Abstract
The authors tested the feasibility and acceptability, and explored the outcomes, of 2 walking interventions based on ecological models among older adults living in retirement communities. An enhanced intervention (EI) was compared with a standard walking intervention (SI) among residents in 4 retirement facilities (N = 87 at baseline; mean age = 84.1 yr). All participants received a walking intervention including pedometers, printed materials, and biweekly group sessions. EI participants also received phone counseling and environmental-awareness components. Measures included pedometer step counts, activities of daily living, environment-related variables, physical function, depression, cognitive function, satisfaction, and adherence. Results indicated improvements among the total sample for step counts, neighborhood barriers, cognitive function, and satisfaction with walking opportunities. Satisfaction and adherence were high. Both walking interventions were feasible to implement among facility-dwelling older adults. Future studies can build on this multilevel approach.
Keywords: healthy aging, physical activity, built environment, pedometer, mapping
The population over age 65 in the U.S. is projected to double to 72 million by 2030 (Federal Interagency Forum on Aging-Related Statistics, 2010). Older adults face many health challenges including obesity, cardiovascular disease, hypertension, cancer, Type 2 diabetes, cognitive decline, depression, and arthritis that could be prevented, reversed, or controlled with regular physical activity (Federal Interagency Forum on Aging-Related Statistics, 2010; Physical Activity Guidelines Advisory Committee, 2008). Physical activity keeps healthy older adults living independently and is associated with recovery from functional limitations and reduced risk of falls (U.S. Department of Health and Human Services, 2008). However, physical activity levels are low and decrease throughout older adulthood (Federal Interagency Forum on Aging-Related Statistics, 2010). Recent data with objective monitoring indicate that only 2.5% of adults over age 60 meet physical activity recommendations (Troiano et al., 2008).
The public health impact of improving physical activity in the older adult population, even if physical activity stays below recommendations, could be significant (Drewnowski & Evans, 2001). While physical activity guidelines recommend that older adults achieve 150 min of moderate or 75 min of vigorous activity per week, they also state that any increase in activity will confer health benefits (U.S. Department of Health and Human Services, 2008). It is therefore important to identify physical activity interventions with wide reach that can be implemented and sustained in community settings. Home- and center-based exercise programs are common with older adults (King, 2001; van der Bij, Laurant, & Wensing, 2002). However, there is evidence that exercise in outdoor environments is beneficial (Frumkin, 2001) and that walking in particular is important for older adults. Walking is inexpensive, can serve as a form of transportation, can be done easily, has low risk of injury, and can protect against mobility loss (Cunningham & Michael, 2004; U.S. Department of Transportation, 2004). To improve walking among older adults, interventions need to occur in places where large numbers of seniors reside.
Assisted-living facilities and continuing-care retirement communities are important settings to consider for physical activity interventions. The scant evidence available suggests that individuals living in such facilities may be more inactive, be more frail, have more chronic conditions, and perform worse on measures of physical functioning than their community-dwelling peers (Kang, White, Hayes, & Snow, 2004; Mihalko & Wickley, 2003; Wert, Talkowski, Brach, & VanSwearingen, 2010). Activity programs are often understaffed, not designed to improve or maintain physical functioning (e.g., arts and crafts), and lack exercise equipment (Mihalko & Wickley, 2003). Such facilities may be an excellent naturally occurring community setting for applying approaches to increase walking based on ecological models. The ecological model promotes change by intervening at multiple levels of influence including the individual, interpersonal, and community (e.g., built environment) levels (Sallis, Owen, & Fisher, 2008). Embedding behavior-change strategies from social cognitive theory (Bandura, 1998) in the individual and interpersonal levels of the ecological model, which highlights the importance of the social and physical environment, provided the multilevel basis of the current interventions. There are no known previous interventions that have sought to use such multilevel approaches, including addressing the built environment, to promote physical activity among older adults. The purpose of the current study was to test the feasibility and acceptability of a novel, multilevel approach to increasing walking among residents of retirement facilities, conducting exploratory comparisons of lower and higher intensity multilevel interventions.
Design and Methods
Participants and Recruitment
Adults over the age of 65 years were recruited from four senior living facilities in the San Diego, CA, area. Participants were recruited from independent and assisted-living residences, depending on the site; those receiving nursing care were not included. Residents were eligible if they were not regularly walking (less than 30 min 3 days/week) and had had no falls within the past 3 months. Additional criteria were ability to walk (including those using a cane or walker), speak and read English, complete assessments, acquire their physician’s permission to participate in the study, complete the Timed Up & Go Test in less than 14 s (to ensure they were at low falls risk; Shumway-Cook, Brauer, & Woollacott, 2000), and provide informed consent.
