Abstract
Purpose of review
EDTA chelation therapy has been in off-label use for the treatment of atherosclerosis. We review the results of the first large-scale randomized trial of this treatment.
Recent findings
The trial to assess chelation therapy was a $30 million National Institutes of Health-funded study of the safety and efficacy of EDTA-based chelation infusions in 1708 post-myocardial infarction (MI) patients. The trial to assess chelation therapy demonstrated a significant (P = 0.035) 18% reduction in a combined primary endpoint of death, MI, stroke, coronary revascularization, or hospitalization for angina. In diabetic patients the benefit was more extreme, with a 41% relative reduction in risk (P = 0.0002) and a 43% reduction in total mortality (P = 0.011). Safety data were favorable. A reduction of oxidative stress by chelation of toxic metals has been proposed as a possible mechanism of action.
Summary
Recent research suggests that EDTA chelation may be a well-tolerated and effective treatment for post-MI patients. Future replication and mechanistic studies are important prior to implementation in all post-MI patients.
Keywords: atherosclerosis, chelation therapy, diabetes mellitus, myocardial infarction
INTRODUCTION
Chelation therapy with disodium EDTA has been in use for the treatment of atherosclerotic disease for 58 years. During most of that period, many medical organizations have declared it to be unsafe and relegated the treatment to the realm of alternative medicine. National surveys have demonstrated, however, a growth in this practice [1]. The present review is timely, as it comes 1 year after the publication of the only large-scale randomized controlled trial of disodium EDTA, which demonstrated reduction in cardiovascular events. This publication was followed by an analysis of a prespecified subgroup with diabetes. The current review will focus on the history of this therapy, its potential mechanisms, and the evidence for clinical benefit.
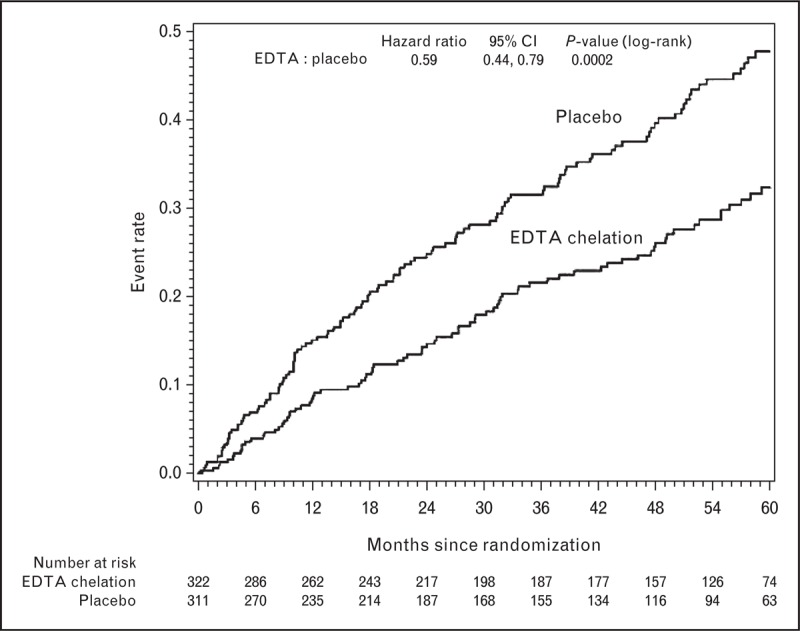
Box 1.
no caption available
BACKGROUND
The chemical process of chelation refers to the creation of a bond formed by a complex molecule (chelating agent) with a (usually) positively charged ion (chelate). The chelating agent binds the chelate, permitting its excretion in the urine or bile, depending on the chelating agent. EDTA and its salts (sodium, calcium, and magnesium) were first developed in the late 1930s for the detoxification of chemical agents being used in the war effort. It was applied in the treatment of lead toxicity in the 1940s; serendipitously, patients also noted that they experienced less angina. EDTA is a powerful and nonspecific chelator of many cations, including metals, calcium and magnesium.
In 1956, Clarke et al.[2] reported on the effects of EDTA infusions in patients with symptomatic coronary disease. They noted a beneficial effect, with diminution of angina in most of the recipients. The results generated interest, but by the 1970s conventional medicine had turned away from chelation therapy – it had become the province of alternative medicine. By the 1990s, most conventional medical organizations had published formal statements advising patients that EDTA chelation was dangerous and ineffective. Yet, patients continued to seek out, and practitioners to administer, chelation therapy.
