Abstract
Breast arterial calcification (BAC), observed as an incidental finding on screening mammograms, represents degenerative calcific changes occurring in the mammary arteries, with increasing age. The aim of this review is to discuss relevant literature examining relation between BAC and atherosclerosis. After a thorough literature search, in OVID and PubMed, 199 studies were identified, of which 25 were relevant to our review. Data were abstracted from each study and statistical analysis was done, including calculation of odds ratios and construction of forest plots. A total of 35,542 patients were enrolled across 25 studies looking at an association between BAC and coronary artery disease, cardiovascular disease, stroke, cerebral artery disease, carotid and peripheral artery diseases, and coronary artery calcification. A majority of the studies showed a statistically significant relation between BAC and presence of coronary artery disease cardiovascular disease and associated mortality. Sensitivity of BAC in predicting cardiovascular events was low, but specificity was high. BAC was predictive of incident and prevalent stroke but not mortality of stroke. Similarly, BAC was predictive of cerebral, carotid, and peripheral artery diseases. The role of BAC as a surrogate marker of coronary and systemic atherosclerosis is currently uncertain. Its role may be further elucidated by more large-scale prospective studies and clinical experience.
Keywords: breast arterial calcification, atherosclerosis, mammography, coronary artery disease, cardiovascular disease, stroke, cerebral artery disease, carotid artery disease, peripheral artery disease, coronary artery calcification
Breast arterial calcification (BAC) is a type of medial calcific or Mönckeberg sclerosis1 and is defined as nonocclusive calcification of the media of small- to medium-sized mammary arteries. It has a characteristic pattern of linear amorphous calcification bounded by 2 parallel lines giving a tram-track appearance (Fig. 1).2 BAC involves the entire circumference of the vessel, making it less compliant, and represents arteriosclerosis of peripheral arteries.
FIGURE 1.
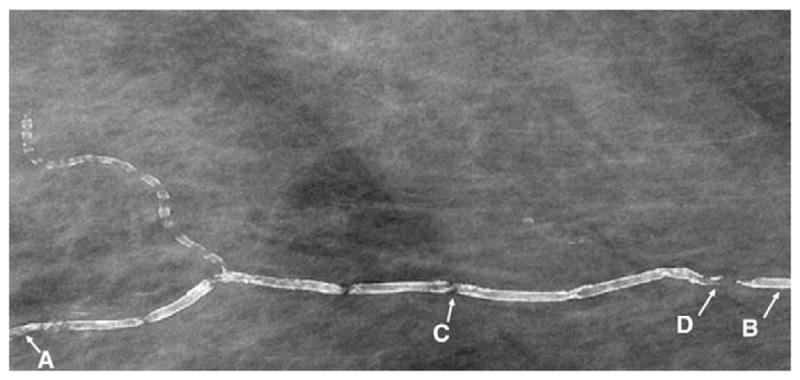
Screening mammogram showing breast arterial calcification. The length of breast arterial calcification is defined as longest continuous calcified segment, which is C to D in the depicted vessel A to B (Reproduced with permission from Zgheib et al11).
The prevalence of BACs on routine screening mammography ranges from 8%3 to 20%.4 Calcifications of mammary arteries frequently represent age-related degenerative changes;5 their incidence increases with age, and they are uncommon in mammograms performed in women less than 50 years of age.
Sickles et al6 showed that there was a statistically significant correlation between BAC and diabetes mellitus, but concluded that this association was not clinically significant. This spurred several studies looking at an association between BAC and cardiovascular diseases (CVDs) and their risk factors. With the relatively low cost of testing and possible association between BAC, coronary artery disease (CAD), stroke, carotid artery disease, and peripheral arterial disease (PAD), the study of BAC and its relation to these comorbid states may be of clinical benefit for diagnosis and prevention of these conditions. Moreover, mammography is routinely used as a screening test for breast cancer, and its use to detect BAC will not entail any extra cost or radiation exposure. This review article explores the relation between BAC and vascular diseases in an attempt to clearly delineate it as a possible CVD predictor using the current available information in the literature.
METHODS
Two investigators independently searched for all published studies on the relation between BAC and CAD, stroke, PAD, carotid atherosclerosis, carotid intima media thickness (CIMT), and coronary calcification. Literature search was conducted in OVID Medline and PubMed databases using the following keywords or phrases as subject headings or in title or abstract search: “breast arterial calcification,” “breast artery calcification,” “BAC,” “mammary arterial calcification,” “mammary artery calcification,” “intramammary arterial calcification,” “intramammary artery calcification,” “Intramammary Arterial Calcification” (IMAC), “breast vascular calcification,” “vascular calcification and mammography,” “atherosclerosis,” “arteriosclerosis,” “cardiovascular diseases,” “coronary artery disease,” “brain ischemia,” “cerebrovascular disorders,” “cerebral artery disease,” “stroke,” “cerebrovascular accident,” “carotid artery diseases,” “carotid atherosclerosis,” “carotid intima media thickness,” “peripheral vascular diseases,” “peripheral arterial disease,” “peripheral artery disease,” “coronary calcification,” “coronary artery calcification,” and “coronary calcium score.” After screening the studies found in the initial search, the full texts of all articles relevant to our study were retrieved. Subsequently, to identify additional studies, references of all relevant articles were thoroughly reviewed. The demographic characteristics of each study were extracted and tabulated. Information regarding the type of the study, sample size, definition of study endpoint, prevalence of BAC in the study, and statistical significance based on P values (with P < 0.05 considered significant) were also collected and recorded.
Statistical Analyses
Two-by-two tables delineating any association between BAC and the endpoint (eg, CAD and stroke) were constructed wherever possible for each study using the available data. Using these tables, odds ratios (ORs) with 95% confidence intervals (CIs) and P values were calculated for each study. Forest plots of ORs with 95% CIs were then constructed using the crude and adjusted ORs/hazards ratios (HRs) reported in each study. All analyses were performed using Microsoft Excel 2010 and Statistical Analysis Software (SAS) version 9.0.
RESULTS
Our initial search yielded 199 studies. On subsequent screening, 25 studies, with a total of 35,542 patients across 7 countries, were found to be relevant and were included in our review. The study period ranged from 1995 to 2011, and the studies looked at relation between BAC and CVD, cardiovascular (CV) mortality, coronary, cerebral or systemic atherosclerosis, CIMT, and coronary calcium. We found 19 studies7–25 looking at the association of BAC and CAD and/or CVD, 8 studies between BAC and stroke,7–9,20,21,23,24,26 2 studies between BAC and PAD,27,28 3 studies between BAC and CIMT,16,19,29 and 2 studies between BAC and coronary artery calcification (CAC).30,31 Tables 1 and 2 show detailed information regarding individual studies.
TABLE 1.
