.10 – 1.45) | 0.001 |
| Number of ADLs with limitation: 2–4 | 1.15 (1.03 – 1.29) | 0.012 |
| Number of ADLs with limitation: 5 | 1.16 (0.98 – 1.38) | 0.078 |
| Lack of sufficient ADL help | 1.14 (1.01 – 1.28) | 0.034 |
DISCUSSION
Insufficient help for ADL disabilities is associated with increased risk of hospital admission after controlling for commonly reported risks for hospitalization such as advanced age, co-morbidities, disabilities and recent admissions. One in five subjects reported insufficient help for one or more ADL disabilities, a percent similar to that reported by other studies.6, 7 Although insufficient ADL help is common, many clinicians are uninformed about whether their patients have sufficient care for their ADL disabilities.23 Insufficient care can occur among recipients who have either informal care from family or friends, paid formal care, or both.24 Thus, it is important that clinicians directly query older adults about whether their ADL needs are met. Improved recognition of unmet ADL needs may result in referral to resources that help older adults with their daily care activities.
Home-based formal services have the potential to reduce insufficient ADL care, but only a third of disabled community-living older adults use home based services.25 The most common reasons disabled older adults do not use formal home based services are: 1)they are not aware of the services, 2) the services are not available in their area, or 3) they can’t afford the services.25 Recent evidence suggests that providing resources for consumer-directed, home-based, formal ADL care may reduce reports of insufficient help for ADL limitations. Studies of Cash and Counseling reveal that when clients direct their own home care they receive significantly more paid care and are significantly less likely to report unmet need for ADL limitations.26 Future work is needed to determine whether other home-based interventions that provide resources for needed ADL care also reduce cases of insufficient help.
Compared to a blunt indicator of presence versus absence of ADL help, self-reports of insufficient help are subjective assessments that are likely to be informed by patients’ collective appraisal of such things as the timeliness, quality, and amount of ADL care received. Subjective assessments are increasingly being used in clinical settings because they reflect a patient-centered approach in which patients are viewed as the ultimate arbiter of their health related needs. Validated guidelines for determining how much personal care is needed by adults with ADL disabilities do not exist. This is likely because such estimates would be extremely complex to calculate given the many interrelated physiologic and social factors that contribute to need for ADL help. In the absence of such guidelines, self-assessments of insufficient help fill a void in assessing whether patients’ ADL needs are met. Such assessments could be done by nonclinical office staff. The clinical utility of such an assessment is that it may help identify patients at risk for hospitalization who might benefit from referral for more extensive assessments of their long-term care needs.27
Prior studies have provided evidence that poor social support is associated with a greater risk of hospital admission among older adults. However, prior studies have used broad indicators of social support such as being unmarried,11 living alone,10 and an indicator of social condition that included marital status and availability of a caregiver.28 These broad indicators do not inform whether an ADL impaired individual has the help needed to complete daily activities. Results from this study reveal that insufficient help provides information about risk for hospitalization that cannot be captured by broad indicators of social support such as being married or living alone. A limitation of this study is that we cannot describe the mechanism by which insufficient ADL help increases risk for future hospitalization. Prior research suggests that insufficient help may contribute to hospital risk directly through immediate consequences such as falls or skin breakdown,8 or indirectly by reducing the likelihood of completing self-care guidelines for chronic conditions.29 Although it is beyond the scope of this study to determine the mechanism by which insufficient ADL help contributes to future hospitalization, the findings provide evidence that clinical assessments of patients’ social support should include determination of whether patients have sufficient ADL help.
The findings of the study must be considered in the context of its limitations. One limitation of this study is that the results are generalizable only to those older adults who reported needing human help or equipment to complete ADL tasks. Consequently, we may have missed cases of insufficient help among subjects who found performing an ADL task difficult even though they did not need human help or equipment to complete the task. Another limitation of the study is that we did not have data to describe why respondents and proxies reported insufficient help, nor could we determine whether respondents and proxies differed in their reasons for reporting insufficient ADL help. However, the association between insufficient help and future hospitalization was similar when proxies were excluded. Further, we used self-reports of chronic conditions and an indicator of hospital admission in the prior year to control for illness status; we recognize this method may not have controlled for all variance in hospital use that is attributable to illness status. Also, we were not able to determine how long the respondent had been experiencing insufficient help. If insufficient help were a long-standing condition it is possible that prior hospitalizations could have resulted from insufficient help. This suggests that including prior hospitalizations in the multivariate model may have resulted in an underestimation of the association between insufficient help on future hospitalizations. The fact that insufficient help was associated with hospitalization despite the lack of information about the timing of onset and duration of insufficient help and whether or not proxies were included provides additional evidence for the prognostic utility of this brief assessment.