Surveys demonstrate that up to 30% of Americans have used alternative medicine [1]. Congressional interest in studying these therapies increased and the Office for Alternative Medicine evolved to become the National Center for Complementary and Alternative Medicine (NCCAM), and funding was provided to support the study of chelation therapy.
From a regulatory perspective, the United States Food and Drug Administration (FDA) had approved the use of calcium EDTA for lead poisoning, but not the use of the disodium salt. Chelation practitioners, however, preferred the disodium salt, hypothesizing that, by causing transient hypocalcemia, it might decalcify atherosclerotic plaque [3]. Disodium EDTA had to be administered slowly to avoid severe hypocalcemia – which had caused some deaths [4]. Ultimately, the FDA failed to approve the manufacture of the disodium salt in the United States. It is now available only through compounding pharmacies, regulated at the state level, not by the FDA.
PRIOR STUDIES
Prior to the publication of the results of the trial to assess chelation therapy (TACT) [5▪▪], the clinical literature regarding EDTA chelation consisted of only case reports and case series reporting benefit for patients with coronary disease, carotid disease, and peripheral artery disease [6–10]. Only three small, randomized studies (one examining its use in the treatment of angina and two the treatment of claudication) involving a total of 269 patients had been published [10–12]. Neither singly, nor in aggregate, could these studies rule out a small to moderate clinical benefit.
BIRTH OF THE TRIAL TO ASSESS CHELATION THERAPY
In 2001, to address the need for clear safety and efficacy data on EDTA chelation, NCCAM and the National Heart, Lung and Blood Institute (NHLBI) released a $30 million Request for Applications for a definitive trial of chelation therapy. In 2002, the Cochrane Collaborative concluded that there was insufficient evidence to decide on the effectiveness or ineffectiveness of chelation therapy in improving clinical outcomes of patients with atherosclerotic cardiovascular disease and recommended a randomized clinical trial [13]. With cofunding from the NHLBI, NCCAM funded TACT, which involved a collaboration of conventional clinical sites and chelation practitioners [5▪▪]. The trial was carried out under the supervision of NHLBI, NCCAM, a Data Safety Monitoring Board, the FDA through the Investigational New Drug mechanism, and Health Canada, as well as multiple Institutional Review Boards and Ethics Boards in both countries.
TRIAL TO ASSESS CHELATION THERAPY PROTOCOL
The Request For Application called for the use of the most commonly utilized EDTA infusion in the treatment of patients with coronary artery disease; disodium EDTA was selected as the agent. The most prevalent EDTA infusion did not contain just EDTA, but also nine other components that have typically been administered by chelation practitioners. Chelation infusion contents are as follows (reproduced from [14]):
- additive:
- up to 3 g of Na2EDTA,
- 2 g of magnesium chloride,
- 100 mg of procaine HCl,
- 2500 units of heparin,
- 7 g of ascorbate,
- 2 mEq of KCl,
- 840 mg of sodium bicarbonate,
- 250 mg of pantothenic acid,
- 100 mg of thiamine,
- 100 mg of pyridoxine,
- QS with sterile water to 500 ml.
The dose of EDTA changes on the basis of estimated glomerular filtration rate; the maximum dose is 3 g.
Moreover, high doses of oral vitamins and minerals have also been administered in conjunction with intravenous chelation (Table 1[14]). Because oral vitamin therapy could be an important confounder, a 2 × 2 factorial design was employed so that there were four randomization groups:
active chelation + active oral vitamins,
active chelation + placebo oral vitamins,
placebo chelation + active oral vitamins,
placebo chelation + placebo oral vitamins.
Table 1.
High-dose oral contents
| High-dose regimen (taken twice daily) | Total amount for six pills | % RDA |
| Vitamin A | 2500 IU | 500% |
| Vitamin C | 1200 mg | 2000% |
| Vitamin D3 | 100 IU | 25% |
| Vitamin E | 400 IU | 1333% |
| Vitamin K1 | 60 μg | 75% |
| Thiamin | 100 mg | 6667% |
| Niacin | 200 mg | 1000% |
| Vitamin B6 | 50 mg | 2500% |
| Folate | 800 μg | 200% |
| Vitamin B12 | 100 μg | 1667% |
| Biotin | 300 μg | 100% |
| Pantothenic acid | 400 mg | 4000% |
| Calcium | 500 mg | 50% |
| Iodine | 150 μg | 100% |
| Magnesium | 500 mg | 125% |
| Zinc | 20 mg | 133% |
| Selenium | 200 μg | 286% |
| Copper | 2 mg | 100% |
| Manganese | 20 mg | 400% |
| Chromium | 200 μg | 167% |
| Molybdenum | 150 μg | 200% |
| Potassium | 99 mg | 3% |
| Choline | 150 mg | a |
| Inositol | 50 mg | a |
| PABA | 50 mg | a |
| Boron | 2 mg | a |
| Vanadium | 39 μg | a |
| Citrus bioflavonoids | 100 mg | a |
PABA, para-amino benzoic acid; RDA, recommended daily allowance. Reproduced with permission [14].