Studies Showing Association Between BAC and CAD, CVD, CV Mortality, and CAC
| Study | Country | Type of Study |
N | Age | BAC Prevalence, % |
Endpoint | Method of Detecting Endpoint |
Prevalence of Endpoint, % |
Result | Crude OR |
95% CI | P | Adjusted Ratio |
95% CI | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schnatz et al7 | United States | Prospective | 1454 | 56.3 | 14.2 | CAD | Self-reported | 4.9* | S | 4.62 | 3.1–7.0 | <0.05 | 3.54 | 2.3–5.5 | <0.001 |
| Iribarren et al8 | United States | Retrospective | 12,761 | 56.3 | 3 | CAD | Hospital discharge | 17.9 | S | 1.9 | 1.5–2.4 | <0.001 | 1.32‡ | 1.1–1.6 | 0.007 |
| Kemmeren et al9 | The Netherlands | Retrospective | 12,084 | 57.7 | 9.2 | CV mortality | ICD-9 coding | 10† | S | 1.76 | 1.5–2.1 | <0.001 | 1.47‡ | 1.1–2.0 | <0.05 |
| Penugonda et al10 | United States | Case control | 94 | 66.7 | 60.6 | CAD§ | Coronary angiography | 56.4 | NS | 0.98 | 0.4–2.3 | 0.72 | — | — | — |
| Zgheib et al11 | United States | Case control | 172 | 62.3 | 33 | CAD§ | Coronary angiography | 54.1 | NS/S¶ | 1.95 | 1.0–3.8 | 0.045 | — | — | — |
| Henkin et al12 | Israel | Case control | 319 | 63 | 41.1 | CAD§ | Coronary angiography | 58.6 | NS | 1.32 | 0.8–2.1 | 0.23 | 0.96 | 0.6–1.6 | 0.89 |
| Moshyedi et al13 | United States | Case control | 182 | 64 | 33.5 | CAD§ | Coronary angiography | 33.5 | NS | 1.16 | 0.6–2.2 | 0.64 | 0.95 | 0.5–1.9 | 0.88 |
| Topal et al14 | Turkey | Case control | 123 | 56.8 | 39.8 | CAD§ | Coronary angiography | 39 | NS/S¶ | 2.31 | 1.1–4.9 | 0.042 | — | — | — |
| Fiuza Ferreira et al15 | Brazil | Case control | 131 | 61.1 | 39.7 | CAD§ | Coronary angiography | 64.9 | S | 2.12 | 1.0–4.3 | 0.007 | 4.6 | 1.7–12.8 | <0.05 |
| Sarrafzadegann et al16 | Iran | Case control | 84 | 43.4 | 7.1 | CAD§ | Coronary angiography | 40.5 | NS | — | — | — | 1.2 | 0.1–4.7 | 0.8 |
| Oliveira et al17 | Brazil | Case control | 80 | 64.6 | 42.5 | CAD | Coronary angiography or history of MI | 50 | S | 4.06 | 1.6–10.5 | 0.003 | 4.71 | 1.4–16.3 | 0.014 |
| Dale et al18 | United States | Case control | 1214 | 65 | 23 | CAD | Coronary angiography | 23 | S | 8.14 | 6.0–11 | <0.001 | 6.2 | 4.3–8.8 | <0.05 |
| Sedighi et al19 | Iran | Case control | 204 | 60.6 | 14.7 | CAD | Self-reported | 13.2 | S | 4.63 | 1.9–11 | <0.001 | 2.63 | 0.8–8.8 | >0.05 |
| Crystal et al20 | Israel | Cross-sectional | 865 | 55.9 | 17.6 | ASCVD | Self-reported | 16.4 | S | 3.91 | 2.6–5.8 | <0.001 | 2.11 | 1.2–3.7 | 0.008 |
| Rotter et al21 | United States | Cross-sectional | 1919 | 56 | 14 | ASCVD | Self-reported | 5.1 | S | 5.65 | 2.7–8.6 | <0.001 | 2.29 | 1.4–3.7 | <0.001 |
| Ferreira et al22 | Brazil | Cross-sectional | 307 | 55.2 | 8.5 | CVD | Self-reported and medical records | 6.8 | S | 5.32 | 1.9–15 | <0.001 | 8.13 | 2.7–24.7 | <0.001 |
| Van Noord et al23 | The Netherlands | Cross-sectional | 12,084 | 57.7 | 9.1 | MI | Self-reported | 4.7 | S | 2.07 | 1.6–2.6 | <0.001 | 1.87 | 1.1–3.2 | <0.05 |
| Kataoka et al24 | United Kingdom | Cross-sectional | 1590 | 63.2 | 16 | CAD | Self-reported | 1.5 | S | 2.68 | 1.1–6.3 | 0.019 | 2.54 | 1.0–6.3 | <0.05 |
| Dale et al25 | United States | Cross-sectional | 1000 | 57.5 | 16 | CAD | self-reported | 7.2 | S | 6.42 | 3.9–11 | <0.001 | 3.6 | 2–6.4 | <0.001 |
| Maas et al30 | The Netherlands | Prospective | 499 | 57.9 | 12 | CAC | MSCT | 53 | S | 3.2 | 1.7–6.0 | <0.001 | 2.0 | 1.0–3.9 | 0.04 |
Calculated from prevalent CAD as reported in subjects at the start of the study.
Calculated from prevalent CVD as reported in subjects at the start of the study.
Hazards ratio (adjusted).
Only obstructive CAD (≥50% stenosis on angiography) considered.
Significant only when obstructive CAD (≥50% stenosis) considered as endpoint.
Age indicates median age in years; ASCVD, atherosclerotic cardiovascular disease; BAC, breast arterial calcification; CAC, coronary artery calcification (defined as coronary calcium score >0); CAD, coronary artery disease; CV, cardiovascular; CVD, cardiovascular disease; ICD-9, International Classification of Diseases, Ninth Revision; MI, myocardial infarction; MSCT, multislice computerized tomography; N, sample size; NS, nonsignificant; OR, odds ratio; S, significant; CI, confidence interval.
TABLE 2.