Potential sites were identified through searches in a local senior-housing directory and on the Internet. The aim for the pilot was to assess feasibility in four sites that were supportive of the study and varied in size and location. The participating sites were all campus style (with a mixture of grounds and buildings as opposed to residential buildings only). The sites differed in size and neighborhood walkability (see Table 1). Two sites were larger (i.e., >400 residents) and two were smaller (<200 residents). Based on proximity to mixed land uses, having continuous sidewalks, and availability of safe road crossings, two sites were classified as having higher walkability and two sites as having lower walkability.
Table 1.
Site and Participant Characteristics
| Characteristic | Total sample | Site 1: SI | Site 2: EI | Site 3: EI | Site 4: SI | p |
|---|---|---|---|---|---|---|
| Site | ||||||
| number of residentsa | 400 | 503 | 133 | 160 | ||
| site size | large | large | small | small | ||
| recruitment from | independent only | independent and assisted | independent only | assisted only | ||
| walkability | lower | higher | lower | higher | ||
| Participants | ||||||
| baseline, n | 87 | 38 | 27 | 14 | 8 | NA |
| age, M (range) | 84.1 (69–98) | 82.3 (72–92) | 84.4 (69–98) | 87.7 (80–92) | 85.1 (75–97) | .01 |
| step counts/day,b M | 3,171.7 | 3,522.4 | 3,244.4 | 2,591.2 | 2,199 | .22 |
| women, n | 66 | 28 | 21 | 13 | 4 | .29 |
| white, n | 84 | 37 | 27 | 14 | 6 | .05 |
| completed college, n | 47 | 29 | 15 | 1 | 2 | .00 |
| BMI, M (SD) | 26.3 (3.9) | 25.4 (2.9) | 27.5 (4.9) | 27.5 (3.6) | 23.9 (3.6) | .05 |
| medical conditions, M (SD) | 1.4 (1.0) | 1.3 (.8) | 1.3 (1.2) | 1.6 (1.2) | 1.9 (1.2) | .48 |
| SPPB score, M (SD) | 8.1 (2.5) | 9.1 (2.2) | 7.8 (2.7) | 6.4 (2.1) | 7.7 (2.4) | .01 |
| months at site, M (SD) | 59.5 (49.4) | 74.2 (53.3) | 52.8 (47.4) | 55.0 (38.0) | 13.9 (9.8) | .02 |
| use a cane or walker (n) | 29 | 8 | 8 | 8 | 5 | .01 |
Note. EI = enhanced intervention; SI = standard intervention; BMI = body-mass index; SPPB = Short Physical Performance Battery. p values are for tests of differences between sites.
Site numbers do not include Alzheimer’s care residents living at sites.
Using the raw, untransformed variable.
A similar process to recruit residents was followed at each site. Study information flyers were mailed to all potential eligible residents (all independent-living or assisted-living residents, depending on site) inviting them to attend a scheduled informational meeting. Eligible and willing participants completed informed consent during the informational meeting. The study was approved by the institutional review boards at the relevant institutions.
Study Design
Intervention Design
We documented the feasibility and acceptability of two walking interventions: a more intensive, multilevel approach (which includes more intervention at the individual and built-environment levels; termed the enhanced intervention [EI]) and a less intensive, standard intervention (SI) that did not address the built environment or provide tailored counseling. The purpose was to assess whether inclusion of the additional multilevel components was feasible and acceptable and to explore whether the EI would yield additional improvements in walking as posited by the ecological model.
A quasi-experimental site-randomized design was used to test the EI. To ensure that a balance of site types were randomized to each condition, sites were matched into pairs based on site size and walkability and then randomly assigned to condition.
Intervention Development and Components
Development of the individual, interpersonal, and environmental intervention components was based on theory (ecological models and social cognitive theory [SCT]), literature reviews, and a prepilot study that tested the intervention with 12 participants at one site. The prepilot demonstrated the ability to develop and implement a multilevel intervention in a 2-week study (Rosenberg et al., 2009). Table 2 describes which components were delivered to each intervention group. Constructs from SCT were incorporated into the individual and interpersonal levels of the intervention for both SI and EI participants. The enhanced multilevel walking intervention included aspects from all three levels of the ecological model—the individual, interpersonal, and community (built-environment) levels. More individual tailoring for goal setting and problem solving was accomplished through phone-based counseling. The built environment was targeted through increasing participants’ awareness of ways the on- and off-site buildings and grounds could support walking. Two main components promoted changes in environmental awareness. First, site-tailored walking-route maps were given to participants (for more details on the mapping process, see Rosenberg et al., 2009). Participants in the EI were given one overview map of the site (that highlighted three or four color-coded walking routes), individual maps detailing each color-coded route, and a walking-route map of the local area. Second, handouts with step counts to and from various destinations around the site and in the local area were provided along with group discussions centered on how participants could attain more steps while accomplishing daily activities (e.g., by taking the longest route to the cafeteria for meals rather than the shortest).