Efforts to contain health care costs among older adults have focused on reducing rates of hospitalization which account for 37% of their total health care costs30 and reducing costs of long-term care expenditures which account for 32% of Medicaid expenditures. Some states have sought to reduce long-term care expenditures by reducing home care benefits, but reductions in home care services are associated with negative health outcomes. For example, as the average hours of home and community-based formal care decreased during economically difficult times in Michigan, participants were more likely to be hospitalized.12 The need for community based ADL services exceeds the amount of services available through governmental resources such as Title III and Medicaid Waiver programs,31 which is unfortunate because Medicaid waiver patients who receive one or fewer hours per week of home based personal care services are at significantly greater risk for future hospitalization than those with several hours per week of home-based personal care services.32Additional research is needed to determine whether home and community-based long-term care programs that are effective in reducing insufficient help for ADL limitations are also effective in reducing risk for future hospitalization.
ACKNOWLEDGMENT
This research was supported by a grant from the National Institutes of Health (R01AG034160) to Dr. Sands.
Sponsor’s Role: The sponsor, the National Institute of Health, had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper. The funding agency had no role in the design, methods, analysis and preparation of this manuscript.
Footnotes
Conflict Of Interest
Drs. Xu, Covinsky, Thomas, and Sands, and Prof. Stallard, do not have any financial interest or personal conflicts with the methodologies discussed in this manuscript.
Author Contributions: Dr. Xu and contributed significantly to the study concept and design, analysis and interpretation of data and the preparation of the manuscript. Prof. Stallard and Dr. Sands contributed significantly to the study concept and design, the acquisition of data, analysis and interpretation of data, and the preparation of the manuscript. Drs. Covinsky and Thomas contributed significantly to the study concept and design, interpretation of data analyses, and the preparation of the manuscript.
REFERENCES
- 1.Chan L, Beaver S, MacLehose R, et al. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil. 2002;83:1196–1201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 2.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 3.Fortinsky R, Covinsky KE, Palmer RM, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54A:M521–M526. doi: 10.1093/gerona/54.10.m521. [DOI] [PubMed] [Google Scholar]
- 4.Walter L, Brand R, Counsell S, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001:2987–2994. doi: 10.1001/jama.285.23.2987. [DOI] [PubMed] [Google Scholar]
- 5.Sands L, Wang Y, McCabe G, et al. Rates of acute care admissions for frail elders living with met versus unmet activity of daily living needs. J Am Geriatr Soc. 2006;54:339–344. doi: 10.1111/j.1532-5415.2005.00590.x. [DOI] [PubMed] [Google Scholar]
- 6.Desai M, Lentzner H, Dawson Weeks J. Unmet need for personal assistance with activities of daily living among older adults. Gerontologist. 2001;41:82–88. doi: 10.1093/geront/41.1.82. [DOI] [PubMed] [Google Scholar]
- 7.Allen S, Mor V. The prevalence and consequences of unmet need: contrasts between older and younger adults with disability. Med Care. 1997;35:1132–1148. doi: 10.1097/00005650-199711000-00005. [DOI] [PubMed] [Google Scholar]
- 8.LaPlante M, Kaye S, Kang T, et al. Unmet need for personal assistance services: Estimating the shortfall in hours of help and adverse consequences. J Gerontol B Psychol Sci Soc Sci. 2004;59B:S98–S108. doi: 10.1093/geronb/59.2.s98. [DOI] [PubMed] [Google Scholar]
- 9.Femia EE, Zarit SH, Johansson B. The disablement process in very late life: A study of the oldest-old in Sweden. J Gerontol B Psychol Sci Soc Sci. 2001;56B:P12–P23. doi: 10.1093/geronb/56.1.p12. [DOI] [PubMed] [Google Scholar]