Studies Showing Association Between BAC and Non-CAD Atherosclerotic Vascular Disease (Stroke, Cerebral Artery Disease, Systemic Vascular Disease, and CIMT)
| Study | Country | Type | N | Age | BAC Prevalence, % |
Endpoint | Method of Detecting Endpoint |
Prevalence of Endpoint, % |
Result | Crude OR |
95% CI | P | Adjusted Ratio |
95% CI | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schnatz et al7 | United States | Prospective | 1454 | 56.3 | 14.2 | Stroke | Self-reported | 1.51 | S | 6.89 | 3.5–13.6 | <0.001 | — | — | — |
| Iribarren et al8 | United States | Retrospective | 12,761 | 56.3 | 3 | Ischemic stroke | Hospital discharge | 10.9 | S | 2.11 | 1.6–2.7 | <0.001 | 1.41‡ | 1.1–1.8 | 0.004 |
| Kemmeren et al9 | The Netherlands | Retrospective | 12,084 | 57.7 | 9.2 | Stroke deaths | ICD-9 coding | 1.1 | NS | 1.18 | 0.7–2.1 | 0.56 | 0.98‡ | 0.6–1.7 | >0.05 |
| Crystal et al20 | Israel | Cross-sectional | 865 | 55.9 | 17.6 | Stroke | Self-reported | 1.85 | S | 4.9 | 1.8–13.3 | 0.0006 | — | — | — |
| Rotter et al21 | United States | Cross-sectional | 1919 | 56 | 14 | Stroke | Self-reported | 1.56 | S | 4.37 | 1.8–10.4 | 0.001 | — | — | — |
| Van Noord et al23 | The Netherlands | Cross-sectional | 12,084 | 57.7 | 9.1 | Stroke/TIA | Self-reported | 4.97 | S | 1.42 | 1.1–1.8 | 0.006 | 1.43 | 1.1–1.9 | <0.05 |
| Kataoka et al24 | United Kingdom | Cross-sectional | 1590 | 63.2 | 16 | Stroke | Self-reported | 0.94 | NS | 1.93 | 0.6–6.1 | 0.26 | 2.02 | 0.6–6.7 | >0.05 |
| Jin Ahn et al26 | Korea | Cross-sectional | 168 | 58 | 17 | Cerebral artery disease | Brain MRI | 11.9* | S | 8.8* | 3.2–34* | <0.001 | 6.86* | 1.8–25* | 0.004 |
| 3.6† | S | 11† | 1.9–63† | 0.001 | 9.04† | 1.2–68† | 0.033 | ||||||||
| Dale et al27 | United States | Case control | 766 | 72 | 19 | PAD | Hospital records | 15.8 | S | 3.09 | 2.1–4.7 | <0.001 | — | — | — |
| Markopoulos et al28 | Greece | Cross-sectional | 110 | 62.2 | 11 | Systemic vascular disease§ | Carotid or femoral duplex | 62.7 | S | 3.83 | 1.7–8.7 | 0.001 | — | — | — |
| Sedighi et al19 | Iran | Case control¶ | 204 | 60.6 | 14.7 | CIMT >0.8 mm or carotid plaque | Carotid USG | 32.4 | S | 6.55 | 3.4–12.5 | <0.001 | 4.88a | 1.5–16a | <0.01 |
| 23.4b | 4.5–120b | <0.01 | |||||||||||||
| 3.13c | 1.3–7.6c | <0.01 | |||||||||||||
| Yildiz et al29 | Turkey | Case control¶ | 54 | 61.1 | 10.2 | CIMT >0.8 mm | Carotid USG | 33.3 | S | 7.95 | 2.1–29.7 | 0.001 | — | — | — |
| Sarrafzadegann et al16 | Iran | Cross-sectional | 84 | 43.4 | 7.1 | CIMT (continuous) | Carotid USG | — | NS | 0.05|| | 0–33|| | 0.51|| | — | — | — |
| NS | 0.14# | 0–13.5# | 0.40# | — | — | — |
For WMH.
For PVH.
Hazards ratio (adjusted).
Defined as >40% stenosis or ≥2.5-mm atheromatous plaque in carotid or femoral arteries.
Case control with BAC-positive women as “cases”; a = adjusted OR and 95% CI for medium- vs. low-risk CIMT; b = adjusted OR and 95% CI for high- vs. low-risk CIMT; c = adjusted OR and 95% CI for carotid plaque.
Univariate OR, 95% CI, and P value for common CIMT (derived from logistic regression with BAC as dependent and CIMT as continuous independent variable).
Univariate OR, 95% CI, and P value for internal CIMT (derived from logistic regression with BAC as dependent and CIMT as continuous independent variable).
Age indicates median age in years; BAC, breast arterial calcification; CAD, coronary artery disease; CI, confidence interval; CIMT, carotid intima media thickness; ICD-9, International Classification of Diseases, Ninth Revision; MRI, magnetic resonance imaging; N, sample size; NS, nonsignificant; OR, odds ratio; PAD, peripheral arterial disease; PVH, periventricular hypodensities; S, significant; TIA, transient ischemic attack; USG, ultrasound; WMH, white matter hypodensities.
Breast Arterial Calcification, Coronary Artery Disease, Cardiovascular Disease, and Cardiovascular Mortality
We identified 19 studies with a total of 33,583 subjects enrolled across all studies. The mean age of women ranged from 43.416 to 66.717 years. Most studies included postmenopausal women older than 40 years of age, with only 1 study including premenopausal women.16 Only 4 of 19 studies did not show an association between BAC and CAD,10,12,13,16 13 of 19 (68%) studies showed a clear cut, statistically significant association, and 2 of 19 studies showed significant association only when obstructive CAD (≥50% stenosis) was considered.11,14 Obstructive CAD was generally defined as ≥50% coronary artery stenosis, except by Sarrafzadegann et al,16 who used ≥50% stenosis in left main coronary artery and/or ≥75% stenosis in other epicardial arteries as the definition of obstructive CAD. There was 1 prospective cohort study,7 2 retrospective cohort studies,8,9 9 case-control studies with CAD,10–18 1 case-control study with BAC,19 and 7 cross-sectional (prevalence) studies.20–25 Table 1 and Figures 2–4 show crude and adjusted ORs calculated from data extracted from each study. Please note that some of the crude ORs and P values shown in Table 1 may not be quoted in full text articles of the respective studies, because we calculated these values by a repeat analysis of data based on the information provided in the methods and results sections of each study (see Statistical Analyses under Methods section for details). In addition, we were able to access the full-study database of Zgheib et al,11 because this study was conducted at our institution (Staten Island University Hospital).
FIGURE 2.
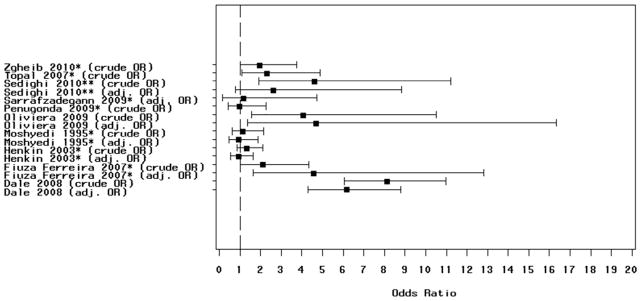
Figure showing crude and adjusted odds ratios (OR) with 95% confidence intervals of case-control studies examining the relation between breast arterial calcification and angiographic coronary artery disease (CAD). *Obstructive CAD (≥50% stenosis) considered as endpoint and ** self-reported CAD used with breast arterial calcification positive considered as case.
FIGURE 4.
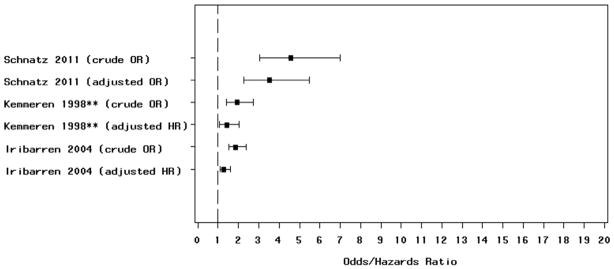
Figure showing crude and adjusted incidence odds ratios (ORs)/hazards ratios with 95% confidence intervals of prospective and retrospective cohort studies examining the relation between breast arterial calcification and coronary artery disease, cardiovascular disease, and cardiovascular mortality. **Cardiovascular mortality used as endpoint.