Table 2.
Intervention Components Mapped to Underlying Theoretical Constructs
| Ecological model level of influence | Specific components | Underlying construct | Underlying theory | SI | EI |
|---|---|---|---|---|---|
| Individual | Pedometers and step-count logs | Self-monitoring Feedback |
SCT | X | X |
| Goal setting | Goal setting | SCT | X | X | |
| Progress charts | Self-monitoring | SCT | X | X | |
| Printed educational materials (e.g., benefits and barriers to walking, safety information) | Outcome expectancies and expectations Self-efficacy |
SCT | X | X | |
| Biweekly tailored phone counseling | Self-regulation Problem solving Goal setting |
SCT | X | ||
| Interpersonal | Biweekly group meetings | Social support Modeling Problem solving |
SCT | X | X |
| Community level (e.g., built environment) | Environmental awareness (e.g., walking route maps, handouts of onsite step counts) | Changing environment perceptions | EM | X |
Note. SI = standard intervention; EI = enhanced intervention; SCT = social cognitive theory; EM = environmental model.
The common goal for both groups was to increase steps on a biweekly basis by a maximum of 5–10% from the previous week’s step count. Overall, everyone was encouraged to increase their step count by at least 1,000 steps. The range for health benefits among older adults has been suggested to be 5,000–11,000 steps a day, depending on health condition, based on expert opinion (Tudor-Locke & Bassett, 2004; Tudor-Locke, Hart, & Washington, 2009).
Measures
Participants completed measures at baseline and 3 months after the intervention period. Self-reported measures were completed through written surveys. Performance measures were conducted by trained research assistants.
Walking
The New Lifestyles NL-800 pedometer served as the main outcome in addition to an intervention tool for participants. The NL-800 has a large display size that is easy for older adults to read and a 7-day memory so that step counts could be retrieved by study researchers at measurement points. A similar version of this pedometer (the NL-2000) has been validated against the pedometer considered the most accurate and reliable, the Yamax Digi-walker, and did not have statistically significant differences in values obtained among adults (Schneider, Crouter, & Bassett, 2004). The NL-800 operates using piezoelectric technology, making it potentially less sensitive to errors than spring-levered pedometers, which have been criticized for underestimating steps among those with the slowest gait speeds, such as older adults (Crouter, Schneider, & Bassett, 2005; Cyarto, Myers, & Tudor-Locke, 2004; Storti et al., 2008).
Functional Performance
Functional performance was measured with the Short Physical Performance Battery (SPPB; Guralnik et al., 1994), which evaluates balance, gait, strength, and endurance by examining the ability to stand with the feet together in the side-by-side, semitandem, and tandem positions; time to walk 8 ft; and time to rise from a chair and sit back down five times. This test has been related to mortality, disability, and nursing-home admission (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995; Guralnik, et al., 1994). The SPPB was administered by trained research assistants at the residential facilities during the measurement visits at baseline and 12 weeks.
Activities of Daily Living
Participation in activities of daily living was assessed with nine self-reported items from the Late Life Function and Disability Instrument: Function Component (Haley et al., 2002). The original instrument consisted of 32 items, but only the nine items that were relevant to walking and older adults living in facilities were included. Response options ranged from 1 (cannot do) to 5 (no difficulty). The original measure has been shown to be reliable and valid in community-dwelling adults over age 60 (Haley et al., 2002). Responses on all items were averaged such that higher scores indicated better ability to perform activities of daily living. At baseline and 12 weeks, the internal consistency of the scale was Cronbach’s α = .90 and .88, respectively.
Environment-Related Measures
Neighborhood barriers were measured with a self-report tool developed by study researchers consisting of five items assessing whether hills, crime, traffic, unsafe street crossings, or lacking places to walk were barriers to walking. Response options ranged from 1 (never a barrier) to 5 (always a barrier). Responses to all items were averaged to represent the scaled score. The internal consistency of the scale (measured with Cronbach’s α) was .78 at baseline and 12 weeks.
Satisfaction with the walking environment was measured with three items assessing satisfaction with the walking and exercise opportunities at their site, in their local area, and their access to safe walking routes. Response categories ranged from 1 (extremely dissatisfied) to 5 (extremely satisfied). The responses for all three items were averaged. Cronbach’s α for the satisfaction subscale was .74 at baseline and .82 at 12 weeks.
Depression
The self-report Geriatric Depression Scale Short Form (GDS) was used to assess depression. The scale consists of 15 items answered yes or no (Yesavage et al., 1982). Research has shown excellent measurement properties for the GDS in screening for major depression as compared with the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, with scores greater than 5 indicating probable depression and scores over 10 indicating depression (Lyness et al., 1997).