aRecommended daily allowance not established. Other ingredients: Croscarmellose sodium, microcrystalline cellulose, magnesium stearate, hydroxypropyl cellulose, and silicon dioxide.
The treatment was arduous, requiring 40 infusions taking over a year to complete. In order to be eligible, patients had to be at least 50 years of age, have had a prior myocardial infarction (MI), and have a creatinine of 2.0 mg/dl or less.
The study was designed to have 85% power to detect a 25% difference in the primary endpoint between the groups. The primary endpoint was a composite one and consisted of time to first occurrence of death from any cause, recurrent MI, stroke, coronary revascularization, or hospitalization for angina. The principal secondary endpoint was the composite of cardiovascular death, nonfatal MI, or nonfatal stroke. The analyses were intent-to-treat and two-sided; the log-rank test was used for treatment comparisons.
The trial took 9 years to complete. It involved 134 sites in the United States and Canada, approximately 60% of which were sites at which chelation therapy had been an ongoing practice. The first patient was randomized in 2003, and the investigators were unblinded in 2012. The results were unexpected. A disodium EDTA-based chelation therapy reduced cardiovascular events.
RESULTS
There were 1708 participants enrolled in 134 sites in the United States and Canada. A total of 55 222 infusions were administered, including placebo and disodium EDTA-based chelation solution. Subjects were followed for a median of 55 months. Several subgroups were prespecified for analysis, including patients with diabetes.
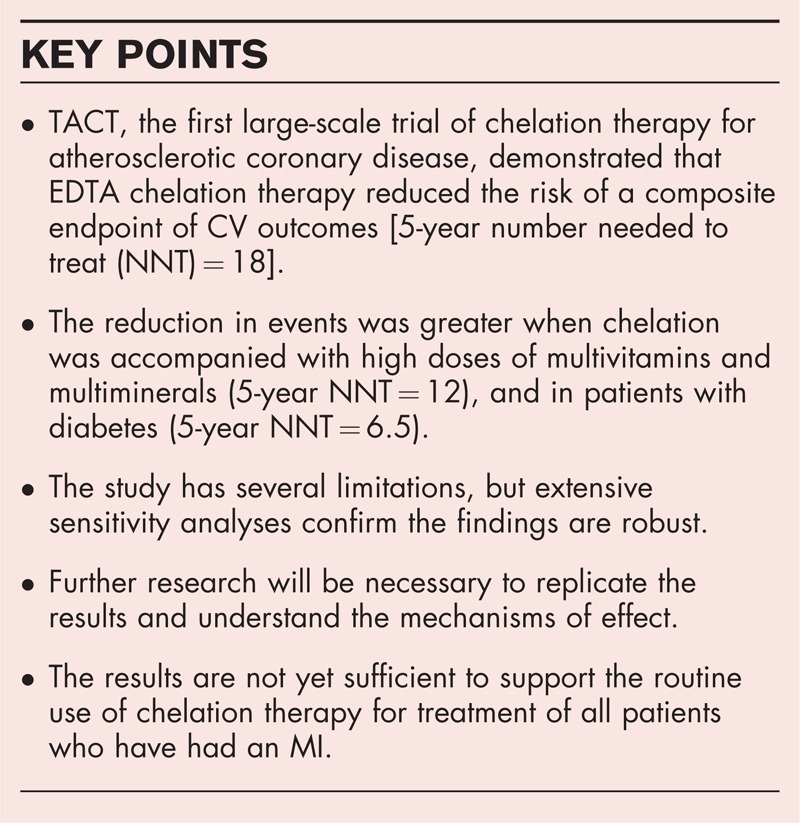
The primary endpoint occurred in 26% (222 patients) in the chelation group and 30% (261 patients) in the placebo group [hazard ratio (HR) 0.82 (95% confidence interval (CI), 0.69–0.99); P = 0.035]. The Kaplan–Meier 5-year estimate for the primary endpoint was 32.8% (95% CI, 29.1%–36.5%) in the chelation group and 38.5% (95% CI, 34.6%–42.3%) in the placebo group (Fig. 1[11]). The 5-year number needed to treat to reduce one event was 18. The effect of EDTA chelation on the components of the primary endpoint was directionally the same as its overall effect, and, other than for death, of greater magnitude (Table 2[7]). These data showed that, in patients with prior MI, disodium EDTA-based chelation therapy offered a reduction in cardiovascular events. This effect persisted after infusions had finished and was additive to standard post-MI therapies, including statins.