All crude and adjusted prevalence and incidence ORs/HRs were statistically significant in cross-sectional and cohort studies. Most case-control studies used angiographically proven CAD as the definition of CAD. For case-control studies, the relation between BAC and obstructive CAD was tenuous, with only 3 of 7 studies involving angiographic obstructive CAD as the endpoint showing a statistically significant relation (Fig. 2; Table 1). One case-control study17 used angiographically documented CAD (obstructive plus nonobstructive) or history of at least one episode of acute myocardial infarction as the definition of the case, and another study18 used only angiographically documented CAD (obstructive plus nonobstructive) as the definition of case. Both studies showed a statistically significant relation between BAC and CAD.
Table 3 shows sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of BAC for primary endpoint of each study in this group. For cross-sectional studies, BAC shows high specificity for coexisting CAD/atherosclerotic CVD, ranging from 84.5%24 to 93%.22 The sensitivity, PPV, and NPV of BAC to detect coexisting CAD are low, with a maximum sensitivity of 50%.25 The cohort studies also report high specificity of BAC for incident CAD morbidity and mortality (88%–97%), with low sensitivity, PPV, and NPV. Case-control studies incorporating the gold standard definition of CAD (ie, angiography) showed a higher PPV (35%–70%) and a higher sensitivity (40%–69%). The specificity of BAC to detect angiographic CAD was generally high, except for 2 studies.10,13
TABLE 3.
Studies Showing Sensitivity, Specificity, PPV, and NPV of BAC for CAD, Cardiovascular Disease, and Cardiovascular Mortality
| Study | Outcome | Sensitivity, % | Specificity, % | PPV, % | NPV, % |
|---|---|---|---|---|---|
| Schnatz et al7 | CAD | 39.1 | 87.8 | 20.8 | 5.4 |
| Iribarren et al8 | CAD | 5 | 97.3 | 29.6 | 18.1 |
| Kemmeren et al9 | CV death | 16.2 | 91 | 4.1 | 2.1 |
| Penugonda et al10 | CAD* | 60.4 | 39 | 56.1 | 56.8 |
| Zgheib et al11 | CAD* | 39.7 | 74.6 | 64.9 | 48.6 |
| Henkin et al12 | CAD* | 43.9 | 62.9 | 62.6 | 55.9 |
| Moshyedi et al13 | CAD* | 57.4 | 46.3 | 35 | 31.7 |
| Topal et al14 | CAD* | 52.1 | 68 | 51 | 31.1 |
| Fiuza Ferreira et al15 | CAD* | 48.5 | 69.2 | 61.5 | 43 |
| Sarrafzadegann et al16 | CAD* | 8.8 | 94 | 50 | 39.7 |
| Oliveira et al17 | CAD | 57.5 | 75 | 69.7 | 36.2 |
| Dale et al18 | CAD | 69.2 | 78.4 | 48.9 | 10.5 |
| Sedighi et al19 | CAD | 70.4 | 66.1 | 24.1 | 6.4 |
| Crystal et al20 | ASCVD | 38 | 86.4 | 35.5 | 12.3 |
| Rotter et al21 | ASCVD | 44.3 | 87.7 | 16 | 3.3 |
| Ferreira et al22 | CVD | 28.5 | 93 | 23.1 | 53.4 |
| Van Noord et al23 | MI | 16.6 | 91.2 | 8.5 | 4.3 |
| Kataoka et al24 | CAD | 33.3 | 84.3 | 3.1 | 1.2 |
| Dale et al25 | CAD | 50 | 86.5 | 22.3 | 4.3 |
Obstructive CAD only (≥50% coronary artery stenosis on angiography).
ASCVD indicates atherosclerotic cardiovascular disease; BAC, breast arterial calcification; CAD, coronary artery disease; CV, cardiovascular; CVD, cardiovascular disease; MI, myocardial infarction; NPV, negative predictive value; PPV, positive predictive value.
Breast Arterial Calcification, Stroke, Cerebral Artery Disease, and Stroke Mortality
We found 7 studies which examined the relation between BAC and stroke,7–9,20,21,23,24 and 1 study26 between BAC and cerebral artery disease detected on brain magnetic resonance imaging (MRI; Table 2). Not all the studies were primarily designed to evaluate the relation between BAC and stroke. One study was a prospective cohort,7 2 studies were retrospective cohorts,8,9 and 4 studies were cross-sectional.20,21,23,24 There were a total of 30,673 subjects enrolled across 7 studies, and the mean age of the subjects ranged from 56 to 63 years. Five of 7 studies (71.4%) reported a statistically significant association between BAC and stroke. Table 2 and Figure 5 show the crude and adjusted ORs with 95% CIs.
FIGURE 5.
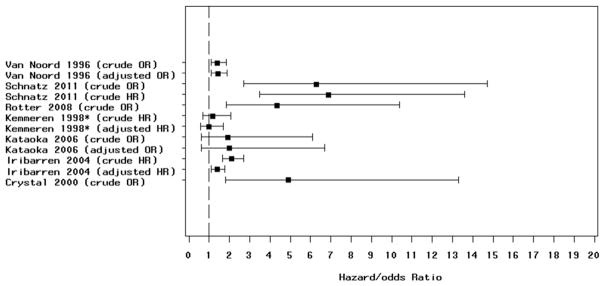
Figure showing crude and adjusted odds ratios (OR)/hazards ratios with 95% confidence intervals of studies examining the relation between breast arterial calcification and stroke and stroke mortality. *Mortality from stroke used as endpoint.
Breast Arterial Calcification, Peripheral Arterial Disease, Carotid Intima Media Thickness, and Coronary Artery Calcification
There were 2 studies showing the association between BAC and PAD,27,28 3 between BAC and CIMT,16,19,29 and 2 between BAC and CAC.30,31 Table 2 shows description of the studies along with their ORs and 95% CIs. Both the studies looking at BAC and PAD and BAC and CAC, and 2 of 3 (66%) of the studies looking at BAC and CIMT showed a statistically significant relation.
DISCUSSION
We aimed to analyze whether BAC seen on screening mammograms correlates with the occurrence of coronary and noncoronary atheroscleroses. The relation between BAC and traditional CV risk factors, such as diabetes mellitus and hypertension, has been controversial. Some studies show a significant association between BAC and hypertension,19,32,33 whereas others show no such association.4,24,34 Similarly, with diabetes mellitus, some studies show a statistically significant association,6,19,35,36 whereas others show none.4,24,37,38
Breast Arterial Calcification and Cardiovascular Disease
In our review, greater than 3 quarters of the studies, examining an association between BAC and CAD, showed a statistically significant relation. Age was a major confounding factor in the association between BAC and CAD because age is a risk factor for CAD and there is a higher prevalence of BAC with increasing age. We found that 16 of 19 studies had adjusted for age. Although BAC has also been shown to be associated with other confounding CAD risk factors, however, this association has not been consistently observed. Most of the reviewed studies included other CAD risk factors in addition to age in multivariate models where applicable.