Cognitive Function
Cognitive functioning was measured with three paper-and-pencil tests: the Symbol Search subtest of the Weschler Adult Intelligence Scale (WAIS-III), Trails A, and Trails B. Raw scores on Trails B and Symbol Search were used as outcome variables.
Satisfaction and Adherence
To assess whether the intervention was feasible and acceptable to participants, we measured adherence and satisfaction. Adherence was measured using group session attendance and completion of phone calls. An index was computed by dividing the number of sessions attended or phone calls completed (from attendance logs kept by researchers) by the total number provided in the study (total of 11 phone and group sessions for EI, total of 6 group sessions for SI).
Satisfaction with the interventions was measured at the 3-month time point with seven self-reported items (11 for EI participants). All participants rated the usefulness of handouts on a scale from 1 (not useful at all) to 5 (extremely useful) and the usefulness/helpfulness of study components on a scale from 1 (did not use) to 4 (very helpful), including step logs, goal setting, pedometers, and group sessions. Four additional satisfaction items for all participants were overall how satisfied are you with this study for helping you increase your walking (1 = not at all satisfied, 5 = extremely satisfied), how confident are you that you could continue to increase your steps on your own (1 = not at all confident, 5 = extremely confident), do you plan to continue walking at your current level or higher (0 = no, 1 = maybe/don’t know, 2 = yes), and would you recommend the study to a friend or fellow resident (1 = no, 2 = maybe, 3 = yes). EI participants also rated walking-route maps, step-count information sheets, and phone calls.
Demographic Characteristics
Self-reported items at baseline assessed gender, age, length of time lived at the site, health status (count of reported chronic conditions), education level (dichotomized to represent having a college degree or not), and height and weight. Body-mass index (BMI) was calculated using the formula weight (lb)/[height (in.)]2 × 703.
Analysis
Because the focus of this pilot study was acceptability and feasibility, statistical analyses of outcome measures were considered exploratory. Differences between the SI and EI conditions on each outcome were assessed using analysis of covariance (ANCOVA) models. Condition was the independent variable, and each outcome variable at posttest was used as the dependent variable, with the baseline outcome value as a covariate. Only eta-squared and p values were reported. Because of the limited sample size, only significant demographic covariates that differed between groups were retained in final models. Within-group changes for outcomes were tested using paired t tests.
The following variables were transformed to improve normality of distributions: step counts (square root), depression (log10), BMI (inverse), and neighborhood barriers (inverse). In tables, the back-transformed means are presented.
All analyses were conducted using SPSS version 15.0 (SPSS Inc., Chicago, IL). All reported p values were for two-sided tests, with effects considered statistically significant at p < .05.
Results
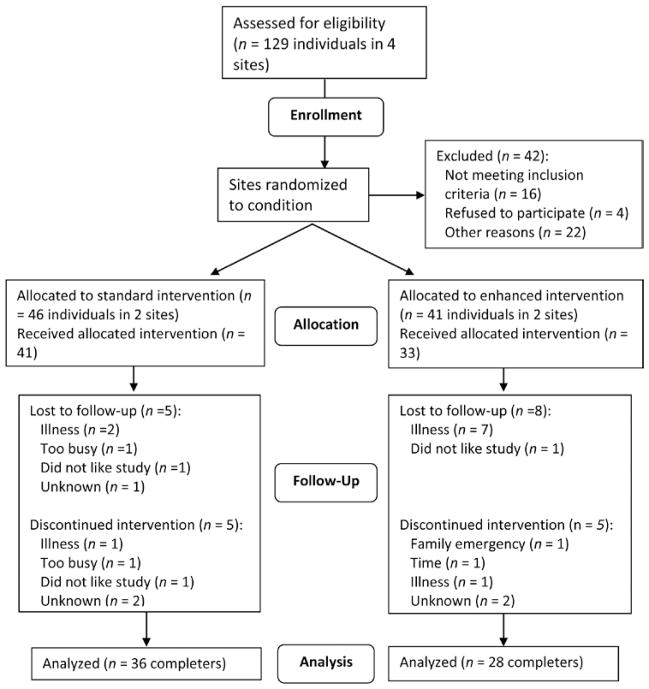
A total of 87 participants provided informed consent and completed baseline measurements. At 3-month follow-up, 64 participants completed measurements (see Figure 1 for reasons for dropout). The percent retained in the study was 74% overall, including seven dropouts due to health problems. Study noncompleters had lower baseline physical functioning and step counts and were more likely to be classified as overweight than completers. There were no significant differences in attrition by condition and no study-related adverse events.
Figure 1.
CONSORT diagram for the study (Altman, Schulz, & Moher, 2001).
Demographic characteristics of the sample are displayed in Table 2. The average, untransformed, baseline step count was 3,171.7 (median = 2,931.0, 25th percentile = 1,739.0, 75th percentile = 4,530.5). There were baseline between-groups differences for physical performance, having a college degree, and BMI. Thus, analyses were adjusted for these variables.