FIGURE 1.
TACT – Kaplan–Meier estimates of the primary composite endpoint chelation therapy vs. placebo. The primary endpoint was a composite of death from any cause, reinfarction, stroke, coronary revascularization, or hospitalization for angina. Reproduced with permission [11], previously published in [5▪▪]. CI, confidence interval; HR, hazard ratio.
Table 2.
TACT clinical endpoints
| End points | EDTA chelation (N = 839) | Placebo (N = 869) | Hazard ratio (95%CI) | P-value |
| Primary endpoint | 222 (26) | 261 (30) | 0.82 (0.69–0.99) | 0.035 |
| Death | 87 (10) | 93 (11) | 0.93 (0.70–1.25) | 0.64 |
| Myocardial infarction | 52 (6) | 67 (8) | 0.77 (0.54–1.11) | 0.17 |
| Stroke | 10 (1) | 13 (1) | 0.77 (0.34–1.76) | 0.53 |
| Coronary revascularization | 130 (15) | 157 (18) | 0.81 (0.64–1.11) | 0.08 |
| Hospitalization for angina | 13 (2) | 18 (2) | 0.72 (0.35–1.47) | 0.36 |
| Secondary endpoint | 96 (11) | 113 (13) | 0.84 (0.64–1.11) | 0.22 |
| Cardiovascular death | 50 (6) | 51 (6) | 0.98 (0.67–1.45) | 0.94 |
Individual components endpoints are all rates and not first occurrence rates. These percentages are simply crude percentages: namely, in each case the number of events divided by the number of patients.
Primary endpoint = first occurrence of death from any cause, MI, stroke, or hospitalization for unstable angina.
Secondary endpoint = first occurrence of death from a cardiovascular cause, MI, or stroke.
Reproduced with permission from [5▪▪].
Subgroup analyses demonstrated that there was a significant interaction between EDTA chelation and diabetes, with greater therapeutic benefit among diabetic patients. There was greater benefit among patients who had sustained a prior anterior wall MI. We also analyzed whether there was an interaction between type of practice, complementary or alternative medicine or conventional, and the effect of EDTA chelation therapy. The interaction P-value for this comparison was nonsignificant.
Extensive safety testing was recorded and analyzed throughout the many patient years of followup, and EDTA-based chelation therapy, within the administration parameters set up for the study, proved to be quite safe. The safety net created in the trial was remarkable, with multiple web-based alarms to detect short infusions (less than 3 h), regular visits of monitors to participating sites and ongoing education of coordinators and investigators. There were also 10 routine laboratory safety checks throughout the infusion phase of the trial.
In spite of the extreme burden placed on participants in this study (40 infusions each lasting at least 3 h), there was fair compliance: 75% of patients completed 30 infusions, and 65% completed all 40 infusions. Moreover, 17% of patients withdrew consent at some point during the trial. Although this is a potentially serious flaw, the loss of data was mitigated by 18% of patients who had a primary endpoint prior to consent withdrawal, and by assessing each country's national death register at the end of the trial. Extensive sensitivity analyses were performed that tested the robustness of the effect by assigning unfavorable event rates to the EDTA patients who withdrew, ranging from no effect to harm. In order to lose significance, unrealistic, highly unfavorable assumptions had to be made. Thus, the P-value was robust.