- 10.Landi F, Onder G, Cesari M, et al. Comorbidity and social factors predicted hospitalization in frail elderly patients. J Clin Epidemiol. 2004;57:832–836. doi: 10.1016/j.jclinepi.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 11.Inouye S, Zhang Y, Jones R, et al. Risk factors for hospitalization among community-dwelling primary care older adults. Med Care. 2008;46:726–731. doi: 10.1097/MLR.0b013e3181649426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Souza J, James M, Szafara K, et al. Hard times: the effects of financial strain on home care services use and participant outcomes in Michigan. Gerontologist. 2009;49:154–165. doi: 10.1093/geront/gnp020. [DOI] [PubMed] [Google Scholar]
- 13.Lima J, Allen S. Targeting risk for unmet need: not enough help versus no help at all. J Gerontol B Psychol Sci Soc Sci. 2001;56B:S302–S310. doi: 10.1093/geronb/56.5.s302. [DOI] [PubMed] [Google Scholar]
- 14.Newcomer R, Kang T, LaPlante M, et al. Living quarters and unmet need for personal care assistance among adults with disabilities. J Gerontol B Psychol Sci Soc Sci. 2005;60B:S206–S213. doi: 10.1093/geronb/60.4.s205. [DOI] [PubMed] [Google Scholar]
- 15.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 16.Tombaugh T, McIntyre N. The Mini-Mental State Examination: A comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 17.Freedman V, Agree E, Martin L, Cornman J. Trends in the use of assistive technology and personal care for late-life disablity, 1992–2001. Gerontologist. 2005;46:124–127. doi: 10.1093/geront/46.1.124. [DOI] [PubMed] [Google Scholar]
- 18.Agree E, Freedman V. A comparison of assistive technology and personal care in alleviating disability and unmet need. Gerontologist. 2003;43:335–344. doi: 10.1093/geront/43.3.335. [DOI] [PubMed] [Google Scholar]
- 19.Anderson P, Gill R. Cox's regression model for counting processes: A large sample study. Ann Stat. 1982;10:1100–1120. [Google Scholar]
- 20.Therneau T, Grambsch P. Modeling survival data: Extending the Cox model. Springer; 2000. [Google Scholar]
- 21.Binder D. Fitting Cox's proportional hazards models from survey data. Biometrika. 1992;79:139–147. [Google Scholar]
- 22.Guo Z, Gill T, Allore H. Modeling repeated time-to-event health conditions with discontinuous risk intervals: An example of a longitudinal study of functional disability among older persons. Methods Inf Med. 2008;47:107–116. [PMC free article] [PubMed] [Google Scholar]
- 23.Patrick D, Peach H, Gregg I. Disablement and care: A comparison of patient views and general practitioner knowledge. Br J Gen Pract. 1982;32:429–434. [PMC free article] [PubMed] [Google Scholar]
- 24.Scharlach A, Gustavson K, Dal Santo T. Assistance received by employed caregivers and their care recipients: Who helps care recipients when caregivers work full time? Gerontologist. 2007;47:752–762. doi: 10.1093/geront/47.6.752. [DOI] [PubMed] [Google Scholar]
- 25.Casado B, van Vulpen K, Davis S. Unmet needs for home and community-based services among frail older Americans and their caregivers. J Aging Health. 2011;23:529–553. doi: 10.1177/0898264310387132. [DOI] [PubMed] [Google Scholar]
- 26.Carlson B, Foster L, Dale S, Brown R. Effects of cash and counseling on personal care and well-being. Health Serv Res. 2007;42:467–487. doi: 10.1111/j.1475-6773.2006.00673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kane R, Kane R. Assessment in long-term care. Annu Rev Public Health. 2000;3:659–686. doi: 10.1146/annurev.publhealth.21.1.659. [DOI] [PubMed] [Google Scholar]
- 28.Di Iorio A, Long A, Costanza M, et al. Characteristics of geriatric patients related to early and late readmissions to hospital. Aging Clin Exp Res. 1998;10:339–346. doi: 10.1007/BF03339797. [DOI] [PubMed] [Google Scholar]
- 29.Jovicic A, Holroyd-Leduc J, Straus S. Effects of self-management intervention on health outcomes of patients with heart failure: A systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. doi: 10.1186/1471-2261-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartman M, Catlin A, Lassman D, et al. U.S. health spending by age, selected years through 2004. Health Aff (Millwood) 2008;27:w1–w12. doi: 10.1377/hlthaff.27.1.w1. [DOI] [PubMed] [Google Scholar]
- 31.Special Committee on Aging, US Senate. Washington DC: Government Accounting Office; 2011. Older Americans Act: More should be done to measure the extent of unmet need for services. [Google Scholar]
- 32.Xu H, Weiner M, Paul S, et al. Volume of home- and community-based Medicaid Waiver services and risk of hospital admissions. J Am Geriatr Soc. 2010;58:109–115. doi: 10.1111/j.1532-5415.2009.02614.x. [DOI] [PubMed] [Google Scholar]