Intervention Feasibility and Acceptability
Adherence to intervention activities did not differ between groups. Among the total sample, adherence was 77%. Participants attended on average 4.55 of six group sessions, with 56.8% of participants attending five or more sessions and 74.4% attending four or more group sessions. Among EI participants, 78.8% completed at least four of five phone calls. Satisfaction with the study was high overall for both intervention groups (see Table 3). The highest rated components were pedometers and step logs. Among EI participants, step-count information sheets and phone calls were most highly rated.
Table 3.
Participant-Reported Satisfaction With the Study and Its Components
| Total sample % rating more highly | SI, n = 36 | EI, n = 28 | |
|---|---|---|---|
| Intervention component | |||
| handoutsa | 91.7 | 83.8 | 100.0 |
| step logb | 95.3 | 94.4 | 96.4 |
| goal settingb | 71.9 | 66.7 | 78.6 |
| walking plannerb | 59.7 | 47.2 | 71.4 |
| progress chartb | 77.8 | 72.2 | 85.2 |
| pedometersb | 98.5 | 100.0 | 96.4 |
| groupsa | 92.1 | 86.1 | 96.4 |
| overall program to increase walkinga | 98.4 | 100.0 | 96.4 |
| will continue to walk at current levelc | 98.4 | 100.0 | 96.4 |
| will continue increasing stepsd | 89.2 | 91.7 | 85.7 |
| would recommend the program to a friendc | 93.7 | 94.4 | 92.6 |
| Enhanced intervention components | |||
| step count information sheetsb | n/a | n/a | 85.7 |
| maps of residenceb | n/a | n/a | 74.1 |
| maps of neighborhoodb | n/a | n/a | 55.6 |
| phone callsa | n/a | n/a | 96.4 |
Note. Note. EI = enhanced intervention; SI = standard intervention. Significance test for the difference between standard and enhanced intervention groups.
Percent reporting somewhat, very, or extremely useful.
Percent reporting helpful or very helpful.
Percent reporting yes.
Percent mean reporting somewhat, very, or extremely confident.
Outcomes
We explored whether there were between-groups differences between the SI and EI groups using data on those completing the study only. No between-groups outcome differences were statistically significant (see Table 4) when using completer data; intent-to-treat analyses were also conducted, with no differences in findings (data not shown). Data were merged to explore within-group effects on the outcomes (see Table 4). There were significant improvements overall for step counts, t(1, 54) = 3.12, p < .01; Trails B, t(1, 61) = −2.77, p < .01; neighborhood barriers, t(1, 59) = 3.88, p < .001; and satisfaction with walking environment, t(1, 60) = 3.52, p < .01 (see Table 4).
Table 4.
Outcomes for Between- and Within-Group Effects (Study Completers Only, N = 64)
| Between-Groups Comparisons at 12 Weeksa
|
Within-Group Changesb
|
|||||
|---|---|---|---|---|---|---|
| Standard intervention, M (CI) | Enhanced intervention, M (CI) | Partial η2 | Baseline, M | 12-week follow-up, M | Cohen’s d | |
| Steps/day | 4,044.96 (3,501.09–4,628.08) | 4,252.34 (3,655.41–4,894.40) | .005 | 3,404.59* | 3,938.92 | .42 |
| Activities of daily living | 3.75 (3.60–3.90) | 3.95 (3.76–4.13) | .04 | 3.73 | 3.79 | .15 |
| Physical function | 8.50 (7.94–9.04) | 8.25 (7.60–8.91) | .005 | 8.54 | 8.32 | .14 |
| Depression | 2.45 (3.76–4.13) | 2.09 (1.78–2.45) | .04 | 2.45 | 2.32 | .14 |
| Trails B | 136.27 (117.52–155.02) | 117.74 (95.09–140.38) | .03 | 154.28* | 131.12 | .35 |
| Symbol Search | 21.21 (19.32–23.10) | 18.74 (16.43–21.06) | .04 | 18.24 | 19.59 | .25 |
| Satisfaction With Walking Opportunities Scale | 3.89 (3.60–4.18) | 3.90 (3.56–4.24) | .00 | 3.51* | 3.90 | .45 |
| Neighborhood Barriers Scalec | 1.33 (1.19–1.51) | 1.57 (1.35–1.87) | .05 | 1.75* | 1.42 | .50 |
ANCOVA was used to test between-groups differences at 12 weeks. Analyses adjusted for completing college, physical functioning, body-mass index, and the baseline value of each outcome.
Paired t tests were conducted for tests of within-group differences from baseline to 12 weeks.
Higher numbers indicate more barriers.
p < .01.