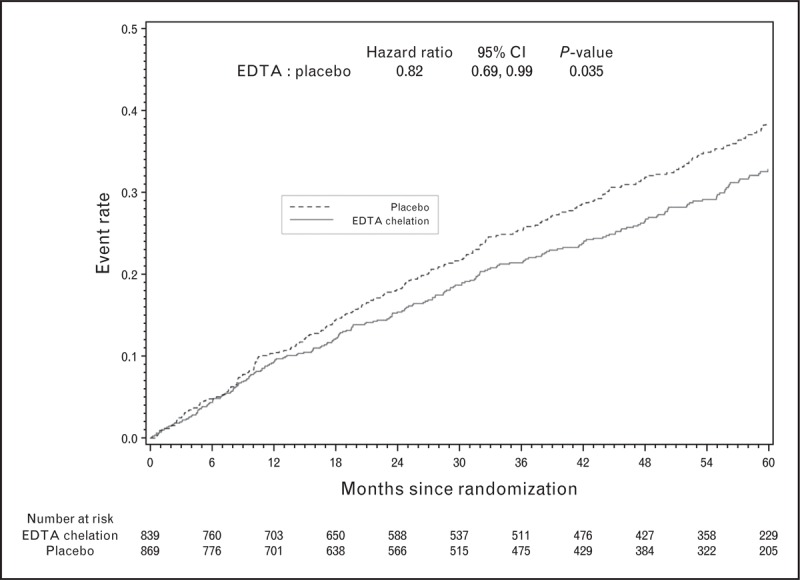
ANALYSES OF THE FACTORIAL GROUPS
TACT was designed as a 2 × 2 factorial trial, randomly assigning patients to intravenous chelation or placebo, and to oral vitamins or placebo. The overall analyses discussed above, of course, have half of the patients in each EDTA arm receiving placebo vitamins and the other half active oral vitamins. These are the highest doses of multivitamins and multiminerals ever tested in a clinical trial. Therefore, the most interesting analyses of the four factorial groups compare patients who are on active chelation and active oral vitamins with those who are on double placebo. There is a greater benefit of therapy when patients are taking double active therapy [HR 0.74 (95% CI 0.57–0.95), P = 0.016, Fig. 2] [15▪]. The 5-year number needed to treat was 12 [15▪].
FIGURE 2.
The factorial group results of TACT – Kaplan–Meier estimates of the primary endpoint per group. (a) Kaplan–Meier curves (four factorial groups, primary endpoint); (b) Kaplan–Meier curves placebo/placebo vs. active/active (primary endpoint). Reproduced with permission [15▪].
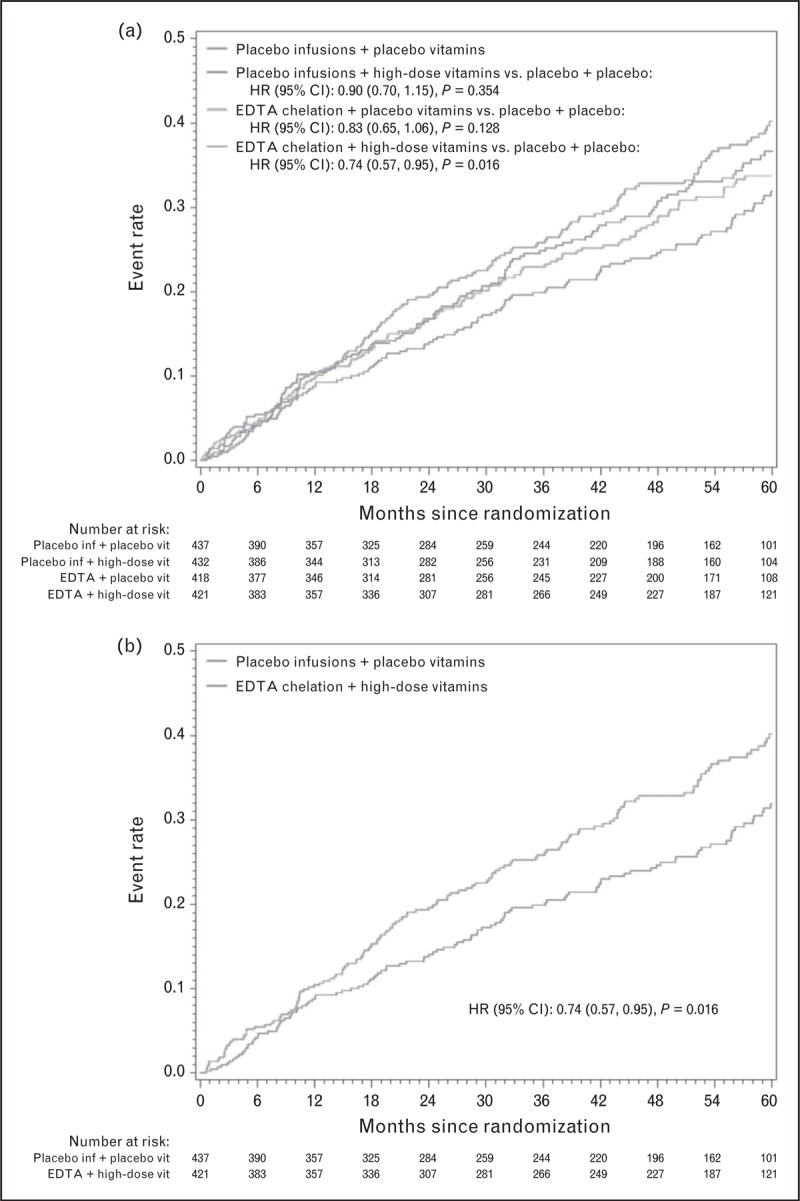
ANALYSIS OF PATIENTS WITH DIABETES
Diabetes mellitus was prespecified as a subgroup for analysis, and defined as self-reported diabetes mellitus, current use of oral or insulin treatment for diabetes mellitus or fasting glucose of at least 6.99 mmol/l (126 mg/dl). A total of 633 (37%) patients enrolled in the study met the definition of diabetes mellitus. Treatment with EDTA infusions reduced the primary endpoint (EDTA chelation vs. placebo: 25% vs. 38%; HR 0.59; 95% CI 0.44 –0.79%; P < 0.001) [16▪▪]. The incidence of primary endpoints remained lower in this group during extended followup for up to 5 years, with a 15% absolute decrease in the 5-year Kaplan–Meier primary event rate (Fig. 3[7]) and a relative reduction in risk of 41%. The 5-year number needed to treat was 6.5 (95% CI, 4.4–12.7). Even after a very conservative Bonferroni adjustment for multiple subgroups was performed, the results remained statistically significant (99.4% CI, 0.39–0.88; adjusted P = 0.002). There were important and consistent reductions in the components of the primary endpoint as well.
FIGURE 3.
TACT – Kaplan–Meier estimates of the primary composite endpoint EDTA chelation therapy vs. placebo subgroup of patients with diabetes mellitus. The primary endpoint was a composite of death from any cause, reinfarction, stroke, coronary revascularization, or hospitalization for angina. Reproduced with permission [16▪▪]. CI, confidence interval; HR, hazard ratio.
STUDY LIMITATIONS