There was marked heterogeneity in the definition of CAD across the studies, with some studies defining CAD as angiographically proven coronary artery stenosis and others using self-reported CAD or hospital discharge data. Two studies used atherosclerotic CVD (defined as self-reported angina, history of myocardial infarction or coronary artery bypass graft, or abnormal coronary angiogram or stroke).20,21 Ferreira et al22 used CVD, defined as atherosclerotic CVD plus congestive heart failure. Kemmeren et al9 used CV mortality according to the ICD-9 criteria (defined as death from coronary heart disease, cerebrovascular diseases, heart failure, complications of heart disease, or sudden cardiac death). Oliveira et al17 used history of myocardial infarction or angiographically documented CAD, and Van Noord et al23 used only acute myocardial infarction as the endpoint.
Breast Arterial Calcification and Angiographic Coronary Artery Disease (Case Control)
Seven studies looked at the relation between BAC and obstructive CAD diagnosed by the “gold standard” coronary angiography. These studies recruited patients undergoing cardiac catheterization for high-risk chest pain or abnormal stress test. Subsequently, the prevalence of BAC in angiographically proven obstructive CAD (≥50% stenosis, except Sarrafzadegann et al16) cases was compared with controls without CAD. Only 3 of 7 studies showed significant P values in the association between BAC and obstructive CAD.11,14,15 In 211,14 of these, the association between BAC and obstructive plus nonobstructive CAD was not statistically significant, but became significant (P < 0.05) when only obstructive CAD was considered. We reviewed a recently conducted meta-analysis looking at pooled data from 5 of the 7 studies, with a total of 927 subjects, showing an OR of 1.59 (95% CI, 1.21–2.09), thus signifying an overall statistically significant association between BAC and angiographically proven obstructive CAD.39 The 2 studies not included in the meta-analysis (Penugonda et al10 and Sarrafzadegann et al16) were not statistically significant, but they were limited due to small sample sizes. The P values of Zgheib et al11 and Topal et al14 were not adjusted for the confounding effect of age, which precludes any inferences based solely on crude OR. In fact, only 1 study15 showed a strong relation between BAC and obstructive CAD after adjustment for age and other potential confounders. Moshyedi et al13 showed that in women younger than 59 years, BAC had a statistically significant association with CAD. Quantification revealed no relation between intensity of BAC and severity of CAD.14,15 All these studies had high CAD prevalence (33.5%–64.9%) because they consisted of a high-risk population undergoing cardiac catheterization.
Two other case-control studies, Dale et al18 and Oliveira et al,17 compared angiographically documented CAD cases to control groups derived from a general population that did not undergo any coronary angiography. Both these studies showed a strong association between BAC and CAD, which remained robust in multivariate analysis, with multivariate ORs of 6.218 and 4.7,17 respectively. Sedighi et al19 compared self-reported CAD prevalence in BAC-positive women with age-matched BAC-negative controls showing a significant age-matched univariate OR; however, it was nonsignificant in multivariate analysis.
Breast Arterial Calcification and Prevalent Coronary Artery Disease (Cross-Sectional)
Most cross-sectional studies used patient-reported CAD or CVD as the endpoint. Van Noord et al23 reported an adjusted relative risk of 1.8 (95% CI, 1.1–2.9) between prevalent myocardial infarction and BAC. We were able to calculate a crude OR of 1.76 (1.5–2.1) of prevalent BAC and CVD (defined as history of myocardial infarction, stroke, transient ischemic attack, or the use of CV drugs) from Kemmeren et al.9 All cross-sectional studies showed significant adjusted cross-sectional ORs (Table 1 and Fig. 3). These studies had large sample sizes, ranging from 30,722 to 12,084.23 Concomitant existence of BAC and CAD suggests that BAC is a marker of underlying CAD and may represent atherosclerosis elsewhere in the body.
FIGURE 3.
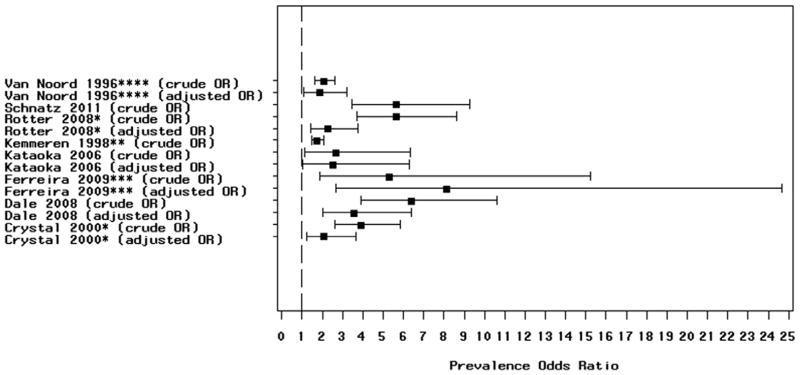
Figure showing crude and adjusted prevalence odds ratios (ORs)/hazards ratios with 95% confidence intervals of cross-sectional studies examining the relation between breast arterial calcification and coronary artery disease, cardiovascular disease (CVD) and cardiovascular mortality. *Atherosclerotic CVD defined as self-reported angina, history of myocardial infarction or coronary artery bypass graft, or abnormal coronary angiogram or stroke; **cardiovascular mortality; ***CVD defined as coronary artery disease or history of myocardial infarction or stroke or congestive heart failure; and ****prevalent myocardial infarction, used as endpoint.
Breast Arterial Calcification and Incident Coronary Artery Disease (Cohort)
Schnatz et al7 did the lone prospective cohort study looking at the relation between BAC and incident self-reported CAD. The 5-year incidence of CAD in those with BAC was 6.3% compared with 2.3% in those without BAC. Iribarren et al8 conducted a retrospective study with 12,761 women and ascertained outcomes such as CAD and stroke by hospital discharge and death records, with a median follow-up of 25 years. They showed a 32% increased risk of CAD in a multivariate analysis. Kemmeren et al9 studied 12,084 patients with CV mortality as the endpoint and a follow-up period of 16–19 years. The age-adjusted HR for mortality from CAD was 1.47 and for overall CV mortality (mortality from CAD, stroke, heart failure, and sudden cardiac arrest) was 1.35. These studies show that women with BAC on screening mammography are at an increased risk of developing or dying from CAD in the subsequent years (Fig. 4).
Sensitivity, Specificity, and Predictive Values
In general, BAC has low sensitivity and predictive values, but high specificity, ranging from 39%10 to 97%8 for coexisting or incident CAD endpoints. Case-control studies using angiography showed a higher sensitivity and PPV, possibly because of the higher prevalence of CAD in this population owing to their study design.
Breast Arterial Calcification and Stroke
Stroke was studied as part of the definition of CVD (CAD plus stroke);20,21,24 other studies looked at stroke as a secondary endpoint.7,23 Only one study8 was primarily designed to study the relation between BAC and stroke. The definition of endpoints in different studies was heterogeneous. Kemmeren et al9 included mortality from stroke (as per ICD-9 coding) as the endpoint, whereas Van Noord et al23 included transient ischemic attack in addition to stroke as the endpoint. Most studies included patient reporting as the method of detecting stroke, whereas Iribarren et al8 used hospital discharge data. Again, age was found to be the major confounding factor in this relation, and 5 of 8 studies8,9,23,24,26 reported multivariate ORs/HRs adjusted for age and/or other confounding variables (Table 2).
