Abstract
Objectives
To investigate clinical and imaging characteristics associated with diagnostic inaccuracy of computed tomography angiography (CTA) for detecting obstructive coronary artery disease (CAD) defined by quantitative coronary angiography (QCA).
Background
While diagnostic performance metrics of CTA have been reported, there are sparse data on predictors of diagnostic inaccuracy by CTA.
Methods
Clinical characteristics of 291 patients enrolled in the CorE-64 study were examined. Pre-defined CTA segment-level characteristics of all true-positive (N=237), false-positive (N=115), false-negative (N=159), and a random subset of true-negative segments (N=511) for ≥50% stenosis with QCA as reference standard were blindly abstracted in a central core-laboratory. Factors independently associated with corresponding levels of CTA diagnostic inaccuracies were determined.
Results
A calcium score of ≥1 per patient (OR=5.2, 95% confidence interval [CI] =1.1–24.6) and the presence of within-segment calcification (OR=10.2 [5.2–19.8]) predicted false-positive diagnoses. Conversely, absence of within-segment calcification was an independent predictor of false-negative diagnosis (OR=2.0 [1.2–3.5]). Prior percutaneous revascularization was independently associated with patient-level misdiagnosis of obstructive CAD (OR=4.2 [1.6–11.2]). Specific segment characteristics on CTA, notably segment tortuosity (OR=3.5 [2.4–5.1], smaller luminal caliber (OR=0.48 [0.36–0.63] per 1-mm increment) and juxta-arterial vein conspicuity (OR=2.1 [1.4–3.2]) were independently associated with segment-level misdiagnoses. Attaining greater intra-luminal contrast enhancement independently lowered the risk for false-negative diagnosis (OR=0.96 [0.94–0.99], per 10-Hounsfield-Unit increment).
Conclusions
We identified clinical and readily-discernable imaging characteristics predicting inaccurate CT angiography diagnosis of obstructive CAD defined by QCA. Knowledge and appropriate considerations of these features may improve accuracy in clinical CTA interpretation.
Keywords: Computed tomography angiography, accuracy, false-positive, false-negative
INTRODUCTION
Delineating the presence and anatomical extent of obstructive coronary artery disease (CAD) provides vital prognostic information and guides the management of patients with ischemic heart disease (1–4). Accumulating evidence from single- and multicenter studies has demonstrated high accuracy of contemporary computed tomography angiography (CTA) for the diagnosis of obstructive CAD (5–8). Accordingly, CTA has been included in recent American and European recommendations as a valuable noninvasive alternative in the diagnostic evaluation of patients at low-to-intermediate probability for CAD (9,10).
While numerous factors affect the comparison between CTA and invasive quantitative coronary angiography (QCA) (11), there is paucity of data on how clinical and CT angiographic imaging characteristics influence diagnostic accuracy of CTA. Accordingly, the objective of this study is to examine patient clinical and coronary arterial segment characteristics on CTA associated with inaccurate diagnosis of obstructive CAD as defined by QCA.
METHODS
Study Design and Population
The Coronary Artery Evaluation Using 64-Row Multi-detector Computed Tomography Angiography(CorE-64) study is a prospective, multicenter investigation to examine the diagnostic accuracy of CTA to detect CAD in comparison to QCA (12). Its study design and primary results have been reported (7,12). Briefly, patients ≥40 years-old referred for clinically-indicated invasive coronary angiography were recruited from 9 international centers. Exclusion criteria included prior cardiac surgery, percutaneous coronary intervention within past 6 months, history of iodinated-contrast allergy, history of or high risk features for contrast-induced nephropathy, tachyarrhythmia or second/third-degree atrioventricular block, advanced heart failure or aortic stenosis, body-mass-index >40kg/m2 and contraindications to beta-blocker. Patients with Agatston score >600 pre-specified to be excluded from the primary analysis. The study was approved by local institutional review board of all participating centers. All patients provided written informed consent.
Invasive Coronary Angiography Acquisition and Analysis
Clinically-indicated invasive angiography was performed within 30-days after CTA using standardized angiographic techniques. Images were forwarded to the QCA core-laboratory for centralized blinded analysis. The coronary tree was segmented and analyzed according to a modified 19-segments model (7,12,13). All non-stented coronary segments ≥1.5mm in diameter were visually assessed for ≥30% stenoses which were quantified by QCA (CASS-II, QCA,v2.0.1, PIE Medical Imaging, The Netherlands). The most severe stenosis was determined within each segment and for each patient. Significant obstructive CAD was defined on QCA as luminal diameter narrowing of ≥50%.