It is important to recognize study limitations that temper the interpretation of TACT. A larger than expected number, 17%, withdrew consent, and the study treatments, infusions and oral both, had important rates of nonadherence. Possibly because there were more events in the group receiving placebo infusions, the rate of consent withdrawal was higher in the placebo infusion group compared with the active infusion group. If more placebo patients withdraw from the study than do active infusion patients, this confers a conservative bias to the trial. That is, more placebo events would fail to be attributed and counted toward the placebo group than would be the case with the active infusion group, narrowing the difference between groups and decreasing the significance. Despite this, statistical significance was maintained. In addition, careful sensitivity analyses were carried out assigning event rates to the EDTA patients who dropped out that were higher than the event rates of the EDTA patients who stayed in the trial. In the overall group, even if the active group that withdraw consent had 20% more events than the placebo infusion group that withdraw consent, significance was maintained. The diabetes sensitivity analyses demonstrated the significance to be even more robust. The study was also criticized for only reaching borderline levels of significance at P = 0.035. Yet, this was less than the prespecified level of significance in the statistical analysis plan.
Another concern voiced about TACT is that the study did not follow a classical pathway for drug development. Typically, a compound or drug is identified in basic research and a mechanism of action is proposed and proved in experimental in-vitro and animal models. With a hypothesis generated, a clinical trial is designed to prove this mechanism of action and its clinical translation. In the case of alternative medicine treatments, the pathway is quite different. Chelation practitioners were infusing EDTA and had done so for decades. TACT was designed to prove whether this existing therapy was safe and effective. The conventional cardiology reaction to TACT has been an exercise in Bayesian interpretation of unexpected results. That is, expectations of trial results color the interpretation of those results. A formal Bayesian analysis was performed on the results of chelation on patients with diabetes in an accompanying editorial [17]. Even if a skeptical or extremely skeptical prior probability was assigned, the effect of EDTA chelation on the primary endpoint was still significant. The results of TACT, therefore, lead us to hypothesize regarding the underlying mechanisms of effect.
POSSIBLE MECHANISMS OF CHELATION THERAPY
EDTA is a nonspecific chelating agent that binds metals with valences of +2 to +6. Therefore, it is logical to first look toward metal chelation as a potential mechanism for the observed results.
There is a long epidemiologic literature describing the association of metals with cardiovascular risk, including hypertension, atherosclerosis, MI, and stroke. Lead, cadmium, antimony, cadmium, cobalt, and tungsten have been associated with cardiovascular disease [18–25]. EDTA chelates and allows excretion of these metals.