Discussion
The current study assessed the feasibility and acceptability of two walking interventions: a lower-intensity standard intervention and a higher-intensity multilevel intervention that included environmental awareness and telephone counseling components to encourage walking in an older facility-dwelling population. We also explored the outcomes of the interventions. Adherence to study meetings and phone calls was good, suggesting that both approaches were feasible to implement in retirement facilities among older adults with an average age of just over 84 years. In addition, both interventions were highly rated by participants, suggesting that the walking interventions were acceptable to participants. We explored differences in outcomes between the two intervention groups and found no statistically significant differences on the outcomes (steps, mental health, physical function, cognitive function, environment variables).
Pre- and posttest results indicated improvements in step counts (the main outcome) for both intervention groups. Step counts improved over time for the overall sample by about 500 steps, which represents a 10–15% increase from a low baseline. Based on data suggesting that healthy adults walk about 100 steps in 1 min, the increase observed in our study translates to approximately 5 min of walking per day (Tudor-Locke, Sisson, Collova, Lee, & Swan, 2005), though it is likely that very old adults walk less than 100 steps/min. It is difficult to compare current results with those of previous pedometer studies because of the advanced age of participants in the current study. A 4-month community-based intervention had a 268-step improvement among those over 85 (Croteau & Richeson, 2006). Other studies with a lower mean age than ours (70–75 years) found 818 (Talbot, Gaines, Huynh, & Metter, 2003) and 848 (Fitzpatrick et al., 2008) steps/day increases over 3–4 months. The data provided in our study can provide a helpful comparison for future studies.
There is no standard pedometer recommendation for older adults in their 70s through 90s to determine the clinical significance of the step-count changes observed in our study. It is likely that had participants not been exposed to the intervention, steps would have declined, as is the natural inclination with increased age. Tudor-Locke et al. (2009) examined pedometer studies in older adults and reported observed values ranging from 2,000 to 9,000 steps/day in the older adult population (age range 50–94). Pal, Chang, and Ho (2011) recently showed that giving overweight and obese middle-aged women a step target of 10,000 per day along with a pedometer was more effective than asking them to walk 30 min per day. Having a target for older adults to achieve could be highly beneficial. Indeed, in our study, the older adults wanted a long-term goal to work toward, but an 8,000+-step recommendation seemed dauntingly high (considering that the average baseline step count was just over 3,000 steps/day). Also important was that the target of a 10% increase in steps from the previous week meant that everyone was working on an individual rather than a common target goal. This did not help with group cohesion or progression toward a long-term goal. Furthermore, for someone with 5,000 steps/week, a 500-step increase was not a realistic goal in this age group. Future studies should aim to test various goal-setting approaches to determine which is the most effective for an older adult population.
Both groups rated intervention components highly. In particular, handouts, step logs, pedometers, and groups were rated by 90% or more of the total sample as being at least somewhat useful. The lowest ratings were for walking planners, which were an optional study component given to participants to help them plan when and where they were going to obtain their extra steps. Goal setting was also rated less highly. This finding is in congruence with researcher observations mentioned previously that a 10% goal did not seem very effective. This lends further support to the need to further examine improved ways of setting goals for step counts in older adult populations. Among EI participants, phone calls were the highest rated component, followed by step-count information sheets.
We had an average attendance of 77% for the six intervention sessions. Participants were phoned by study staff with reminders to attend group sessions, which could have helped bolster attendance. All group sessions were held at the target retirement facility to eliminate travel barriers. One of the main reasons for missing sessions was illness, something that is unavoidable in older adult populations. Overall, attendance data suggested that the intervention was feasible to conduct in a group-based setting at a retirement facility.
The finding that perceptions of the environment changed whether they were targeted in the intervention strengthens the importance of addressing the built environment and supports previous findings that environmental features are related to physical activity among older adults (Cunningham & Michael, 2004; Yen, Michael, & Perdue, 2009). Our understanding of walkability for seniors was challenged by our study findings. The large SI site had few walking paths around the grounds but many long indoor corridors. Participants in this site were content to walk indoors, similar to benefits found in mall-walking studies (Culos-Reed, Stephenson, Doyle-Baker, & Dickinson, 2008). It is possible that with a longer intervention program, participants’ walking behavior could have been shaped to walk around the grounds and eventually off site.
Our findings are not conclusive regarding whether the individual and environmental components of the multilevel intervention are necessary. There are costs involved in each of these components, and the EI group did not appear to perform any better than the SI group. The mapping component of this study could become an automated process and be quite inexpensive compared with the cost of individual phone counselors, making the environmental component worthy of further study. It is difficult to detect differences between two active interventions, and this pilot study was known to be underpowered. There are several other potential reasons for not finding statistically significant group differences, particularly regarding the environmental components. One reason is that the SI participants did not receive the additional maps and step-count materials, but they reported becoming more aware of environmental supports as they walked more in their environment and experienced self-discovery of step distances and locations. The findings that neighborhood barriers and environment satisfaction improved for everyone confirms this, but it may have served to reduce the distinction between the study conditions. An additional noted difference was the high level of engagement and involvement in the study among participants at the large SI site. Our study lacked a measure of participant engagement in the intervention, including group cohesiveness and staff support, so we could not adjust for such site differences. These are potential moderators of the intervention that should be measured in future studies.