CTA Acquisition and Post-processing
All images were acquired using a commercially-available CT scanner (Aquilion 64, Toshiba Medical Systems, Tochigi, Japan). Non-contrast imaging was performed using prospective ECG-gating for Agatston calcium scoring. CT angiography was completed with retrospective ECG-gating. Beta-blockers were administrated in compliance with local institutional standards at each center when resting heart-rate was >70bpm to achieve target heart-rate of <70bpm. Sublingual nitroglycerine was routinely prescribed along with weight-based intravenous administration of iopamidol (Isovue 370, Bracco Diagnostics) at 3.5–5.0 ml/s before image acquisition as triggered by bolus-tracking during a single 12–14seconds breath-hold.
Raw data were transferred to CTA core-laboratory for post-processing and blinded interpretation per standardized protocols (7,12). Images were reconstructed at 0.5 mm slice-thickness with 0.3 mm overlap. Multiple systolic and diastolic phases with least cardiac motion were routinely reconstructed with standard (FC43) and as appropriate additional sharper (FC05) kernels. Optimal reconstruction was identified for each vessel from which it was segmented and labeled in accordance with the modified 19-segment model for cross-comparison with QCA (12,13).
CTA Stenosis Interpretation
Two independent CTA readers visually graded each non-stented segment for stenosis according to an ordinal scale (12). All segments with visible luminal narrowing of ≥30% were quantified for maximum percentage luminal diameter stenosis by a semi-automatic contour detection algorithm using commercially-available software (VitreaVersion 3.9.0.1, Vital Images). Segments deemed non-evaluable or with inter-reader visual and/or quantitative stenosis discrepancies crossing 50% threshold underwent consensus grading incorporating a third experienced observer. After finalization of all qualitative and quantitative segmental stenosis measurements independently by both QCA and CTA core-laboratories for the entire trial cohort, an adjudication process was performed to ensure correct cross-modality correspondence of segments as interpreted.
Definitions of CTA Diagnostic Inaccuracy and Abstractions for Inaccuracy-Associated Features
Diagnostic inaccuracy of CTA was examined on both a) per-patient and b) per-segment levels, and was defined as diagnostic discordance between quantitative CTA and reference standard QCA for the presence of ≥50% luminal stenosis. Consistent with CorE-64 primary outcome analysis (7), stented and non-evaluable segments were excluded in this substudy. On patient-based and segment-based levels, overall diagnostic inaccuracy (i.e. misdiagnoses -- all QCA-CTA discordant diagnoses) was further stratified by the a) presence and b) absence of obstructive CAD per reference standard QCA, representing correspondingly false-negative (FN) and false-positive (FP) diagnoses. True-positive (TP) and true-negative (TN) findings were conventionally defined respectively as the correct identification and exclusion of obstructive CAD.
Patient-level factors examined included patient baseline clinical characteristics (demographics, traditional risk factors, prior CAD diagnosis/interventions), physical and laboratory parameters (body-mass-index, serum creatinine, cholesterol), and selected core laboratory-determined CTA acquisition parameters (mean and variability of acquisition heart-rate) and patient-level findings (breathing artifacts and Agatston calcium score) known to impact CTA interpretation.
For this post-hoc analysis, all evaluable coronary segments with TP, FN, and FP diagnoses of obstructive CAD together with a randomly-selected subset of TN-segments were re-evaluated without knowledge of diagnosis or stenosis measurements by either modality for additional prospectively-defined segment-level features. Random selection of TN-segment as referent control was pre-specified in this substudy because characterization of all TN-segments (>3,000) was felt to be impractical. From the entire clinical trial patient cohort, TN-segments in number matched to the total of all TP, FN and FP segments were pre-specified to be randomly selected. To minimize potential effects of clustering, we stipulated a-priori that no more than 5 random TN-segments samples are to be selected from any one individual patient. Segment-level features examined included 1) segment image quality (good--absence of motion or other artifacts; adequate--assessable with minor motion artifacts; poor--assessable with substantial motion/other artifacts; and non-evaluable), 2) segmental-arterial calcification (none/presence), 3) tortuosity (segment assuming ≥1 within-segment arc(s) of visually-estimated ≥60° on multi-planar and/or maximum-intensity projections), 4) vein-crossing (cardiac venous structure(s) visualized as crossing or contacting with arterial segment on maximum-intensity projections of ≤2.5mm slap-thickness), 5) segment reference diameter (most proximal disease-free portion of segment determined by semi-automatic contour detection algorithm with manual contour editing), 6) segment-specific luminal contrast attenuation (mean Hounsfield-Units of cross-sectional region-of-interest excluding wall/plaque/calcification at proximal disease-free portion of segment). All post-hoc segmental characteristics were abstracted from restored multi-planar-reformations, maximum-intensity-projections, and cross-sectional images as utilized for original stenosis assessment. Reference to adjudicated segmentation labeling assured exact correspondence of coronary segments between successive reads and across modalities.