With regard to the apparent enhanced efficacy in patients with diabetes, observational studies suggest a role for the products of nonenzymatic glycooxidation of proteins and/or lipids, also known as advanced glycation end-products [26,27▪,28–30] in the microvascular complications in diabetes. Most advanced glycation end-products require metal-catalyzed oxygen chemistry for their creation. When metals bind to glycation end-products, reactive oxygen species are generated. Oxidative stress and inflammation are promoted as the oxidized end-products accumulate in different tissues, changes that are characteristic of atherosclerosis. The role of oxidized lipids in atherosclerosis is well known. They not only participate in foam cell formation but also have endothelial proinflammatory, proapoptotic, and prothrombotic effects. Metal chelation may reduce toxicity mediated through enhanced metal-catalyzed oxidation [31].
CONCLUSION
TACT, the first large-scale trial of chelation therapy for atherosclerotic coronary disease, found that EDTA chelation therapy reduced the risk of a composite of adverse cardiovascular outcomes, particularly among patients with diabetes. Before disodium EDTA chelation can take its place among other accepted therapies in the routine care of post-MI patients, however, it is important that further replicative and mechanistic clinical trials be performed.
Acknowledgements
The National Heart, Lung, and Blood Institute and the National Center for Complementary and Alternative Medicine provided funding and oversight, grants U01AT001156 and U01HL092607.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008; 6:1–23 [PubMed] [Google Scholar]
- 2.Clarke CN, Clarke NE, Mosher RE. Treatment of angina pectoris with disodium ethylene diamine tetraacetic acid. Am J Med Sci 1956; 232:654–666 [DOI] [PubMed] [Google Scholar]
- 3.Bolick LE, Blankenhorn DH. A quantitative study of coronary arterial calcification. Am J Pathol 1961; 39:511–519 [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Deaths associated with hypocalcemia from chelation therapy – Texas, Pennsylvania, and Oregon, 2003–2005. MMWR Morb Mortal Wkly Rep 2006; 55:204–207 [PubMed] [Google Scholar]
- 5▪▪.Lamas GA, Goertz C, Boineau R, et al. Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: the TACT randomized trial. JAMA 2013; 309:1241–1250 [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the first large, randomized trial of chelation therapy for atherosclerosis. Its surprising results have urged the need to continue exploring the use of chelation in cardiovascular disease.
- 6.Olszewer E, Carter JP. EDTA chelation therapy in chronic degenerative disease. Med Hypothesis 1998; 4:91–95 [DOI] [PubMed] [Google Scholar]
- 7.Lamar CP. Chelation therapy of occlusive arteriosclerosis in diabetic patients. Angiology 1964; 15:379–395 [DOI] [PubMed] [Google Scholar]
- 8.Ernst E. Chelation therapy for peripheral arterial occlusive disease: a systematic review. Circulation 1997; 96:1031–1033 [DOI] [PubMed] [Google Scholar]
- 9.Ernst E. Chelation therapy for coronary heart disease: an overview of all clinical investigations. Am Heart J 2000; 140:139–141 [DOI] [PubMed] [Google Scholar]
- 10.Guldager B, Jelnes R, Jørgensen SJ, et al. EDTA treatment of intermittent claudication—a double-blind, placebo-controlled study. J Intern Med 1992; 231:261–267 [DOI] [PubMed] [Google Scholar]
- 11.van Rij AM, Solomon C, Packer SG, Hopkins WG. Chelation therapy for intermittent claudication: a double-blind, randomized, controlled trial. Circulation 1994; 90:1194–1199 [DOI] [PubMed] [Google Scholar]
- 12.Knudtson M, Galbraith PD. Chelation therapy for ischemic heart disease: a randomized controlled trial. JAMA 2002; 287:481–486 [DOI] [PubMed] [Google Scholar]
- 13.Dans AL, Tan FN, Villarruz-Sulit EC. Chelation therapy for atherosclerotic cardiovascular disease. Cochrane Database of Systematic Reviews 2002, Issue 4. Art. No.: CD002785. 10.1002/14651858.CD002785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamas GA, Goertz C, Boineau R, et al. Design of the trial to assess chelation therapy (TACT). Am Heart J 2012; 163:7–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪.Lamas GA, Boineau R, Goertz C, et al. EDTA chelation therapy alone and in combination with oral high-dose multivitamins and minerals for coronary disease: the factorial group results of the trial to assess chelation therapy. Am Heart J 2014; 168: 37–44.e5 [DOI] [PMC free article] [PubMed] [Google Scholar]; This TACT report showed that the combination of oral high-dose vitamins and EDTA chelation therapy compared with double placebo significantly reduced cardiovascular events. High-dose vitamins may play a role in the beneficial effect of EDTA chelation therapy.