The study by Schnatz et al7 of the relation between BAC and incident CAD also reported stroke as a secondary outcome. This study reported both prevalent stroke and incident stroke at baseline. The OR of prevalent stroke at baseline was 6.3 (95% CI, 2.7–14.7), and the 5-year incidence of stroke was 8.7% vs. 1.4% in the 2 BAC groups with crude incidence OR of 6.9 (95% CI, 3.5–13.6). Iribarren et al8 reported an age-adjusted multivariate HR of 1.41 (95% CI, 1.1–1.8) for the relation between BAC and ischemic stroke. Kemmeren et al9 reported no significant association between BAC and mortality from stroke, with adjusted OR of 0.98 (95% CI, 0.56–1.71).
All cross-sectional studies used self-reported stroke as the endpoint. Crystal et al20 and Rotter et al21 included stroke as part of atherosclerotic CVD, and crude ORs for stroke were 4.9 and 4.4, respectively (Table 2). Van Noord et al23 looked at the association between BAC and prevalent strokes and reported an adjusted OR of 1.4 (95% CI, 1.1–1.9). Kataoka et al24 showed a statistically significant association of BAC with prevalent CAD, but not with prevalent stroke (adjusted OR, 2.02; 95% CI, 0.61–6.69).
Breast Arterial Calcification and Cerebral Artery Disease
The studies discussed earlier used subjective methods such as patient reporting for detecting stroke. A more objective way to demonstrate stroke is an MRI of the brain. Only one study was identified in the literature, which examined the association between BAC and MRI-proven cerebral artery disease,26 but this study did not use stroke as the endpoint. It used microvascular ischemic changes, demonstrated by either white matter hypodensities (WMHs) or periventricular hypodensities (PVHs), as the endpoint.
The investigators26 recruited 168 Korean women with age 40–78 years who underwent screening mammograms and brain MRI to study the relation between BAC and T2 hyperintensities on brain MRI (WMH and PVH), which are considered precursors for stroke.40–42 Cerebral artery disease was defined as grades 2 and 3 WMH or grade 3 PVH. The adjusted OR for WMH was 6.86 (1.83–25.7) and for PVH was 9.04 (1.2–68.3). Thus, BAC may be a marker of higher risk of future stroke in women as demonstrated by its association with precursor WMH in this study.
Breast Arterial Calcification and Systemic Vascular Disease
We found 2 studies looking at the relation between BAC and peripheral vessel atherosclerosis.27,28 Dale et al27 looked at women undergoing mammography and identified those with documented PAD using hospital data. They reported a prevalent OR of 3.09, with sensitivity and specificity of BAC being 42% and 80%, respectively. Markopoulos et al28 divided study subjects into 3 groups as follows: those undergoing mammography, those undergoing vascular surgery, and BAC-negative women undergoing breast surgery. They showed a relation between BAC and systemic vascular disease in carotid or femoral arteries detected by duplex scan.
Breast Arterial Calcification and Carotid Intima Media Thickness
CIMT is itself a marker of atherosclerosis and it has been proposed as a surrogate marker for underlying CAD.43 There are 3 studies looking at the association between BAC and carotid atherosclerosis detected by CIMT. CIMT greater than 0.8 mm was considered high risk, and ORs were calculated in reference to that value from study data (Table 2). Sedighi et al19 compared 79 subjects with BAC to 125 age-matched controls and subjected them to carotid ultrasound to measure CIMT. This study showed an association between carotid plaque and BAC, although the association between BAC and IMT was stronger. Yildiz et al29 conducted a similar study and reported mean CIMT of 0.87 ± 0.17 in BAC-positive women compared with 0.60 ± 0.19 in BAC-negative women with a coefficient of 0.463 (P < 0.001). However, Sarrafzadegann et al,16 who included only premenopausal women referred for coronary angiography, failed to show any statistically significant relation.
Breast Arterial Calcification and Coronary Computerized Tomography
Coronary calcification represents chronic atherosclerotic plaque burden and usually represents more advanced lesions. The use of CAC improves the prediction of risk for future CAD.44 There is, however, a difference in etiology of the 2 types of calcification, with BAC being predominantly medial compared with CAC which is predominantly intimal calcium deposition.30 Maas et al30 randomly selected 499 women undergoing screening mammograms and subjected them to multislice computerized tomography (MSCT) to detect the amount of CAC. Seventy-six percent of the women with BAC had CAC detected on MSCT compared with only 49% of women without BAC, with an adjusted OR of 2. Another study by Pecchi et al,31 conducted in an Italian population involving only 74 patients, showed a strong correlation between BAC and CAC on MSCT.
Most studies have used patient self-reporting or hospital chart reviews as the method of detecting CAD, which is not very accurate. Other studies have reported coronary angiography, which is the gold standard. However, the drawback of such studies is that they include a high-risk CAD population and inferences from these studies cannot be extended to a low-risk general population. An ideal way to study the relation between BAC and CAD would be to subject all asymptomatic patients undergoing screening mammograms to coronary angiography to detect CAD. However, such large-scale population-based angiographies are neither feasible nor cost effective. Therefore, the best way to accurately document CAD in an asymptomatic population would be to use noninvasive testing such as cardiac computerized tomography for evaluating the coronary circulation.
Breast Arterial Calcification and Smoking
Interestingly, many studies have reported a paradoxical inverse relation between BAC and smoking8,9,20,23,24 (Table 4). The exact cause of this phenomenon is unclear, especially because smoking has been shown to increase CAC.45 One explanation may be that smoking-related inflammation plays only a little role in mammary artery calcifications.5 CV events in smokers are more related to inflammation, thrombosis, and endothelial dysfunction than to vascular calcification.46,47 Other theories are the selective survival of smokers after the age of 50 and the effect of smoking on weight or estrogen metabolism.23
TABLE 4.
Studies Showing Relation Between BAC and Smoking
| Study | Country | N | OR | 95% CI | P |
|---|---|---|---|---|---|
| Kataoka et al24 | United Kingdom | 1590 | 0.46 | 0.23–0.94 | <0.05 |
| Iribarren et al8 | United States | 12,761 | 0.45 | 0.31–0.63 | <0.001 |
| Van Noord et al23 | The Netherlands | 12,084 | 0.41 | 0.35–0.49 | <0.001 |
| Crystal et al20 | Israel | 865 | 0.24 | 0.14–0.43 | <0.001 |
| Maas et al30 | The Netherlands | 499 | 0.6 | 0.25–1.39 | >0.05 |
| Schnatz et al7 | United States | 1454 | 0.53 | 0.26–1.06 | 0.068 |
| Rotter et al21 | United States | 1919 | 0.41 | 0.22–0.77 | 0.004 |
| Penugonda et al10 | United States | 94 | 0.31 | 0.12–0.82 | 0.015 |
| Henkin et al12 | Israel | 319 | 0.35 | 0.19–0.65 | <0.001 |
| Sedighi et al19 | Iran | 204 | 0.11 | 0.01–0.86 | 0.01 |
CI indicates confidence interval; BAC, breast arterial calcification; N, sample size; OR, odds ratio.