Statistical Analysis
Continuous variables unless otherwise stated are reported as medians with inter-quartile ranges (IQR) and compared using the Kruskal-Wallis test. Categorical data are presented as counts and percentages with comparisons conducted by the Pearson chi-square or Fisher’s exact test. Patient-level features and segment-level CT angiographic characteristics were separately examined for respective relationships with patient-level and segment-level diagnostic inaccuracy of CTA. The respective study samples of the entire cohort (N=291) and their studied segments (N=1022) were stratified for unadjusted pair-wise comparisons of features by diagnostic discordance versus concordance of CTA vs. QCA a) overall (misdiagnosis versus accurate-diagnosis), among subgroups b) with (FN-diagnosis versus TP-diagnosis) and c) without (FP-diagnosis versus TN-diagnosis) obstructive CAD per reference standard QCA. Features significant (P<0.05) on univariable pair-wise comparisons were entered into corresponding multivariable logistic regression models to determine their independent association with inaccurate CTA interpretation expressed as odds for QCA-discordant diagnoses. To account for the clustered nature of segment characteristics within patients, complex sample analyses and generalized estimating equations were utilized for unadjusted and multivariable analyses of segment-level data to compensate for clustering-related underestimation of standard errors. Statistical analyses were performed using SPSS v16.0 (SPSS Inc, Chicago, Illinois). Statistical significance was defined as two-sided p-value <0.05.
RESULTS
Patient-Level Factors in Relation to Patient-Level CTA Diagnostic Inaccuracy
Overall, patients with an inaccurate diagnosis of obstructive CAD by CTA were more likely to have known CAD with prior myocardial infarction (32.4% vs. 17.7%, p=0.035) and/or percutaneous coronary intervention(s) (27.0% vs. 7.1%, p=0.001). Specifically, patients with FN-diagnosis more frequently had previous myocardial infarction (45.8% vs. 25.2%, p=0.038) and percutaneous intervention(s)(33.3% vs. 10.1%, p=0.006). While patients with accurate diagnosis versus misdiagnosis had similar Agatston scores (85 vs. 56, p=0.89), there was a heterogeneous relationship between coronary calcification burden and patient-level inaccuracy. Individuals with TN-diagnosis vs. FP-diagnosis had lower coronary calcification burden (Agatston score:1 vs. 49, p=0.047). Conversely, patients with TP-diagnosis vs. FN-diagnosis had greater calcium scores: 172 vs. 57 (p=0.035). No other patient-level characteristic was significantly associated with CTA diagnostic inaccuracy. The clinical characteristics, acquisition parameters and patient-level findings of CTA examination related to the different patient-level inaccuracies are presented in Appendix-1.
Independent Association Between Patient-Level Factors and CTA Diagnostic Inaccuracy
In multivariable analyses, previous percutaneous coronary intervention was the only patient-level characteristic independently associated with patient-level misdiagnosis – even while considering only non-stented coronary arterial segments (OR=4.18; 95%CI=1.56–11.22). History of prior percutaneous coronary intervention(s) was independently associated with patient-level FN-diagnosis (OR=4.29; 95%CI=1.33–13.79); whereas the presence and greater extent of coronary artery calcification independently conferred lower likelihood of FN-diagnosis (OR=0.96; 95%CI=0.93–0.99; per 10-unit Agatston Score increment). The presence of coronary calcification (positive Agatston score) was the only patient-level feature independently associated with FP-diagnosis (OR=5.22; 95%CI=1.11–24.61; referent: zero Agatston score). These findings were consistent in a series of sensitivity analyses incorporating additional adjustment for previously observed correlates with image quality (14) including body-mass-index, heart-rate (mean and variability) during image acquisition and presence of breathing artifact (data not shown).
Segment Characteristics on CTA in Relation to Segment-level CTA Diagnostic Inaccuracy
The proportional distribution across major coronary vessels of the random TN-segment samples examined and the remaining non-selected TN-samples in the entire trial cohort was not different (P>0.05 for differences -- Appendix-2). The characteristics on CTA examination of all segments with TP, FP and FN diagnoses as well as the random subset of TN-segment samples examined are summarized in Table-1. Compared to correctly diagnosed segments, misdiagnosed segments were less likely to reside in the left-main artery and more likely in the diagonal branches (Table-1a). Of all segments harboring obstructive CAD, those with FN-diagnosis were disproportionally more frequent in the diagonal and obtuse marginal/left-posterolateral branch or ramus-intermedius, but less often in the left-anterior-descending artery (Table-1b). Amongst segments without significant disease, FP-segments were more likely in the left-anterior-descending artery and less likely in the posterior-descending/posterolateral branches of the right coronary artery (Table-1c).
Table 1.