- 16▪▪.Escolar E, Lamas GA, Mark DB, et al. The effect of an EDTA-based chelation regimen on patients with diabetes mellitus and prior myocardial infarction in the trial to assess chelation therapy (TACT). Circ Cardiovasc Qual Outcomes 2014; 7:15–24 [DOI] [PMC free article] [PubMed] [Google Scholar]; Results of this subgroup analysis of the diabetic population in the TACT trial suggest a novel mechanism and potential new target to treat atherosclerosis in diabetic patients.
- 17.Kaul S. Are concerns about reliability in the trial to assess chelation therapy fair grounds for a hasty dismissal?: An alternative perspective. Circ Cardiovasc Qual Outcomes 2014; 7:5–7 [DOI] [PubMed] [Google Scholar]
- 18.Menke A, Muntner P, Batuman V, et al. Blood lead below 0.48 μmol/l (10 μg/dl) and mortality among US adults. Circulation 2006; 114:1388–1394 [DOI] [PubMed] [Google Scholar]
- 19.Nawrot TS, Staessen JA. Low-level environmental exposure to lead unmasked as silent killer. Circulation 2006; 114:1347–1349 [DOI] [PubMed] [Google Scholar]
- 20.Navas-Acien A, Selvin E, Sharrett AR, et al. Lead, cadmium, smoking, and increased risk of peripheral arterial disease. Circulation 2004; 109:3196–3201 [DOI] [PubMed] [Google Scholar]
- 21.Tellez-Plaza M, Guallar E, Howard BV, et al. Cadmium exposure and incident cardiovascular disease. Epidemiology 2013; 24:421–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaziri ND. Mechanisms of lead-induced hypertension and cardiovascular disease. Am J Physiol Heart Circ Physiol 2008; 295:H454–H465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frustaci A, Magnavita N, Chimenti C, et al. Marked elevation of myocardial trace elements in idiopathic dilated cardiomyopathy compared with secondary cardiac dysfunction. J Am Coll Cardiol 1999; 33:1578–1583 [DOI] [PubMed] [Google Scholar]
- 24.Weisskopf MG, Jain N, Nie H, et al. A prospective study of bone lead concentration and death from all causes, cardiovascular diseases, and cancer in the Department of Veterans Affairs Normative Aging study. Circulation 2009; 120:1056–1064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agarwal S, Zaman T, Tuzcu EM, Kapadia SR. Heavy metals and cardiovascular disease: results from the National Health and Nutrition Examination Survey (NHANES) 1999–20. Angiology 2011; 62:422–429 [DOI] [PubMed] [Google Scholar]
- 26.Schmidt AM, Stern DM. RAGE: a new target for the prevention and treatment of the vascular and inflammatory complications of diabetes. Trends Endocrinol Metab 2000; 11:368–375 [DOI] [PubMed] [Google Scholar]
- 27▪.Manigrasso MB, Juranek J, Ramasamy R, Schmidt AM. Unlocking the biology of RAGE in diabetic microvascular complications. Trends Endocrinol Metab 2014; 25:22–25 [DOI] [PMC free article] [PubMed] [Google Scholar]; This review focuses on the role of advanced glycation end-products in the vascular complications of diabetes mellitus. This is a potential pathway involved in the mechanism of action of EDTA chelation in cardiovascular disease.
- 28.Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes 1991; 40:405–412 [DOI] [PubMed] [Google Scholar]
- 29.Hodgkinson CP, Laxton RC, Patel K, Ye S. Advanced glycation end-product of low density lipoprotein activates the toll-like 4 receptor pathway implications for diabetic atherosclerosis. Arterioscler Thromb Vasc Biol 2008; 28:2275–2281 [DOI] [PubMed] [Google Scholar]
- 30.Goh SY, Cooper ME. The role of advanced glycation end products in progression and complications of diabetes. J Clin Endocrinol Metab 2008; 93:1143–1152 [DOI] [PubMed] [Google Scholar]
- 31.Frizzell N, Baynes JW. Chelation therapy for the management of diabetic complications: a hypothesis and a proposal for clinical laboratory assessment of metal ion homeostasis in plasma. Clin Chem Lab Med 2014; 52:69–75 [DOI] [PubMed] [Google Scholar]