LIMITATIONS
There was a marked heterogeneity in the definition of endpoints (CAD, PAD, or stroke) across all the studies. Adjustment for age was not done in all studies. The population enrolled across different studies was also heterogeneous, with some studies enrolling younger women16 and others enrolling solely postmenopausal women.22,24 There was also a potential for an inherent selection bias in all these studies, as the population choosing to undergo screening mammograms may be systematically different from those not choosing to undergo the same. Moreover, publication bias (positive results getting published easily) is a consideration.
CONCLUSIONS
Our analysis of the published data suggests that BAC is associated with CVD, stroke, CIMT, and CAC. BAC’s relation with angiographic CAD is uncertain and presently debatable. Future prospective studies and an accumulation of clinical knowledge may further elucidate the place of BAC among the indicators of risk of coronary and systemic atherosclerosis.
RECOMMENDATIONS TO THE RADIOLOGIST
Given the evidence available from the current literature, we recommend that mammograms be carefully scrutinized for the presence of BAC. BAC, if present, should be mentioned in the mammography report and should be flagged for the clinician to correlate clinically with the presence of coronary or systemic atherosclerosis. With the available evidence, we do not recommend any further testing solely based on the presence of BAC at this time.
Footnotes
Disclosure: The authors have no conflicts of interest to report.
References
- 1.Micheletti RG, Fishbein GA, Currier JS, et al. Mönckeberg sclerosis revisited: a clarification of the histologic definition of Mönckeberg sclerosis. Arch Pathol Lab Med. 2008;132:43–47. doi: 10.5858/2008-132-43-MSRACO. [DOI] [PubMed] [Google Scholar]
- 2.Kim H, Greenberg JS, Javitt MC. Breast calcifications due to Mönckeberg medial calcific sclerosis. Radiographics. 1999;19:1401–1403. doi: 10.1148/radiographics.19.5.g99se221401. [DOI] [PubMed] [Google Scholar]
- 3.Taşkin F, Akdilli A, Karaman C, et al. Mammographically detected breast arterial calcifications: indicators for arteriosclerotic diseases? Eur J Radiol. 2006;60:250–255. doi: 10.1016/j.ejrad.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Akinola RA, Ogbera OA, Onakoya JA, et al. Mammograms and breast arterial calcifications: looking beyond breast cancer: a preliminary report. BMC Res Notes. 2011;4:207. doi: 10.1186/1756-0500-4-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nielsen BB, Holm NV. Calcification in breast arteries. The frequency and severity of arterial calcification in female breast tissue without malignant changes. Acta Pathol Microbiol Immunol Scand A. 1985;93:13–16. [PubMed] [Google Scholar]
- 6.Sickles EA, Galvin HB. Breast arterial calcification in association with diabetes mellitus: too weak a correlation to have clinical utility. Radiology. 1985;155:577–579. doi: 10.1148/radiology.155.3.4001355. [DOI] [PubMed] [Google Scholar]
- 7.Schnatz PF, Marakovits KA, O’Sullivan DM. The association of breast arterial calcification and coronary heart disease. Obstet Gynecol. 2011;117(2 Pt 1):233–241. doi: 10.1097/AOG.0b013e318206c8cb. [DOI] [PubMed] [Google Scholar]
- 8.Iribarren C, Go AS, Tolstykh I, et al. Breast vascular calcification and risk of coronary heart disease, stroke, and heart failure. J Womens Health (Larchmt) 2004;13:381–9. doi: 10.1089/154099904323087060. discussion 390. [DOI] [PubMed] [Google Scholar]
- 9.Kemmeren JM, van Noord PA, Beijerinck D, et al. Arterial calcification found on breast cancer screening mammograms and cardiovascular mortality in women: the DOM Project. Doorlopend Onderzoek Morbiditeit en Mortaliteit. Am J Epidemiol. 1998;147:333–341. doi: 10.1093/oxfordjournals.aje.a009455. [DOI] [PubMed] [Google Scholar]
- 10.Penugonda N, Billecke SS, Yerkey MW, et al. Usefulness of breast arterial calcium detected on mammography for predicting coronary artery disease or cardiovascular events in women with angina pectoris and/or positive stress tests. Am J Cardiol. 2010;105:359–361. doi: 10.1016/j.amjcard.2009.09.039. [DOI] [PubMed] [Google Scholar]
- 11.Zgheib MH, Buchbinder SS, Abi Rafeh N, et al. Breast arterial calcifications on mammograms do not predict coronary heart disease at coronary angiography. Radiology. 2010;254:367–373. doi: 10.1148/radiol.09090102. [DOI] [PubMed] [Google Scholar]
- 12.Henkin Y, Abu-Ful A, Shai I, et al. Lack of association between breast artery calcification seen on mammography and coronary artery disease on angiography. J Med Screen. 2003;10:139–142. doi: 10.1177/096914130301000308. [DOI] [PubMed] [Google Scholar]
- 13.Moshyedi AC, Puthawala AH, Kurland RJ, et al. Breast arterial calcification: association with coronary artery disease. Work in progress. Radiology. 1995;194:181–183. doi: 10.1148/radiology.194.1.7997548. [DOI] [PubMed] [Google Scholar]
- 14.Topal U, Kaderli A, Topal NB, et al. Relationship between the arterial calcification detected in mammography and coronary artery disease. Eur J Radiol. 2007;63:391–395. doi: 10.1016/j.ejrad.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 15.Fiuza Ferreira EM, Szejnfeld J, Faintuch S. Correlation between intramammary arterial calcifications and CAD. Acad Radiol. 2007;14:144–150. doi: 10.1016/j.acra.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Sarrafzadegann N, Ashrafi F, Noorbakhsh M, et al. Association of breast artery calcification with coronary artery disease and carotid intima-media thickness in premenopausal women. East Mediterr Health J. 2009;15:1474–1482. [PubMed] [Google Scholar]
- 17.Oliveira EL, Freitas-Junior R, Afiune-Neto A, et al. Vascular calcifications seen on mammography: an independent factor indicating coronary artery disease. Clinics (Sao Paulo) 2009;64:763–767. doi: 10.1590/S1807-59322009000800009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dale PS, Mascarhenas C, Richards M, et al. Mammography as a screening tool for coronary artery disease. J Surg Res. 2008;148:1–6. doi: 10.1016/j.jss.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 19.Sedighi N, Radmard AR, Radmehr A, et al. Breast arterial calcification and risk of carotid atherosclerosis: focusing on the preferentially affected layer of the vessel wall. Eur J Radiol. 2011;79:250–256. doi: 10.1016/j.ejrad.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Crystal P, Crystal E, Leor J, et al. Breast artery calcium on routine mammography as a potential marker for increased risk of cardiovascular disease. Am J Cardiol. 2000;86:216–217. doi: 10.1016/s0002-9149(00)00860-2. [DOI] [PubMed] [Google Scholar]