Segment characteristics on CTA according to segment-level diagnostic concordance between CTA and QCA for (a) all studied segments; (b) segments with obstructive CAD on QCA; and (c) segments without obstructive CAD on QCA
| (a) All segments | (b) Segments with obstructive CAD on QCA | (c) Segments without obstructive CAD on QCA | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Concordance (CTA- Accuracy) (TP and TN) (N=748) | Diagnostic Discordance (CTA- Inaccuracy/Misdiagnosis) (FP and FN) (N=274) | P- value* | Diagnostic Concordance (CTA- Accuracy) (TP) (N=237) | Diagnostic Discordance (CTA- Inaccuracy) (FN) (N=159) | P- value* | Diagnostic Concordance (CTA- Accuracy) (TN) (N=511) | Diagnostic Discordance (CTA- Inaccuracy) (FP) (N=115) | P- value* | |
| Segment location | |||||||||
| Left-main artery† | 31(4.1) | 3(1.1) | 0.017 | 2(0.8) | 1(0.6) | 0.81 | 29(5.7) | 2(1.7) | 0.081 |
| LAD† | 187(25.0) | 71(25.9) | 0.77 | 85(35.9) | 30(18.9) | <0.001 | 102(20.0) | 41(35.7) | 0.001 |
| Diagonal branches† | 70(9.4) | 46(16.8) | 0.001 | 19(8.0) | 32(20.1) | 0.001 | 51(10.0) | 14(12.2) | 0.48 |
| RCA† | 145(19.4) | 52(19.0) | 0.89 | 55(23.2) | 31(19.5) | 0.43 | 90(17.6) | 21(18.3) | 0.88 |
| PDA/PLV† | 82(11.0) | 19(6.9) | 0.081 | 9(3.8) | 14(8.8) | 0.76 | 73(14.3) | 5(4.3) | 0.004 |
| LCx† | 109(14.6) | 29(10.6) | 0.11 | 25(10.5) | 9(5.7) | 0.10 | 84(16.4) | 20(17.4) | 0.80 |
| OM/Ramus-intermedius/Left-PLV† | 124(16.6) | 54(19.7) | 0.22 | 42(17.7) | 42(26.4) | 0.038 | 82(16.0) | 12(10.4) | 0.102 |
| Tomographic segment characteristics | |||||||||
| Segment tortuosity† | 111(14.9) | 102(37.5) | <0.001 | 53(22.6) | 66(41.8) | <0.001 | 58(11.4) | 36(31.6) | <0.001 |
| Vein crossing† | 127(17.0) | 79(29.0) | <0.001 | 41(17.4) | 48(30.4) | 0.003 | 86(16.9) | 31(27.2) | 0.005 |
| Motion artifact-related suboptimal segment image quality† | 445(59.5) | 207(75.5) | <0.001 | 157(66.2) | 129(81.1) | 0.001 | 288(56.4) | 78(67.8) | 0.027 |
| Presence of segmental coronary calcification† | 294(39.8) | 164(61.2) | <0.001 | 168(72.4) | 79(51.0) | <0.001 | 126(24.9) | 85(75.2) | <0.001 |
| Segment diameter‡ (mm) | 2.71±0.04 | 2.33±0.04 | <0.001 | 2.66±0.05 | 2.21±0.05 | <0.001 | 2.72±0.04 | 2.50±0.06 | 0.002 |
| Mean segment luminal opacification‡(HU) | 441±8 | 424±10 | 0.093 | 459±10 | 400±12 | <0.001 | 433±9 | 457±12 | 0.078 |
CAD=coronary artery disease, QCA=quantitative coronary angiography; CTA= computed tomography angiography; TP=true-positive; TN=true-negative; FP=false-positive; FN=false-negative, LAD=left anterior descending artery, RCA= right coronary artery, LCx=left circumflex coronary artery, PDA=posterior descending artery, PLV=posterolateral branches, OM=obtuse marginal branches.
Unadjusted complex sample analysis accounted for within-patients clustering;
counts(%);
mean ± standard error.
The angiographic appearances of segments on CTA stratified by diagnostic accuracy a) overall amongst all segments; and within subgroups exclusively b) with and c) without significant stenosis; are summarized in Table-1. Segments with misdiagnosis were more likely to be torturous, of smaller caliber, of suboptimal image quality impaired by motion and other artifacts, containing calcification, and visualized with cardiac vein over-crossing (Table-1a). Segments with FN-diagnosis compared to TP-segments exhibited similar variations in CT angiographic appearances as with overall misdiagnosis, with the exception of paradoxically fewer calcification and additionally lower segment-specific luminal contrast opacification (Table-1b). Segments with FP-diagnosis compared to TN-segments revealed similar differences as observed with overall misdiagnosis (Table-1c).