Another reason for the lack of differences between groups is that the EI may not have been an adequate test of the multilevel approach, as it did not include physical or policy changes at the community level of influence due to funding limitations. Rather, the EI approach focused on educating participants about how to use their environment to walk more, be aware of supportive features of their environment for walking, and become more aware of places they could walk on and off site. Additional components such as improved maintenance of walking routes, policies to support walking groups or active excursions, or placing signs encouraging residents to walk may have improved the impact of the EI. Future studies can determine the efficacy of multilevel walking interventions for older adults, along with increased emphasis on the environmental-level interventions.
Several secondary outcomes were explored, including activities of daily living, depression, cognitive function, and physical function. Each of these was feasible to obtain and generally showed little change from baseline to 12 months. There were improvements among the sample for one of the cognitive-functioning indicators, Trails B, which has been demonstrated in other studies examining the impact of physical activity on cognitive function (e.g.,: Baker et al., 2010).
As this was a pilot feasibility study, limitations of our study included a small sample size; inclusion of only four sites, making us unable to account for clustering; lack of a true control group; and use of some measures that were developed for the current study. Because of our small sample size statistical tests were underpowered to detect these differences. Another limitation of the study was that the residents living in the retirement facilities were predominantly White non-Hispanic, and based on the cost of living at such sites, had higher income than the general population of older adults. Finally, we did not collect information on adherence to keeping step logs and using the pedometers. Anecdotally, when researchers visited the sites for group sessions to check step count logs, compliance with both of these components were high. Strengths included the use of objective measures for physical activity and physical function and a novel intervention approach aiming to intervene at multiple levels of influence. The intervention encouraged unsupervised, unstructured walking for very old adults, with no adverse events, whereas previous studies focused on group or supervised exercise. Future studies should aim to use longer intervention periods with extended follow-up, focus on altering community policies and environments to facilitate walking, and use a comparison condition that is not a physical activity intervention. They should aim to use a true group-randomized trial design with sufficient sites randomized to formally test outcome differences between the interventions. Randomizing more sites to study conditions would allow for a multilevel modeling approach to the intervention evaluation that could include site-level and individual-level variables.
Conclusion
Two types of walking interventions were feasible and acceptable among older adults living in retirement facilities. Both interventions used components that were highly rated as useful, including pedometers and step logs. Future studies should incorporate such approaches and build on them. The results of this study suggest that more research is needed to determine whether addressing built-environment variables and personalized counseling to promote physical activity among facility-dwelling older adults could be beneficial.
Acknowledgments
This work was supported by the National Institutes of Health National Heart, Lung, and Blood Institute [Grant #F31HL090071-0 to D.R.] and the Stein Institute for Research on Aging, the University of California, San Diego (to J.K.).
Contributor Information
Dori E. Rosenberg, Group Health Research Institute, Group Health Cooperative Seattle, WA
Jacqueline Kerr, Dept. of Family and Preventive Medicine, University of California, San Diego, La Jolla, CA.
James F. Sallis, Dept. of Family and Preventive Medicine, University of California, San Diego, La Jolla, CA
Gregory J. Norman, Dept. of Family and Preventive Medicine, University of California, San Diego, La Jolla, CA
Karen Calfas, Dept. of Family and Preventive Medicine, University of California, San Diego, La Jolla, CA.
Kevin Patrick, Dept. of Family and Preventive Medicine, University of California, San Diego, La Jolla, CA.