- 21.Rotter MA, Schnatz PF, Currier AA, Jr, et al. Breast arterial calcifications (BACs) found on screening mammography and their association with cardiovascular disease. Menopause. 2008;15:276–281. doi: 10.1097/gme.0b013e3181405d0a. [DOI] [PubMed] [Google Scholar]
- 22.Ferreira JA, Pompei LM, Fernandes CE, et al. Breast arterial calcification is a predictive factor of cardiovascular disease in Brazilian postmenopausal women. Climacteric. 2009;12:439–444. doi: 10.1080/13697130902957287. [DOI] [PubMed] [Google Scholar]
- 23.van Noord PA, Beijerinck D, Kemmeren JM, et al. Mammograms may convey more than breast cancer risk: breast arterial calcification and arteriosclerotic related diseases in women of the DOM cohort. Eur J Cancer Prev. 1996;5:483–487. [PubMed] [Google Scholar]
- 24.Kataoka M, Warren R, Luben R, et al. How predictive is breast arterial calcification of cardiovascular disease and risk factors when found at screening mammography? AJR Am J Roentgenol. 2006;187:73–80. doi: 10.2214/AJR.05.0365. [DOI] [PubMed] [Google Scholar]
- 25.Dale PS, Richards M, Mackie GC. Vascular calcifications on screening mammography identify women with increased risk of coronary artery disease and diabetes. Am J Surg. 2008;196:537–540. doi: 10.1016/j.amjsurg.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Ahn KJ, Kim YJ, Cho HJ, et al. Correlation between breast arterial calcification detected on mammography and cerebral artery disease. Arch Gynecol Obstet. 2011;284:957–964. doi: 10.1007/s00404-010-1742-4. [DOI] [PubMed] [Google Scholar]
- 27.Dale PS, Graham J, Nichols KW, et al. Mammography as a screening tool for peripheral vascular disease. Am J Surg. 2006;192:488–491. doi: 10.1016/j.amjsurg.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Markopoulos C, Mantas D, Revenas K, et al. Breast arterial calcifications as an indicator of systemic vascular disease. Acta Radiol. 2004;45:726–729. doi: 10.1080/02841850410008261. [DOI] [PubMed] [Google Scholar]
- 29.Yildiz S, Yildiz A, Ertug N, et al. Association of breast arterial calcification and carotid intima-media thickness. Heart Vessels. 2008;23:376–382. doi: 10.1007/s00380-008-1058-5. [DOI] [PubMed] [Google Scholar]
- 30.Maas AH, van der Schouw YT, Atsma F, et al. Breast arterial calcifications are correlated with subsequent development of coronary artery calcifications, but their aetiology is predominantly different. Eur J Radiol. 2007;63:396–400. doi: 10.1016/j.ejrad.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Pecchi A, Rossi R, Coppi F, et al. Association of breast arterial calcifications detected by mammography and coronary artery calcifications quantified by multislice CT in a population of post-menopausal women. Radiol Med. 2003;106:305–312. [PubMed] [Google Scholar]
- 32.Cetin M, Cetin R, Tamer N, et al. Breast arterial calcifications associated with diabetes and hypertension. J Diabetes Complications. 2004;18:363–366. doi: 10.1016/j.jdiacomp.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Cetin M, Cetin R, Tamer N. Prevalence of breast arterial calcification in hypertensive patients. Clin Radiol. 2004;59:92–95. doi: 10.1016/j.crad.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 34.Maas AH, van der Schouw YT, Beijerinck D, et al. Arterial calcifications seen on mammograms: cardiovascular risk factors, pregnancy, and lactation. Radiology. 2006;240:33–38. doi: 10.1148/radiol.2401050170. [DOI] [PubMed] [Google Scholar]
- 35.Baum JK, Comstock CH, Joseph L. Intramammary arterial calcifications associated with diabetes. Radiology. 1980;136:61–62. doi: 10.1148/radiology.136.1.7384525. [DOI] [PubMed] [Google Scholar]
- 36.Milosević Z, Bjekić J, Radulović S, et al. Clinical significance of intramammary arterial calcifications in women with diabetes mellitus. Vojnosanit Pregl. 2004;61:163–167. doi: 10.2298/vsp0402163m. [DOI] [PubMed] [Google Scholar]
- 37.Schmitt EL, Norbeck JM, Threatt B. Incidence of mammary intra-arterial calcification: an age-matched control study. South Med J. 1985;78:1440–1442. doi: 10.1097/00007611-198512000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Schmitt EL, Threatt BA. Relationship of mammographic intra-arterial calcifications and diabetes. South Med J. 1984;77:988–989. doi: 10.1097/00007611-198408000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Abi Rafeh N, Castellanos MR, Khoueiry G, et al. Association between coronary artery disease diagnosed by coronary angiography and breast arterial calcifications on mammography: meta-analysis of the data. J Womens Health (Larchmt) 2012;21:1053–1058. doi: 10.1089/jwh.2011.3388. [DOI] [PubMed] [Google Scholar]
- 40.Streifler JY, Eliasziw M, Benavente OR, et al. North American Symptomatic Carotid Endarterectomy Trial Group. Development and progression of leukoaraiosis in patients with brain ischemia and carotid artery disease. Stroke. 2003;34:1913–1916. doi: 10.1161/01.STR.0000080939.39414.83. [DOI] [PubMed] [Google Scholar]
- 41.Vermeer SE, Hollander M, van Dijk EJ, et al. Rotterdam Scan Study. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003;34:1126–1129. doi: 10.1161/01.STR.0000068408.82115.D2. [DOI] [PubMed] [Google Scholar]
- 42.Kuller LH, Longstreth WT, Jr, Arnold AM, et al. Cardiovascular Health Study Collaborative Research Group. White matter hyperintensity on cranial magnetic resonance imaging: a predictor of stroke. Stroke. 2004;35:1821–1825. doi: 10.1161/01.STR.0000132193.35955.69. [DOI] [PubMed] [Google Scholar]
- 43.Bots ML. Carotid intima-media thickness as a surrogate marker for cardiovascular disease in intervention studies. Curr Med Res Opin. 2006;22:2181–2190. doi: 10.1185/030079906X148472. [DOI] [PubMed] [Google Scholar]
- 44.Arad Y, Spadaro LA, Goodman K, et al. Predictive value of electron beam computed tomography of the coronary arteries. 19-month follow-up of 1173 asymptomatic subjects. Circulation. 1996;93:1951–1953. doi: 10.1161/01.cir.93.11.1951. [DOI] [PubMed] [Google Scholar]
- 45.Oei HH, Vliegenthart R, Hofman A, et al. Risk factors for coronary calcification in older subjects. The Rotterdam Coronary Calcification Study. Eur Heart J. 2004;25:48–55. doi: 10.1016/j.ehj.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 46.FitzGerald GA, Oates JA, Nowak J. Cigarette smoking and hemostatic function. Am Heart J. 1988;115(1 Pt 2):267–271. doi: 10.1016/0002-8703(88)90648-5. [DOI] [PubMed] [Google Scholar]
- 47.Martin JL, Wilson JR, Ferraro N, et al. Acute coronary vasoconstrictive effects of cigarette smoking in coronary heart disease. Am J Cardiol. 1984;54:56–60. doi: 10.1016/0002-9149(84)90303-5. [DOI] [PubMed] [Google Scholar]