CT Angiographic Segment-Level Characteristics Independently Predictive of CTA Segment-Level Diagnostic Inaccuracy
The independent association between segment characteristics on CTA and segment-level diagnostic inaccuracy is presented in Table-2. Segment tortuosity, cardiac vein over-crossing and smaller luminal diameter each independently conferred increased odds for CTA misdiagnosis (Table-2a), and specifically FN-diagnosis (Table-2b) and FP-diagnosis (Table-2c). Furthermore, greater luminal contrast enhancement was independently associated with lower likelihood for under-recognizing within-segment stenosis (FN-diagnosis) (Table-2b). While the presence of calcification independently increased odds for overall misdiagnosis (OR=2.49;95%CI=1.73–3.58) and specifically more significantly FP-diagnosis (OR=10.16;95%CI=5.23–19.77)(Figure-1), it conferred reduced odds for FN-diagnosis (OR=0.50;95%CI=0.29–0.86). Conversely, obstructive disease in segment without calcification as in non-calcified atherosclerotic plaque, is more likely to be missed, compared to obstructive disease with calcification in segment, independent of other segment characteristics (OR=2.01;95%CI=1.17–3.46).
Table 2.
Independent association between segment characteristics on CTA and segment-level CTA (a) overall misdiagnosis; (b) false-negative diagnosis; and (c) false-positive diagnosis; with QCA as reference standard.
| (a) Overall Misdiagnosis | (b) False-Negative Diagnosis | (c) False-positive Diagnosis | ||||
|---|---|---|---|---|---|---|
| Odds ratio*(95%CI) | P-value | Odds ratio*(95%CI) | P-value | Odds ratio*(95%CI) | P-value | |
| Segment location | ||||||
| Left-anterior-descending artery† | 1.02(0.27–3.83) | 0.97 | 0.14(0.008–2.390) | 0.17 | 2.59(0.45–14.71) | 0.28 |
| Diagonal branches† | 1.06(0.26–4.40) | 0.94 | 0.22(0.01–4.37) | 0.32 | 1.52(0.20–11.67) | 0.69 |
| Right coronary artery† | 1.17(0.31–4.35) | 0.82 | 0.25(0.01–4.54) | 0.35 | 1.96(0.33–11.47) | 0.46 |
| Right posterior descending artery/right posterolateral branch† | 0.46(0.13–1.67) | 0.24 | 0.17(0.01–3.78) | 0.26 | 0.65(0.09–4.79) | 0.68 |
| Circumflex artery† | 0.56(0.15–2.05) | 0.38 | 0.06(0.01–1.12) | 0.06 | 1.24(0.22–6.93) | 0.81 |
| Obtuse marginal/left posterolateral branches/ramus-intermedius† | 0.79(0.20–3.22) | 0.75 | 0.16(0.01–2.91) | 0.21 | 0.65(0.09–4.79) | 0.68 |
| CT angiographic segment characteristics | ||||||
| Segment tortuosity | 3.54(2.44–5.14) | <0.001 | 3.12(1.89–5.17) | <0.001 | 5.22(3.00–9.11) | <0.001 |
| Vein crossing | 2.13(1.42–3.19) | <0.001 | 2.04(1.14–3.62) | 0.016 | 2.58(1.28–5.17) | 0.008 |
| Motion artifact related suboptimal segment image quality | 1.39(0.98–1.98) | 0.068 | 1.45(0.81–2.62) | 0.21 | 1.30(0.77–2.19) | 0.34 |
| Presence of segmental coronary calcification | 2.49(1.73–3.58) | <0.001 | 0.50(0.29–0.86) | 0.012 | 10.16(5.23–19.77) | <0.001 |
| Segment diameter (per 1mm increment) | 0.48(0.36–0.63) | <0.001 | 0.40(0.25–0.65) | 0.008 | 0.49(0.33–0.73) | <0.001 |
| Mean segment luminal opacification (per 10-HU increment) | 1.00(0.98–1.01) | 0.75 | 0.96(0.94–0.99) | 0.008 | 1.03(1.00–1.05) | 0.056 |
QCA=quantitative coronary angiography; CTA= computed tomography angiography
Generalized estimating equations models accounted for within-patient clustering of segment characteristics.
Left-main artery as referent.
Figure 1.
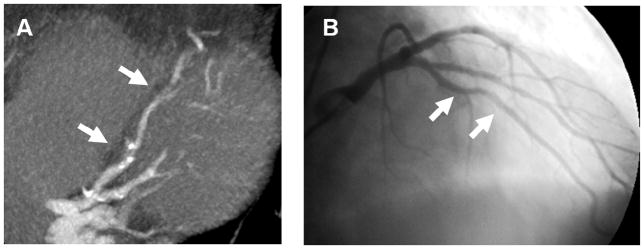
Panel A. An example of false-positive diagnoses by CT angiography at the mid left-anterior-descending artery (arrows) with focal tortuosity, motion and coronary calcification (proximal site) as well as poor contrast opacification in the distal portion.. Panel B. Corresponding conventional angiography without significant stenoses.