References
- Altman DG, Schulz KF, Moher D. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Annals of Internal Medicine. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan A, Craft S. Effects of aerobic exercise on mild cognitive impairment. Archives of Neurology. 2010;67:71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology & Health. 1998;13:623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- Croteau K, Richeson NE. A matter of health: Using pedometers to increase the physical activity of older adults. Activities, Adaptation and Aging. 2006;30:37–47. doi: 10.1300/J016v30n02_03. [DOI] [Google Scholar]
- Crouter SE, Schneider PL, Bassett DR., Jr Spring-levered versus piezo-electric pedometer accuracy in overweight and obese adults. Medicine and Science in Sports and Exercise. 2005;37:1673–1679. doi: 10.1249/01.mss.0000181677.36658.a8. [DOI] [PubMed] [Google Scholar]
- Culos-Reed SN, Stephenson L, Doyle-Baker PK, Dickinson JA. Mall walking as a physical activity option: Results of a pilot project. Canadian Journal on Aging. 2008;27:81–87. doi: 10.3138/cja.27.1.81. [DOI] [PubMed] [Google Scholar]
- Cunningham GO, Michael YL. Concepts guiding the study of the impact of the built environment on physical activity for older adults: A review of the literature. American Journal of Health Promotion. 2004;18:435–443. doi: 10.4278/0890-1171-18.6.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyarto EV, Myers AM, Tudor-Locke C. Pedometer accuracy in nursing home and community-dwelling older adults. Medicine and Science in Sports and Exercise. 2004;36:205–209. doi: 10.1249/01.MSS.0000113476.62469.98. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults: Summary. Journal of Gerontology. 2001;56:M89–M94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2010: Key indicators of well-being. Washington, DC: Author; 2010. [Google Scholar]
- Fitzpatrick SE, Reddy S, Lommel TS, Fischer JG, Speer EM, Stephens H, Johnson MA. Physical activity and physical function improved following a community-based intervention in older adults in Georgia senior centers. Journal of Nutrition for the Elderly. 2008;27:135–154. doi: 10.1080/01639360802060223. [DOI] [PubMed] [Google Scholar]
- Frumkin H. Beyond toxicity: Human health and the natural environment. American Journal of Preventive Medicine. 2001;20:234–240. doi: 10.1016/S0749-3797(00)00317-2. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. The New England Journal of Medicine. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Haley SM, Jette AM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, Ashba J. Late Life Function and Disability Instrument: II. Development and evaluation of the function component. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2002;57:M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- Kang K, White K, Hayes W, Snow C. Agility and balance differ between older community and retirement facility residents. Journal of Applied Gerontology. 2004;23:457–468. doi: 10.1177/0733464804271275. [DOI] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. Journal of Gerontology. 2001;56:M36–M46. doi: 10.1093/geronb/56.1.S36. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Archives of Internal Medicine. 1997;157:449–454. doi: 10.1001/archinte.1997.00440250107012. [DOI] [PubMed] [Google Scholar]
- Mihalko SL, Wickley KL. Active living for assisted living: Promoting partnerships within a systems framework. American Journal of Preventive Medicine. 2003;25:193–203. doi: 10.1016/S0749-3797(03)00184-3. [DOI] [PubMed] [Google Scholar]
- Pal S, Cheng C, Ho S. The effect of two different health messages on physical activity levels and health in sedentary overweight, middle-aged women. BMC Public Health. 2011;11:204. doi: 10.1186/1471-2458-11-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee report, 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Rosenberg D, Kerr J, Sallis JF, Patrick K, Moore DJ, King A. Feasibility and outcomes of a multilevel place-based walking intervention for seniors: A pilot study. Health Place. 2009;15(1):173–179. doi: 10.1016/j.healthplace.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Schneider PL, Crouter SE, Bassett DR. Pedometer measures of free-living physical activity: Comparison of 13 models. Medicine and Science in Sports and Exercise. 2004;36:331–335. doi: 10.1249/01.MSS.0000113486.60548.E9. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical Therapy. 2000;80:896–903. [PubMed] [Google Scholar]
- Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR, Kriska AM. Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and Science in Sports and Exercise. 2008;40:59–64. doi: 10.1249/mss.0b013e318158b504. [DOI] [PubMed] [Google Scholar]
- Talbot LA, Gaines JM, Huynh TN, Metter EJ. A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: A preliminary study. Journal of the American Geriatrics Society. 2003;51:387–392. doi: 10.1046/j.1532-5415.2003.51113.x. [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Bassett DR., Jr How many steps/day are enough? Preliminary pedometer indices for public health. Sports Medicine (Auckland, NZ) 2004;34:1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Hart TL, Washington TL. Expected values for pedometer-determined physical activity in older populations. The International Journal of Behavioral Nutrition and Physical Activity. 2009;6:59. doi: 10.1186/1479-5868-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C, Sisson SB, Collova T, Lee SM, Swan PD. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Canadian Journal of Applied Physiology. 2005;30:666–676. doi: 10.1139/h05-147. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008 physical activity guidelines for Americans. Washington, DC: Author; 2008. [Google Scholar]
- U.S. Department of Transportation. Stepping out: Mature adults: Be healthy, Walk safely. Washington, DC: Author; 2004. [Google Scholar]
- van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: A review. American Journal of Preventive Medicine. 2002;22:120–133. doi: 10.1016/S0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- Wert DM, Talkowski JB, Brach J, VanSwearingen J. Characteristics of walking, activity, fear of falling, and falls in community-dwelling older adults by residence. Journal of Geriatric Physical Therapy. 2010;33:41–45. [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventive Medicine. 2009;37:455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]