After accounting for segment intrinsic CT angiographic characteristics, segment location per major vessel categories within the coronary tree was no longer found to be associated with segment-level diagnostic inaccuracy (Table-2a–c). Furthermore, patient-level parameters correlating with patient-level diagnostic performance as observed in this study (e.g. history of CAD) or conceivably image quality (body-mass-index, heart-rate, breathing or ectopy during acquisition) when added to the models were not found to affect the segment-level results or be associated with segment-level diagnostic inaccuracy (data not shown).
DISCUSSION
While the diagnostic accuracy of CTA for detecting CAD has been extensively delineated, few data are available addressing factors predicting its diagnostic inaccuracy (15–18). Existing data in this regard were derived from single-center experiences on modest patient and segment samples of which characteristics were qualitatively determined without case–control comparisons (15–18). To our best knowledge, this is the first study to report patient clinical and their coronary arterial segment CT angiographic characteristics independently associated with the different specific CTA inaccuracies on both per-patient and per-segment levels.
Lower patient-level diagnostic accuracy for CTA has been reported amongst obese patients and in patients with poor heart-rate control resulting from images with low signal-to-noise ratio and motion artifacts (8,14,18–22). However, consistent with our prior investigation on this topic (14), we found that neither body-mass-index nor heart-rate is an independent predictor of patient-level diagnostic inaccuracy. Potential explanation for this counterintuitive finding may be our adaptive adjustment of tube-current to body-mass-index and protocol-stipulated prescription of beta-blockers. History of prior percutaneous coronary intervention surrogated higher disease prevalence amongst non-stented coronary segments in our studied population and independently conferred increased risk for patient-level FN-diagnosis, confirming the dependency of CTA accuracy on pre-test probability of CAD (23).
We and others have shown that high calcium scores are associated with lower patient-level specificity and NPV (5,19,20,23). Consistent with these reports, we found that a higher Agatston score independently increases the risk of patient-level false-positive diagnosis. Importantly, we also found that the absence of coronary calcification is an independent predictor of stenosis under-recognition. We have previously reported among our trial cohort that the absence of coronary calcification does not exclude obstructive CAD (24), and that overall segment-level diagnostic inaccuracy is lower in non-calcified arterial segments of lower disease prevalence than in calcified coronary artery segments (25). In this present study, we establish the absence of coronary calcification as an underappreciated independent risk-marker for false-negative diagnoses. Our results suggest that the absence of calcification may reduce reader’s vigilance for stenoses and that potential lesions - without obvious (i.e. calcified) evidence of atherosclerosis - may be dismissed as artifacts.
Despite technological advancement of scanners provisioning better spatial resolution, small vessels remain diagnostically challenging. Using contemporary 64-detector technology, segment-level sensitivity was lower amongst smaller segments (6). Our study extended beyond these unadjusted observations and demonstrated that smaller luminal caliber is an independent attributor to segment-level misdiagnoses. For the first time, we established arterial segment tortuosity as an independent predictor of segment-level diagnostic inaccuracy (Figure-1). Of note, cardiac motion degraded segment-level image quality which was associated with segment-level misdiagnosis but not after adjustment for other segment-level factors (Table-2). This may suggest that cardiac motion may be more tolerable in the absence of other features independently attributable for misinterpretation. Similarly, our findings also underscore that specific segment-level characteristics as reported, rather than segment location per se, are independent parameters affecting diagnostic accuracy.
Aside from intrinsic segment properties, intra-arterial luminal enhancement and conspicuity of juxta-arterial cardiac veins emerge as independent factors affecting segment-level accuracy. Previous studies had shown higher unadjusted segment-level sensitivity and PPV in patients achieving greater vascular contrast enhancement at the aortic root and origins of the left-main and right coronary arteries (26). Our adjusted segment-specific luminal-attenuation analyses affirm the importance of optimizing luminal contrast opacification to avert false-negative diagnoses. Conspicuity of juxta-arterial venous structures is first identified associated with segment-level misinterpretations. Consequential to partial volume averaging, focal luminal attenuation at the over-crossed arterial segment may appear artifactually lower or higher, potentially mimicking or masking stenosis, respectively (Figure-2). These pitfalls advocate for optimized contrast bolus timing to achieve high intra-arterial while minimizing venous contrast enhancement.
Figure 2.
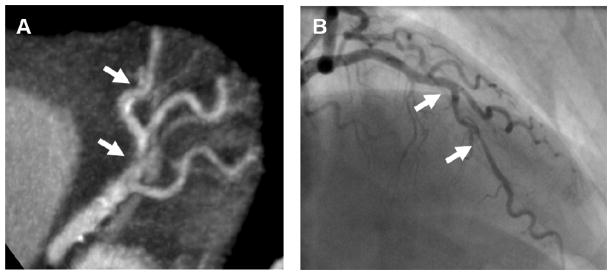
An example of conspicuous adjacent cardiac venous structure confounding coronary arterial interpretation. Panel A. Partial volume averaging effect by CT with adjacent cardiac vein mimicking focal non-calcified stenosis (first arrow) leading to false positive diagnosis. The distal arrow marks a false-negative diagnosis (CTA=15%, QCA=74% stenosis) masked by an adjacent cardiac vein. Panel B. Conventional angiography correlation revealing no stenosis at the proximal site but significant lesion at the distal site.
Study Limitations
The principal limitation of this investigation is the use of categorical decision points for determining the absence/presence of obstructive CAD, which – while almost invariably used for clinical investigations - may not reflect clinical practice. The use of specific thresholds to define disease is also associated with observer-bias that may affect diagnostic accuracy (23). Our study was performed in a selected cohort having clinical indications for invasive coronary angiography. Our findings may not necessarily generalize to lower-risk populations of which CTA is more intended for CAD assessment. As one of the largest multi-center investigations, the number of misdiagnosed patient is still modest, thus implications of our patient-level associations should be considered as hypothesis-generating, advocating for larger confirmative studies. Given the effort entailed in our detailed segment-level analysis and the large number of TN-segments within our entire multi-centre cohort, we pre-specified and analyzed segment-level features of diagnostic inaccuracy on only a randomly-selected TN-segment subset as comparative control. Our TN-segment characteristics may thus be subjected to potential selection bias. However, we verified that the proportional constitution of segments of the different major vessels within this randomly-selected TN-segment subset and the remainder of all non-selected TN-segments in our entire patient cohort was not significantly different (Appendix-2).
CONCLUSIONS
In this systematic evaluation of factors associated with diagnostic inaccuracy for coronary artery stenosis assessment by CTA compared to QCA in a multi-center diagnostic study, we observed pitfalls as well as clinical and CT angiographic features predictive of patient-level and segment-level CTA misdiagnoses. Particularly, our observations reveal the absence of coronary calcification as an independent risk-marker for under-recognition of stenoses defined by QCA. Specific segment-level CT angiographic features, notably small segment caliber, segment tortuosity, suboptimal intra-arterial contrast-enhancement and juxta-arterial venous conspicuity are independent predictors for segment-level misdiagnoses. Knowledge and appropriate considerations of these CT angiographic predictors of misdiagnosis may improve limitations awareness and accuracy in clinical CTA interpretation.
Supplementary Material
Figure 3.
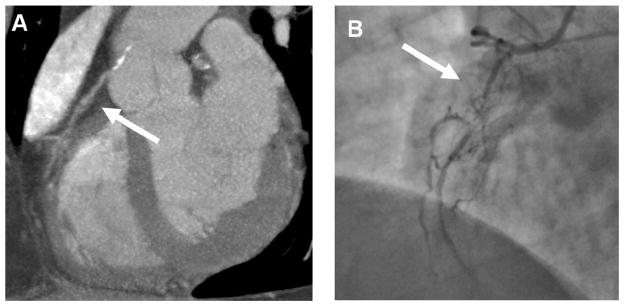
An example of poor contrast opacification leading to ambiguous lumen evaluation by CT. Panel A. Poor contrast filling of a proximal right coronary artery (arrow) does not allow visualization of a subtotal occlusion. Panel B. Corresponding invasive angiogram reveals severe lumen narrowing in the proximal right coronary artery (arrow).
Figure 4.
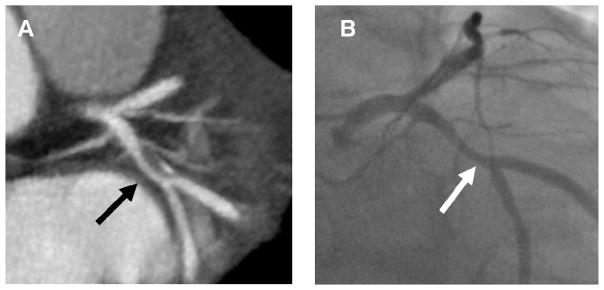
Effect of cardiac motion on CT interpretation. A minor motion artifact leads to slightly smaller lumen appearance by CT (arrow, Panel A) compared to conventional angiography (arrow, Panel B) resulting in a false positive diagnosis of obstructive coronary artery disease.
Acknowledgments
Funding/Support: This study was supported in part by National, Heart, Lung, and Blood Institute (RO1-HL66075-01 and HO1-HC-95162-01), the National Institute on Aging (R01-AG021570-01), the Donalds W. Reynolds Foundation, the Doris Duke Charitable Foundation, and Toshiba Medical Systems.
Dr. Raymond Yan was supported by Fellowship Awards from the Canadian Institutes of Health Research and the Detweiler Travelling Fellowship Award from the Royal College of Physicians and Surgeons of Canada.
ABBREVIATIONS
- QCA
quantitative coronary angiography
- CAD
coronary artery disease
- CTA
computed tomography angiography
- OR
odds ratio
- FN
false-negative
- FP
false-positive
- TP
true-positive
- TN
true-negative
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–16. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 2.Ringqvist I, Fisher LD, Mock M, et al. Prognostic value of angiographic indices of coronary artery disease from the Coronary Artery Surgery Study (CASS) J Clin Invest. 1983;71:1854–66. doi: 10.1172/JCI110941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1999;33:1756–824. doi: 10.1016/s0735-1097(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–70. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 5.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–32. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–44. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 7.Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–36. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 8.Schuetz GM, Zacharopoulou NM, Schlattmann P, Dewey M. Meta-analysis: noninvasive coronary angiography using computed tomography versus magnetic resonance imaging. Ann Intern Med. 2010;152:167–77. doi: 10.7326/0003-4819-152-3-201002020-00008. [DOI] [PubMed] [Google Scholar]
- 9.Fox K, Garcia MA, Ardissino D, et al. Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J. 2006;27:1341–81. doi: 10.1093/eurheartj/ehl001. [DOI] [PubMed] [Google Scholar]
- 10.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. Circulation. 2010;122:e525–55. doi: 10.1161/CIR.0b013e3181fcae66. [DOI] [PubMed] [Google Scholar]
- 11.Arbab-Zadeh A, Hoe J. Quantification of coronary arterial stenoses by multidetector CT angiography in comparison with conventional angiography methods, caveats, and implications. JACC Cardiovasc Imaging. 2011;4:191–202. doi: 10.1016/j.jcmg.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Miller JM, Dewey M, Vavere AL, et al. Coronary CT angiography using 64 detector rows: methods and design of the multi-centre trial CORE-64. Eur Radiol. 2009;19:816–28. doi: 10.1007/s00330-008-1203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery. American Heart Association Circulation. 1975;51:5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 14.Dewey M, Vavere AL, Arbab-Zadeh A, et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am J Roentgenol. 2010;194:93–102. doi: 10.2214/AJR.09.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann MH, Shi H, Schmitz BL, et al. Noninvasive coronary angiography with multislice computed tomography. Jama. 2005;293:2471–8. doi: 10.1001/jama.293.20.2471. [DOI] [PubMed] [Google Scholar]
- 16.Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;26:1482–7. doi: 10.1093/eurheartj/ehi261. [DOI] [PubMed] [Google Scholar]
- 17.Pugliese F, Mollet NR, Runza G, et al. Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol. 2006;16:575–82. doi: 10.1007/s00330-005-0041-0. [DOI] [PubMed] [Google Scholar]
- 18.Ropers U, Ropers D, Pflederer T, et al. Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol. 2007;50:2393–8. doi: 10.1016/j.jacc.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 19.Alkadhi H, Scheffel H, Desbiolles L, et al. Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur Heart J. 2008;29:766–76. doi: 10.1093/eurheartj/ehn044. [DOI] [PubMed] [Google Scholar]
- 20.Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–7. doi: 10.1016/j.jacc.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 21.Brodoefel H, Reimann A, Burgstahler C, et al. Noninvasive coronary angiography using 64-slice spiral computed tomography in an unselected patient collective: effect of heart rate, heart rate variability and coronary calcifications on image quality and diagnostic accuracy. Eur J Radiol. 2008;66:134–41. doi: 10.1016/j.ejrad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Dewey M, Hoffmann H, Hamm B. CT coronary angiography using 16 and 64 simultaneous detector rows: intraindividual comparison. Rofo. 2007;179:581–6. doi: 10.1055/s-2007-963112. [DOI] [PubMed] [Google Scholar]
- 23.Arbab-Zadeh A, Miller JM, Rochitte CE, et al. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification. The CORE-64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) International Multicenter Study. J Am Coll Cardiol. 2012;59:379–87. doi: 10.1016/j.jacc.2011.06.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gottlieb I, Miller JM, Arbab-Zadeh A, et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627–34. doi: 10.1016/j.jacc.2009.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vavere AL, Arbab-Zadeh A, Rochitte CE, et al. Coronary Artery Stenoses: Accuracy of 64-Detector Row CT Angiography in Segments with Mild, Moderate, or Severe Calcification--A Subanalysis of the CORE-64 Trial. Radiology. 2011;261:100–108. doi: 10.1148/radiol.11110537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cademartiri F, Maffei E, Palumbo AA, et al. Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur Radiol. 2008;18:576–83. doi: 10.1007/s00330-007-0773-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


